Chapter 10 AdrenoceptorActivating Other Sympathomimetic Cao Yongxiao Department

- Slides: 33
Chapter 10 Adrenoceptor-Activating & Other Sympathomimetic Cao Yongxiao 曹永孝 Department of Pharmacology yxy@xjtu. edu. cn; 029 -82655140 http: //pharmacology. xjtu. edu. cn 1
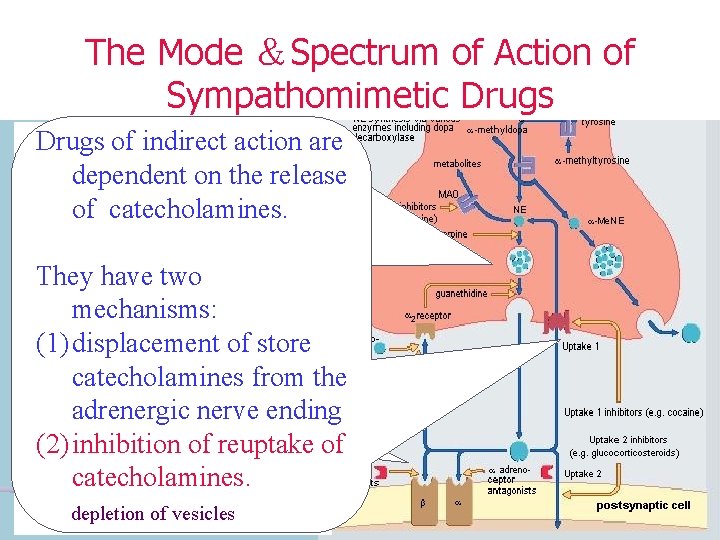
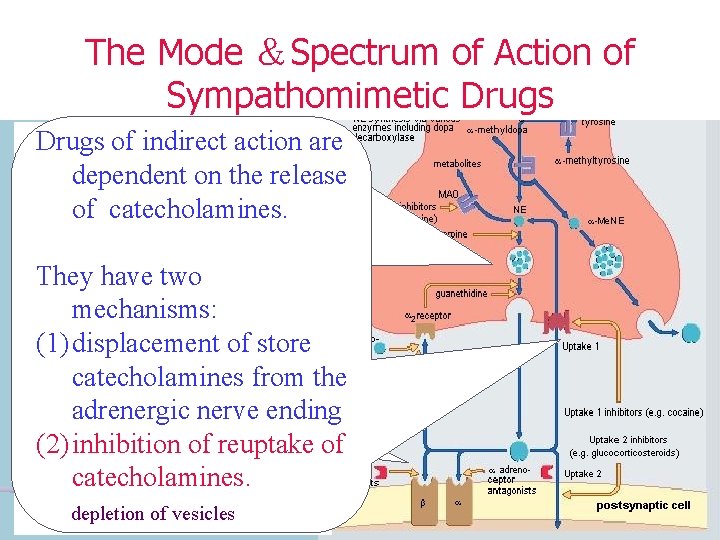
The Mode &Spectrum of Action of Sympathomimetic Drugs of indirect action are Drugs of indirect action Sympathomimetics dependent on the release are dependent on the are grouped by action of catecholamines. release of mode. catecholamines. They have two mechanisms: They have either of two (1) displacement of store Some of these drugs different mechanisms: catecholamines from the act by direct mode, (1) displacement of store adrenergic nerve ending ie, they activate catecholamines from the (2) inhibition of reuptake of adrenoceptors. adrenergic nerve ending. catecholamines. depletion of vesicles
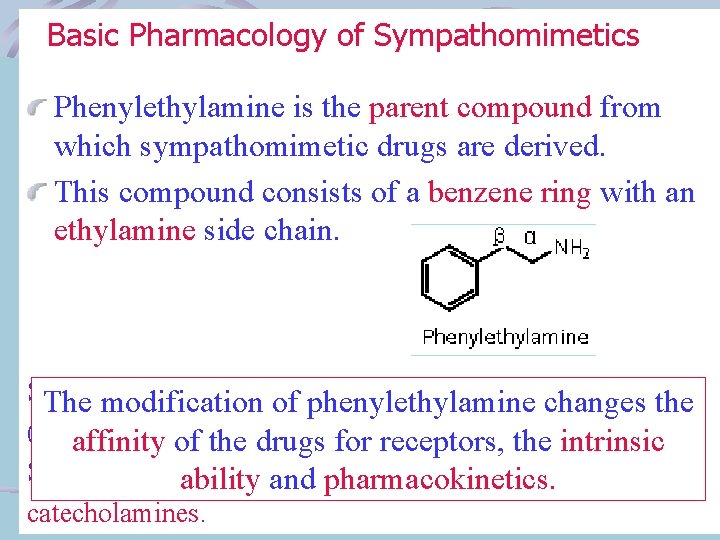
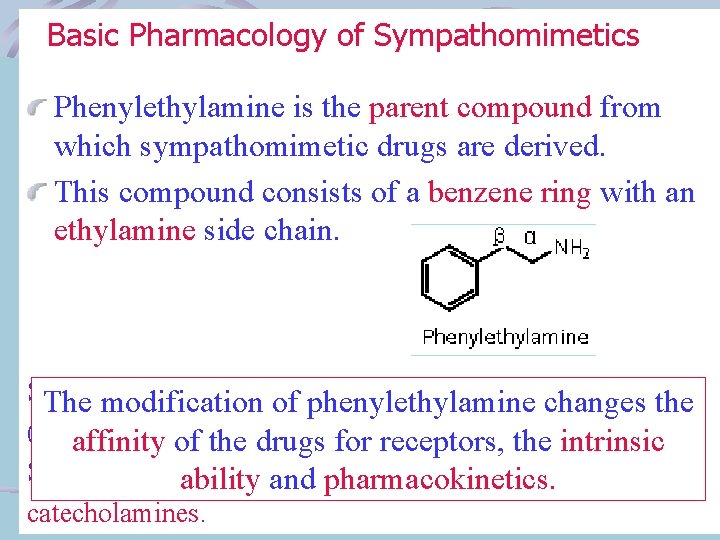
Basic Pharmacology of Sympathomimetics Phenylethylamine is the parent compound from which sympathomimetic drugs are derived. This compound consists of a benzene ring with an ethylamine side chain. Substitutions may be made (1) on the terminal amino group, The modification of phenylethylamine changes the (2) on the benzene ring, (3) on the α or β-carbons. affinity of the drugs for receptors, the intrinsic Substitution by -OH group at the 3 and 4 positions yield ability and pharmacokinetics. catecholamines.
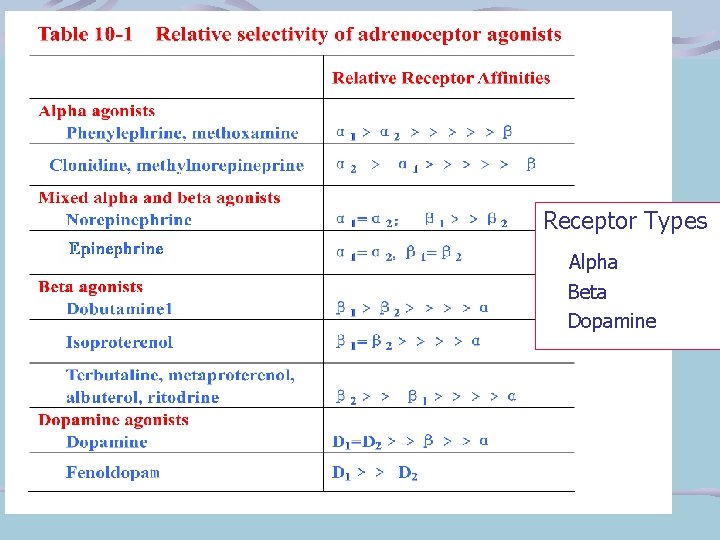
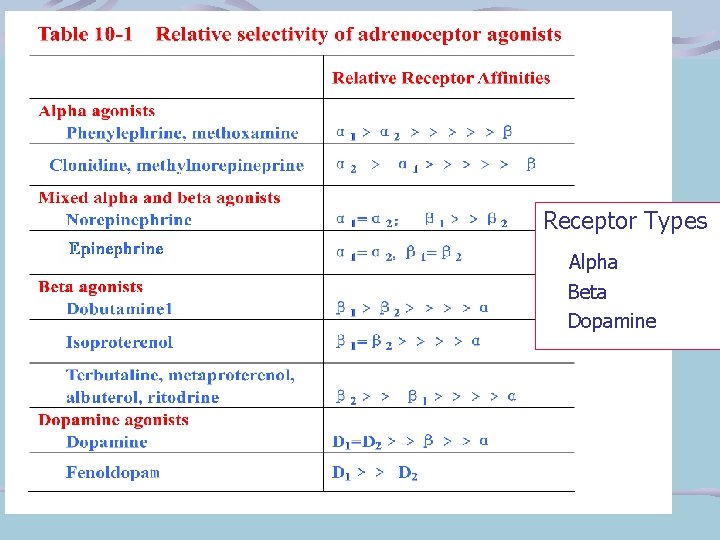
Receptor Types Alpha Beta Dopamine
Receptor Selectivity means that a drugs may preferentially bind to one subgroup.
Cardiovascular System A. Blood Vessels Adrenoceptors regulate vascular tone. Catecholamines are important in controlling peripheral vascular resistance and venous capacitance. Alpha receptors increase arterial resistance, whereas β 2 receptors relax smooth muscle. There are differences in receptor types in the various vascular beds.
The skin vessels have predominantly αreceptors and constrict in the presence epinephrine and norepinephrine, as do the splanchnic vessels. Vessels in skeletal muscle have both αand βreceptors, which mediate constriction or dilatation, respectively.
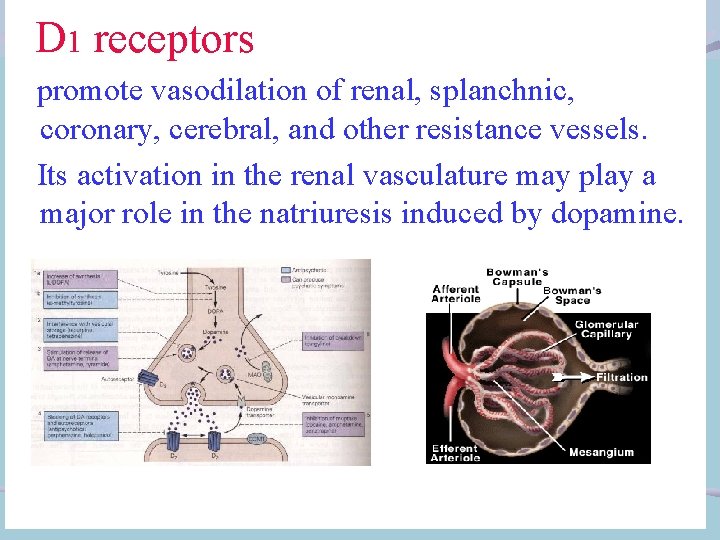
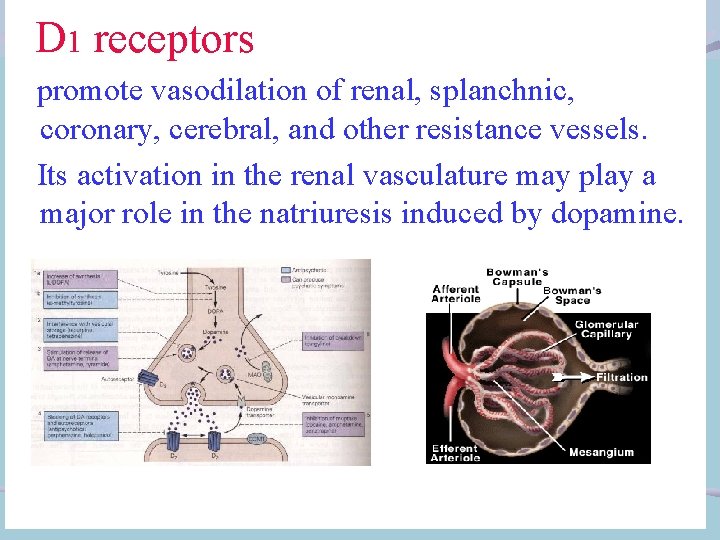
D 1 receptors promote vasodilation of renal, splanchnic, coronary, cerebral, and other resistance vessels. Its activation in the renal vasculature may play a major role in the natriuresis induced by dopamine.
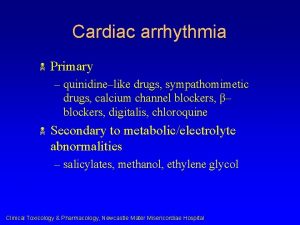
B. Heart The heart are determined largely by β 1 receptors. β-receptor activation increase calcium influx in cardiac cells. Pacemaker activity, both normal and abnormal, is increased. Conduction velocity in the atrio-ventricular node is increased. Intrinsic contractility is increased, and relaxation is accelerated.
As a result, the cardiac twitch response is increased in tension but abbreviated in duration. In the intact heart, intraventricular pressure rises and falls more rapidly, and ejection time is decreased.
Blood Pressure The effects of sympathomimetic drugs on BP is based on their effects on the heart, the peripheral vascular resistance, and the venous return. Phenylephrine, aαagonist, increases peripheral resistance and venous capacitance and rises the BP. The rise in BP increases baroreceptor-mediated vagal tone with slowing of the heart rate.
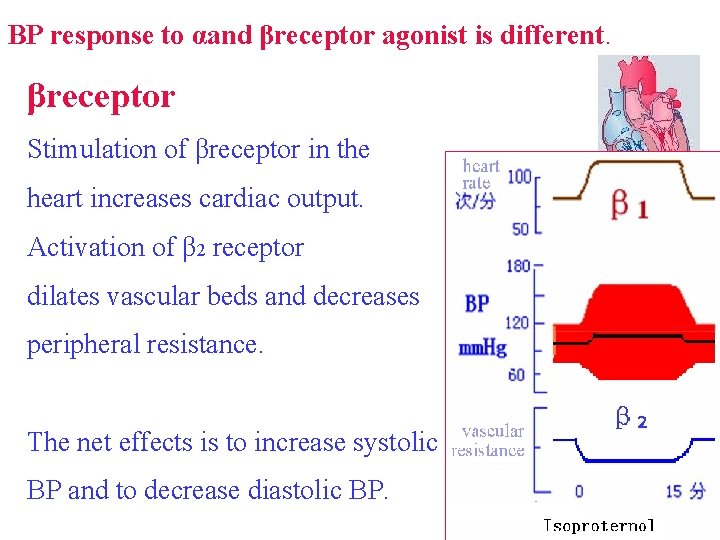
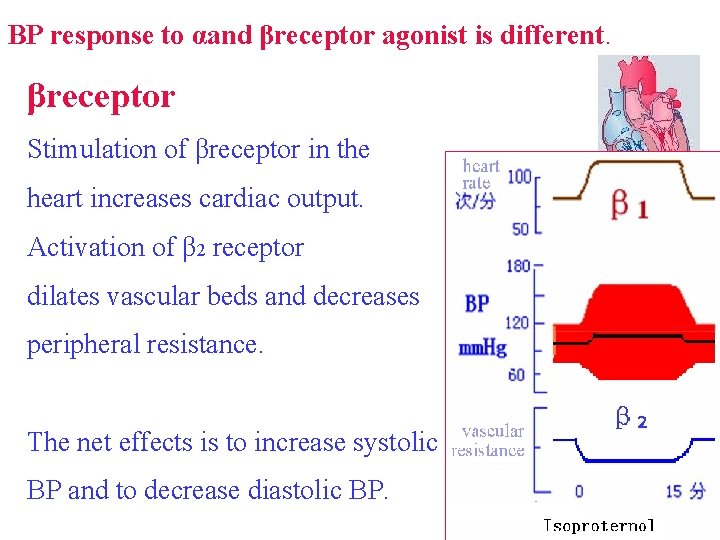
BP response to αand βreceptor agonist is different. βreceptor Stimulation of βreceptor in the heart increases cardiac output. Activation of β 2 receptor dilates vascular beds and decreases peripheral resistance. The net effects is to increase systolic BP and to decrease diastolic BP.
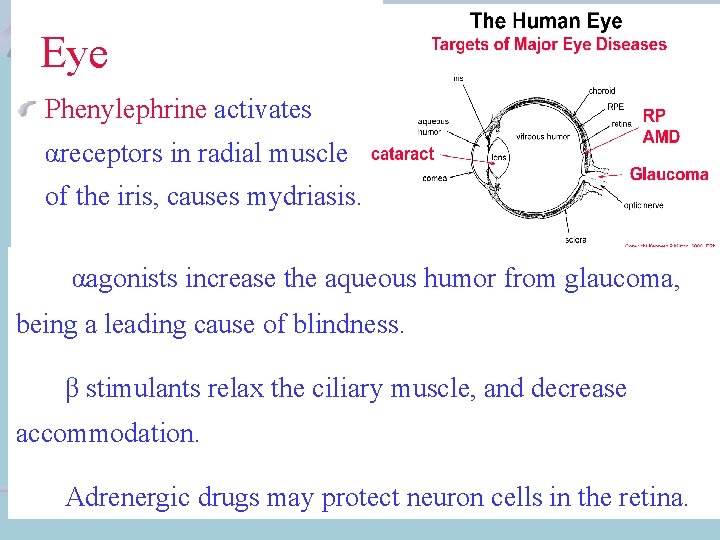
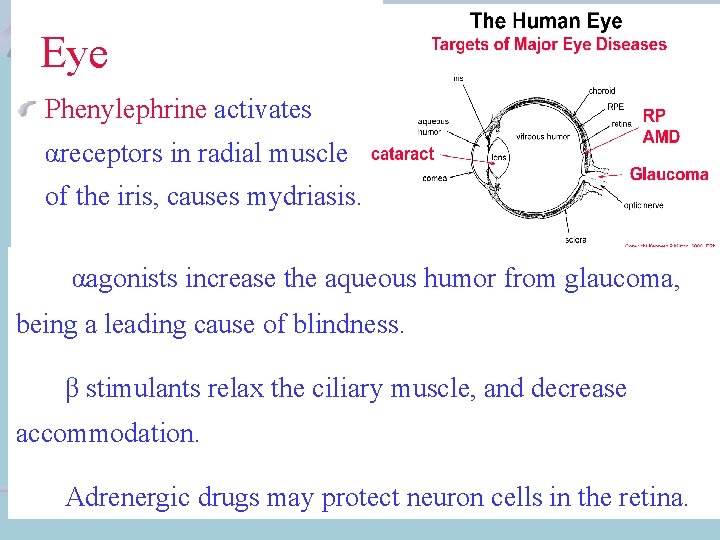
Eye Phenylephrine activates αreceptors in radial muscle of the iris, causes mydriasis. αagonists increase the aqueous humor from glaucoma, being a leading cause of blindness. β stimulants relax the ciliary muscle, and decrease accommodation. Adrenergic drugs may protect neuron cells in the retina.
Respiratory Tract Bronchial smooth muscle contains β 2 receptors that cause bronchodilation. The blood vessels of the respiratory tract mucosa contains αreceptors; The decongestant action of adrenoceptor stimulants is clinically useful. snuffle
Gastrointestinal Tract Beta receptors locate on the smooth muscle cells and mediate relaxation. Alpha stimulants, α 2 -selective agonists, decrease muscle activity by presynaptically reducing the release of ACh within the enteric nervous system. Alpha 2 receptors may also decrease slat and water flux into the lumen of the intestine.
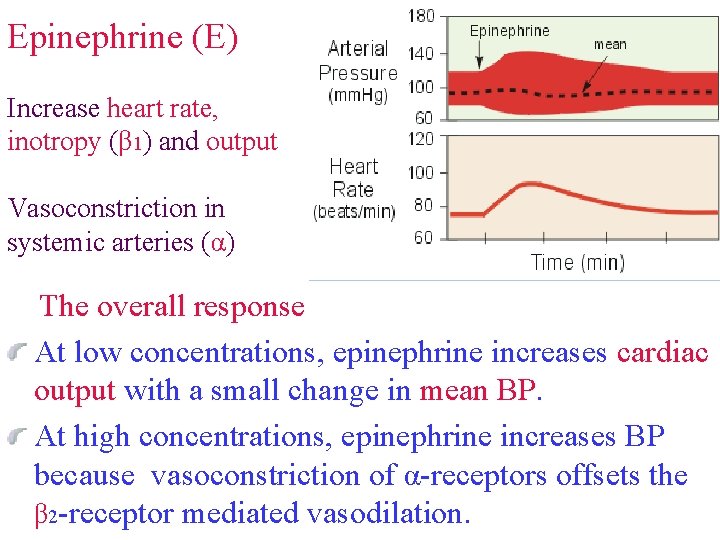
Specific Sympathomimetic Drugs Catecholamines Epinephrine is a potent vasoconstrictor (α) and cardiac stimulant(β 1). It can rise systolic BP by positive inotropic and chronotropic actions on the heart. Epinephrine activates β 2 receptors, leading to vasodilation. Consequently, total peripheral resistance and diastolic BP may fall. Vasodilation in skeletal muscle increases blood flow during exercise.
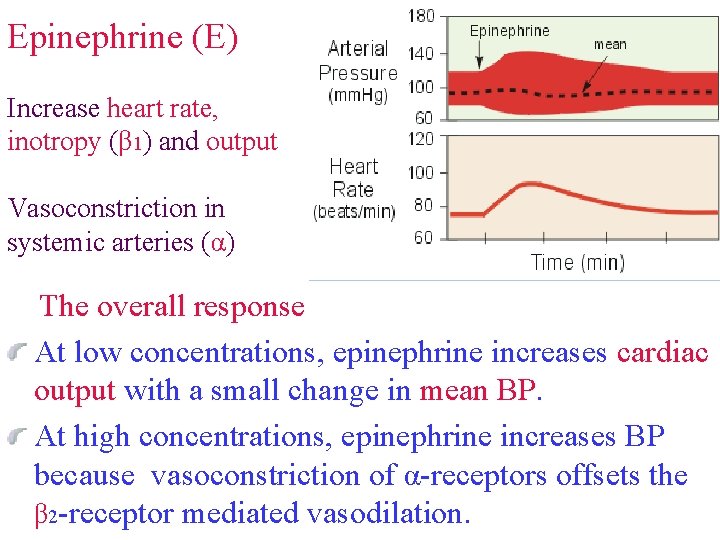
Epinephrine (E) Increase heart rate, inotropy (β 1) and output Vasoconstriction in systemic arteries (α) The overall response Vasodilation in muscle at low concentrations (β 2); At low concentrations, epinephrine increases cardiac output with a small change in mean BP. Vasoconstriction at high At high concentrations, epinephrine increases BP concentrations (α) because vasoconstriction of α-receptors offsets the β 2 -receptor mediated vasodilation.
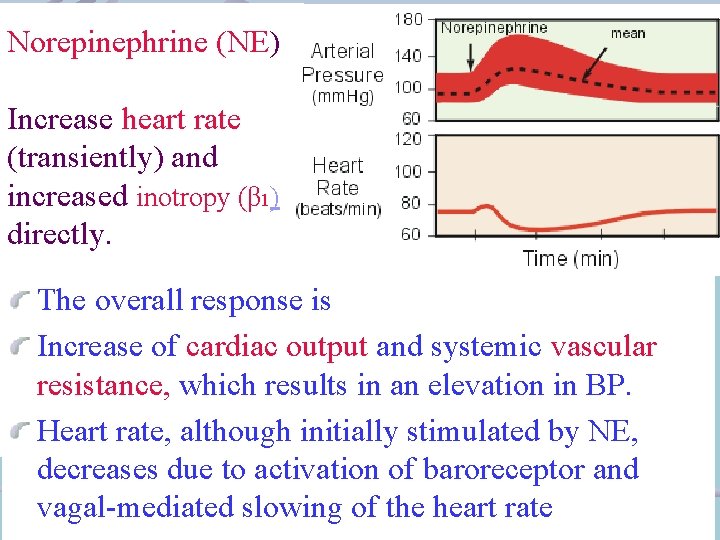
Norepinephrine (NE) NE and epinephrine have similar effects on β 1 and αreceptors, but has relatively little effect on β 2 receptors. NE increase peripheral resistance and both diastolic and systolic BP. Compensatory vagal reflexes tend to overcome the direct positive chronotropic effects; however, the positive inotropic effects on the heart are maintained.
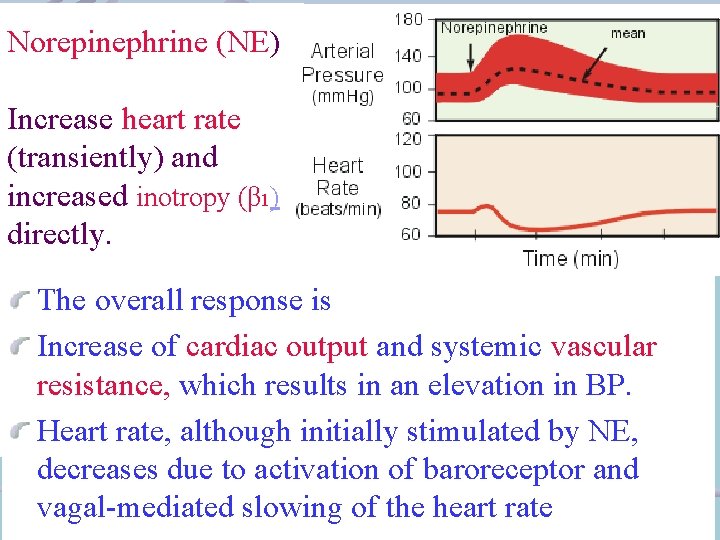
Norepinephrine (NE) Increase heart rate (transiently) and increased inotropy (β 1) directly. The overall response is Vasoconstriction in Increase of cardiac output and systemic vascular systemic artery and resistance, which results in an elevation in BP. vein ( α) Heart rate, although initially stimulated by NE, decreases due to activation of baroreceptor and vagal-mediated slowing of the heart rate
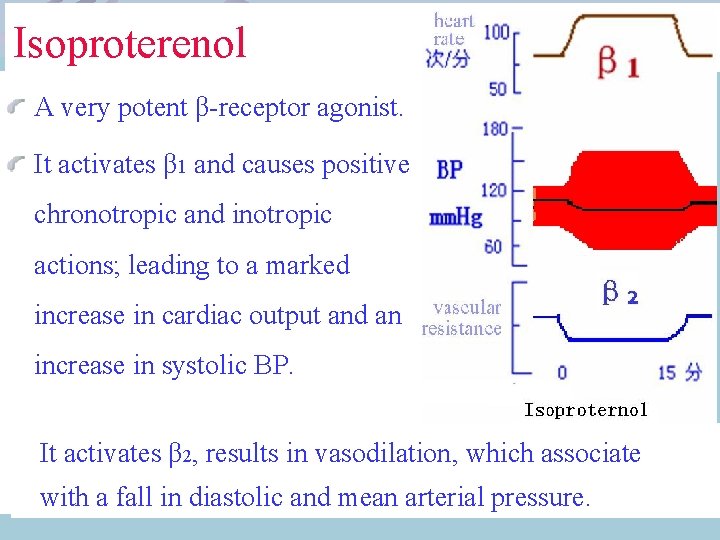
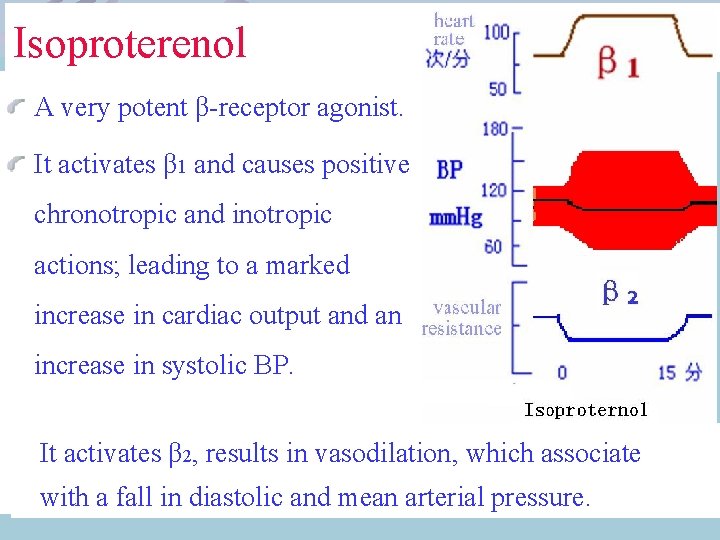
Isoproterenol A very potent β-receptor agonist. It activates β 1 and causes positive chronotropic and inotropic actions; leading to a marked increase in cardiac output and an increase in systolic BP. It activates β 2, results in vasodilation, which associate with a fall in diastolic and mean arterial pressure.
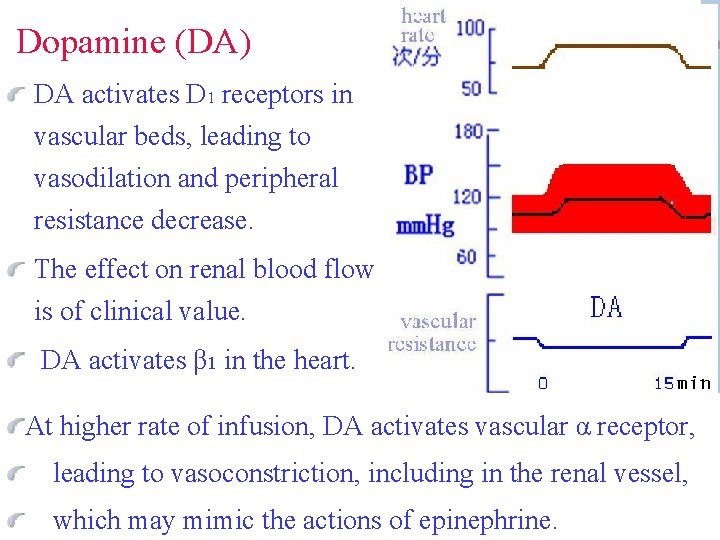
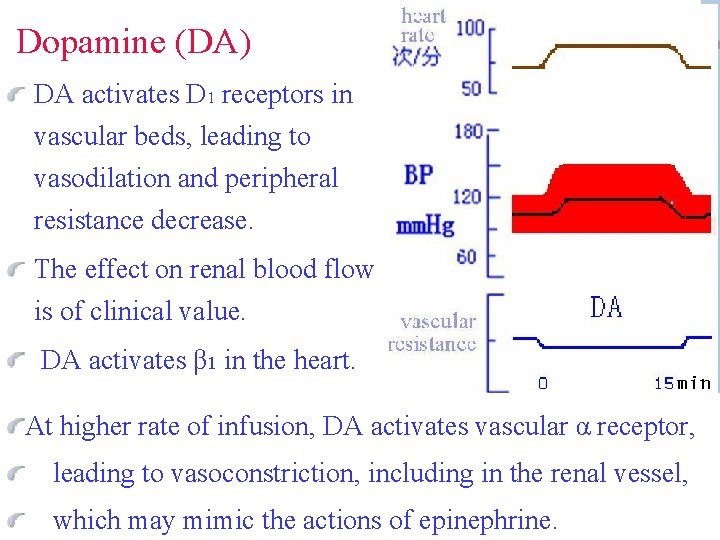
Dopamine (DA) DA activates D 1 receptors in vascular beds, leading to vasodilation and peripheral resistance decrease. The effect on renal blood flow is of clinical value. DA activates β 1 in the heart. At higher rate of infusion, DA activates vascular α receptor, leading to vasoconstriction, including in the renal vessel, which may mimic the actions of epinephrine.
Fenoldopam is a D 1 receptor agonist that selectively leads to periopheral vasodilation in some vascular beds. The primary indication is for treatment of severe hypertension.
Other Sympathomimetics They have pharmacokinetic features or relative selectivity for specific receptors. Phenylephrine is a relatively pure α agonist. Because it is not a catechol derivative, it is not inactivated by COMT and has a much longer duration of action than the catecholamines. It is an effective mydriatic and decongestant and can be used to raise the blood pressure.
Ephedrine occurs in plants and has been used in China for over 2000 years. Ephedrine can activate both αand βreceptors Because ephedrine is a noncatechol, it has high bioavailability and a long duration of action –hours rather than minutes.
Clinical application Conditions in which blood flow or pressure is to be enhanced Sympathomimetic drugs are used in hypotensive emergency on short duration αagonist such as norepinephrine, phenylephrine, methoxamine and ephedrine have been used for chronic hypotension.
Shock is a complex acute cardiovascular syndrome that results in a critical reduction in perfusion of vital tissues, and usually associated with hypotension, oliguria. The major mechanisms are hypovolemia, cardiac insufficiency, and altered vascular resistance. Sympathomimetic drugs have been used in the treatment of all forms of shock.
Cardiogenic Shock usually due to decrease of cardiac output. In low to moderate doses, positive inotropic agents such as dopamine or dobutamine may increase cardiac output and, compared with norepinephrine, cause relative little peripheral vasoconstriction. Isoproterenol increases heart rate and work more than either dopamine or dobutamine.
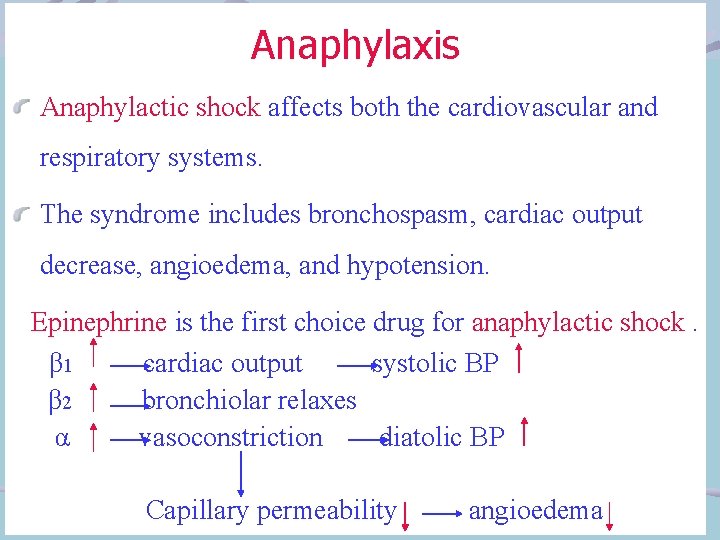
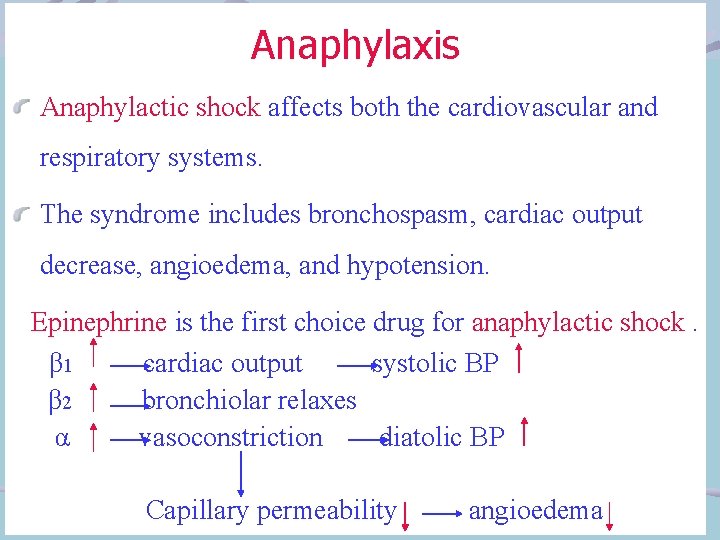
Anaphylaxis Anaphylactic shock affects both the cardiovascular and respiratory systems. The syndrome includes bronchospasm, cardiac output decrease, angioedema, and hypotension. Epinephrine is the first choice drug for anaphylactic shock. β 1 cardiac output systolic BP β 2 bronchiolar relaxes α vasoconstriction diatolic BP Capillary permeability angioedema
Conditions in Which Blood Flow is to be Reduced Epinephrine is usually applied topically in nasal packs or in a gingival string. Combining αagonists with local anesthetics greatly prolongs the duration of infiltration nerve block. The total doses of anesthetic can be reduced. Epinephrine is the favored agent for this applicant.
Cardiac Applications Isoproterenol and epinephrine have been utilized in the management of complete heart block and cardiac arrest. Heart failure may respond to the positive inotropic effects of drugs such as dobutamine.
Pulmonary Applications The most important use is in therapy of bronchial asthma. Nonspecific drugs, βagents, and β 2 - specific agents are all available for this indication. β 2 -specific drugs have less adverse effects.
Toxicity of Sympathomimetic Drugs The adverse effects of adrenoceptor agonist are primarily extensions of their pharmacologic effects in the cardiovascular and central nervous systems. Adverse cardiovascular effects include marked elevations in BP that cause increased cardiac work, which may precipitate cardiac ischemia and failure.

 Roughness and fierceness
Roughness and fierceness What is the starting material for synthesis of salbutamol
What is the starting material for synthesis of salbutamol Sympathomimetic drugs
Sympathomimetic drugs Sar of sympathomimetic agents
Sar of sympathomimetic agents Sympathomimetic drugs
Sympathomimetic drugs Sympathomimetic agents
Sympathomimetic agents Sympathomimetics
Sympathomimetics Sympathomimetic drugs
Sympathomimetic drugs Sympathomimetic agents
Sympathomimetic agents Self initiated other repair examples
Self initiated other repair examples Soh cah toa cho sha cao
Soh cah toa cho sha cao Cho sha cao
Cho sha cao Cây rơm đã cao và tròn nóc
Cây rơm đã cao và tròn nóc Guohong cao
Guohong cao Núi cao bởi có đất bồi
Núi cao bởi có đất bồi Hàm cobb-douglas toán cao cấp
Hàm cobb-douglas toán cao cấp Xin cao unsw
Xin cao unsw Thế nào là hệ số cao nhất
Thế nào là hệ số cao nhất Hàm cobb-douglas toán cao cấp
Hàm cobb-douglas toán cao cấp Cao 104
Cao 104 Cao 104
Cao 104 Project desgin
Project desgin Cao qualifications & assessment summary
Cao qualifications & assessment summary Cao mature student
Cao mature student Região epigástrica mesogástrica hipogástrica cão
Região epigástrica mesogástrica hipogástrica cão Dãy hoàng liên sơn
Dãy hoàng liên sơn đạo cao đài
đạo cao đài Dãy núi cao nhất châu á
Dãy núi cao nhất châu á Dãy núi cao nhất châu á
Dãy núi cao nhất châu á Cao points 2019
Cao points 2019 Con thờ lạy hết tình chúa ngự trong phép thánh
Con thờ lạy hết tình chúa ngự trong phép thánh Dãy núi cao nhất châu á
Dãy núi cao nhất châu á Cao 90 voorbeelden doelstellingen
Cao 90 voorbeelden doelstellingen Cao welzijn maatschappelijke dienstverlening
Cao welzijn maatschappelijke dienstverlening