CELIAC DISEASE ESPGHAN 2012 Guidelines for the Diagnosis
- Slides: 22
CELIAC DISEASE
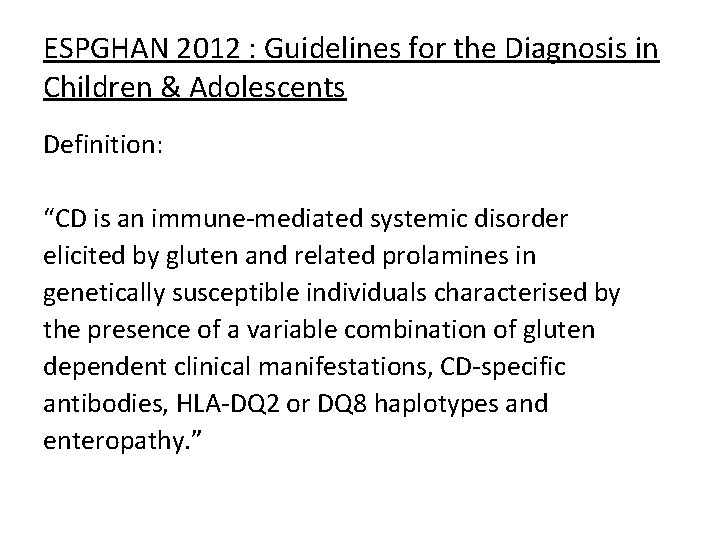
ESPGHAN 2012 : Guidelines for the Diagnosis in Children & Adolescents Definition: “CD is an immune-mediated systemic disorder elicited by gluten and related prolamines in genetically susceptible individuals characterised by the presence of a variable combination of gluten dependent clinical manifestations, CD-specific antibodies, HLA-DQ 2 or DQ 8 haplotypes and enteropathy. ”
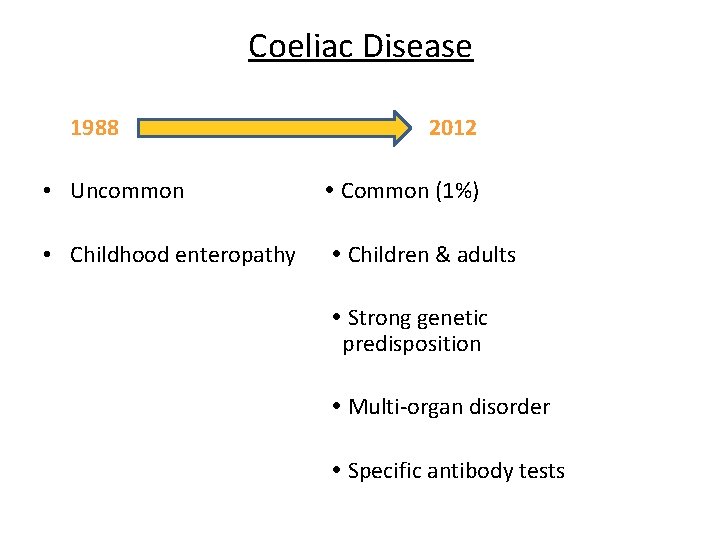
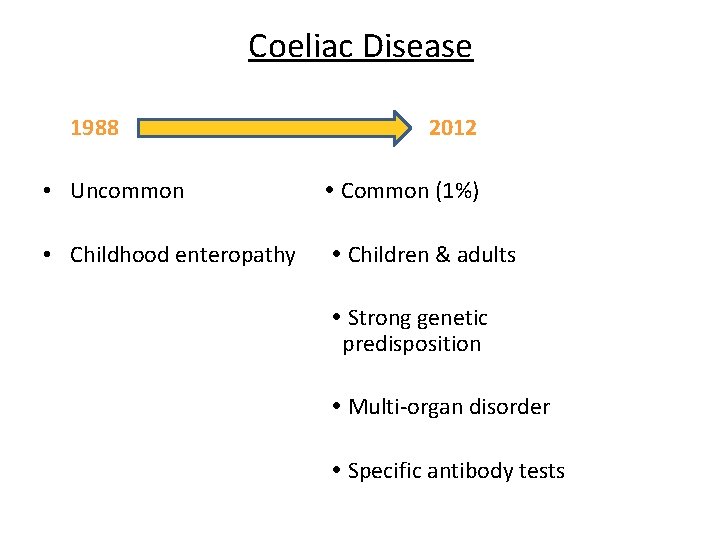
Coeliac Disease 1988 2012 • Uncommon Common (1%) • Childhood enteropathy Children & adults Strong genetic predisposition Multi-organ disorder Specific antibody tests
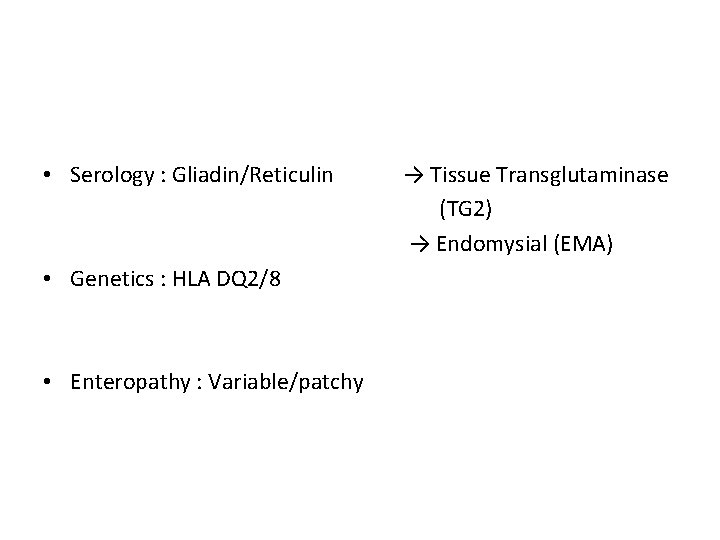
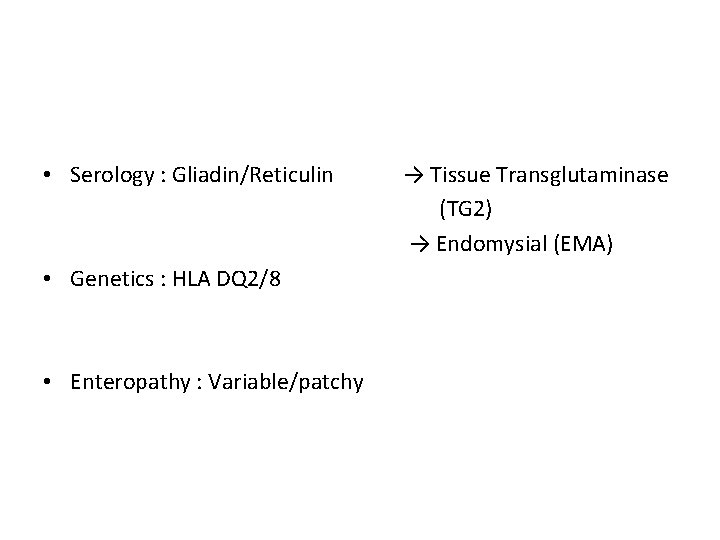
• Serology : Gliadin/Reticulin • Genetics : HLA DQ 2/8 • Enteropathy : Variable/patchy → Tissue Transglutaminase (TG 2) → Endomysial (EMA)
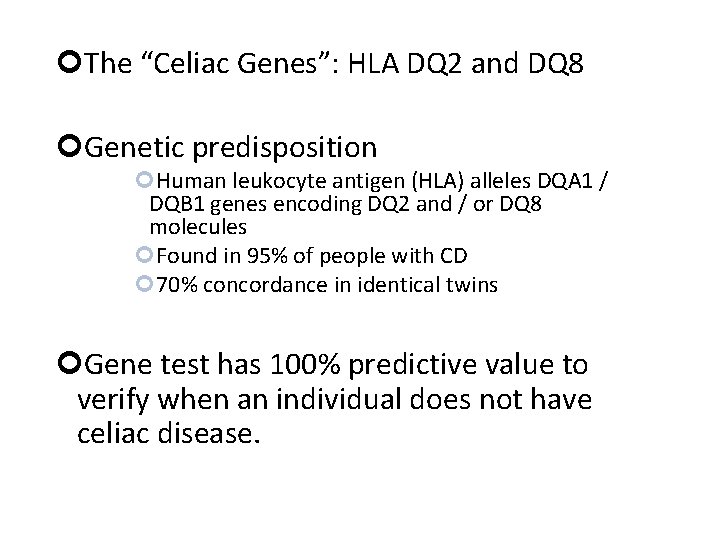
The “Celiac Genes”: HLA DQ 2 and DQ 8 Genetic predisposition Human leukocyte antigen (HLA) alleles DQA 1 / DQB 1 genes encoding DQ 2 and / or DQ 8 molecules Found in 95% of people with CD 70% concordance in identical twins Gene test has 100% predictive value to verify when an individual does not have celiac disease.
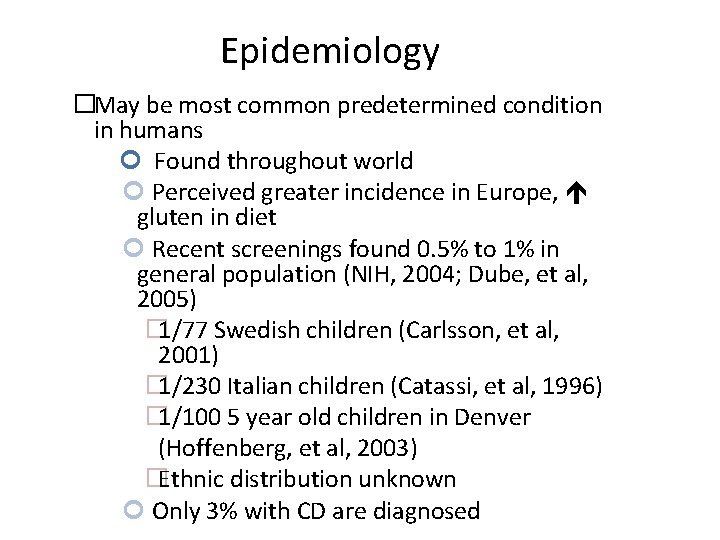
Epidemiology �May be most common predetermined condition in humans Found throughout world Perceived greater incidence in Europe, gluten in diet Recent screenings found 0. 5% to 1% in general population (NIH, 2004; Dube, et al, 2005) � 1/77 Swedish children (Carlsson, et al, 2001) � 1/230 Italian children (Catassi, et al, 1996) � 1/100 5 year old children in Denver (Hoffenberg, et al, 2003) �Ethnic distribution unknown Only 3% with CD are diagnosed
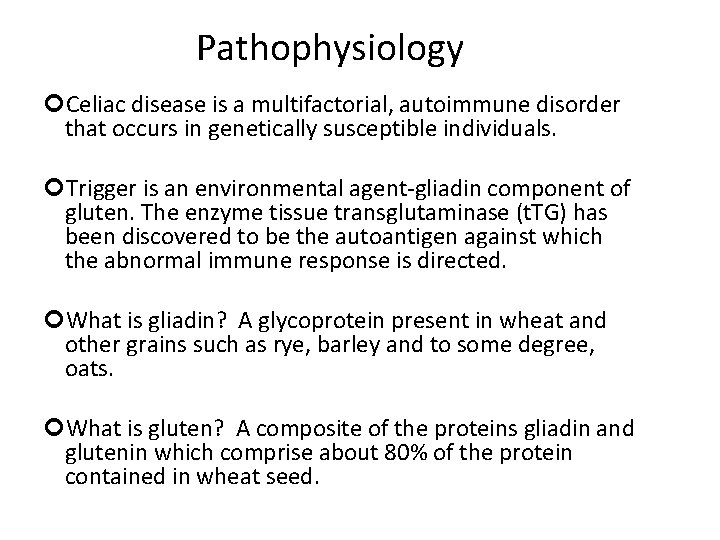
Pathophysiology Celiac disease is a multifactorial, autoimmune disorder that occurs in genetically susceptible individuals. Trigger is an environmental agent-gliadin component of gluten. The enzyme tissue transglutaminase (t. TG) has been discovered to be the autoantigen against which the abnormal immune response is directed. What is gliadin? A glycoprotein present in wheat and other grains such as rye, barley and to some degree, oats. What is gluten? A composite of the proteins gliadin and glutenin which comprise about 80% of the protein contained in wheat seed.
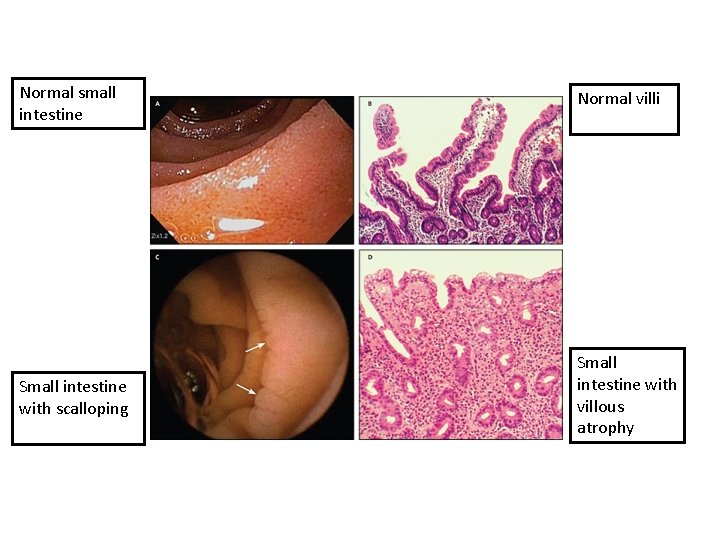
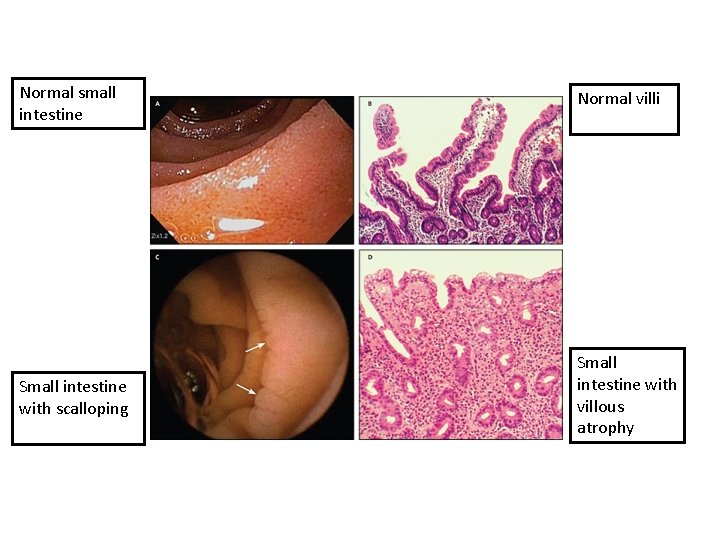
Normal small intestine Normal villi Small intestine with scalloping Small intestine with villous atrophy
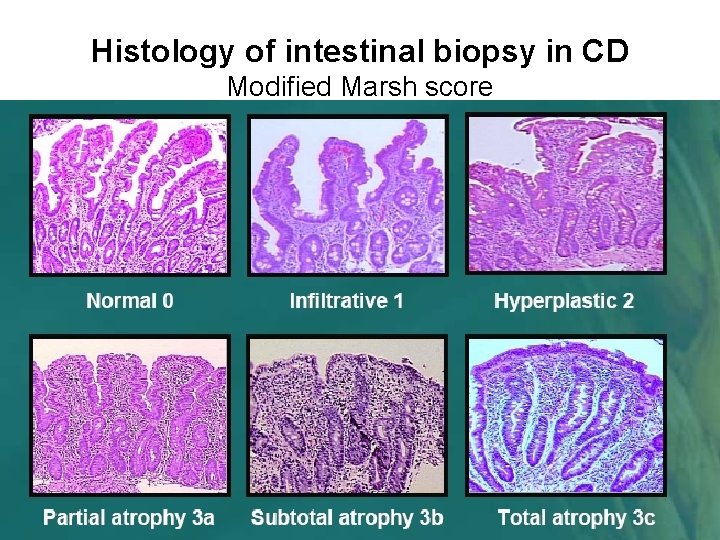
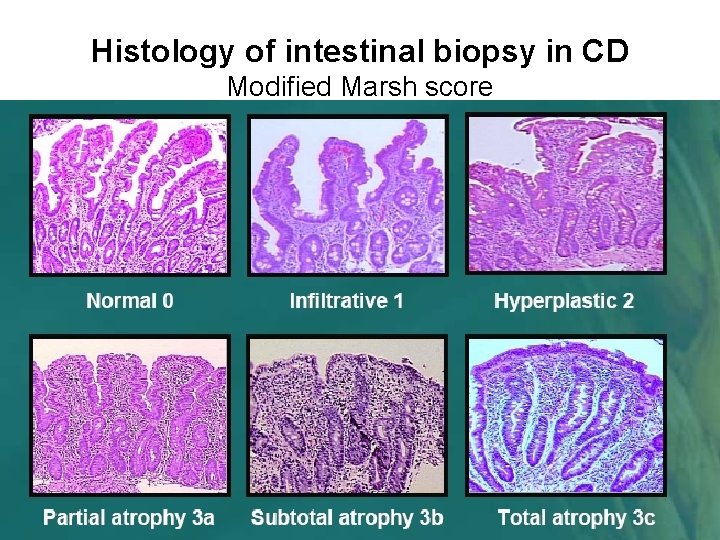
Histology of intestinal biopsy in CD Modified Marsh score
Classic physical presentation London, year 1938
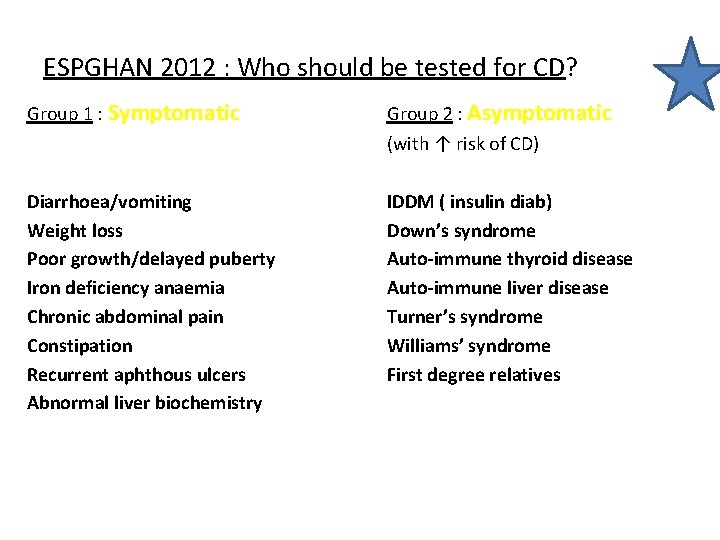
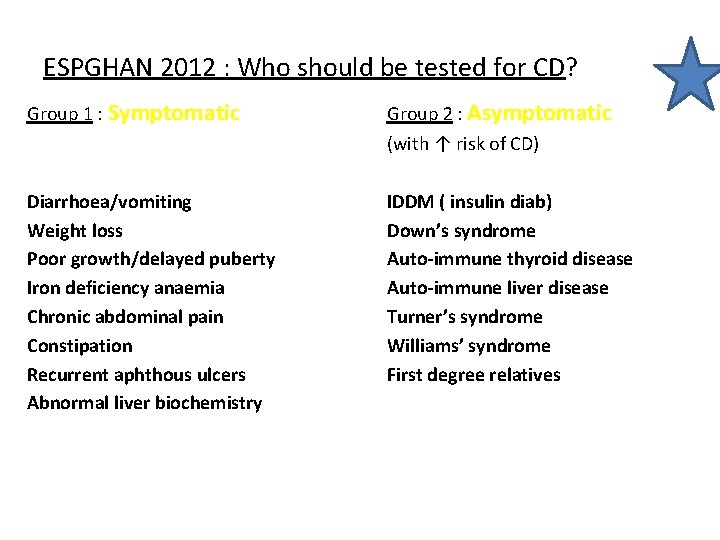
ESPGHAN 2012 : Who should be tested for CD? Group 1 : Symptomatic Group 2 : Asymptomatic (with ↑ risk of CD) Diarrhoea/vomiting Weight loss Poor growth/delayed puberty Iron deficiency anaemia Chronic abdominal pain Constipation Recurrent aphthous ulcers Abnormal liver biochemistry IDDM ( insulin diab) Down’s syndrome Auto-immune thyroid disease Auto-immune liver disease Turner’s syndrome Williams’ syndrome First degree relatives
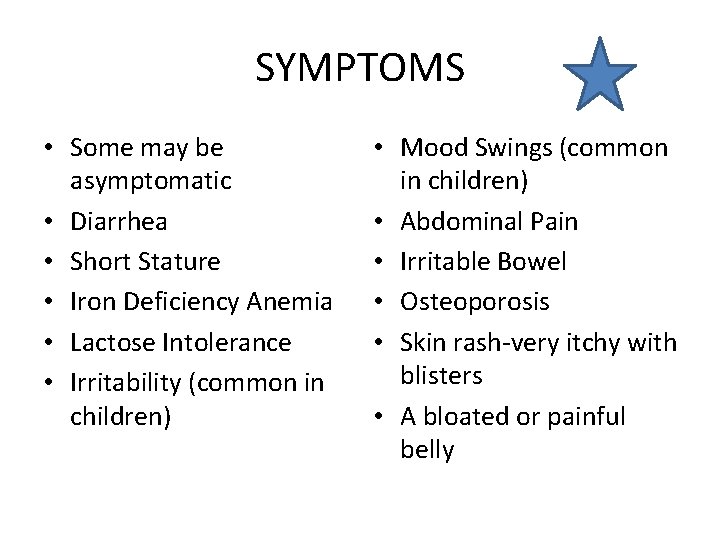
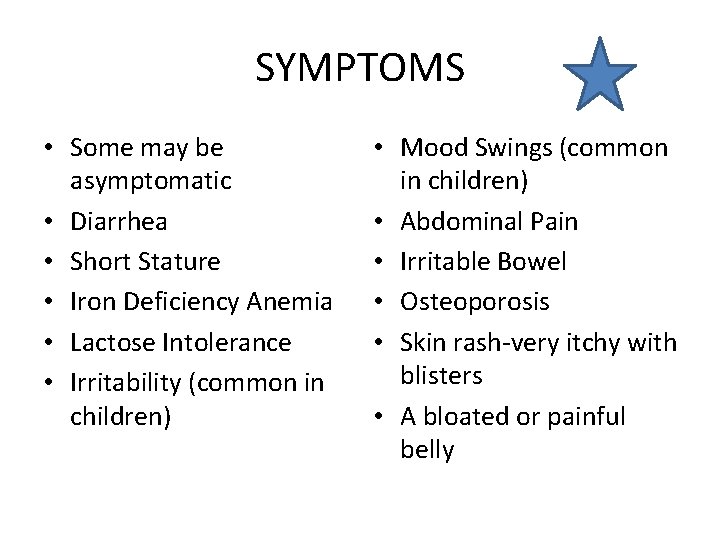
SYMPTOMS • Some may be asymptomatic • Diarrhea • Short Stature • Iron Deficiency Anemia • Lactose Intolerance • Irritability (common in children) • Mood Swings (common in children) • Abdominal Pain • Irritable Bowel • Osteoporosis • Skin rash-very itchy with blisters • A bloated or painful belly
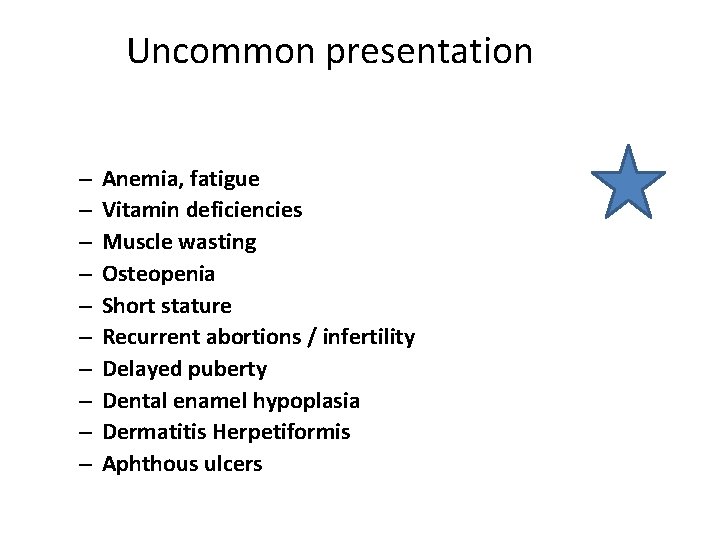
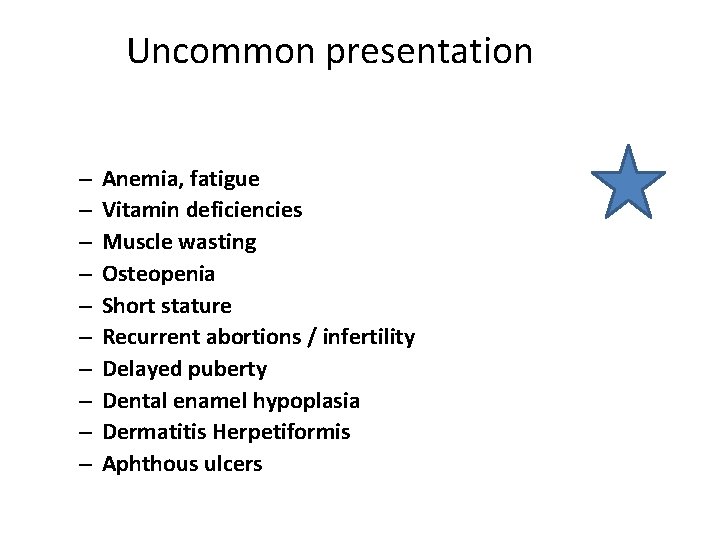
Uncommon presentation – – – – – Anemia, fatigue Vitamin deficiencies Muscle wasting Osteopenia Short stature Recurrent abortions / infertility Delayed puberty Dental enamel hypoplasia Dermatitis Herpetiformis Aphthous ulcers
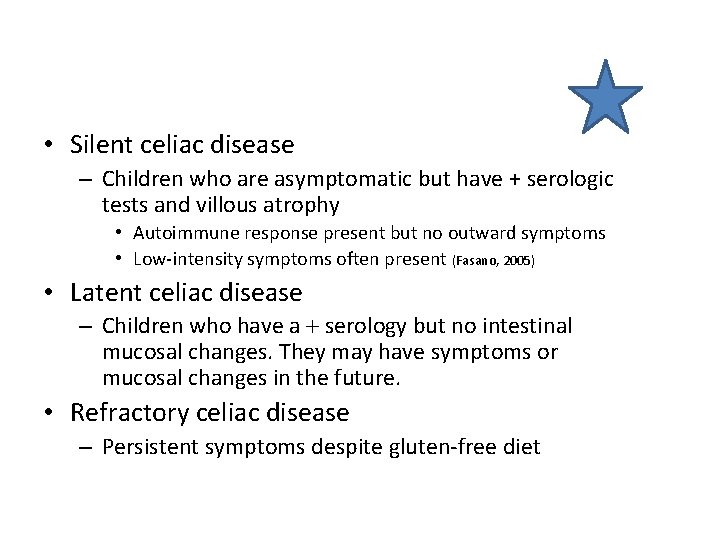
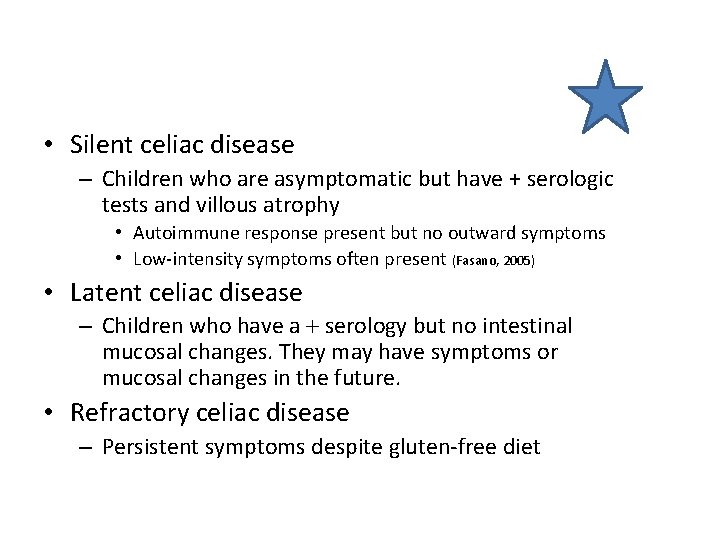
• Silent celiac disease – Children who are asymptomatic but have + serologic tests and villous atrophy • Autoimmune response present but no outward symptoms • Low-intensity symptoms often present (Fasano, 2005) • Latent celiac disease – Children who have a serology but no intestinal mucosal changes. They may have symptoms or mucosal changes in the future. • Refractory celiac disease – Persistent symptoms despite gluten-free diet
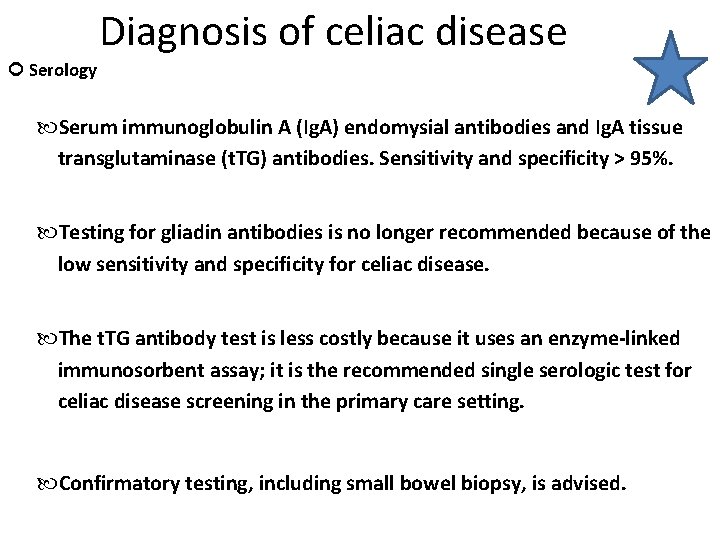
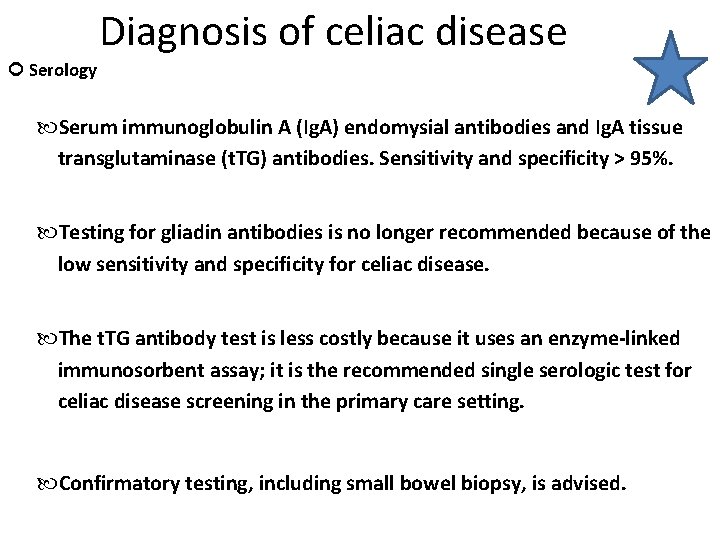
Diagnosis of celiac disease Serology Serum immunoglobulin A (Ig. A) endomysial antibodies and Ig. A tissue transglutaminase (t. TG) antibodies. Sensitivity and specificity > 95%. Testing for gliadin antibodies is no longer recommended because of the low sensitivity and specificity for celiac disease. The t. TG antibody test is less costly because it uses an enzyme-linked immunosorbent assay; it is the recommended single serologic test for celiac disease screening in the primary care setting. Confirmatory testing, including small bowel biopsy, is advised.
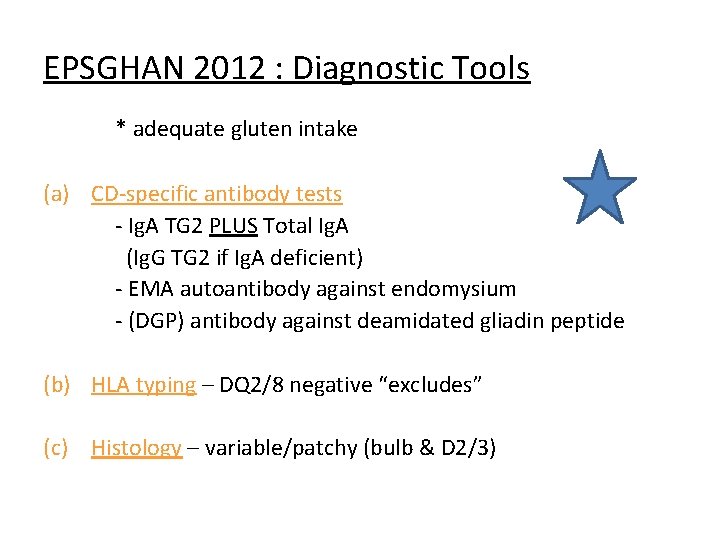
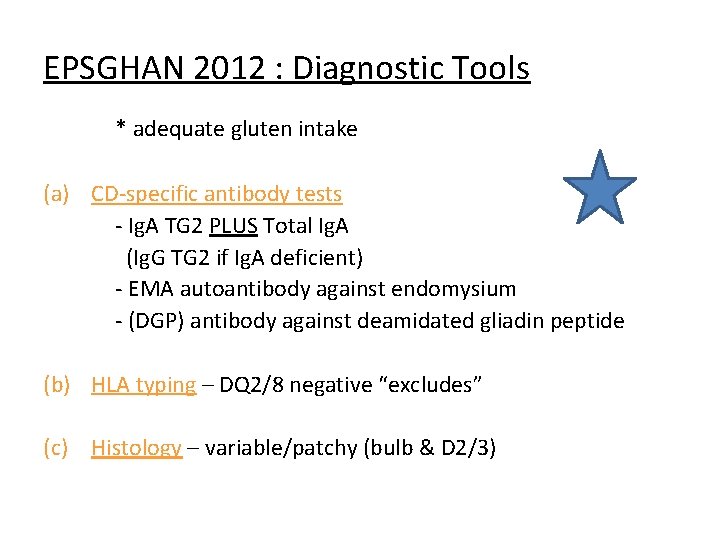
EPSGHAN 2012 : Diagnostic Tools * adequate gluten intake (a) CD-specific antibody tests - Ig. A TG 2 PLUS Total Ig. A (Ig. G TG 2 if Ig. A deficient) - EMA autoantibody against endomysium - (DGP) antibody against deamidated gliadin peptide (b) HLA typing – DQ 2/8 negative “excludes” (c) Histology – variable/patchy (bulb & D 2/3)
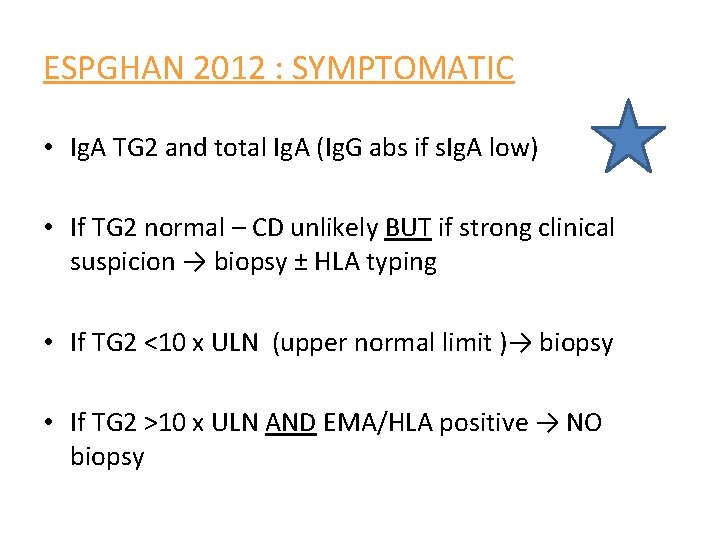
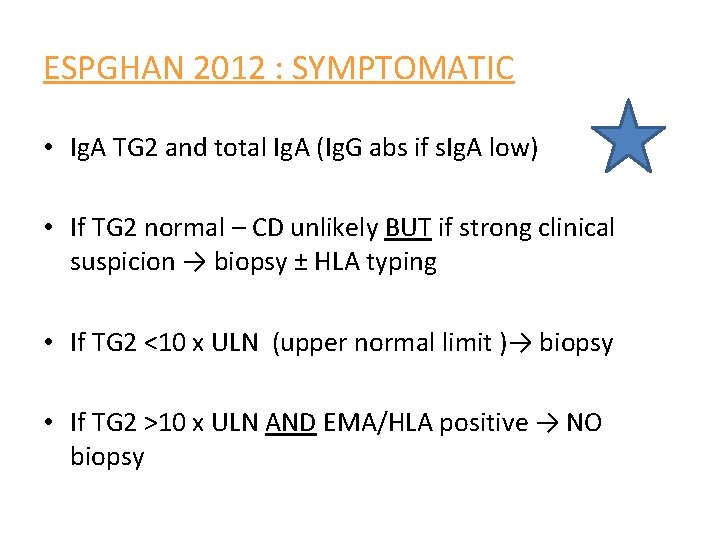
ESPGHAN 2012 : SYMPTOMATIC • Ig. A TG 2 and total Ig. A (Ig. G abs if s. Ig. A low) • If TG 2 normal – CD unlikely BUT if strong clinical suspicion → biopsy ± HLA typing • If TG 2 <10 x ULN (upper normal limit )→ biopsy • If TG 2 >10 x ULN AND EMA/HLA positive → NO biopsy
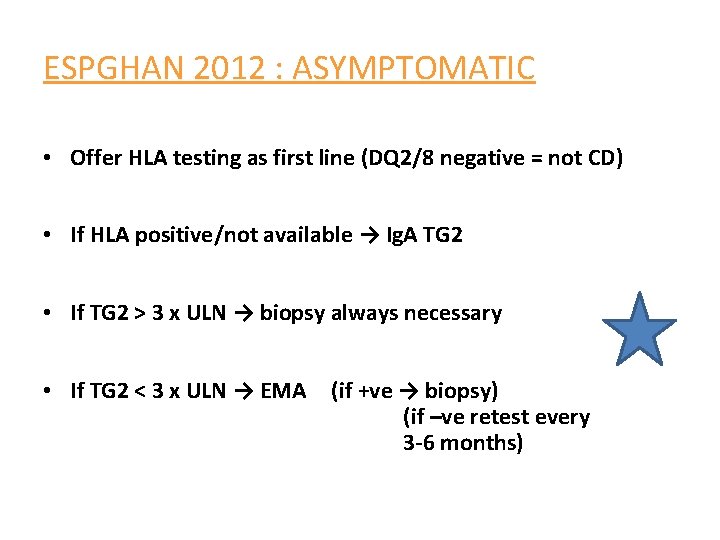
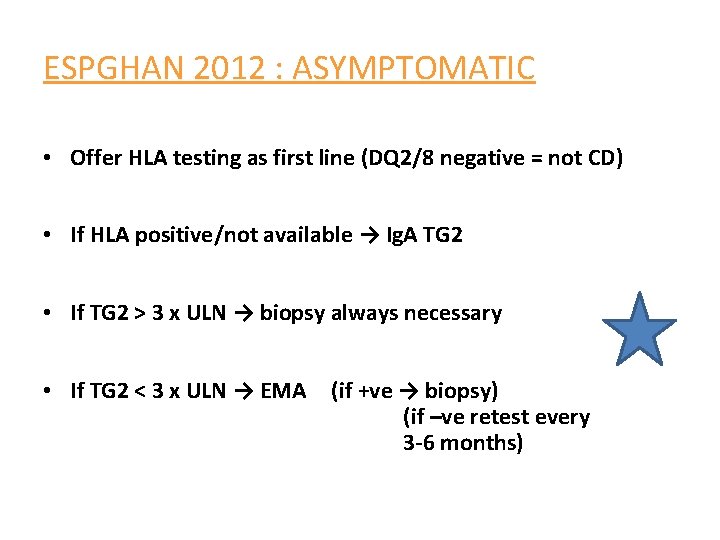
ESPGHAN 2012 : ASYMPTOMATIC • Offer HLA testing as first line (DQ 2/8 negative = not CD) • If HLA positive/not available → Ig. A TG 2 • If TG 2 > 3 x ULN → biopsy always necessary • If TG 2 < 3 x ULN → EMA (if +ve → biopsy) (if –ve retest every 3 -6 months)
Treatment of celiac disease Avoidance of food products that contain gluten proteins. It is essential that the diagnosis be confirmed before submitting patients to this therapy. Key elements to successful treatment include the motivation of the patient, the attentiveness of the physician to comorbidities that need to be addressed. Formal consultation with a trained dietitian is necessary. The dietitian plays a vital role in helping the patient successfully adapt to the necessary behavioral changes and may provide much of the required follow-up. National celiac disease support organizations can provide patients invaluable resources for information and support.
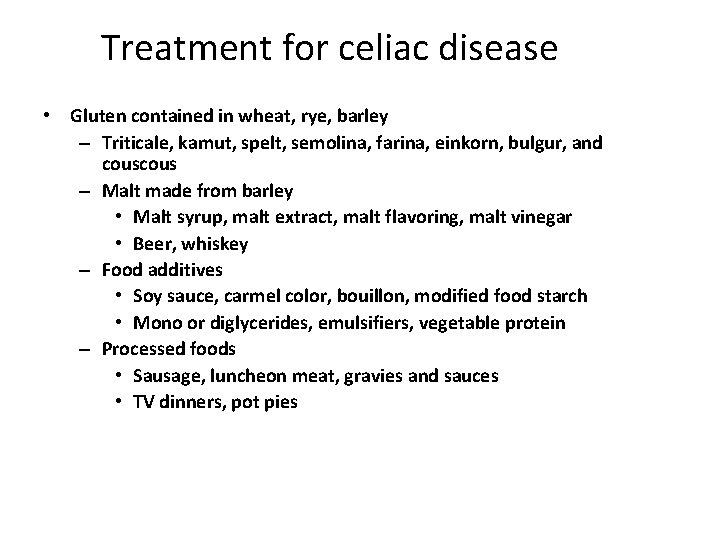
Treatment for celiac disease • Gluten contained in wheat, rye, barley – Triticale, kamut, spelt, semolina, farina, einkorn, bulgur, and cous – Malt made from barley • Malt syrup, malt extract, malt flavoring, malt vinegar • Beer, whiskey – Food additives • Soy sauce, carmel color, bouillon, modified food starch • Mono or diglycerides, emulsifiers, vegetable protein – Processed foods • Sausage, luncheon meat, gravies and sauces • TV dinners, pot pies
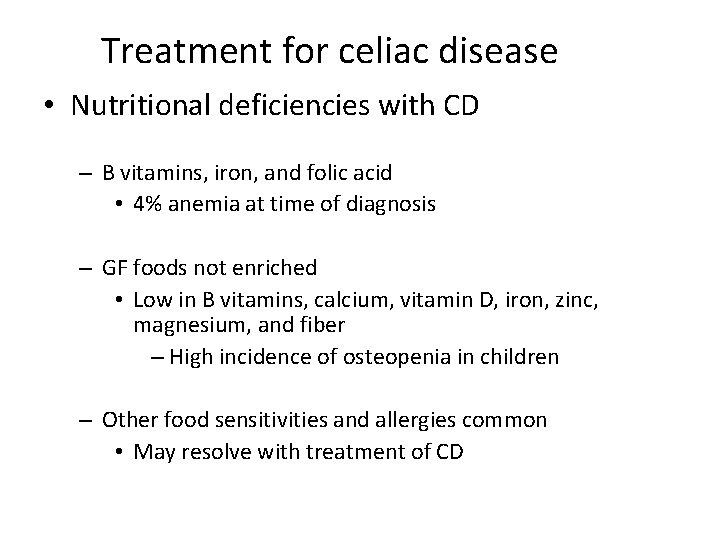
Treatment for celiac disease • Nutritional deficiencies with CD – B vitamins, iron, and folic acid • 4% anemia at time of diagnosis – GF foods not enriched • Low in B vitamins, calcium, vitamin D, iron, zinc, magnesium, and fiber – High incidence of osteopenia in children – Other food sensitivities and allergies common • May resolve with treatment of CD
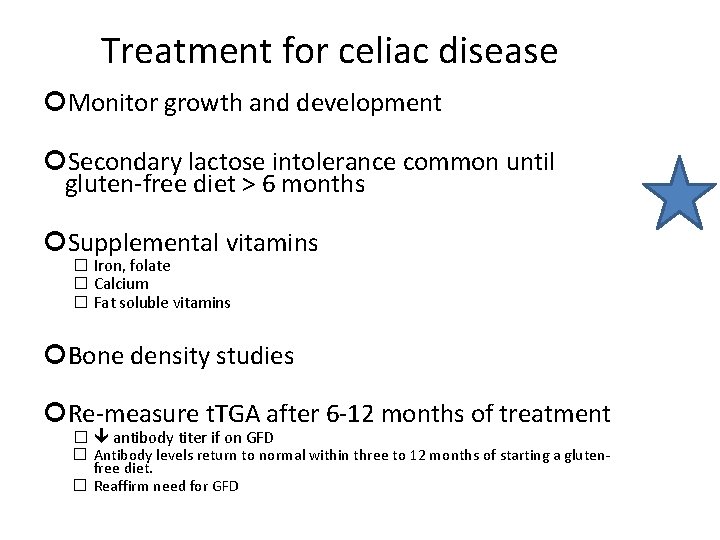
Treatment for celiac disease Monitor growth and development Secondary lactose intolerance common until gluten-free diet > 6 months Supplemental vitamins � Iron, folate � Calcium � Fat soluble vitamins Bone density studies Re-measure t. TGA after 6 -12 months of treatment � antibody titer if on GFD � Antibody levels return to normal within three to 12 months of starting a glutenfree diet. � Reaffirm need for GFD
 Pes statement for celiac disease
Pes statement for celiac disease Celiac disease pes statement
Celiac disease pes statement Celiac disease colville
Celiac disease colville Prof dr tufan kutlu
Prof dr tufan kutlu Marsh classification of celiac disease
Marsh classification of celiac disease Malabsorption treatment
Malabsorption treatment Celiac disease pes statement
Celiac disease pes statement Celiac disease french
Celiac disease french Linee guida espghan
Linee guida espghan Perbedaan diagnosis gizi dan diagnosis medis
Perbedaan diagnosis gizi dan diagnosis medis Medical diagnosis and nursing diagnosis difference
Medical diagnosis and nursing diagnosis difference Medical diagnosis and nursing diagnosis difference
Medical diagnosis and nursing diagnosis difference Nursing process objectives
Nursing process objectives Nursing process assessment
Nursing process assessment Nursing diagnosis for meniere's disease
Nursing diagnosis for meniere's disease Nursing diagnosis for vision impairment
Nursing diagnosis for vision impairment Behcet disease diagnosis
Behcet disease diagnosis Diagnosis of periodontal disease
Diagnosis of periodontal disease Communicable disease and non communicable disease
Communicable disease and non communicable disease Celiac 504 plan
Celiac 504 plan Celiac beri beri
Celiac beri beri Embryology of git
Embryology of git Dorsal pedis vein
Dorsal pedis vein