Caterina P Minniti MD Leg Ulcers in patients




- Slides: 39
Caterina P Minniti, MD Leg Ulcers in patients with Sickle Cell Disease: What providers and patients need to know! 10 th Annual Sickle Cell Disease Educational Seminar: Integrative Medicine and Sickle Cell Disease: A Multi-Disciplinary 21 st Century Approach September 8 th, 2018 Sacramento, CA
Disclosures • • • Advisory Board: Novartis Pharmaceutical Advisory Board: Global Blood therapeutics Research support: GBT and Bayer Advisory Board: Teutona IND: Sodium Nitrite for SCD leg uclers FDA research support: Sodium nitrite for leg ulcers in SCD
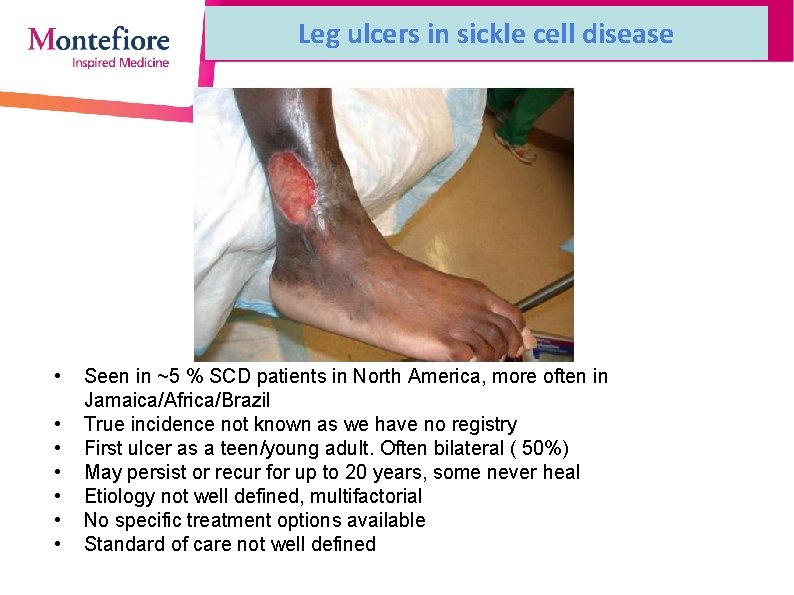
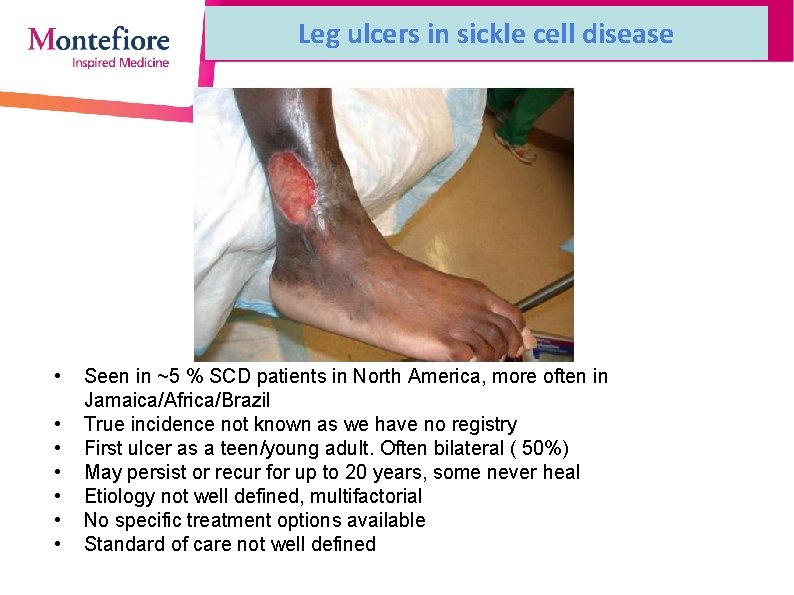
Leg ulcers in sickle cell disease • • Seen in ~5 % SCD patients in North America, more often in Jamaica/Africa/Brazil True incidence not known as we have no registry First ulcer as a teen/young adult. Often bilateral ( 50%) May persist or recur for up to 20 years, some never heal Etiology not well defined, multifactorial No specific treatment options available Standard of care not well defined
Clinical presentation • M: F : 1. 1 Low BMI (~ 21 -24) ; “Tall and thin” • HBSS>>>HBSC/Sbeta thal • High prevalence of elevated TRV(and RHC proven PH), priapism and renal dysfunction( high uric acid, high NT-Pro. BNP, low serum albumin, proteinuria) • Thrombophilia markers: Low ATIII, low prot. C and S, high VIII, positive LA • History of DVT’s/PE in ~40% • History of minor trauma prior to occurrence in 50% • Indices of hemolysis: Low Hb, high LDH, high retic • Low Pulse Ox
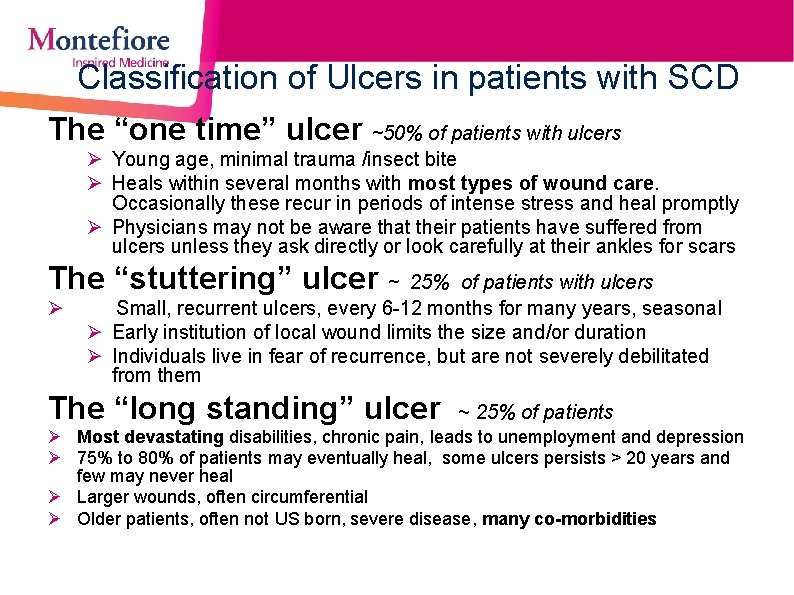
Classification of Ulcers in patients with SCD The “one time” ulcer ~50% of patients with ulcers Ø Young age, minimal trauma /insect bite Ø Heals within several months with most types of wound care. Occasionally these recur in periods of intense stress and heal promptly Ø Physicians may not be aware that their patients have suffered from ulcers unless they ask directly or look carefully at their ankles for scars The “stuttering” ulcer ~ 25% of patients with ulcers Ø Small, recurrent ulcers, every 6 -12 months for many years, seasonal Ø Early institution of local wound limits the size and/or duration Ø Individuals live in fear of recurrence, but are not severely debilitated from them The “long standing” ulcer ~ 25% of patients Ø Most devastating disabilities, chronic pain, leads to unemployment and depression Ø 75% to 80% of patients may eventually heal, some ulcers persists > 20 years and few may never heal Ø Larger wounds, often circumferential Ø Older patients, often not US born, severe disease, many co-morbidities
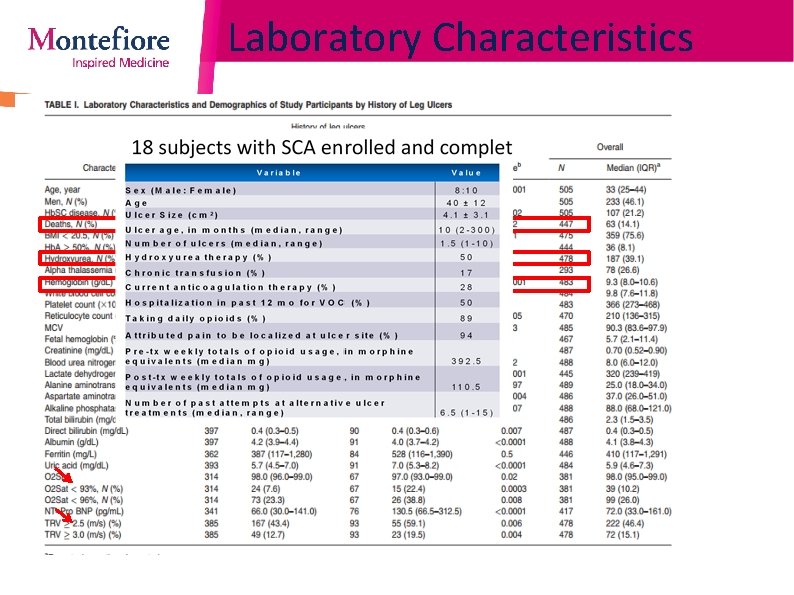
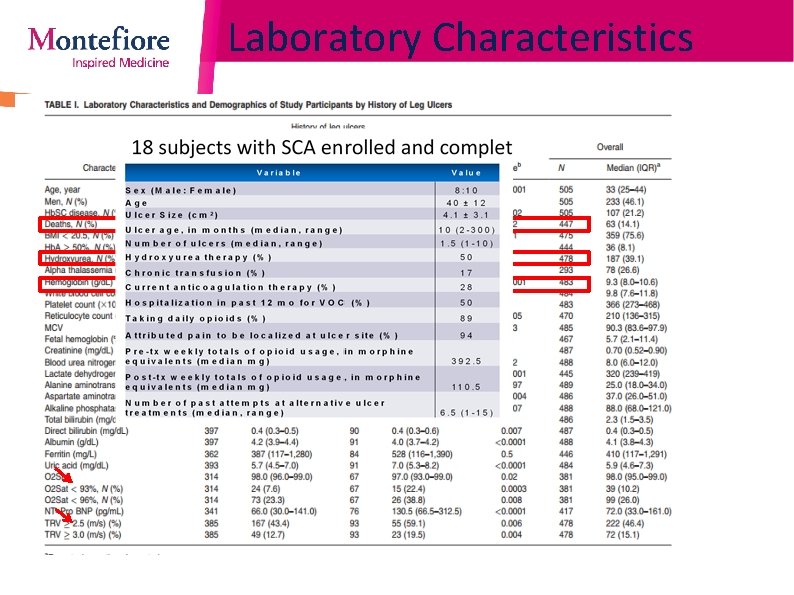
Laboratory Characteristics Minniti, 2011 AJH
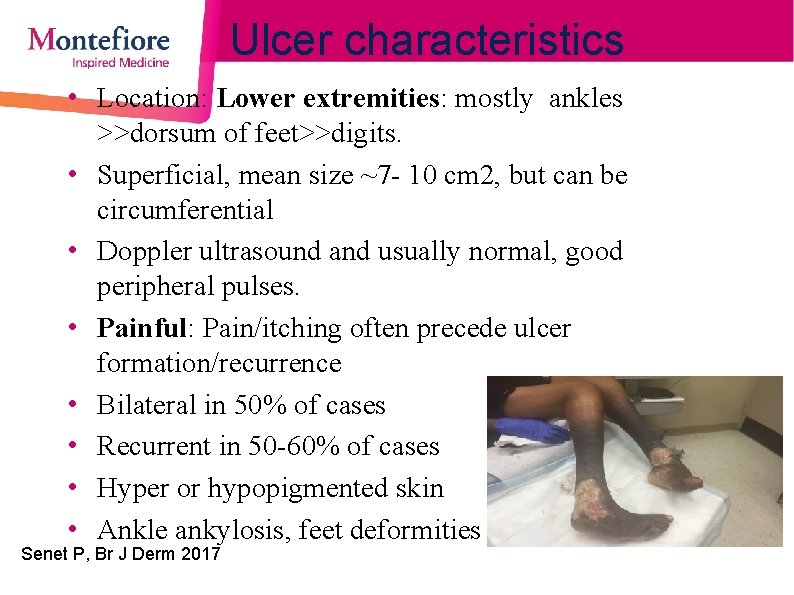
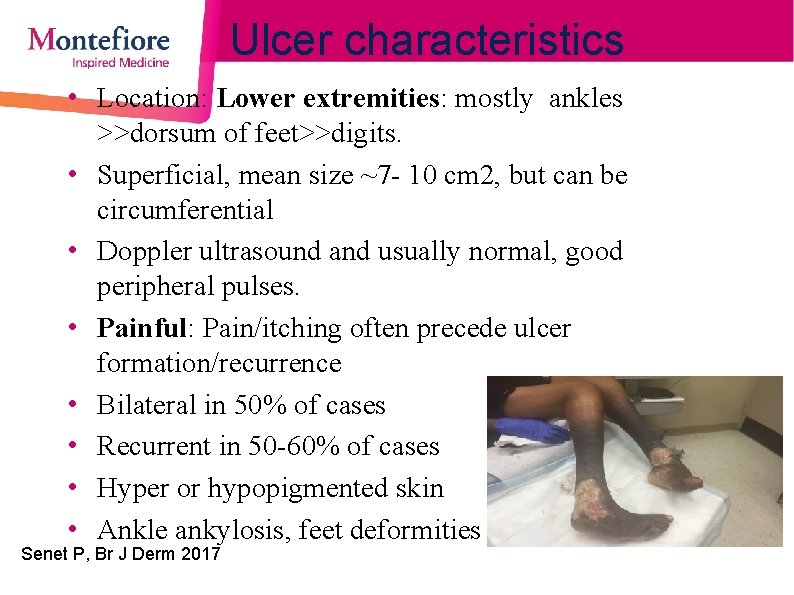
Ulcer characteristics • Location: Lower extremities: mostly ankles >>dorsum of feet>>digits. • Superficial, mean size ~7 - 10 cm 2, but can be circumferential • Doppler ultrasound and usually normal, good peripheral pulses. • Painful: Pain/itching often precede ulcer formation/recurrence • Bilateral in 50% of cases • Recurrent in 50 -60% of cases • Hyper or hypopigmented skin • Ankle ankylosis, feet deformities Senet P, Br J Derm 2017 Minniti AJH 2013, personal observations
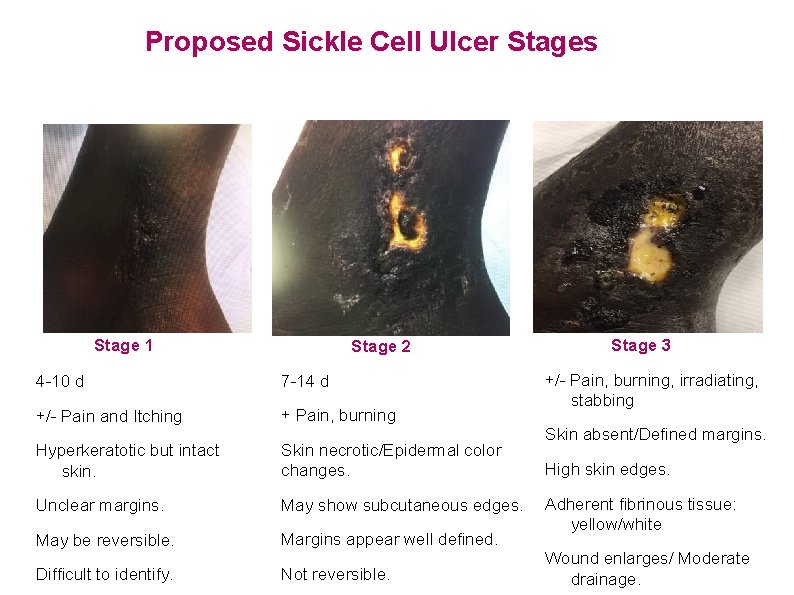
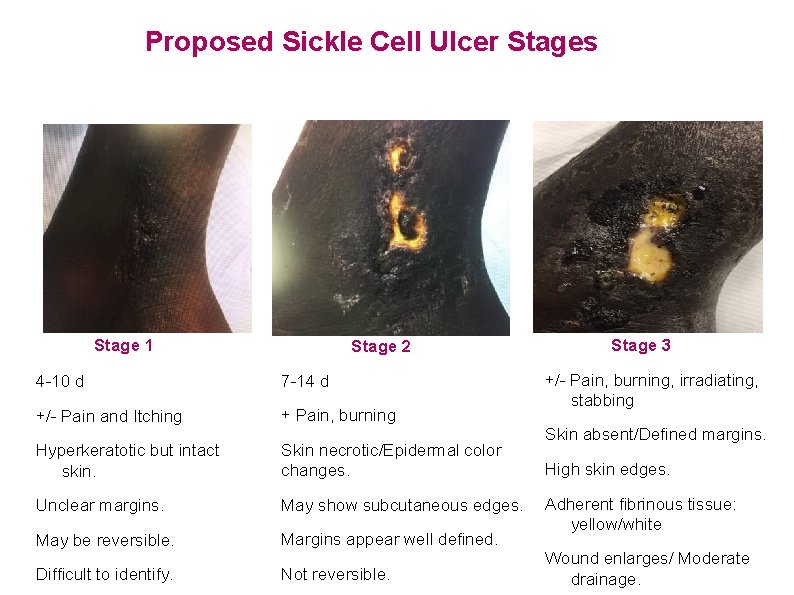
Proposed Sickle Cell Ulcer Stages Stage 1 Stage 2 4 -10 d 7 -14 d +/- Pain and Itching + Pain, burning Hyperkeratotic but intact skin. Skin necrotic/Epidermal color changes. Unclear margins. May show subcutaneous edges. May be reversible. Margins appear well defined. Difficult to identify. Not reversible. Stage 3 +/- Pain, burning, irradiating, stabbing Skin absent/Defined margins. High skin edges. Adherent fibrinous tissue: yellow/white Wound enlarges/ Moderate drainage.
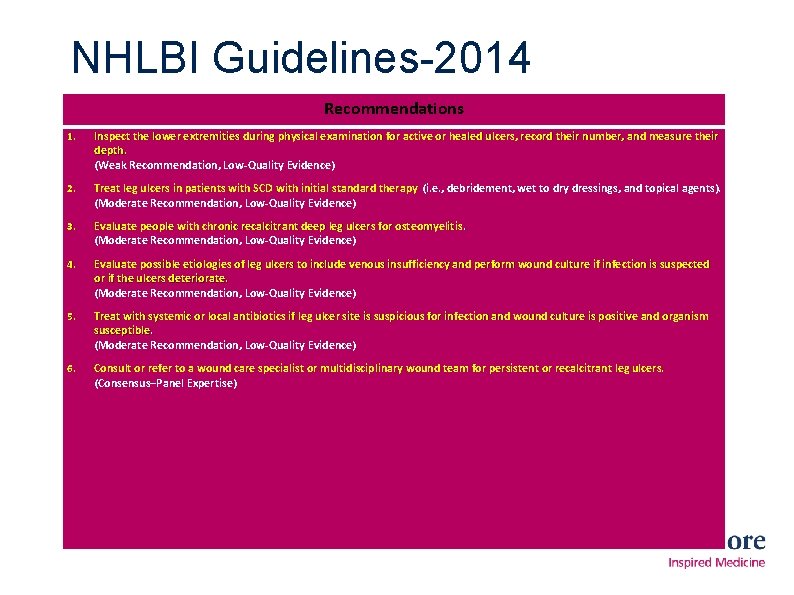
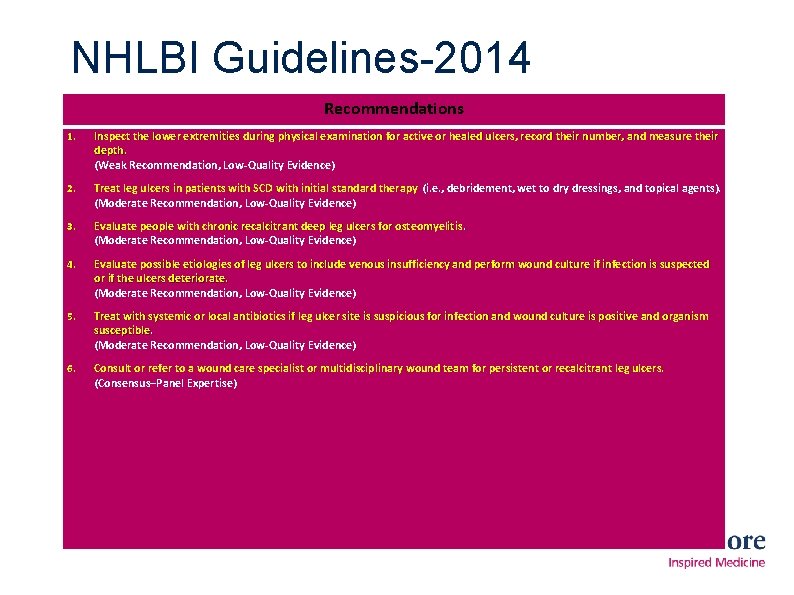
NHLBI Guidelines-2014 Recommendations 1. Inspect the lower extremities during physical examination for active or healed ulcers, record their number, and measure their depth. (Weak Recommendation, Low-Quality Evidence) 2. Treat leg ulcers in patients with SCD with initial standard therapy (i. e. , debridement, wet to dry dressings, and topical agents). (Moderate Recommendation, Low-Quality Evidence) 3. Evaluate people with chronic recalcitrant deep leg ulcers for osteomyelitis. (Moderate Recommendation, Low-Quality Evidence) 4. Evaluate possible etiologies of leg ulcers to include venous insufficiency and perform wound culture if infection is suspected or if the ulcers deteriorate. (Moderate Recommendation, Low-Quality Evidence) 5. Treat with systemic or local antibiotics if leg ulcer site is suspicious for infection and wound culture is positive and organism susceptible. (Moderate Recommendation, Low-Quality Evidence) 6. Consult or refer to a wound care specialist or multidisciplinary wound team for persistent or recalcitrant leg ulcers. (Consensus–Panel Expertise)
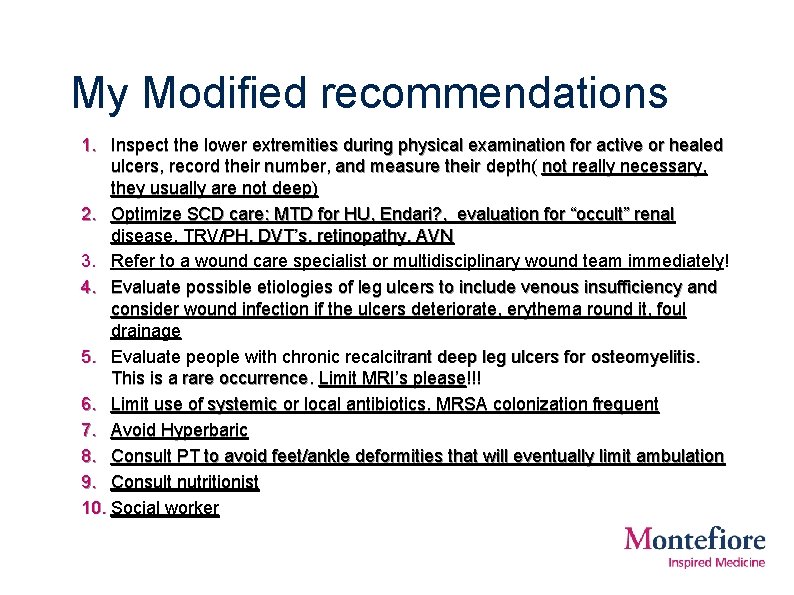
My Modified recommendations 1. Inspect the lower extremities during physical examination for active or healed ulcers, record their number, and measure their depth( not really necessary, they usually are not deep) 2. Optimize SCD care: MTD for HU, Endari? , evaluation for “occult” renal disease, TRV/PH, DVT’s, retinopathy, AVN 3. Refer to a wound care specialist or multidisciplinary wound team immediately! 4. Evaluate possible etiologies of leg ulcers to include venous insufficiency and consider wound infection if the ulcers deteriorate, erythema round it, foul drainage 5. Evaluate people with chronic recalcitrant deep leg ulcers for osteomyelitis. This is a rare occurrence. Limit MRI’s please!!! 6. Limit use of systemic or local antibiotics. MRSA colonization frequent 7. Avoid Hyperbaric 8. Consult PT to avoid feet/ankle deformities that will eventually limit ambulation 9. Consult nutritionist 10. Social worker
Treatment of the patient with SCD and a chronic leg ulcer • Provide Systemic therapy and support: Treat the patient!!! – Physical – Psychosocial – Nutritional • Provide principle-based topical therapy • Ongoing evaluations, comprehensive care
Systemic Support: What is the right intervention? • Treatments aimed at improving SCD – Hydroxyurea, Endari – Transfusions – Bone marrow transplantation • Treatments aimed at improving the host – Nutrition – Pain management – Psychosocial/Stigma – Environmental/Stress
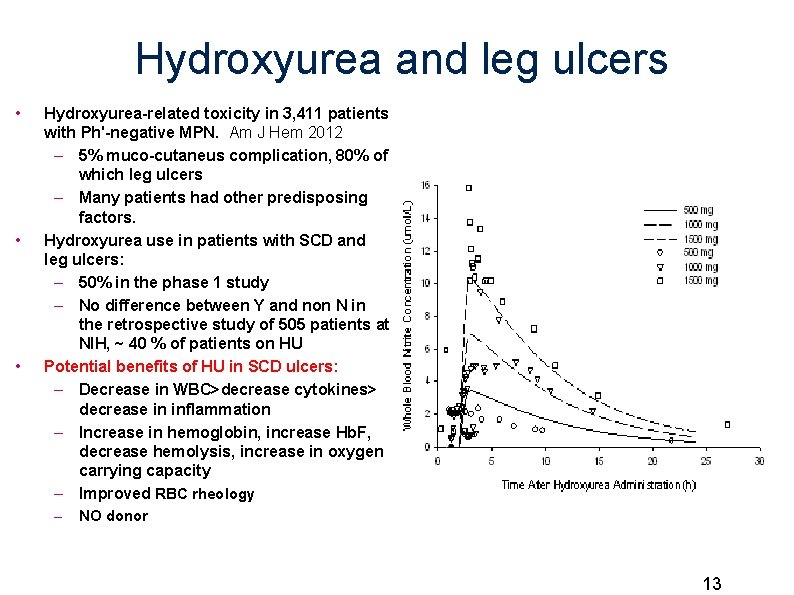
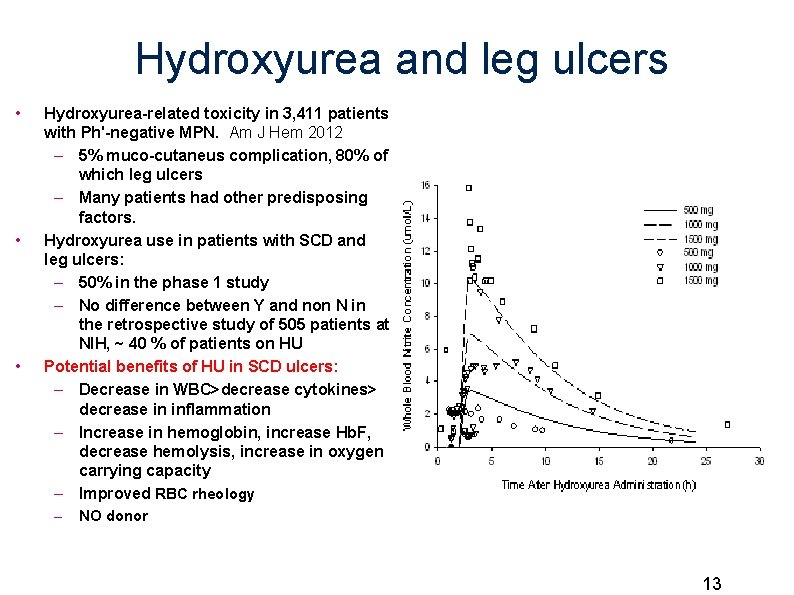
Hydroxyurea and leg ulcers • • • Hydroxyurea-related toxicity in 3, 411 patients with Ph'-negative MPN. Am J Hem 2012 – 5% muco-cutaneus complication, 80% of which leg ulcers – Many patients had other predisposing factors. Hydroxyurea use in patients with SCD and leg ulcers: – 50% in the phase 1 study – No difference between Y and non N in the retrospective study of 505 patients at NIH, ~ 40 % of patients on HU Potential benefits of HU in SCD ulcers: – Decrease in WBC>decrease cytokines> decrease in inflammation – Increase in hemoglobin, increase Hb. F, decrease hemolysis, increase in oxygen carrying capacity – Improved RBC rheology – NO donor 13
My approach to HU and leg ulcers • Make sure you have reached MTD and a robust F response • Do not stop it unless you are convinced that it is necessary • If you stop it, consider switching to transfusions to avoid increase in VOC, other complications • Measure the wound carefully when you stop it and, if not healed within 3 -6 months, go back to HU, it probably was not the culprit
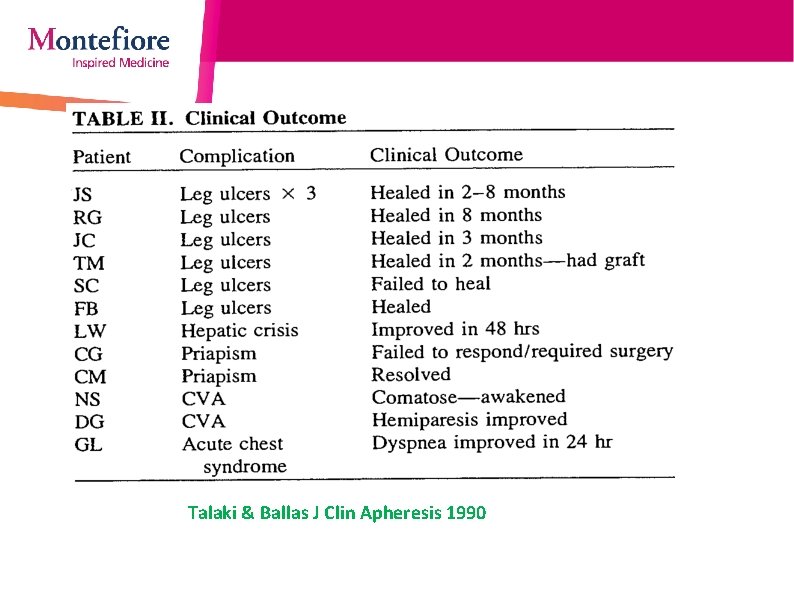
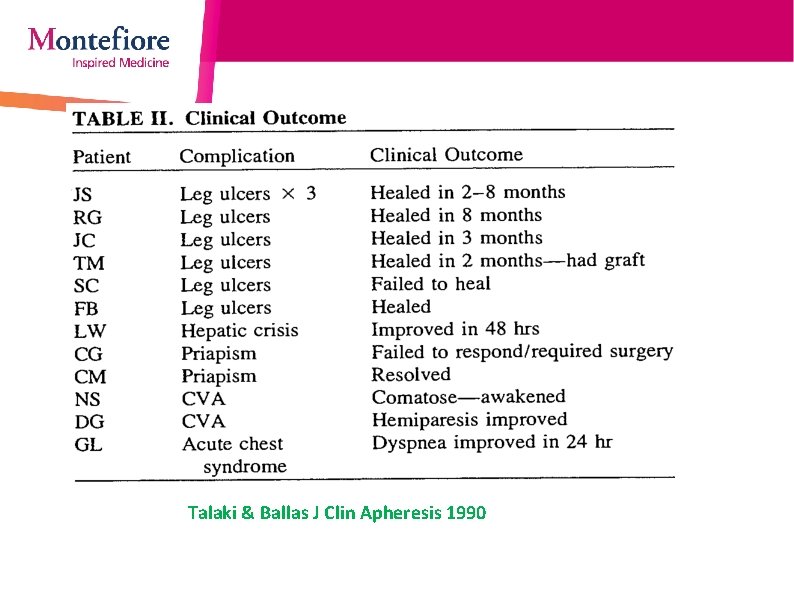
Transfusion and leg ulcers Talaki & Ballas J Clin Apheresis 1990
My approach to transfusions and leg ulcers • The highest chance of success is with the first ulcer, less than 60 days old, less than 10 cm 2 • In chronic wounds : Do not do it only for wound healing, most of the times there will be no improvement • If you have other reasons to start and the patient has a leg ulcer, go ahead • Do it for a pre-determined amount of time, and measure before you start and when you stop to see if there is a significant change in size • Beware of iron overload, as it could defeat the purpose
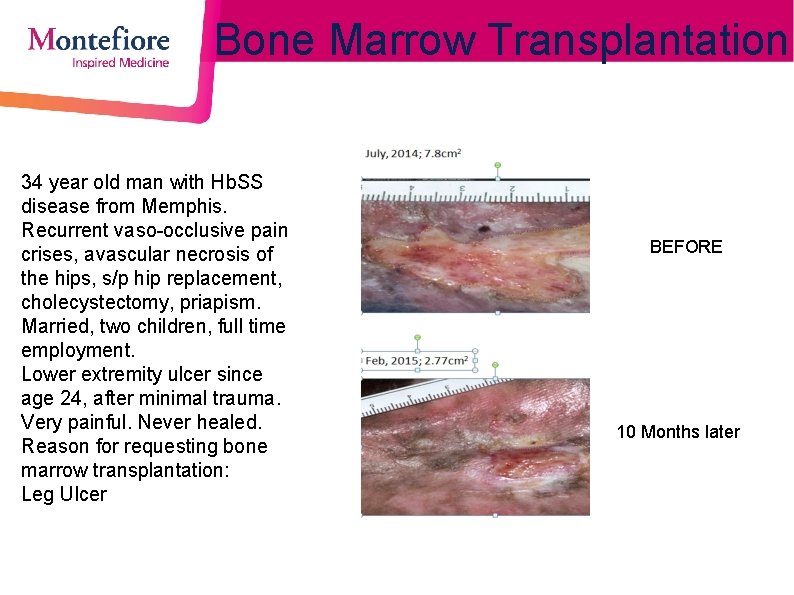
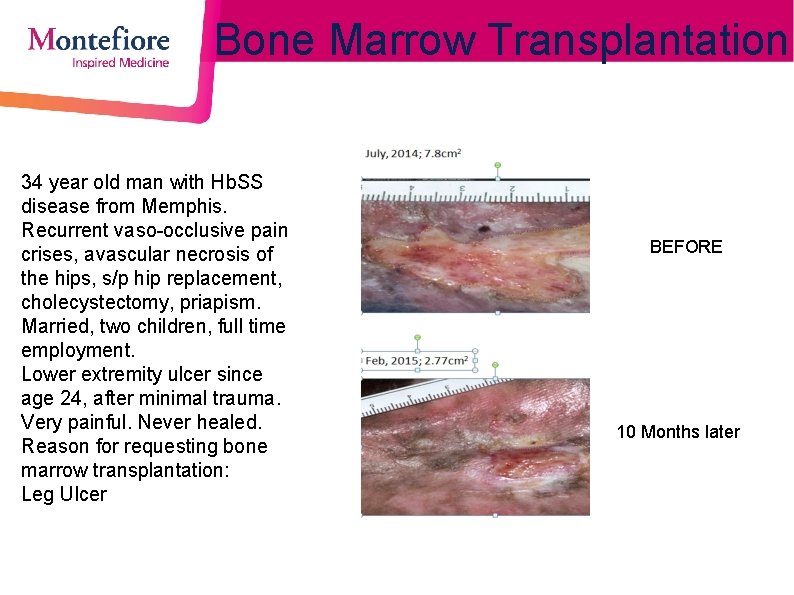
Bone Marrow Transplantation 34 year old man with Hb. SS disease from Memphis. Recurrent vaso-occlusive pain crises, avascular necrosis of the hips, s/p hip replacement, cholecystectomy, priapism. Married, two children, full time employment. Lower extremity ulcer since age 24, after minimal trauma. Very painful. Never healed. Reason for requesting bone marrow transplantation: Leg Ulcer BEFORE 10 Months later
Pain in SCD ulcers: Personal observations • Acute, stabbing, burning pain starts BEFORE ulcer appear • Pain not correlated with ulcer size • If there is an acute pain exacerbation often ulcer is deteriorating • Less pain as ulcer become more chronic, then neuropathy ensues • Chronic ulcers often associated with numbing, tingling of lateral aspect of foot, nail atrophy/abnormalities • Pain leads to poor use of the fulcrum of the foot: – Frozen ankle> walking on tippy toes – Poor use of gastrocnemius pump: calf atrophy – Feet deformities – Weal chair bound
Goal of nutrition in wound healing • Provision of an adequate nutritional substrate on a daily base – – Calories Fluids Protein Minerals and vitamins • Goal: maintain body composition and replete any lost lean body mass • Patients that do not meet these requirements are unlikely to be able to build new tissue to heal a wound
Nutritional/self care for optimal wound healing • Eat five meals a day: three major, with breakfast as the main one and two snacks, rich in antioxidants and protein( 20 -30 gr/day) • Arginine/Glutamine supplementation: Endari? • Vit C: 200 mg tid a day • Zinc oxide: 220 tid • B vitamin complex • Omega 3: ? • Sleep: at least 6 hours • Decrease stress: Yoga, meditation


Approach to the care of lower extremities ulcers in SCD patients 1. History 2. Infection 3. Debridement 4. Primary Dressing 5. Control Drainage 6. Compression
Approach to Sickle Cell Ulcers: History • Size, location, duration and past treatments –Duration >60 -90 days, poor prognosis • 82 v 35% healing at 24 weeks –Size >8 -10 cm 2, poor prognosis • 65 v 35% healing at 24 weeks • Work up before compression –Arterial Doppler : ABI –Venous reflux studies: to r/o venous insufficiency. Very Common! • 32% in a series from France –Venous doppler: to r/o DVT ( 10 -15%) –ELEVATION-Bed Rest: first recommendation to patients Factors predictive of leg-ulcer healing in sickle cell disease: a multicentre, prospective cohort study. Senet P, et al. Br J Dermatol. 2017 Use of a national Electronic Health Record network to describe characteristics and healing patterns of sickle cell ulcers. Flattau A … Minniti, C. Adv Wound Care. 2018, in press
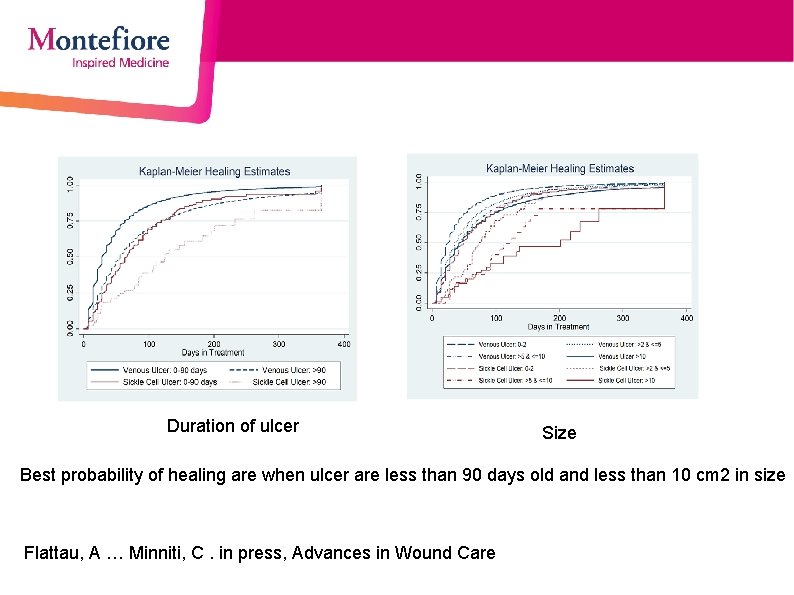
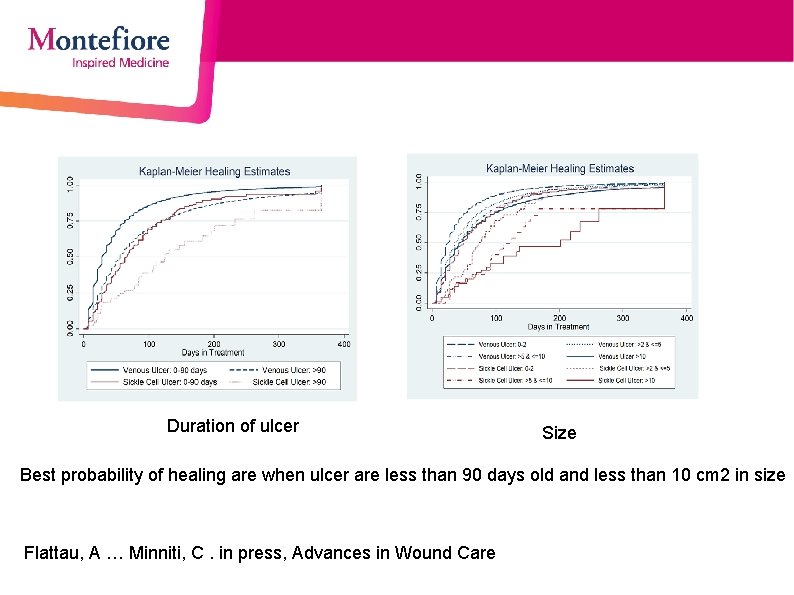
Duration of ulcer Size Best probability of healing are when ulcer are less than 90 days old and less than 10 cm 2 in size Flattau, A … Minniti, C. in press, Advances in Wound Care
Approach to Sickle Cell Ulcers: How to Evaluate for Infection • All (chronic) wounds are colonized and have a biofilm – Often colonized by Staph/MRSA – Wound cultures have limited use • Look for signs of infection: increase in pain, worsening wound, odor, green drainage, cellulitis, peri-wound erythema – obtain deep tissue culture → topical/oral abs • Avoid over treating with Abx, as resistance develops quickly • If positive culture + no change in acute signs of infection → IV abs • If suspicious for osteomyelitis – CRP levels → MRI →Bone biopsy and > 6 weeks of Abx (consult ID)
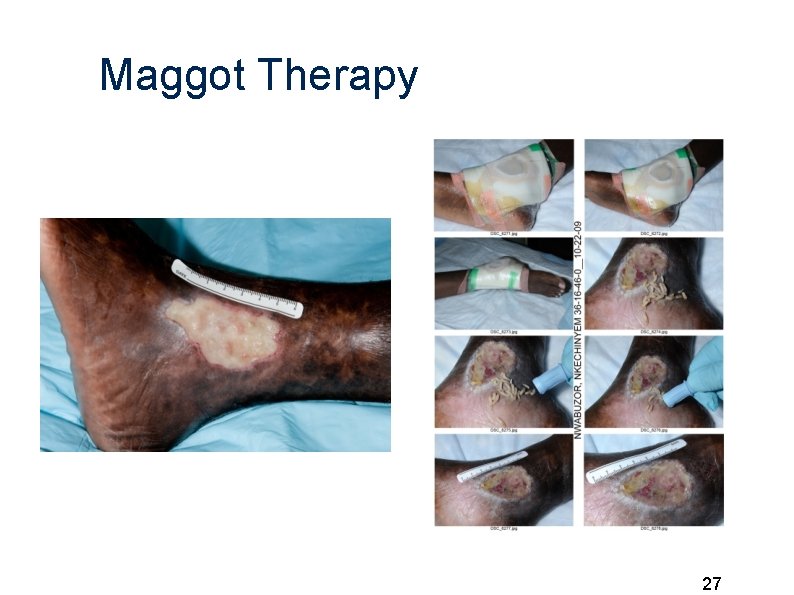
Approach to Sickle Cell Ulcers: Debridement • Evaluate for necrotic tissue ---> if needed, weekly bed-side, conservative sharp debridement until 100% granulation. • Needs topical anesthetic and sometimes oral opioids • May use biologic debridement: Maggots (for patients that could not go to the OR) • If epibole occurs (close edges), may need surgical debridement/ and cut margins to re-ignite the proliferation of cells, to be done in the OR
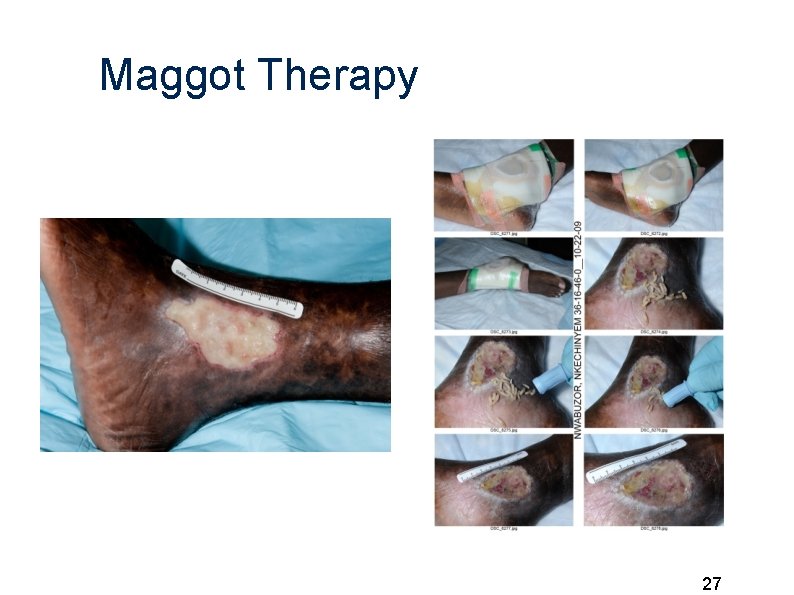
Maggot Therapy 27
Approach to Sickle Cell Ulcers: Control drainage • Moderate-Severe: –Calcium Alginate vs Cellulose + secondary absorbent dressing • Light: –Foam dressing –Silicone dressings
Primary Dressing: In contact with the wound Once drainage decreases primary dressing changes to: • -Hydrophera blue • -Acticoat • -Bactroban • -Honey
Approach to Sickle Cell Ulcers: Compression • Four Layer dressing: Profore vs • Two layer dressing: Kerlix + Coban vs • Real Compression stockings ( not the ted hose that are used in the hospital)

Questions? Suggestions? • Email at cminniti@montefiore. org • Call : 718 -920 -4180
Topical Sodium Nitrite may restore Nitric Oxide bioactivity in sickle cell leg ulcers • Human hemoglobin serves as an oxygen- and p. H dependent nitrite reductase. Reduces Sodium Nitrite into Nitric Oxide (NO) in low oxygen tissues • Thus, topical Sodium Nitrite treatment may restore NO bioactivity and provide selective vasodilation to hypoxemic tissues in sickle cell ulcers. • Sodium Nitrite has antimicrobial activity, which may alter the ulcer biofilm/microbiome and promote wound healing
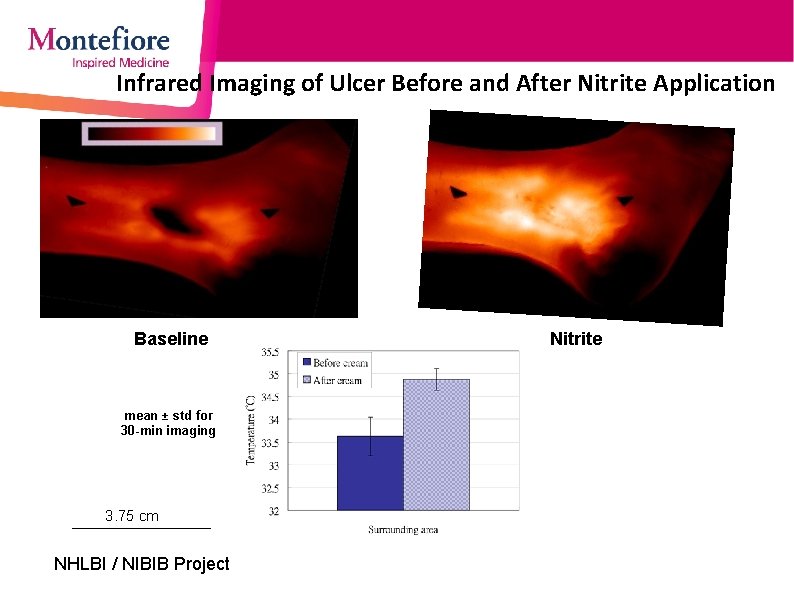
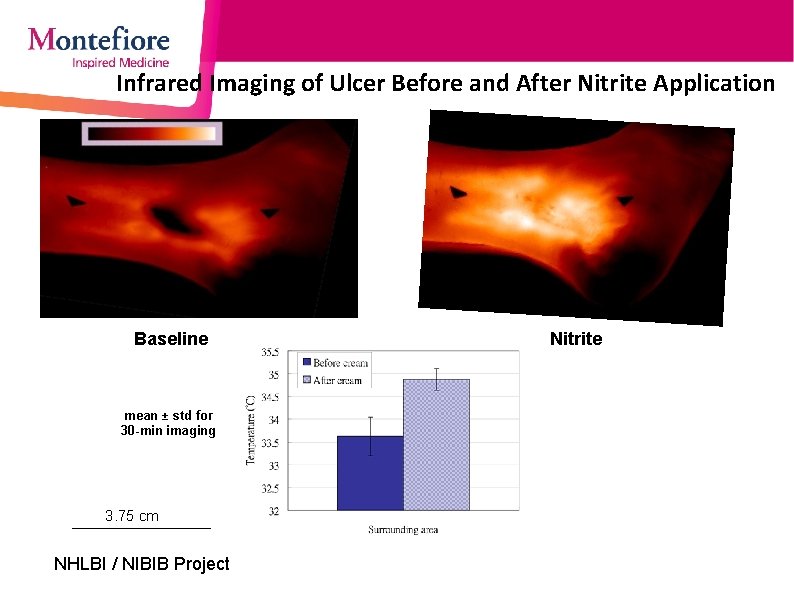
Infrared Imaging of Ulcer Before and After Nitrite Application Baseline mean ± std for 30 -min imaging 3. 75 cm NHLBI / NIBIB Project Nitrite
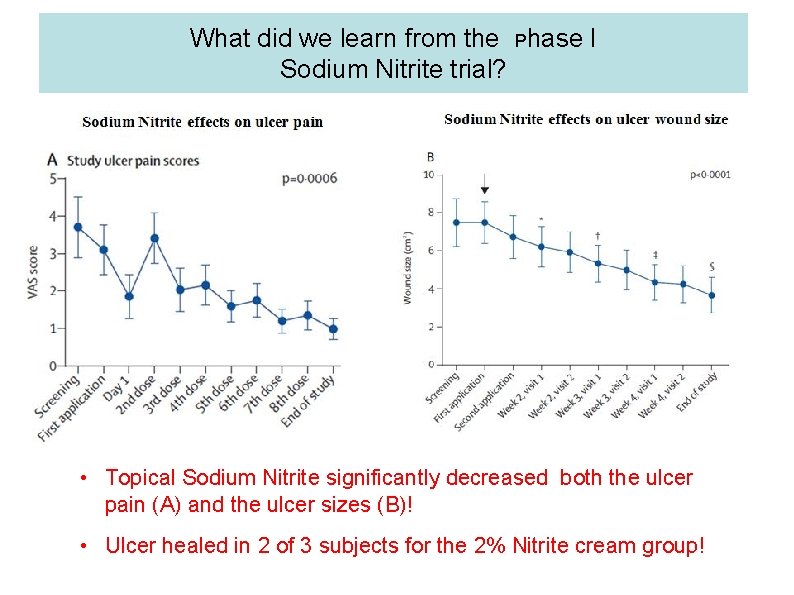
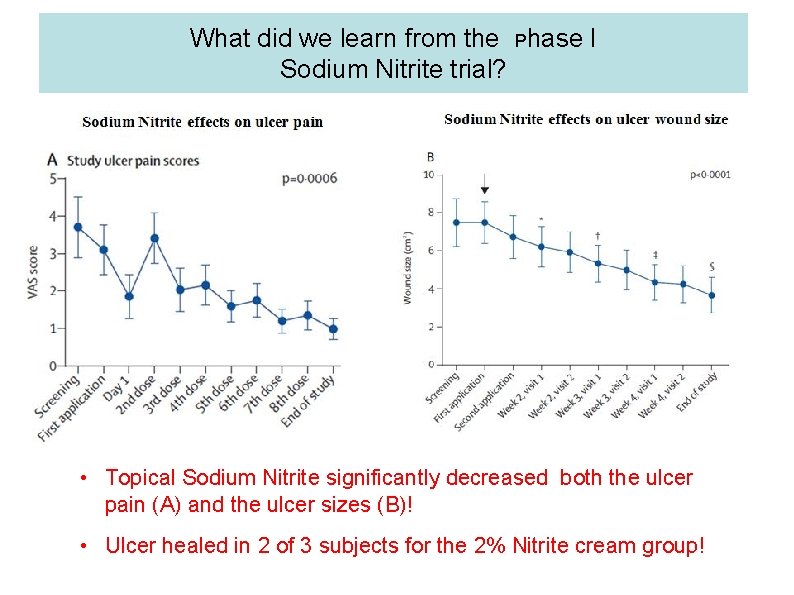
What did we learn from the Phase I Sodium Nitrite trial? • Topical Sodium Nitrite significantly decreased both the ulcer pain (A) and the ulcer sizes (B)! • Ulcer healed in 2 of 3 subjects for the 2% Nitrite cream group!
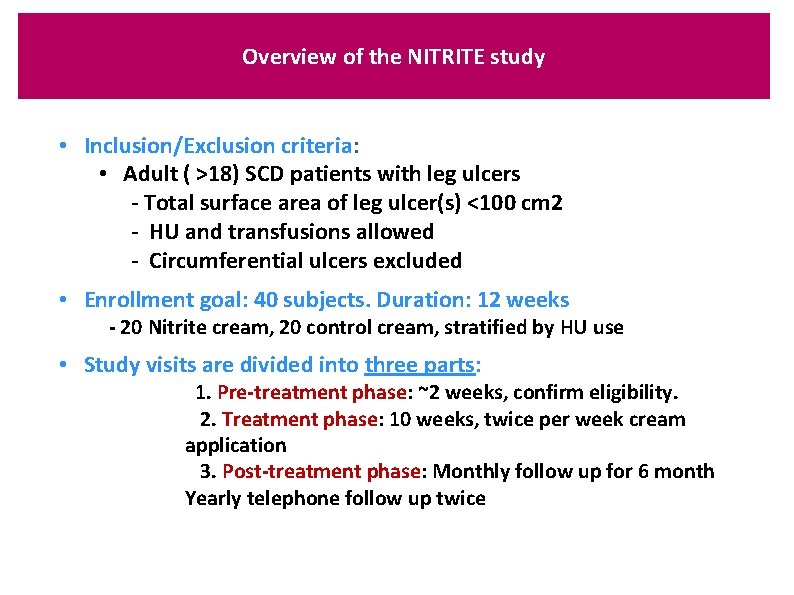
Overview of the NITRITE study • Inclusion/Exclusion criteria: • Adult ( >18) SCD patients with leg ulcers - Total surface area of leg ulcer(s) <100 cm 2 - HU and transfusions allowed - Circumferential ulcers excluded • Enrollment goal: 40 subjects. Duration: 12 weeks - 20 Nitrite cream, 20 control cream, stratified by HU use • Study visits are divided into three parts: 1. Pre-treatment phase: ~2 weeks, confirm eligibility. 2. Treatment phase: 10 weeks, twice per week cream application 3. Post-treatment phase: Monthly follow up for 6 month Yearly telephone follow up twice
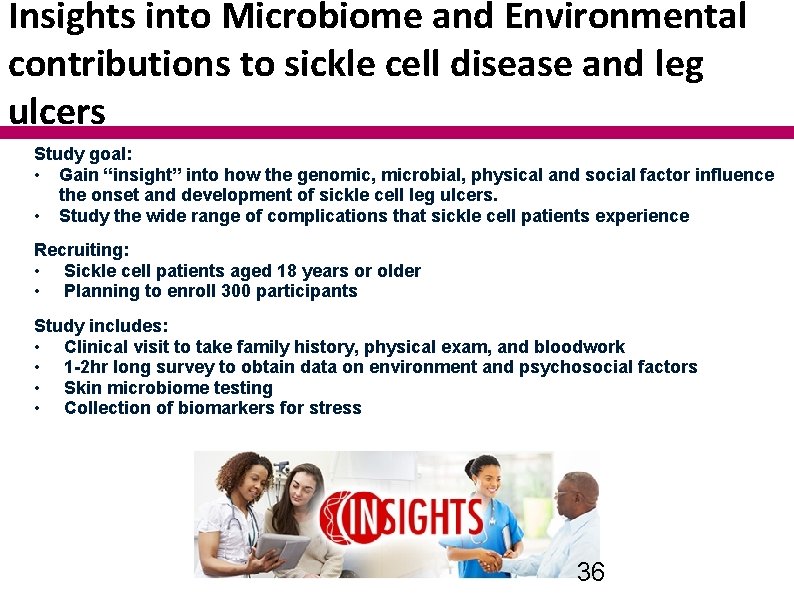
Insights into Microbiome and Environmental contributions to sickle cell disease and leg ulcers Study goal: • Gain “insight” into how the genomic, microbial, physical and social factor influence the onset and development of sickle cell leg ulcers. • Study the wide range of complications that sickle cell patients experience Recruiting: • Sickle cell patients aged 18 years or older • Planning to enroll 300 participants Study includes: • Clinical visit to take family history, physical exam, and bloodwork • 1 -2 hr long survey to obtain data on environment and psychosocial factors • Skin microbiome testing • Collection of biomarkers for stress 36
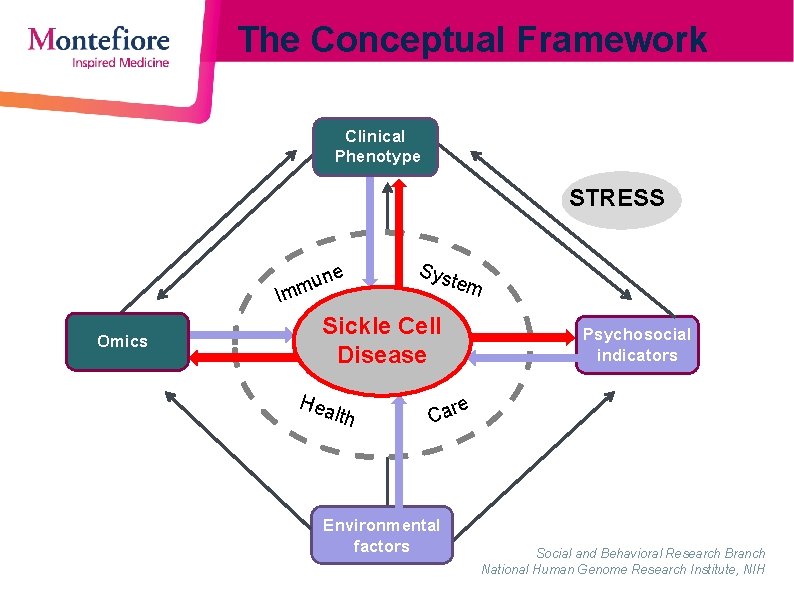
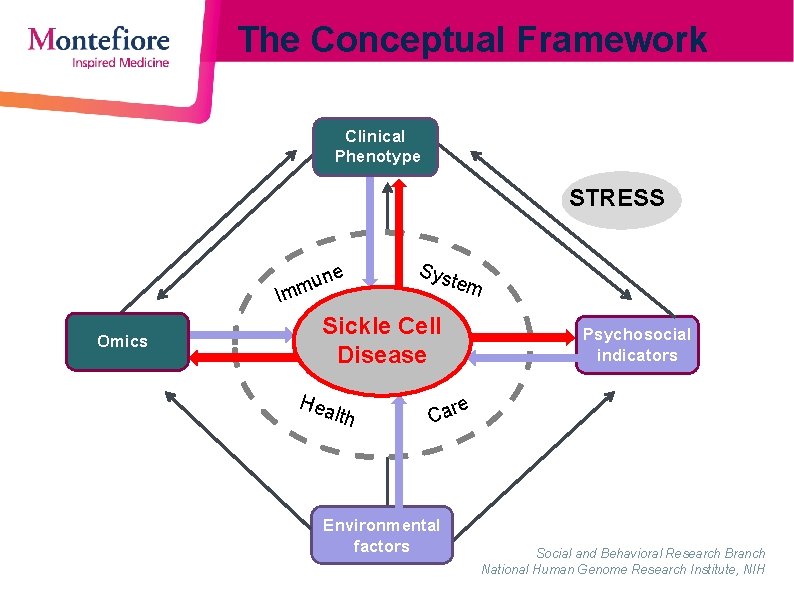
The Conceptual Framework Clinical Phenotype STRESS ne mu Im Omics Sys tem Sickle Cell Disease Hea lth Psychosocial indicators e Car Environmental factors Social and Behavioral Research Branch National Human Genome Research Institute, NIH
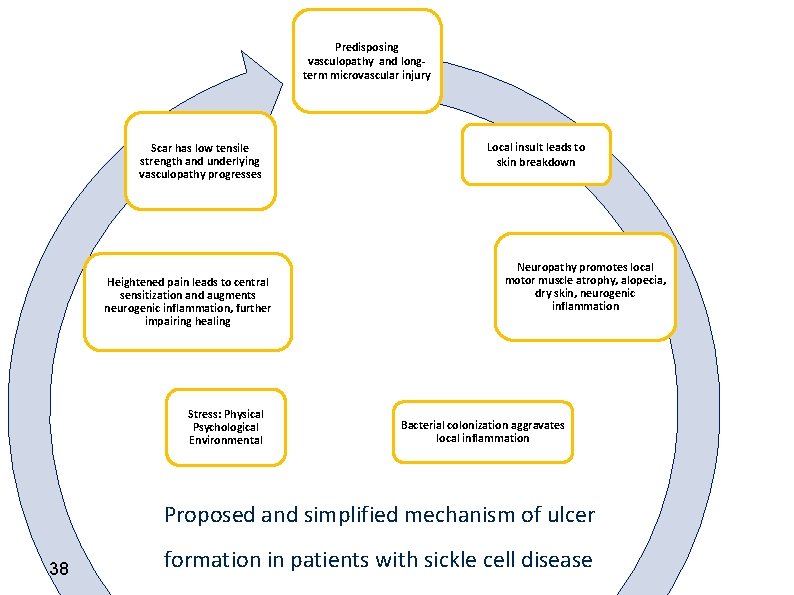
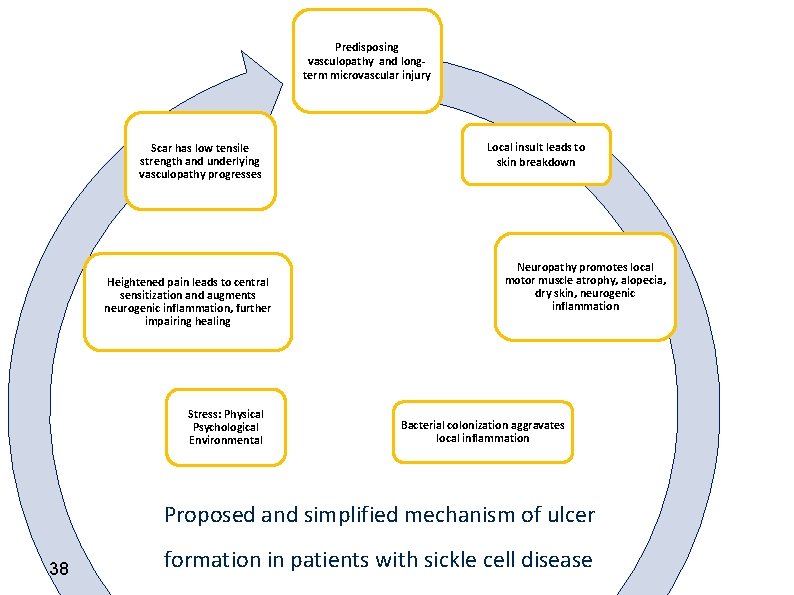
Predisposing vasculopathy and longterm microvascular injury Scar has low tensile strength and underlying vasculopathy progresses Heightened pain leads to central sensitization and augments neurogenic inflammation, further impairing healing Stress: Physical Psychological Environmental Local insult leads to skin breakdown Neuropathy promotes local motor muscle atrophy, alopecia, dry skin, neurogenic inflammation Bacterial colonization aggravates local inflammation Proposed and simplified mechanism of ulcer 38 formation in patients with sickle cell disease

 Hydrophera blue
Hydrophera blue Hypotonuse leg
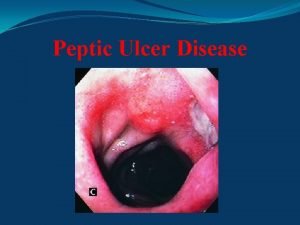
Hypotonuse leg Peptic ulcer classification
Peptic ulcer classification Gastric ulcer
Gastric ulcer Types of ulcer edge
Types of ulcer edge Pressure mapping for pressure ulcers
Pressure mapping for pressure ulcers Anorexia and stomach ulcers
Anorexia and stomach ulcers Dehydration gastritis
Dehydration gastritis Gastric ulcer definition
Gastric ulcer definition Ambulatory venous hypertension theory
Ambulatory venous hypertension theory Typhoid ulcer and tuberculous ulcer
Typhoid ulcer and tuberculous ulcer Caterina bertone - wikipedia
Caterina bertone - wikipedia Caterina biscari
Caterina biscari Caterina spinaris
Caterina spinaris Caterina ranieri alba
Caterina ranieri alba Caterina cas
Caterina cas Chiara giugliano
Chiara giugliano Etichette ambientali
Etichette ambientali Caterina todaro
Caterina todaro Adriana radu colegiul national iasi
Adriana radu colegiul national iasi Leonardo da vinci e caterina da siena
Leonardo da vinci e caterina da siena Caterina perugini
Caterina perugini Cubierta mercado santa caterina
Cubierta mercado santa caterina Perimylolysis
Perimylolysis Chapter 55 care of patients with stomach disorders
Chapter 55 care of patients with stomach disorders Nursing management of liver abscess
Nursing management of liver abscess Pico question
Pico question Periodontal management of medically compromised patients
Periodontal management of medically compromised patients Nursing care of cataract
Nursing care of cataract Module 70 introduction to therapy
Module 70 introduction to therapy Medicare improvements for patients and providers act
Medicare improvements for patients and providers act Patients rights and responsibilities nabh
Patients rights and responsibilities nabh Diagnosis and treatment plan of complete denture
Diagnosis and treatment plan of complete denture Dealing with challenging patients
Dealing with challenging patients Dope mnemonic emt
Dope mnemonic emt Factors of care that patients can expect to receive
Factors of care that patients can expect to receive Ems lifting and moving patients
Ems lifting and moving patients Safe staffing ratios benefiting nurses and patients
Safe staffing ratios benefiting nurses and patients Some patients shout in pain while ______ an injection.
Some patients shout in pain while ______ an injection. Safe patient handling algorithms
Safe patient handling algorithms