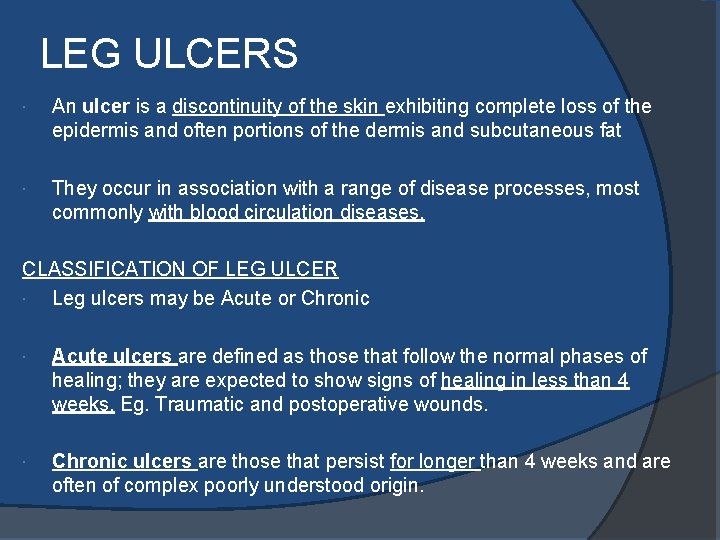
LEG ULCERS An ulcer is a discontinuity of


- Slides: 20
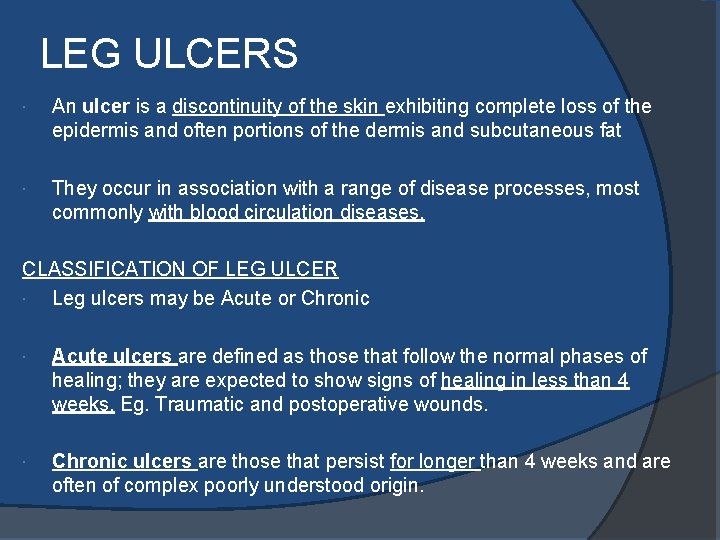
LEG ULCERS An ulcer is a discontinuity of the skin exhibiting complete loss of the epidermis and often portions of the dermis and subcutaneous fat They occur in association with a range of disease processes, most commonly with blood circulation diseases. CLASSIFICATION OF LEG ULCER Leg ulcers may be Acute or Chronic Acute ulcers are defined as those that follow the normal phases of healing; they are expected to show signs of healing in less than 4 weeks. Eg. Traumatic and postoperative wounds. Chronic ulcers are those that persist for longer than 4 weeks and are often of complex poorly understood origin.
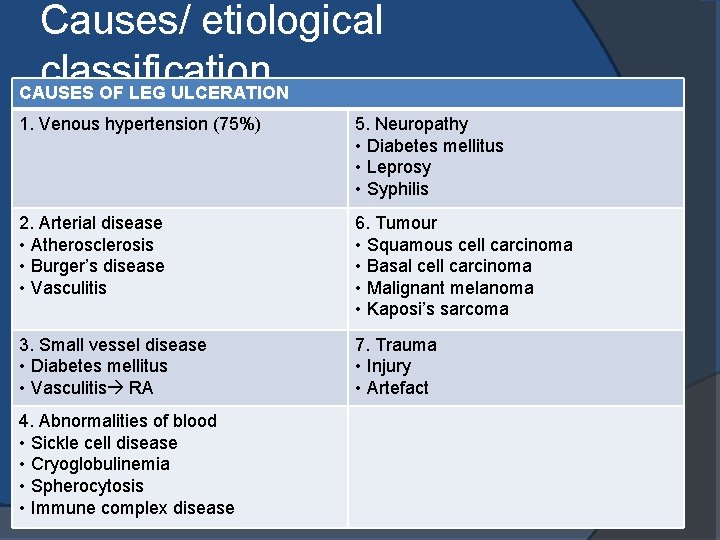
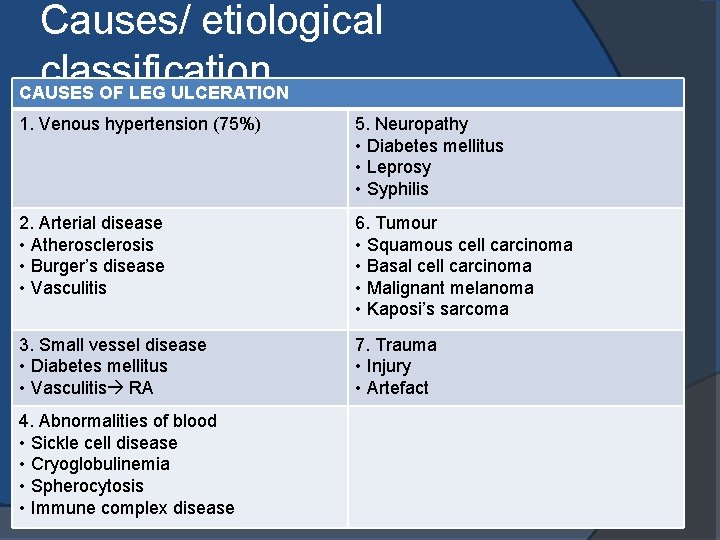
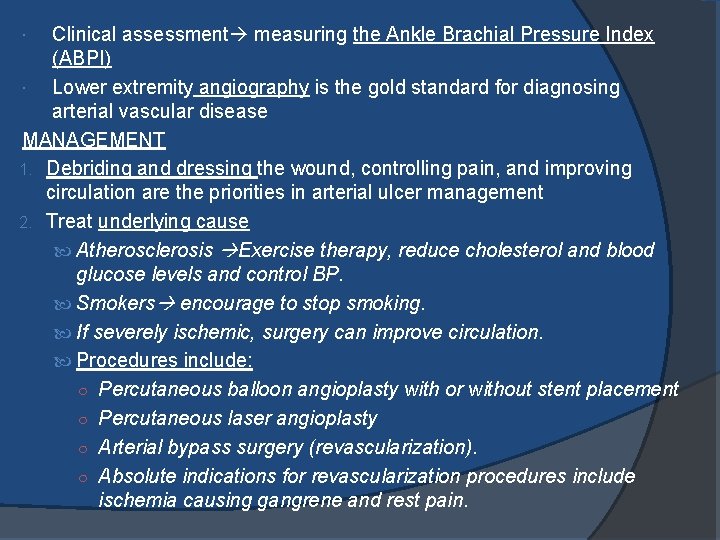
Causes/ etiological classification CAUSES OF LEG ULCERATION 1. Venous hypertension (75%) 5. Neuropathy • Diabetes mellitus • Leprosy • Syphilis 2. Arterial disease • Atherosclerosis • Burger’s disease • Vasculitis 6. Tumour • Squamous cell carcinoma • Basal cell carcinoma • Malignant melanoma • Kaposi’s sarcoma 3. Small vessel disease • Diabetes mellitus • Vasculitis RA 7. Trauma • Injury • Artefact 4. Abnormalities of blood • Sickle cell disease • Cryoglobulinemia • Spherocytosis • Immune complex disease
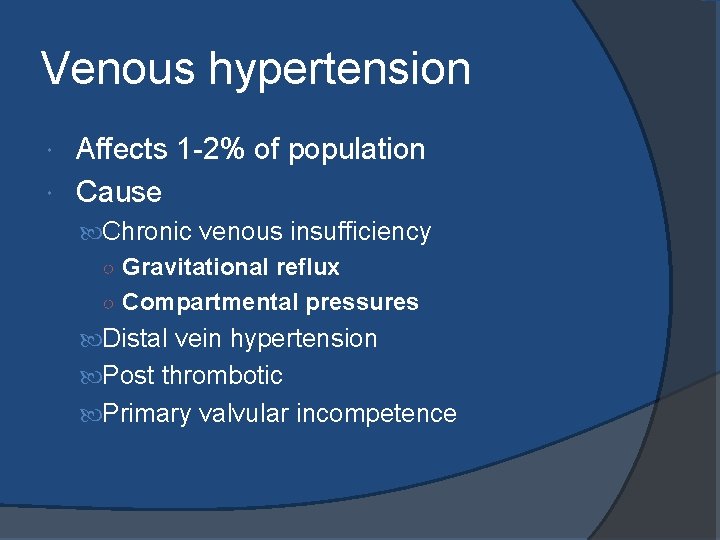
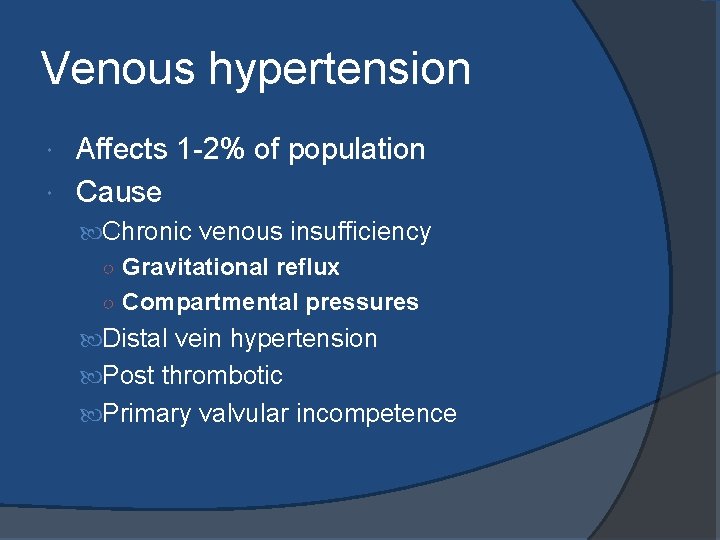
Venous hypertension Affects 1 -2% of population Cause Chronic venous insufficiency ○ Gravitational reflux ○ Compartmental pressures Distal vein hypertension Post thrombotic Primary valvular incompetence
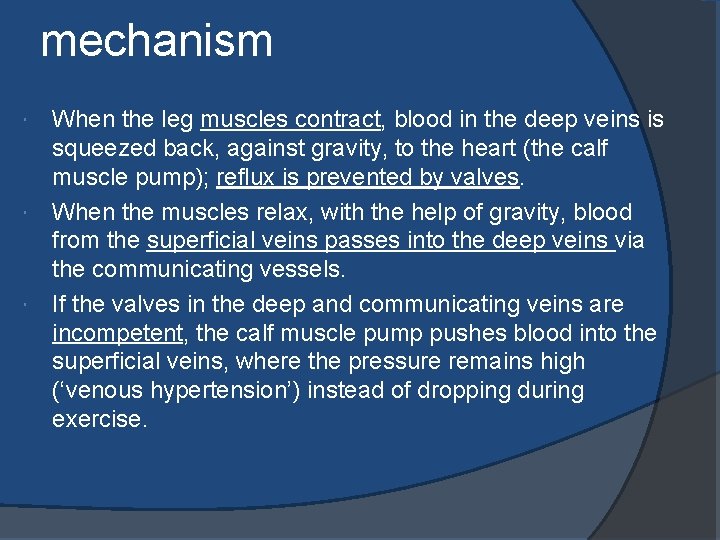
mechanism When the leg muscles contract, blood in the deep veins is squeezed back, against gravity, to the heart (the calf muscle pump); reflux is prevented by valves. When the muscles relax, with the help of gravity, blood from the superficial veins passes into the deep veins via the communicating vessels. If the valves in the deep and communicating veins are incompetent, the calf muscle pump pushes blood into the superficial veins, where the pressure remains high (‘venous hypertension’) instead of dropping during exercise.
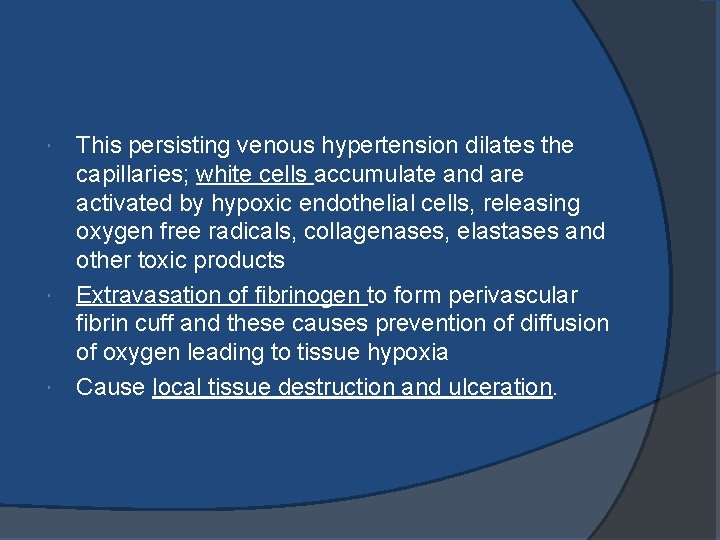
This persisting venous hypertension dilates the capillaries; white cells accumulate and are activated by hypoxic endothelial cells, releasing oxygen free radicals, collagenases, elastases and other toxic products Extravasation of fibrinogen to form perivascular fibrin cuff and these causes prevention of diffusion of oxygen leading to tissue hypoxia Cause local tissue destruction and ulceration.
local examination- venous ulcer Occur anywhere between the knee and the ankle, with medial and lateral malleolus the most common sites. Usually superficial. Wound beds vary in appearance, frequently beefy red, granular tissue Calcification in wound base is common Have moderate to heavy exudate. Tend to be large with irregular margins.
Local examination-venous ulcer Surrounding skin is characterized by hyperpigmentation, dermatitis, and lipodermatosclerosis. Associated with aching and heavy legs that feel more comfortable when elevated Relatively painless unless infected. Pitting oedema Surrounded by mottled brown or black staining and/or dry, itchy and reddened skin (gravitational or venous eczema). May be associated with varicose veins due to incompetence of the superficial venous system (50%). Thickened skin, hyperkeratosis (scaliness), papillomatosis, fissuring, oozing. Scattered petechiae

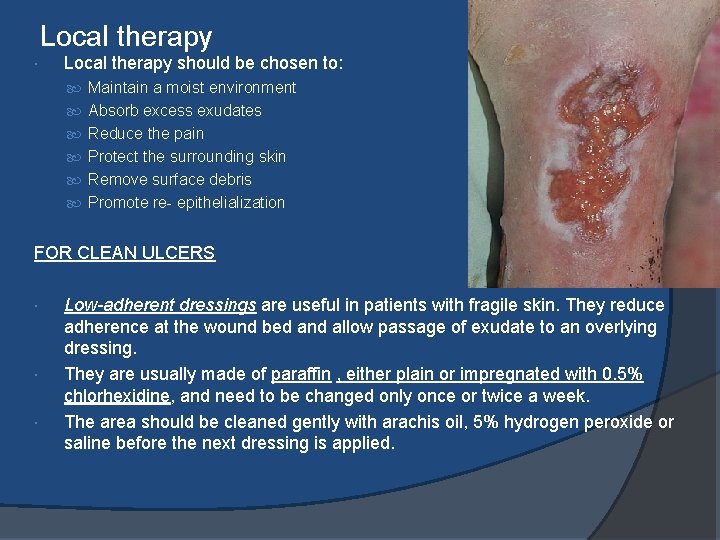
Large venous ulcer overlying the medial malleolus.
investigations Blood glucose. Full blood count to detect anaemia Wound Swabs for culture and sensitivity Venography, color flow duplex scanning and the measurement of ambulatory venous pressure to detect surgically remediable causes of venous incompetence. Doppler ultrasound to assess arterial circulation when atherosclerosis is likely. Cardiac evaluation for congestive failure. If the maximal systolic ankle pressure divided by the systolic brachial pressure (‘ankle brachial pressure index’) is greater than 0. 8, the ulcer is unlikely to be caused by arterial disease. Normal range 1. 0 - 1. 2 >0. 8 Venous Ulcer <0. 8 Arterial Ulcer
management GENERAL MEASURES Pressure bandages, leg elevation and bed in absence of arterial disease Compression bandages and stockings Compression results in healing of 40 -70% of chronic venous ulcers within 12 weeks. Achieved by using a stocking or bandage that is wrapped from the toes or foot to the area below the knee. This externally created pressure on the leg helps to heal the ulcer by increasing the calf muscle pump action and reduce swelling in the leg. Compression is not used if the ABPI is below 0. 8. Elevation of the affected limb Preferably above the hips, this aids venous drainage, decreases oedema and raises oxygen tension in the limb. for at least 2 h every afternoon. Walking, in moderation, is beneficial Physiotherapy such as leg exercises, elevation, gentle massage, intermittent pneumatic compression and graduated compression bandaging. Diet For patients who are obese and should lose weight.
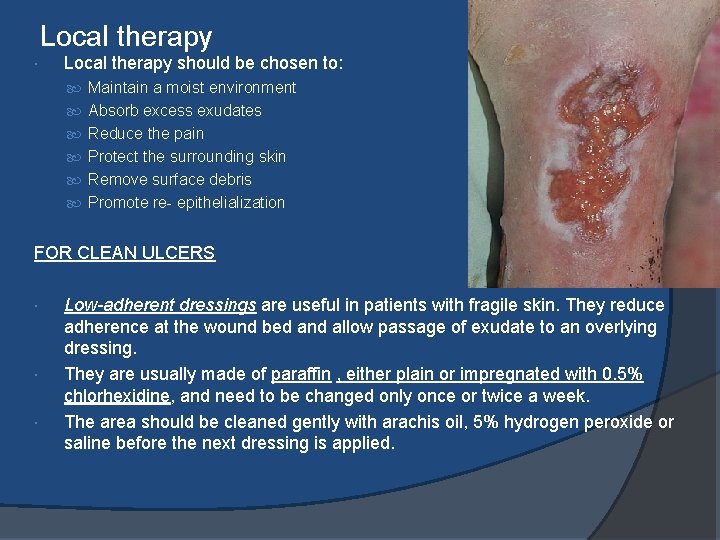
Local therapy should be chosen to: Maintain a moist environment Absorb excess exudates Reduce the pain Protect the surrounding skin Remove surface debris Promote re- epithelialization FOR CLEAN ULCERS Low-adherent dressings are useful in patients with fragile skin. They reduce adherence at the wound bed and allow passage of exudate to an overlying dressing. They are usually made of paraffin , either plain or impregnated with 0. 5% chlorhexidine, and need to be changed only once or twice a week. The area should be cleaned gently with arachis oil, 5% hydrogen peroxide or saline before the next dressing is applied.
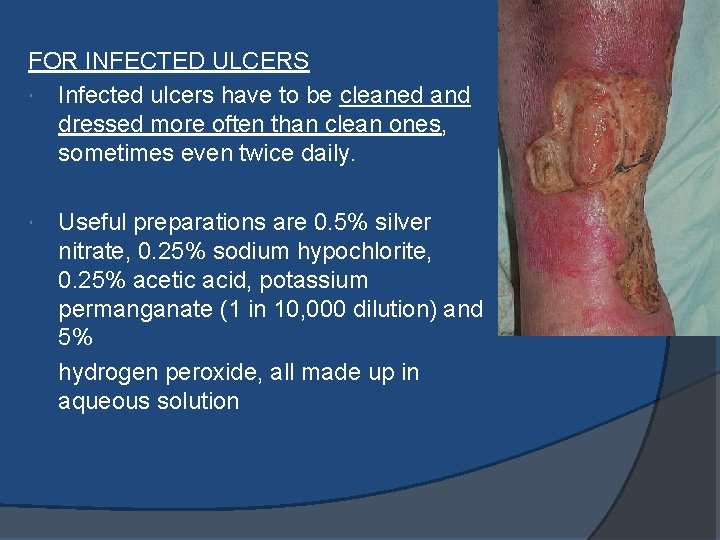
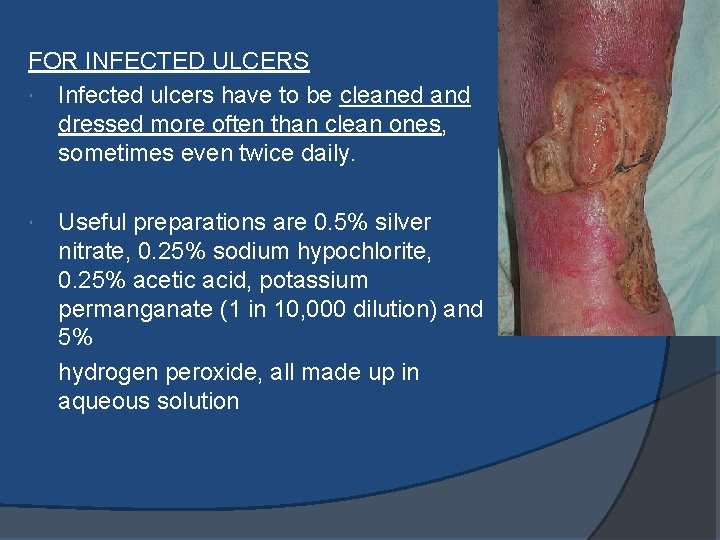
FOR INFECTED ULCERS Infected ulcers have to be cleaned and dressed more often than clean ones, sometimes even twice daily. Useful preparations are 0. 5% silver nitrate, 0. 25% sodium hypochlorite, 0. 25% acetic acid, potassium permanganate (1 in 10, 000 dilution) and 5% hydrogen peroxide, all made up in aqueous solution
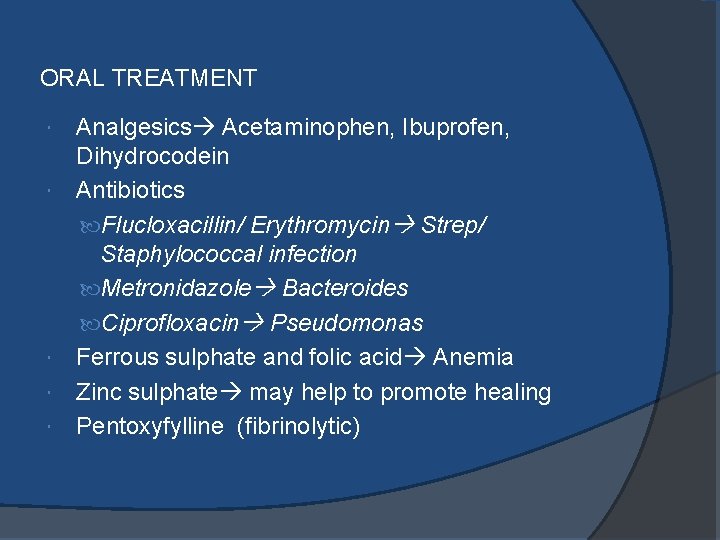
ORAL TREATMENT Analgesics Acetaminophen, Ibuprofen, Dihydrocodein Antibiotics Flucloxacillin/ Erythromycin Strep/ Staphylococcal infection Metronidazole Bacteroides Ciprofloxacin Pseudomonas Ferrous sulphate and folic acid Anemia Zinc sulphate may help to promote healing Pentoxyfylline (fibrinolytic)
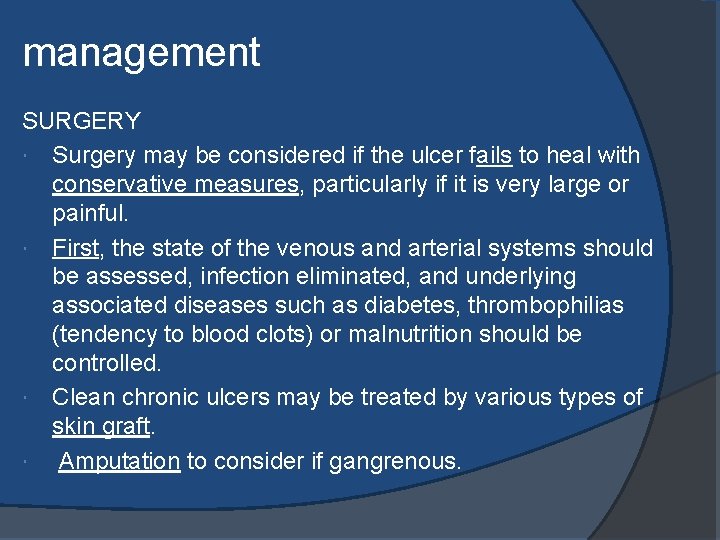
management SURGERY Surgery may be considered if the ulcer fails to heal with conservative measures, particularly if it is very large or painful. First, the state of the venous and arterial systems should be assessed, infection eliminated, and underlying associated diseases such as diabetes, thrombophilias (tendency to blood clots) or malnutrition should be controlled. Clean chronic ulcers may be treated by various types of skin graft. Amputation to consider if gangrenous.
complications Bacterial colonization is inevitable in a longstanding ulcer But needs systemic antibiotics only if there is pyrexia, a purulent discharge, rapid extension or an increase in pain, cellulitis, lymphangitis or septicaemia. Eczema is common around venous ulcers. Allergic contact dermatitis is a common complication and should be suspected if the rash worsens, itches or fails to improve with local treatment. Malignant change can occur. If an ulcer has a hyperplastic base or a rolled edge, biopsy may be needed to rule out a squamous cell carcinoma
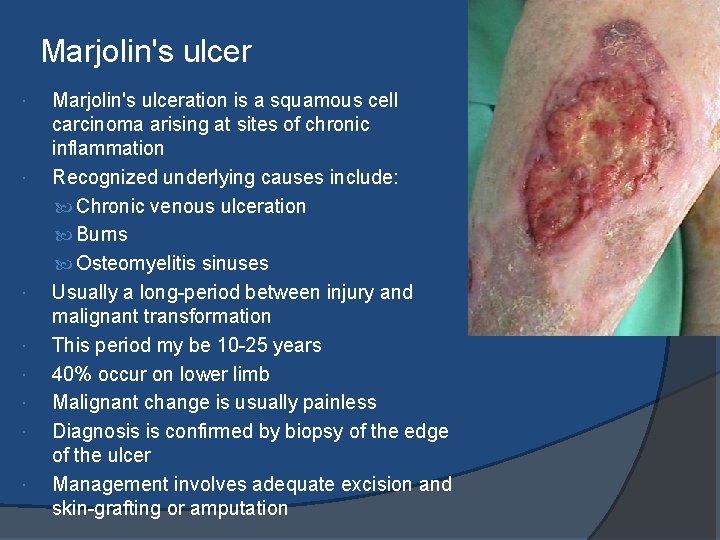
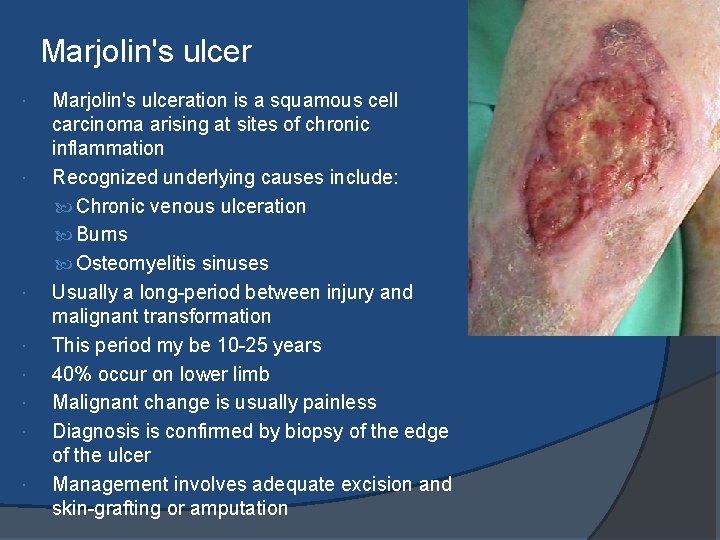
Marjolin's ulcer Marjolin's ulceration is a squamous cell carcinoma arising at sites of chronic inflammation Recognized underlying causes include: Chronic venous ulceration Burns Osteomyelitis sinuses Usually a long-period between injury and malignant transformation This period my be 10 -25 years 40% occur on lower limb Malignant change is usually painless Diagnosis is confirmed by biopsy of the edge of the ulcer Management involves adequate excision and skin-grafting or amputation
prevention To prevent leg ulcers and to promote healing of ulcers: Walk and exercise for at least an hour a day to keep the calf muscle pump working properly. Lose weight if overweight. Proper and balanced diet Stop smoking. Control diabetes Diabetic wound care Vascular ultrasounds to R/O varicose Cracks, sores or changes in colour should be sought for. Moisturizers should be applied after bathing. Comfortable well-fitting shoes and socks. When sitting, wriggle the toes, move the feet up and down and frequent walks to take. Avoid extremes of temperature such as hot baths or sitting close to a heater. Keep cold feet warm with socks and slippers.
Arterial ulcers Arterial ulcers result from an inadequate blood supply due to peripheral vascular disease, diabetes mellitus, trauma, or advanced age. Usually found on the feet, heels or toes. Frequently painful, particularly at night in bed or when the legs are at rest and elevated. This pain is relieved when the legs are lowered with feet on the floor as gravity causes more blood to flow into the legs. There may be cramp-like pains in the legs when walking, known as intermittent claudication, as the leg muscles do not receive enough oxygenated blood to function properly. Rest will relieve this pain during early stage.

The margins of the arterial ulcer are even, sharply demarcated and punched out. Wound maybe superficial or deep Wound beds are pale, gray or yellow with no evidence of new tissue growth Necrosis or cellulitis may be present; commonly accompanied by dry necrotic eschar and exposed tendons. Have minimum exudate. Periwound tissue may appear blanched or purpuric and is often shiny and tight Associated with cold white or bluish, shiny feet. Loss of hair at ankle or foot.
Clinical assessment measuring the Ankle Brachial Pressure Index (ABPI) Lower extremity angiography is the gold standard for diagnosing arterial vascular disease MANAGEMENT 1. Debriding and dressing the wound, controlling pain, and improving circulation are the priorities in arterial ulcer management 2. Treat underlying cause Atherosclerosis Exercise therapy, reduce cholesterol and blood glucose levels and control BP. Smokers encourage to stop smoking. If severely ischemic, surgery can improve circulation. Procedures include: ○ Percutaneous balloon angioplasty with or without stent placement ○ Percutaneous laser angioplasty ○ Arterial bypass surgery (revascularization). ○ Absolute indications for revascularization procedures include ischemia causing gangrene and rest pain.
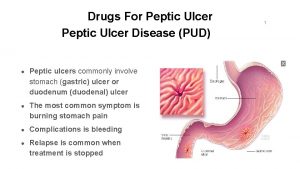
 Stomach ulcer diet menu
Stomach ulcer diet menu Classification of ulcer
Classification of ulcer Gasrectomy
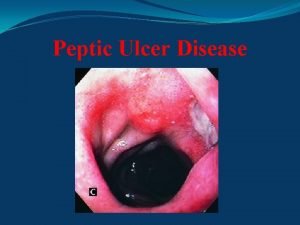
Gasrectomy Peptic ulcer classification
Peptic ulcer classification Gastric ulcer differential diagnosis
Gastric ulcer differential diagnosis Typhoid ulcer vs tuberculous ulcer
Typhoid ulcer vs tuberculous ulcer Hypotenuse-leg theorem
Hypotenuse-leg theorem Mendel sign peptic ulcer
Mendel sign peptic ulcer Peptic ulcer causes
Peptic ulcer causes Pictures of different types of ulcers
Pictures of different types of ulcers Excessive acid production
Excessive acid production Dehydration gastritis
Dehydration gastritis Ambulatory venous hypertension theory
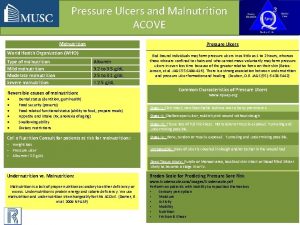
Ambulatory venous hypertension theory Pressure mapping for pressure ulcers
Pressure mapping for pressure ulcers Vertical asymptote
Vertical asymptote Interrupted time series vs regression discontinuity
Interrupted time series vs regression discontinuity 8-3 practice rational functions and their graphs
8-3 practice rational functions and their graphs Mohorovicic discontinuity
Mohorovicic discontinuity Technological discontinuity definition
Technological discontinuity definition Vertical
Vertical Removable discontinuity algebraically
Removable discontinuity algebraically