Case Report Medical Nutrition Therapy for Septic Shock
- Slides: 15
Case Report: Medical Nutrition Therapy for Septic Shock ANGELA GASBARRE ARAMARK DIETETIC INTERNSHIP UPPER CHESAPEAKE MEDICAL CENTER JANUARY 4, 2013
Objectives Disease Description Evidence-Based Nutrition Recommendations Case Presentation NCP: Assessment, Diagnosis, Interventions, Monitoring and Evaluation Conclusion
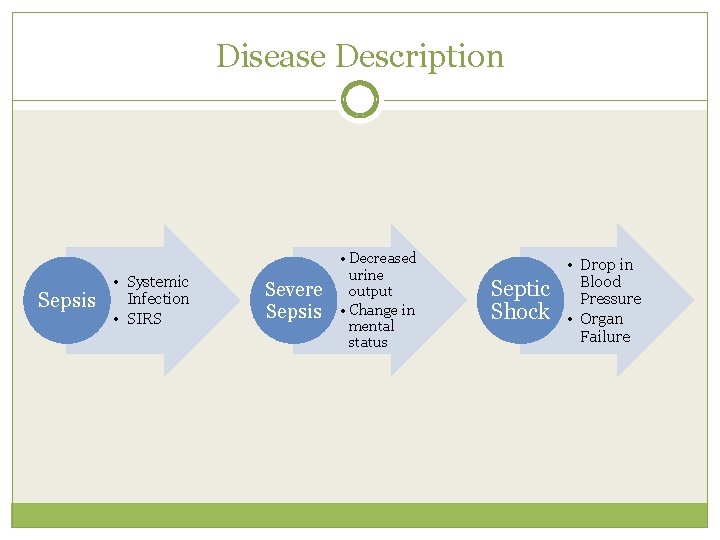
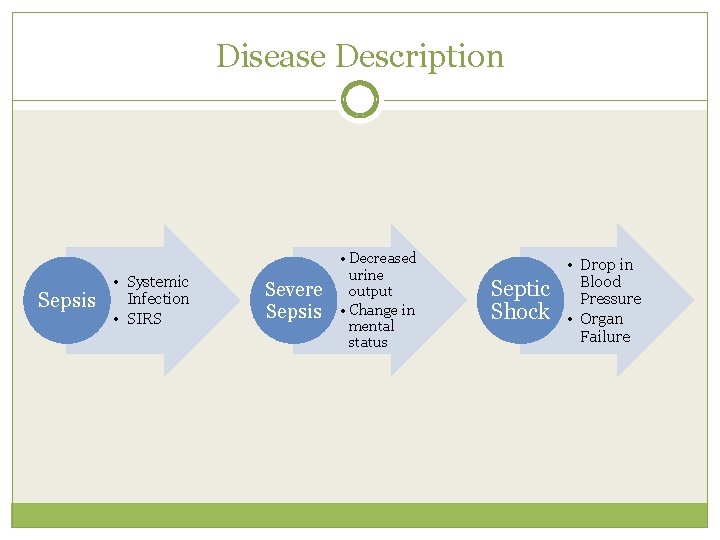
Disease Description Sepsis • Systemic Infection • SIRS Severe Sepsis • Decreased urine output • Change in mental status Septic Shock • Drop in Blood Pressure • Organ Failure
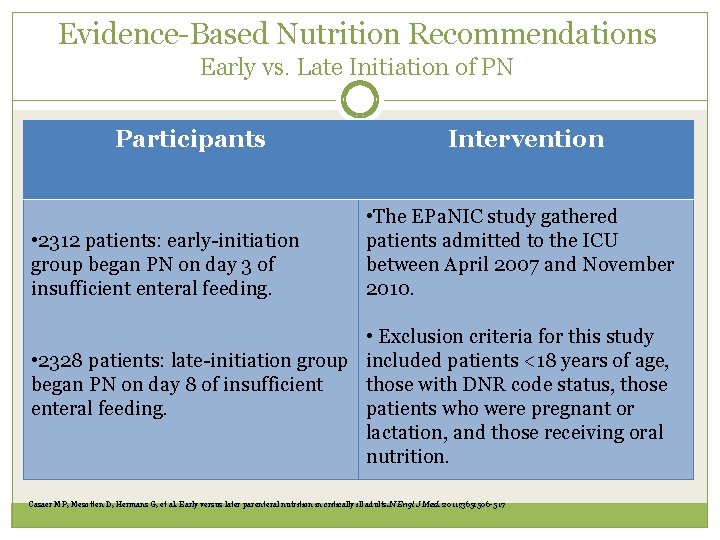
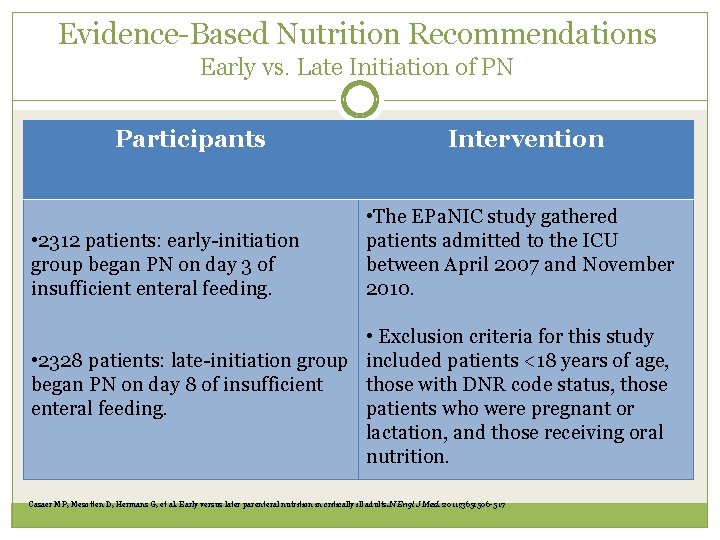
Evidence-Based Nutrition Recommendations Early vs. Late Initiation of PN Participants • 2312 patients: early-initiation group began PN on day 3 of insufficient enteral feeding. Intervention • The EPa. NIC study gathered patients admitted to the ICU between April 2007 and November 2010. • Exclusion criteria for this study • 2328 patients: late-initiation group included patients <18 years of age, began PN on day 8 of insufficient those with DNR code status, those enteral feeding. patients who were pregnant or lactation, and those receiving oral nutrition. Casaer MP, Mesotten D, Hermans G, et al. Early versus later parenteral nutrition in critically ill adults. N Engl J Med. 2011; 365: 506 -517
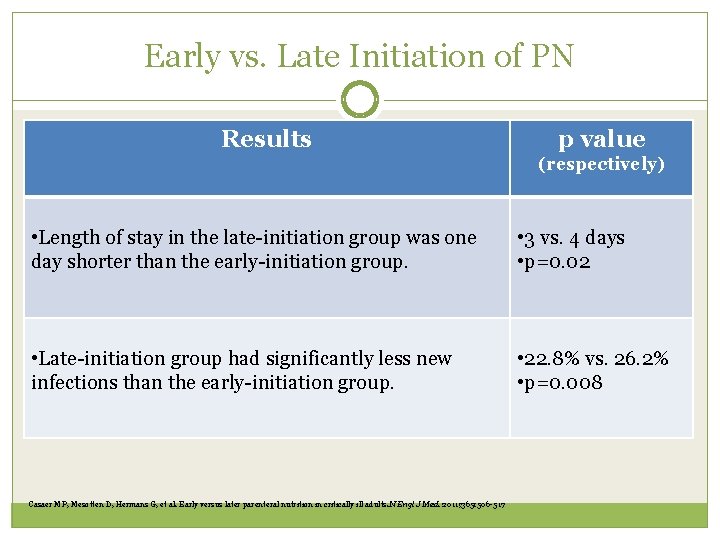
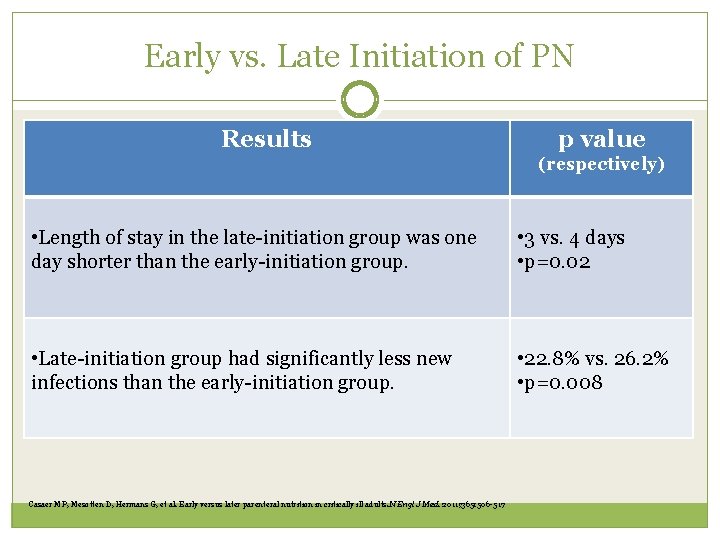
Early vs. Late Initiation of PN Results p value (respectively) • Length of stay in the late-initiation group was one day shorter than the early-initiation group. • 3 vs. 4 days • p=0. 02 • Late-initiation group had significantly less new infections than the early-initiation group. • 22. 8% vs. 26. 2% • p=0. 008 Casaer MP, Mesotten D, Hermans G, et al. Early versus later parenteral nutrition in critically ill adults. N Engl J Med. 2011; 365: 506 -517
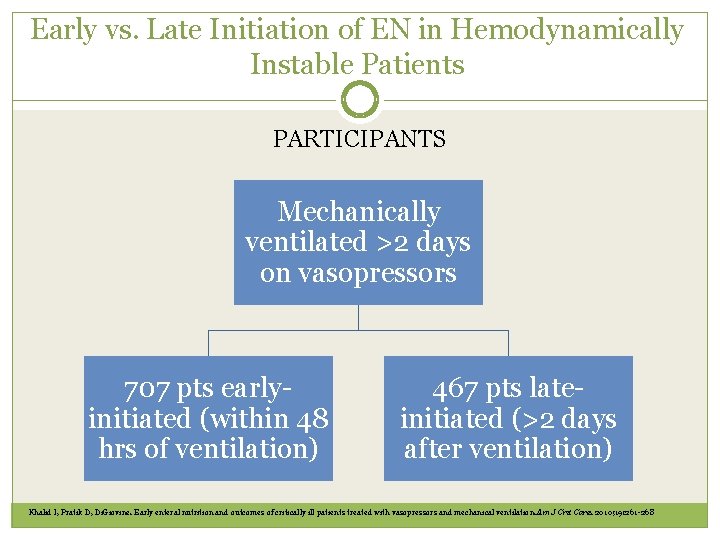
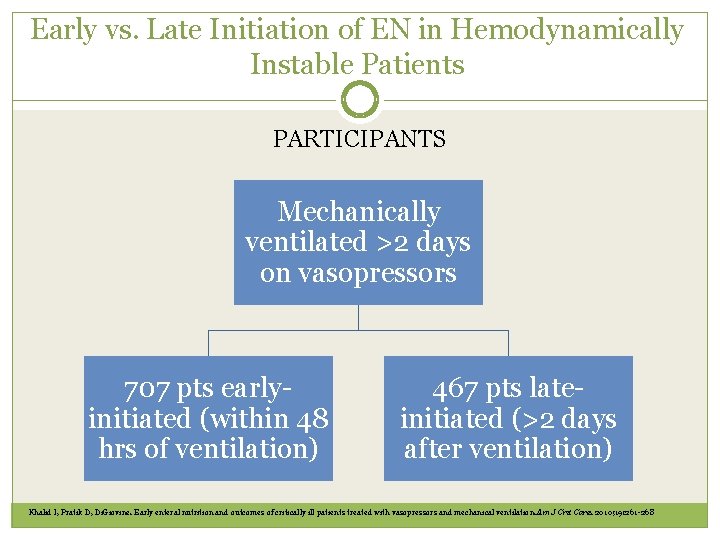
Early vs. Late Initiation of EN in Hemodynamically Instable Patients PARTICIPANTS Mechanically ventilated >2 days on vasopressors 707 pts earlyinitiated (within 48 hrs of ventilation) 467 pts lateinitiated (>2 days after ventilation) Khalid I, Pratik D, Di. Giovine. Early enteral nutrition and outcomes of critically ill patients treated with vasopressors and mechanical ventilation. Am J Crit Care. 2010; 19: 261 -268
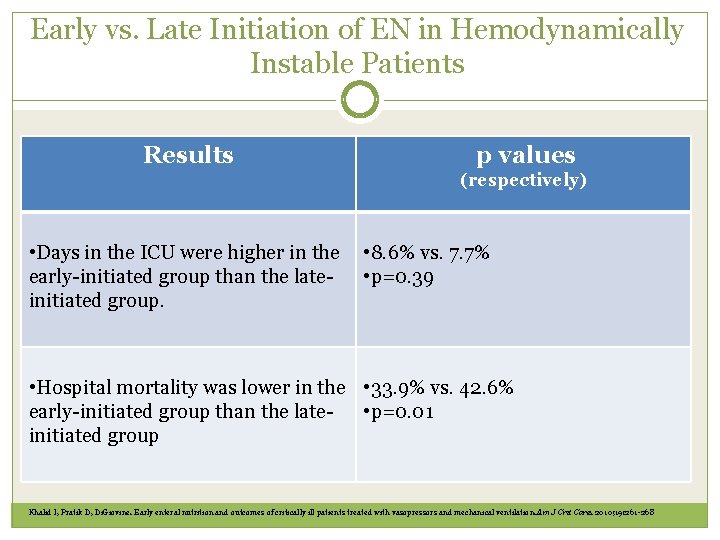
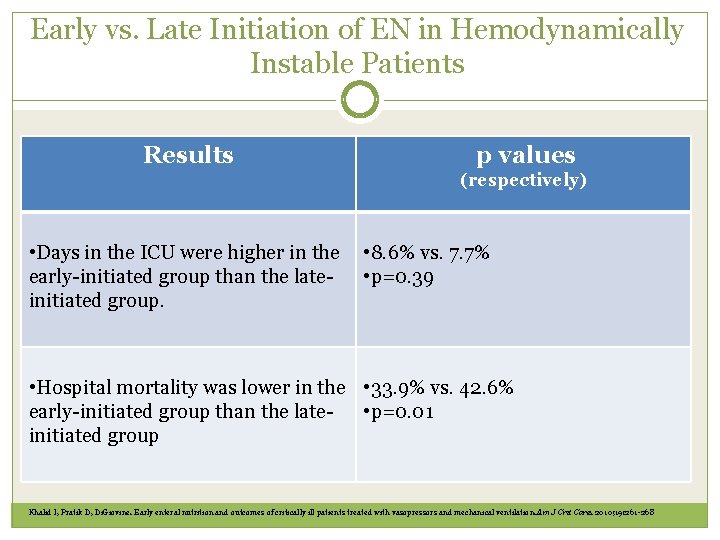
Early vs. Late Initiation of EN in Hemodynamically Instable Patients Results p values (respectively) • Days in the ICU were higher in the early-initiated group than the lateinitiated group. • 8. 6% vs. 7. 7% • p=0. 39 • Hospital mortality was lower in the • 33. 9% vs. 42. 6% early-initiated group than the late- • p=0. 01 initiated group Khalid I, Pratik D, Di. Giovine. Early enteral nutrition and outcomes of critically ill patients treated with vasopressors and mechanical ventilation. Am J Crit Care. 2010; 19: 261 -268
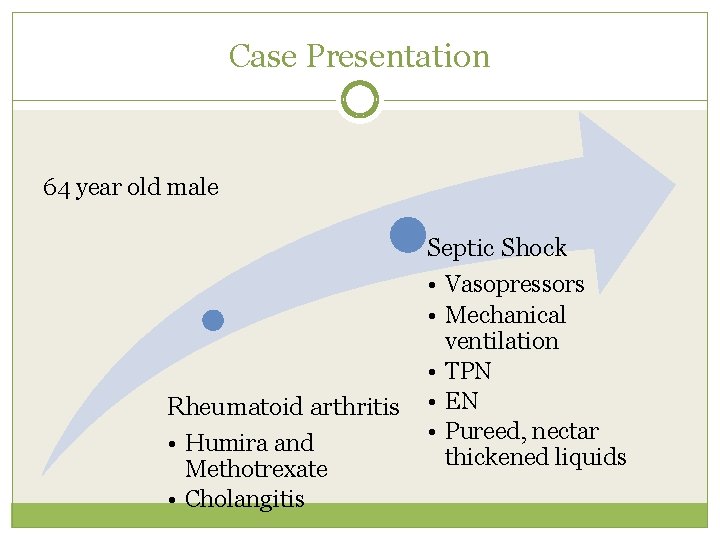
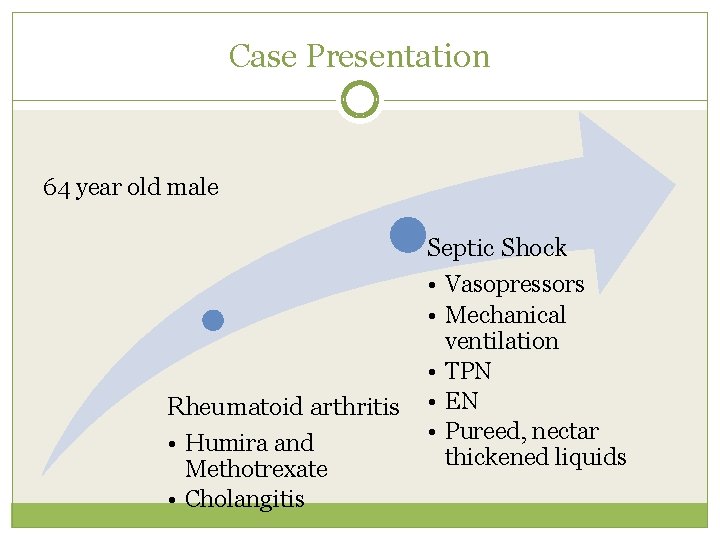
Case Presentation 64 year old male Rheumatoid arthritis • Humira and Methotrexate • Cholangitis Septic Shock • Vasopressors • Mechanical ventilation • TPN • EN • Pureed, nectar thickened liquids
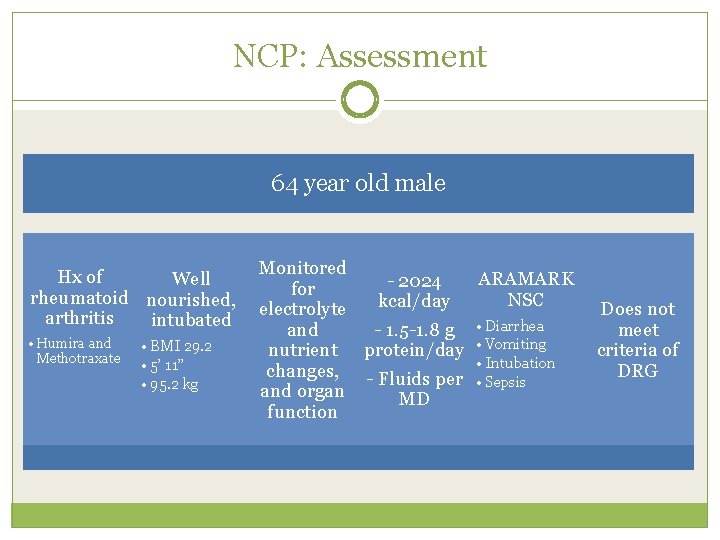
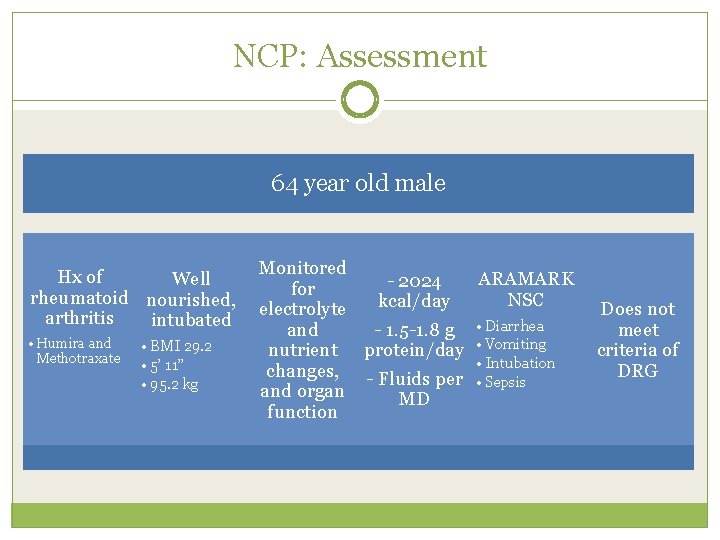
NCP: Assessment 64 year old male Hx of Well rheumatoid nourished, arthritis intubated • Humira and Methotraxate • BMI 29. 2 • 5’ 11” • 95. 2 kg Monitored ARAMARK - 2024 for NSC kcal/day electrolyte and - 1. 5 -1. 8 g • Diarrhea nutrient protein/day • Vomiting changes, - Fluids per • Intubation • Sepsis and organ MD function Does not meet criteria of DRG
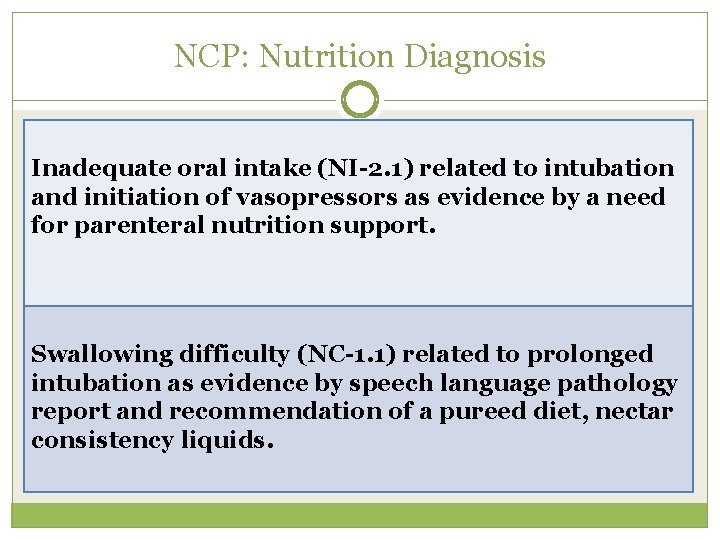
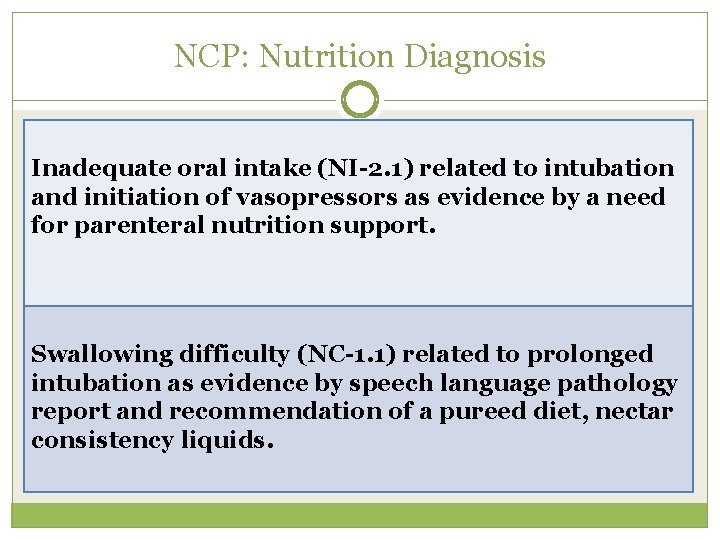
NCP: Nutrition Diagnosis Inadequate oral intake (NI-2. 1) related to intubation and initiation of vasopressors as evidence by a need for parenteral nutrition support. Swallowing difficulty (NC-1. 1) related to prolonged intubation as evidence by speech language pathology report and recommendation of a pureed diet, nectar consistency liquids.
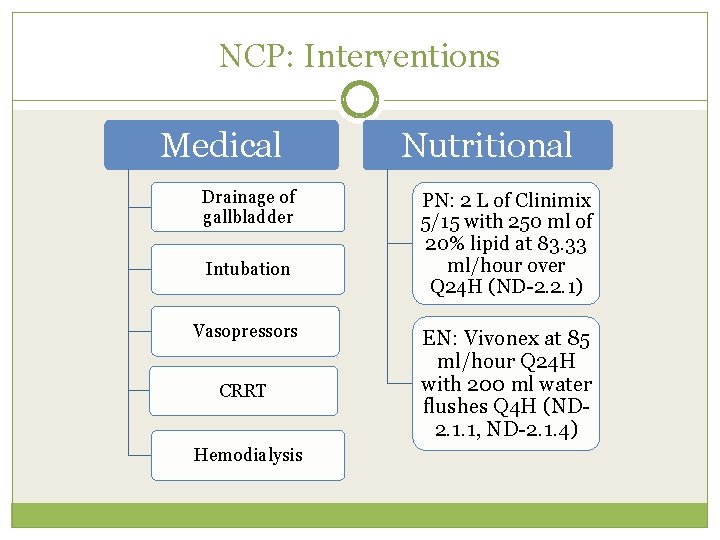
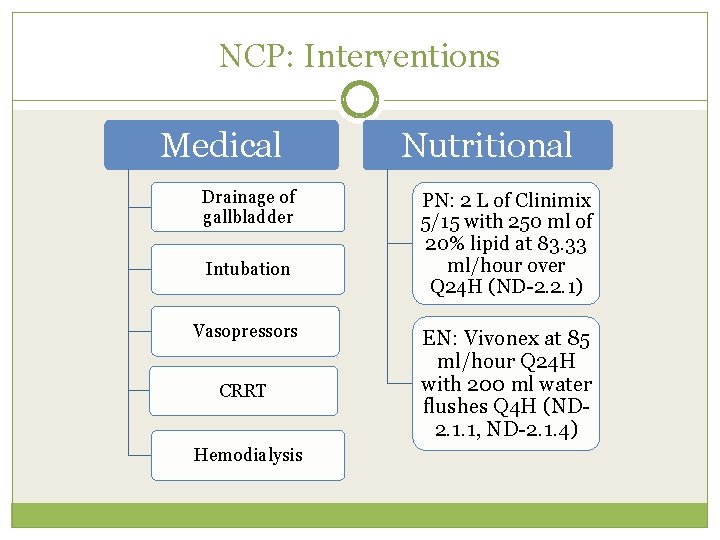
NCP: Interventions Medical Drainage of gallbladder Intubation Vasopressors CRRT Hemodialysis Nutritional PN: 2 L of Clinimix 5/15 with 250 ml of 20% lipid at 83. 33 ml/hour over Q 24 H (ND-2. 2. 1) EN: Vivonex at 85 ml/hour Q 24 H with 200 ml water flushes Q 4 H (ND 2. 1. 1, ND-2. 1. 4)
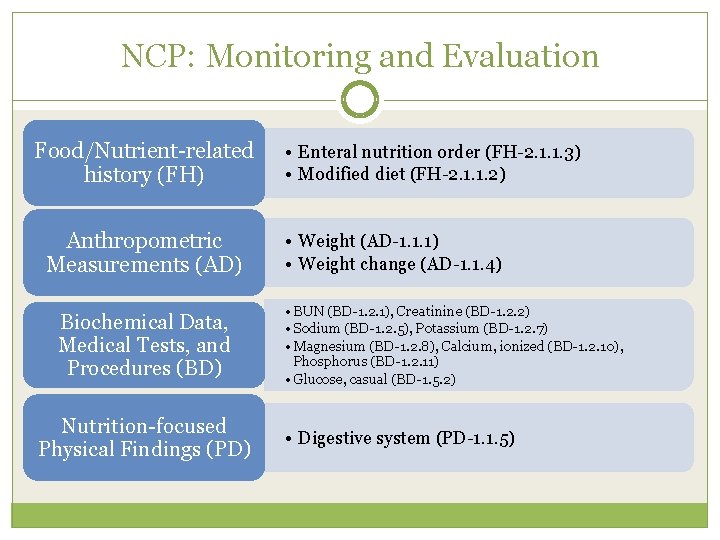
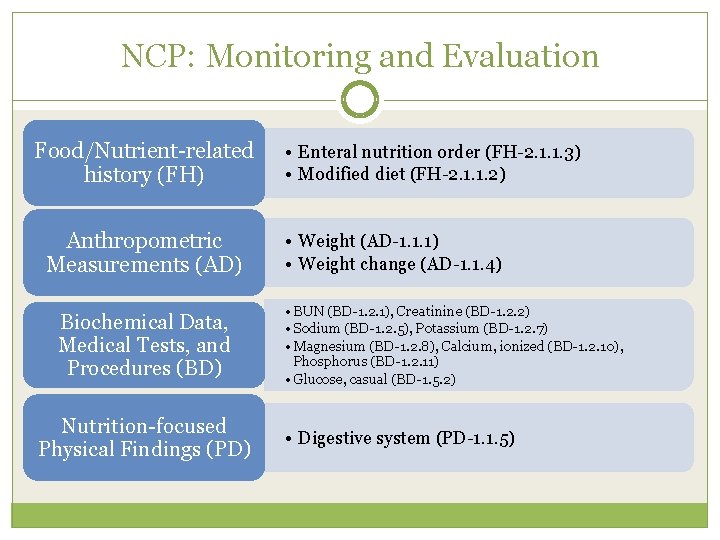
NCP: Monitoring and Evaluation Food/Nutrient-related history (FH) Anthropometric Measurements (AD) Biochemical Data, Medical Tests, and Procedures (BD) Nutrition-focused Physical Findings (PD) • Enteral nutrition order (FH-2. 1. 1. 3) • Modified diet (FH-2. 1. 1. 2) • Weight (AD-1. 1. 1) • Weight change (AD-1. 1. 4) • BUN (BD-1. 2. 1), Creatinine (BD-1. 2. 2) • Sodium (BD-1. 2. 5), Potassium (BD-1. 2. 7) • Magnesium (BD-1. 2. 8), Calcium, ionized (BD-1. 2. 10), Phosphorus (BD-1. 2. 11) • Glucose, casual (BD-1. 5. 2) • Digestive system (PD-1. 1. 5)
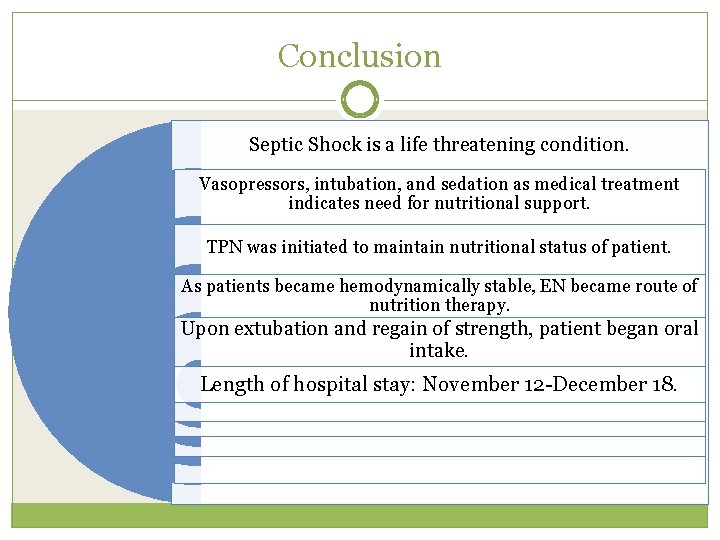
Conclusion Septic Shock is a life threatening condition. Vasopressors, intubation, and sedation as medical treatment indicates need for nutritional support. TPN was initiated to maintain nutritional status of patient. As patients became hemodynamically stable, EN became route of nutrition therapy. Upon extubation and regain of strength, patient began oral intake. Length of hospital stay: November 12 -December 18.
References Sepsis. A. D. A. M Medical Encyclopedia. Pub. Med Health. http: //www. ncbi. nlm. nih. gov/pubmedhealth/PMH 0001687/. Updated August 23, 2012. Accessed December 28, 2012. Siner, JM. Sepsis: Definitions, Etiology, Epidemiology, and Pathogensis. Chest. 2009; 4. http: //www. chestnet. org/accp/pccsu/sepsis-definitionsepidemiology-etiology-and-pathogenesis? page=0, 3. Accessed December 23, 2012. Septic Shock. Medline Plus. http: //www. nlm. nih. gov/medlineplus/ency/article/000668. htm. Updated January 14, 2010. Accessed December 28, 2012. Pinsky MR, Mink S, Sharma S, et al. Septic Shock: Epidemiology. Medscape Reference. http: //emedicine. medscape. com/article/168402 -overview#a 0156. Updated August 13, 2012. Accessed December 28, 2012. Shock. A. D. A. M Medical Encyclopedia. Pubmed Health. http: //www. ncbi. nlm. nih. gov/pubmedhealth/PMH 0001106/. Updated January 10, 2012. Accessed December 23, 2012. Casaer MP, Mesotten D, Hermans G, et al. Early versus later parenteral nutrition in critically ill adults. N Engl J Med. 2011; 365: 506 -517. Khalid I, Pratik D, Di. Giovine. Early enteral nutrition and outcomes of critically ill patients treated with vasopressors and mechanical ventilation. Am J Crit Care. 2010; 19: 261 -268. Mc. Clave SA, Martindale RG, Vanek VW, et al. Guidelines for the provision and assessment of nutrition support therapy in the adult critically ill patients. J Parenter Enteral Nutr. 2009; 33: 279 -285. American Dietetic Association. International Dietetics and Nutrition. Terminology (IDNT) Reference Manual. 3 rd ed. Chicago, Il: American Dietetic Association; 2011. Academy of Nutrition and Dietetics: Evidence Analysis Library. Critical Illness Nutrition Practice Guidelines. A. N. D. Evidence Analysis Library website. http: //andevidencelibrary. com/template. cfm? key=1309. Accessed 2 Jan 2013. Pronsky ZM. Food-Medication Interactions, 16 th ed. Birchrunville, PA: Food-Medication Interactions; 2010. ARAMARK Healthcare. Assessment and education policy #2: Nutrition status classification worksheet. Patient Food Services: Policies and Procedures, Volume IV; 2010.
QUESTIONS?
 Medical nutrition therapy for stroke
Medical nutrition therapy for stroke Medical nutrition therapy for hypertension
Medical nutrition therapy for hypertension Related image
Related image Spinal shock vs neurogenic shock
Spinal shock vs neurogenic shock Normovolemico
Normovolemico Spinal shock vs neurogenic shock
Spinal shock vs neurogenic shock Spinal shock symptoms
Spinal shock symptoms Subacute combined degeneration
Subacute combined degeneration Shock therapy economics
Shock therapy economics Shock therapy vs gradualism
Shock therapy vs gradualism Hepburn osteometric board
Hepburn osteometric board Best worst and average case
Best worst and average case Insulin shock medical definition
Insulin shock medical definition Nutrition and diet therapy nursing
Nutrition and diet therapy nursing Psychodynamic and humanistic therapies have in common
Psychodynamic and humanistic therapies have in common Bioness bits cost
Bioness bits cost