Cardiovascular system L 1 Faisal I Mohammed MD




- Slides: 24
Cardiovascular system L 1 Faisal I. Mohammed, MD, Ph. D Yanal A. Shafagoj, MD, Ph. D University of Jordan 1
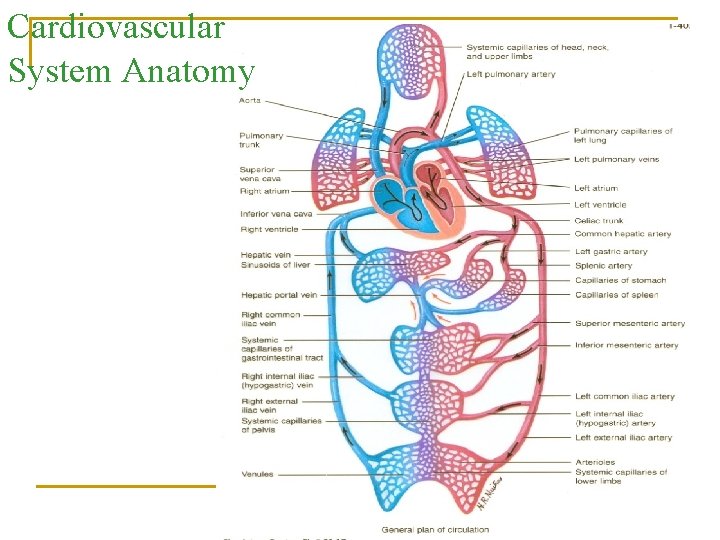
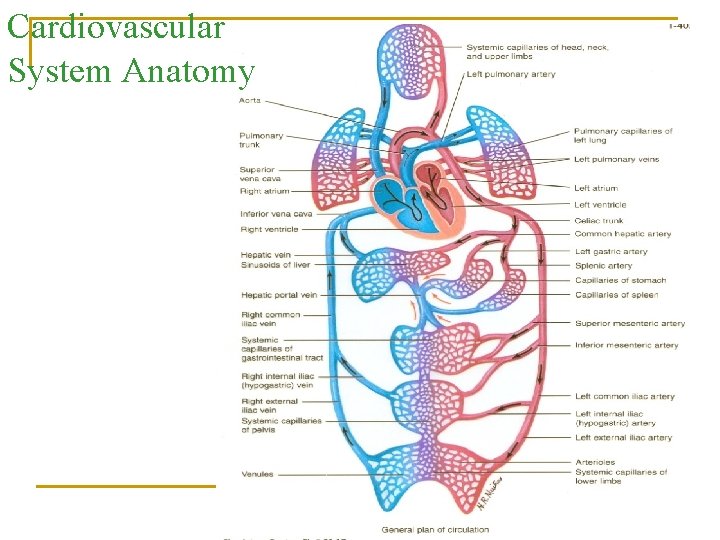
Cardiovascular System Anatomy
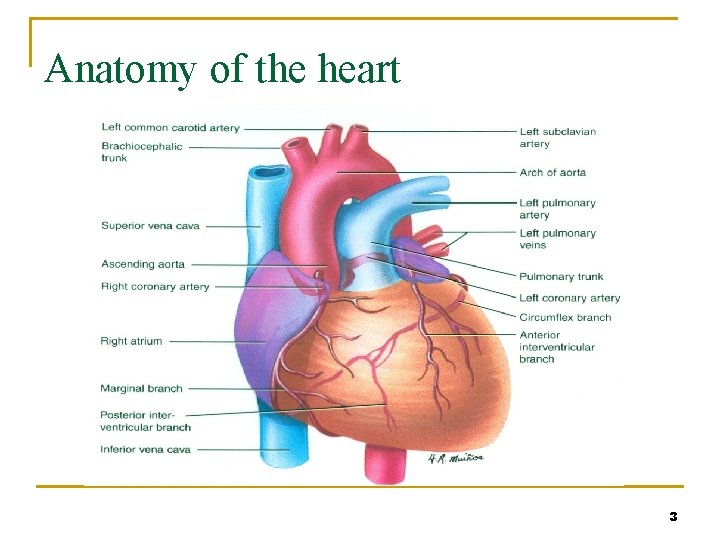
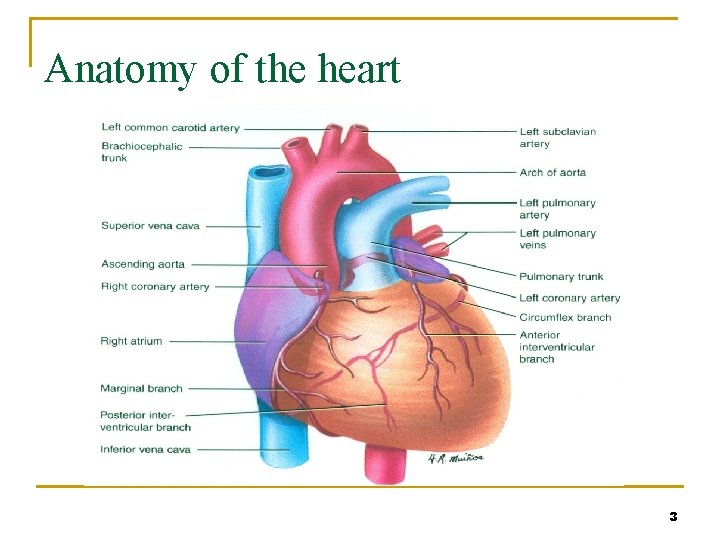
Anatomy of the heart 3
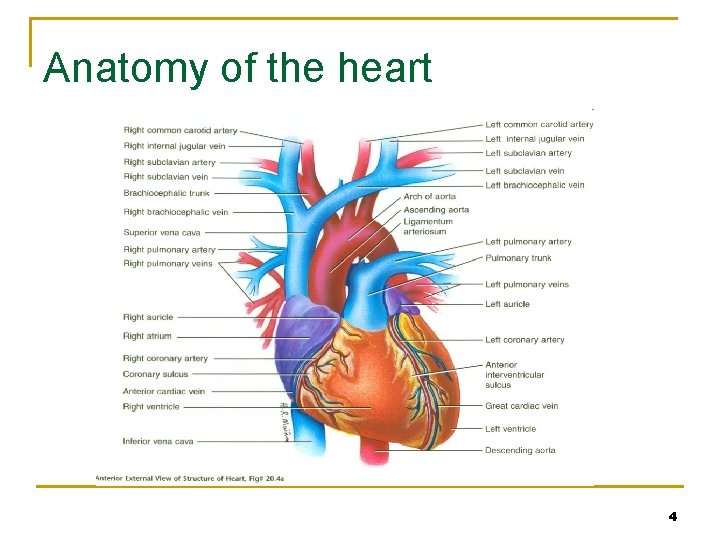
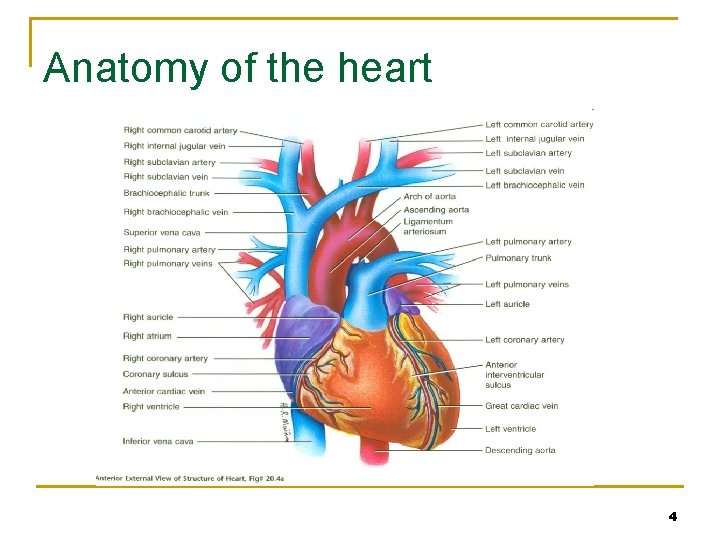
Anatomy of the heart 4

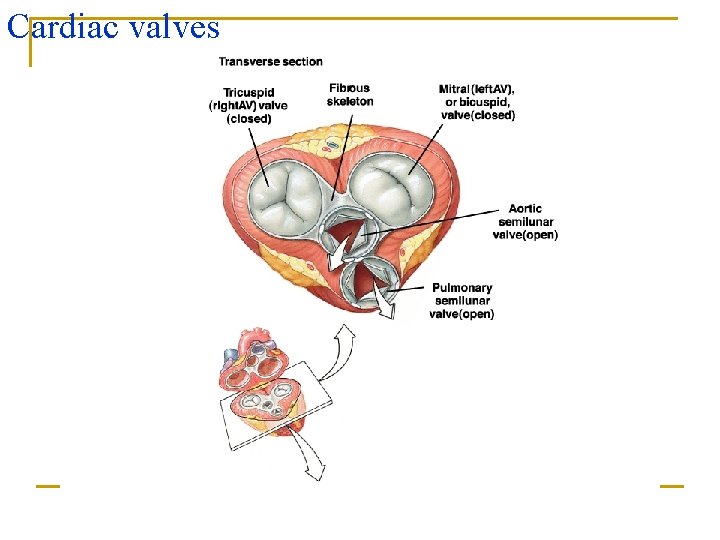
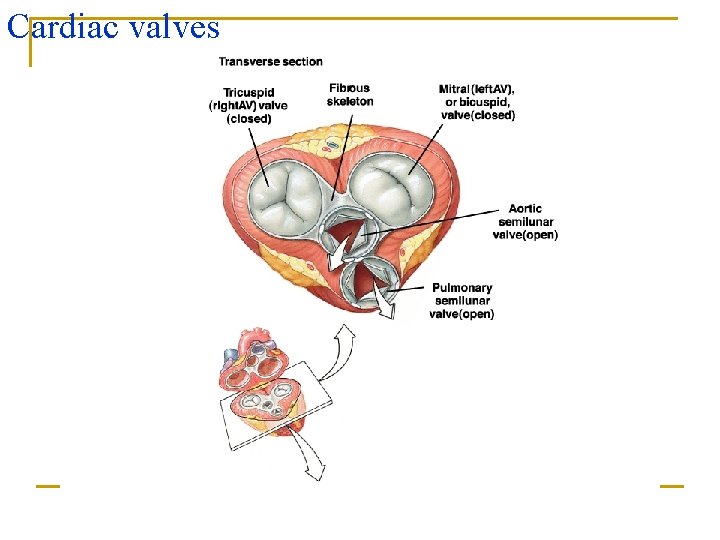
Cardiac valves
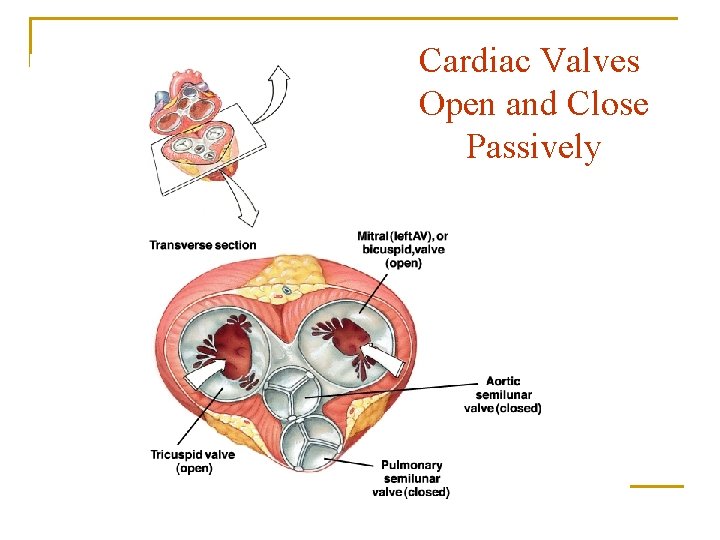
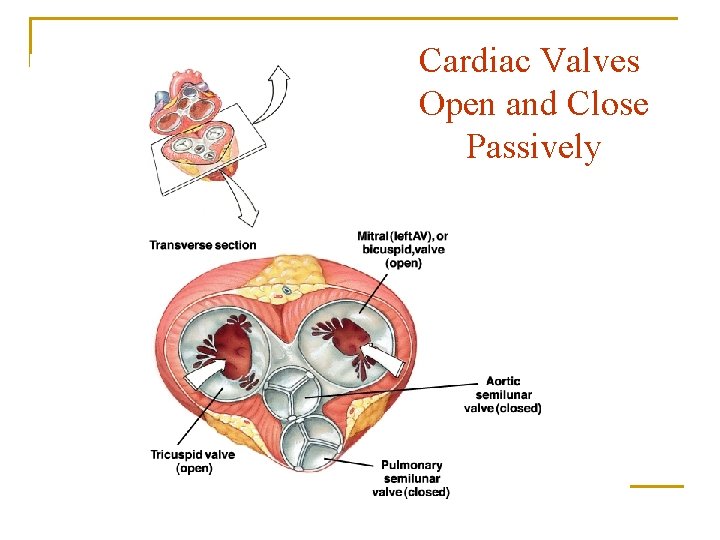
Cardiac Valves Open and Close Passively
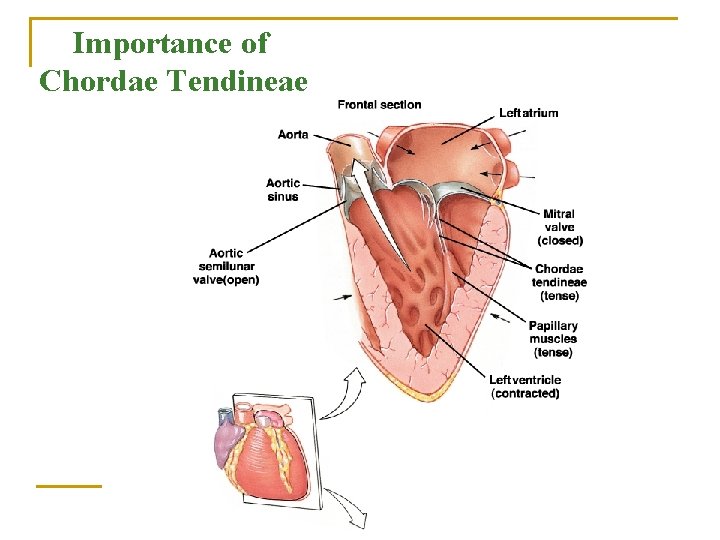
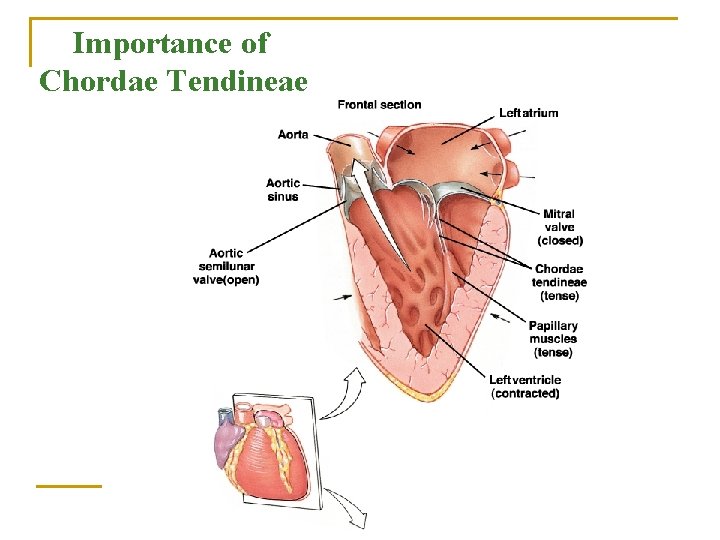
Importance of Chordae Tendineae
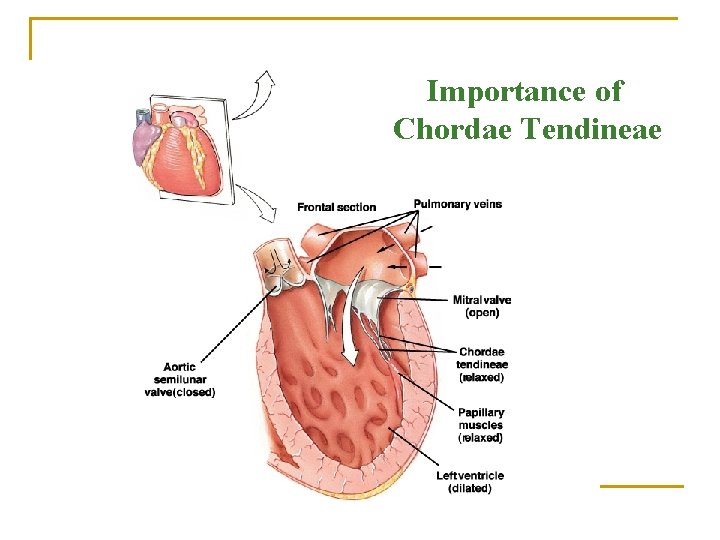
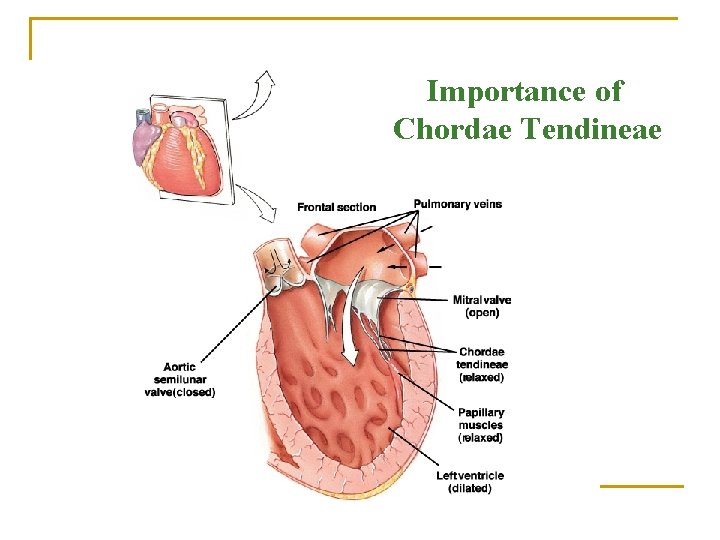
Importance of Chordae Tendineae
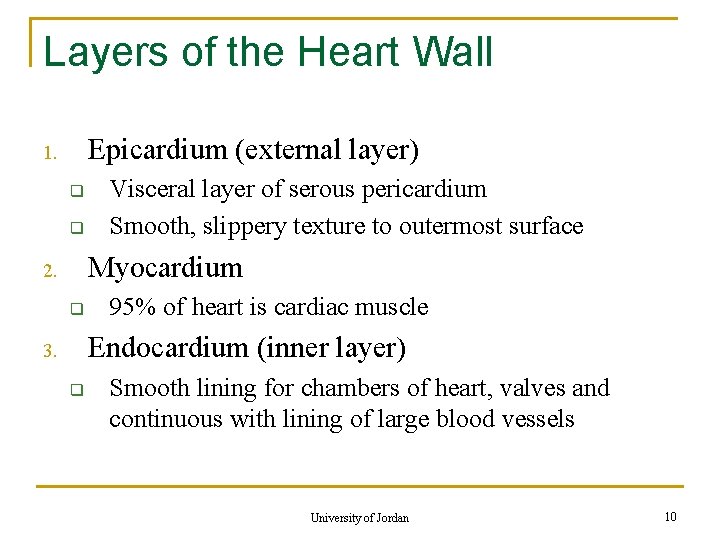
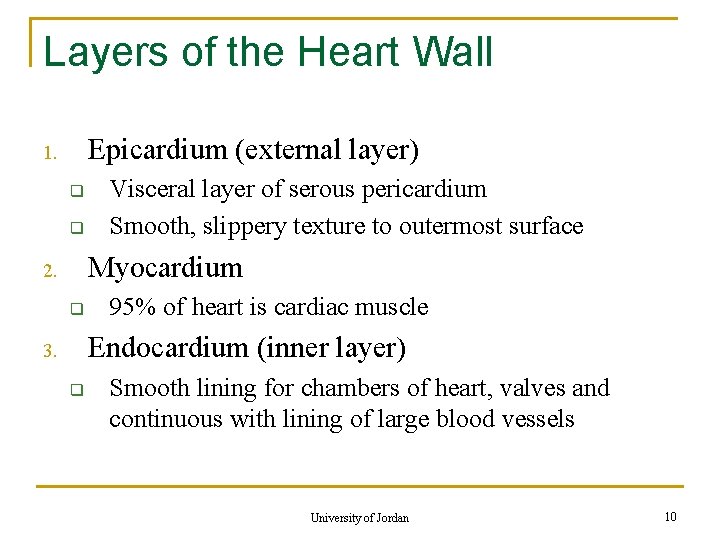
Layers of the Heart Wall Epicardium (external layer) 1. q q Visceral layer of serous pericardium Smooth, slippery texture to outermost surface Myocardium 2. q 95% of heart is cardiac muscle Endocardium (inner layer) 3. q Smooth lining for chambers of heart, valves and continuous with lining of large blood vessels University of Jordan 10

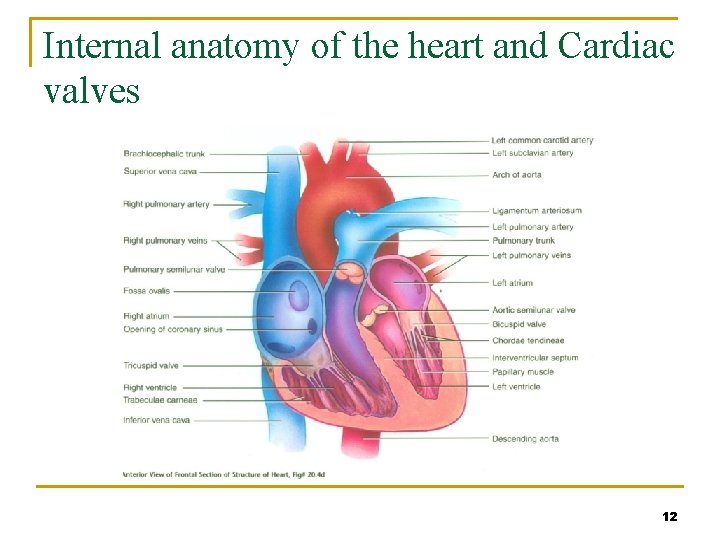
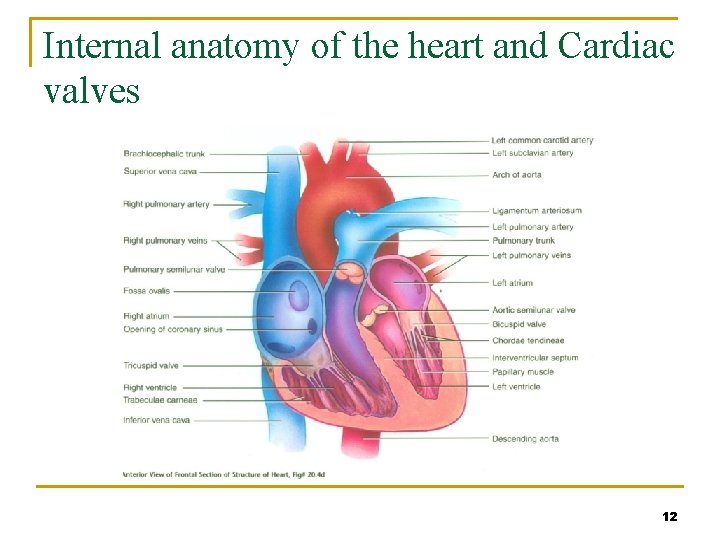
Internal anatomy of the heart and Cardiac valves 12
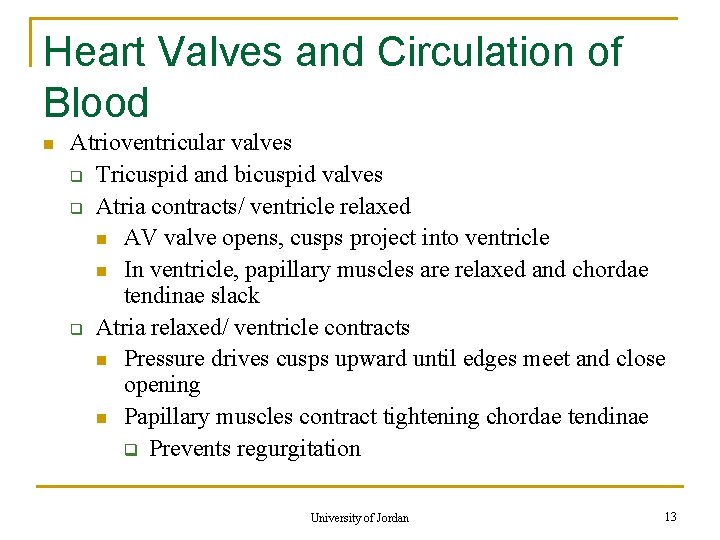
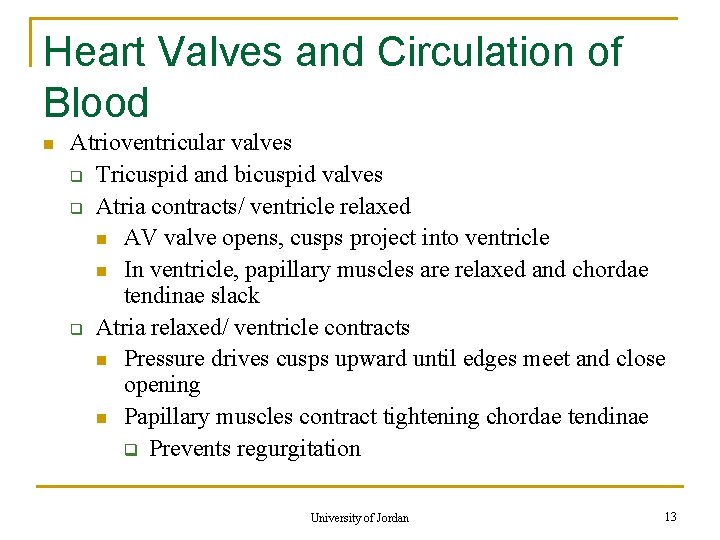
Heart Valves and Circulation of Blood n Atrioventricular valves q Tricuspid and bicuspid valves q Atria contracts/ ventricle relaxed n AV valve opens, cusps project into ventricle n In ventricle, papillary muscles are relaxed and chordae tendinae slack q Atria relaxed/ ventricle contracts n Pressure drives cusps upward until edges meet and close opening n Papillary muscles contract tightening chordae tendinae q Prevents regurgitation University of Jordan 13
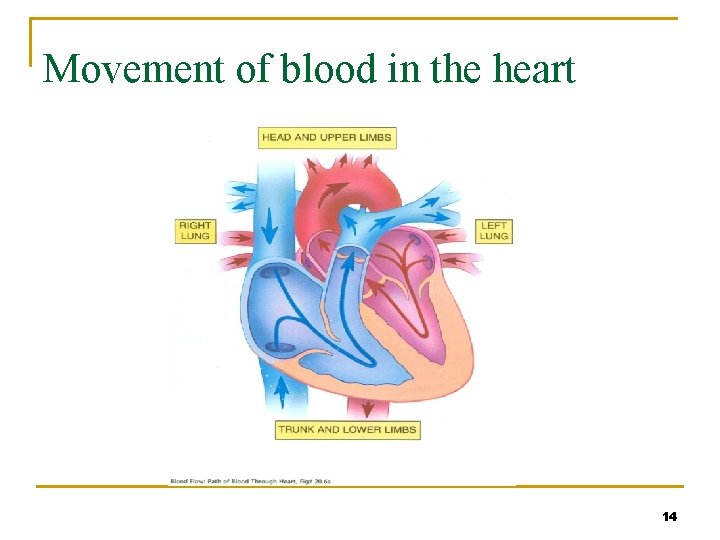
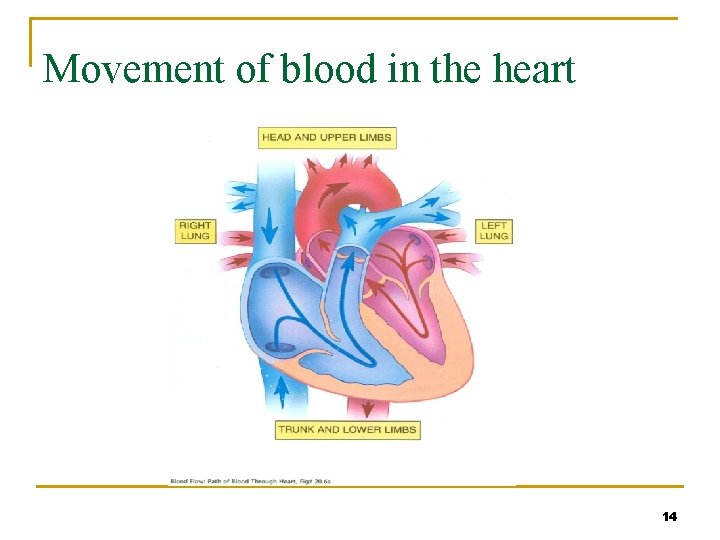
Movement of blood in the heart 14
Systemic and pulmonary circulation - 2 circuits in series q Systemic circuit n n n q Left side of heart Receives blood from lungs Ejects blood into aorta Systemic arteries, arterioles Gas and nutrient exchange in systemic capillaries Systemic venules and veins lead back to right atrium Pulmonary circuit n n n Right side of heart Receives blood from systemic circulation Ejects blood into pulmonary trunk then pulmonary arteries Gas exchange in pulmonary capillaries Pulmonary veins takes blood to left atrium University of Jordan 15
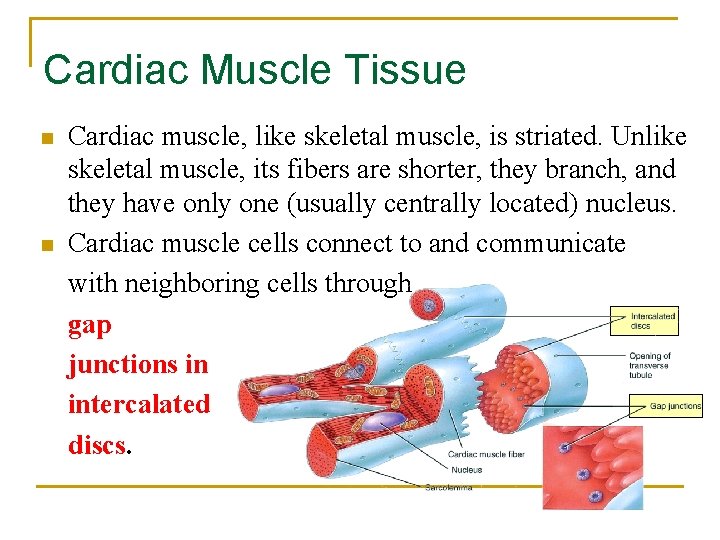
Cardiac Muscle Tissue and the Cardiac Conduction System n Histology q q q q Shorter and less circular than skeletal muscle fibers Branching gives “stair-step” appearance Usually one centrally located nucleus Ends of fibers connected by intercalated discs Discs contain desmosomes (hold fibers together) and gap junctions (allow action potential conduction from one fiber to the next) Mitochondria are larger and more numerous than skeletal muscle Same arrangement of actin and myosin University of Jordan 16

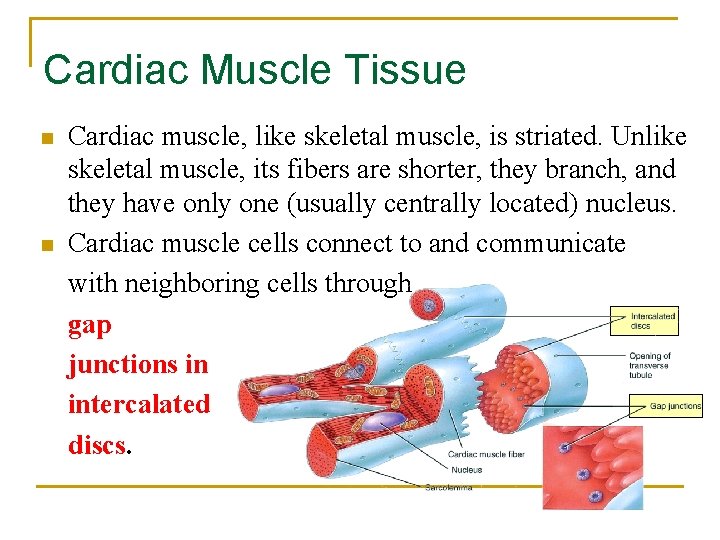
Cardiac Muscle Tissue n n Cardiac muscle, like skeletal muscle, is striated. Unlike skeletal muscle, its fibers are shorter, they branch, and they have only one (usually centrally located) nucleus. Cardiac muscle cells connect to and communicate with neighboring cells through gap junctions in intercalated discs.
Action Potentials and Contraction q 1. 2. 3. Action potential initiated by SA node spreads out to excite “working” fibers called contractile fibers Depolarization Plateau Repolarization University of Jordan 19
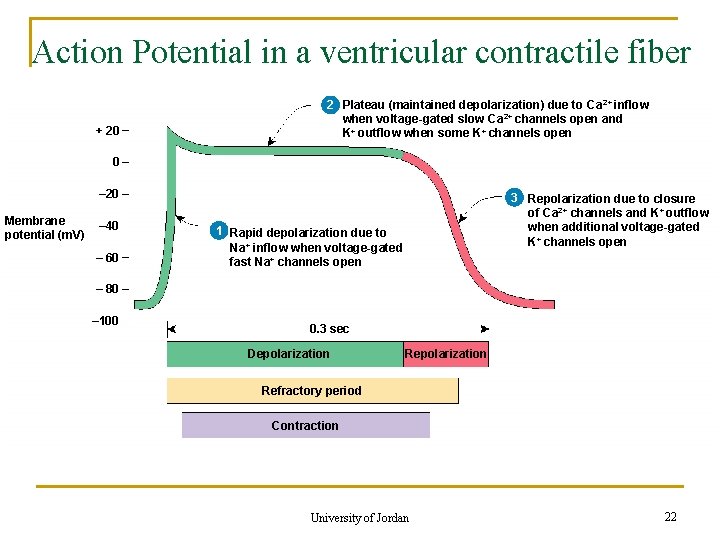
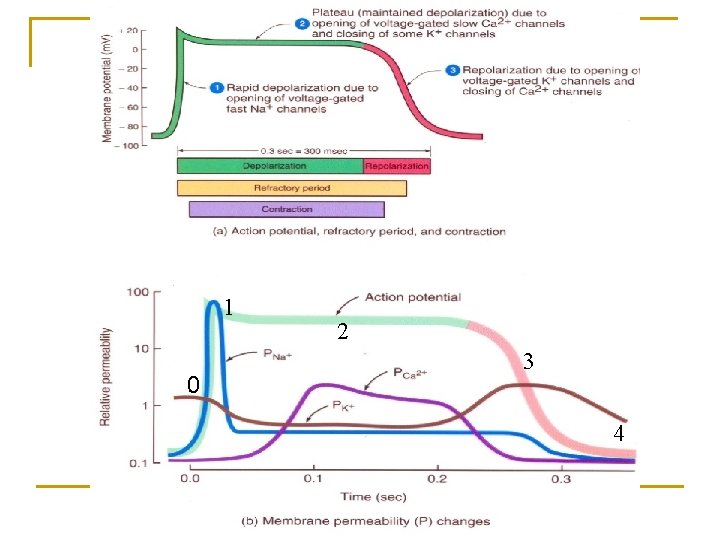
Action Potentials and Contraction 1. 2. Depolarization – contractile fibers have stable resting membrane potential n Voltage-gated fast Na+ channels open – Na+ flows in n Then deactivate and Na+ inflow decreases Plateau – period of maintained depolarization n Due in part to opening of voltage-gated slow Ca 2+ channels – Ca 2+ moves from interstitial fluid into cytosol n Ultimately triggers contraction n Depolarization sustained due to voltage-gated K+ channels balancing Ca 2+ inflow with K+ outflow University of Jordan 20
Action Potentials and Contraction Repolarization – recovery of resting membrane potential q Resembles that in other excitable cells q Additional voltage-gated K+ channels open q Outflow K+ of restores negative resting membrane potential q Calcium channels closing Refractory period – time interval during which second contraction cannot be triggered q Lasts longer than contraction itself q Tetanus (maintained contraction) cannot occur q Blood flow would cease 3. q University of Jordan 21
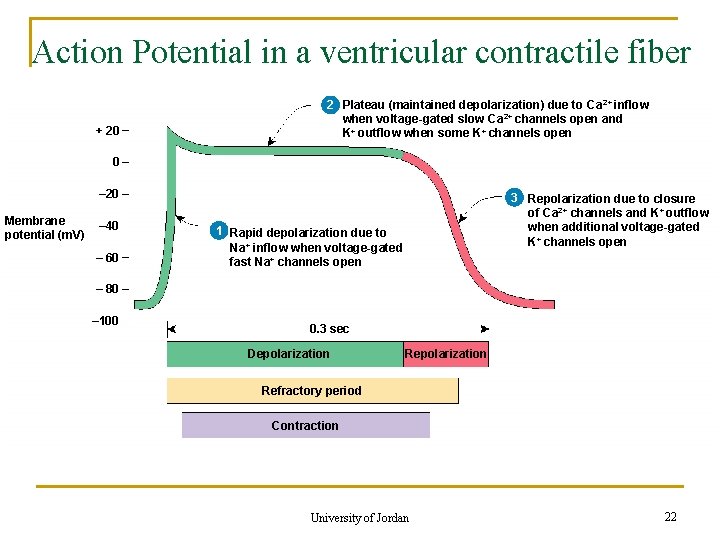
Action Potential in a ventricular contractile fiber + 20 2+ 22 Plateau (maintained depolarization) due to Ca inflow 2+ when voltage-gated slow Ca channels open and K+ outflow when some K + channels open 0 – 20 Membrane potential (m. V) – 40 – 60 33 Repolarization due to closure of Ca 2+ channels and K+ outflow when additional voltage-gated K+ channels open 11 Rapid depolarization due to Na+ inflow when voltage-gated fast Na+ channels open – 80 – 100 0. 3 sec Depolarization Refractory period Contraction University of Jordan 22
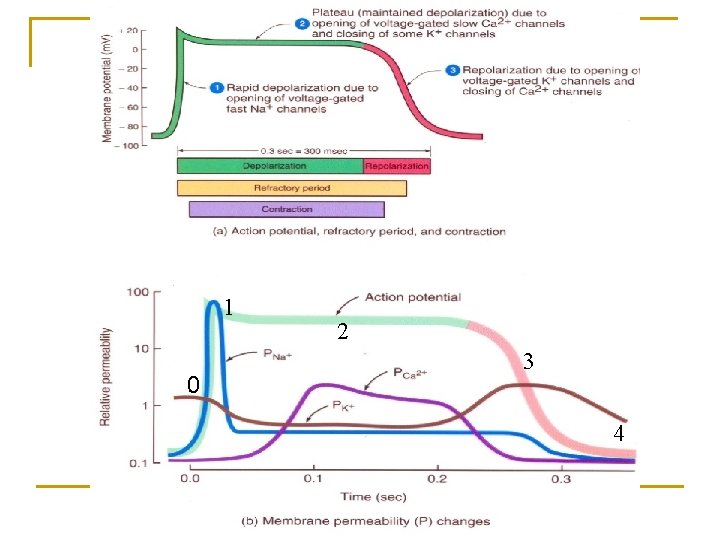
1 0 2 3 4

University of Jordan 24