Cardiopulmonary Resuscitation Shamiel Salie Paediatric Intensive Care Unit


- Slides: 28
Cardiopulmonary Resuscitation Shamiel Salie Paediatric Intensive Care Unit Red Cross Children’s Hospital, University of Cape Town

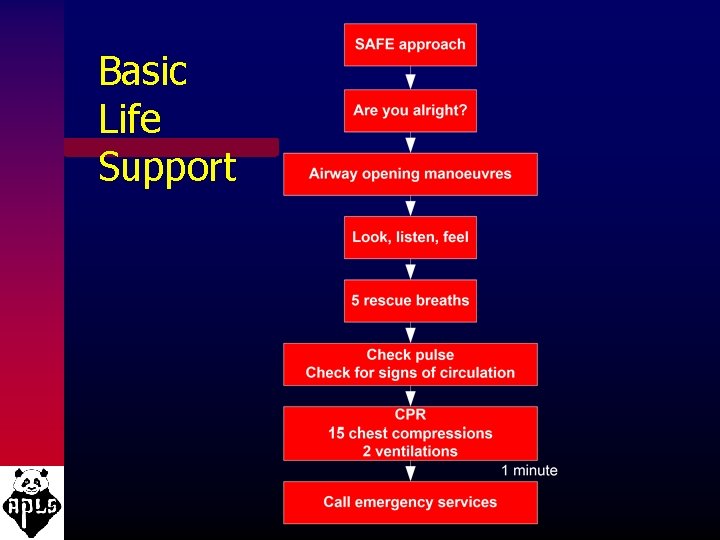
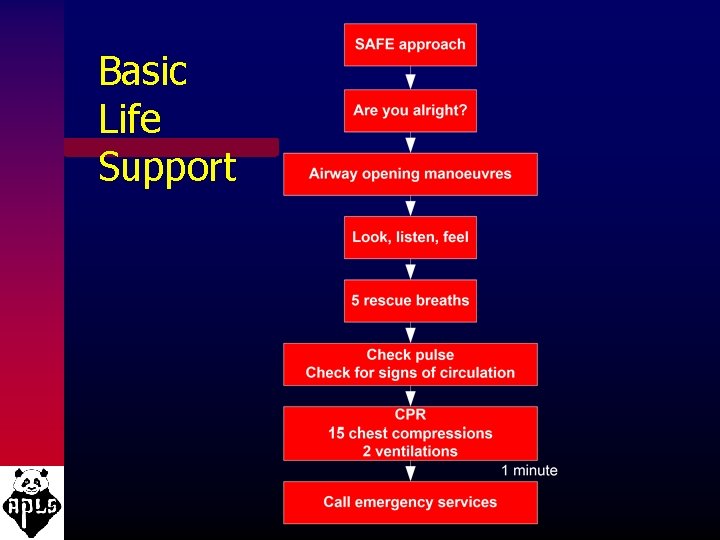
Basic Life Support
Age Definitions: • Newborn • Infant - under 1 year • Child - from 1 year to puberty
2005 BLS Changes: • Lay rescuers should start compressions for an unresponsive child who is not breathing/moving • Universal compression-ventilation ratio of 30: 2 for the lone rescuer of infants, children and adults • Increased evidence on the importance of uninterrupted chest compressions
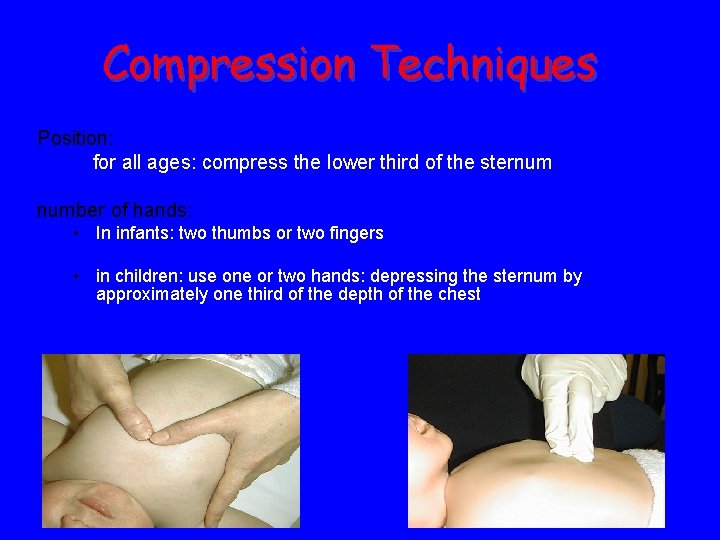
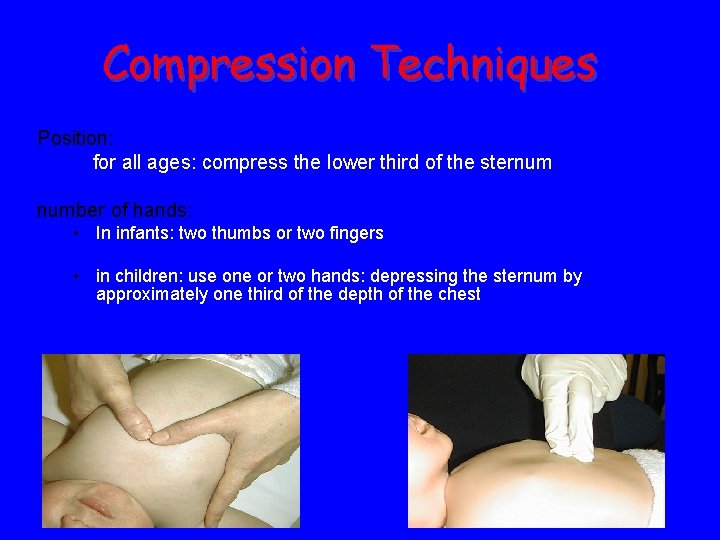
Compression Techniques Position: for all ages: compress the lower third of the sternum number of hands: • In infants: two thumbs or two fingers • in children: use one or two hands: depressing the sternum by approximately one third of the depth of the chest
Chest Compressions • Push hard • Push Fast • Complete chest recoil • Minimize interruptions
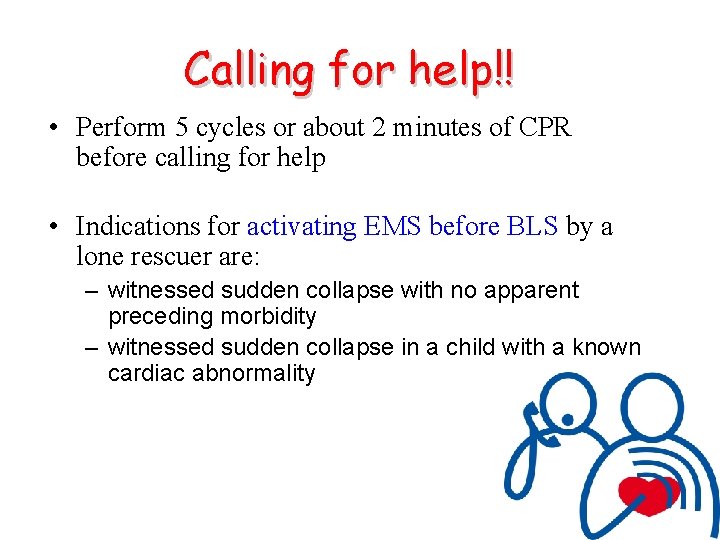
Calling for help!! • Perform 5 cycles or about 2 minutes of CPR before calling for help • Indications for activating EMS before BLS by a lone rescuer are: – witnessed sudden collapse with no apparent preceding morbidity – witnessed sudden collapse in a child with a known cardiac abnormality
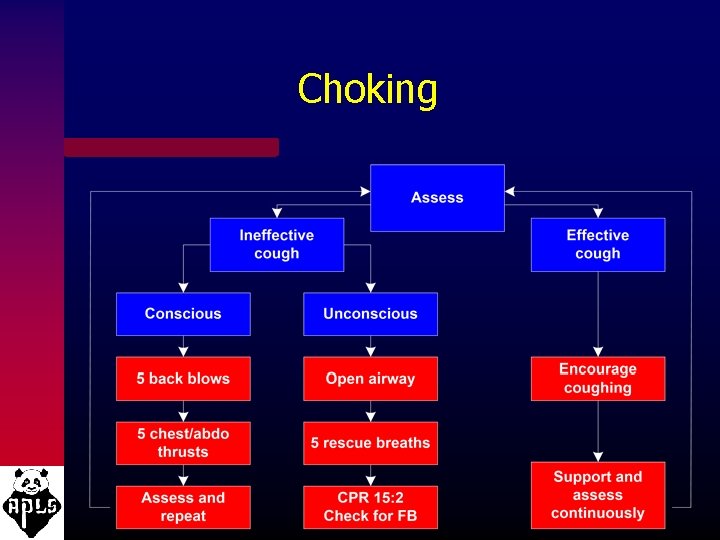
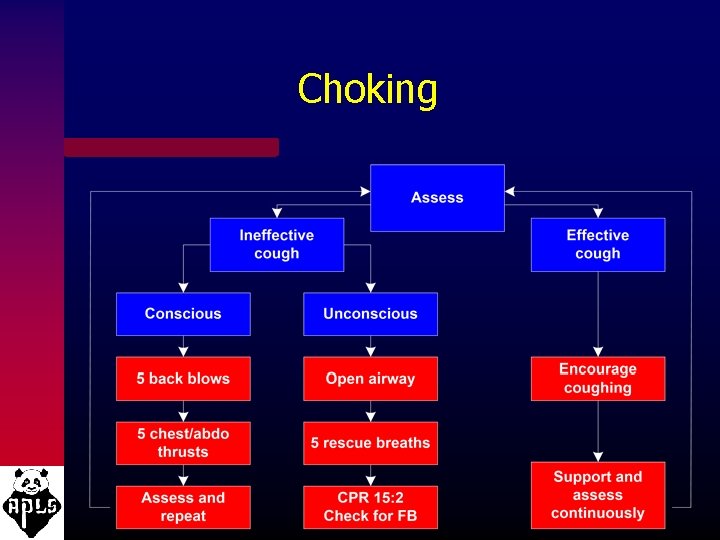
Choking
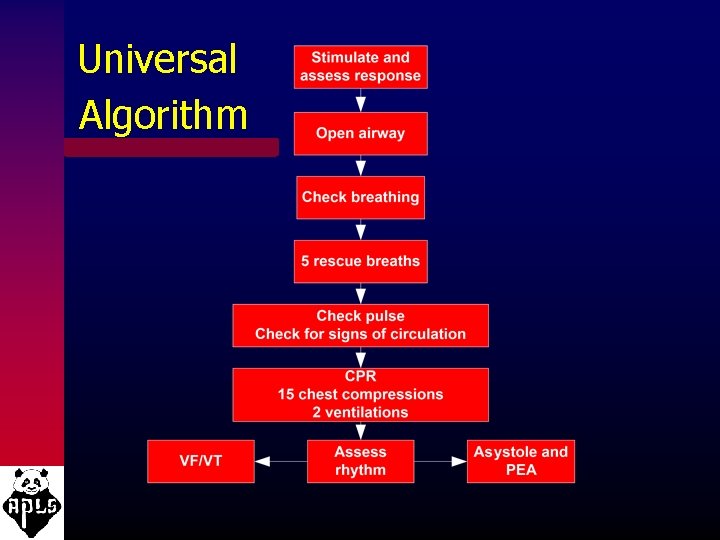
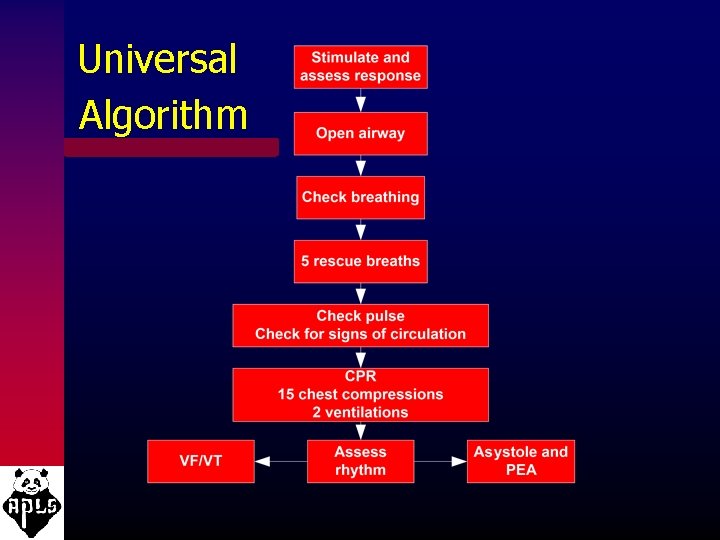
Universal Algorithm
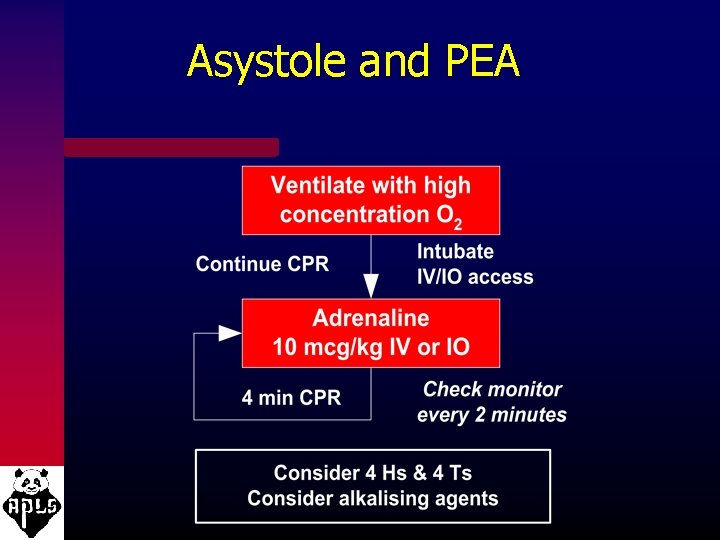
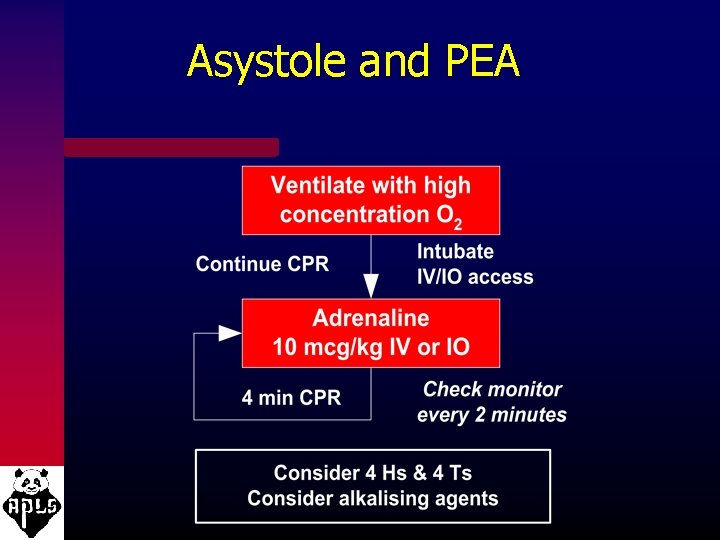
Asystole and PEA
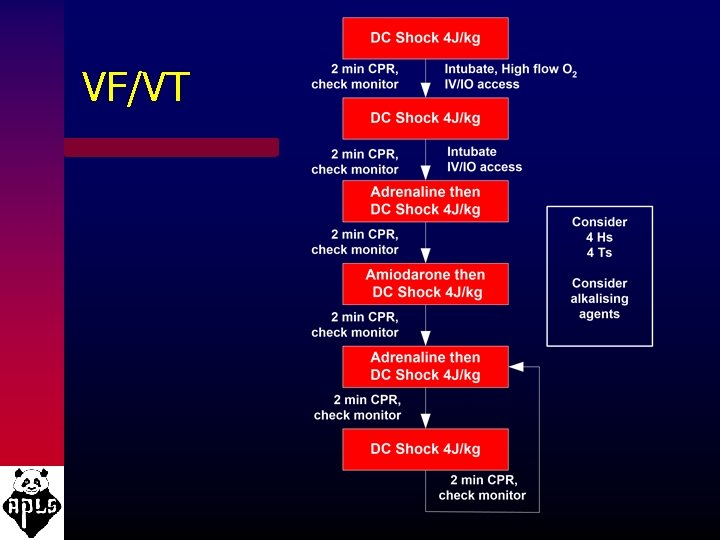
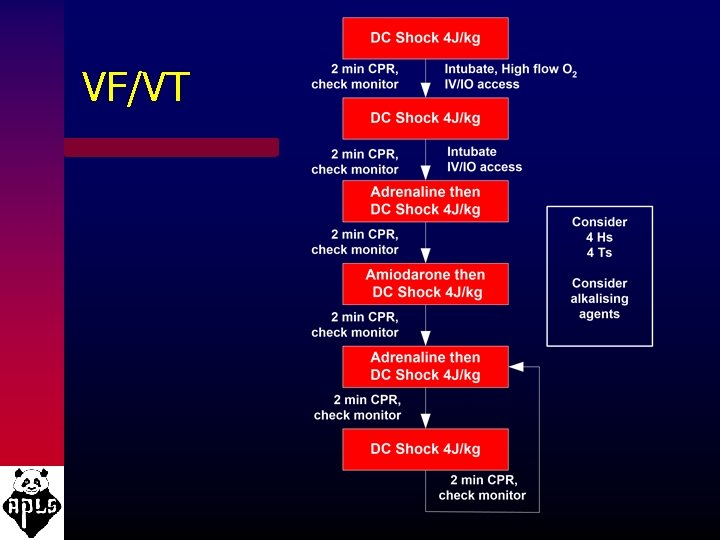
VF/VT
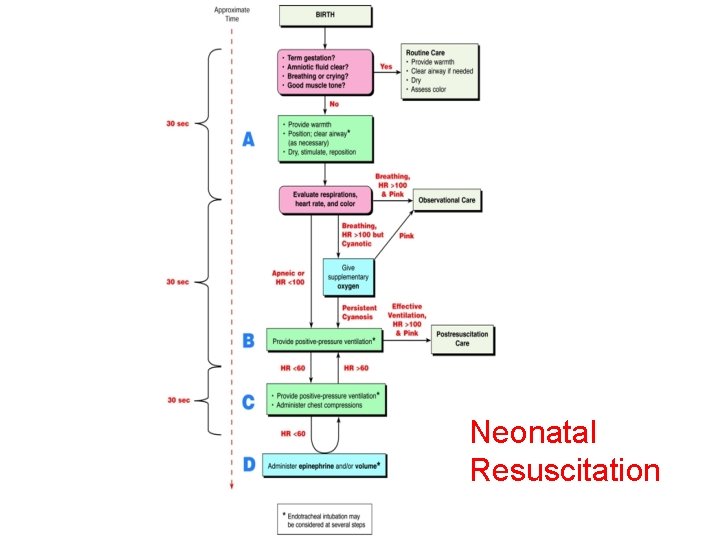
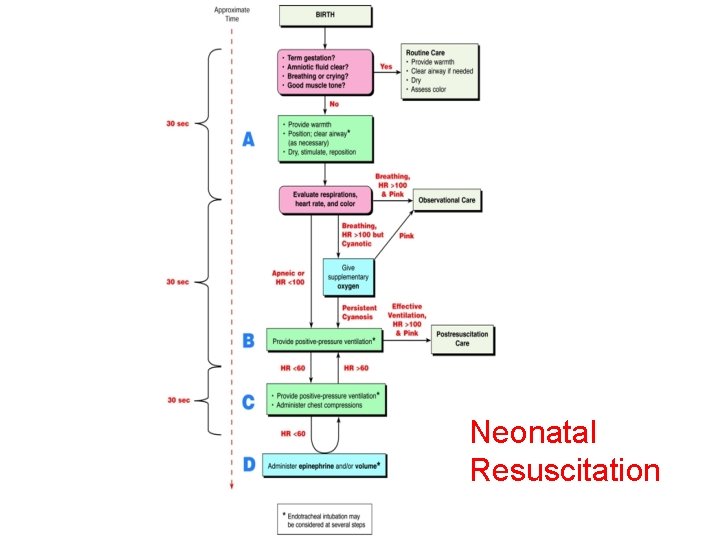
Neonatal Resuscitation
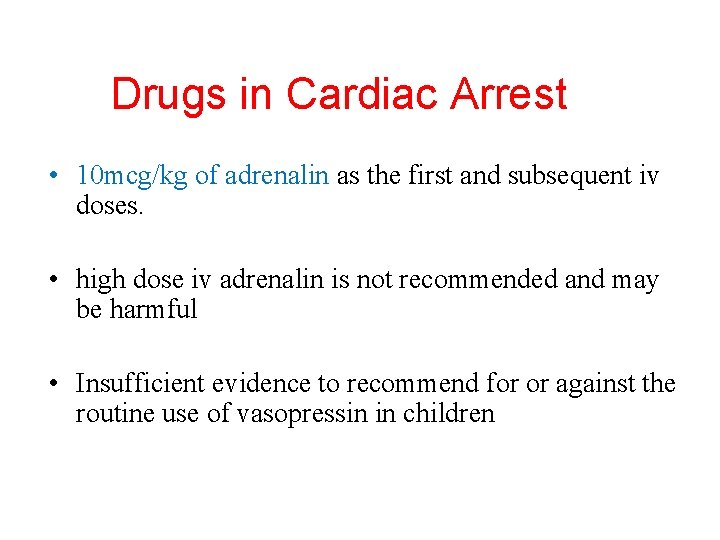
Drugs in Cardiac Arrest • 10 mcg/kg of adrenalin as the first and subsequent iv doses. • high dose iv adrenalin is not recommended and may be harmful • Insufficient evidence to recommend for or against the routine use of vasopressin in children
Route of drug delivery in ALS • where possible give drugs intra-vascularly rather than via the tracheal route – lower adrenaline concentrations may produce transient beta adrenergic effects resulting in hypotension. • Intra-osseous access is safe for fluid resuscitation and drug delivery.
Airway Management • guedel airways • laryngeal airways • Cuffed or uncuffed endotracheal tubes
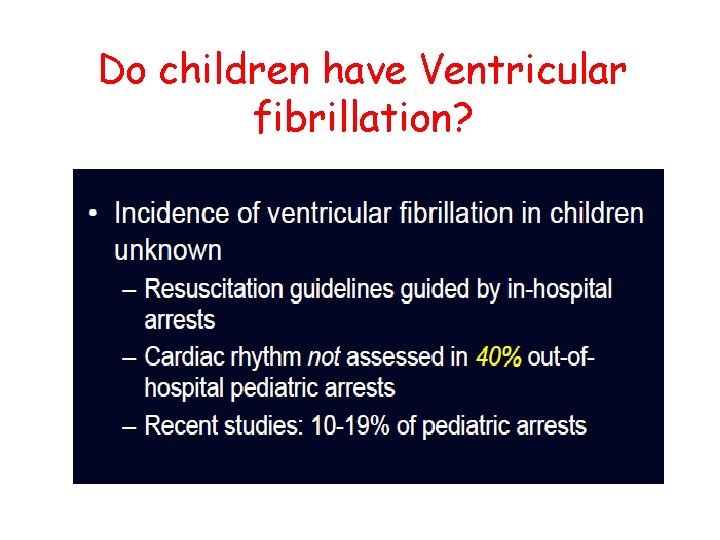
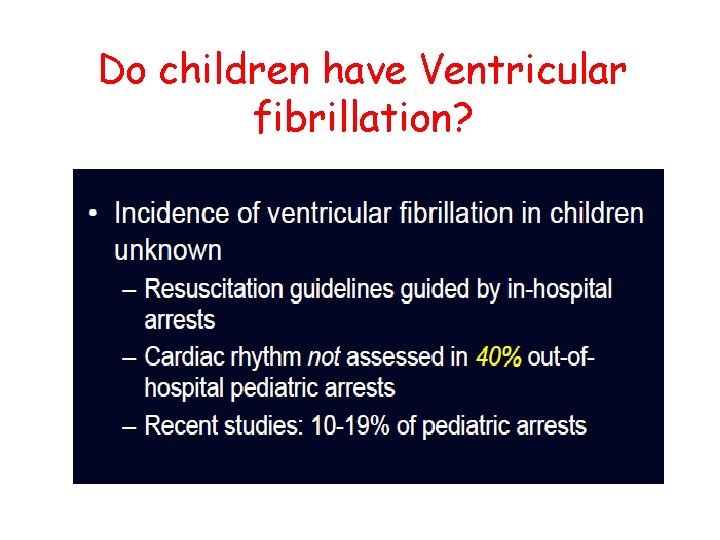
Do children have Ventricular fibrillation?
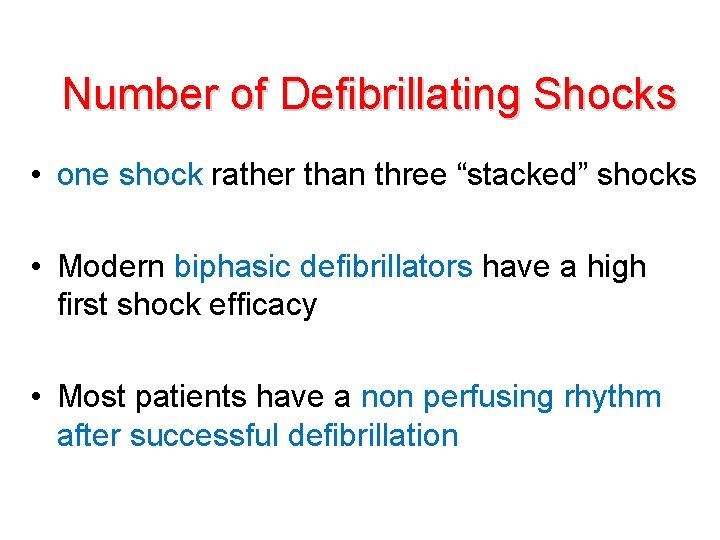
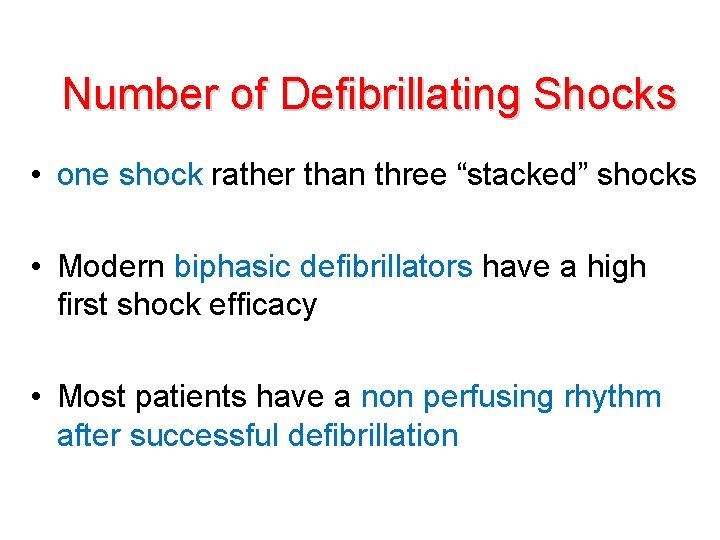
Number of Defibrillating Shocks • one shock rather than three “stacked” shocks • Modern biphasic defibrillators have a high first shock efficacy • Most patients have a non perfusing rhythm after successful defibrillation
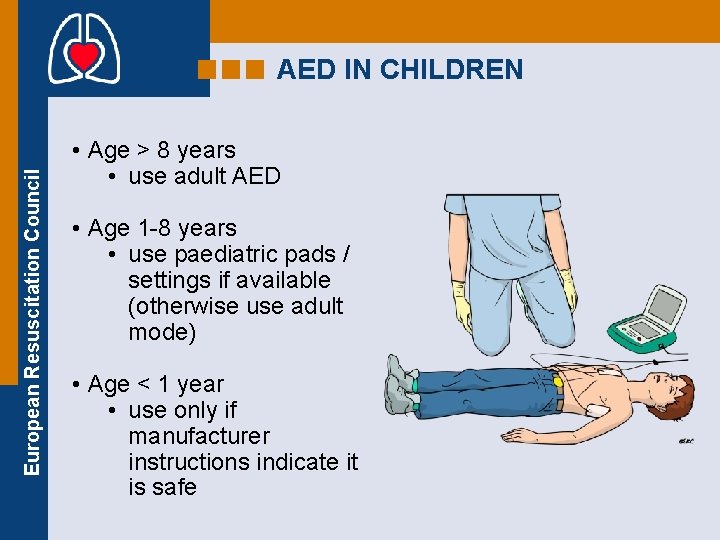
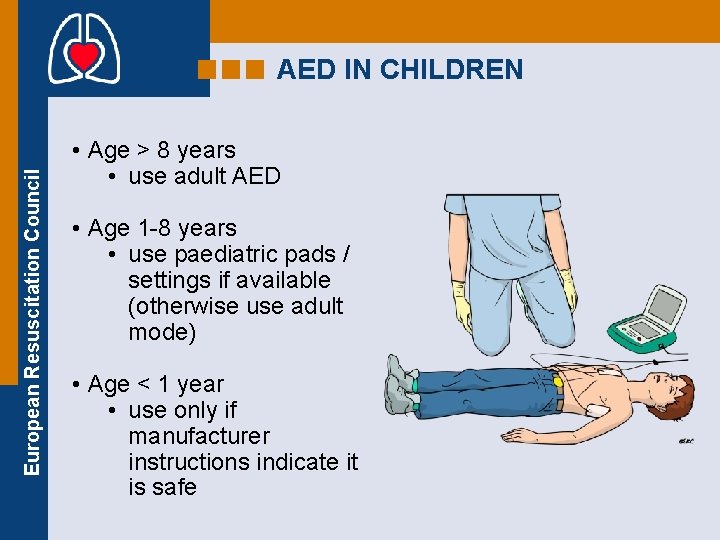
European Resuscitation Council AED IN CHILDREN • Age > 8 years • use adult AED • Age 1 -8 years • use paediatric pads / settings if available (otherwise use adult mode) • Age < 1 year • use only if manufacturer instructions indicate it is safe
Fluid Resuscitation • Boluses of fluid may be required to maintain systemic perfusion • Crystalloids - ringers or normal saline • Septic children may require in excess of 100 ml/kg fluid resuscitation
Family Presence during Resuscitation • Evidence suggests that the majority of parents would like to be present during resuscitation, that they gain a realistic understanding of the efforts made to save the child, and they subsequently show less anxiety and depression.

When do you start?
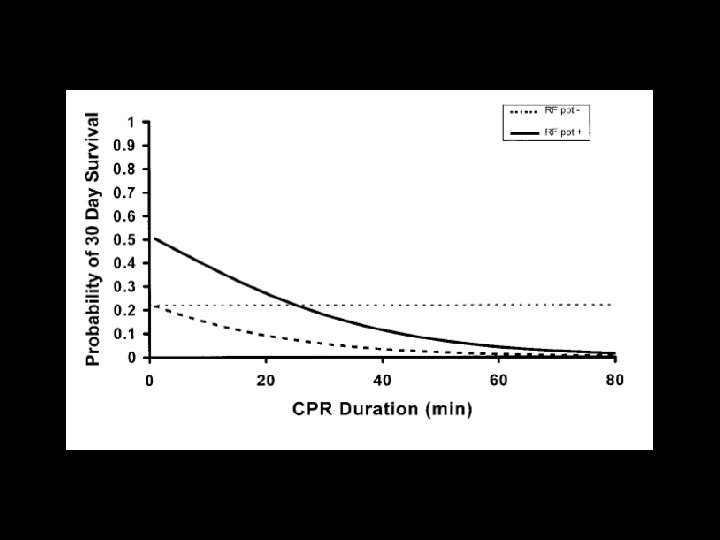
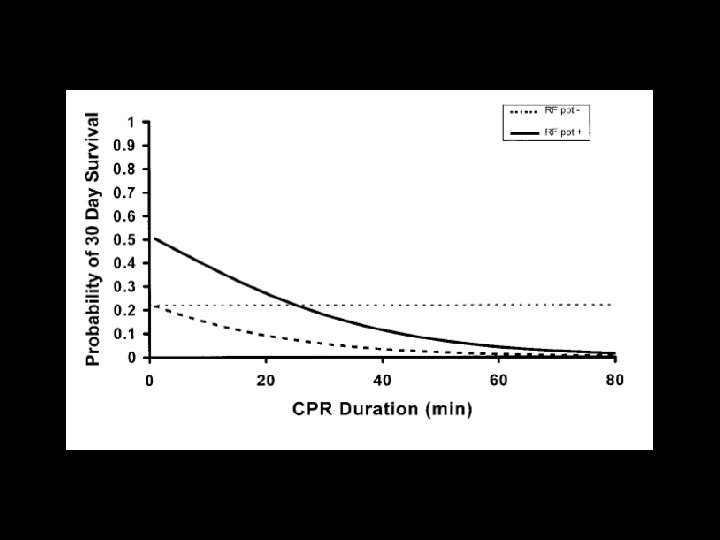
When do you stop? • In the absence of reversible causes eg drowning with severe hypothermia, poisoning, prolonged CPR in children is unlikely to result in intact neurological survival. • One should consider stopping resuscitation after 20 minutes.
Post Resuscitation Care • Ventilate to normo-capnoea • Hypothermia for 12 -24 hours post arrest may be helpful, whilst hyperthermia should be treated aggressively • Vaso-active drugs should be considered to improve haemodynamic status. • Maintain normoglycaemia
Conclusions: • The 2005 guidelines minimizes the differences in the steps and techniques of CPR used for infants, children and adults. • Push hard, push fast, minimizing interruptions • Respiratory failure and hypoxia is the commonest reason for paediatric arrests. • There are usually warning signs of impending doom, and early and effective therapy will prevent cardiac arrest
Questions
 Shamiel salie
Shamiel salie Chapter 17:2 performing cardiopulmonary resuscitation
Chapter 17:2 performing cardiopulmonary resuscitation Icu unit meaning
Icu unit meaning Chapter 27 cardiopulmonary procedures
Chapter 27 cardiopulmonary procedures Moro reflex
Moro reflex Cardiopulmonary
Cardiopulmonary Megalocardia word breakdown
Megalocardia word breakdown Overview of the major systemic arteries
Overview of the major systemic arteries Care of sick child ppt
Care of sick child ppt Levels of care primary secondary tertiary quaternary
Levels of care primary secondary tertiary quaternary Intensive care units
Intensive care units Difference between resuscitation and resurrection
Difference between resuscitation and resurrection Singapore resuscitation and first aid council
Singapore resuscitation and first aid council Acute resuscitation plan
Acute resuscitation plan Dope neonatal resuscitation
Dope neonatal resuscitation Bronze baby syndrome
Bronze baby syndrome Amber care bundle nice
Amber care bundle nice Endpoint of resuscitation
Endpoint of resuscitation Pediatric color code
Pediatric color code Principles of resuscitation
Principles of resuscitation European resuscitation council
European resuscitation council Resuscitation cpr
Resuscitation cpr European resuscitation council
European resuscitation council Bls
Bls Cpr meaning medical
Cpr meaning medical Dr sneha sood
Dr sneha sood Neonatal resuscitation
Neonatal resuscitation Management of asphyxia neonatorum after resuscitation
Management of asphyxia neonatorum after resuscitation Immediate newborn care steps
Immediate newborn care steps