NeonatalPediatric Cardiopulmonary Care Resuscitation 2 When To Resuscitate












- Slides: 58
Neonatal/Pediatric Cardiopulmonary Care Resuscitation

2 When To Resuscitate n Need usually related n Combination of n Can occur in
3 Causes of Fetal Asphyxia n n
4 Apnea
5 Effect of Asphyxia on Lungs n Initial adaption to extrauterine life requires 2 steps: – –

6 Effect of Asphyxia on Lungs Blood flow continues through d. a. & f. o. (by-passing lungs) Pulmonary hypertension Pulmonary vasoconstriction Asphyxia Apneic or ineffective respirations Negative pressure not generated to open Alveo li to push fluid out Pa. O 2 , Pa. CO 2 , p. H
7 Effect of Asphyxia on Lungs If asphyxia severe with lactic acidosis Ventilation alone will not change acid-base imbalance
8 Effect of Asphyxia on Lungs n In severe cases - might be beneficial to give HCO 3 to – – –
9 Effect of Asphyxia on Lungs n NOTE: Adequate ventilation must be maintained when bicarb given!!! Why? ?
10 Effect of Asphyxia on Lungs
11 Preparation For Resuscitation n
12 Basics of Neonatal Resuscitation 3 steps: n A- n B- n C-

13 Resuscitation Cycle Evaluation Decision Action
14 Steps in Resuscitation 1 st step =
15 Mechanisms of Heat Loss n Radiation – Loss to n Conduction – Loss to n Evaporation – Loss when n Convection – Loss to
16 Causes of Heat Loss n n n

Cold Stress 17
18 Steps in Resuscitation Next Step = Open airway n n
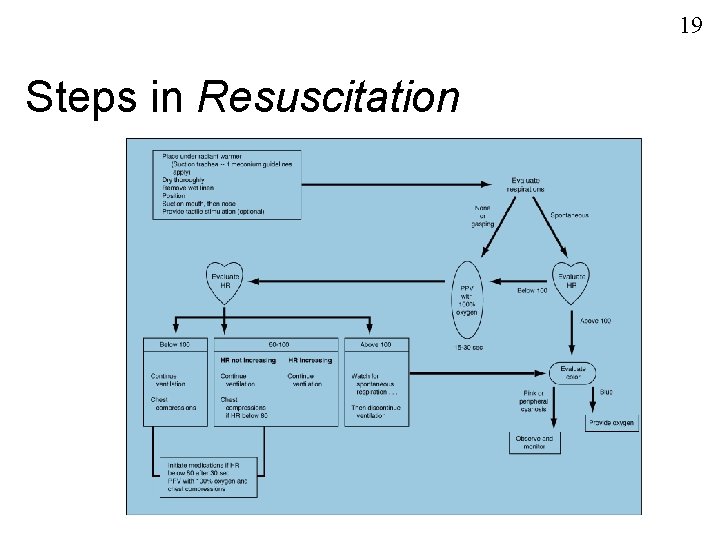
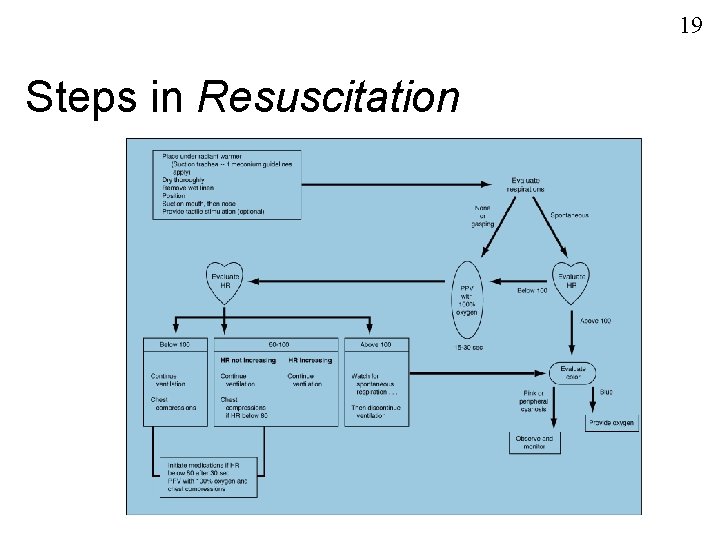
19 Steps in Resuscitation
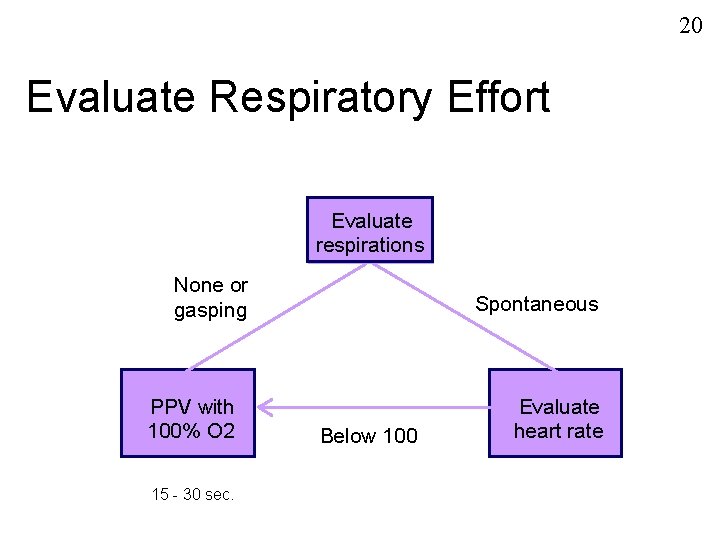
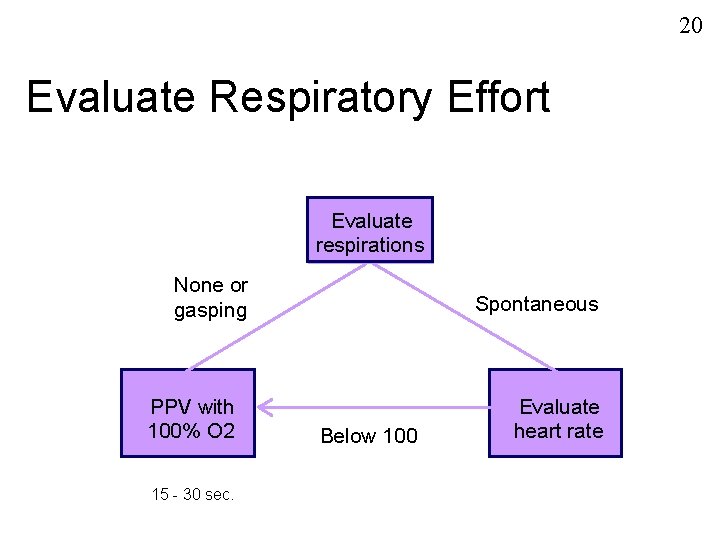
20 Evaluate Respiratory Effort Evaluate respirations None or gasping PPV with 100% O 2 15 - 30 sec. Spontaneous Below 100 Evaluate heart rate
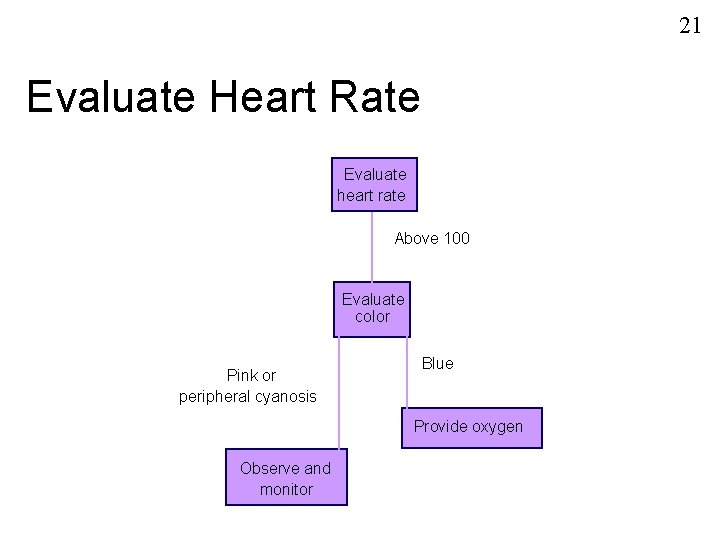
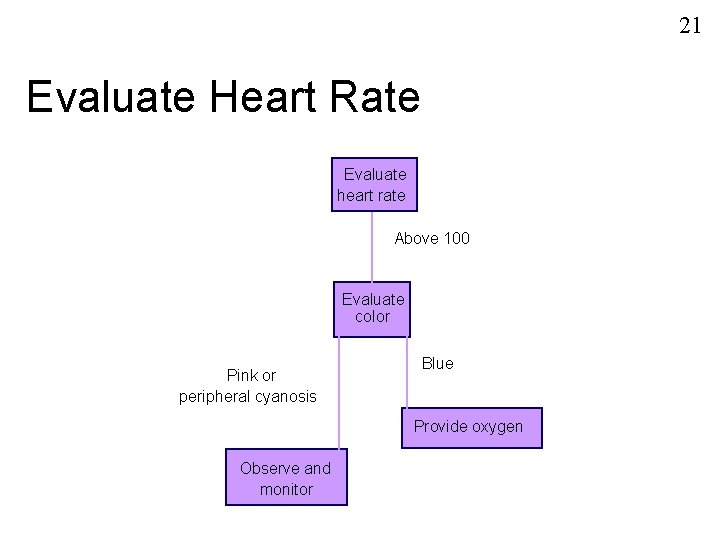
21 Evaluate Heart Rate Evaluate heart rate Above 100 Evaluate color Pink or peripheral cyanosis Blue Provide oxygen Observe and monitor
22 Indications for PPV n n
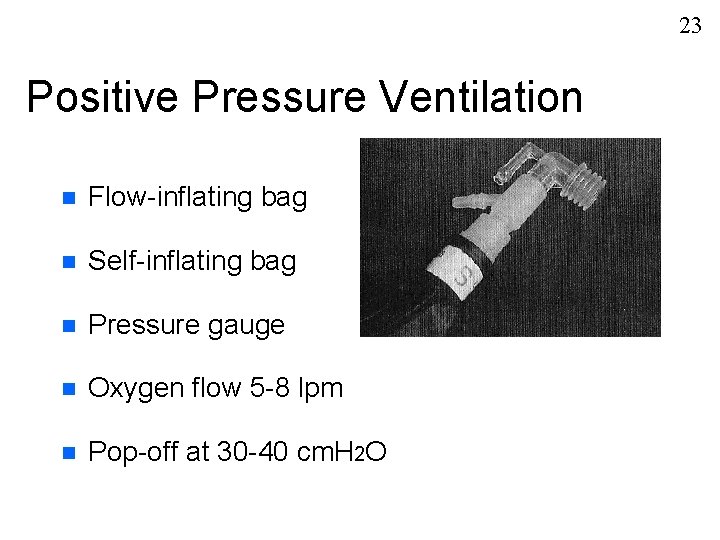
23 Positive Pressure Ventilation n Flow-inflating bag n Self-inflating bag n Pressure gauge n Oxygen flow 5 -8 lpm n Pop-off at 30 -40 cm. H 2 O
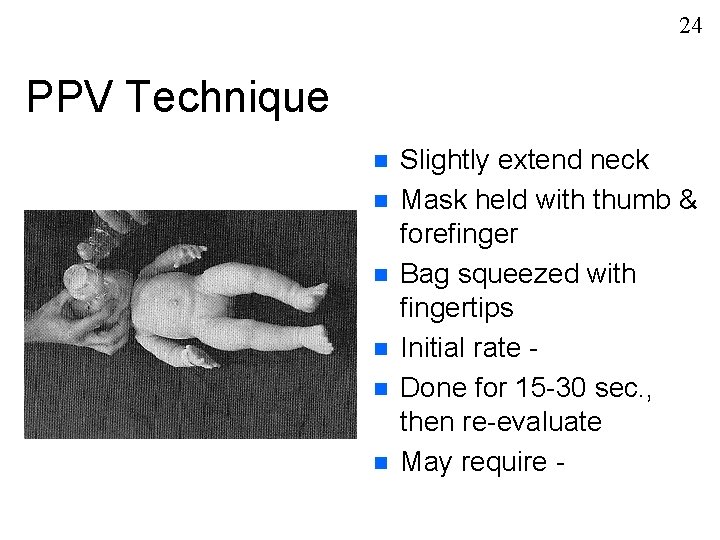
24 PPV Technique n n n Slightly extend neck Mask held with thumb & forefinger Bag squeezed with fingertips Initial rate Done for 15 -30 sec. , then re-evaluate May require -

25 Re-evaluate Heart Rate
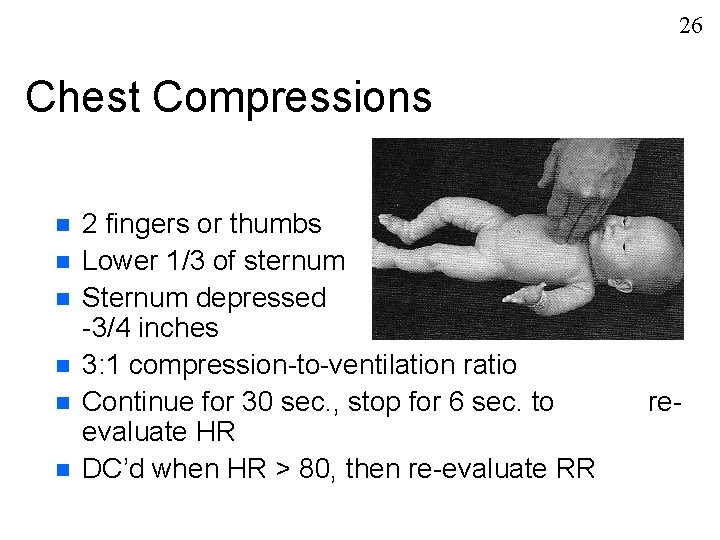
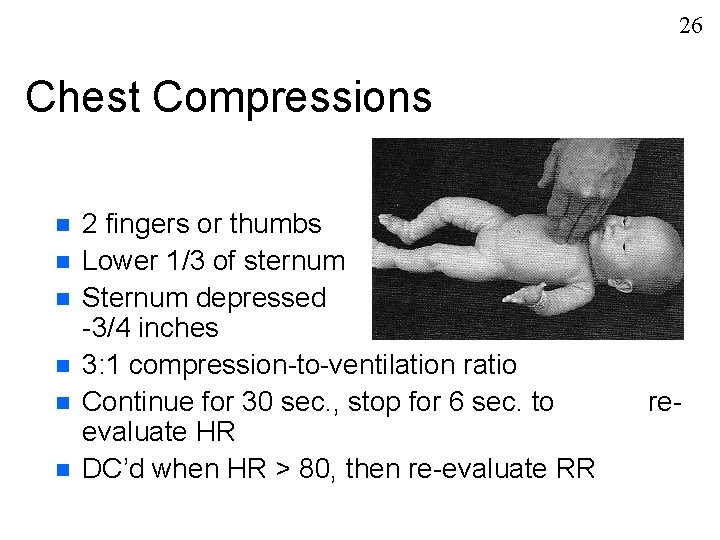
26 Chest Compressions n n n 2 fingers or thumbs Lower 1/3 of sternum Sternum depressed -3/4 inches 3: 1 compression-to-ventilation ratio Continue for 30 sec. , stop for 6 sec. to evaluate HR DC’d when HR > 80, then re-evaluate RR 1/2 re-
27 Indications for Intubation Bag/mask ventilation is difficult or ineffective n Prolonged PPV is required n Thick meconium is present in amniotic fluid n Suspicion of diaphragmatic hernia n
28 ETT Sizes
29 Laryngoscope Blades n Size 1 for n Size 0 for n

30 Intubation Technique n Same as adult n Limit attempts to - n Provide blow-by oxygen at - n ETT tip midway between carina & clavicles n Cut ETT to leave -
31 Medications - Uses n n n
32 Medications - Routes n n
33 Instillation Into ETT N A V E L O 2
34 Medications - Indications n HR < 80 despite PPV and chest compressions for at least 30 sec. n HR is 0
35 Epinephrine n Powerful sympathomimetic – – – 1 st drug given n IV or ETT, delivered rapidly n Repeated q 3 -5’ until HR n
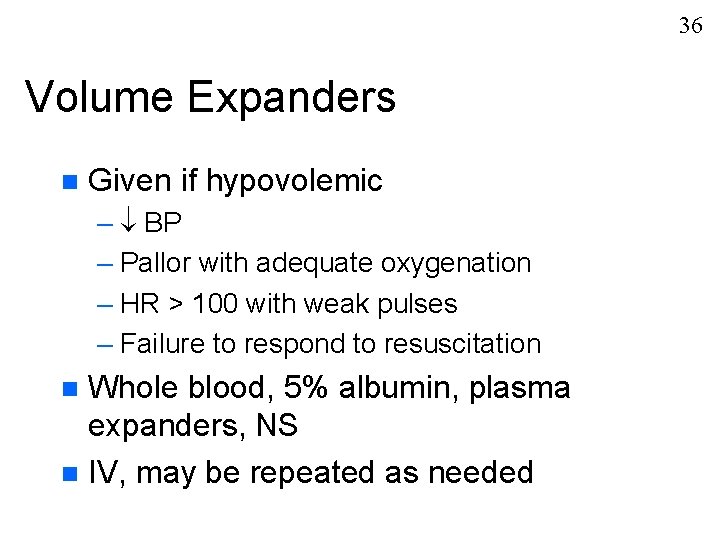
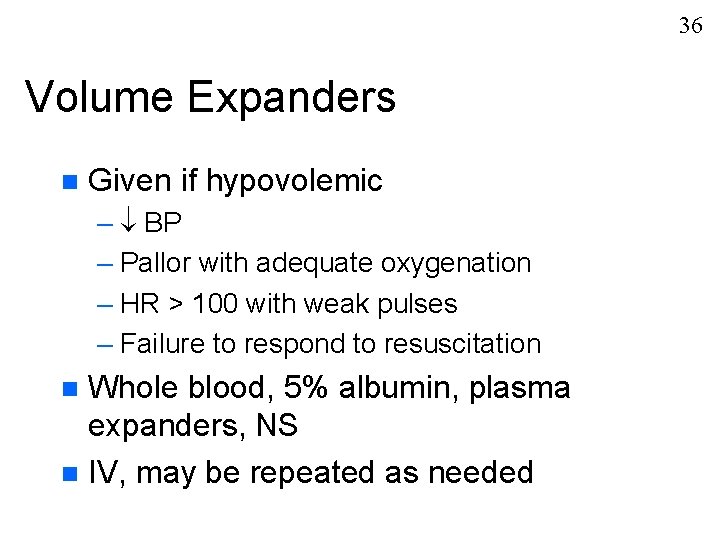
36 Volume Expanders n Given if hypovolemic – BP – Pallor with adequate oxygenation – HR > 100 with weak pulses – Failure to respond to resuscitation Whole blood, 5% albumin, plasma expanders, NS n IV, may be repeated as needed n

37 Sodium Bicarbonate n Prolonged arrest & not responding n Alkaline to buffer metabolic acidosis n Only given when ventilation is adequate n IV

38 Narcan (naloxone) n Reversal of narcotic depression – Demerol (meperidine) – Morphine sulfate – Fentanyl (Sublimaze) n IV, IM, sub-q, ETT n Given rapidly
39 Dopamine n n n
40 APGAR Scoring n n
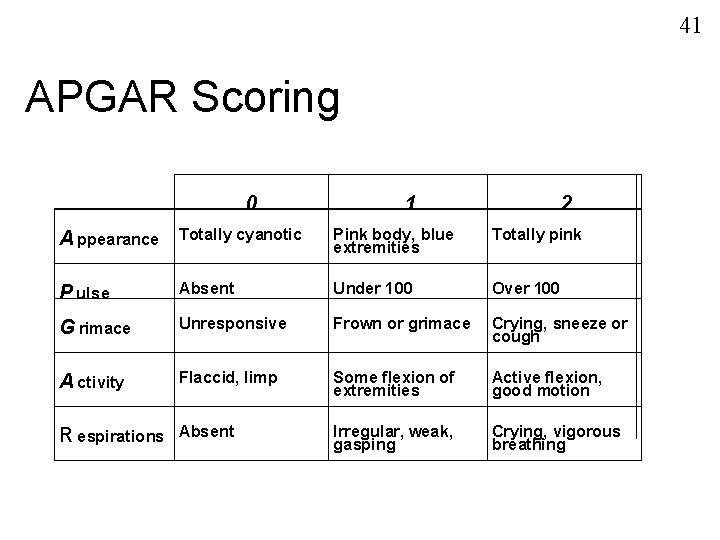
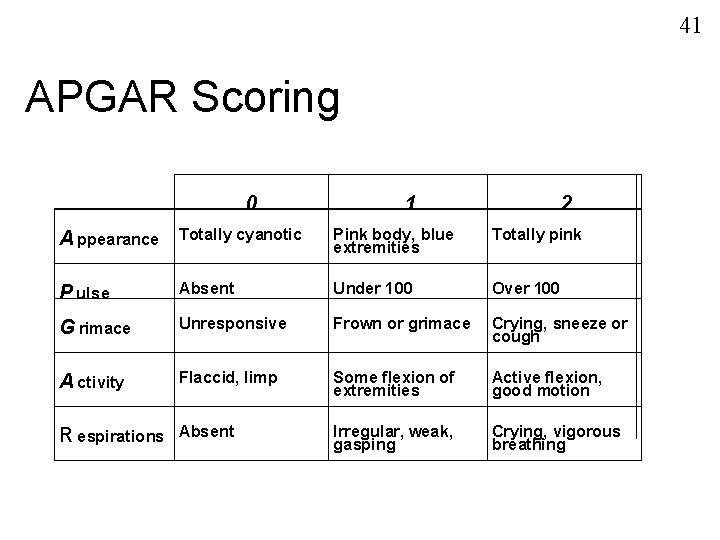
41 APGAR Scoring 0 A ppearance Totally cyanotic 1 2 Pink body, blue extremities Totally pink P ulse Absent Under 100 Over 100 G rimace Unresponsive Frown or grimace Crying, sneeze or cough A ctivity Flaccid, limp Some flexion of extremities Active flexion, good motion Irregular, weak, gasping Crying, vigorous breathing R espirations Absent
42 Serum Glucose Sources n Nutritional needs of fetus supplied by Mom & regulated by placenta n Fetus prepares for postnatal life by energy stores & developing enzymedependant processes for usage of stored energy
43 Serum Glucose Energy Storage n Glycogen – – n Triglycerides (brown fat) – –
44 Serum Glucose Post-delivery At 2 hours By 3 days -
45 Serum Glucose Hypoglycemia Term Preterm -
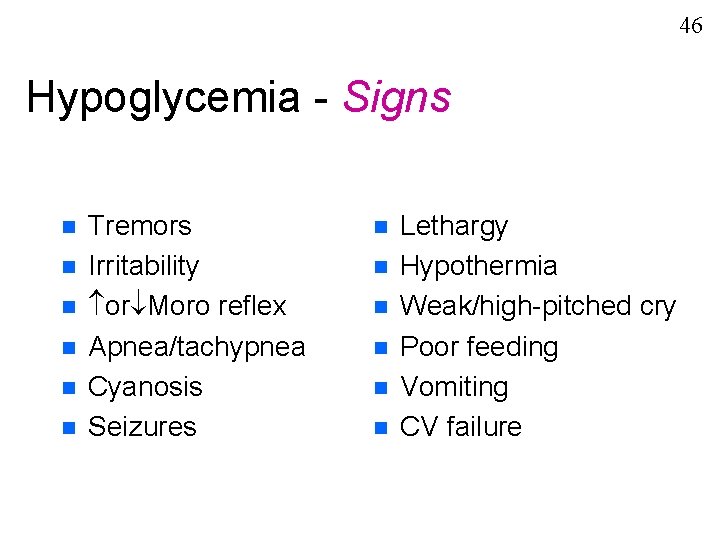
46 Hypoglycemia - Signs n n n Tremors Irritability or Moro reflex Apnea/tachypnea Cyanosis Seizures n n n Lethargy Hypothermia Weak/high-pitched cry Poor feeding Vomiting CV failure
47 Hypoglycemia
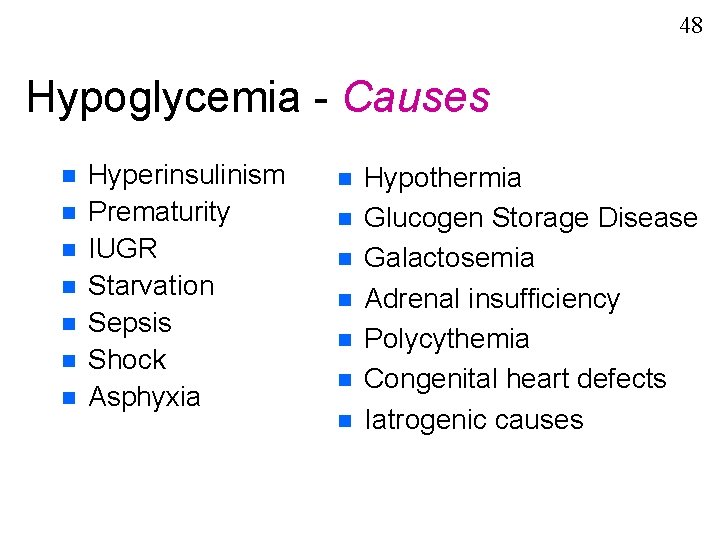
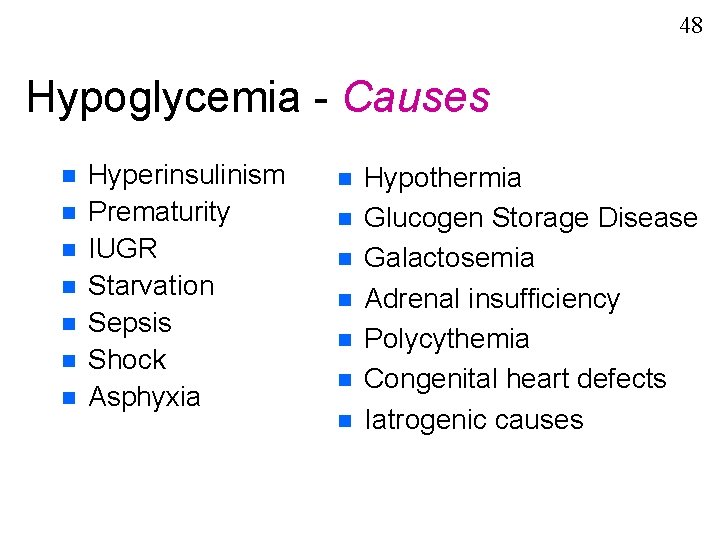
48 Hypoglycemia - Causes n n n n Hyperinsulinism Prematurity IUGR Starvation Sepsis Shock Asphyxia n n n n Hypothermia Glucogen Storage Disease Galactosemia Adrenal insufficiency Polycythemia Congenital heart defects Iatrogenic causes
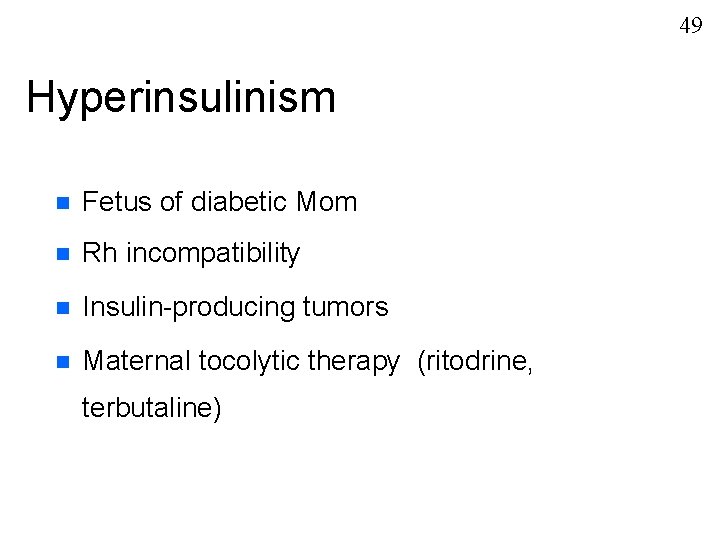
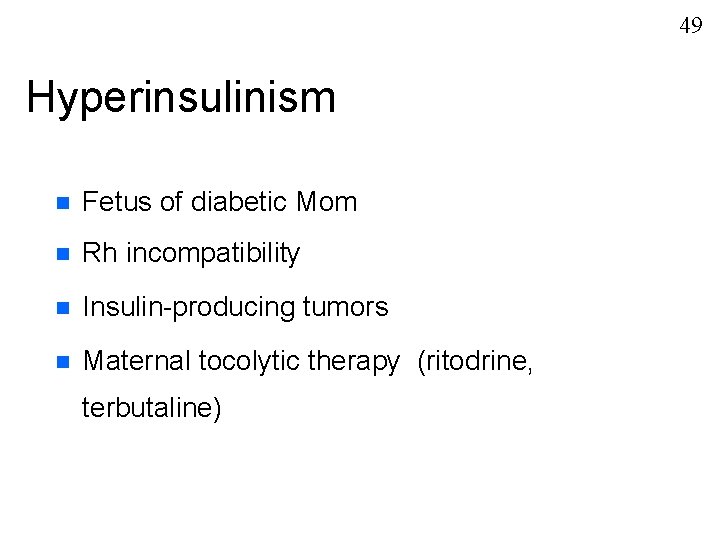
49 Hyperinsulinism n Fetus of diabetic Mom n Rh incompatibility n Insulin-producing tumors n Maternal tocolytic therapy (ritodrine, terbutaline)

50 Glucose Measurement n Glucose Test Strip “Dextrostik” n “One Touch” n Lab sample (blood glucose)

51 Hypoglycemia Treatment Early feeding (oral) n D 10 W n – 200 mg/kg bolus over 1 -3 minutes – Con’t IV, 4 -8 mg/kg/min. until feedings started n Treat cause
52 Umbilical Blood Sampling n n
53 Umbilical Vein Catheter (UVC) n Usually placed in - n Drug administration during -
54 Umbilical Artery Catheter (UAC) Indications n n n
55 Umbilical Artery Catheter (UAC) Placement 5 Fr. catheter (>1250 g), 3. 5 Fr. catheter (<1250 g) n Sterile procedure n Heparinized-filled catheter n Tip L 3 -4 for low catheter, T 8 for high catheter (in aorta below renal a. , above bifurcation of femoral a. ) n

56 UAC
57 Umbilical Artery Catheter Complications n n n

58 Umbilical Artery Catheter Sampling Technique n n
 Chapter 17:2 performing cardiopulmonary resuscitation
Chapter 17:2 performing cardiopulmonary resuscitation Pediatric trach ties
Pediatric trach ties Peter neronha
Peter neronha Cardiopulmonary word breakdown
Cardiopulmonary word breakdown Crossword puzzle cardiopulmonary procedures
Crossword puzzle cardiopulmonary procedures Pulmonary circulation diagram
Pulmonary circulation diagram Moro reflex
Moro reflex Emergency medical responder first on scene 10th edition
Emergency medical responder first on scene 10th edition Primary secondary and tertiary care
Primary secondary and tertiary care Bls
Bls Bronze baby syndrome
Bronze baby syndrome Management of asphyxia neonatorum after resuscitation
Management of asphyxia neonatorum after resuscitation European resuscitation council
European resuscitation council Parkland formula
Parkland formula National resuscitation council singapore
National resuscitation council singapore Introduction to cpr
Introduction to cpr Endpoint of resuscitation
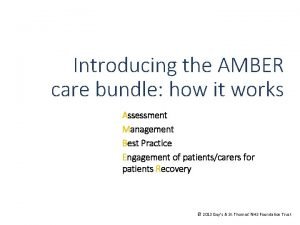
Endpoint of resuscitation Amber care bundle nice
Amber care bundle nice Grimace reflex
Grimace reflex Resuscitation cpr
Resuscitation cpr Acute resuscitation plan
Acute resuscitation plan Neonatal resuscitation definition
Neonatal resuscitation definition Pediatric color code
Pediatric color code Cardioprotection resuscitation
Cardioprotection resuscitation European resuscitation council
European resuscitation council Site:slidetodoc.com
Site:slidetodoc.com Preterm classification
Preterm classification Principles of resuscitation
Principles of resuscitation Pulseless electrical activity
Pulseless electrical activity Difference between resuscitation and resurrection
Difference between resuscitation and resurrection Care certificate answers standard 3
Care certificate answers standard 3 Palliative care versus hospice care
Palliative care versus hospice care Hip fracture clinical care standard
Hip fracture clinical care standard Animale care nasc un singur pui
Animale care nasc un singur pui Care value base health and social care
Care value base health and social care Standard 3 care certificate
Standard 3 care certificate Care sunt simturile prin care sunt evocate
Care sunt simturile prin care sunt evocate Polii magnetici de acelasi nume se
Polii magnetici de acelasi nume se Aarti home care
Aarti home care Care information exchange
Care information exchange Benefits of primary care networks
Benefits of primary care networks Why did people care about the butler act?
Why did people care about the butler act? Nursing care plan case scenario
Nursing care plan case scenario Dhcs 4026
Dhcs 4026 Basic skin care definition
Basic skin care definition Homecare worker orientation
Homecare worker orientation Soars login
Soars login How care
How care Wound care pretest
Wound care pretest Self care plan
Self care plan Graded care profile derbyshire
Graded care profile derbyshire Types of jawless fish
Types of jawless fish South west london health and care partnership
South west london health and care partnership Barbara starfield primary care principles
Barbara starfield primary care principles Care voyant
Care voyant Intuitive curl care
Intuitive curl care Secondary care definition
Secondary care definition Preferred priorities for care
Preferred priorities for care Factors of care a patient can expect
Factors of care a patient can expect