Approach to Pediatric Neutropenia June 9 2016 Stefani
- Slides: 33
Approach to Pediatric Neutropenia June 9 2016 Stefani Doucette PGY-3
Objectives Recognize clinical presentations of neutropenia ID patients needing work up for immunodeficiency Formulate differential diagnosis List risk factors for serious bacterial infection
Objectives Differentiate between benign and serious causes of neutropenia List treatment approaches for neutropenia Know when to refer to pediatric hematology/oncology
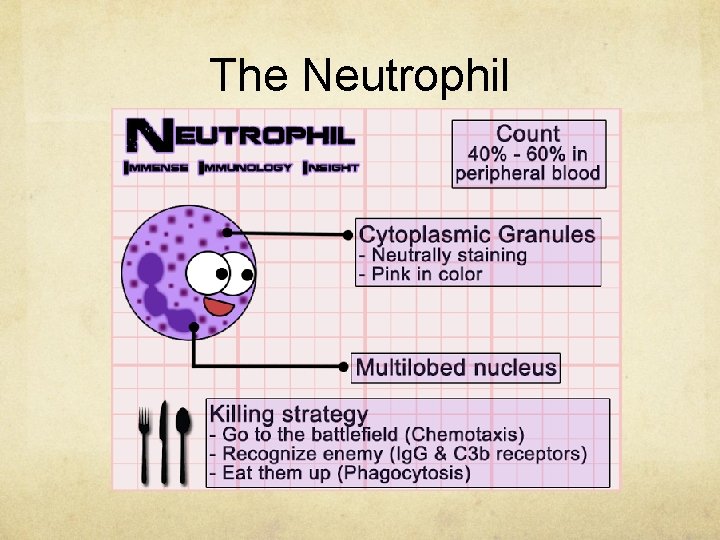
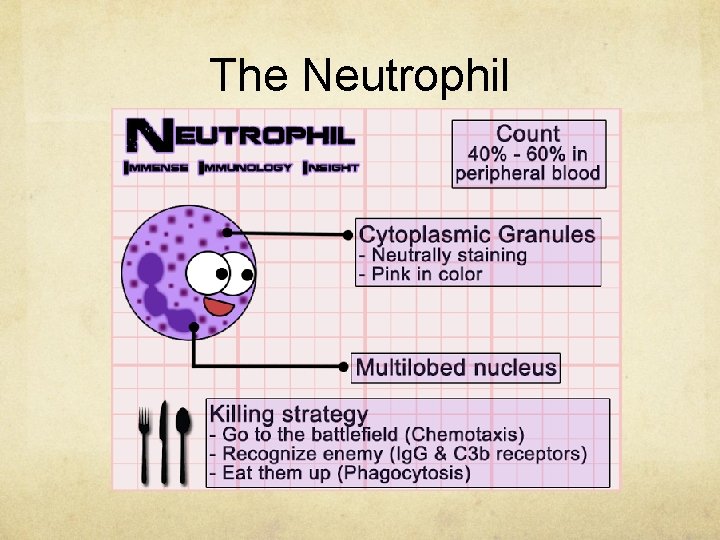
The Neutrophil
Terminology Neutropenia: decrease in the absolute number of circulating segmented neutrophils and band forms in the blood Absolute neutrophil count: multiply WBC by percentage of segmented and band forms of leukocytes Normal ANC 1. 5 -8 x 109/L
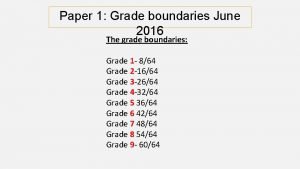
Definitions Acute neutropenia: less than 3 months duration Chronic neutropenia: over four months duration Mild neutropenia: ANC 1. 0 -1. 5 x 109/L Moderate neutropenia: ANC 0. 5 -1. 0 x 109/L Severe neutropenia: ANC < 0. 5 x 109/L
Clinical Presentations Pyogenic infection: cellulitis, abscesses, furunculosis, pneumonia, septicemia Stomatitis, gingivitis Perirectal inflammation, AOM Diffuse intestinal lesions presenting with abdominal pain and diarrhea
Caution! Don’t be reassured by “mild” infection Signs and symptoms of localized infections diminished in neutropenic patients May not see as much exudate, abscess formation, regional lymphadenopathy Redness, pain, tenderness, warmth and fever are mediated by cytokines should be present
Most Common Pathogens Staphylococcus aureus Gram negative organisms Staphylococcus epidermidis Streptococci Enterococci
Risk of Severe Infection Acute neutropenia d/t chemotherapy, BM failure, marrow exhaustion Neutropenic patients receiving cytotoxic or immunosuppressive drugs Patients with disorders of neutrophil production and release with higher risk of infection Patients receiving chemotherapy for malignancy at greater risk of infection
Evaluation of Neutropenia With ANC < 1. 0 x 109/L, ask for manual differential to rule out blasts or circulating immature neutrophils History and physical Severity and duration of neutropenia determines extent of lab evaluation and investigations ordered
History Onset of neutropenia Type, frequency, severity of infections Drug or toxin exposures Family history of recurrent infection or unexplained infant deaths
Red Flags > 2 systemic bacterial infections /yr (sepsis, meningitis, osteomyelitis) > 2 episodes of pneumonia in a year Multiple bacterial infections in a year (cellulitis, draining AOM, lymphadenitis) Unusual infections involving liver, brain abscess Infections caused by unusual bugs (aspergillus, caididiasis, serratia, nocardia, burkholderia) Infections of unusual severity Chronic gingivitis, recurrent apthous ulcers
Physical Exam Growth and development Phyenotypic abnormalities Mucous membranes, gingiva, skin, tympannic membranes, rectum Look for lymphadenopathy, hepatosplenomegaly, signs of possible underlying disease Look for petechiae and purpura Measure temp, but not rectally!
Investigations Extent of work up depends on duration of symptoms If neutropenic at present rpt CBC in 3 -4 weeks If neutropenia persists in an asymptomatic infant, order antineutrophil antibody If neutropenia persists in a symptomatic child consider referral to hematology for serial CBCs and consideration of BMA If neutropenia and malabsorption consider Scwachman-Diamond Syndrome
Acquired Neutropenias Infection Drug Induced Immune Neutropenia Sequestration/hypersplenism Marrow replacement, chemo, radiation effects Ineffective myelopoeisis
Infection Viral infection is the major cause! RSV, varicella, flu A and B, measles, rubella, EBV Neutropenia seen 24 -48 into illness; lasts 3 -8 days Mechanisms of neutropenia: Redistribution to marginating pool Increased use of neutrophils at sites of infection Decreased neutrophil production
Drug Induced Immunologic, toxic, hypersensitivity mediated mechanisms of causing neutropenia Phenothiazines, sulfonamides, anticonvulsants, penicillins, aminopyrine Treat by discontinuing the offending agent If neutropenia does not improve and patient is symptomatic, consider 5 ug/kg G-CSF
Immune Neutropenias Circulating antineutrophil antibodies Immunofluorescence and microcapillary agglutination assays are used to determine antibody presence If antibodies against RBCs and platelets are also present think about Evans syndrome
Alloimmune Neonatal Neutroenia Transplacental transfer of maternal alloantibodies against an antigen on infant’s neutrophils 0. 2% pregnancies Delayed cord separation mild skin infections, fever, pneumonia in the first 2 weeks of life Recovers by 7 weeks after birth as maternal antibodies will no longer be present Supportive care, antibiotics, G-CSF if severe infection
Autoimmune Neutropenia of Infancy Caused by granulocyte specific autoantibodies Infants aged 5 -15 months 90% do not have increased risk of pyogenic infections 95% undergo spontaneous remission in 7 -30 months Repeat antibody screening until antibodies are detected Supportive treatment with antibiotics as needed These kids can receive live vaccines
Sequestration/Hyperspleni sm Splenic enlargement causing neutropenia Neutropenia most often mild to moderate Seen with thrombocytopenia and anemia Treat underlying disease and cytopenias improve Rarely splenectomy indicated to restore neutrophils
Marrow Replacement Malignancies suppress myelopoeisis by infiltrating BM Chemo and radiation damage BM stem cells Aplastic anemia also leads to neutropenia Manage with prompt treatment of infections with broad spectrum antibiotics to cover s. aureus and p. aeruginosa Only manifestation of infection might be fever
Ineffective Myelopoeisis Congenital or acquired vitamin B 12/folate deficiency Rare in pediatrics! May be seen in infants with starvation/marasmus Adolescents with anorexia nervosa Extended use of antibiotics
Intrinsic Neutropenia Congenital disorders Cyclic neutropenia Severe congenital neutropenia
Congenital Disorders Severe combined immunodeficiency syndromes Hyper Ig. M syndrome Common variable immunodeficiencies Glycogen storage disease type 1 b Schwachman Diamond syndrome Cyclic neutropenia Severe congenital neutropenia
Cyclic Neutropenia AD inheritance Incidence 0. 6/million Mutation in neutrophil elastase gene Regular periodic oscillations of neutrophils Reciprocity between neutrophil and monocyte counts Oral ulcers, stomatitis, cutaneous infections, pneumonia, mucosal ulcerations
Cyclic Neutropenia Repeat CBC 2 -3 times per week for two months to establish oscillating pattern of cell counts Diagnosis confirmed with molecular genetic studies to demonstrate mutations in elastase gene Treat with daily G-CSF to decrease risk of fatal infections with clostridium or gram negatives and also to decrease amount of antibiotic use
Severe Congenital Neutropenia Arrest in myeloid maturation at the promyelocyte stage ANC < 0. 2 x 109/L three separate times in a month Incidence 1 per million AD and AR inheritance Mouth ulcers, gingivitis, stomatitis, AOM, resp infections, cellulitis, skin abscesses, pneumonia and deep tissue abscesses
Severe Congenital Neutropenia Peripheral eosinophilia and monocytosis Thrombocytosis and anemia of chronic disease Bone marrow: arrest of myeloid cell maturation 10 -20% develop MDS or AML Require yearly bone marrow studies to screen Following leukemic transformation, only treatment option is stem cell transplant
Management Depends on cause! Viral induced, ANN, AIN: watchful waiting Drug induced: stop offending drug if possible Chemo/radiation/immunosuppressed: antibiotics Cyclic neutropenia: G-CSF Severe congenital neutropenia: G-CSF or HSCT
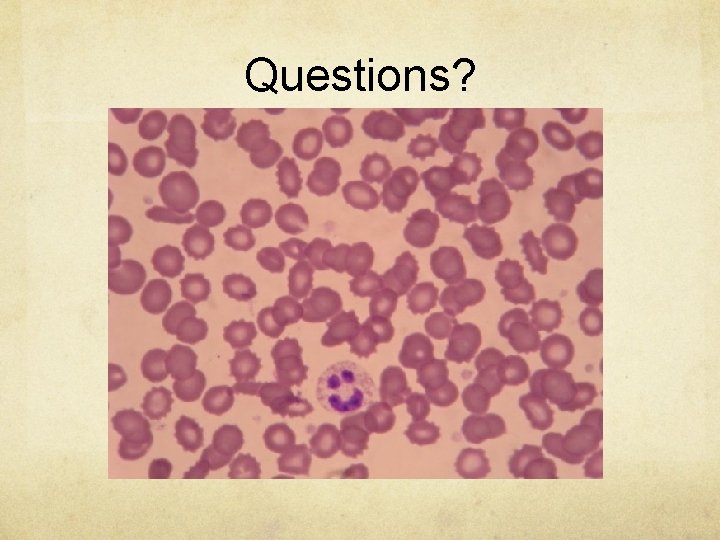
Questions?
References Pomeranz, A. J. et al. (2016). Pediatric Decision Making Strategies 2 nd edition. Philadelphia, PA: Elsevier Kliegman, R. M. et al. (2011). Nelson Textbook of Pediatrics 19 th edition. Philadelphia, PA: Elsevier Walkovich, K. , Boxer, L. A. “How to Approach Neutropenia in Childhood”. Pediatrics in Review. 34(4): 173 -184 http: //immense-immunologyinsight. blogspot. ca/search/label/Get%20 to%20 immuknow%20 the%20 cells http: //www. picturegr. am/tag/blood. Smear
 Raffaella stefani
Raffaella stefani Stefani coverson
Stefani coverson The skin cracks like a pod
The skin cracks like a pod Flacs checkpoint b spanish exam june 2016 answers
Flacs checkpoint b spanish exam june 2016 answers Raquel bratos lorenzo
Raquel bratos lorenzo Granulocyes
Granulocyes Neutropenia febril
Neutropenia febril Cisne neutropenia
Cisne neutropenia Neutropenia grade
Neutropenia grade Criterios de neutropenia febril
Criterios de neutropenia febril Otanr
Otanr Alopecia cuidados de enfermeria
Alopecia cuidados de enfermeria Neutropenia febril
Neutropenia febril Masc neutropenia febril
Masc neutropenia febril Marcos melian sosa
Marcos melian sosa Research approach meaning
Research approach meaning International market selection model
International market selection model Traditional approach vs object oriented approach
Traditional approach vs object oriented approach Avoidance
Avoidance Deep learning approach and surface learning approach
Deep learning approach and surface learning approach Virtual circuit and datagram networks in computer networks
Virtual circuit and datagram networks in computer networks Cognitive approach vs behavioral approach
Cognitive approach vs behavioral approach Theoretical models of counseling
Theoretical models of counseling Welcome june blessings
Welcome june blessings Nysedregents
Nysedregents Good morning 1 june
Good morning 1 june June preschool newsletter
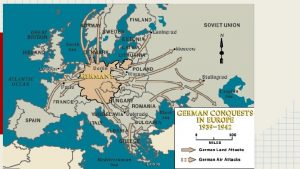
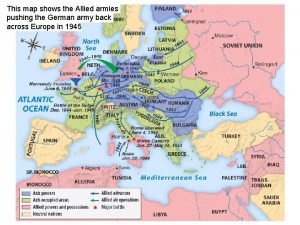
June preschool newsletter June 6th 1944
June 6th 1944 Battle of midway june 1942
Battle of midway june 1942 Prince waste collection pays a yearly
Prince waste collection pays a yearly Network weaver
Network weaver June 21 2019 geometry regents answers
June 21 2019 geometry regents answers 1 june children's day
1 june children's day Flacs checkpoint b spanish exam june 2018 answers
Flacs checkpoint b spanish exam june 2018 answers