Adrenal Pathology Kristine Krafts M D Adrenal Path










- Slides: 45
Adrenal Pathology Kristine Krafts, M. D.
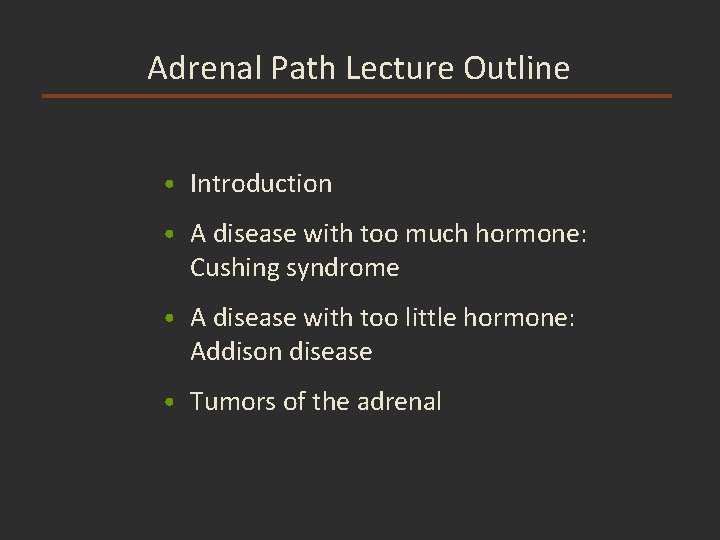
Adrenal Path Lecture Outline • Introduction • A disease with too much hormone: Cushing syndrome • A disease with too little hormone: Addison disease • Tumors of the adrenal
Adrenal Path Lecture Outline • Introduction
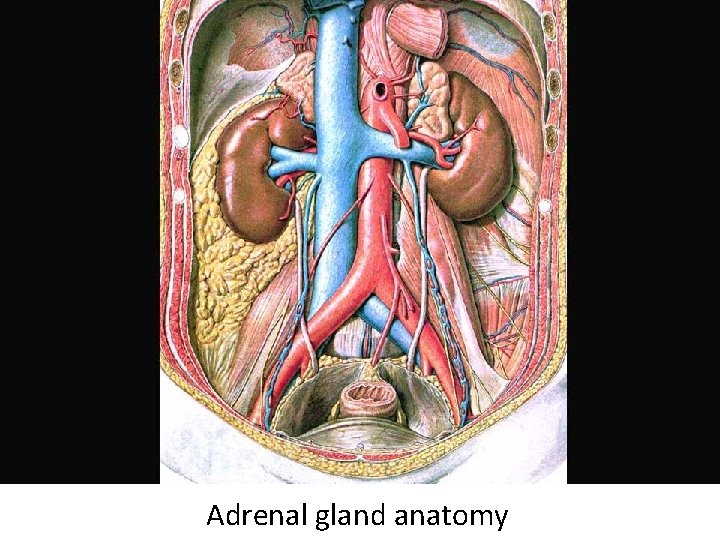
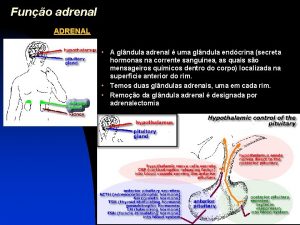
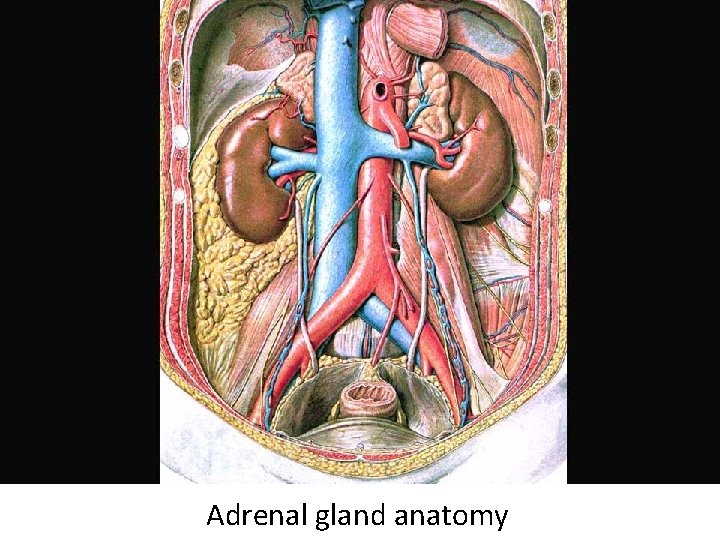
Adrenal gland anatomy
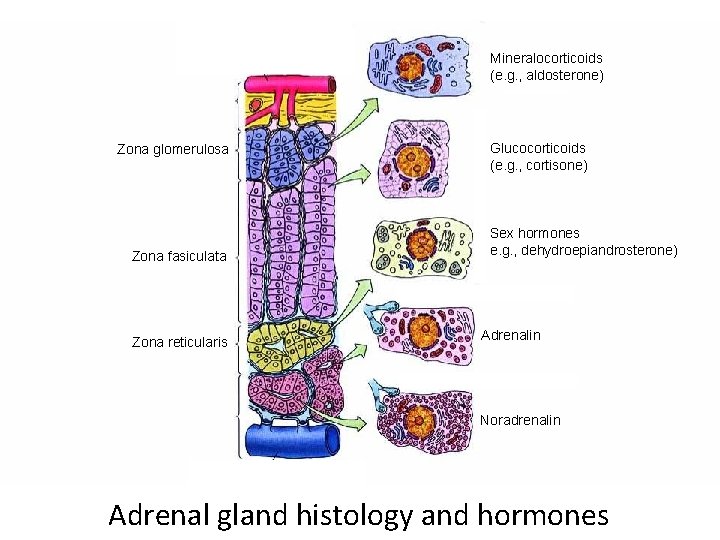
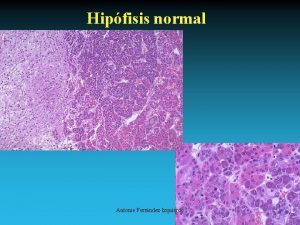
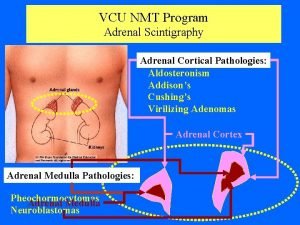
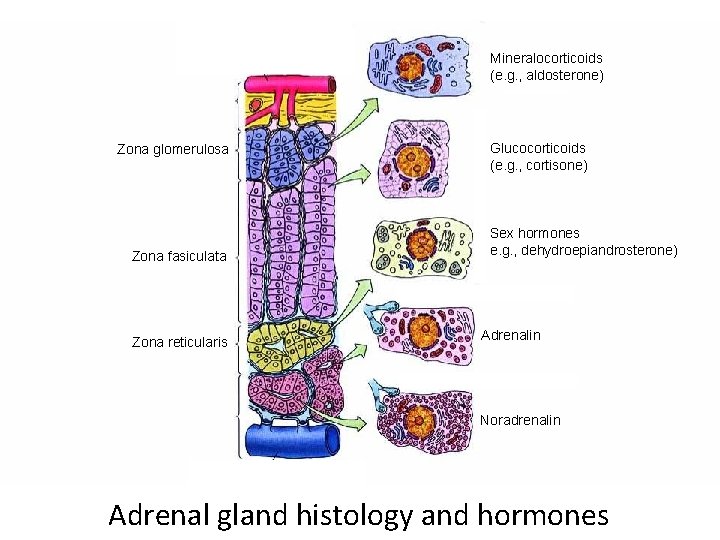
Mineralocorticoids (e. g. , aldosterone) Hormones: Zona glomerulosa Capsule Zona fasiculata Zona reticularis Glucocorticoids (e. g. , cortisone) Sex hormones e. g. , dehydroepiandrosterone) and Adrenalin Noradrenalin Medulla Adrenal gland histology and hormones
Adrenal Path Lecture Outline • Introduction • A disease with too much hormone: Cushing syndrome
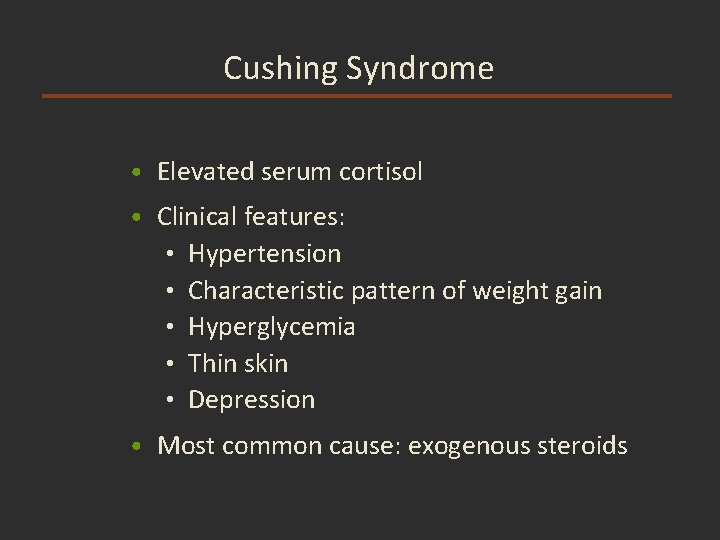
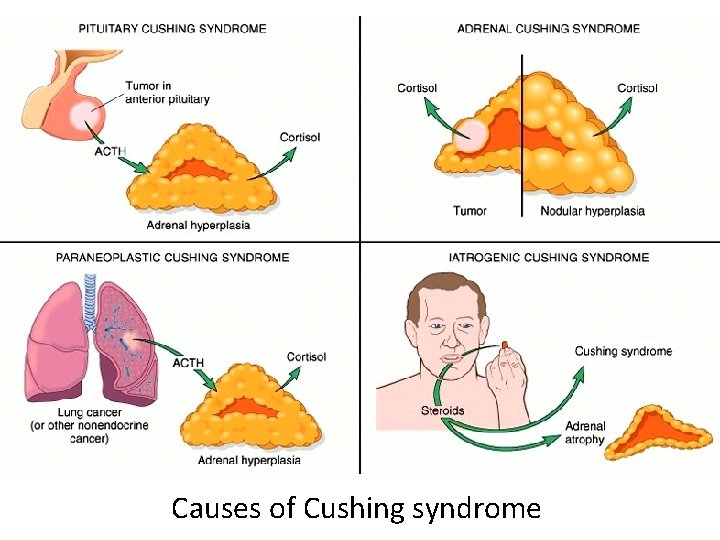
Cushing Syndrome • Elevated serum cortisol • Clinical features: • Hypertension • Characteristic pattern of weight gain • Hyperglycemia • Thin skin • Depression • Most common cause: exogenous steroids
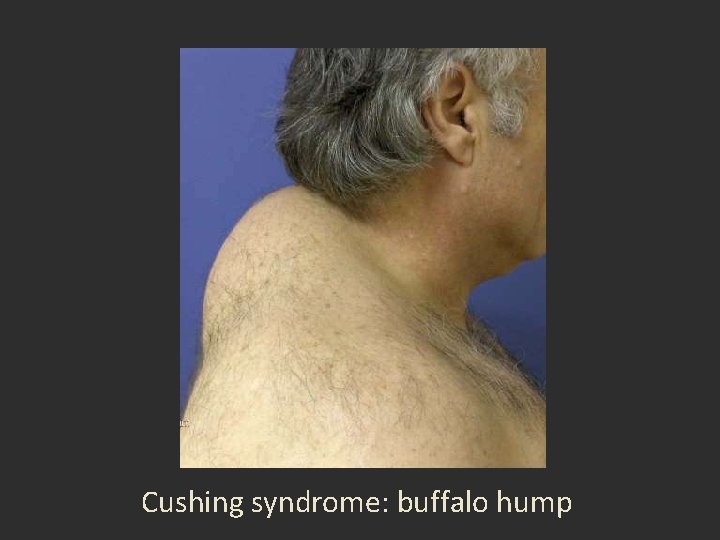
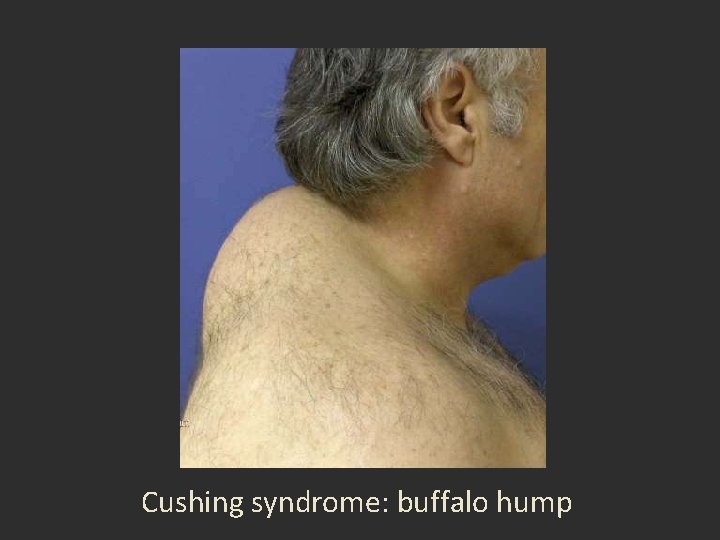
Cushing syndrome: buffalo hump
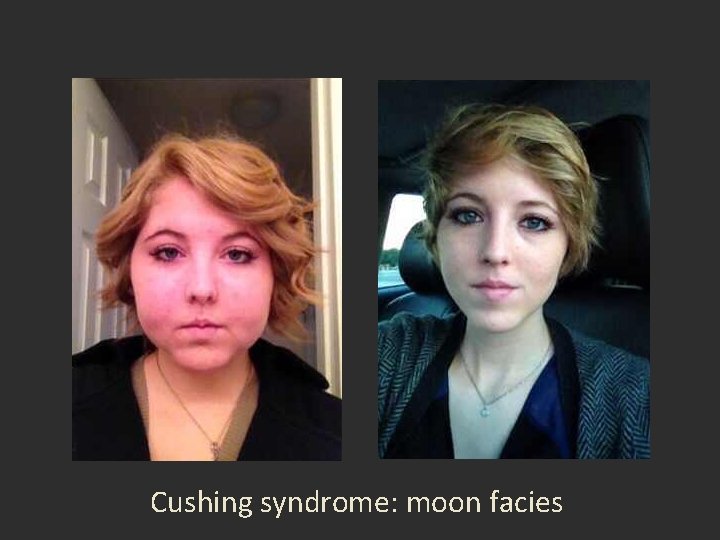
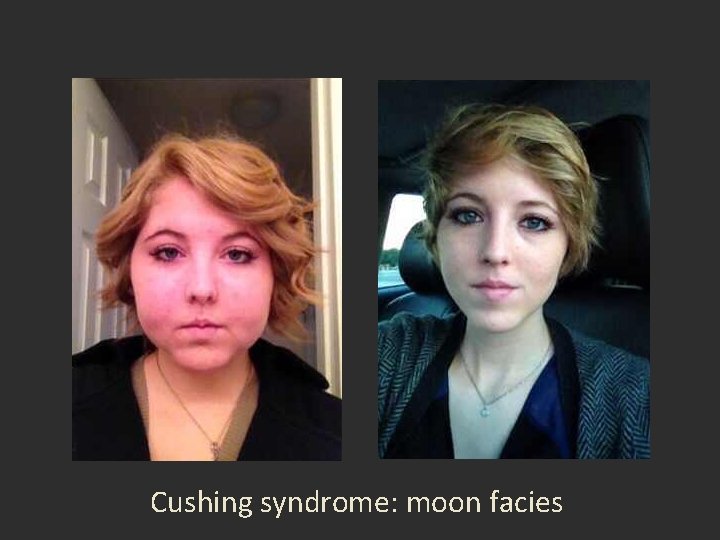
Cushing syndrome: moon facies
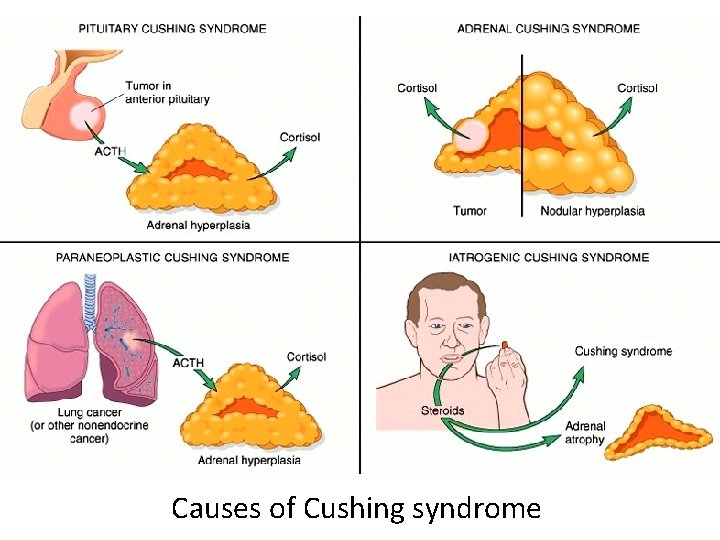
Causes of Cushing syndrome
Adrenal Path Lecture Outline • Introduction • A disease with too much hormone: Cushing syndrome • A disease with too little hormone: Addison disease
Addison Disease • Also called primary chronic adrenal insufficiency • Decreased serum cortisol and mineralocorticoids • Most common cause: autoimmune attack on adrenal cortex • Eventually fatal if not treated
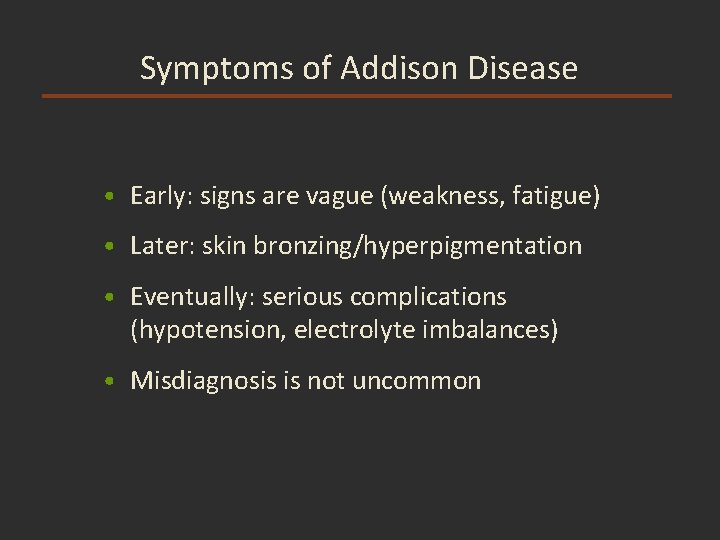
Symptoms of Addison Disease • Early: signs are vague (weakness, fatigue) • Later: skin bronzing/hyperpigmentation • Eventually: serious complications (hypotension, electrolyte imbalances) • Misdiagnosis is not uncommon
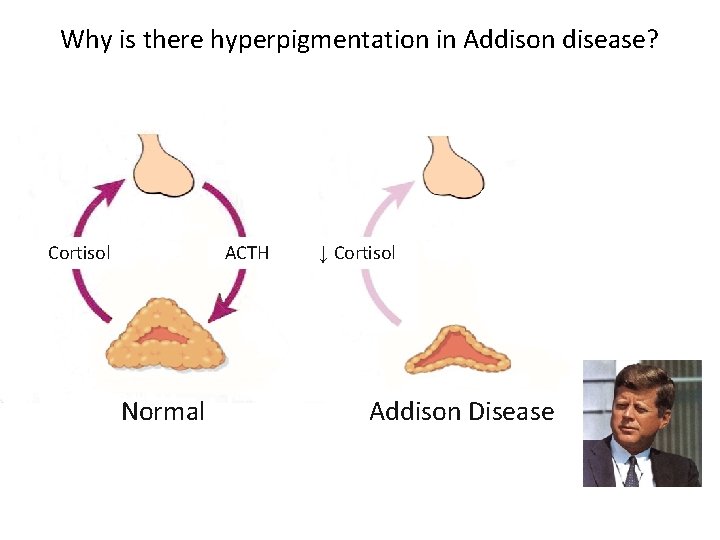
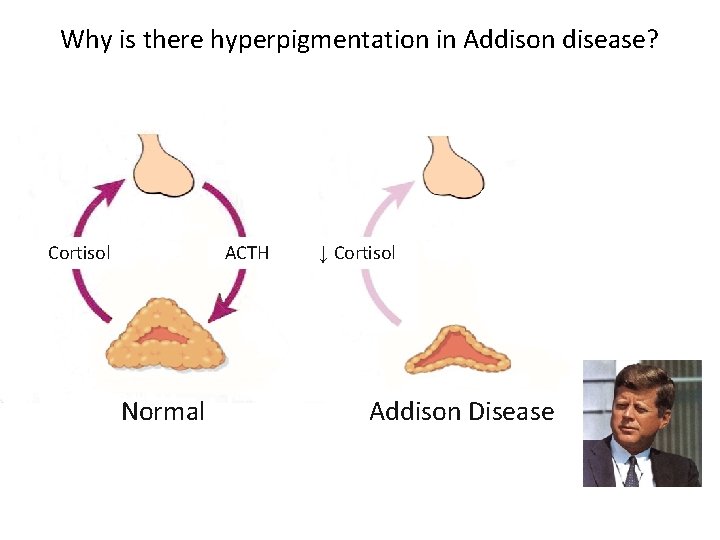
Why is there hyperpigmentation in Addison disease? Cortisol ACTH Normal ↓ Cortisol Addison Disease
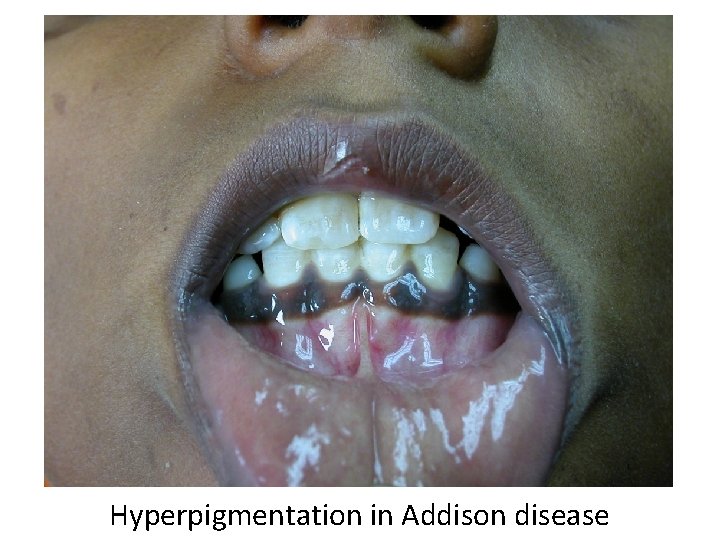
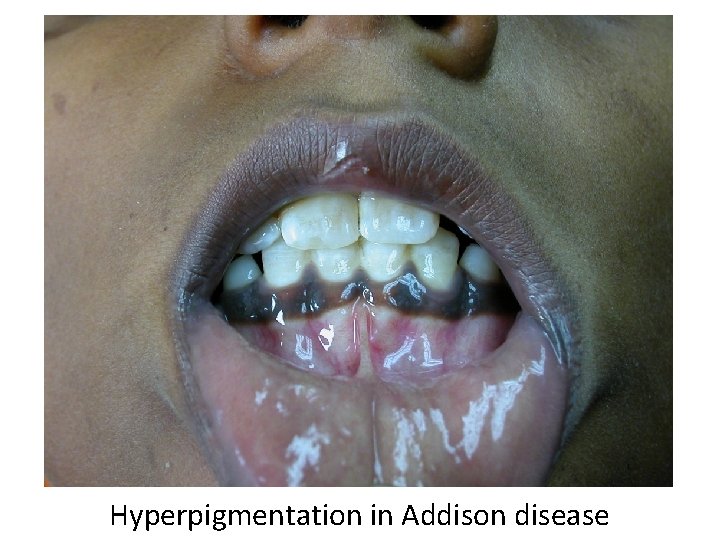
Hyperpigmentation in Addison disease
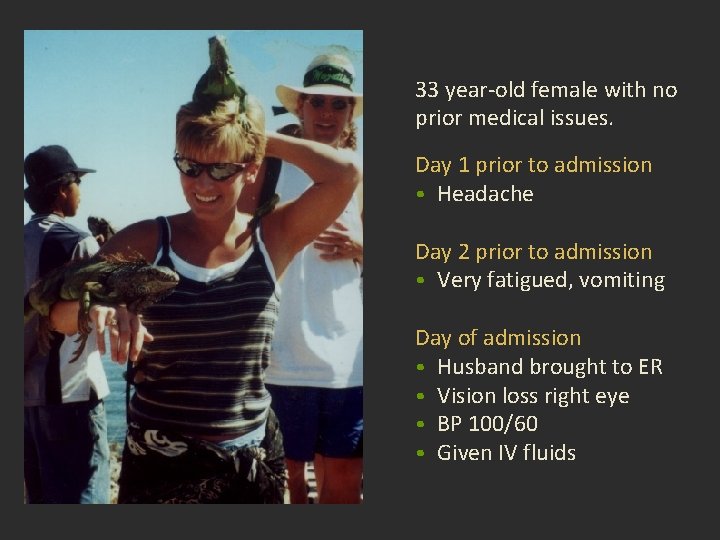
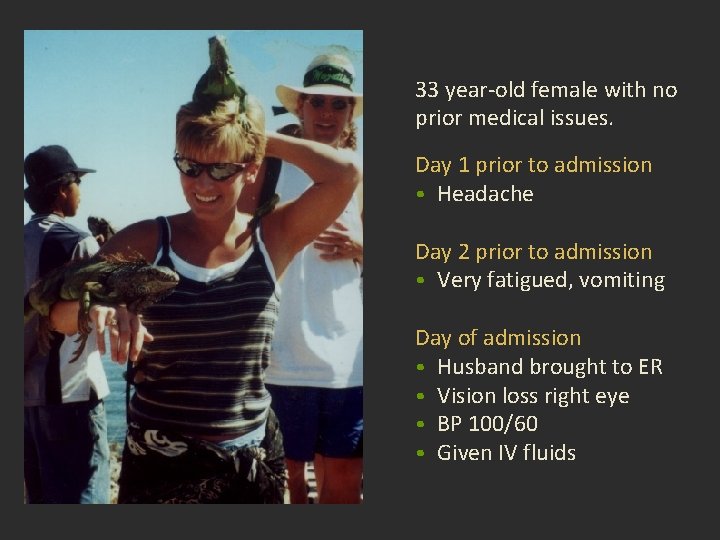
33 year-old female with no prior medical issues. Day 1 prior to admission • Headache Day 2 prior to admission • Very fatigued, vomiting Day of admission • Husband brought to ER • Vision loss right eye • BP 100/60 • Given IV fluids
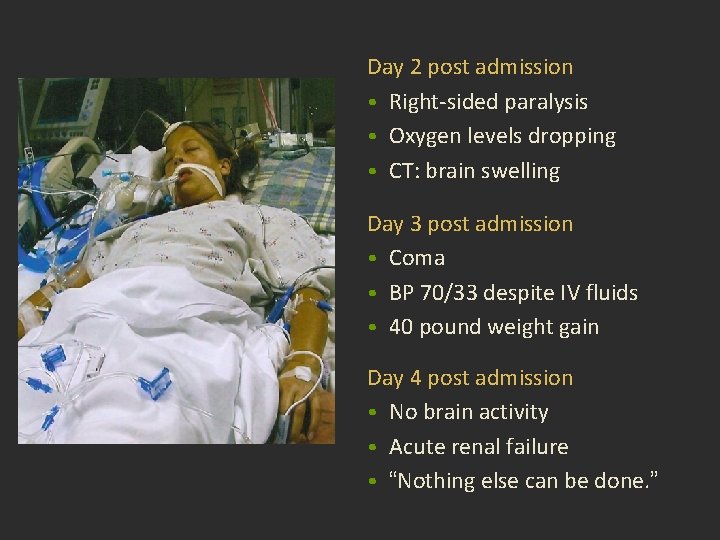
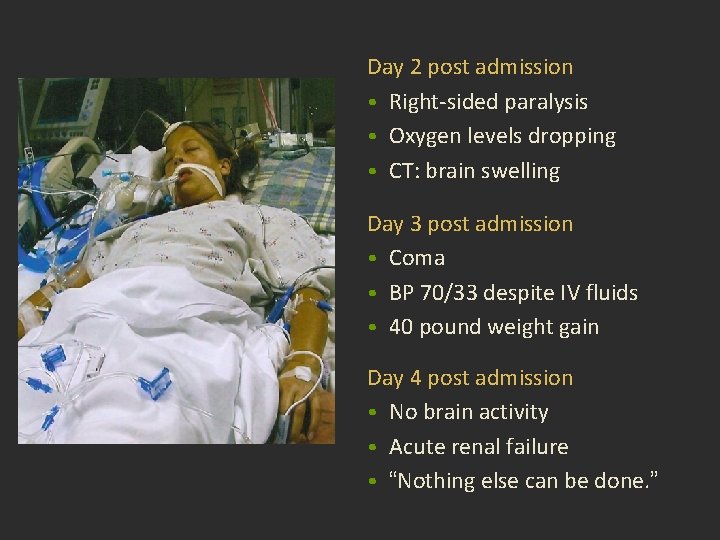
Day 2 post admission • Right-sided paralysis • Oxygen levels dropping • CT: brain swelling Day 3 post admission • Coma • BP 70/33 despite IV fluids • 40 pound weight gain Day 4 post admission • No brain activity • Acute renal failure • “Nothing else can be done. ”
Day 5 post admission • Different doctor • IV Na+, hydrocortisone, dextrose Day 6 post admission • Opened eyes Day 10 post admission • IV removed
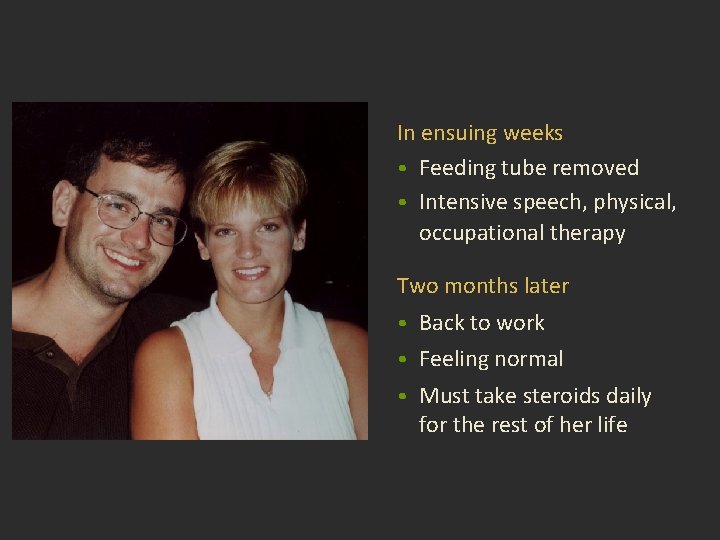
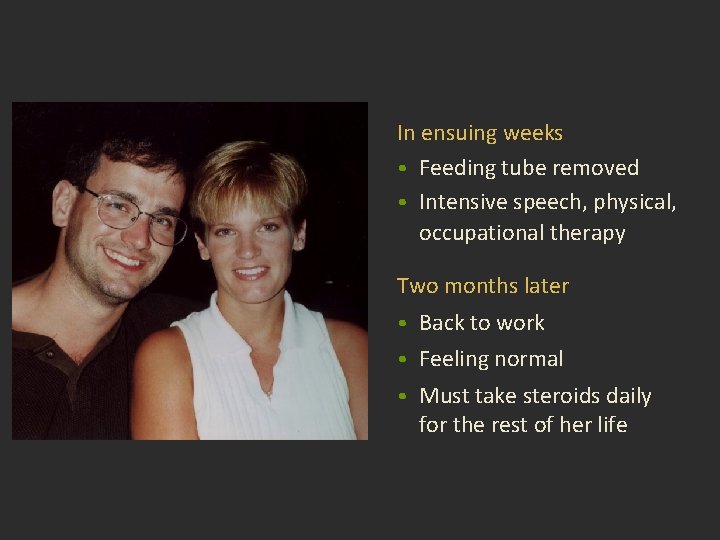
In ensuing weeks • Feeding tube removed • Intensive speech, physical, occupational therapy Two months later • Back to work • Feeling normal • Must take steroids daily for the rest of her life

Adrenal Path Lecture Outline • Introduction • A disease with too much hormone: Cushing syndrome • A disease with too little hormone: Addison disease • Tumors of the adrenal
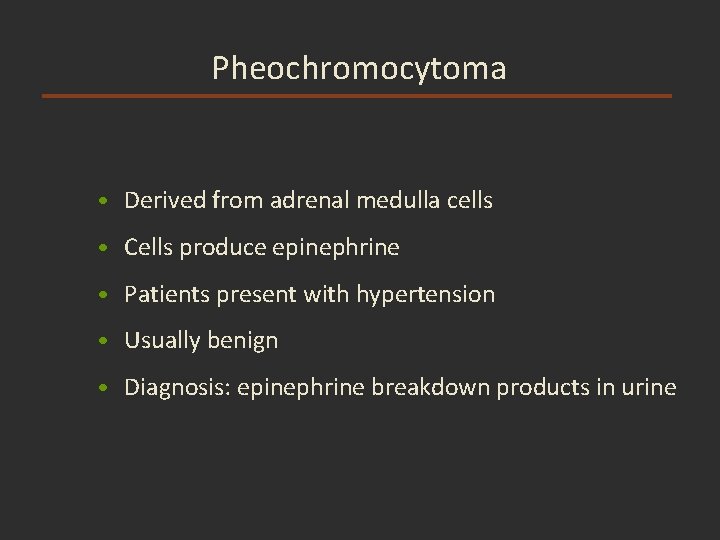
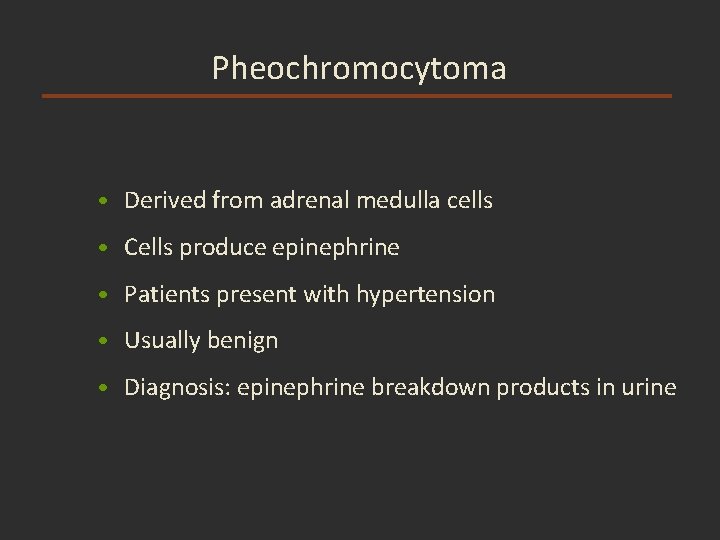
Pheochromocytoma • Derived from adrenal medulla cells • Cells produce epinephrine • Patients present with hypertension • Usually benign • Diagnosis: epinephrine breakdown products in urine
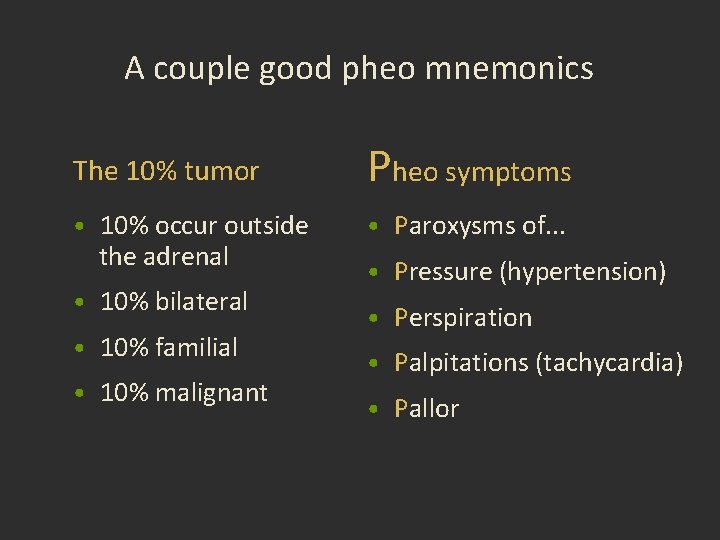
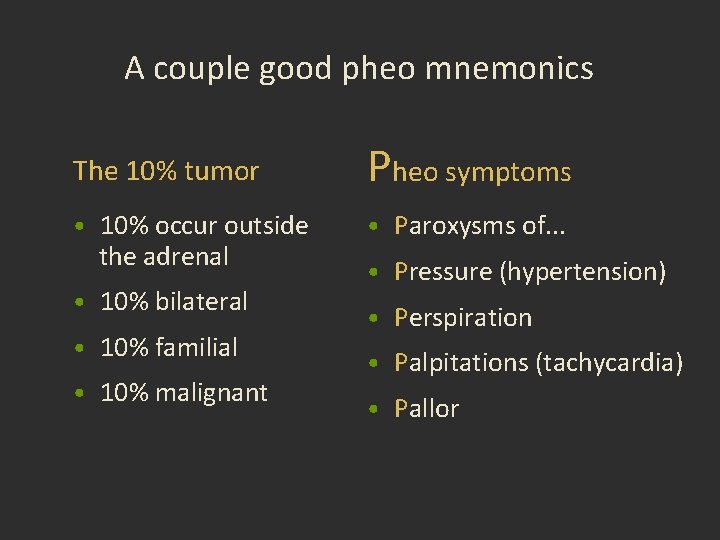
A couple good pheo mnemonics The 10% tumor Pheo symptoms • 10% occur outside • Paroxysms of. . . the adrenal • 10% bilateral • 10% familial • 10% malignant • Pressure (hypertension) • Perspiration • Palpitations (tachycardia) • Pallor
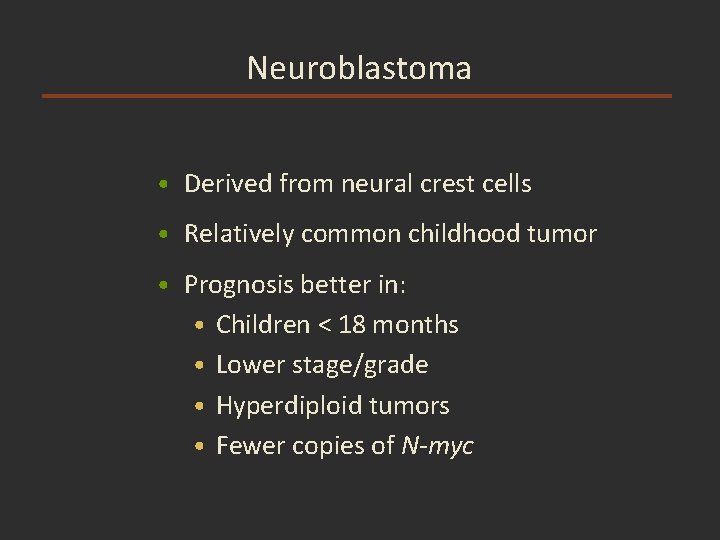
Neuroblastoma • Derived from neural crest cells • Relatively common childhood tumor • Prognosis better in: • Children < 18 months • Lower stage/grade • Hyperdiploid tumors • Fewer copies of N-myc
MEN Syndromes
Brad Pitt vs. John Cleese









No contest!
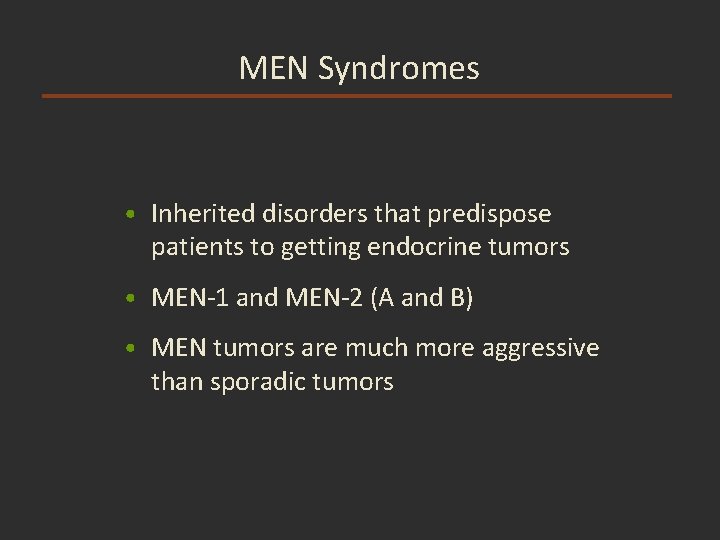
MEN Syndromes • Inherited disorders that predispose patients to getting endocrine tumors • MEN-1 and MEN-2 (A and B) • MEN tumors are much more aggressive than sporadic tumors
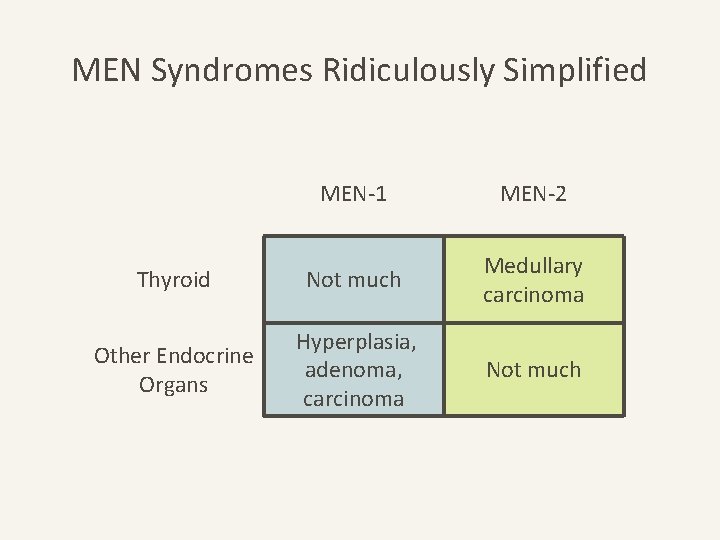
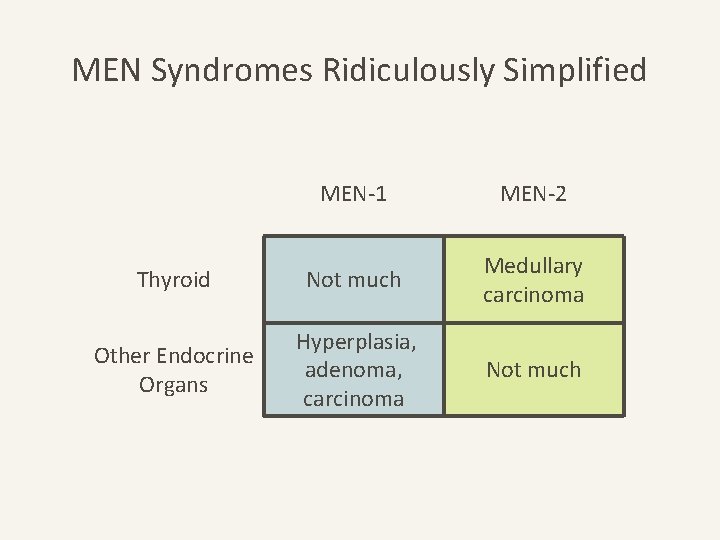
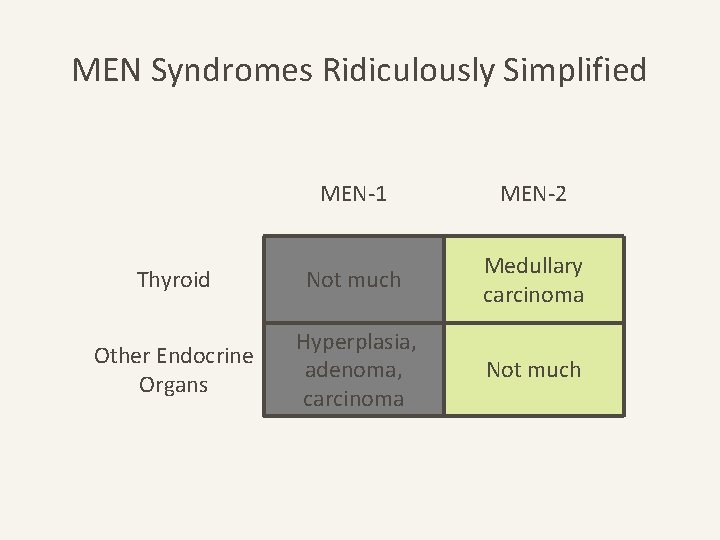
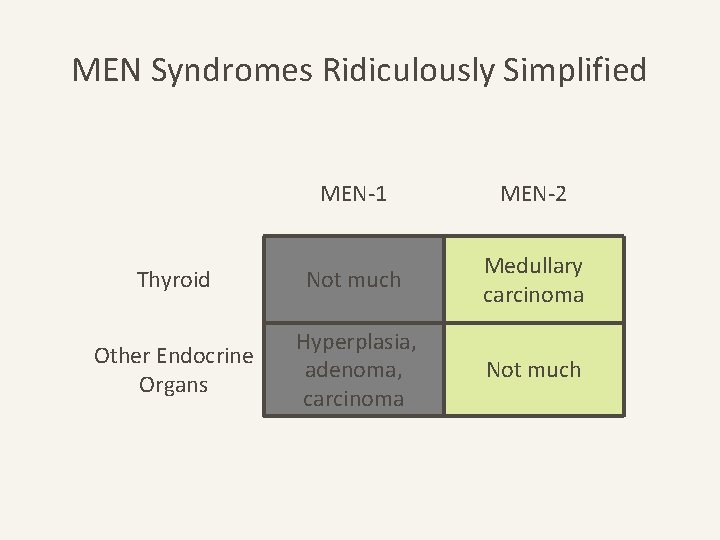
MEN Syndromes Ridiculously Simplified MEN-1 MEN-2 Thyroid Not much Medullary carcinoma Other Endocrine Organs Hyperplasia, adenoma, carcinoma Not much
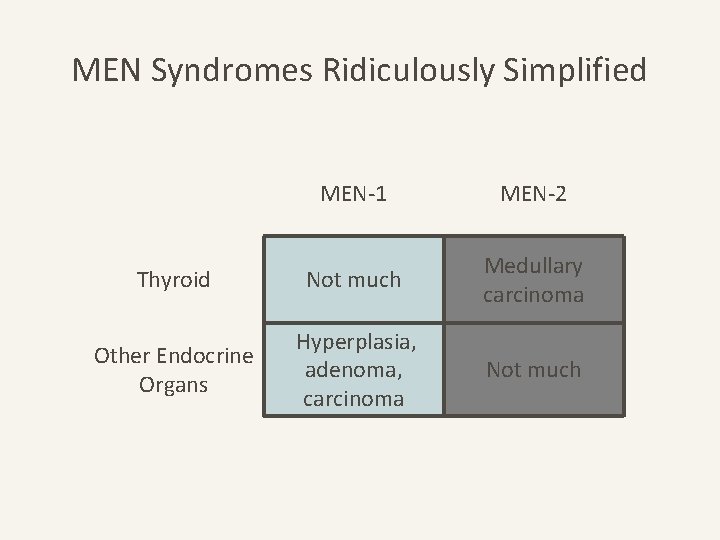
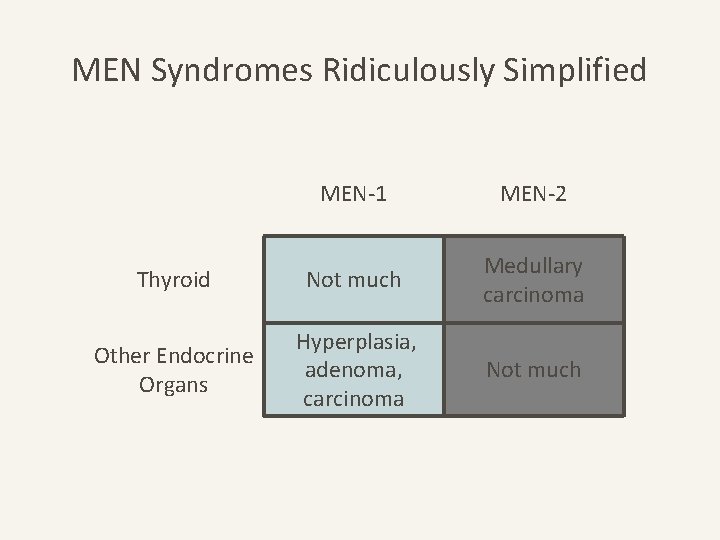
MEN Syndromes Ridiculously Simplified MEN-1 MEN-2 Thyroid Not much Medullary carcinoma Other Endocrine Organs Hyperplasia, adenoma, carcinoma Not much
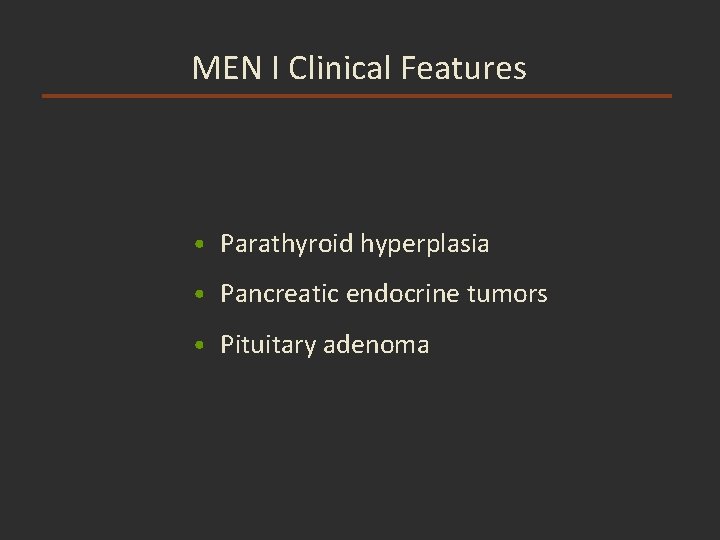
MEN I Clinical Features • Parathyroid hyperplasia • Pancreatic endocrine tumors • Pituitary adenoma
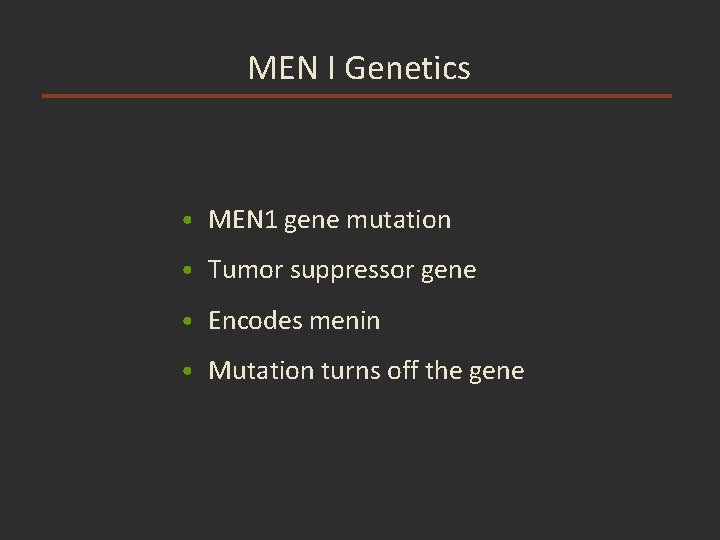
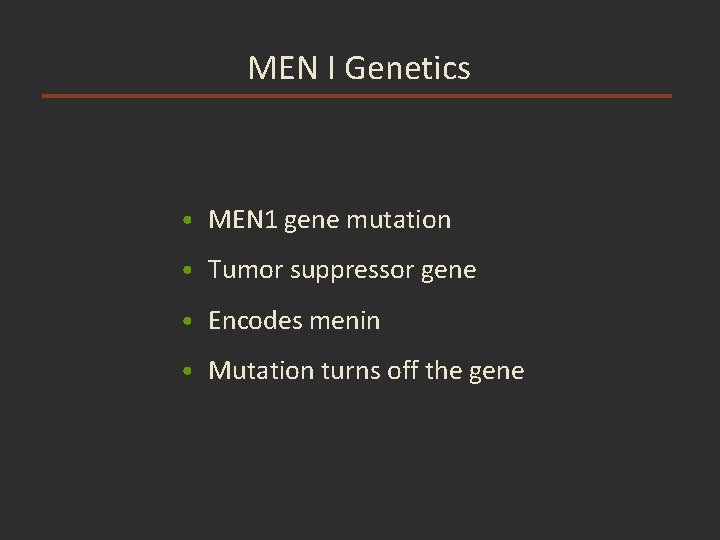
MEN I Genetics • MEN 1 gene mutation • Tumor suppressor gene • Encodes menin • Mutation turns off the gene
MEN-1 Pitt-uitary adenoma MEN 1 gene run-of-the-mill inactive turn off
MEN Syndromes Ridiculously Simplified MEN-1 MEN-2 Thyroid Not much Medullary carcinoma Other Endocrine Organs Hyperplasia, adenoma, carcinoma Not much
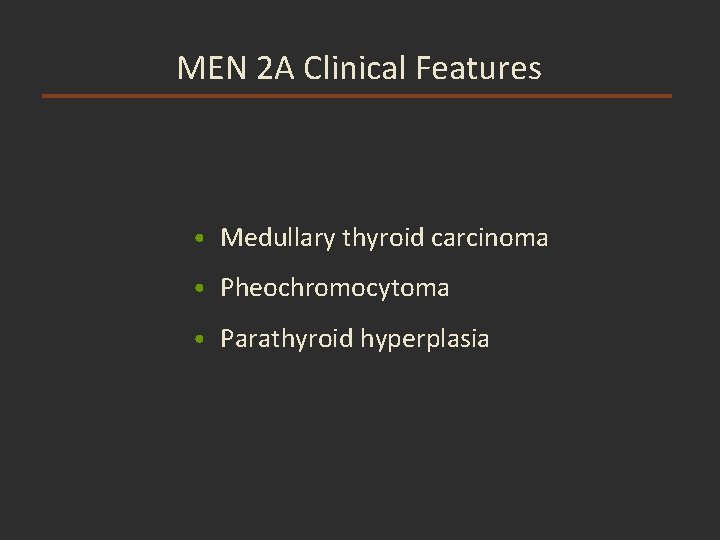
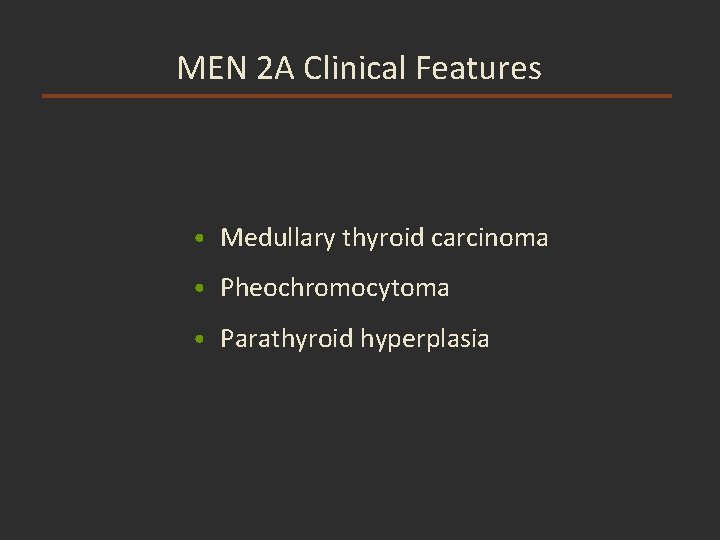
MEN 2 A Clinical Features • Medullary thyroid carcinoma • Pheochromocytoma • Parathyroid hyperplasia
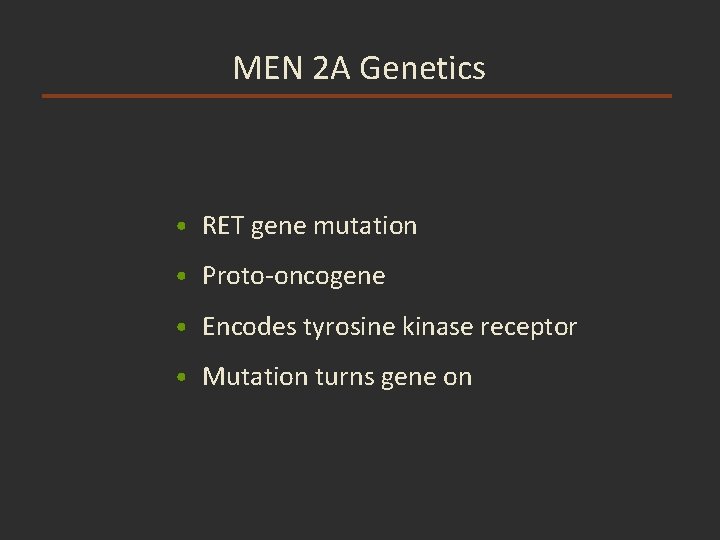
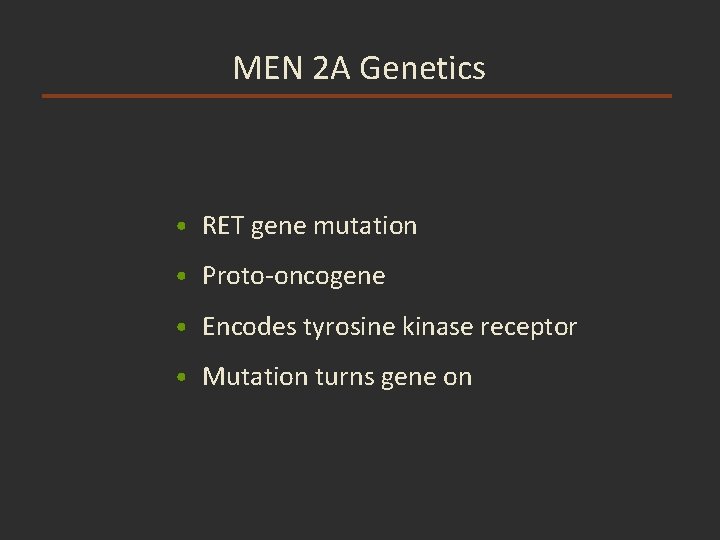
MEN 2 A Genetics • RET gene mutation • Proto-oncogene • Encodes tyrosine kinase receptor • Mutation turns gene on
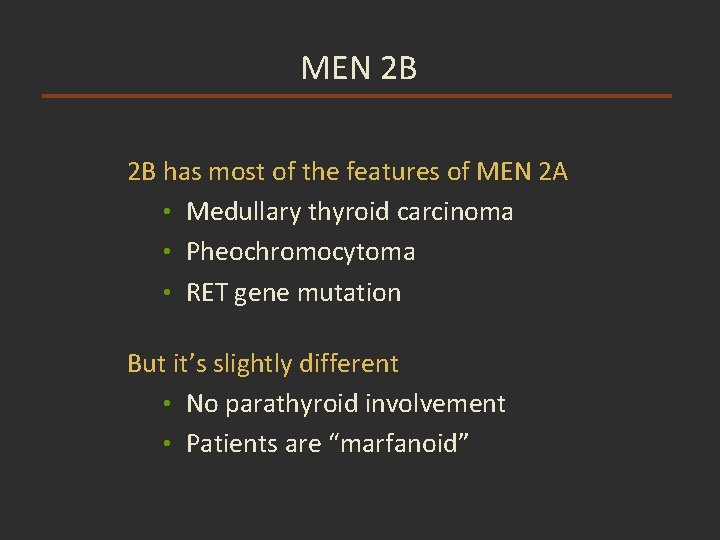
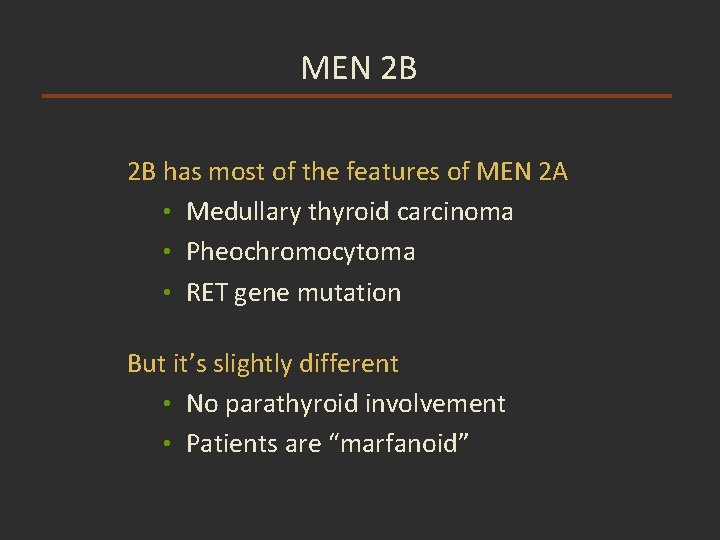
MEN 2 B 2 B has most of the features of MEN 2 A • Medullary thyroid carcinoma • Pheochromocytoma • RET gene mutation But it’s slightly different • No parathyroid involvement • Patients are “marfanoid”
MEN-2 Cleese-cell hyperplasia b. RETon gene of a kind always turned on
 Kristine krafts
Kristine krafts Real chromosome
Real chromosome Kristine krafts
Kristine krafts Art
Art Kristine krafts
Kristine krafts Kristine krafts
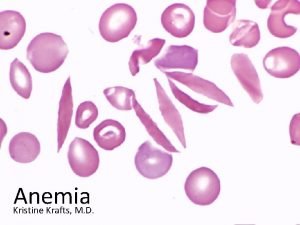
Kristine krafts Aplastic anemia
Aplastic anemia Unity signalr
Unity signalr Kristine tveit
Kristine tveit Kristīne madelāne
Kristīne madelāne Bo bendtsen
Bo bendtsen Sahar anwar
Sahar anwar Kristīne freiberga
Kristīne freiberga Kristine nagel
Kristine nagel Kristīne detkova
Kristīne detkova Dr noza
Dr noza Kristine atiyeh
Kristine atiyeh Kristine kousholt
Kristine kousholt Kristine nutt
Kristine nutt Kaitlin bonner
Kaitlin bonner Kristine hanna
Kristine hanna Kristine ruggiero
Kristine ruggiero One source multi use
One source multi use Kristine casey
Kristine casey Kristine fong
Kristine fong Kristīne bernarde
Kristīne bernarde Kristine brosjö
Kristine brosjö Kristine kopperud timberlid
Kristine kopperud timberlid Thyroiditis
Thyroiditis Aydede yüz
Aydede yüz Congenital adrenal hyperplasia characteristics
Congenital adrenal hyperplasia characteristics Visceral nervous system
Visceral nervous system Congenital adrenal hyperplasia electrolytes
Congenital adrenal hyperplasia electrolytes Adrenal gland epithelium
Adrenal gland epithelium Adrenal glands
Adrenal glands Adrenal gland
Adrenal gland Adenoma
Adenoma Cow adrenal gland
Cow adrenal gland Adrenal cortex develops from
Adrenal cortex develops from Zone of adrenal cortex
Zone of adrenal cortex Zona reticularis
Zona reticularis Neural plate formation
Neural plate formation Objectives for stress management
Objectives for stress management Adrenal sympathetic pathway
Adrenal sympathetic pathway Adrenal cushing
Adrenal cushing Dr wilson adrenal rebuilder side effects
Dr wilson adrenal rebuilder side effects