Administering Medications Chapter 35 Copyright 2011 2007 2003














- Slides: 68
Administering Medications Chapter 35 Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 1
Safety in Drug Administration Safety precautions in the management of medication administration should be consistently applied. MA must clearly understand the medication, dose, strength, and route of administration for the drug ordered by the physician. Once the order is clarified, look up the drug in the PDR. A drug should not be given until the MA knows the purpose, potential side effects, precautions, and recommended dose. Patients have the right to refuse medication. Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 2
Seven Rights of Drug Administration Right patient Right drug Right dose Right route of administration Right time Right technique Right documentation Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 3
Drug Label Checks EACH TIME a medication is dispensed, the MA MUST do the three label checks. Compare the physician’s written order with the label: 1. When removing the drug from the storage site 2. Just before dispensing the medication from the container 3. When replacing the container or before discarding it Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 4
Additional Safety Steps Dispense medications in a quiet, well-lit area. Consult the physician if there is ANY difference between the medication ordered and medication available. Store medications as directed on package. The person administering the medication is responsible for any drug errors. Physician should write every medication order before the medication is dispensed. Routinely check medication expiration dates. Discard drug containers with damaged labels. Discard medication that has been dispensed but not administered. Observe all patients for a minimum of 20 minutes after drug administration. Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 5
Patient Assessment Factors Before administering any medication the MA should assess the patient, the drug, and the environment. Use the holistic approach to patient assessment: Ø Complete an accurate patient history • Current and past use of prescription and OTC drugs • Accurate list of drug allergies Assess the patient’s ability to understand the drug regimen and afford the treatment. Record accurate age and weight. Liver or kidney disease may alter drug orders. Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 6
Patient Population Precautions with pregnant and lactating women; drugs can pass through the placenta into the fetus and into breast milk. Pediatric special precautions are necessary because of alterations in absorption, distribution, metabolism, and excretion of drugs. Ø Ø Ø Explain to the child why medication is needed. Attempt to gain the child’s cooperation. Offer choices if possible. Use diversion during stressful moments. Encourage parents to help. Offer a treat at the end of the visit. Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 7

Geriatric Precautions Aging patients are more sensitive to effects of drugs because: Ø Ø Ø Metabolic rate slows with aging causing susceptibility to accumulated effects and toxic reactions Loss of subcutaneous fat may affect parenteral routes of administration Accompanying circulatory, liver, and kidney diseases may affect distribution, metabolism, and excretion of medications Many aging patients are ordered multiple drugs, which increases the risk of drug interactions and contraindications Poor diet may affect drug therapy May not be able to afford medications Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 8
Geriatric Patient Guidelines Clearly write instructions for medication therapy. Monitor patient for swallowing difficulty. Encourage patient to drink plenty of water. Reinforce that patient take medication as ordered. Request that patient bring all medications currently taking to the office visit and keep accurate records of each. Suggest patient use the same pharmacy for all prescriptions. Suggest use of daily or weekly pill dispensers. Encourage patients not to save or share medication. Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 9
Assessment of the Patient’s Environment Allergy injections should not be given unless a physician is present. Place the patient in a correct and safe position for injections. Make sure the patient’s head is elevated before giving oral medications. Make sure emergency medications are accessible to counteract adverse reactions that might occur. Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 10
Suggested Questions for Gathering Medication Information What physician-prescribed drugs are you currently taking? Do you take any OTC drugs on a regular basis? What medications have you taken over the past 6 months to 1 year? Why? Do you regularly use any alternative or herbal products? What are they? How much do you use? How frequently? For what purpose? What time of day do you take your medicine? Are you having any side effects? Can you afford to take the medication? Are you having the desired response? Where do you store your medications? Have you checked expiration dates on your containers? Can you tell me why you are taking the prescribed medication? Do you use the same pharmacy to fill all of your prescriptions? Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 11
Drug Forms and Administration Oral medications include both solid and liquid preparations; mucous membrane medications are absorbed either rectally, vaginally, orally, nasally, or through the skin topically. Each form has specific guidelines for administration, but all require the consistent use of the three label checks and the seven rights. Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 12
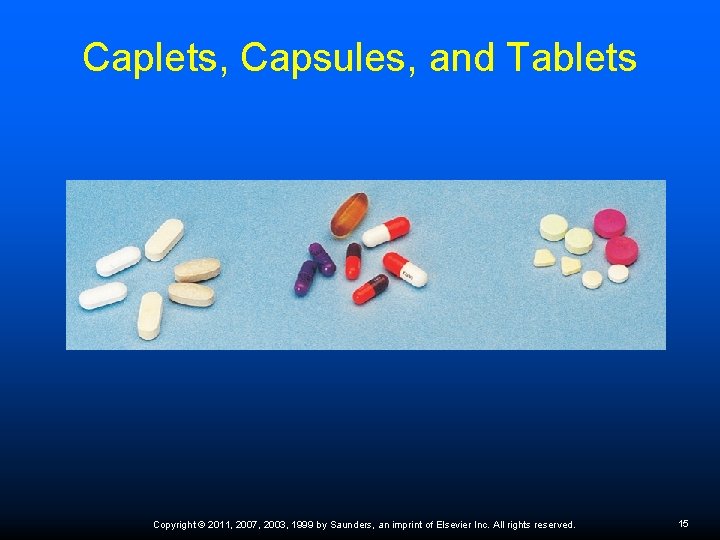
Solid Oral Dosage Forms The basic forms are tablets, capsules, and lozenges (troches). Caplets are oblong, like capsules. Capsules are gelatin coated and dissolve in the stomach, or they may be coated to protect them from the acid action of the stomach. Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 13
Caplets and Capsules Some tablets are coated with a volatile liquid that dissolves in the mouth, such as an antacid tablet. Tablets are compressed powders or granules that, when wet, break apart in the stomach, or in the mouth if they are not swallowed quickly. Ø Should not crush: • Enteric-coated tabs—coating that resists gastric secretions; protects stomach mucosa • Buffered tabs—prevent stomach irritation by combining drug with buffering agent • Timed or sustained release (SR) capsules or spansules— dissolve at different rates over a period of time Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 14
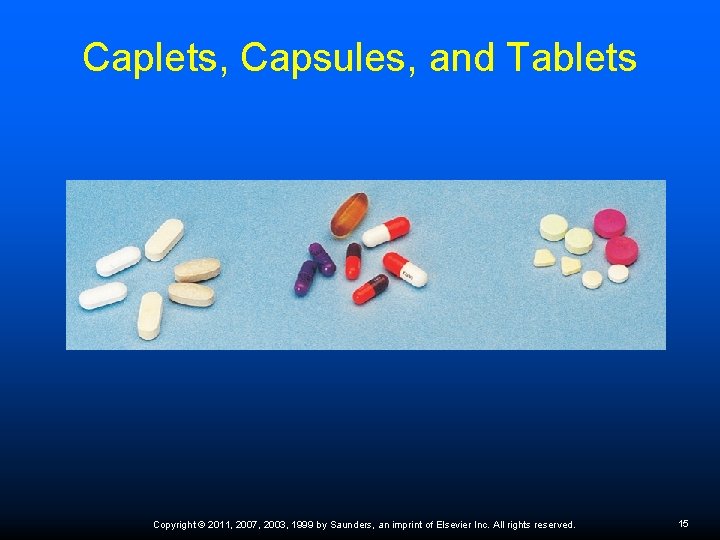
Caplets, Capsules, and Tablets Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 15
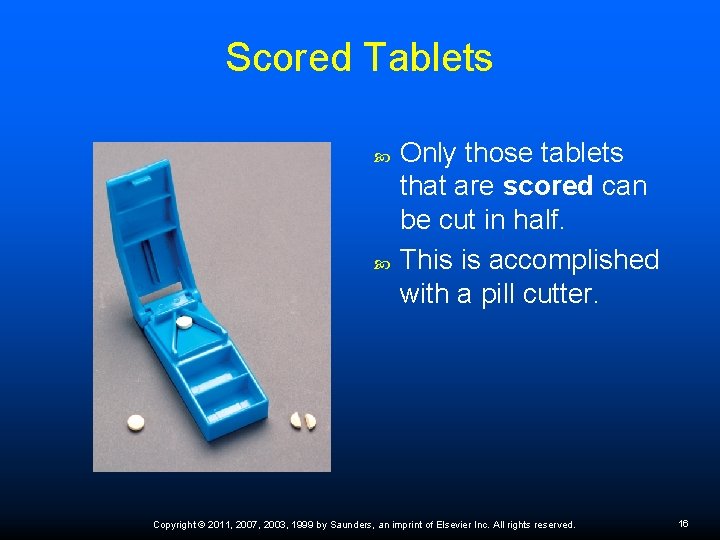
Scored Tablets Only those tablets that are scored can be cut in half. This is accomplished with a pill cutter. Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 16
Liquid Oral Dosage Forms Liquid forms differ mainly in the type of substance used to dissolve the drug: water, oils, or alcohol. Solutions are drug substances contained in a homogeneous mixture with a liquid. There are multiple forms of liquid preparations. Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 17
Liquid Medications Solutions: Mixture of liquid (usually water) and a powdered drug product; will separate if left standing so you must shake the container before administering the medication Ø Syrups: Solutions of sugar and water, usually containing flavoring and medicinal substances. Cough syrups are the most common. Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 18
Suspensions are insoluble drug substances contained in a liquid. Emulsions: Mixtures of oil and water that improve the taste of otherwise distasteful products such as cod liver oil. Ø Gels and magmas: Minerals suspended in water. Minerals settle, so products containing minerals must be shaken before use (Milk of Magnesia). Ø Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 19
Alcohol Mixes Fluid extracts: Combinations of alcohol and vegetable products that are more potent than tinctures Tinctures: Alcoholic preparation of a soluble drug or chemical substance, usually from plant sources Extracts: Concentrated combinations of vegetable products and alcohol or ether that are evaporated until a syrupy liquid, solid mass, or powder is formed; many times stronger than the crude drug Elixirs: Aromatic, alcoholic, sweetened preparation; differ from tinctures in that they are sweetened; some pediatric medications retain the name elixir, although they no longer contain alcohol Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 20

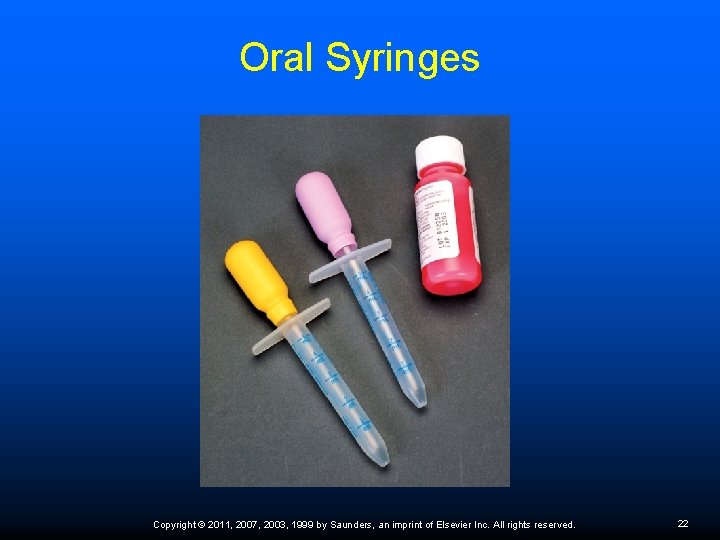
Oral Administration Taken with plenty of water unless designed to coat the mouth or throat (such as cough syrup). Make sure patient is able to swallow. Liquid medications best type of administration for children. Oral syringes can be used for pediatric administration. N/V requires alternative route of administration. Always remain with the patient until the medication is swallowed. Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 21
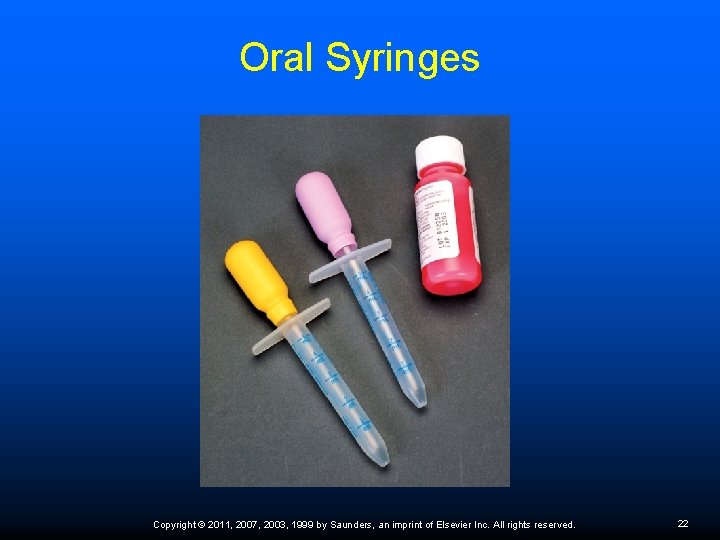
Oral Syringes Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 22
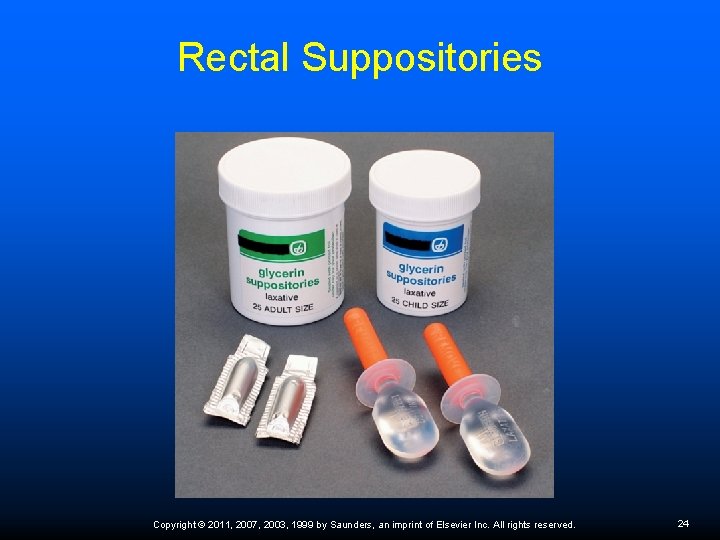
Mucous Membrane Forms Rectal administration: Rapid absorption without irritation to gastric mucosa. Ø Suppositories melt and release the medication. Ø Administer after bowel movement. Ø Patient remains lying down for 20 to 30 minutes. Ø Insert suppository 2 inches above rectal sphincter. Ø Vaginal administration: Suppositories, tabs, creams, fluid solutions. Ø Treat local infections; creams and foams for contraception. Ø Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 23
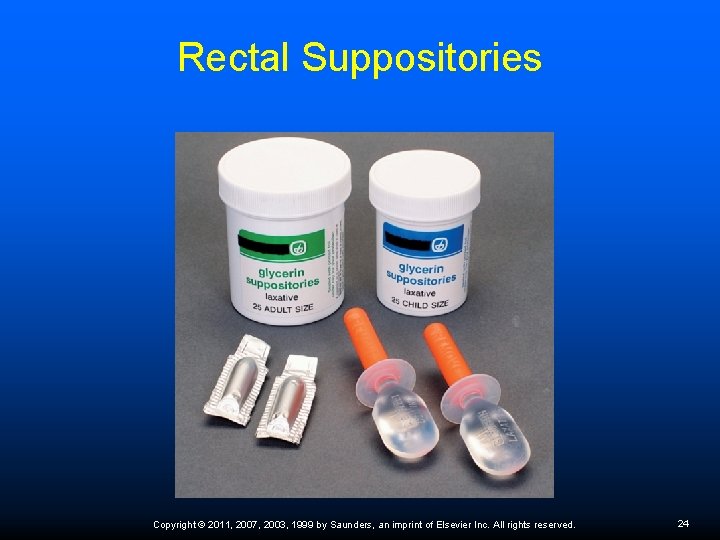
Rectal Suppositories Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 24
Mucous Membrane Forms Oral administration: Sl tabs: placed under the tongue and rapidly absorbed into the bloodstream; systemic absorption that bypasses gastric mucosa (nitroglycerin) Ø Buccal: placed between cheek and upper molars; quickly absorbed Ø Nasal administration: Nose drops and nasal sprays for localized action Ø May cause systemic reactions including tachycardia, hypertension, CNS stimulation Ø Treatment of nasal congestion, nose bleeds; instillation of medications Ø Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 25
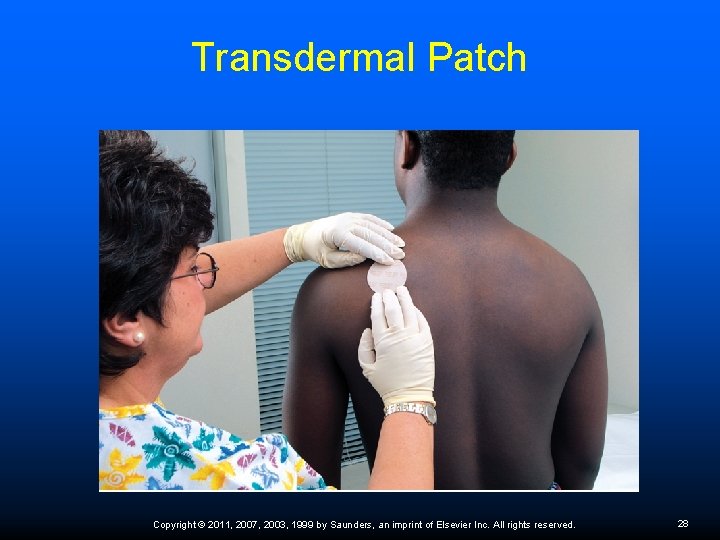
Topical Forms Lotions: relieve pruritus, treat localized infection Liniments: emulsion; protect skin Ointments (ung): have a petroleum and lanolin base Transdermal patches: absorbed slowly for a time-released systemic effect (nitro, hormone patches) Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 26
Transdermal Patch Recommendations Write application date on patch and document on patient chart. Patient may shower with patch intact. If ordered to apply every 24 hours, apply new patch at same time every day. Keep old patch on for 30 minutes after applying new one. Rotate application sites to prevent irritation. Avoid areas with scars or large amount of body hair. Use caution when disposing of used patch. Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 27
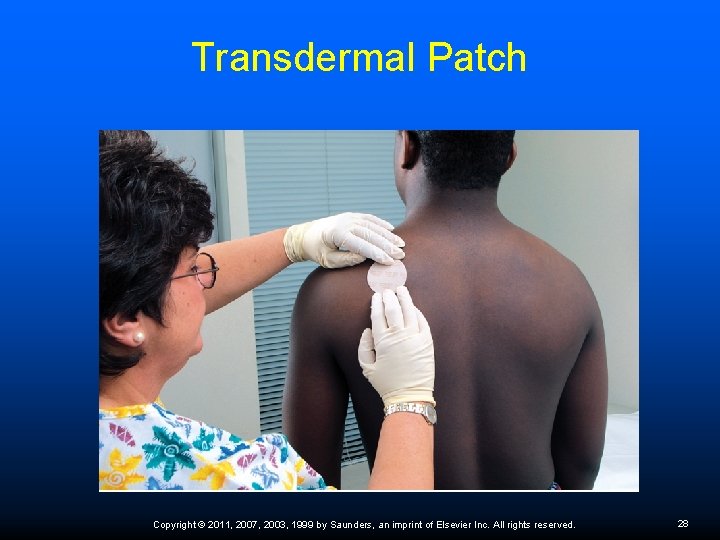
Transdermal Patch Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 28
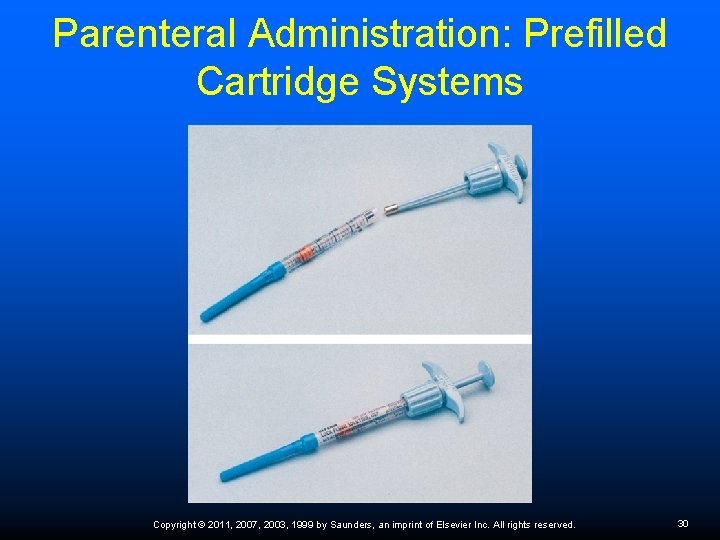
Parenteral Administration Parenteral medications must be sterile and in liquid form. Are manufactured in ampules, single-dose or multidose vials, prefilled syringes, or cartridge systems. Before dispensing, check expiration date and examine solution for possible deterioration. Drug characteristics and individual patient factors determine the correct gauge and length of the needle needed. Must use Standard Precautions when disposing of needles and wear gloves when administering. Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 29
Parenteral Administration: Prefilled Cartridge Systems Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 30

Needle Parts Bevel—angled tip of a needle Gauge—diameter or lumen size of a needle The larger the gauge number, the smaller the diameter of the needle Smallest gauges are 27 to 28 for ID injections Ø Gauges 25 to 26 for SC injections Ø Gauges 20 to 23 for IM—viscous drugs and deeper injections Ø Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 31
Needle Length depends on two factors Area of body for injection Ø Depth of administration (SC versus IM) Ø Lengths vary from 3/8 inch to 4 inches ID: 3/8 inch; bevel only part of needle injected Ø SC: 1/2 to 5/8 inch Ø IM: 1 to 3 inches; length depends on the muscle being used and patient size Ø Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 32
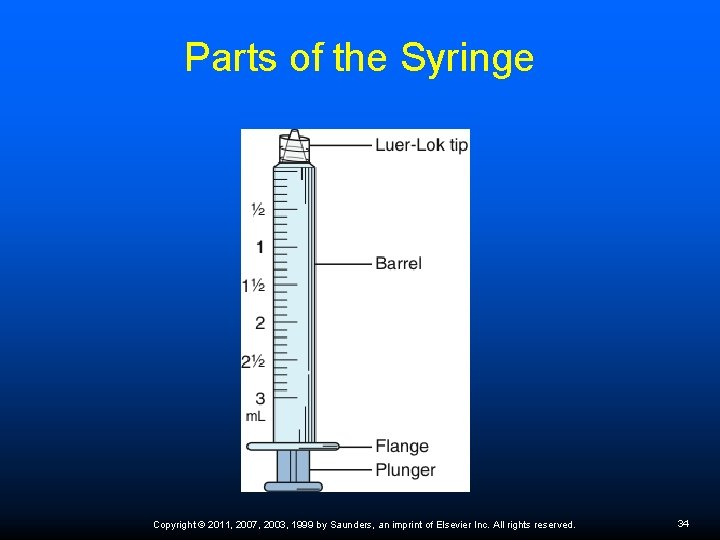
Syringes Parts of syringe—barrel, calibrated scale, plunger, tip 3 -cc syringe—calibrated with cc and minims Tuberculin syringe—holds 1 ml Insulin syringe—calibrated in units, 50 U or 100 U The appropriate syringe is determined by the type of medication and the amount of drug. Specialty syringe units, such as the Nova Pen and the Epi. Pen, are designed for quick administration of certain medications in public or in an emergency. Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 33
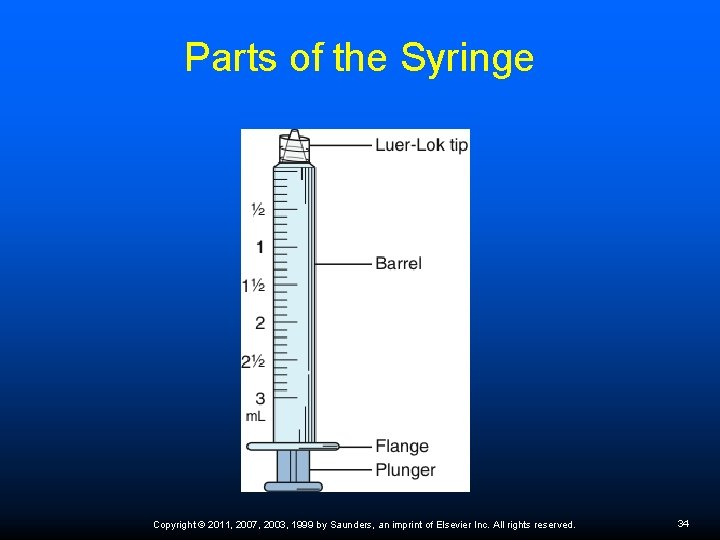
Parts of the Syringe Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 34

Retractable Needle Cover Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 35
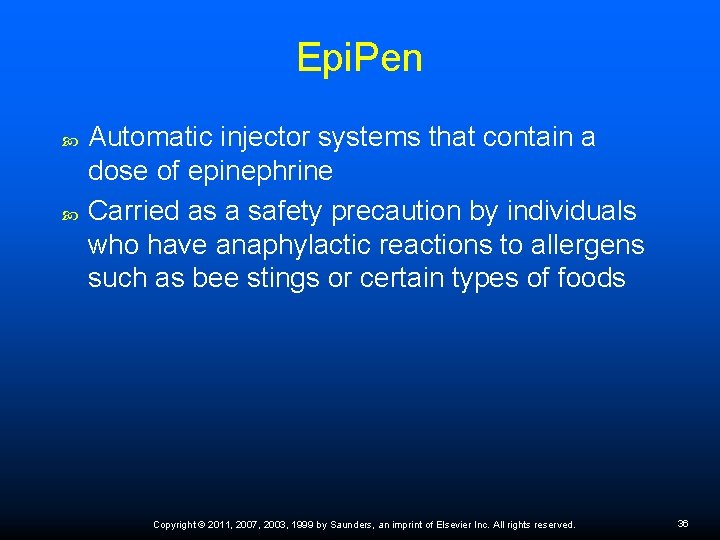
Epi. Pen Automatic injector systems that contain a dose of epinephrine Carried as a safety precaution by individuals who have anaphylactic reactions to allergens such as bee stings or certain types of foods Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 36

Anaphylactic Signs and Symptoms Hypotension resulting from systemic vasodilation Urticaria Dyspnea caused by bronchoconstriction Vomiting and diarrhea Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 37

Epi. Pen Injection Epi. Pen can be injected through clothing. Firmly press tip of injector on outer aspect of thigh and hold in place for 10 seconds. Remove Epi. Pen and massage to promote absorption. Notify physician or go to ER for follow up. Periodically check unit expiration date. Store in a readily available location. Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 38
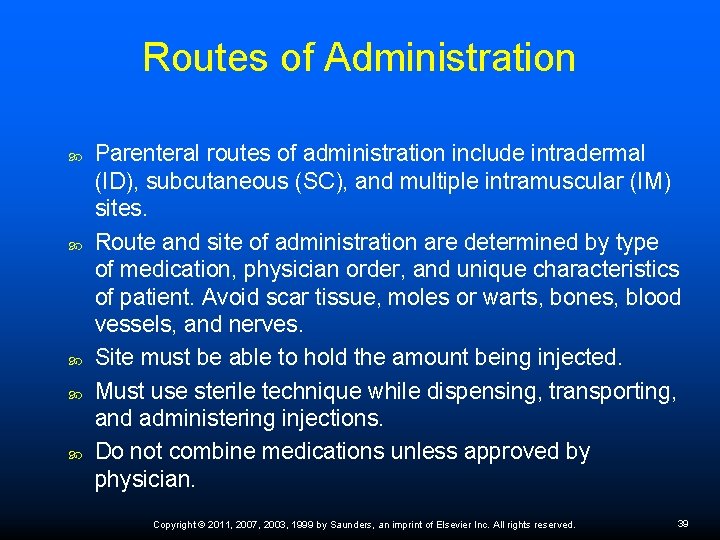
Routes of Administration Parenteral routes of administration include intradermal (ID), subcutaneous (SC), and multiple intramuscular (IM) sites. Route and site of administration are determined by type of medication, physician order, and unique characteristics of patient. Avoid scar tissue, moles or warts, bones, blood vessels, and nerves. Site must be able to hold the amount being injected. Must use sterile technique while dispensing, transporting, and administering injections. Do not combine medications unless approved by physician. Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 39
Parenteral Guidelines OSHA guidelines include using syringe units with retractable needle covers and wearing disposable nonsterile gloves. Never recap a contaminated needle, and immediately discard it into a sharps container. Dispose of contaminated nonsharp materials in biohazard containers. Disinfect contaminated work areas. Sanitize hands before and after procedures. Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 40
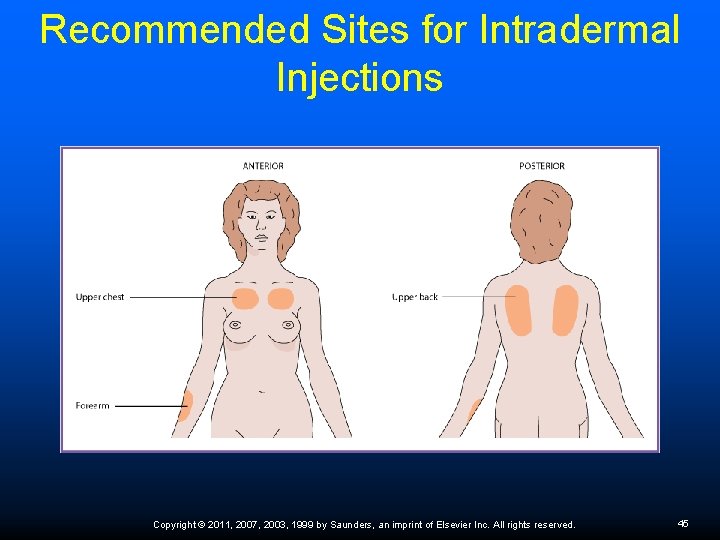
Intradermal Injections Drug administered within the skin layers just under the epidermis. Many nerves present, so injection causes burning and stinging. Inject minute amount of solution. Insert only the bevel point of the needle. Proper administration causes a wheal to rise at the injection site. Used for allergy testing and tuberculin screening. Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 41
Tuberculosis Screening Mantoux test Injects 0. 1 ml of PPD in center of anterior forearm. Ø Angle of injection 15 degrees, almost parallel to skin surface. Ø Monitor site 48 to 72 hours later for induration. Ø Patient must return to have the test read. Ø Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 42

Positive TB Skin Test Induration of 5 mm or greater – HIV+ patients; anyone in close contact with a newly diagnosed patient; and patients who have undergone recent organ transplants or are taking immunosuppressant medications. Induration of 10 mm or greater – recent immigrants from countries in which TB is prevalent; IV drug users; residents and employees of correctional institutions, homeless shelters, and healthcare facilities; and children under 4 years of age. Regardless of risk factors, anyone with an induration of 15 mm or greater in diameter is considered positive. Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 43

Intradermal Injection The intradermal injection is administered just under the epidermis. Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 44
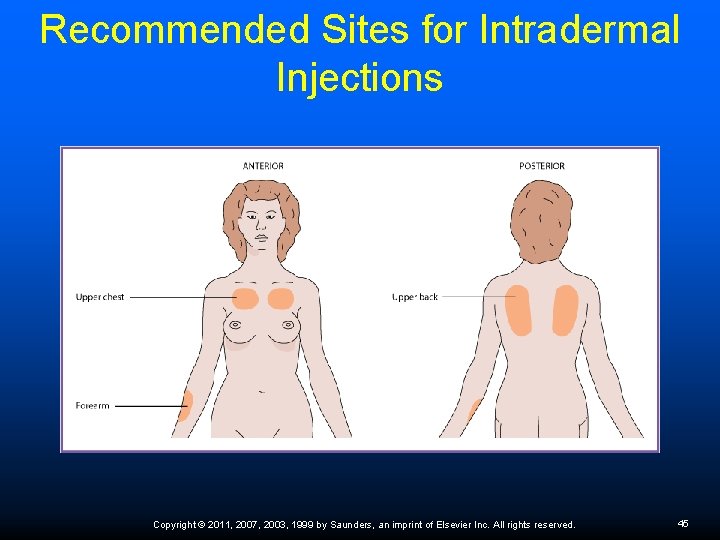
Recommended Sites for Intradermal Injections Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 45
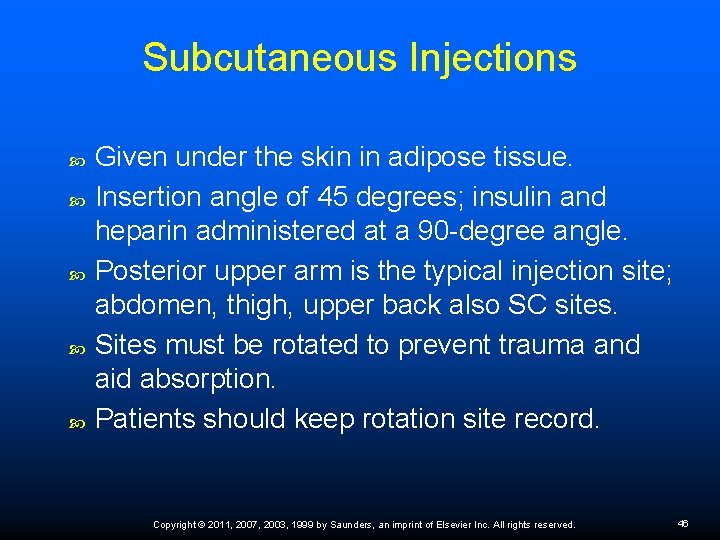
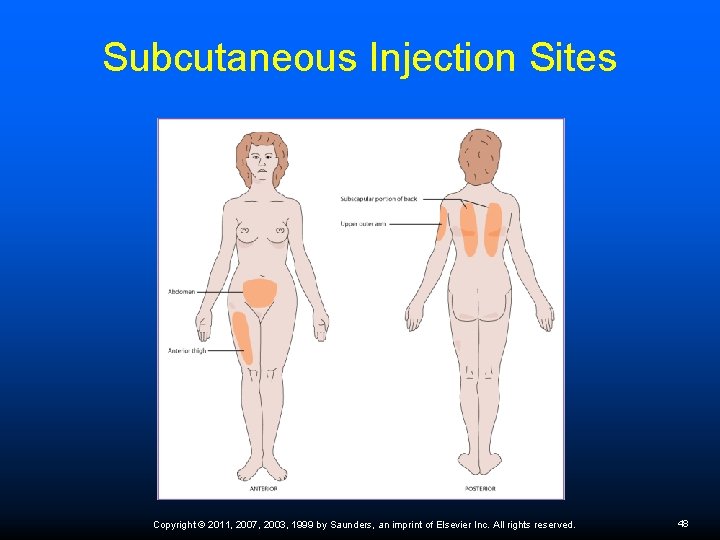
Subcutaneous Injections Given under the skin in adipose tissue. Insertion angle of 45 degrees; insulin and heparin administered at a 90 -degree angle. Posterior upper arm is the typical injection site; abdomen, thigh, upper back also SC sites. Sites must be rotated to prevent trauma and aid absorption. Patients should keep rotation site record. Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 46

Subcutaneous Injection Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 47
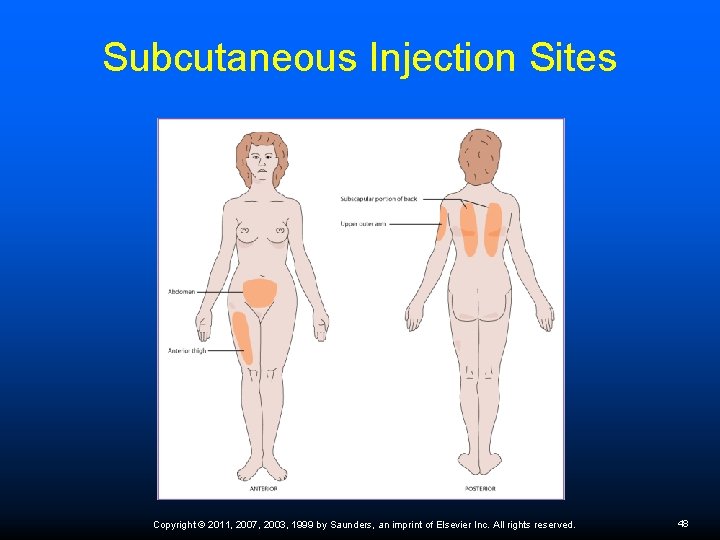
Subcutaneous Injection Sites Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 48
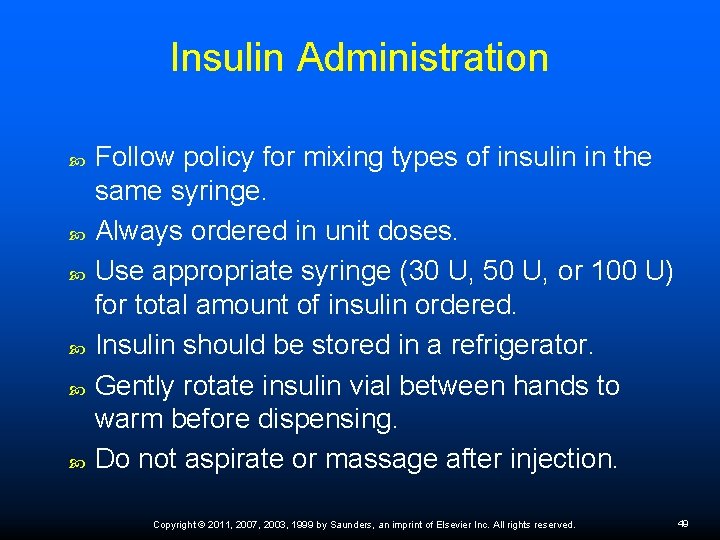
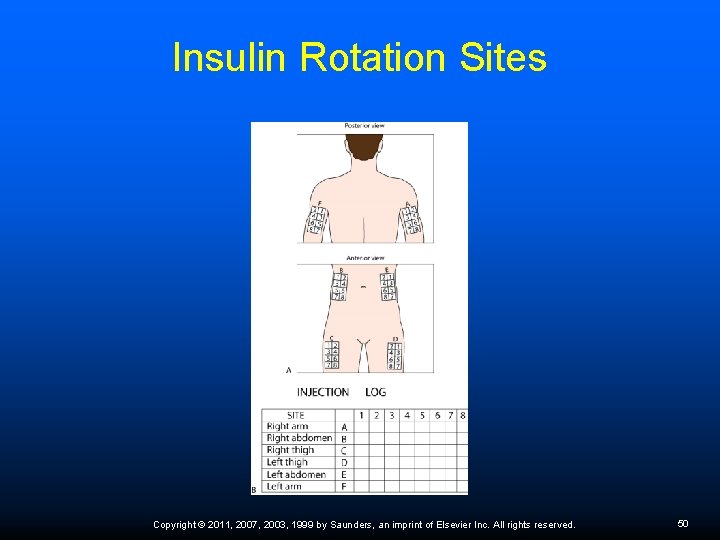
Insulin Administration Follow policy for mixing types of insulin in the same syringe. Always ordered in unit doses. Use appropriate syringe (30 U, 50 U, or 100 U) for total amount of insulin ordered. Insulin should be stored in a refrigerator. Gently rotate insulin vial between hands to warm before dispensing. Do not aspirate or massage after injection. Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 49
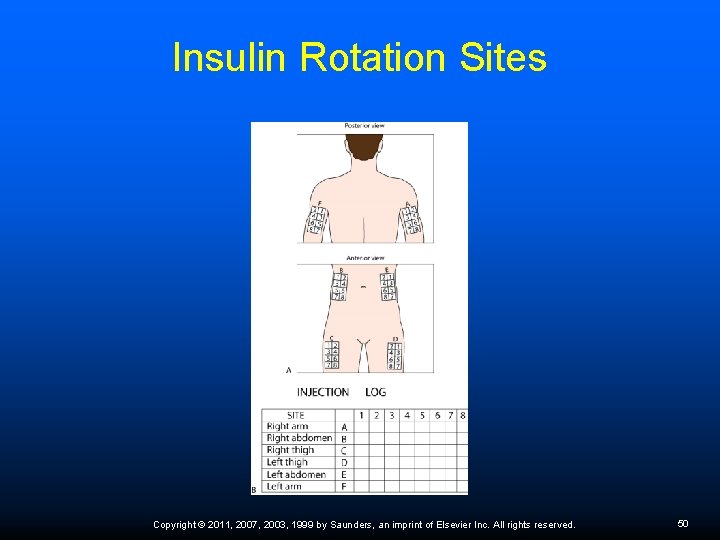
Insulin Rotation Sites Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 50
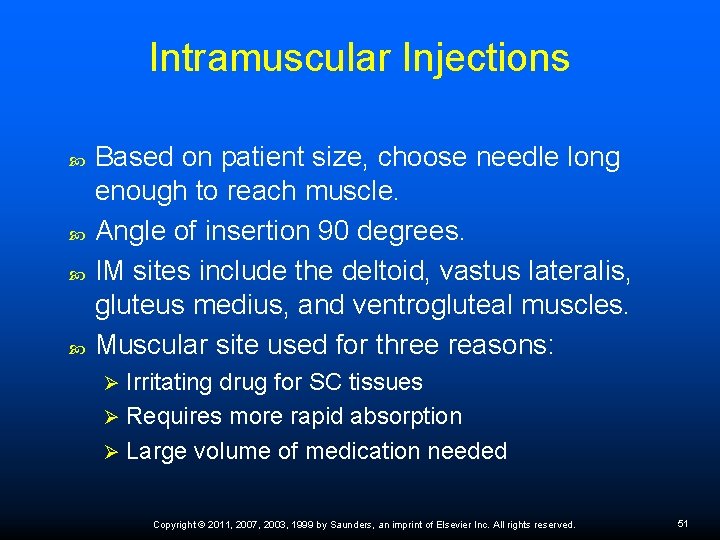
Intramuscular Injections Based on patient size, choose needle long enough to reach muscle. Angle of insertion 90 degrees. IM sites include the deltoid, vastus lateralis, gluteus medius, and ventrogluteal muscles. Muscular site used for three reasons: Irritating drug for SC tissues Ø Requires more rapid absorption Ø Large volume of medication needed Ø Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 51

Intramuscular Injection Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 52
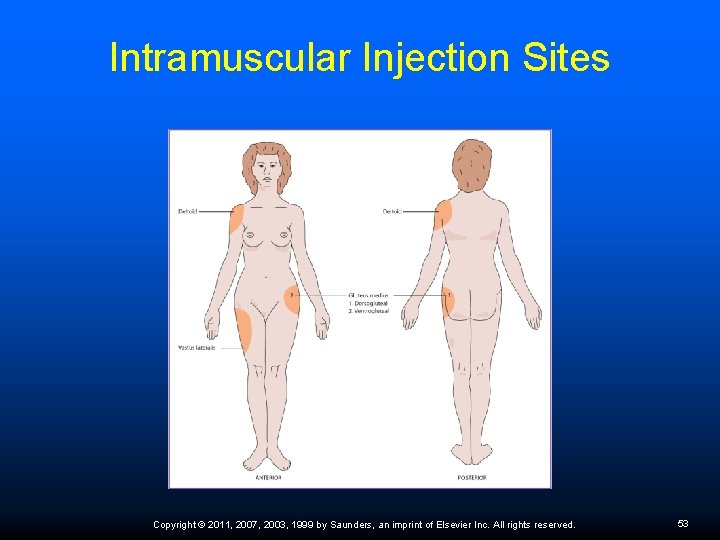
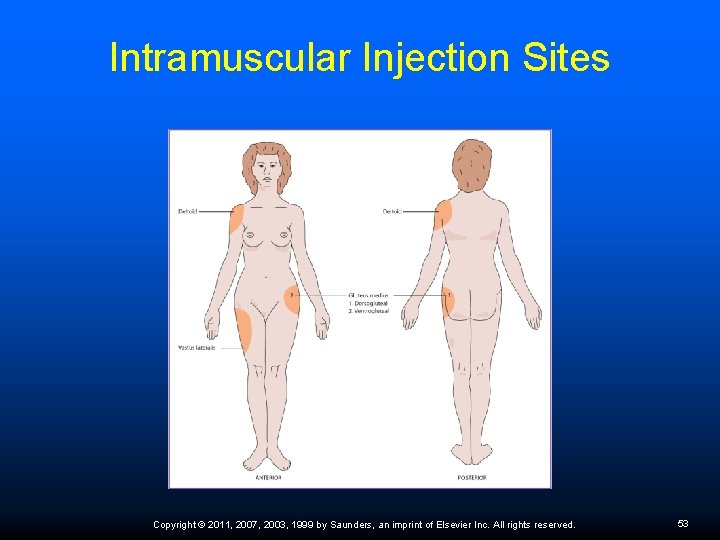
Intramuscular Injection Sites Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 53
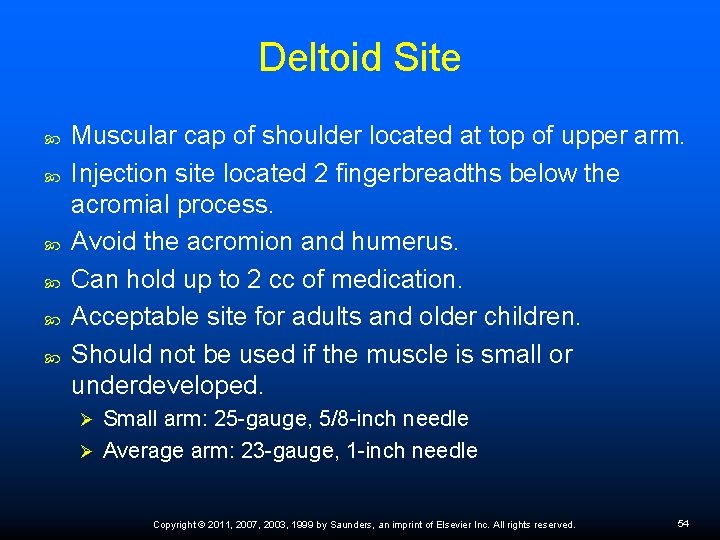
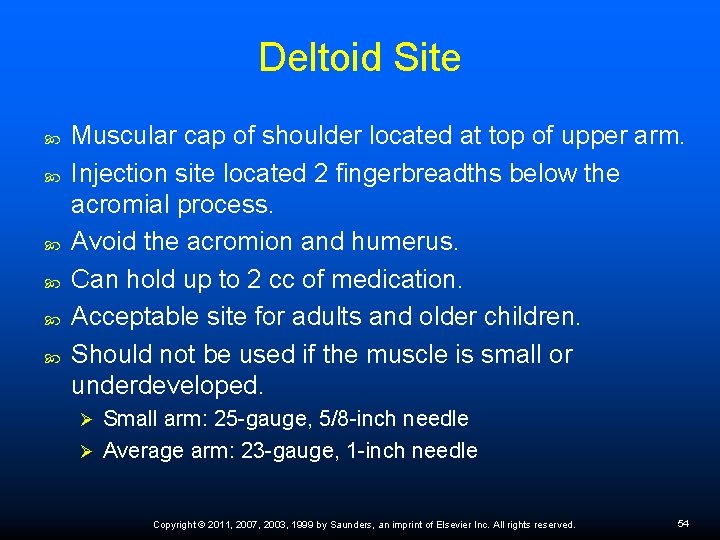
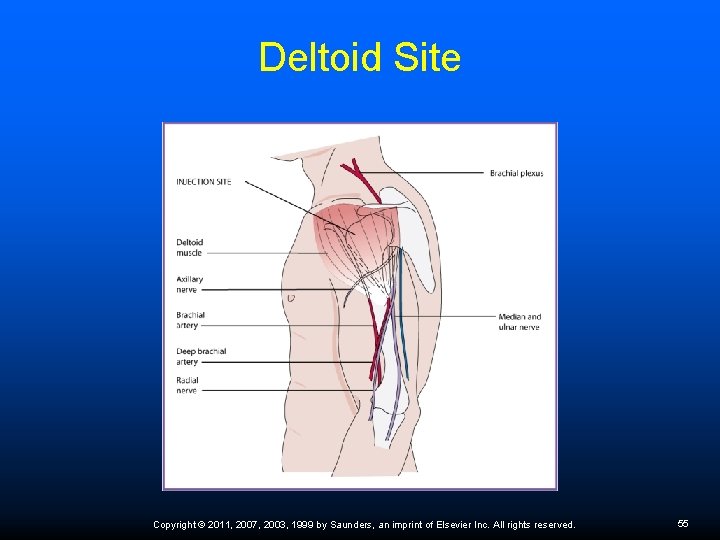
Deltoid Site Muscular cap of shoulder located at top of upper arm. Injection site located 2 fingerbreadths below the acromial process. Avoid the acromion and humerus. Can hold up to 2 cc of medication. Acceptable site for adults and older children. Should not be used if the muscle is small or underdeveloped. Small arm: 25 -gauge, 5/8 -inch needle Ø Average arm: 23 -gauge, 1 -inch needle Ø Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 54
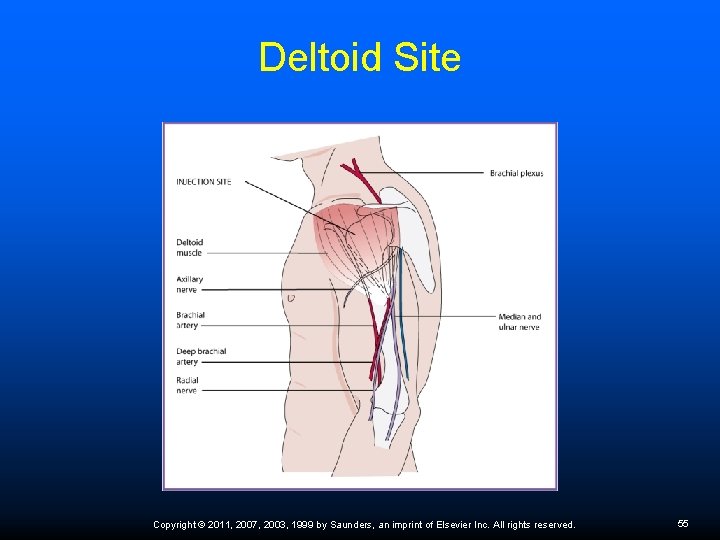
Deltoid Site Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 55
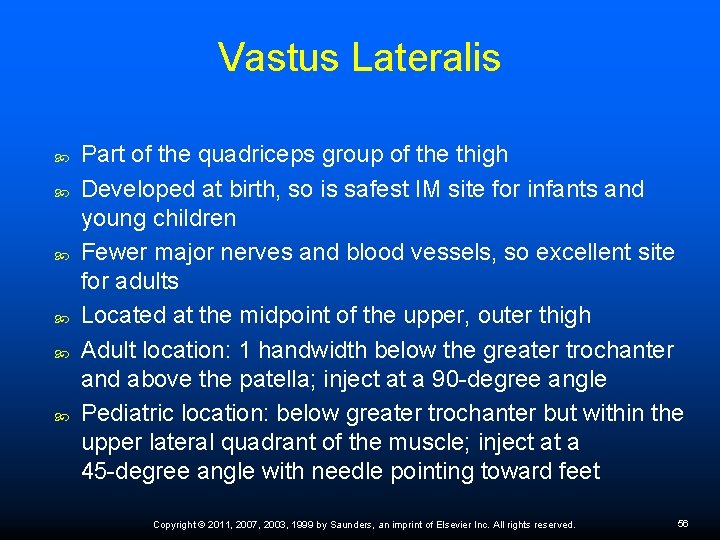
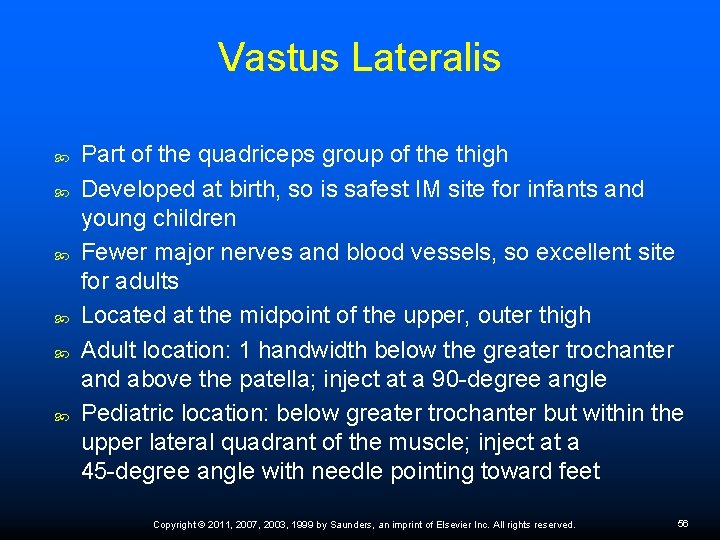
Vastus Lateralis Part of the quadriceps group of the thigh Developed at birth, so is safest IM site for infants and young children Fewer major nerves and blood vessels, so excellent site for adults Located at the midpoint of the upper, outer thigh Adult location: 1 handwidth below the greater trochanter and above the patella; inject at a 90 -degree angle Pediatric location: below greater trochanter but within the upper lateral quadrant of the muscle; inject at a 45 -degree angle with needle pointing toward feet Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 56
Dorsogluteal Site Traditional site for deep IM injections in adults High risk of sciatic nerve damage Must take great care in locating the exact site Patient should be in Sims’ position Ø Palm on greater trochanter of femur with finger pointed toward posterior iliac spine Ø Inject into the gluteus medius muscle above the imaginary line drawn between the two anatomic markings Ø Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 57

Dorsogluteal Site Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 58
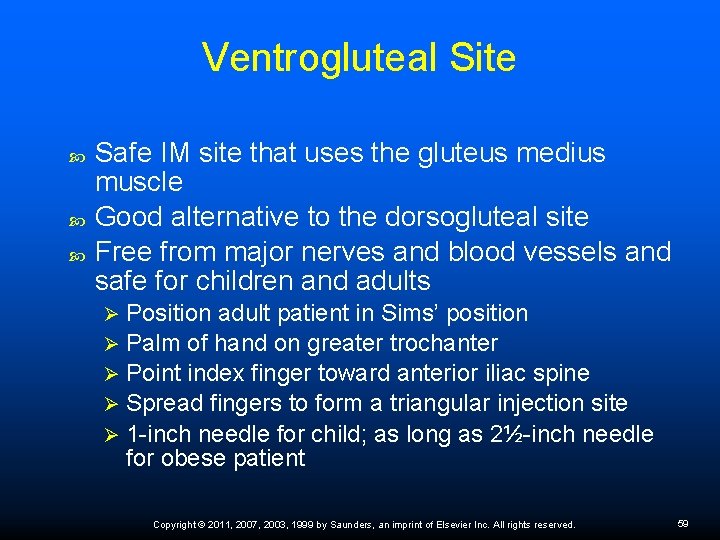
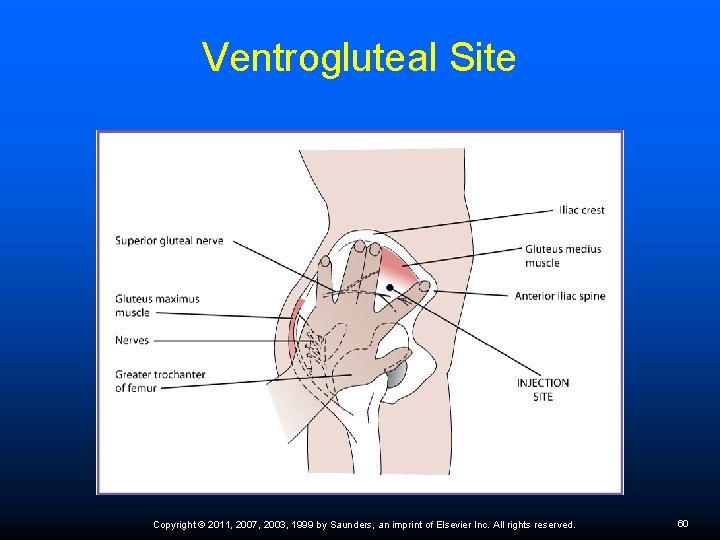
Ventrogluteal Site Safe IM site that uses the gluteus medius muscle Good alternative to the dorsogluteal site Free from major nerves and blood vessels and safe for children and adults Position adult patient in Sims’ position Ø Palm of hand on greater trochanter Ø Point index finger toward anterior iliac spine Ø Spread fingers to form a triangular injection site Ø 1 -inch needle for child; as long as 2½-inch needle for obese patient Ø Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 59
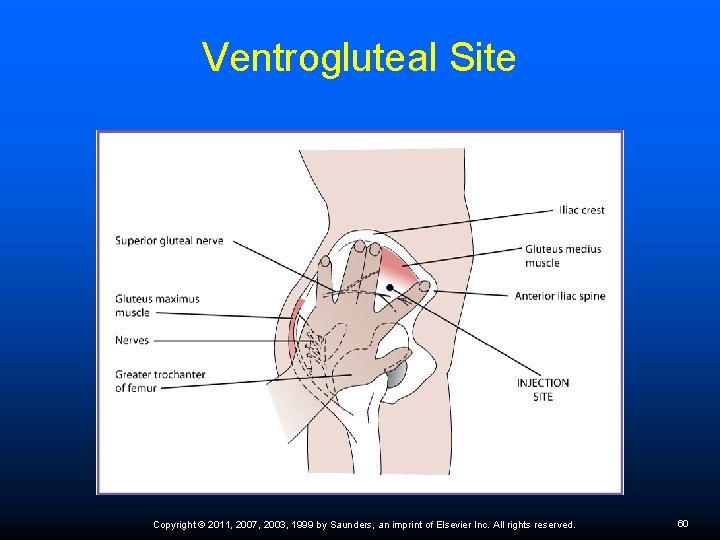
Ventrogluteal Site Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 60

Z-Track Injection Used when medication irritates skin and SC tissues Displace upper tissue before inserting needle to prevent leakage of medication from deep muscle to upper SC tissues Change needle after dispensing medication Ø Skin pushed aside and held, site cleansed Ø Needle inserted and medication slowly injected into deep muscle Ø After needle is withdrawn, release skin Ø Do not massage after injection Ø Rotate sites to prevent tissue damage Ø Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 61
Principles of Intravenous Therapy IV therapy is often the route of choice when the physician wants to speed up the action of a drug. The medical assistant must be familiar with both legal restrictions and employer policies before having anything to do with IV therapy. Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 62
Intravenous Terminology and Practices Three types of IV fluids Isotonic Ø Hypertonic Ø Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 63
Dangers of Intravenous Treatment Infection or inflammation Localized phlebitis Infiltration Fluid overload Medication error Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 64
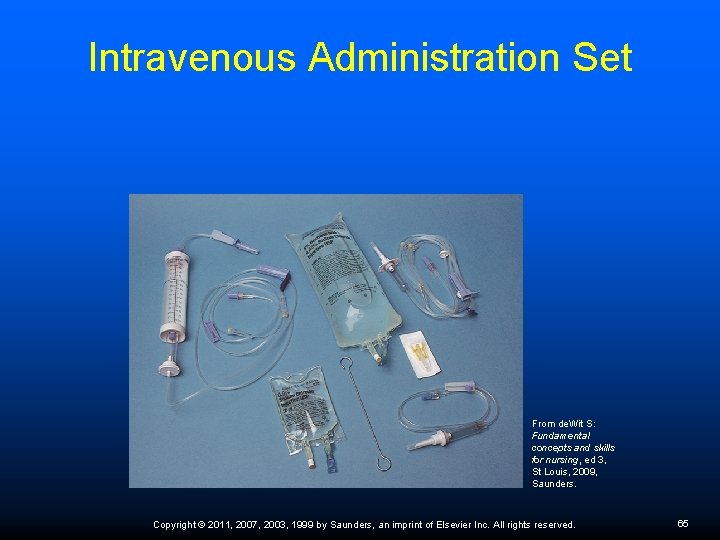
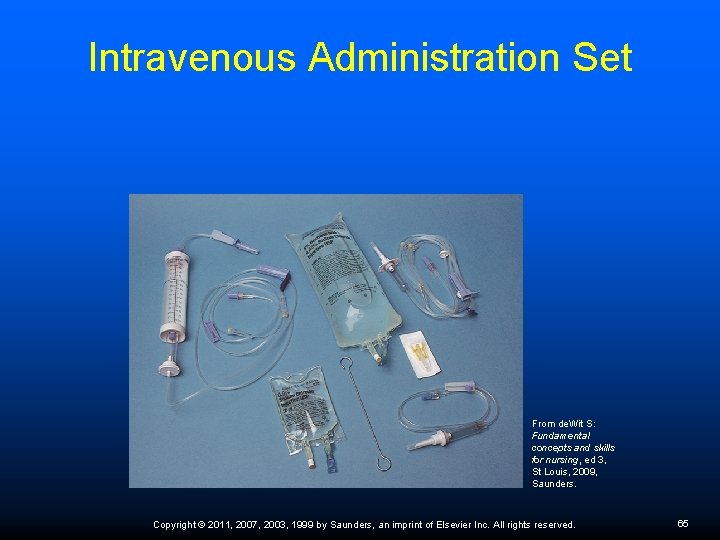
Intravenous Administration Set From de. Wit S: Fundamental concepts and skills for nursing, ed 3, St Louis, 2009, Saunders. Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 65
Role of the Medical Assistant in Assisting with Intravenous Therapy Follow state practice acts. Gather a comprehensive health history to determine indications for IV therapy. Weigh the patient before and monitor vital signs during infusion to alert the physician of possible complications; do not take blood pressure in arm with IV. Be alert for signs of infiltration and phlebitis. Monitor equipment for problems. Watch for the too-rapid infusion of fluids, which might lead to circulatory overload. Document all pertinent information in the patient record. Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 66

Drug Treatment The more the patient knows and understands about how to take the medication and why it is prescribed, the greater the chances that the drug treatment will be successful. Patient education is absolutely crucial to the correct administration of medication at home. Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 67

Patient Education The patient should understand: Purpose of the drug Ø Time, frequency, and amount of the dose Ø Storage requirements Ø Typical side effects Ø Take medicine as prescribed Ø Discard all expired drugs Ø Keep medicine away from light, heat, air, moisture Ø Do not combine different drugs in the same container Ø Copyright © 2011, 2007, 2003, 1999 by Saunders, an imprint of Elsevier Inc. All rights reserved. 68