Addressing Iron Deficiency Anemia 181 st Street Clinic






- Slides: 19

Addressing Iron Deficiency Anemia 181 st Street Clinic (Washington Heights Family Health Center) 2006 -7 PDSA Project

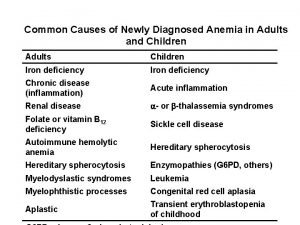
Why Tackle Iron Deficiency? #1 Nutritional Disorder in World 80% Fe Deficient 30% some form of Fe Deficient Anemia Easily Administered Therapy
SUPPLEMENTATION WORKS! Effect on of treatment n . 78 mg/d. L difference in those treated Positive Effects on Developmental Outcomes Cognition?
AIM Statement Reduce the impact of iron deficiency and iron deficiency anemia in children under 3 in our practice by: Increasing the identification of children at risk Implementing evidencebased treatment of iron deficiency anemia Establishing primary prevention of iron deficiency for an at-risk population (Patients aged 1 -3 years)
PDSA for Prevention of Anemia P: Implement primary prevention of iron deficiency D: Providers began prescribing prophylactic MVI with iron to all patients aged 1 -3 years S: Chart Review (2 wks post intervention): n Providers prescribing prophylactic MVI with Iron to 81% of patients 1 -3 years A: Expanded education efforts to ALL providers including nurse practitioners
AAP Iron-deficiency Screening and Treatment Guidelines Universal Screening in high risk communities n Hgb or Hct between 9 -12 months, and again 6 months later Treatment n Treat pts 6 m-1. 9 y with Hb <11. 0 mg/d. L, 2 -5 yrs with Hb < 11. 1 with 3 - 6 mg/kg/day of elemental iron n Repeat CBC 1 month into treatment – if hgb increased by 1 g/dl then continue for 2 more months, if NOT then further testing recommended n Repeat testing 6 months after successful treatment
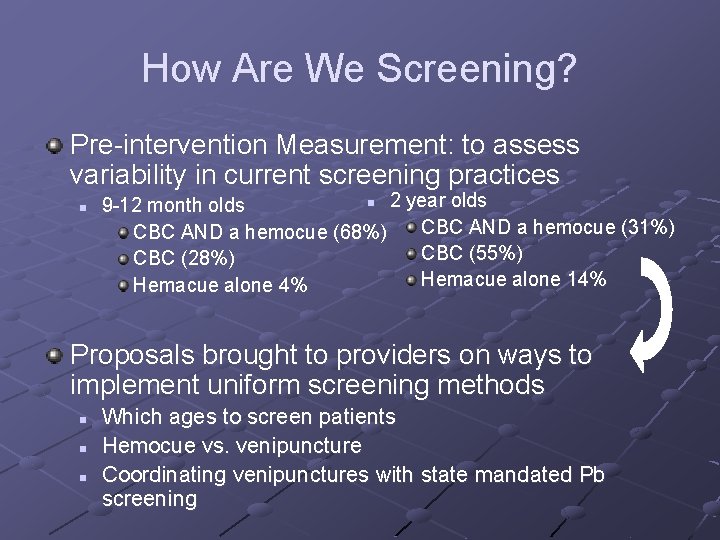
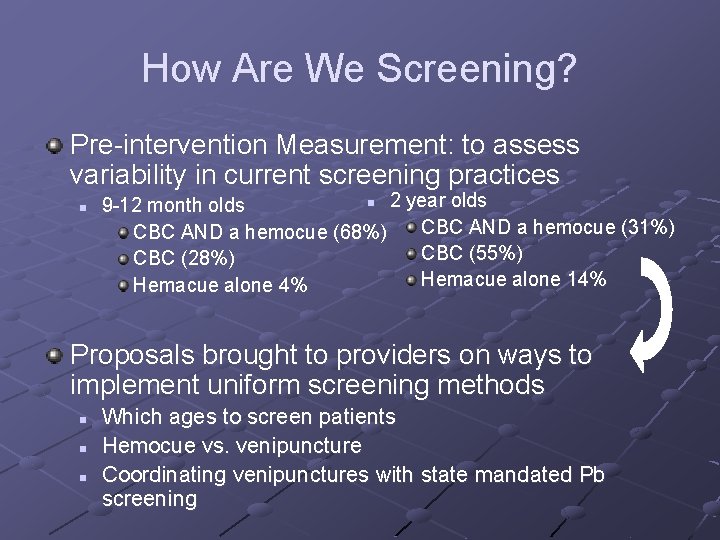
How Are We Screening? Pre-intervention Measurement: to assess variability in current screening practices n n 2 year olds 9 -12 month olds CBC AND a hemocue (68%) CBC AND a hemocue (31%) CBC (55%) CBC (28%) Hemacue alone 14% Hemacue alone 4% Proposals brought to providers on ways to implement uniform screening methods n n n Which ages to screen patients Hemocue vs. venipuncture Coordinating venipunctures with state mandated Pb screening
Changes Made To Screening At/ around 12 months: CBC and lead At/around 18 months: Hemocue At/around 24 months: CBC and lead
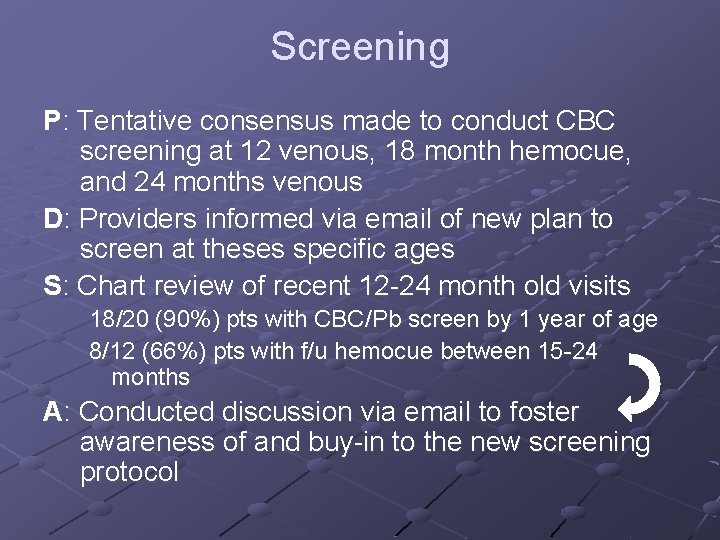
Screening P: Tentative consensus made to conduct CBC screening at 12 venous, 18 month hemocue, and 24 months venous D: Providers informed via email of new plan to screen at theses specific ages S: Chart review of recent 12 -24 month old visits 18/20 (90%) pts with CBC/Pb screen by 1 year of age 8/12 (66%) pts with f/u hemocue between 15 -24 months A: Conducted discussion via email to foster awareness of and buy-in to the new screening protocol
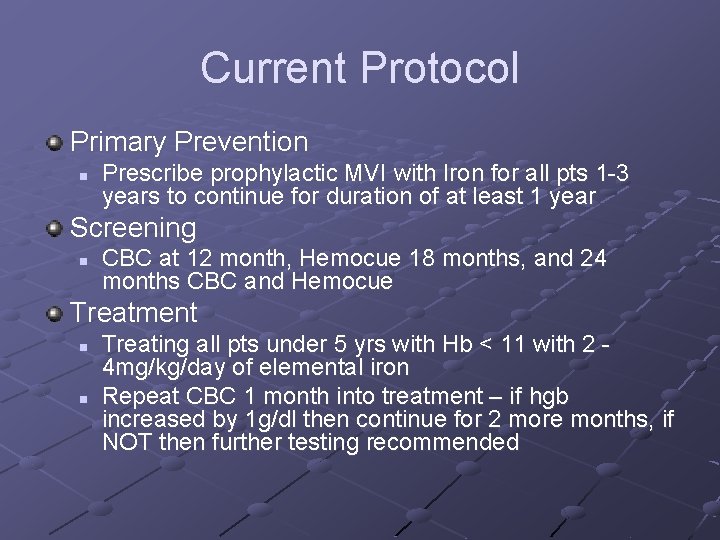
Current Protocol Primary Prevention n Prescribe prophylactic MVI with Iron for all pts 1 -3 years to continue for duration of at least 1 year Screening n CBC at 12 month, Hemocue 18 months, and 24 months CBC and Hemocue Treatment n n Treating all pts under 5 yrs with Hb < 11 with 2 - 4 mg/kg/day of elemental iron Repeat CBC 1 month into treatment – if hgb increased by 1 g/dl then continue for 2 more months, if NOT then further testing recommended
Treatment Pre-Intervention Measurement: n 4/16 (25%) patients with iron-deficiency anemia given correct treatment doses of Iron according to AAP Providers educated on AAP guidelines Discussion of how we plan to implement/adapt the AAP guidelines, e. g: n n Dosage Anemia definition (i. e. cut-offs by age – vs AAP)
Chart Review—Are we appropriately documenting, diagnosing, & treating anemia? patients age 1 to 3 with dx code of anemia over a 6 month period Results: n n n (1) 94% proper “anemia diagnosis (2) 81% treated with 2 -4 mg/kg/day dosing of Fer-in-sol (3) 81% correctly instructed for follow-up as per documentation (4) 94% followed up regardless of documentation (5) 63% documented resolution of anemia (though some still in Tx at time of review) Goals: Are we reaching them? Documentation might not lead us to believe so…
Compliance Problem Randomly selected group of parents of one to 3 year olds. Only 40% took the vitamins nearly all the time (5 times a week or more). 50% of the parents surveyed admitted non-compliance (one dose a week or less)
Compliance Chart Review 1 to 3 year olds from each provider 59% had documentation of child taking Polyvisol with Fe. All charts documented appropriate screening times for CBC Reasons for non-compliance

Steps Towards Compliance IRON RICH FOOD HANDOUT English version: revised the handout at a 4 th grade reading level using the Flesch-Kincaid Grade Level Index. b) Spanish version: translators and Fernandez-Huerta scale between 5 th and 6 th grade.
Future Directions Finalize consensus screening protocol and achieve provider buy-in Why are parents not giving the Iron? n Are the Handouts helping? Chart reviews n Treatment – Are we treating for kids who meet criteria? For patients diagnosed with anemia how is the follow-up – testing at 1 month? Continuing for 3 months at least? n Primary Prevention – Are patients staying on the MVI with Iron? Is it resulting in fewer kids with anemia?

Previous PDSA? Dental Health n 50% documentation of discussion Developmental or Speech Delay n n 50% documented discussion 0% used sticker’s from last year’s project

The Team Attendings n n n Steve Caddle Adriana Matiz Mary Mc. Cord Melanie Gissen Patricia Hametz Dodi Meyer Elise Olshen Kharbanda Mary Zweighaft Carol Pafundi Harriet Mc. Gurk Annie Armstrong Melissa Glassman Residents n n n n Monique Collier Brenton Mar Eliza Auerback Sarah Schrager Carol Senkler Paula Ayora Dawn Wetzel John Babineau Rachelle Gandica Maja Castillo Brenda Ritson Matt Laurich Patricia Tae Ola Aganga Mahbod Mohazzebi Staff n n n n Joan Mahoney Maralin Bautista Candida Rodriguez Petra Ortiz Beatrice Frempong Annes Silver Annie Hertz Bill Johnson Leilani Vinales Ivelisse Rodriguez Iliana Torres Cindy Ferrer Evelyn Mejia Denise Connolly. Hoyt

 Iron deficiency anemia labs
Iron deficiency anemia labs Dietary iron
Dietary iron Menstrual blood
Menstrual blood Megaloblastic anemia laboratory findings
Megaloblastic anemia laboratory findings What are the 3 stages of iron deficiency
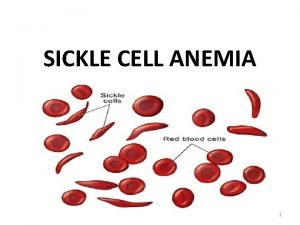
What are the 3 stages of iron deficiency Diagnose iron deficiency anemia
Diagnose iron deficiency anemia Serum ferritin in iron deficiency anemia
Serum ferritin in iron deficiency anemia Minerals are inorganic elements that the body
Minerals are inorganic elements that the body Losmosis
Losmosis Feroba-you sr tab
Feroba-you sr tab Dashod dog
Dashod dog Anemiam
Anemiam Flat addressing vs hierarchical addressing
Flat addressing vs hierarchical addressing Anemia
Anemia Megaloblastic anemia causes
Megaloblastic anemia causes Megaloblastic anemia vs pernicious anemia
Megaloblastic anemia vs pernicious anemia Causes of iron deficiency
Causes of iron deficiency Dactylitis
Dactylitis Chlorsis
Chlorsis Street addressing system
Street addressing system