Acute Mesenteric Ischemia Isaac George MD Resident in

- Slides: 58
Acute Mesenteric Ischemia Isaac George, MD Resident in Surgery Department of Surgery Columbia University College of Physicians and Surgeons The PVD. org
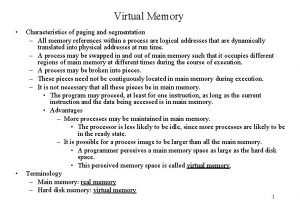
Acute Mesenteric Ischemia • • • Incidence Pathophysiology Diagnosis Therapy Treatment Algorithm Objectives The PVD. org
Objectives • • • Understand pathophysiology Identify patients at high-risk for mesenteric ischemia Develop treatment plan for each patient/apply treatment algorithm The PVD. org
Introduction • Cokkinis (1921): “occlusion of the mesenteric vessels is regarded as one of those conditions of which the diagnosis is impossible, the prognosis hopeless, and the treatment almost useless. ” • Occlusive or non-occlusive mechanism leading to hypoperfusion of one or more mesenteric vessels The PVD. org
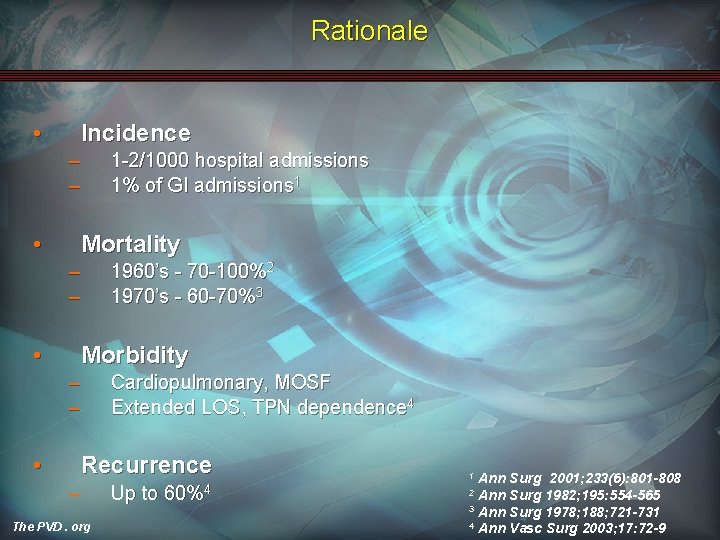
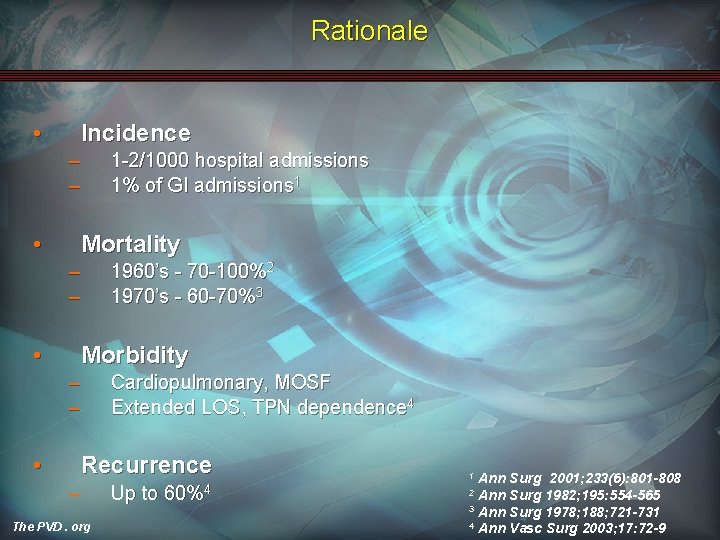
Rationale • Incidence – – • Mortality – – • 1960’s - 70 -100%2 1970’s - 60 -70%3 Morbidity – – • 1 -2/1000 hospital admissions 1% of GI admissions 1 Cardiopulmonary, MOSF Extended LOS, TPN dependence 4 Recurrence – The PVD. org Up to 60%4 Ann Surg 2001; 233(6): 801 -808 Ann Surg 1982; 195: 554 -565 3 Ann Surg 1978; 188; 721 -731 4 Ann Vasc Surg 2003; 17: 72 -9 1 2
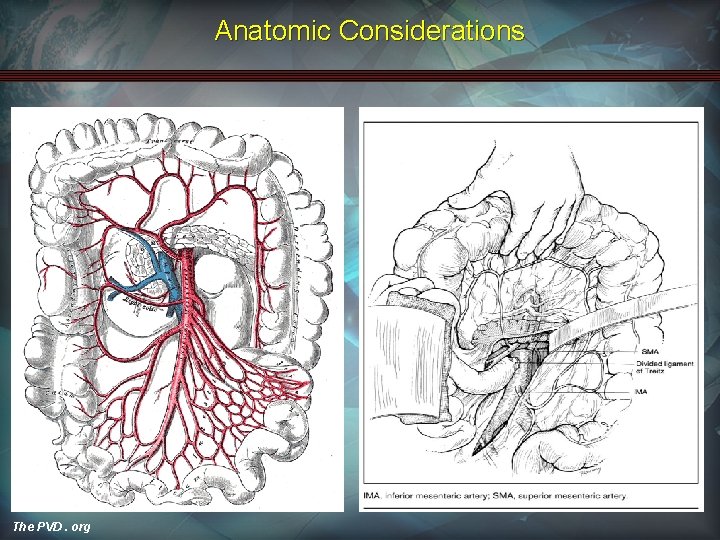
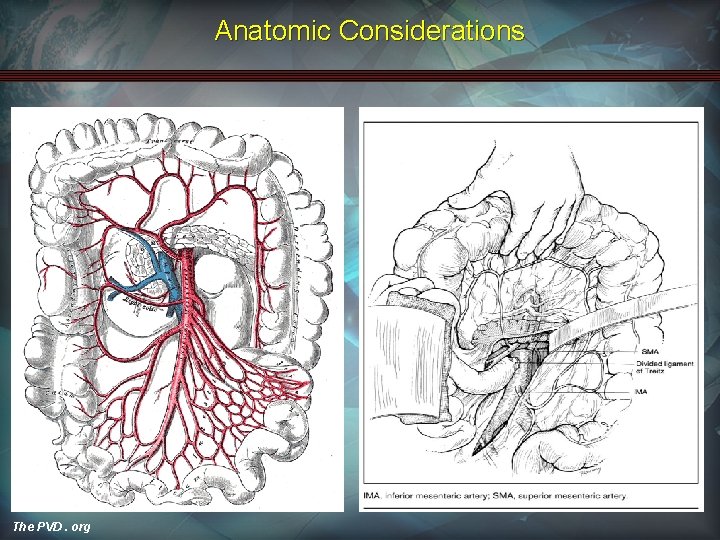
Anatomic Considerations The PVD. org
Pathophysiology: Etiology • Arterial Embolic Disease • Arterial Thrombotic Disease • Venous Thrombotic Disease • Non-occlusive Mesenteric Ischemia The PVD. org
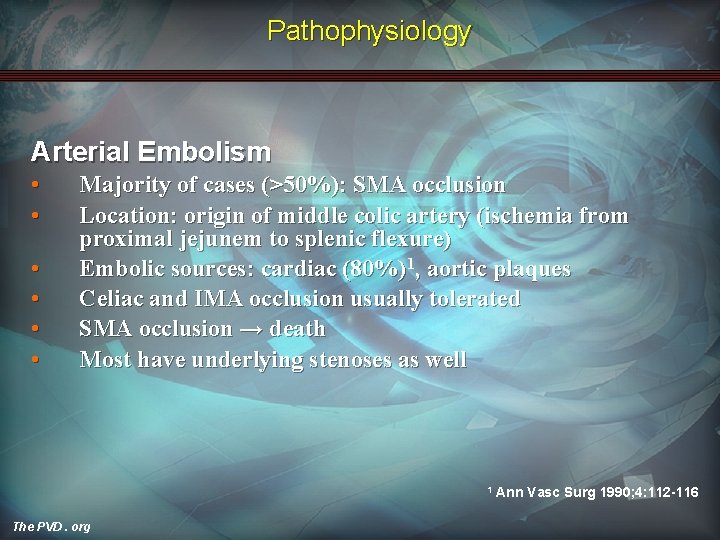
Pathophysiology Arterial Embolism • • • Majority of cases (>50%): SMA occlusion Location: origin of middle colic artery (ischemia from proximal jejunem to splenic flexure) Embolic sources: cardiac (80%)1, aortic plaques Celiac and IMA occlusion usually tolerated SMA occlusion → death Most have underlying stenoses as well 1 The PVD. org Ann Vasc Surg 1990; 4: 112 -116
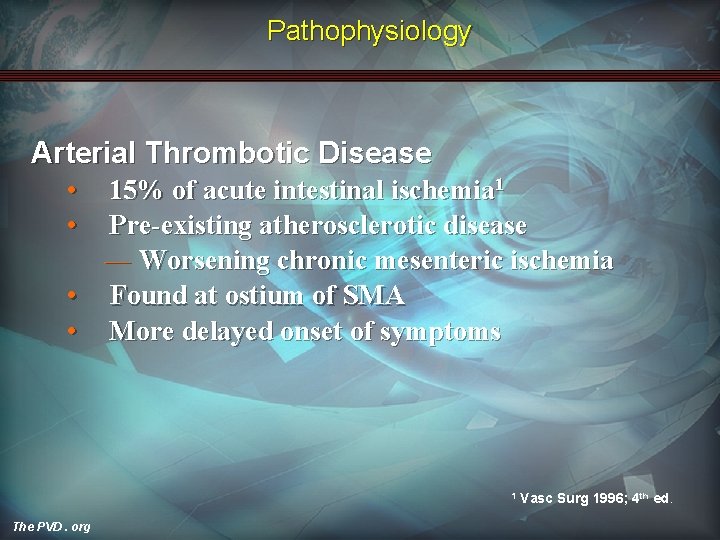
Pathophysiology Arterial Thrombotic Disease • • 15% of acute intestinal ischemia 1 Pre-existing atherosclerotic disease ― Worsening chronic mesenteric ischemia • Found at ostium of SMA • More delayed onset of symptoms 1 The PVD. org Vasc Surg 1996; 4 th ed.
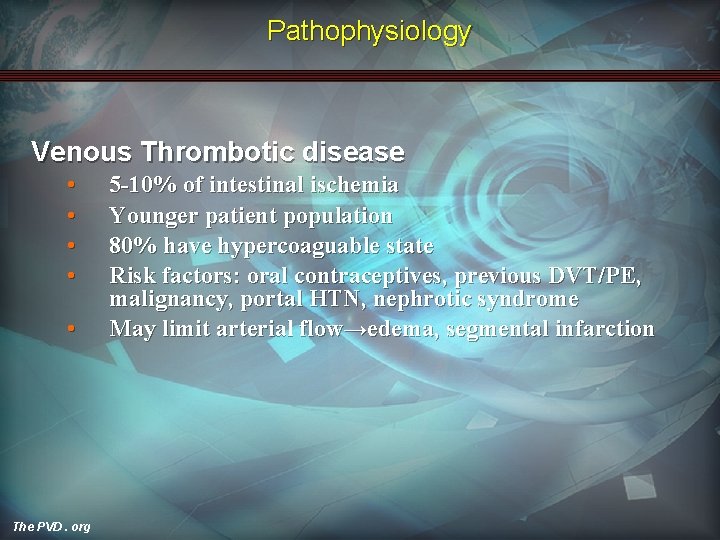
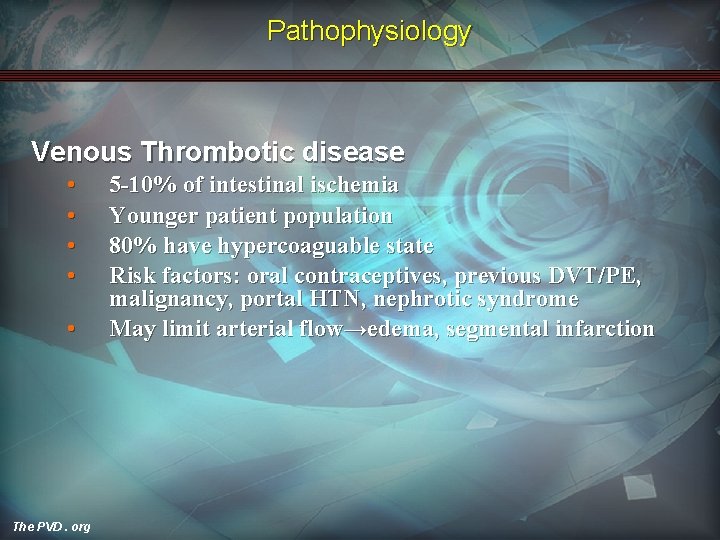
Pathophysiology Venous Thrombotic disease • • • The PVD. org 5 -10% of intestinal ischemia Younger patient population 80% have hypercoaguable state Risk factors: oral contraceptives, previous DVT/PE, malignancy, portal HTN, nephrotic syndrome May limit arterial flow→edema, segmental infarction
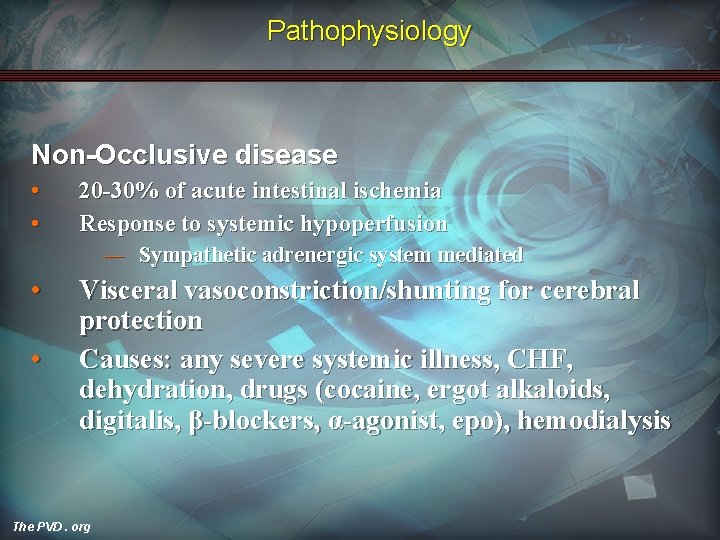
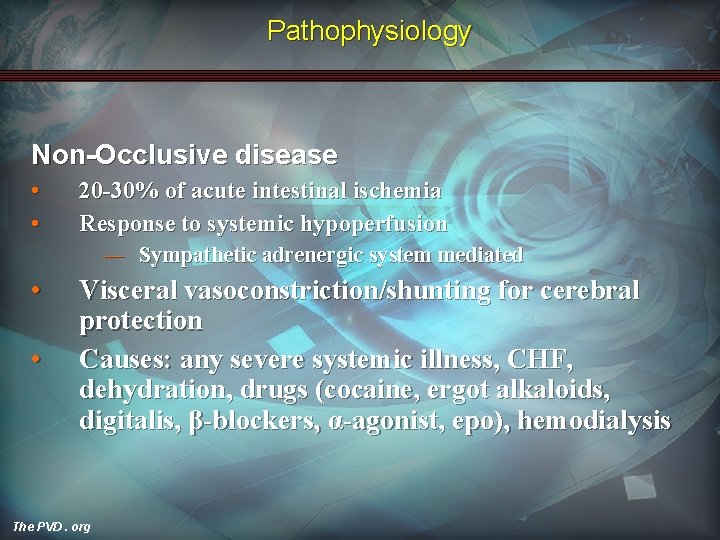
Pathophysiology Non-Occlusive disease • • 20 -30% of acute intestinal ischemia Response to systemic hypoperfusion ― Sympathetic adrenergic system mediated • • Visceral vasoconstriction/shunting for cerebral protection Causes: any severe systemic illness, CHF, dehydration, drugs (cocaine, ergot alkaloids, digitalis, β-blockers, α-agonist, epo), hemodialysis The PVD. org
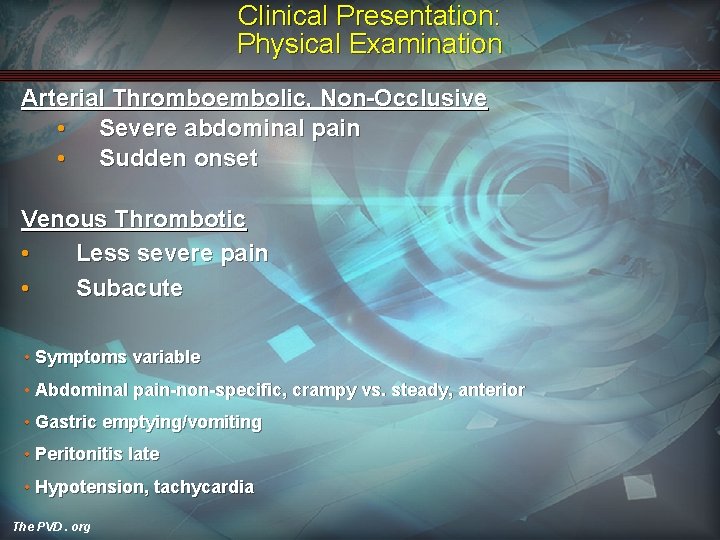
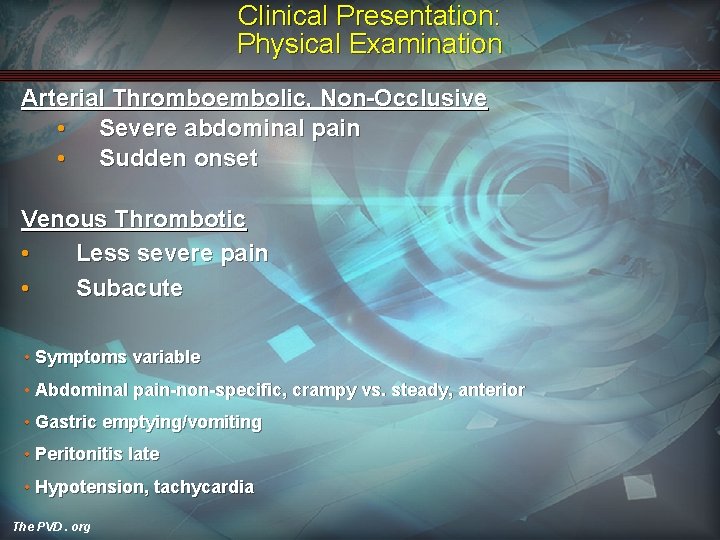
Clinical Presentation: Physical Examination Arterial Thromboembolic, Non-Occlusive • Severe abdominal pain • Sudden onset Venous Thrombotic • Less severe pain • Subacute • Symptoms variable • Abdominal pain-non-specific, crampy vs. steady, anterior • Gastric emptying/vomiting • Peritonitis late • Hypotension, tachycardia The PVD. org
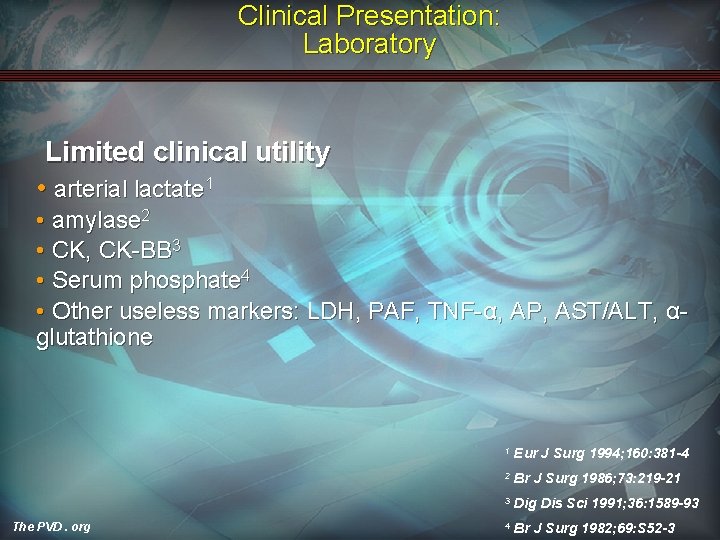
Clinical Presentation: Laboratory Limited clinical utility • arterial lactate 1 • amylase 2 • CK, CK-BB 3 • Serum phosphate 4 • Other useless markers: LDH, PAF, TNF-α, AP, AST/ALT, αglutathione The PVD. org 1 Eur J Surg 1994; 160: 381 -4 2 Br J Surg 1986; 73: 219 -21 3 Dig Dis Sci 1991; 36: 1589 -93 4 Br J Surg 1982; 69: S 52 -3
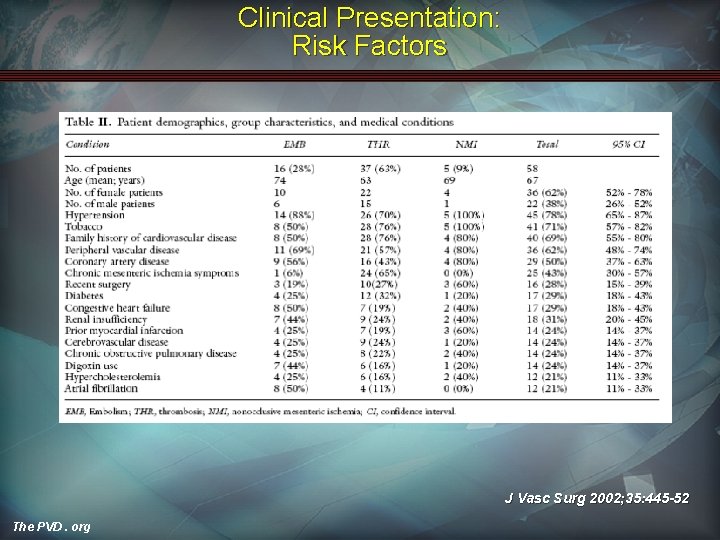
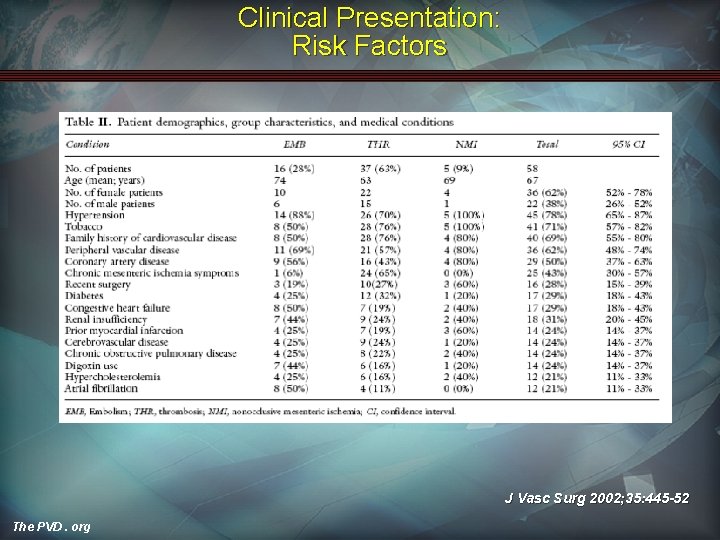
Clinical Presentation: Risk Factors J Vasc Surg 2002; 35: 445 -52 The PVD. org
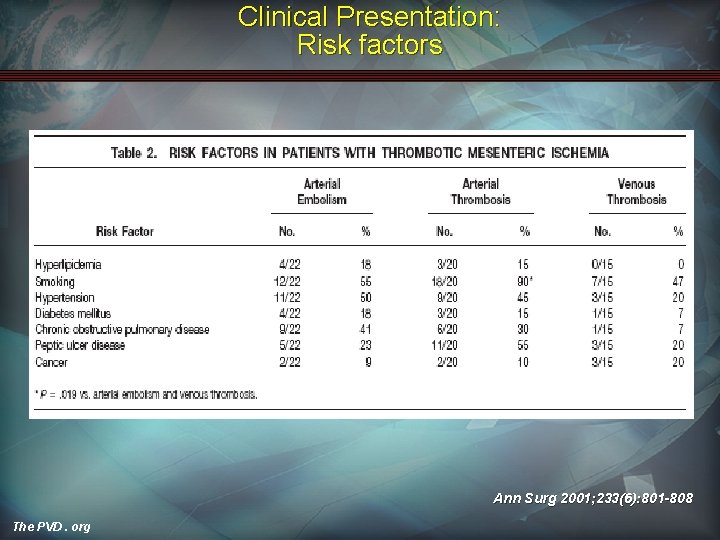
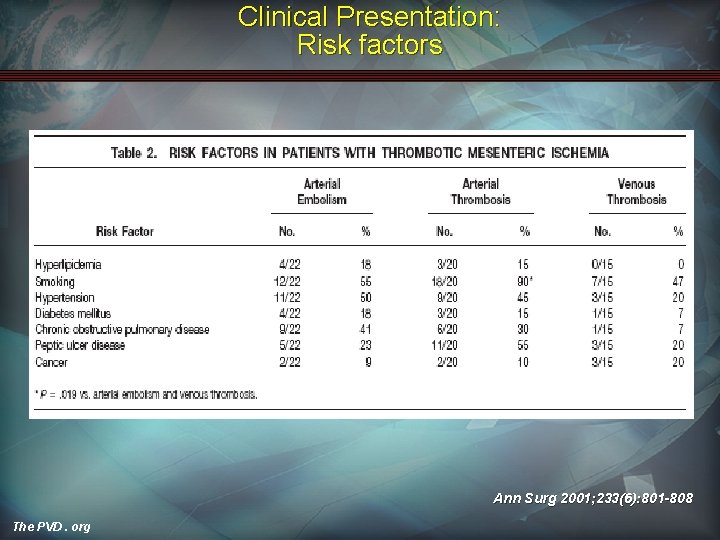
Clinical Presentation: Risk factors Ann Surg 2001; 233(6): 801 -808 The PVD. org
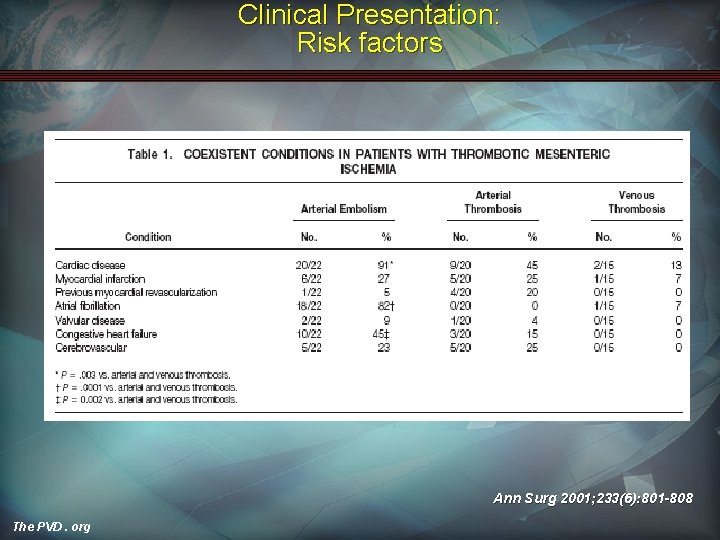
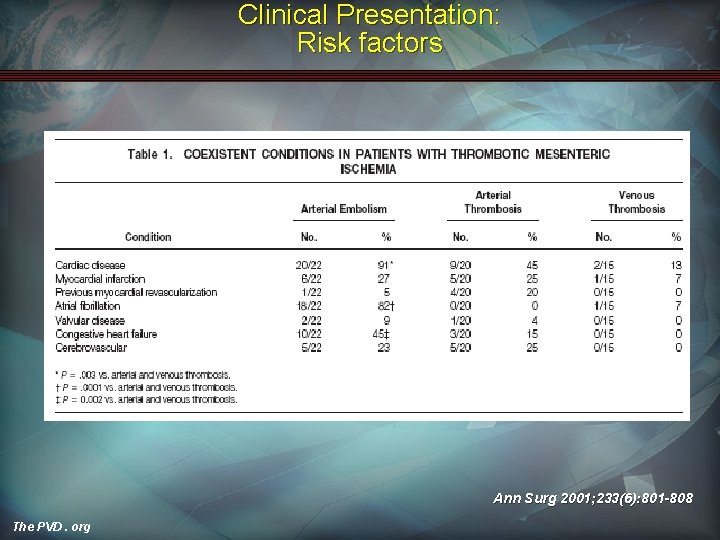
Clinical Presentation: Risk factors Ann Surg 2001; 233(6): 801 -808 The PVD. org
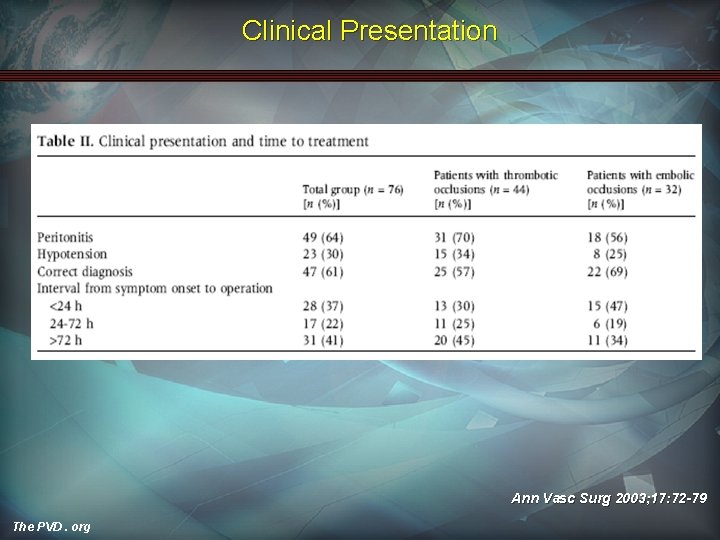
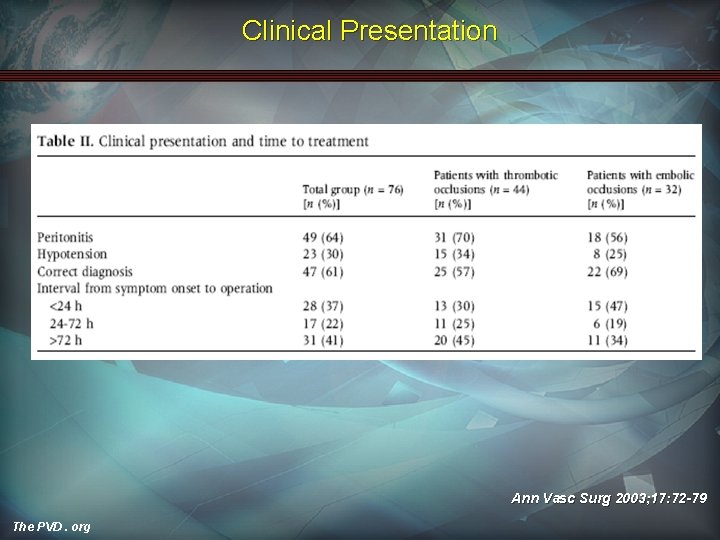
Clinical Presentation Ann Vasc Surg 2003; 17: 72 -79 The PVD. org
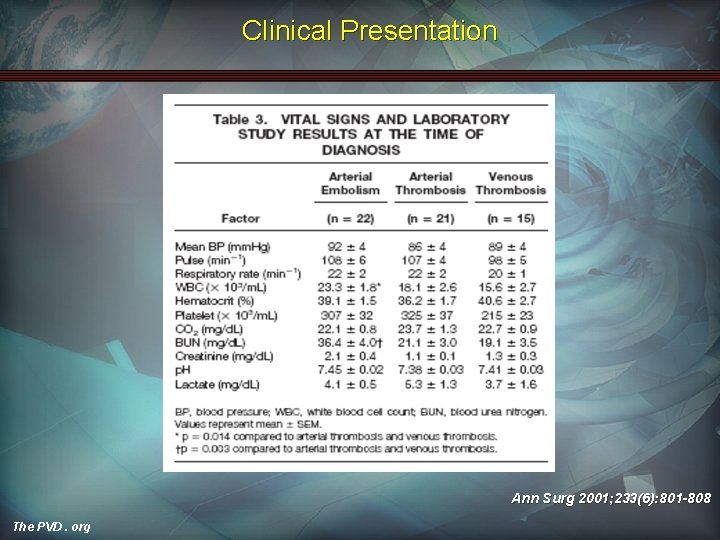
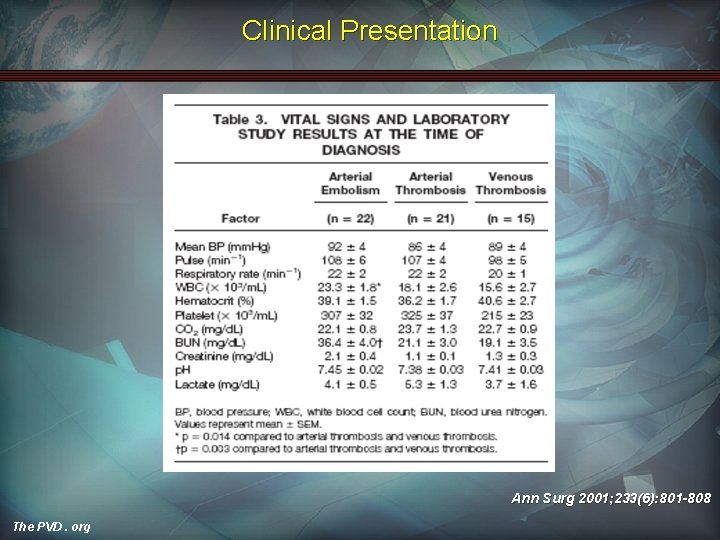
Clinical Presentation Ann Surg 2001; 233(6): 801 -808 The PVD. org
Diagnosis: Non-Invasive Imaging X-ray Computed Tomography (helical/angiography) Ultrasound MRI/MRA The PVD. org
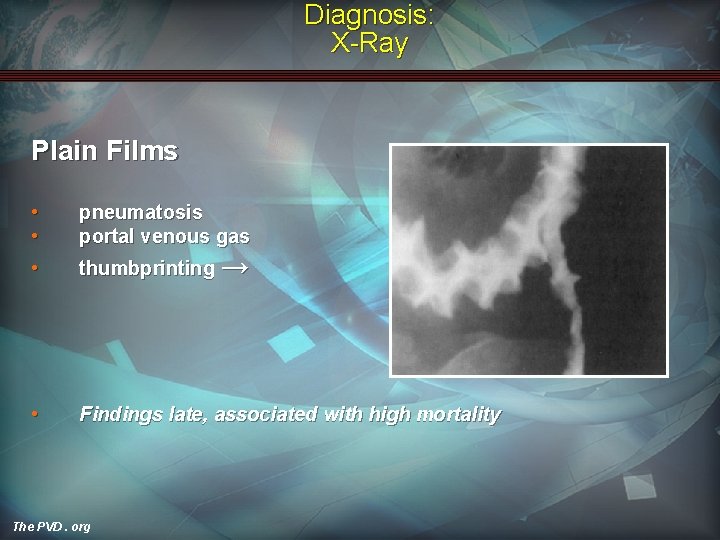
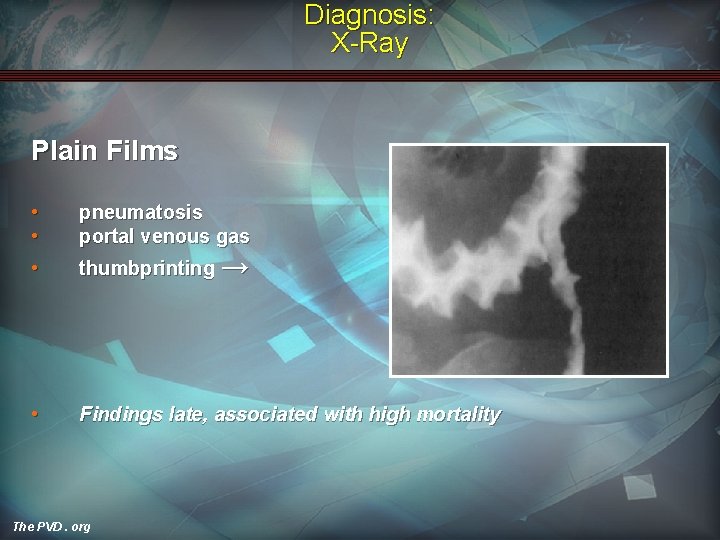
Diagnosis: X-Ray Plain Films • • pneumatosis portal venous gas • thumbprinting → • Findings late, associated with high mortality The PVD. org
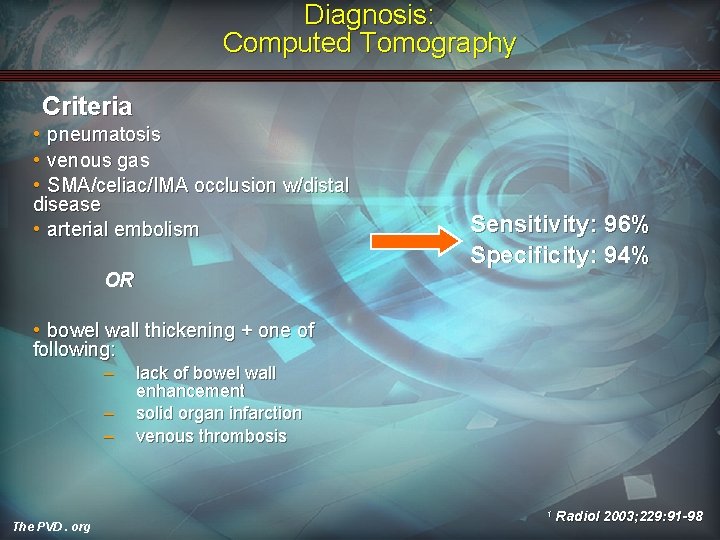
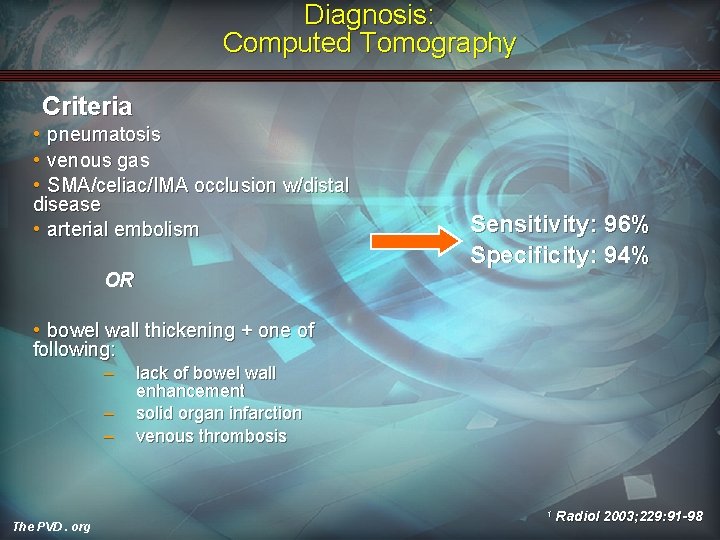
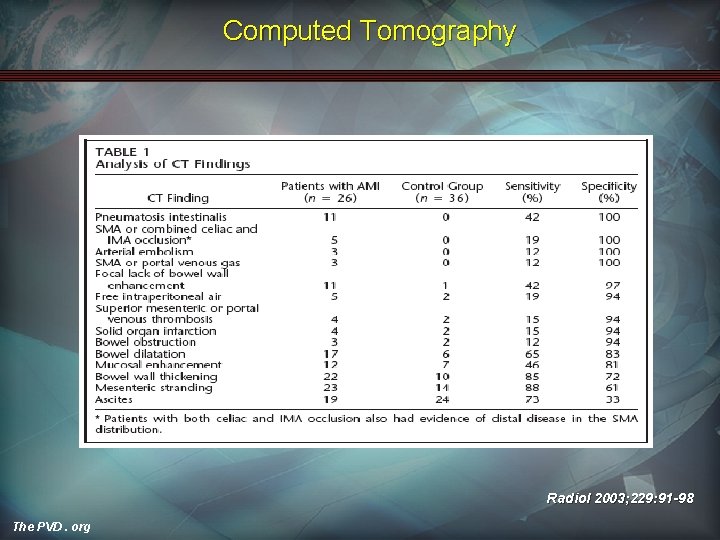
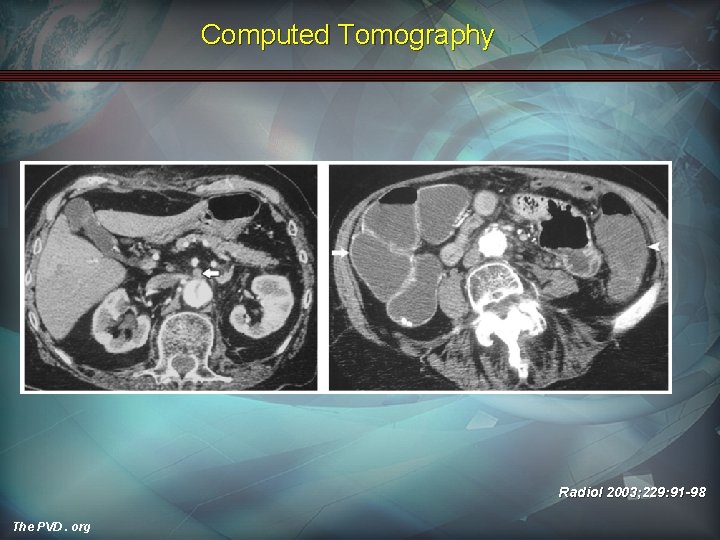
Diagnosis: Computed Tomography Criteria • pneumatosis • venous gas • SMA/celiac/IMA occlusion w/distal disease • arterial embolism Sensitivity: 96% Specificity: 94% OR • bowel wall thickening + one of following: – – – lack of bowel wall enhancement solid organ infarction venous thrombosis 1 The PVD. org Radiol 2003; 229: 91 -98
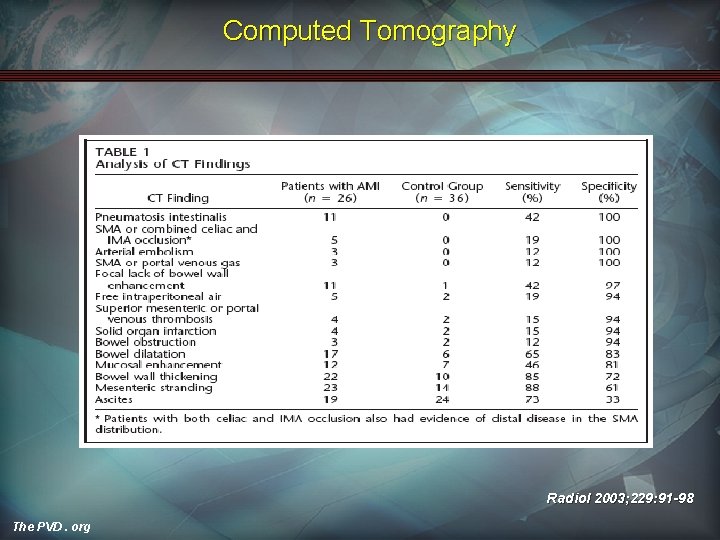
Computed Tomography Radiol 2003; 229: 91 -98 The PVD. org
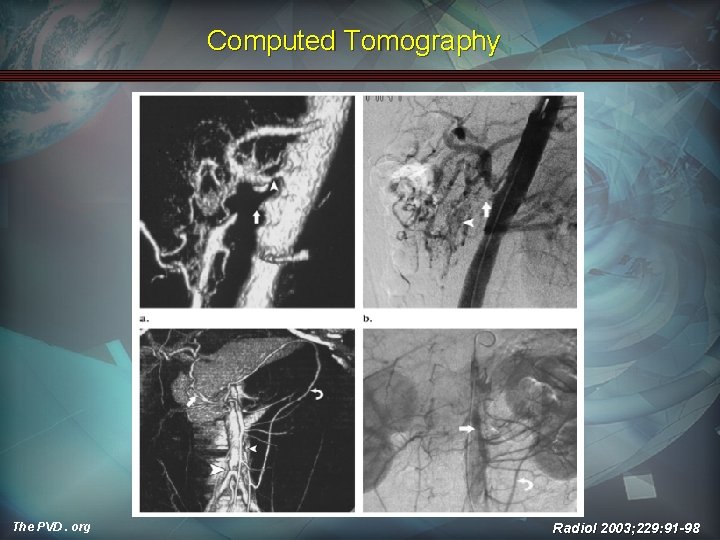
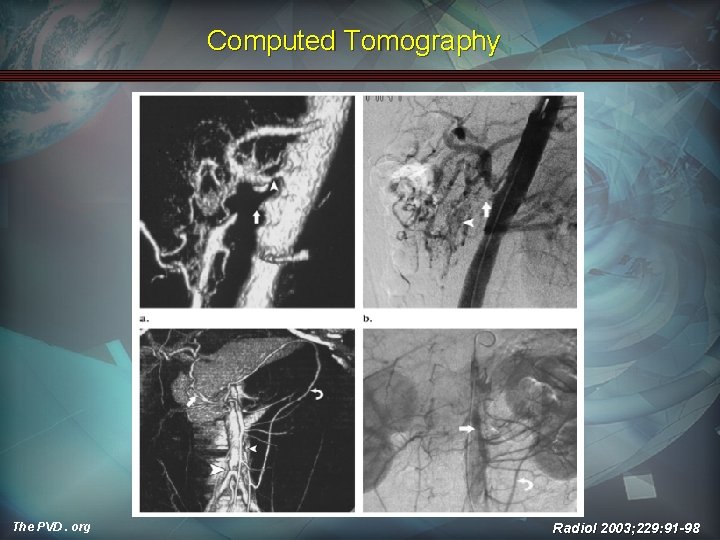
Computed Tomography The PVD. org Radiol 2003; 229: 91 -98
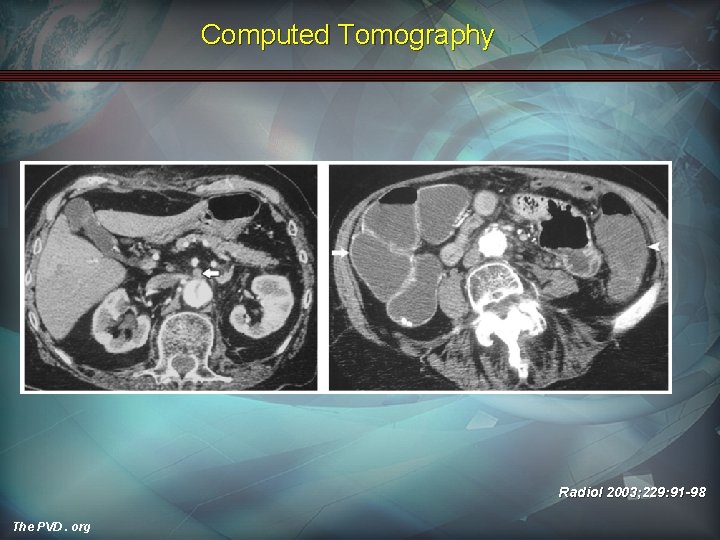
Computed Tomography Radiol 2003; 229: 91 -98 The PVD. org
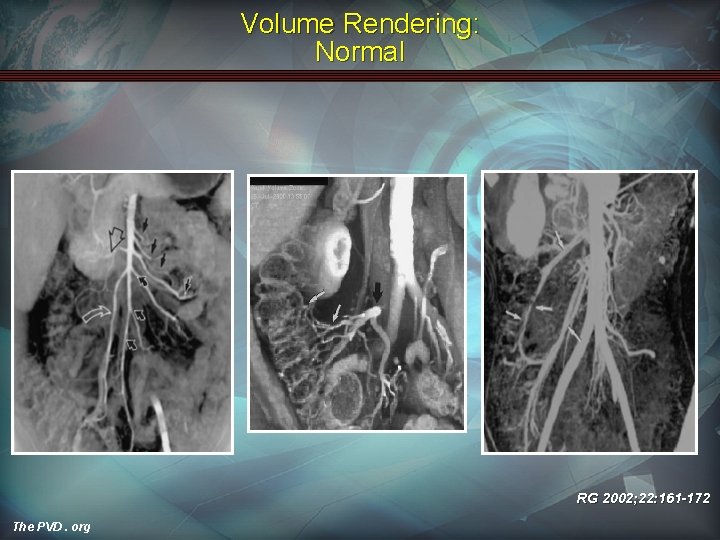
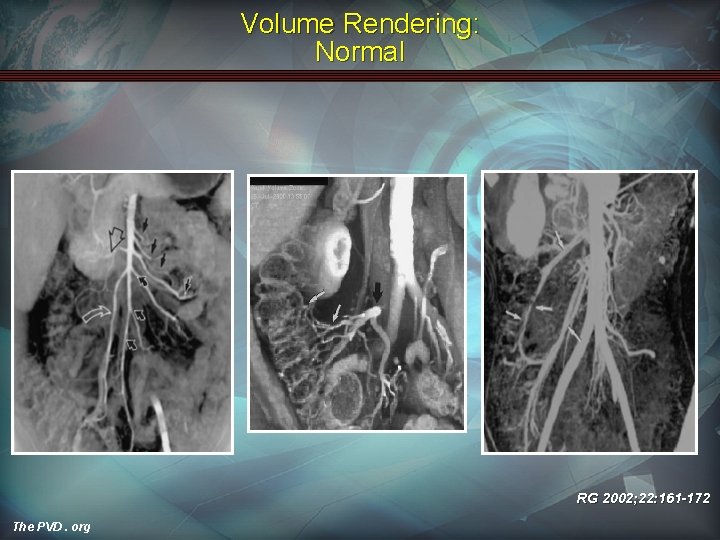
Volume Rendering: Normal RG 2002; 22: 161 -172 The PVD. org
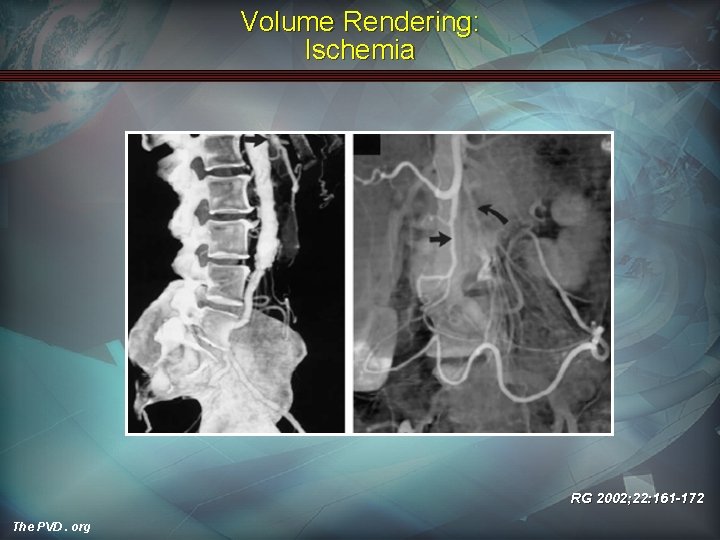
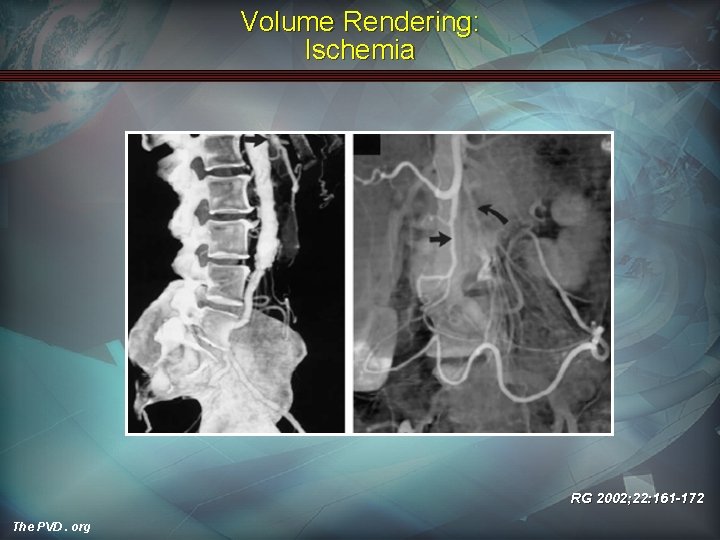
Volume Rendering: Ischemia RG 2002; 22: 161 -172 The PVD. org
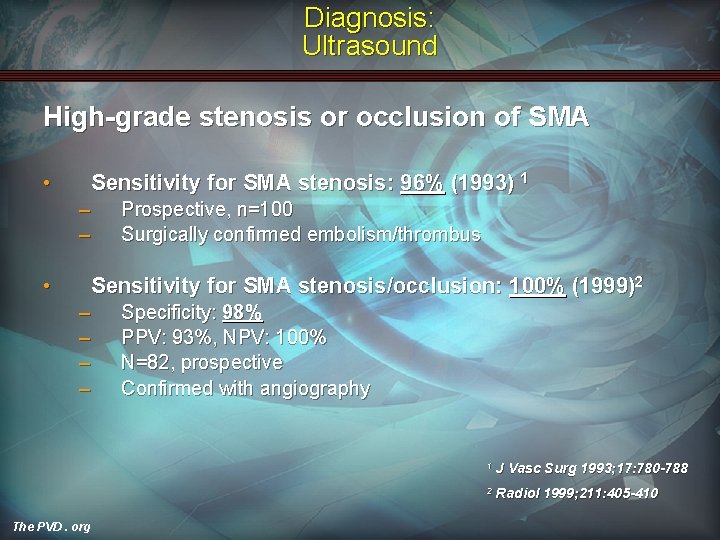
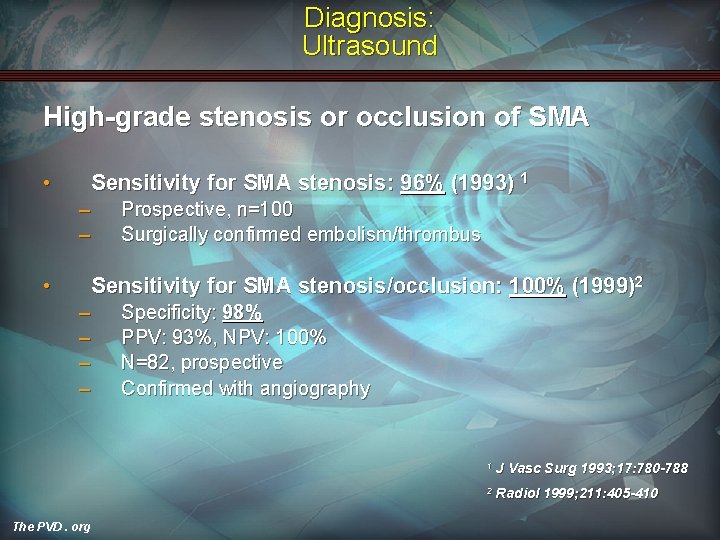
Diagnosis: Ultrasound High-grade stenosis or occlusion of SMA • Sensitivity for SMA stenosis: 96% (1993) 1 – – • Prospective, n=100 Surgically confirmed embolism/thrombus Sensitivity for SMA stenosis/occlusion: 100% (1999)2 – – The PVD. org Specificity: 98% PPV: 93%, NPV: 100% N=82, prospective Confirmed with angiography 1 J Vasc Surg 1993; 17: 780 -788 2 Radiol 1999; 211: 405 -410
Diagnosis: MRI • • • Poor delineation of smaller vessels Limited clinical application Perfusion flow contrast studies show promise 1 1 The PVD. org Radiol 2004; 234: 569 -575
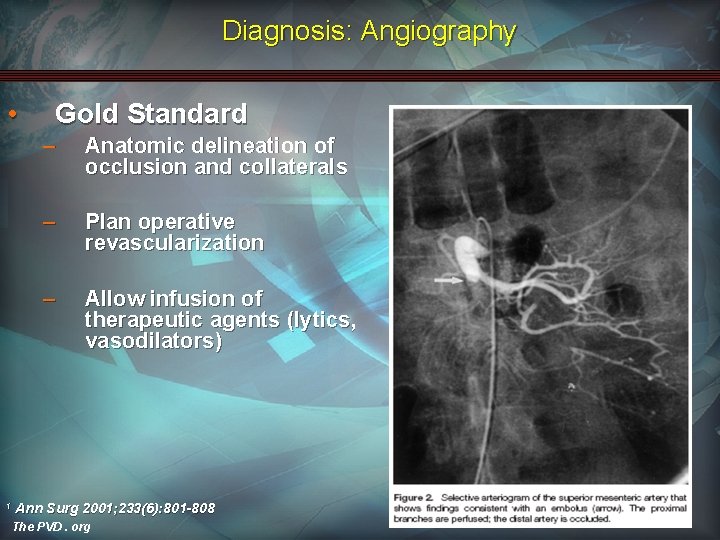
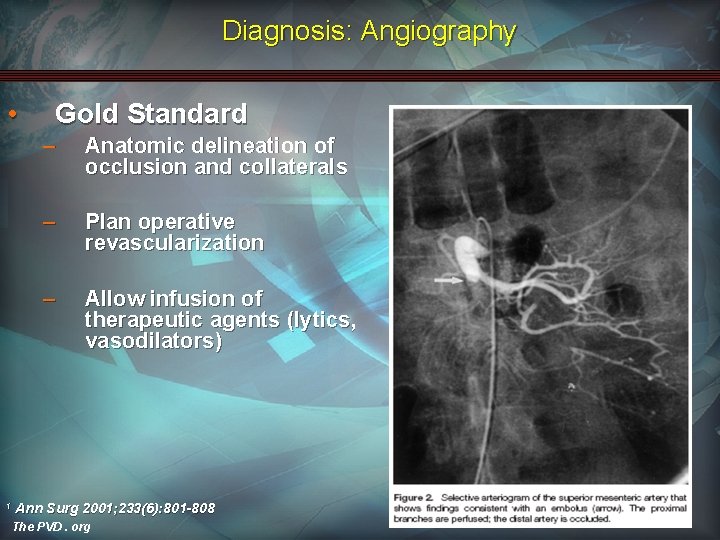
Diagnosis: Angiography • 1 Gold Standard – Anatomic delineation of occlusion and collaterals – Plan operative revascularization – Allow infusion of therapeutic agents (lytics, vasodilators) Ann Surg 2001; 233(6): 801 -808 The PVD. org
Principles of Treatment • Diagnose • Restore Flow • Resect non-viable tissue • Supportive Care • Second-Look The PVD. org
Therapy Supportive measures • IV resuscitation • Optimize cardiac status • Broad-spectrum antibiotics (no data) • Nasogastric decompression The PVD. org
Therapy: Pharmacologic Anticoagulation • Heparin IV – – – Prevents clot propagation Systemic vs. intra-arterial Timing of initiation • – • Immediately vs. 48 hr delay 1, 2 Restart 48 hrs after surgical intervention Warfarin – – The PVD. org Prevents clot propagation Give for 6 -12 mos if no clotting disorder (no data) 1 Surg Gynecol Obstet 1981; 153: 561 -569 2 Vascular Emergencies. 1982; 553 -561
Therapy: Pharmacologic Vasodilators • Papaverine (30 -60 mg/hr) – Increases c. AMP, relaxes smooth muscle – Primary indication: Non-occlusive arterial disease – Criterion for use: • • • The PVD. org Peritoneal signs absent Cannot undergo surgery Must have good distal perfusion bed
Therapy: Pharmacologic Vasodilators (cont. ) • Papaverine – Early SMA infusion reduces mortality to 40 -50%1 – Directed infusion via angiography – Rx: 24 -48 hrs • • Endpoints both clinical and angiographic Subsequent surgery 1 The PVD. org Surg 1977; 82: 848 -855
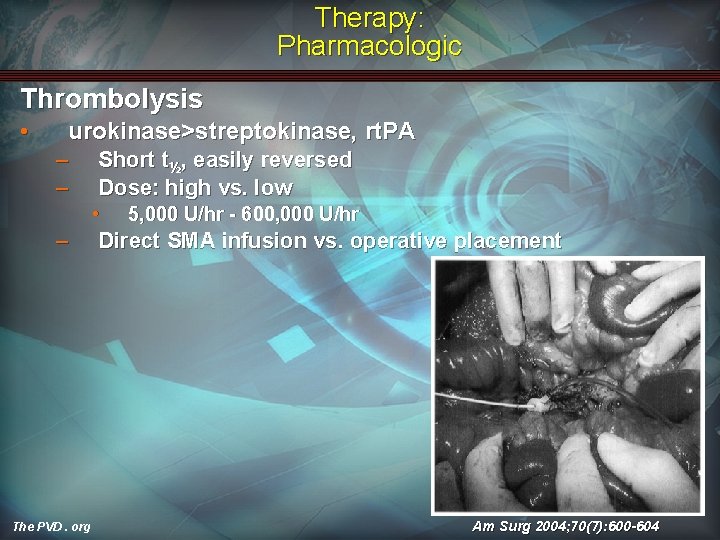
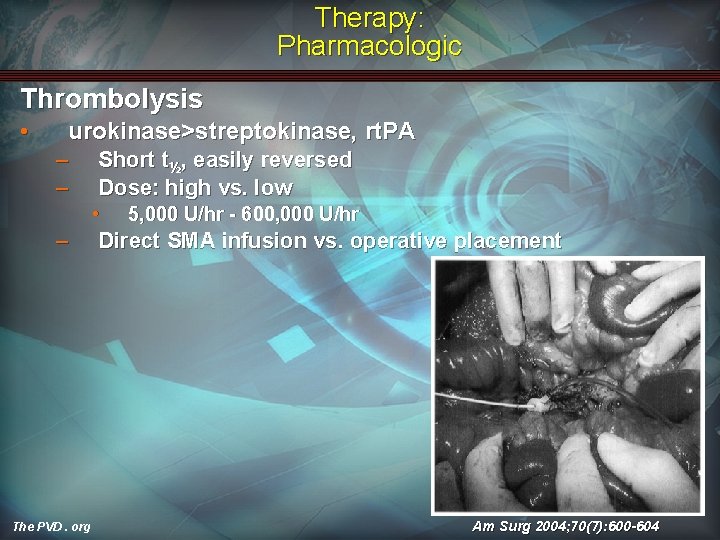
Therapy: Pharmacologic Thrombolysis • urokinase>streptokinase, rt. PA – – Short t½, easily reversed Dose: high vs. low • – The PVD. org 5, 000 U/hr - 600, 000 U/hr Direct SMA infusion vs. operative placement Am Surg 2004; 70(7): 600 -604
Therapy: Pharmacologic Thrombolysis • Duration: minutes – 48 hrs 1 – too long → risk of bowel necrosis – Treat to re-establish flow vs. complete dissolution – > 48 hrs • – Greater risk of bleeding Discontinue • • • Worsening abdominal symptoms without evidence of thrombolysis Bleeding No angiographic improvement 1 The PVD. org JVIR 2005; 16: 317 -329
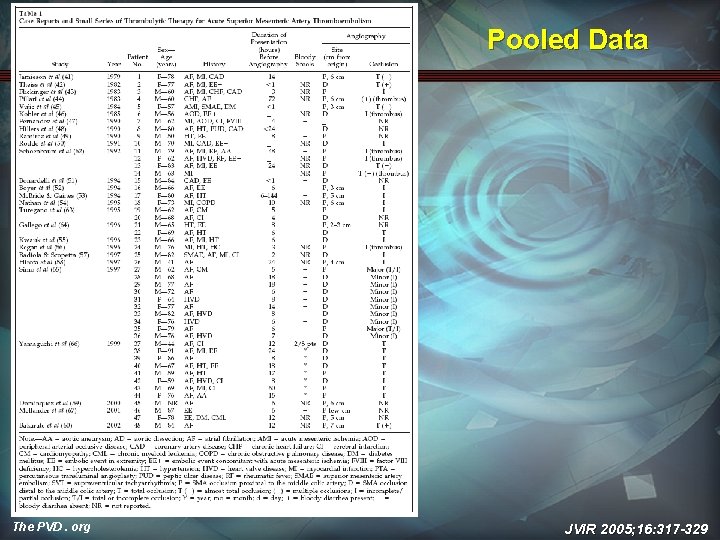
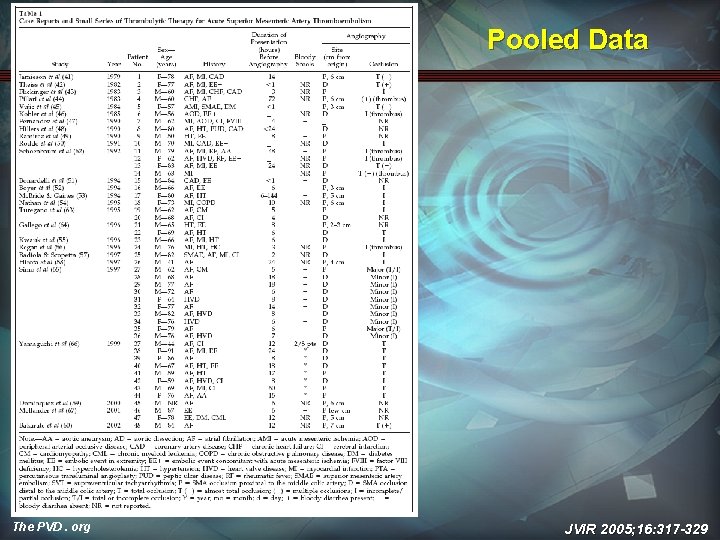
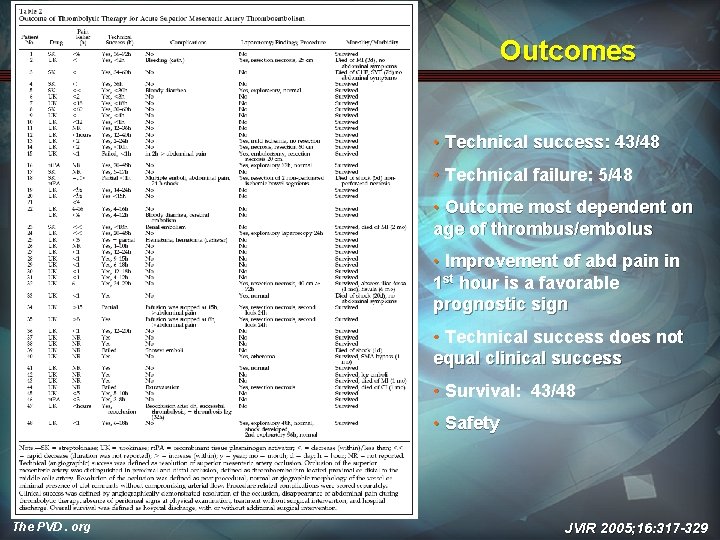
Pooled Data The PVD. org JVIR 2005; 16: 317 -329
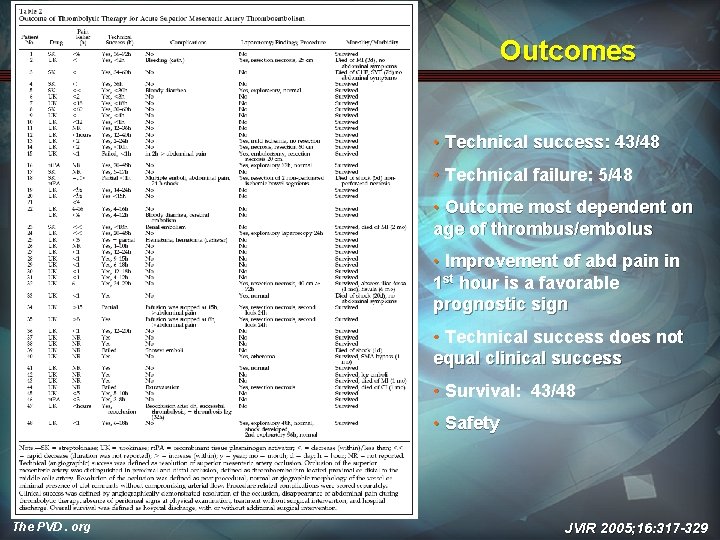
Outcomes • Technical success: 43/48 • Technical failure: 5/48 • Outcome most dependent on age of thrombus/embolus • Improvement of abd pain in 1 st hour is a favorable prognostic sign • Technical success does not equal clinical success • Survival: 43/48 • Safety The PVD. org JVIR 2005; 16: 317 -329
Therapy: Pharmacologic Thrombolysis • Criterion for use: – – • Embolic/thrombotic disease Poor operative candidates No contraindications to fibrinolytics No bowel infarction (no peritonitis/acidosis) Expansion of use to all patients without bowel infarction The PVD. org
Therapy: Endovascular Angioplasty/Stenting • • • Long-term durability questioned vs. surgical repair Utility in acute ischemia setting Advantages: – Shorter duration of treatment than thrombolysis – Definitive treatment JVIR 1999; 10(7): 861 -867 The PVD. org
Therapy: Endovascular Angioplasty/Stenting • Ideal for thrombotic lesions – – – • Calcified ostial lesions Flow-limiting dissections Chronic occlusion Advanced techniques for embolic lesions – – The PVD. org Flow-limiting dissections Embolectomy w/distal protection
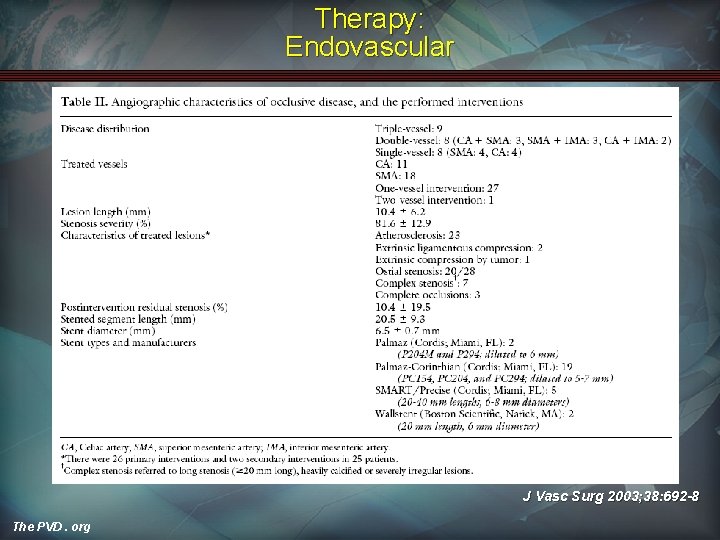
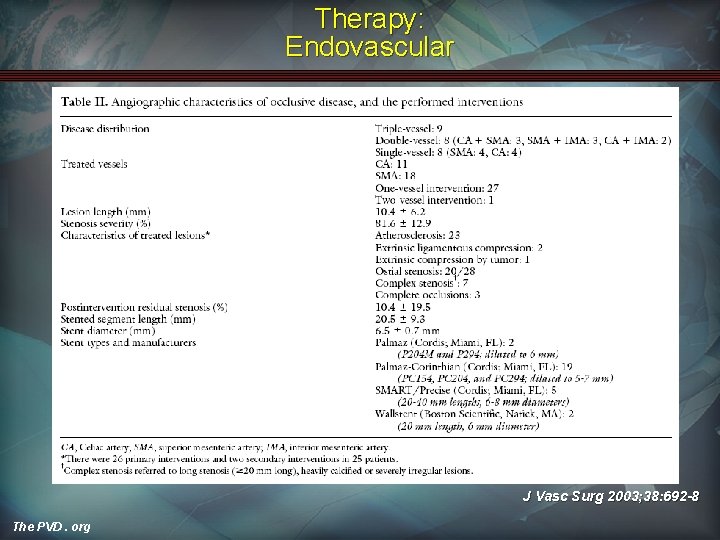
Therapy: Endovascular J Vasc Surg 2003; 38: 692 -8 The PVD. org
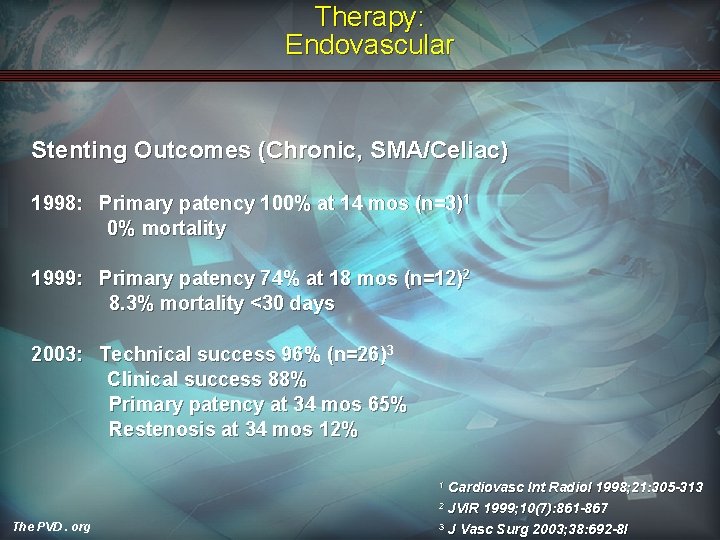
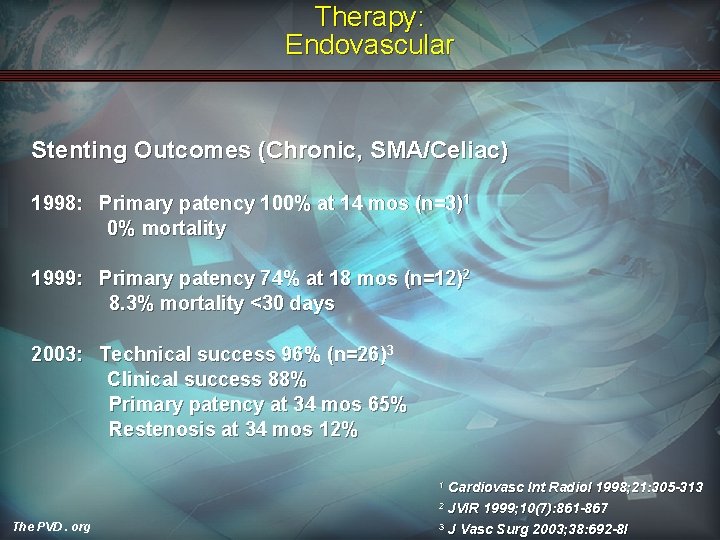
Therapy: Endovascular Stenting Outcomes (Chronic, SMA/Celiac) 1998: Primary patency 100% at 14 mos (n=3)1 0% mortality 1999: Primary patency 74% at 18 mos (n=12)2 8. 3% mortality <30 days 2003: Technical success 96% (n=26)3 Clinical success 88% Primary patency at 34 mos 65% Restenosis at 34 mos 12% Cardiovasc Int Radiol 1998; 21: 305 -313 2 JVIR 1999; 10(7): 861 -867 3 J Vasc Surg 2003; 38: 692 -8 I 1 The PVD. org
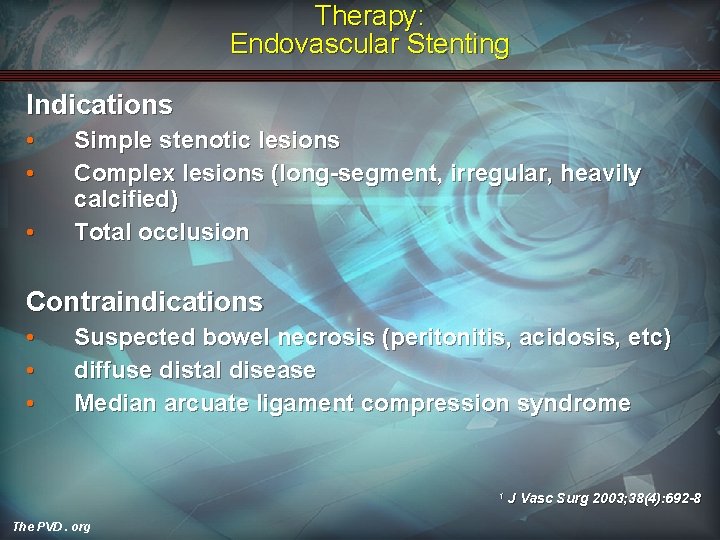
Therapy: Endovascular Stenting Indications • • • Simple stenotic lesions Complex lesions (long-segment, irregular, heavily calcified) Total occlusion Contraindications • • • Suspected bowel necrosis (peritonitis, acidosis, etc) diffuse distal disease Median arcuate ligament compression syndrome 1 The PVD. org J Vasc Surg 2003; 38(4): 692 -8
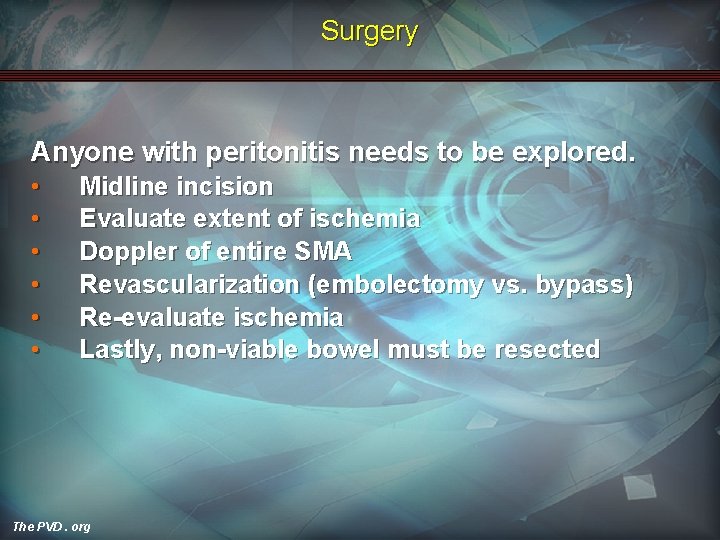
Surgery Anyone with peritonitis needs to be explored. • • • Midline incision Evaluate extent of ischemia Doppler of entire SMA Revascularization (embolectomy vs. bypass) Re-evaluate ischemia Lastly, non-viable bowel must be resected The PVD. org
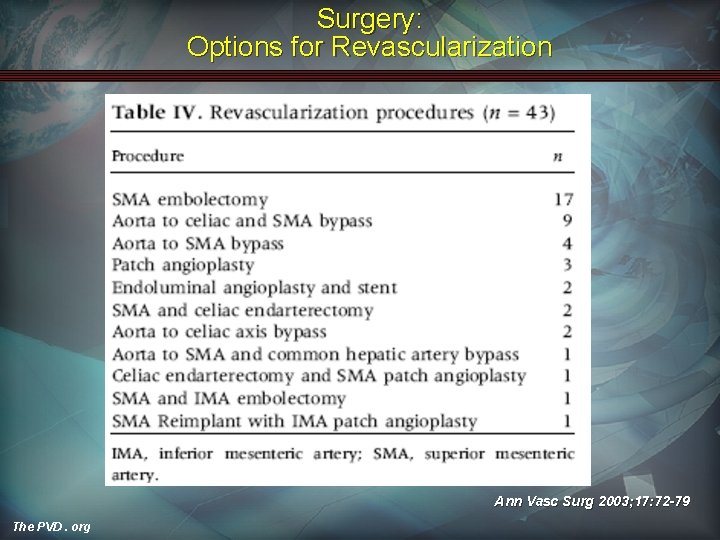
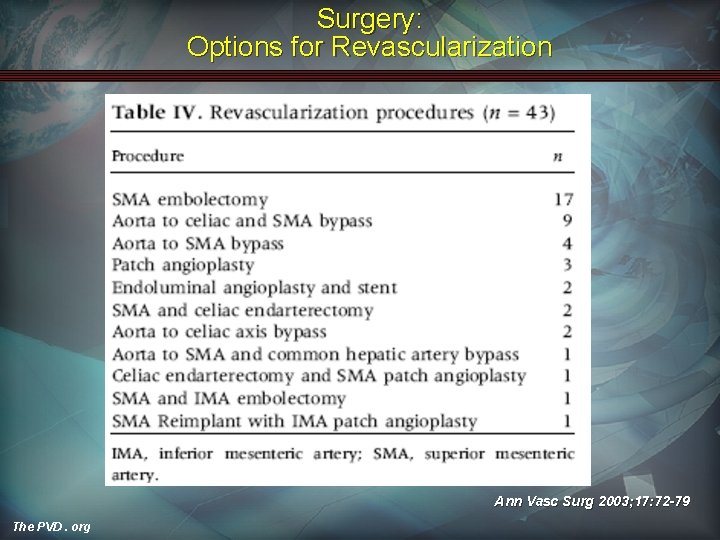
Surgery: Options for Revascularization Ann Vasc Surg 2003; 17: 72 -79 The PVD. org
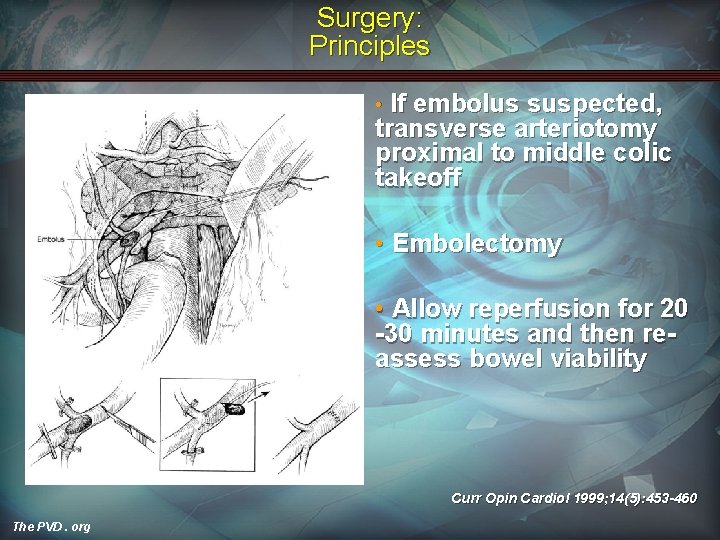
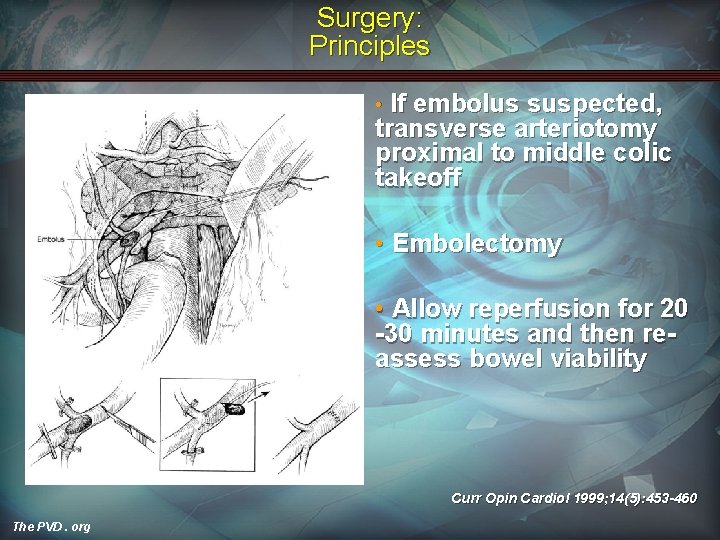
Surgery: Principles If embolus suspected, transverse arteriotomy proximal to middle colic takeoff • • Embolectomy • Allow reperfusion for 20 -30 minutes and then reassess bowel viability Curr Opin Cardiol 1999; 14(5): 453 -460 The PVD. org
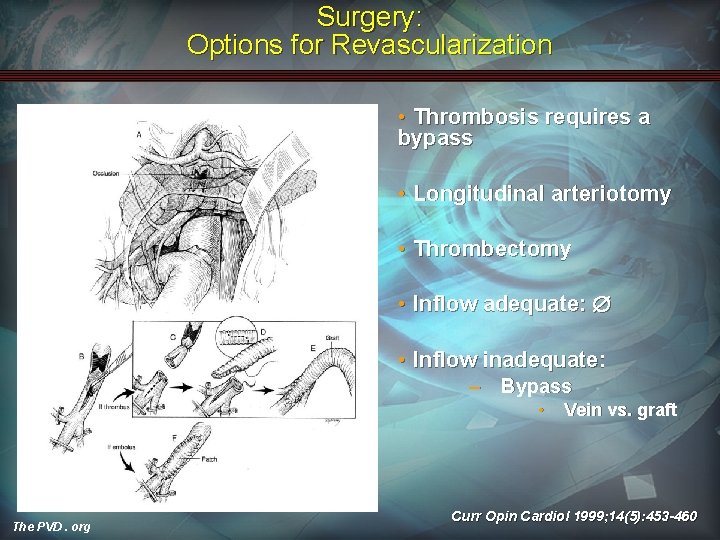
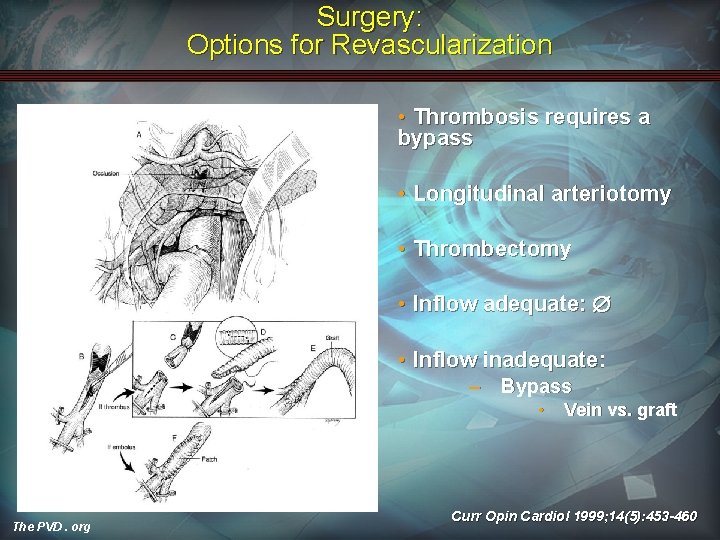
Surgery: Options for Revascularization • Thrombosis requires a bypass • Longitudinal arteriotomy • Thrombectomy • Inflow adequate: • Inflow inadequate: – Bypass • The PVD. org Vein vs. graft Curr Opin Cardiol 1999; 14(5): 453 -460
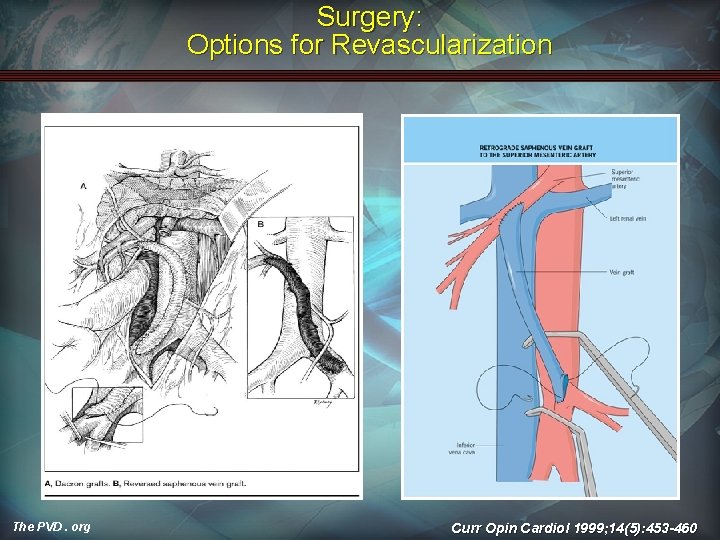
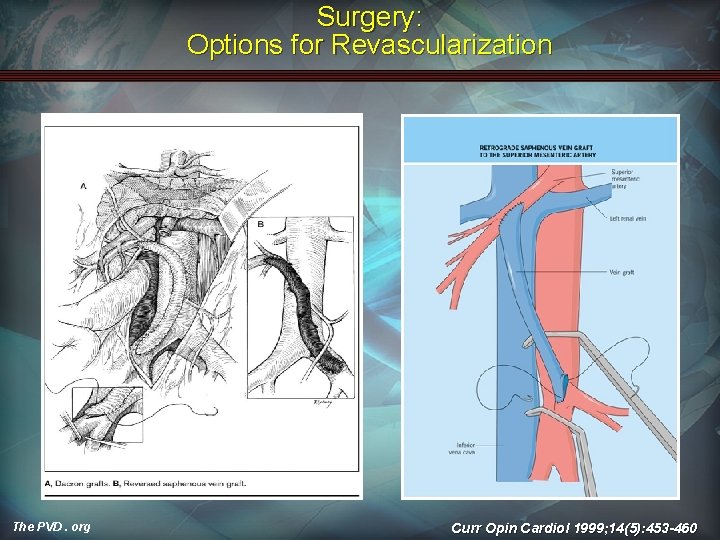
Surgery: Options for Revascularization The PVD. org Curr Opin Cardiol 1999; 14(5): 453 -460
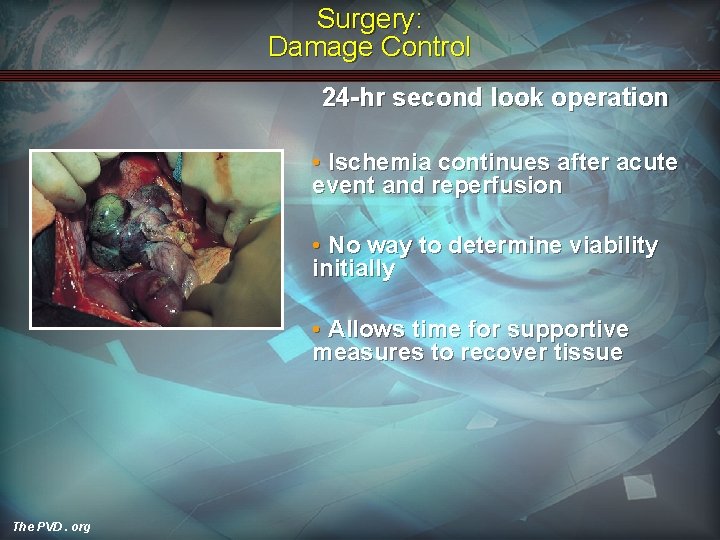
Surgery: Damage Control 24 -hr second look operation • Ischemia continues after acute event and reperfusion • No way to determine viability initially • Allows time for supportive measures to recover tissue The PVD. org

Surgery: Options Case Reports • Angiography + Laparoscopy The PVD. org
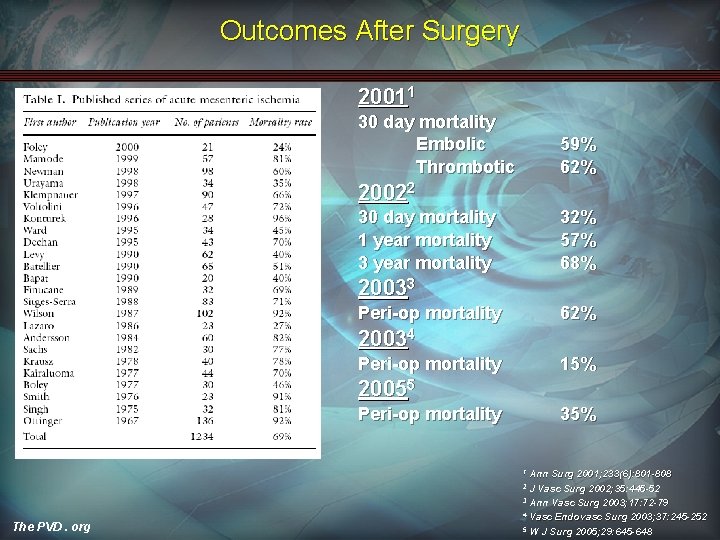
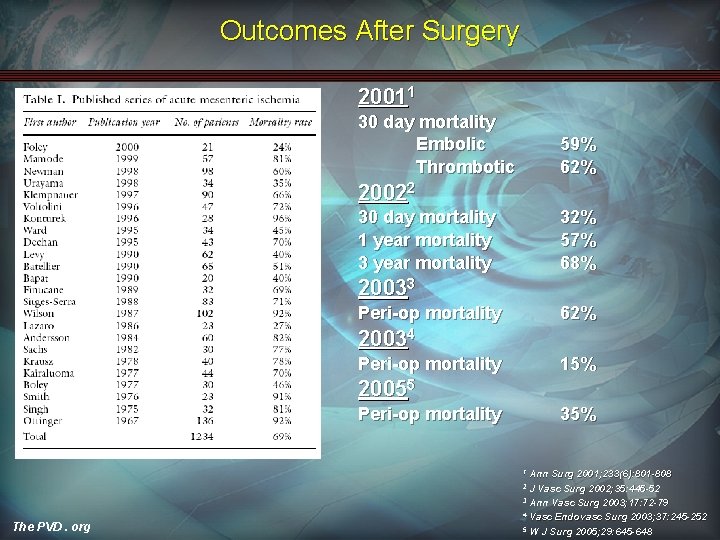
Outcomes After Surgery 20011 30 day mortality Embolic Thrombotic 59% 62% 20022 30 day mortality 1 year mortality 32% 57% 68% 20033 Peri-op mortality 62% 20034 Peri-op mortality 15% 20055 Peri-op mortality 35% Ann Surg 2001; 233(6): 801 -808 J Vasc Surg 2002; 35: 445 -52 3 Ann Vasc Surg 2003; 17: 72 -79 4 Vasc Endovasc Surg 2003; 37: 245 -252 5 W J Surg 2005; 29: 645 -648 1 2 The PVD. org
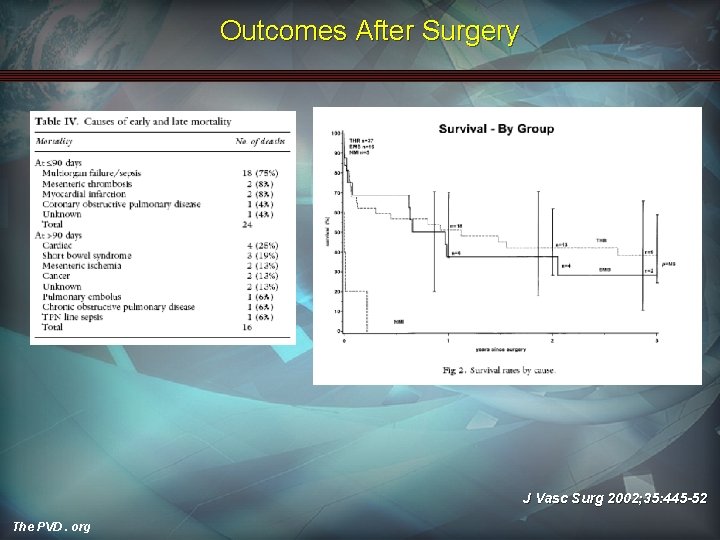
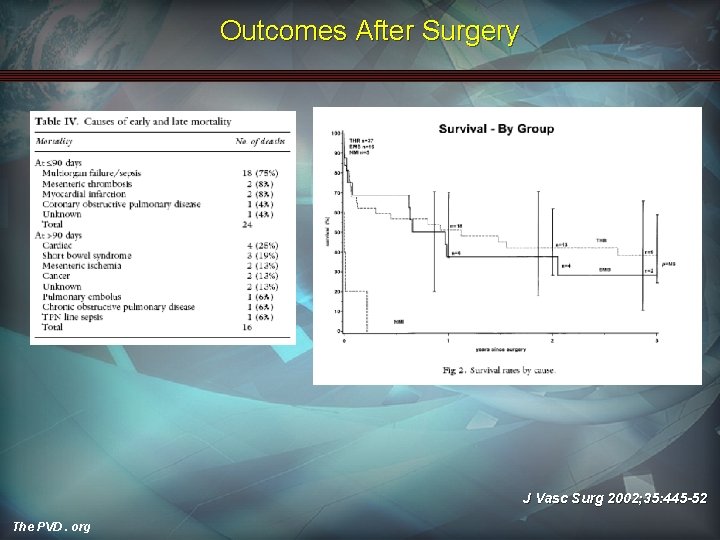
Outcomes After Surgery J Vasc Surg 2002; 35: 445 -52 The PVD. org
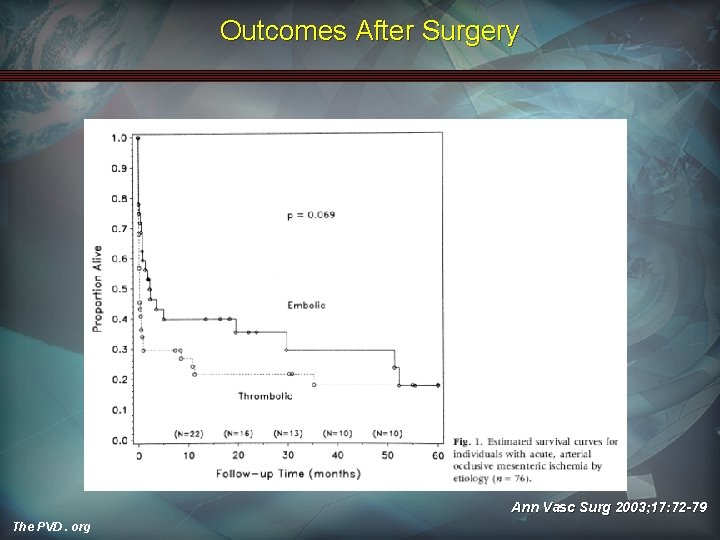
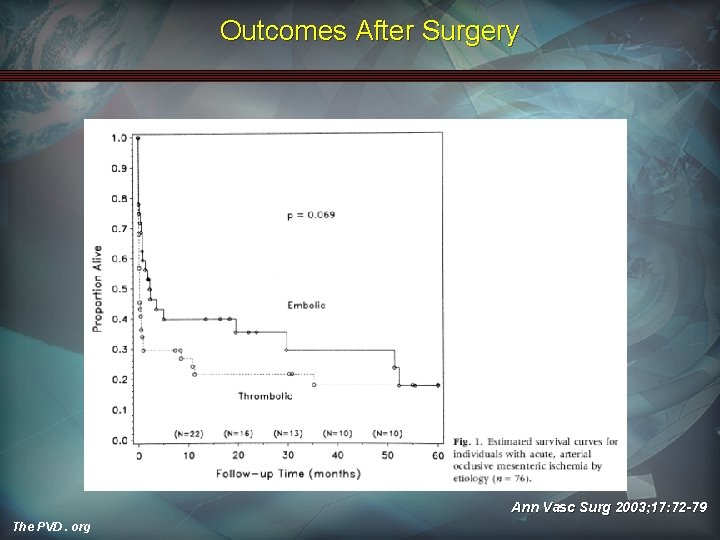
Outcomes After Surgery Ann Vasc Surg 2003; 17: 72 -79 The PVD. org
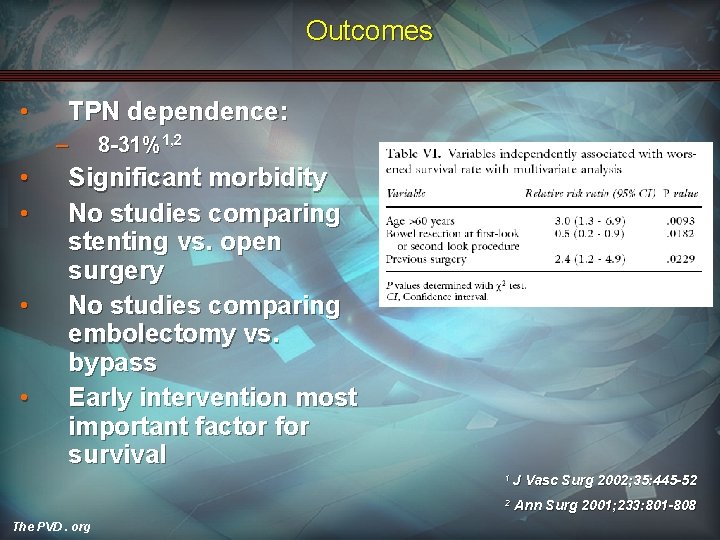
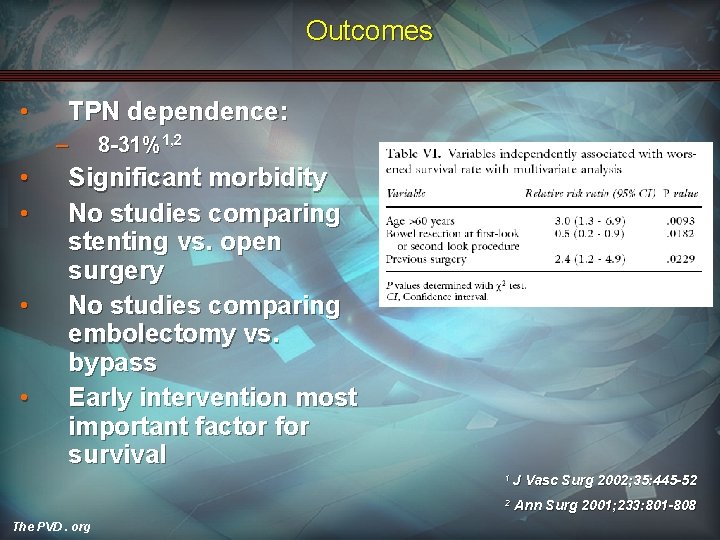
Outcomes • TPN dependence: – • • 8 -31%1, 2 Significant morbidity No studies comparing stenting vs. open surgery No studies comparing embolectomy vs. bypass Early intervention most important factor for survival 1 J 2 The PVD. org Vasc Surg 2002; 35: 445 -52 Ann Surg 2001; 233: 801 -808
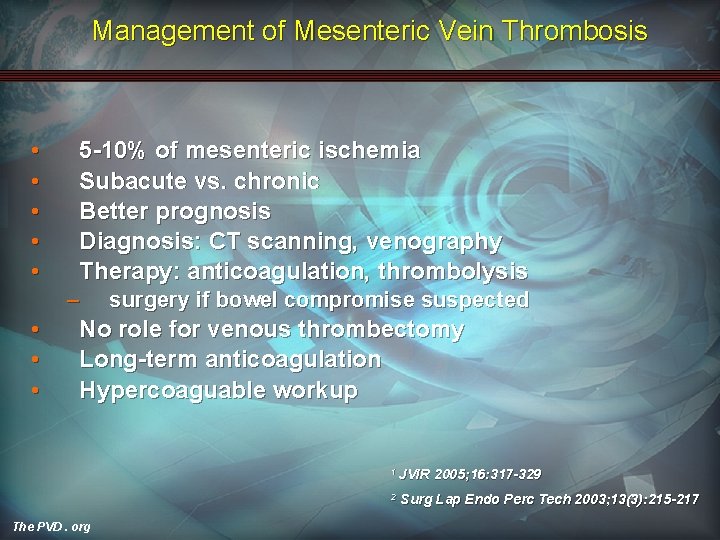
Management of Mesenteric Vein Thrombosis • • • 5 -10% of mesenteric ischemia Subacute vs. chronic Better prognosis Diagnosis: CT scanning, venography Therapy: anticoagulation, thrombolysis – • • • surgery if bowel compromise suspected No role for venous thrombectomy Long-term anticoagulation Hypercoaguable workup 1 JVIR 2 The PVD. org 2005; 16: 317 -329 Surg Lap Endo Perc Tech 2003; 13(3): 215 -217
What Should You Do? Supportive • • • IV heparin Broad-spectrum antibiotics Hemodynamic optimization ― Volume status ― Cardiac function The PVD. org
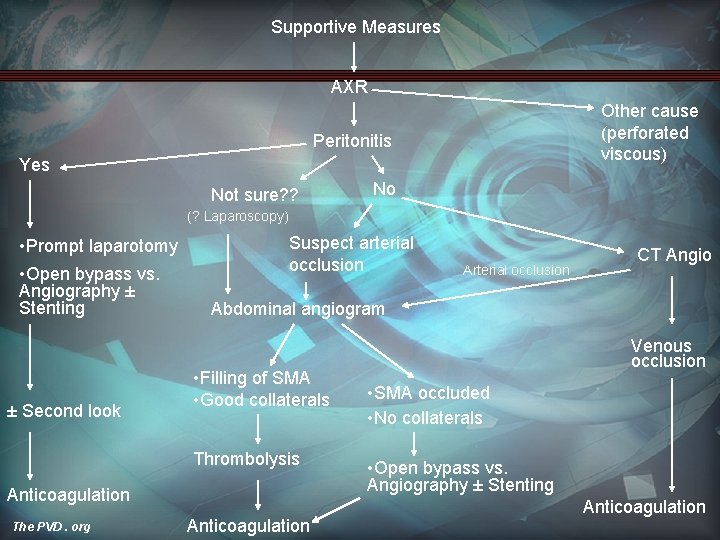
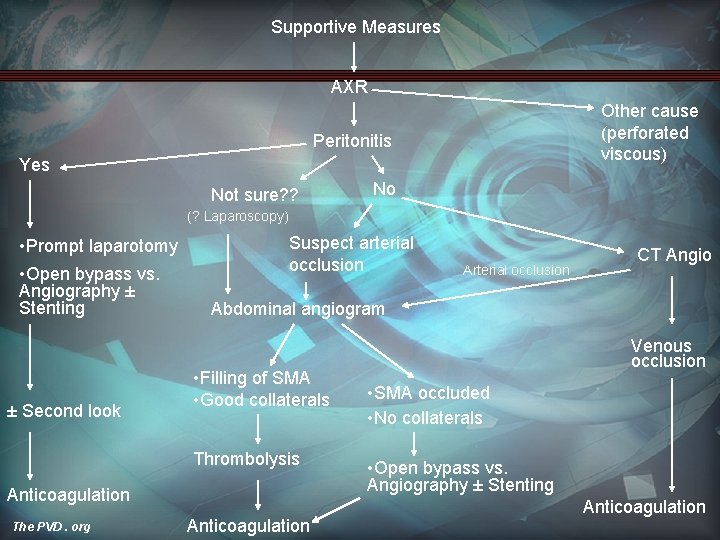
Supportive Measures AXR Other cause (perforated viscous) Peritonitis Yes Not sure? ? No (? Laparoscopy) • Prompt laparotomy • Open bypass vs. Angiography ± Stenting ± Second look Suspect arterial occlusion CT Angio Abdominal angiogram • Filling of SMA • Good collaterals Thrombolysis Anticoagulation The PVD. org Arterial occlusion Anticoagulation Venous occlusion • SMA occluded • No collaterals • Open bypass vs. Angiography ± Stenting Anticoagulation
 Myocardial ischemia meaning
Myocardial ischemia meaning Transmural ischemia
Transmural ischemia Ischemia acuta degli arti
Ischemia acuta degli arti What is ischemia guided strategy
What is ischemia guided strategy Anterior wall ischemia
Anterior wall ischemia Isaac george md
Isaac george md Lig teres hepatis
Lig teres hepatis Mesenteric arteriogram
Mesenteric arteriogram Omental appendices
Omental appendices Ligaments of the stomach
Ligaments of the stomach Origin of superior mesenteric artery
Origin of superior mesenteric artery Pre aortic lymph nodes
Pre aortic lymph nodes Upper mesenteric artery
Upper mesenteric artery Artery model labeled
Artery model labeled Diverticulosis
Diverticulosis Mesenteric root
Mesenteric root Mesenteric angiogram
Mesenteric angiogram The radial and ulnar veins merge to form the
The radial and ulnar veins merge to form the King george vs george washington
King george vs george washington John adams vs thomas jefferson venn diagram
John adams vs thomas jefferson venn diagram Resident lifecycle
Resident lifecycle Tarrytown chief resident conference
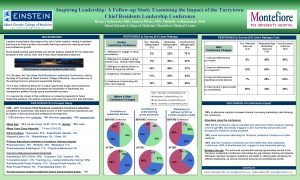
Tarrytown chief resident conference A helpful way for an na to respond to hallucinations is to
A helpful way for an na to respond to hallucinations is to Acgme resident survey
Acgme resident survey The working set strategy
The working set strategy Yelena bogdan
Yelena bogdan Define resident flora
Define resident flora Chapter 2 foundations of resident care
Chapter 2 foundations of resident care Transamerica estate planning foreign nationals
Transamerica estate planning foreign nationals Employment of non-resident aliens in the philippines
Employment of non-resident aliens in the philippines Taxpayer identifying number
Taxpayer identifying number Acgme survey questions
Acgme survey questions Magic mask
Magic mask Attending vs resident
Attending vs resident Chapter 10 positioning transfers and ambulation
Chapter 10 positioning transfers and ambulation Resident set management
Resident set management Resident and family engagement
Resident and family engagement Telephone 911
Telephone 911 Divine intervention episode 143
Divine intervention episode 143 Resident assessment instrument definition
Resident assessment instrument definition Misappropriation of resident property
Misappropriation of resident property Partially resident textures
Partially resident textures Resident retention
Resident retention Resident and family engagement
Resident and family engagement Ota core curriculum
Ota core curriculum What is conflict resolution in customer service
What is conflict resolution in customer service Caret drone
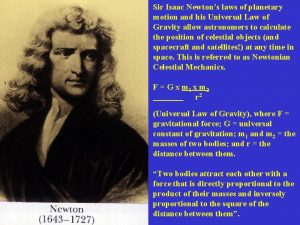
Caret drone Sir isaac newton
Sir isaac newton Biography isaac asimov
Biography isaac asimov Vector form of gravitational force
Vector form of gravitational force Who is this
Who is this Isaac babcock
Isaac babcock Colegio isaac ochoterena
Colegio isaac ochoterena Isaac meditating in the field
Isaac meditating in the field Neptunus isaac
Neptunus isaac Ley de la inercia y el cinturón de seguridad
Ley de la inercia y el cinturón de seguridad Isaac lustgarten
Isaac lustgarten Newton one of the greatest scientists
Newton one of the greatest scientists The fun they had theme
The fun they had theme