A New Look at Hydrops Fetalis Laura Klee
![Two Main Types of Hydrops Immune Hydrops [IHF] • Secondary to maternal RBC alloimmune Two Main Types of Hydrops Immune Hydrops [IHF] • Secondary to maternal RBC alloimmune](https://slidetodoc.com/presentation_image_h2/c6e6117a53fe0cb0b78b618f45373519/image-6.jpg)
![What causes hydrops • Disorder of fluid [distribution] management – Fluid overload – Severe What causes hydrops • Disorder of fluid [distribution] management – Fluid overload – Severe](https://slidetodoc.com/presentation_image_h2/c6e6117a53fe0cb0b78b618f45373519/image-11.jpg)
![Thoracic Disorders CPAM [CCAM] Congenital Pulmonary Airway Malformation Extra-pulmonary sequestration Congenital hydro or chylothorax Thoracic Disorders CPAM [CCAM] Congenital Pulmonary Airway Malformation Extra-pulmonary sequestration Congenital hydro or chylothorax](https://slidetodoc.com/presentation_image_h2/c6e6117a53fe0cb0b78b618f45373519/image-21.jpg)




![References Peebles, S. [UAMS] NICU management of Hydrops Fetalis. ANGELS Perinatal Conference. 2010. uams. References Peebles, S. [UAMS] NICU management of Hydrops Fetalis. ANGELS Perinatal Conference. 2010. uams.](https://slidetodoc.com/presentation_image_h2/c6e6117a53fe0cb0b78b618f45373519/image-53.jpg)
![References Yuan, S. The Application of ex utero intrapartum treatment [EXIT] procedure for cardiothoracic References Yuan, S. The Application of ex utero intrapartum treatment [EXIT] procedure for cardiothoracic](https://slidetodoc.com/presentation_image_h2/c6e6117a53fe0cb0b78b618f45373519/image-54.jpg)
![Lymph system Left side [thoracic duct] drains about 75% of the body Right side Lymph system Left side [thoracic duct] drains about 75% of the body Right side](https://slidetodoc.com/presentation_image_h2/c6e6117a53fe0cb0b78b618f45373519/image-56.jpg)
- Slides: 56
A New Look at Hydrops Fetalis Laura Klee RNC MSN
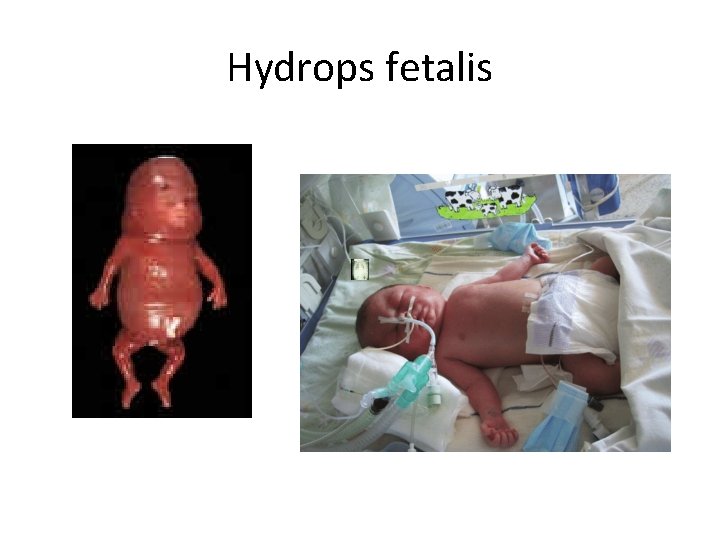
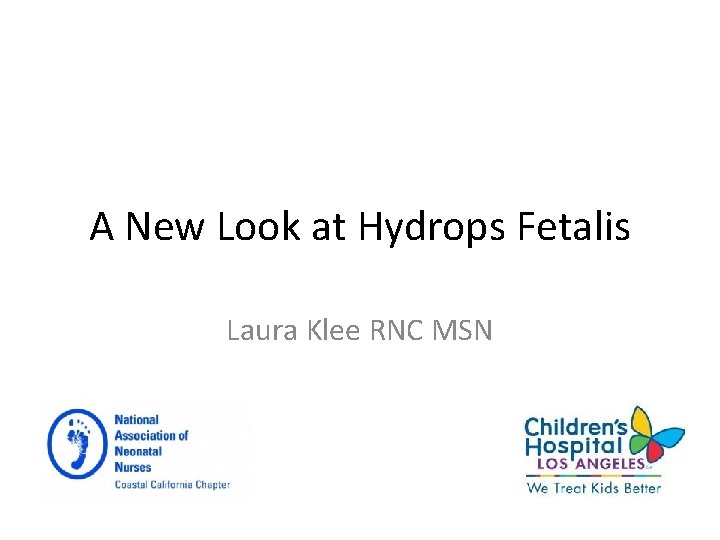
Hydrops fetalis
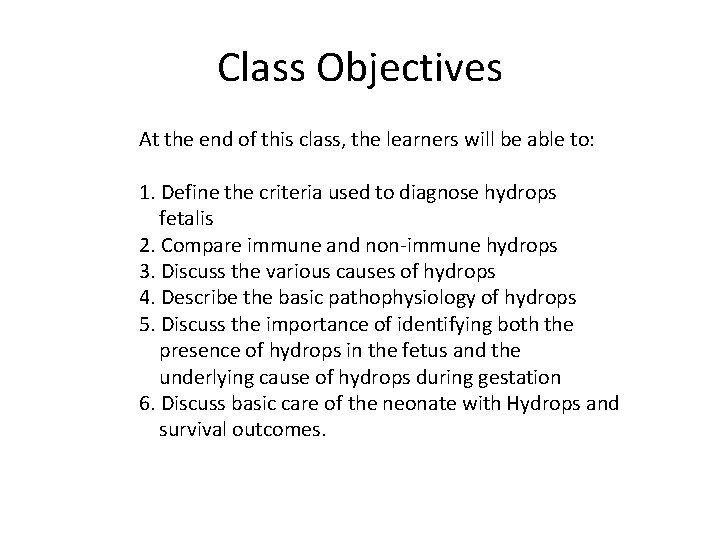
Class Objectives At the end of this class, the learners will be able to: 1. Define the criteria used to diagnose hydrops fetalis 2. Compare immune and non-immune hydrops 3. Discuss the various causes of hydrops 4. Describe the basic pathophysiology of hydrops 5. Discuss the importance of identifying both the presence of hydrops in the fetus and the underlying cause of hydrops during gestation 6. Discuss basic care of the neonate with Hydrops and survival outcomes.
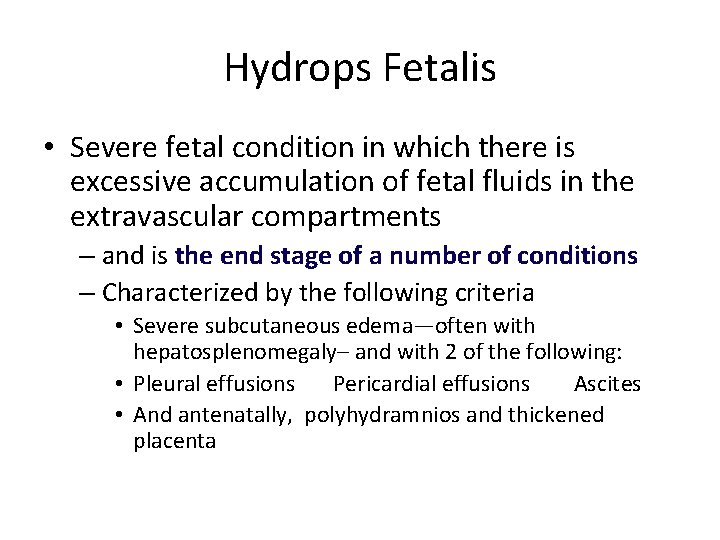
Hydrops Fetalis • Severe fetal condition in which there is excessive accumulation of fetal fluids in the extravascular compartments – and is the end stage of a number of conditions – Characterized by the following criteria • Severe subcutaneous edema—often with hepatosplenomegaly– and with 2 of the following: • Pleural effusions Pericardial effusions Ascites • And antenatally, polyhydramnios and thickened placenta
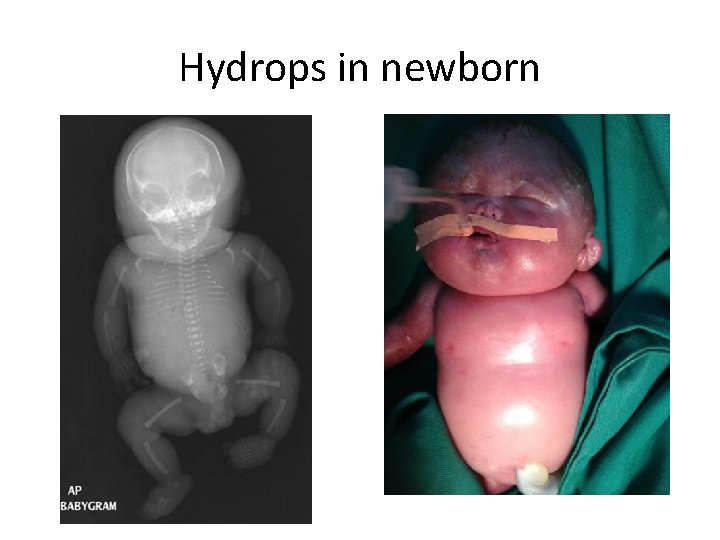
Hydrops in newborn
![Two Main Types of Hydrops Immune Hydrops IHF Secondary to maternal RBC alloimmune Two Main Types of Hydrops Immune Hydrops [IHF] • Secondary to maternal RBC alloimmune](https://slidetodoc.com/presentation_image_h2/c6e6117a53fe0cb0b78b618f45373519/image-6.jpg)
Two Main Types of Hydrops Immune Hydrops [IHF] • Secondary to maternal RBC alloimmune response to fetal antigens • Mother develops sensitization to paternally* derived antigens on fetal RBCs [Rh (D and E), and rarely Kell, Duffy/Fya, Kidd/ Jka and ABO] • Antibodies produced cross the placenta and attack/lyse fetal RBCs resulting in severe anemia and CHF • New reports also implicate IV drug abusers who share needles becoming inadvertently sensitized • This used to be the main cause of hydrops, but is no longer the most common cause
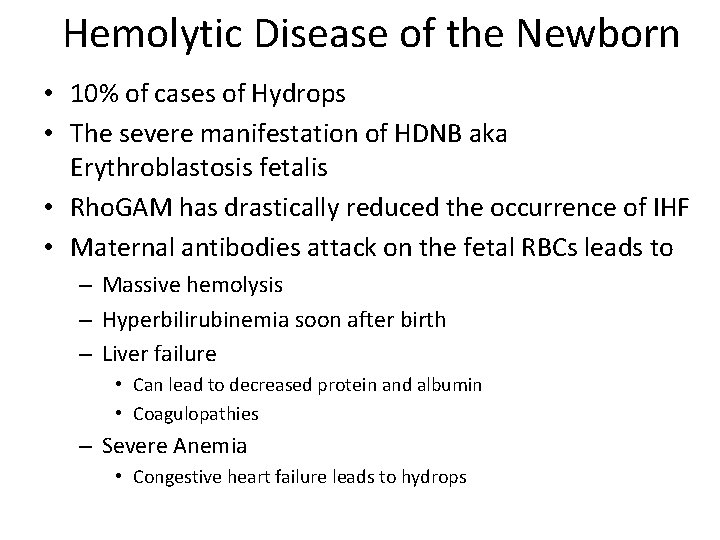
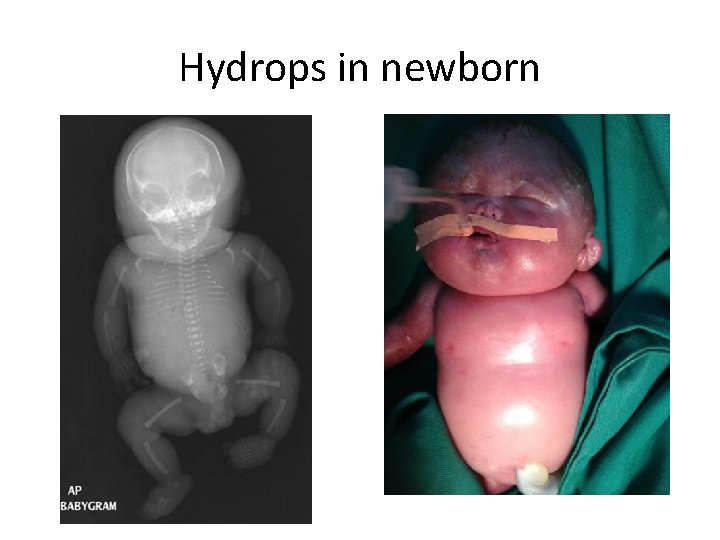
Hemolytic Disease of the Newborn • 10% of cases of Hydrops • The severe manifestation of HDNB aka Erythroblastosis fetalis • Rho. GAM has drastically reduced the occurrence of IHF • Maternal antibodies attack on the fetal RBCs leads to – Massive hemolysis – Hyperbilirubinemia soon after birth – Liver failure • Can lead to decreased protein and albumin • Coagulopathies – Severe Anemia • Congestive heart failure leads to hydrops
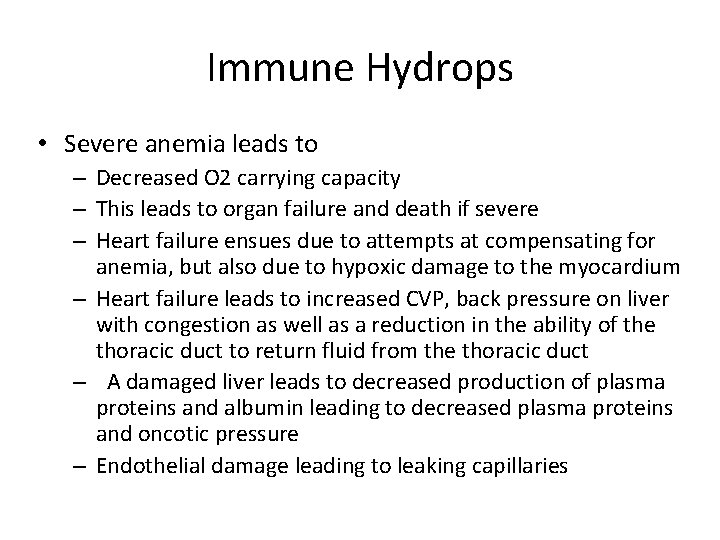
Immune Hydrops • Severe anemia leads to – Decreased O 2 carrying capacity – This leads to organ failure and death if severe – Heart failure ensues due to attempts at compensating for anemia, but also due to hypoxic damage to the myocardium – Heart failure leads to increased CVP, back pressure on liver with congestion as well as a reduction in the ability of the thoracic duct to return fluid from the thoracic duct – A damaged liver leads to decreased production of plasma proteins and albumin leading to decreased plasma proteins and oncotic pressure – Endothelial damage leading to leaking capillaries
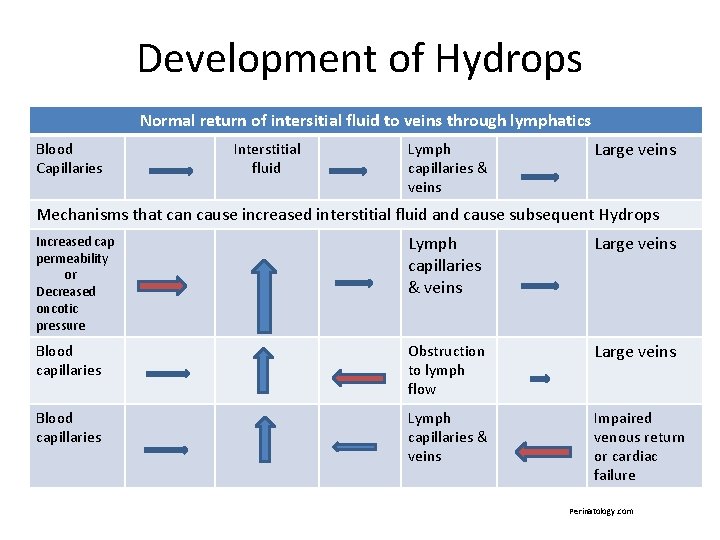
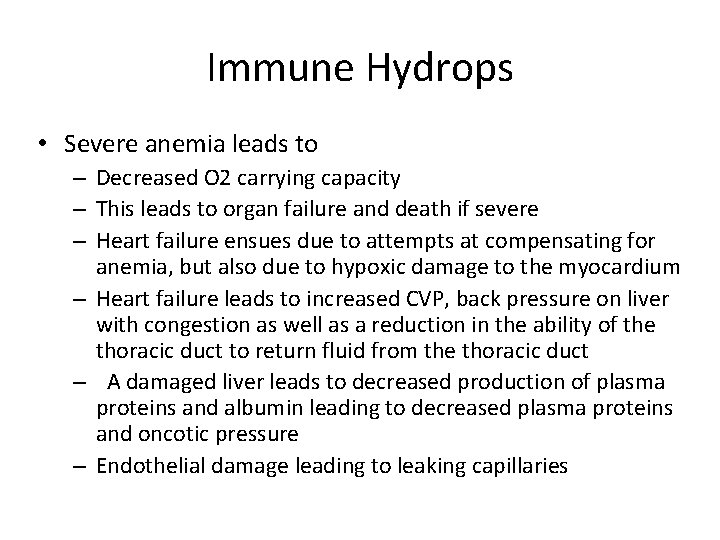
Development of Hydrops Normal return of intersitial fluid to veins through lymphatics Blood Capillaries Interstitial fluid Lymph capillaries & veins Large veins Mechanisms that can cause increased interstitial fluid and cause subsequent Hydrops Increased cap permeability or Decreased oncotic pressure Lymph capillaries & veins Large veins Blood capillaries Obstruction to lymph flow Large veins Blood capillaries Lymph capillaries & veins Impaired venous return or cardiac failure Perinatology. com
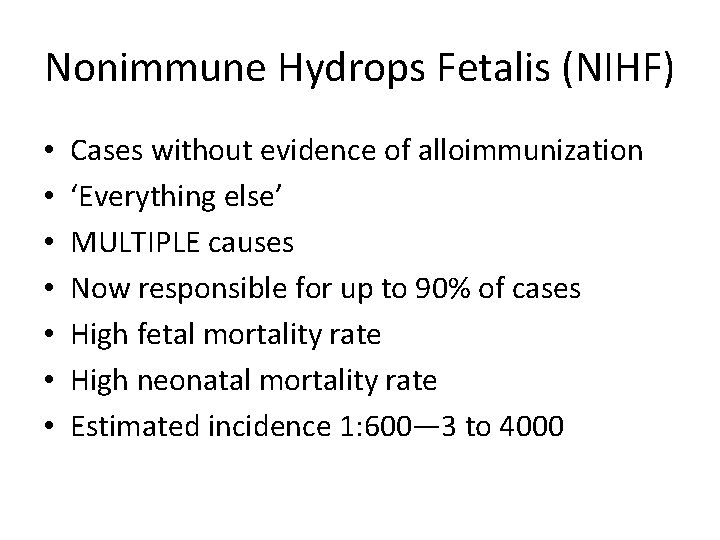
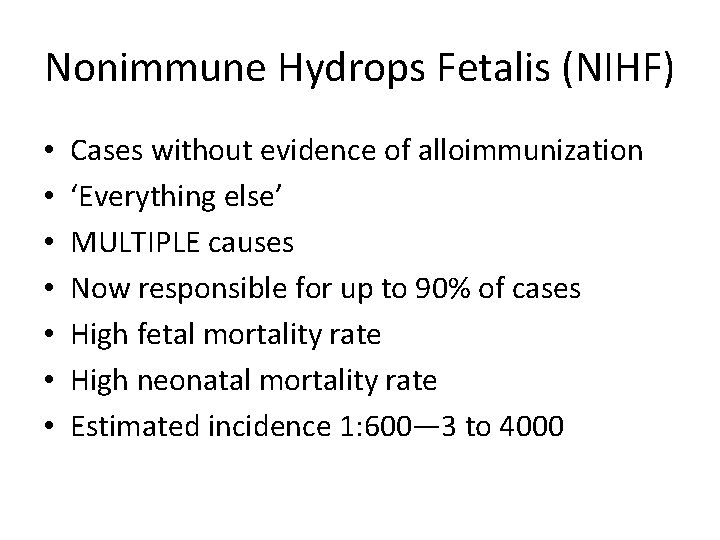
Nonimmune Hydrops Fetalis (NIHF) • • Cases without evidence of alloimmunization ‘Everything else’ MULTIPLE causes Now responsible for up to 90% of cases High fetal mortality rate High neonatal mortality rate Estimated incidence 1: 600— 3 to 4000
![What causes hydrops Disorder of fluid distribution management Fluid overload Severe What causes hydrops • Disorder of fluid [distribution] management – Fluid overload – Severe](https://slidetodoc.com/presentation_image_h2/c6e6117a53fe0cb0b78b618f45373519/image-11.jpg)
What causes hydrops • Disorder of fluid [distribution] management – Fluid overload – Severe anemia – Severe hypoxemia, especially ischemic/anoxic injury to the heart and liver – Which causes cardiac failure and increased CVP – Liver failure – Decreased oncotic pressure – Increased vascular permeability – Interference with lymphatic removal of fluid and return to the heart
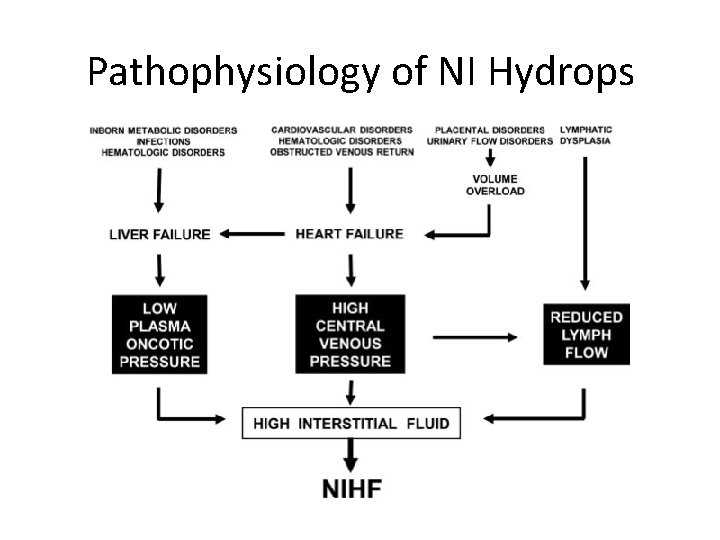
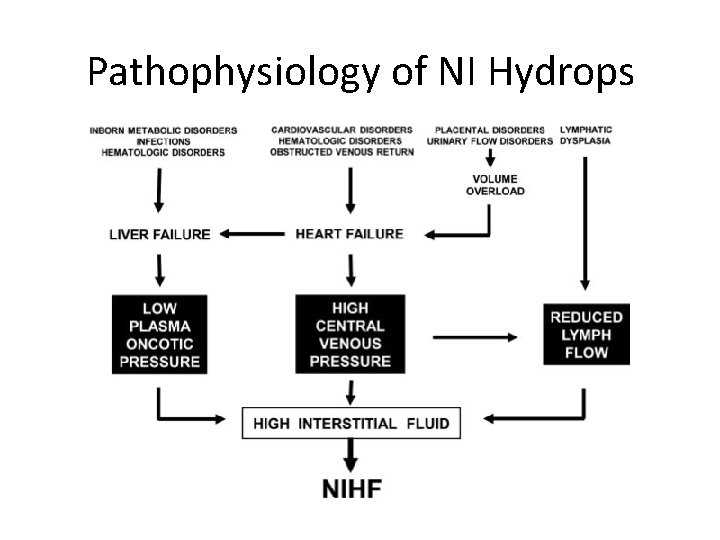
Pathophysiology of NI Hydrops
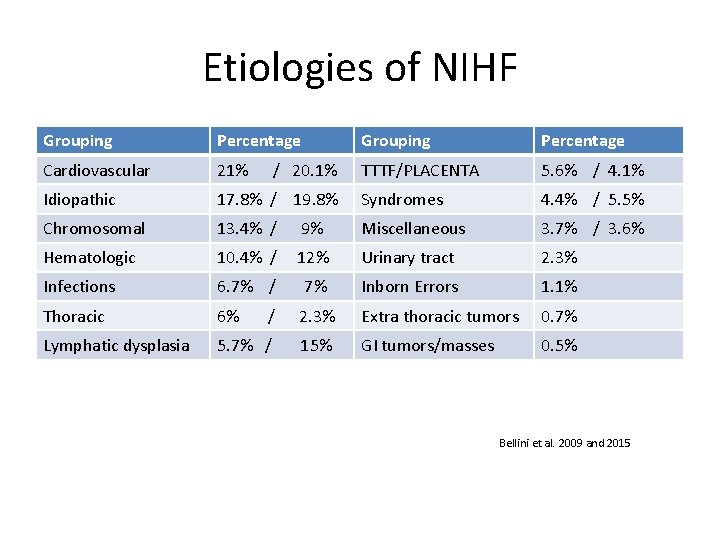
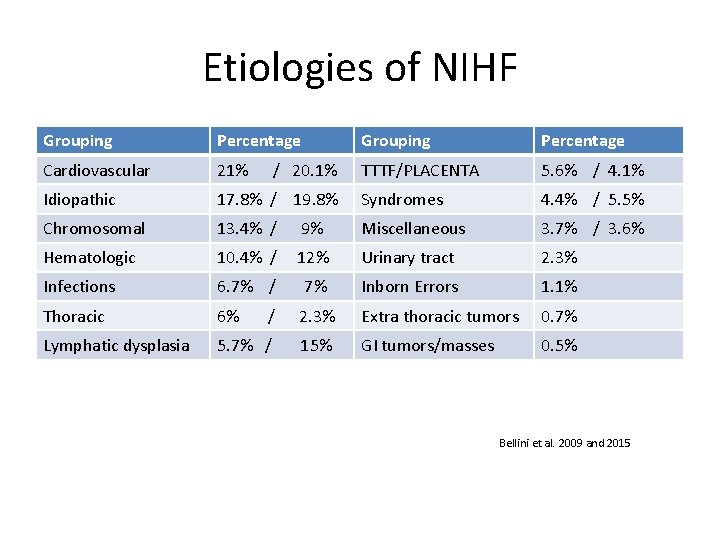
Etiologies of NIHF Grouping Percentage Cardiovascular 21% TTTF/PLACENTA 5. 6% / 4. 1% Idiopathic 17. 8% / 19. 8% Syndromes 4. 4% / 5. 5% Chromosomal 13. 4% / 9% Miscellaneous 3. 7% / 3. 6% Hematologic 10. 4% / 12% Urinary tract 2. 3% Infections 6. 7% / 7% Inborn Errors 1. 1% Thoracic 6% / 2. 3% Extra thoracic tumors 0. 7% Lymphatic dysplasia 5. 7% / 15% GI tumors/masses 0. 5% / 20. 1% Bellini et al. 2009 and 2015
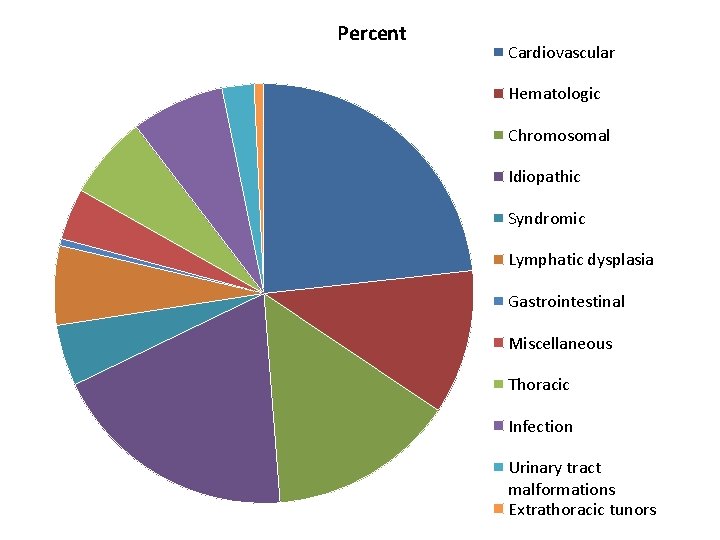
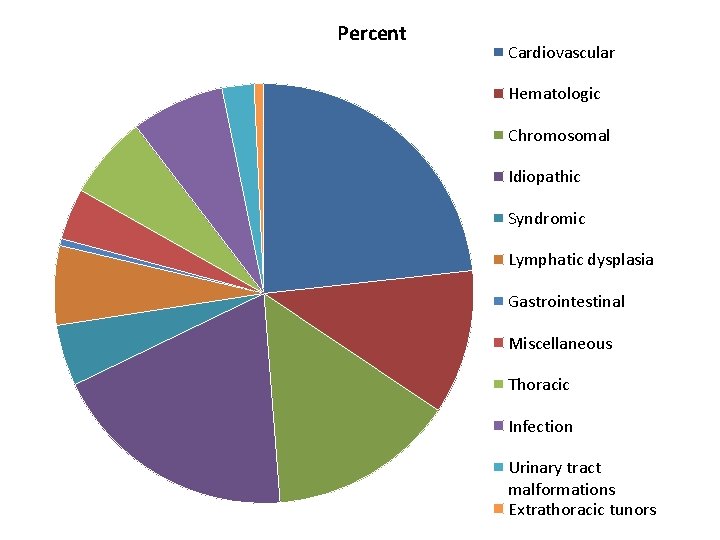
Percent Cardiovascular Hematologic Chromosomal Idiopathic Syndromic Lymphatic dysplasia Gastrointestinal Miscellaneous Thoracic Infection Urinary tract malformations Extrathoracic tunors
Cardiac causes of NIHF • • • Responsible for about 1 in 5 cases of NIHF Both right and left sided CHD Systolic and/or diastolic overload conditions High output conditions Congestive heart failure conditions Impaired Right heart filling conditions – Thrombosis – Tumors – Cystic hygroma
Causes of NIHF • Cardiac – – – – – Complex CHDs. Including heterotaxy syndrome Arrhythmias, especially tachyarrythmias like SVT Complete Heart block Maternal SLE etc. which can cause immune mediated damage of the fetal heart causing arrhythmias and heart block Myocarditis Cardiomyopathy Endocardial fibro elastosis Notably anything that obstructs blood flow and results in cardiac failure, right atrial enlargement, right heart failure with increased CVP/preload Arterial calcification Intracardiac tumors (intrapericardial teratoma, rhabdomyoma…)
Causes of NIHF • Vascular defects – Arteriovenous malformations – Diffuse hemangiomatosis – Placental, umbilical cord, abdominal, liver, etc. hemangiomas – SVC or IVC occlusion – Absent ductus venosus – Umbilical torsion – Tumors causing external compression
Chromosomal Disorders • • • Beckwith Wiedemann (trisomy 11 p 21) Cri du chat (chromosomes 4 and 5) Opitz G syndrome (5 p duplication) Trisomies 10 mosaic, 13, 18, 21 Turners (45 XO) Common threads in this disparate group: – – – Severe CHD Disorders of lymph drainage AV malformations Impaired production of functional RBCs Presence of thoracic or abdominal masses that impair venous return
Hematologic causes of NIHF • Hemoglobinopathies • Alpha thalassemia – – – – – No normal alpha hemoglobin chains Destroys oxygen release at normal physiologic levels Results in extreme hypoxia Fetal demise common Neonates with congestive heart failure, ascites, edema, hepatospenomegaly, prenatal and post natal asphyxia. Reliant on repetitive transfusions with risks for contracting blood borne infections, and developing iron overload Might benefit from stem cell transplant Was universally fatal until in utero diagnosis and repeated in utero transfusions became available With transfusions, chelation therapy for iron overload, and advent of stem cell transplant, the mortality rate is dropping
Causes of NIHF Infectious • Maternal/fetal infections TORCHES+ CLAP – Toxoplasmosis Chickenpox – Rubella Lyme disease – CMV AIDS – Herpes simplex Parvovirus B 19* – Enterovirus – Syphilis – Lymphocytic choriomeningitis virus (from rat vector)
![Thoracic Disorders CPAM CCAM Congenital Pulmonary Airway Malformation Extrapulmonary sequestration Congenital hydro or chylothorax Thoracic Disorders CPAM [CCAM] Congenital Pulmonary Airway Malformation Extra-pulmonary sequestration Congenital hydro or chylothorax](https://slidetodoc.com/presentation_image_h2/c6e6117a53fe0cb0b78b618f45373519/image-21.jpg)
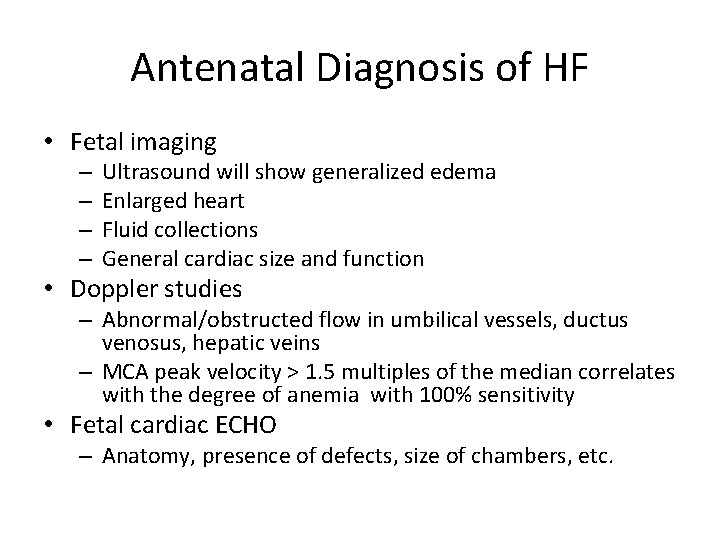
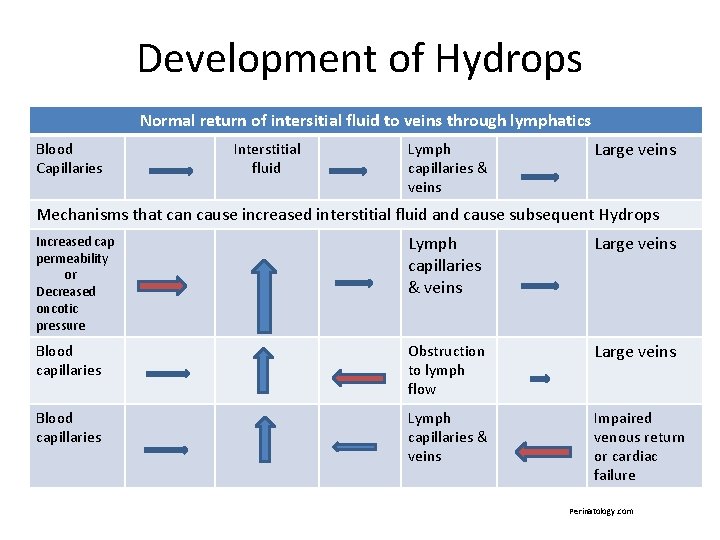
Thoracic Disorders CPAM [CCAM] Congenital Pulmonary Airway Malformation Extra-pulmonary sequestration Congenital hydro or chylothorax Mediastinal tumors Constricting/restricting thoracic dystrophies associated with skeletal dysplasias • AVMs and cystic hygromas in the neck/chest • CDH • CHAOS [Congenital high airway obstruction] • • •
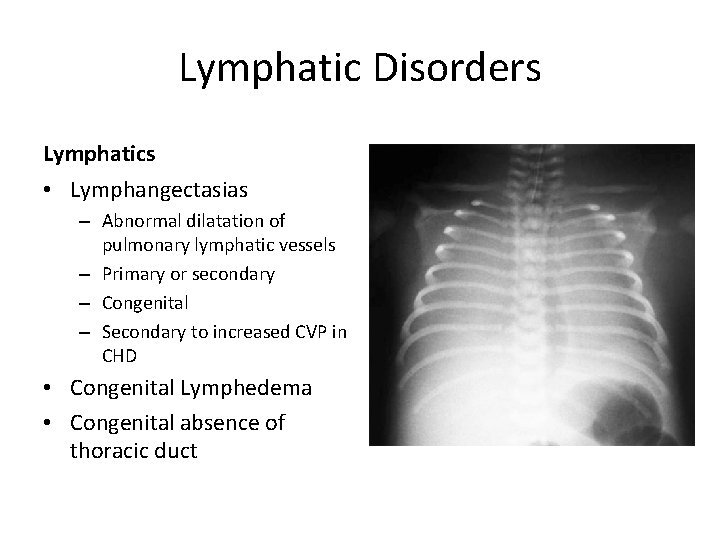
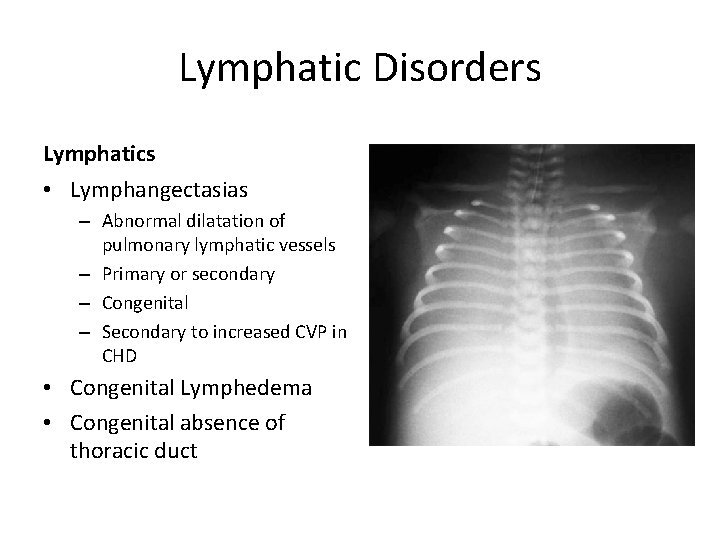
Lymphatic Disorders Lymphatics • Lymphangectasias – Abnormal dilatation of pulmonary lymphatic vessels – Primary or secondary – Congenital – Secondary to increased CVP in CHD • Congenital Lymphedema • Congenital absence of thoracic duct
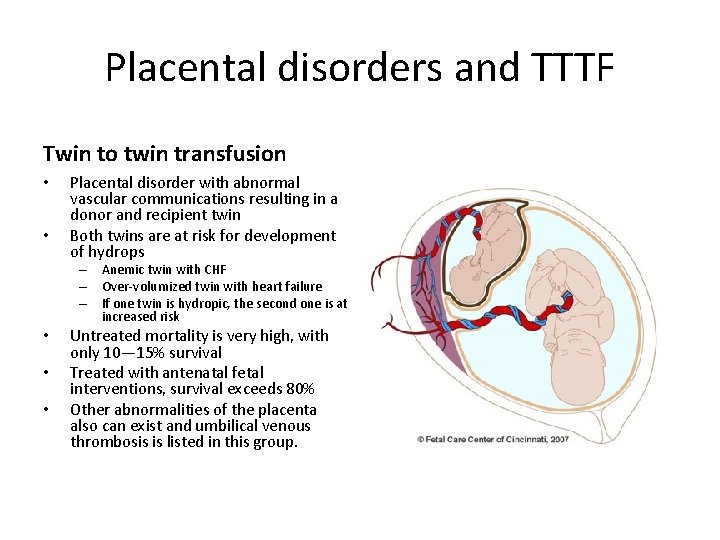
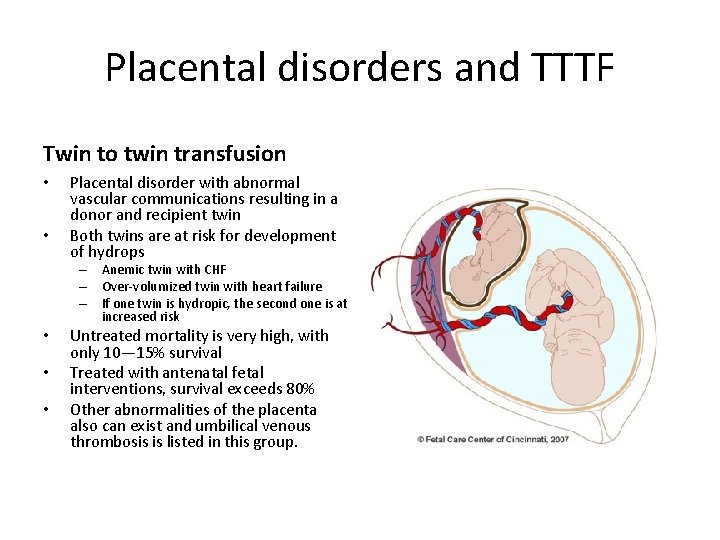
Placental disorders and TTTF Twin to twin transfusion • • Placental disorder with abnormal vascular communications resulting in a donor and recipient twin Both twins are at risk for development of hydrops – Anemic twin with CHF – Over-volumized twin with heart failure – If one twin is hydropic, the second one is at increased risk • • • Untreated mortality is very high, with only 10— 15% survival Treated with antenatal fetal interventions, survival exceeds 80% Other abnormalities of the placenta also can exist and umbilical venous thrombosis is listed in this group.
Genetic syndromes • • • Select achondroplasias Arthrogryposis multiplex congenita Eagle Barrett Syndrome (prune belly) Fryn’s syndrome Lethal short limbed dwarfism Noonan syndrome* Smith Lemli Opitz syndrome Tuberous sclerosis* Myotonic dystrophy* Most of the above are autosomal recessive with 25% recurrence risk. (* Autosomal dominant)
Metabolic/Inborn Errors of Metabolism • • Lysosomal storage disorders(10/50 types) Glycogen storage disorders Mucopolysaccharidosis type IV-A and Hurlers Niemann Pick Disease Salla Disease Hypo and Hyperthyroidism Carnitine deficiency Mitochondrial disorders
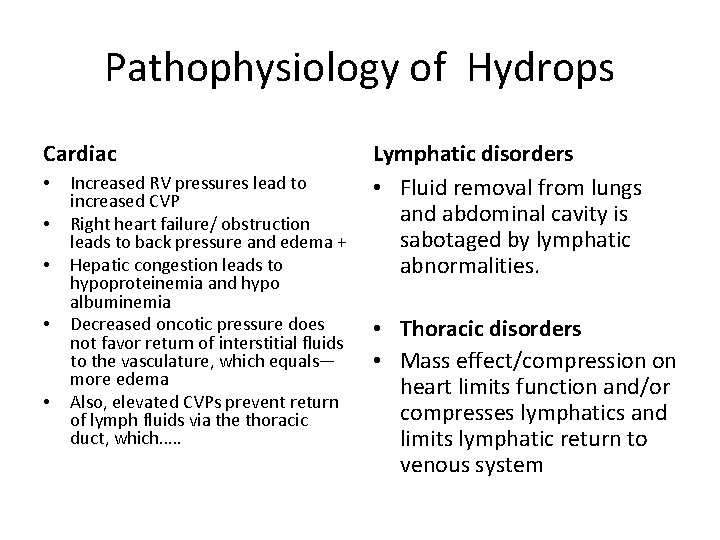
Pathophysiology of Hydrops Cardiac • • • Increased RV pressures lead to increased CVP Right heart failure/ obstruction leads to back pressure and edema + Hepatic congestion leads to hypoproteinemia and hypo albuminemia Decreased oncotic pressure does not favor return of interstitial fluids to the vasculature, which equals— more edema Also, elevated CVPs prevent return of lymph fluids via the thoracic duct, which…. . Lymphatic disorders • Fluid removal from lungs and abdominal cavity is sabotaged by lymphatic abnormalities. • Thoracic disorders • Mass effect/compression on heart limits function and/or compresses lymphatics and limits lymphatic return to venous system
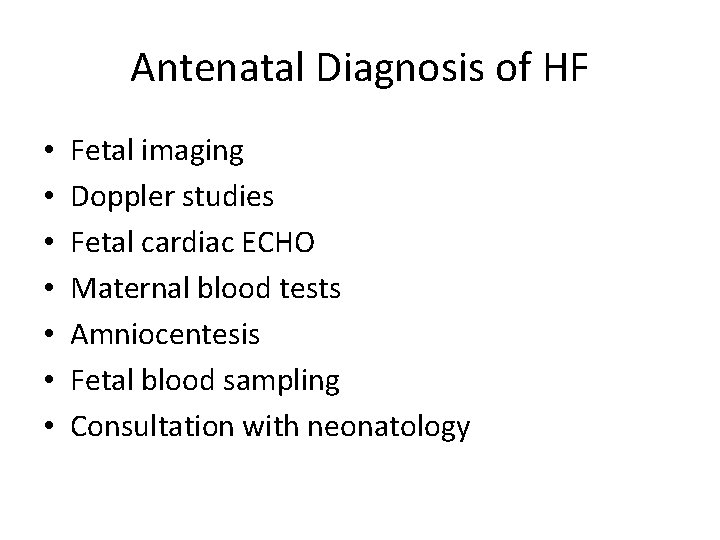
Antenatal Diagnosis of HF • • Fetal imaging Doppler studies Fetal cardiac ECHO Maternal blood tests Amniocentesis Fetal blood sampling Consultation with neonatology
Antenatal Diagnosis of HF • Fetal imaging – – Ultrasound will show generalized edema Enlarged heart Fluid collections General cardiac size and function • Doppler studies – Abnormal/obstructed flow in umbilical vessels, ductus venosus, hepatic veins – MCA peak velocity > 1. 5 multiples of the median correlates with the degree of anemia with 100% sensitivity • Fetal cardiac ECHO – Anatomy, presence of defects, size of chambers, etc.
Antenatal Diagnosis of HF • Maternal blood tests – – – CBC, indirect Coombs Kleihauer-Betke test [tests for fetal RCs in mother] TORCH etc. cultures, PCRs, Acute phase titers SSA and SSB antibodies [arrhythmias] Fetal electrophoresis (Southeast Asia) G 6 PD deficiency testing • Amniocentesis – – Cell retrieval for culture and genetic testing FISH, karyotype, microarray DNA for Alpha thalassemia Fetal lung maturity testing
Antenatal Diagnosis of HF • Fetal blood sampling – CBC and direct Coombs – Blood typing – Karyotyping, genetic testing – TORCH and viral serology – Protein and albumin levels – LFTs – Hemoglobin electrophoresis prn • Consultation with high risk perinatology and neonatology

Diagnostic Considerations Etiology matters Determines prognosis and management Treatments available for some of the causes Predicts future recurrence in families Provides knowledge to parents to facilitate informed consent • Fetal interventions do come with risk • Mirror syndrome may necessitate IMMEDIATE delivery • • •
Mirror syndrome • Ballantyne Syndrome • Development of severe edema in the mother carrying a hydropic fetus and placenta • Seems to manifest when fetal hydrops is worsening/progressing to fatal hydrops • Associated with mild albuminuria and hypertension • Rarely associated with pre ecclampsia • Etiology is not understood • May necessitate early delivery • Is often associated with fetal demise •
Available fetal therapy • • Anti arrhythmia drugs for fetal arrhythmias Fetal cardioversion or pacing In utero transfusion for anemia Drainage of cystic CPAM lesions with Cyst to amniotic shunt – Rh incompatibility, alpha thalassemia, and Parvo B 19 • Drainage or shunting procedures for pleural or cardiac effusion or ascites – If aspirated: sent for lymphocyte count, protein and albumin levels, PCR and cultures, ascites fluid sent for creatinine and ionogram • Placental laser therapy or ablation therapy for shared blood vessels in twin to twin transfusion syndrome • Antibiotic or antiviral therapy
Fetal Therapy Risks • Maternal antiarrhythmic drugs can cause complications in mother – Digoxin, Furosemide, Amiodarone, Adenosine, Procainamide, Flecainide, Sotolol and Verapamil • Fetal administration of drugs is invasive • Infection, hemorrhage and fetal demise can occur with all invasive procedures • Many fetal therapies have little clinical evidence and are based on small case series
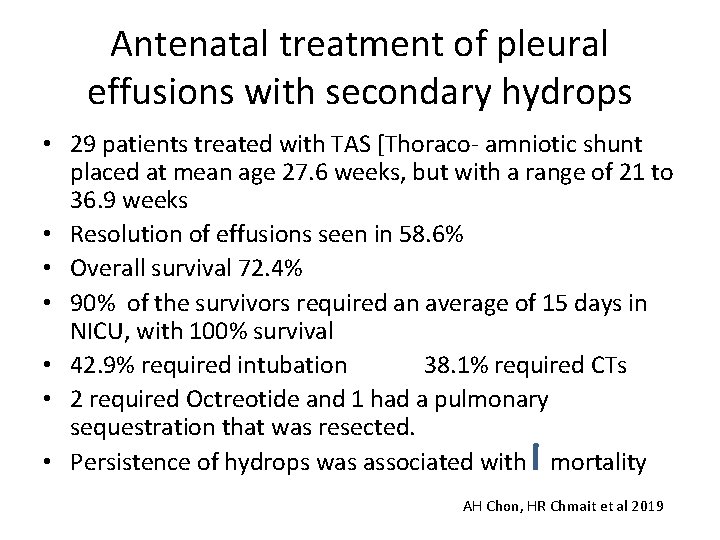
Antenatal treatment of pleural effusions with secondary hydrops • 29 patients treated with TAS [Thoraco- amniotic shunt placed at mean age 27. 6 weeks, but with a range of 21 to 36. 9 weeks • Resolution of effusions seen in 58. 6% • Overall survival 72. 4% • 90% of the survivors required an average of 15 days in NICU, with 100% survival • 42. 9% required intubation 38. 1% required CTs • 2 required Octreotide and 1 had a pulmonary sequestration that was resected. • Persistence of hydrops was associated with mortality AH Chon, HR Chmait et al 2019

EXIT Procedures for Hydrops • Ex utero intrapartum treatment • Partial delivery with placental circulation as bypass • CHAOS with Hydrops – Congenital high airway obstruction syndrome • Unilateral or bilateral pleural effusions with hydrops – Placement of pleural drains prior to intubation and ventilation • CPAM – Removal of large cyst – Subsequent to fetal intervention with displaced shunts
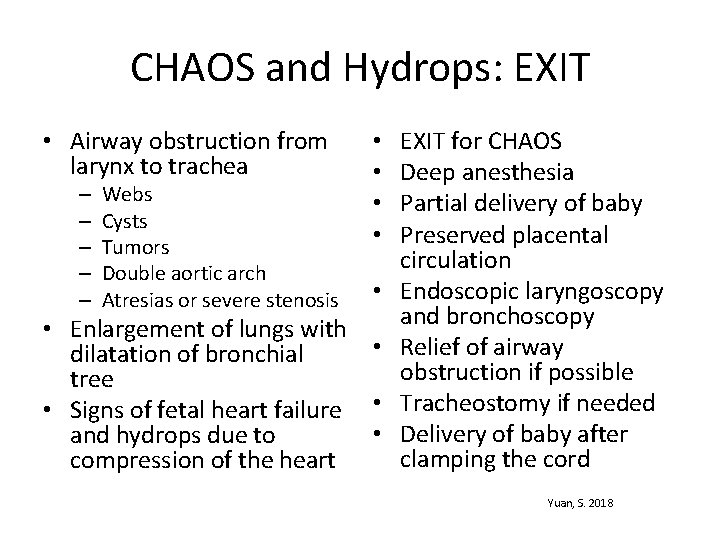
CHAOS and Hydrops: EXIT • Airway obstruction from larynx to trachea – – – Webs Cysts Tumors Double aortic arch Atresias or severe stenosis • • • Enlargement of lungs with • dilatation of bronchial tree • Signs of fetal heart failure • • and hydrops due to compression of the heart EXIT for CHAOS Deep anesthesia Partial delivery of baby Preserved placental circulation Endoscopic laryngoscopy and bronchoscopy Relief of airway obstruction if possible Tracheostomy if needed Delivery of baby after clamping the cord Yuan, S. 2018
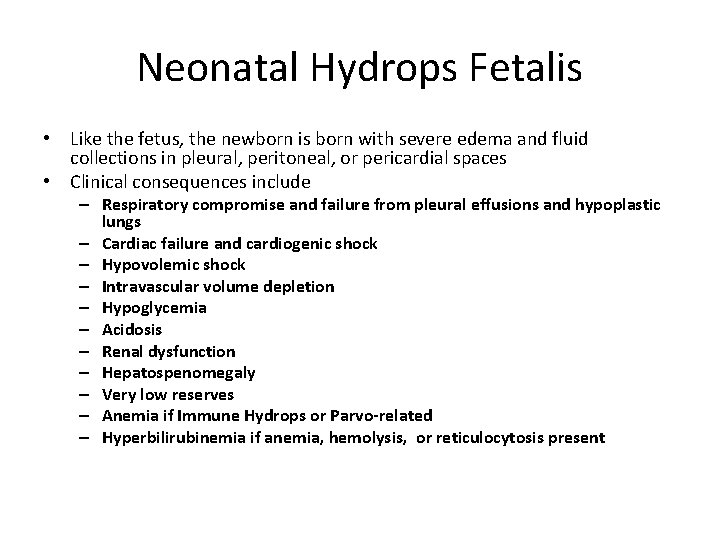
Neonatal Hydrops Fetalis • Like the fetus, the newborn is born with severe edema and fluid collections in pleural, peritoneal, or pericardial spaces • Clinical consequences include – Respiratory compromise and failure from pleural effusions and hypoplastic lungs – Cardiac failure and cardiogenic shock – Hypovolemic shock – Intravascular volume depletion – Hypoglycemia – Acidosis – Renal dysfunction – Hepatospenomegaly – Very low reserves – Anemia if Immune Hydrops or Parvo-related – Hyperbilirubinemia if anemia, hemolysis, or reticulocytosis present
Management of Neonatal Hydrops • Antenatal diagnosis will assist in planning • Preparation for delivery after transfer to high risk center with NICU • Family counseling crucial – Direct resuscitation plans – Prognosis – Comfort care – Post death testing and autopsy
Preparation for Delivery • Appropriate equipment – Intubation supplies – Umbilical lines – Resuscitation meds, volume, blood products – Paracentesis and/or thoracentesis supplies – Chest tube set up, with chest tube care ongoing • Appropriate personnel – Location in tertiary facility – Nursing, Respiratory care, neonatology – Pediatric subspecialty physicians
ABCs in Delivery Room Management • Airway and Breathing: intubation and ventilation to support respiratory failure – Compromised by soft tissue edema, airway malformations or cystic hygroma – Hypoplastic lungs may necessitate increased pressures to ventilate – Immediate thoracentesis or paracentesis required to remove effusions/ascites preventing lung expansion
ABCs in the Delivery Room • Circulation: immediate support of myocardial dysfunction and insufficiency • Reversal of intravascular volume depletion – Normal saline and/or blood • Reversal of acidosis and assessment of oxygenation • Treatment determined by type of hydrops – Availability of blood when severe anemia is predicted
Immune Hydrops • Transfusion to normalize hematocrit – Partial exchange transfusion prn • Aggressive treatment of hyperbilirubinemia, which develops within an hour or so – – – Adequate hydration Phototherapy, likely double lights IVIG Exchange transfusion based on bili nomogram Metalloporphyrins [synthetic heme analogs which are competitive inhibitors of heme oxygenase—the ratelimiting enzyme in bilirubin production] • Adequate treatment of late anemia
Immune Hydrops • • • Well defined cause of hydrops Established diagnostic criteria With a consistent therapeutic approach Good prognosis Decreased incidence with use of Rho (D) immune globulin
NICU management… • Treatment of respiratory failure – Mechanical ventilation – Surfactant – Inhaled nitric oxide [Sildenafil…Milrinone…] for PPHN – Removal of pleural effusions/chest tube management • Support of cardiovascular function – Volume support – Inotropic and pressor support – Correction/palliation of CHD • Intravascular fluid support balanced with excess fluid removal – Fluid resuscitation – Blood replacement [replacement of effusion losses] – Repletion of serum protein and albumin – Diuretics – Base fluids and medications on estimated dry weight [50 th percentile for gestational age]
NICU management… • Treatment of underlying cause – – – – Diagnostic battery to identify cause Immediate cardiac ECHO, X rays, necessary ultrasounds Analysis of ascites to r/o leakage of urine versus effusion Genetics and chromosomes Metabolic studies CBC, bili levels, LFTs, type and cross, electrolytes, Ca, Mg etc. Cultures and viral studies • Supportive care and management of symptoms – – – – Management of temperature Correction of acid base, electrolyte and glucose abnormalities Support of oxygenation Pre and post operative surgical management of surgical candidates Pain management and sedation Ongoing search for etiology Prevention of pressure injury related to poor perfusion and edema

Management of skin care • Sick & edematous patients – Severe edema poor perfusion – Mechanical ventilation – Chest tubes • Prevention of pressure injury and device injury – Skin risk assessment daily – Skin condition monitoring – Initiation of Pressure injury bundle Frequent turning to offload Fluidized mattress Gel pillows for head Mepilex foam dressing on occiput Follow up with Wound Ostomy RN for all stage 1 injuries • Prevention of device-related injuries • Barrier under IVs and other devices • • •

Prognosis and Outcome Issues • Counseling on disease and cause • Follow up with genetics and other specialty services – May be important to counsel for future recurrent risk • Palliative care and pain team consults early – Palliative care for all those with serious life threatening illnesses – Possibly for advanced directives and end of life care – Appropriate pain management for long-term ventilator needs, chest tubes, etc.
Management of Chylothorax • Chylothorax is a cause of and complicated by NIHF • Chyle is the lymphatic fluid collected in the splanchnic system via the thoracic duct • Leakage occurs from the thoracic duct or its tributaries • Neonatal chylothorax is often transient and resolves spontaneously but severe congenital chylothorax can persist
Management of Chylothorax • Initial treatment of chylothorax can include: o Holding enteral feedings and support of nutrition with TPN o Octreotide—synthetic somatostatin—which decreases chyle production o o Decreases splanchnic blood flow Inhibits of pancreatic secretions Inhibits GI peptide hormone secretion Minimizes lymphatic fluid excretion o Use of low fat/no fat formulas supplemented with MCTs and essential fatty acids such as Portgen, Enfaport or Vivonex TEN • Research being done on low-fat breast milk use, which helps resolve the chylothorax but results in poor growth
Management of Chylothorax • Chylothorax persisting longer than 5 weeks requires a pediatric surgical consultation – Thoracic duct ligation – Pleuroperitoneal shunt placement – Pleurectomy – 15% of chylothorax patients die as a result of complications of therapy
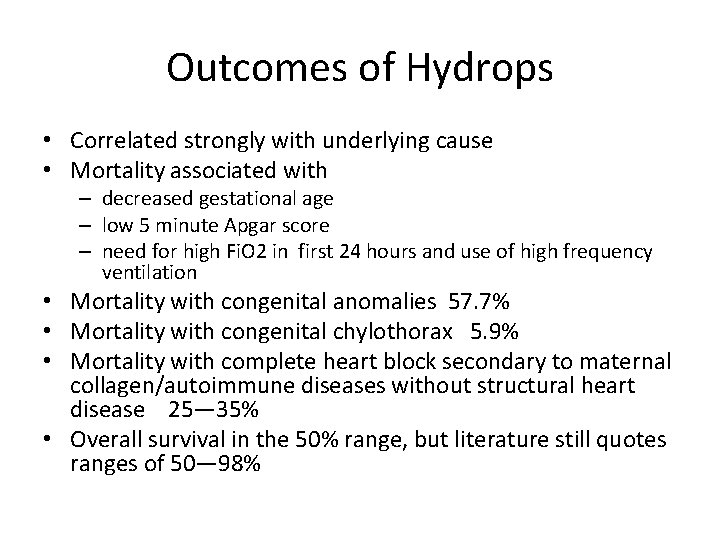
Outcomes of Hydrops • Correlated strongly with underlying cause • Mortality associated with – decreased gestational age – low 5 minute Apgar score – need for high Fi. O 2 in first 24 hours and use of high frequency ventilation • Mortality with congenital anomalies 57. 7% • Mortality with congenital chylothorax 5. 9% • Mortality with complete heart block secondary to maternal collagen/autoimmune diseases without structural heart disease 25— 35% • Overall survival in the 50% range, but literature still quotes ranges of 50— 98%
![References Peebles S UAMS NICU management of Hydrops Fetalis ANGELS Perinatal Conference 2010 uams References Peebles, S. [UAMS] NICU management of Hydrops Fetalis. ANGELS Perinatal Conference. 2010. uams.](https://slidetodoc.com/presentation_image_h2/c6e6117a53fe0cb0b78b618f45373519/image-53.jpg)
References Peebles, S. [UAMS] NICU management of Hydrops Fetalis. ANGELS Perinatal Conference. 2010. uams. edu Bellini, C. et al. Etiology of non-immune hydrops fetalis: A systematic review. American Journal of Medical Genetics. 2009. 844 -51 Bellini C et al. Etiology of non-immne hydrops fetals: An Update. American Journal of Medical Genetics. 2015: 167 (5): 1082 -88 Bellini C. and Hennekam R. Non-immune hydrops fetalis: A short review of etiology and pathophysiology. American Journal of Medical Genetics. 2012. 158 A: 597 -605 Desilets, V. and Audibert, F. Investigation and management of non-immune hydrops fetalis. Journal of Obstetrics and Gynaecology, Canada. 2013. 35 (10): e 1 -14. Hamdan, A and Nimavat, D. Pediatric hydrops fetalis. Available at https: //emedicine. Medscape. com/article/974571 -print Chon, A. et al. Long-term outcomes after thoracoamniotic shunt for pleural effusions with secondary hydrops. Journal of Surgical Research. 2019. 233: 304 -09. Tran, L/ Cheung, K and Kirby, M. Trisomy 21 and hydrops: Parvovirus B 19 or transient abnormal myelopoiesis? Journal of Obstetrics and Gynaecology. 2018. available at https: //doi. org/10. 1080/01443615. 2018. 15300470 Melber. et al. Novel Mutation un CCPE 1 as a cause of recurrent hydrops fetalis from Hennekam lymphangectasia-lymphedema syndrome. Clinical Case reports. 2018. 6: 2358 -63 Perinatology. com Hydrops Fetalis. . Available at http: //perinatology. com/conditions/Hydrops. htm
![References Yuan S The Application of ex utero intrapartum treatment EXIT procedure for cardiothoracic References Yuan, S. The Application of ex utero intrapartum treatment [EXIT] procedure for cardiothoracic](https://slidetodoc.com/presentation_image_h2/c6e6117a53fe0cb0b78b618f45373519/image-54.jpg)
References Yuan, S. The Application of ex utero intrapartum treatment [EXIT] procedure for cardiothoracic disorders. Signa Vitae. 1018. 14 (1) EXIT to airway procedures for Congenital High Airway Obstruction Syndrome. Cincinnati Children’s Hospital. Available at http: //www. cincinnatichildrens. org/services/f/fetal-care/ethical Agarwal, A. et al. EXIT procedure for fetal mediastinal teratoma with large pericardial effusion: Case report and review of the literature. 2018. 31 (8): 1099— 1103
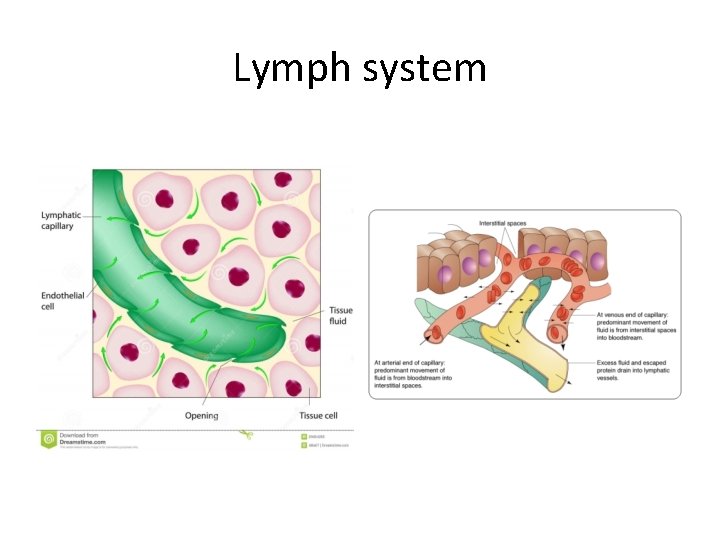
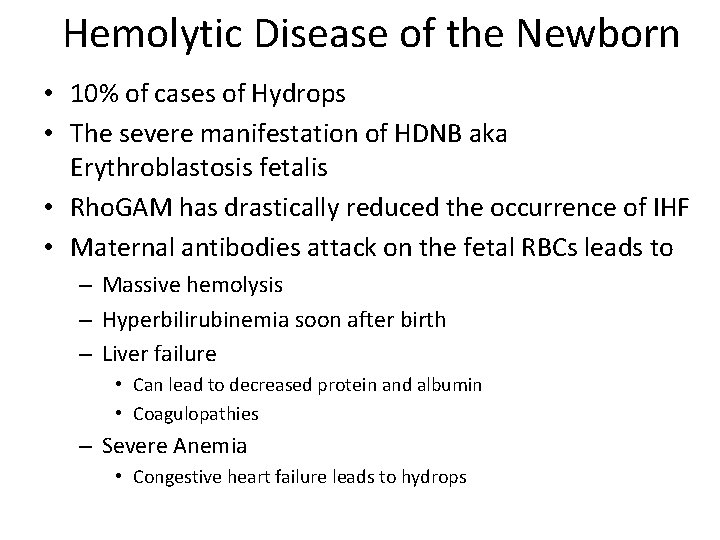
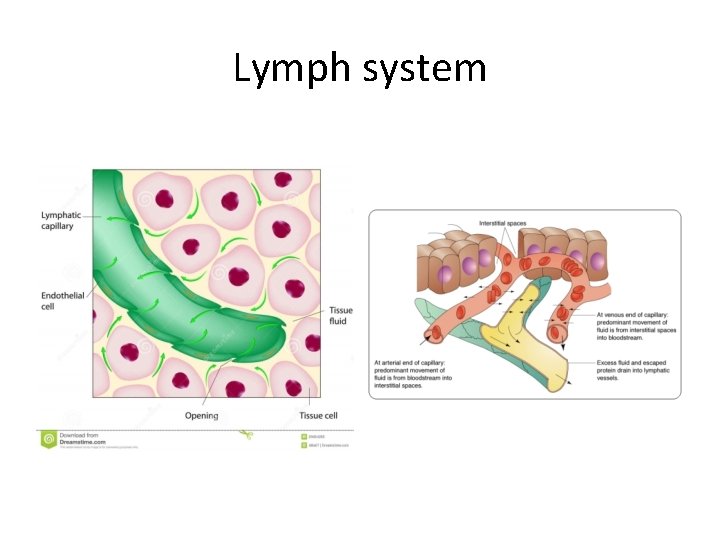
Lymph system
![Lymph system Left side thoracic duct drains about 75 of the body Right side Lymph system Left side [thoracic duct] drains about 75% of the body Right side](https://slidetodoc.com/presentation_image_h2/c6e6117a53fe0cb0b78b618f45373519/image-56.jpg)
Lymph system Left side [thoracic duct] drains about 75% of the body Right side drains head and right arm with some of right
 Non immune hydrops fetalis
Non immune hydrops fetalis Edwards syndrome
Edwards syndrome Dr ajit nambiar
Dr ajit nambiar Look down look up
Look down look up Lanugo fetalis
Lanugo fetalis Szőr felépítése
Szőr felépítése Iat
Iat Starling hipotezi
Starling hipotezi Hydrops knä
Hydrops knä Hydrops knie
Hydrops knie Sagging brain
Sagging brain Percutane galblaasdrainage
Percutane galblaasdrainage Laura conocía bien a elián. elián conocía bien a laura
Laura conocía bien a elián. elián conocía bien a laura Kandinsky and klee experiment
Kandinsky and klee experiment Paul klee take a line for a walk
Paul klee take a line for a walk Paul klee haus
Paul klee haus Fuoco nella sera klee
Fuoco nella sera klee Ville fiorentine klee
Ville fiorentine klee Biografia de paul klee
Biografia de paul klee Paul klee ligne brisée
Paul klee ligne brisée Paul klee color theory
Paul klee color theory Paul klee
Paul klee Etnografismo
Etnografismo Paul klee senecio 1922
Paul klee senecio 1922 Klee eating fish
Klee eating fish Paul klee pedagogický náčrtník
Paul klee pedagogický náčrtník Picture analysis activity 1
Picture analysis activity 1 By looking at the picture from your first activity
By looking at the picture from your first activity Look at activity 1 and answer
Look at activity 1 and answer Bruner stadi
Bruner stadi New look on perception bruner
New look on perception bruner Look new
Look new Bruner fasi di sviluppo
Bruner fasi di sviluppo Engleski jezik pripreme
Engleski jezik pripreme Unit 9 a new look
Unit 9 a new look Waxing crescent phase
Waxing crescent phase Speech
Speech New york, new jersey, pennsylvania, and delaware
New york, new jersey, pennsylvania, and delaware Fresh oil new wine
Fresh oil new wine Marquee theatre new hartford ny
Marquee theatre new hartford ny Weaknesses and strengths of the articles of confederation
Weaknesses and strengths of the articles of confederation New-old approach to creating new ventures
New-old approach to creating new ventures Marketing kotler keller
Marketing kotler keller Njbta
Njbta New classical macroeconomics
New classical macroeconomics Chapter 16 toward a new heaven and a new earth
Chapter 16 toward a new heaven and a new earth Both new hampshire and new york desire more territory
Both new hampshire and new york desire more territory New classical and new keynesian macroeconomics
New classical and new keynesian macroeconomics New nationalism vs new freedom venn diagram
New nationalism vs new freedom venn diagram Laura herrera scott
Laura herrera scott Laura jankovich
Laura jankovich Laura savarese
Laura savarese Laura gourlay
Laura gourlay Hydronefroosi aikuisella
Hydronefroosi aikuisella Usenet message to franciele
Usenet message to franciele Laura soriano dieste
Laura soriano dieste Chaffey college chino community center
Chaffey college chino community center