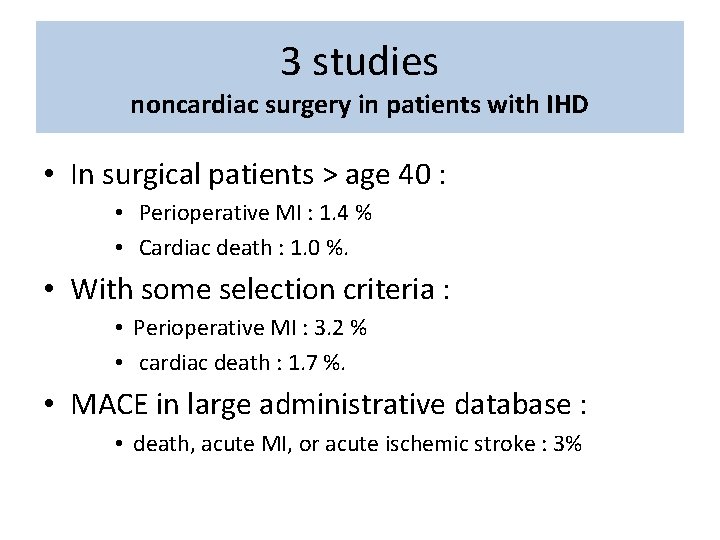
3 studies noncardiac surgery in patients with IHD










- Slides: 32

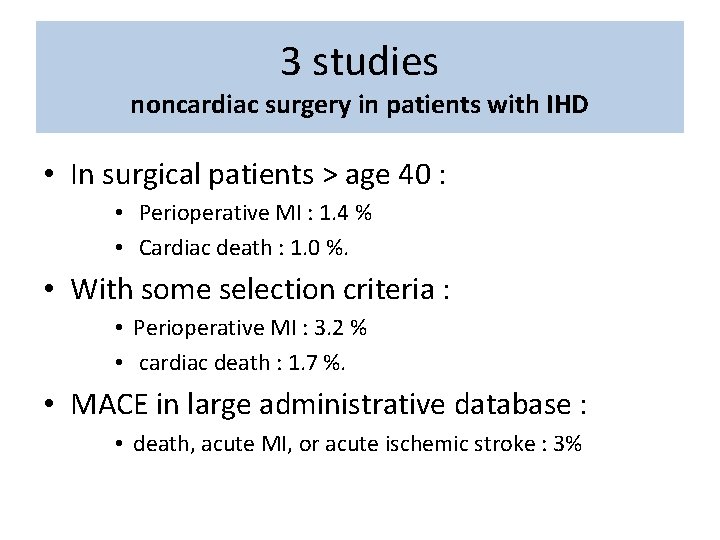
3 studies noncardiac surgery in patients with IHD • In surgical patients > age 40 : • Perioperative MI : 1. 4 % • Cardiac death : 1. 0 %. • With some selection criteria : • Perioperative MI : 3. 2 % • cardiac death : 1. 7 %. • MACE in large administrative database : • death, acute MI, or acute ischemic stroke : 3%
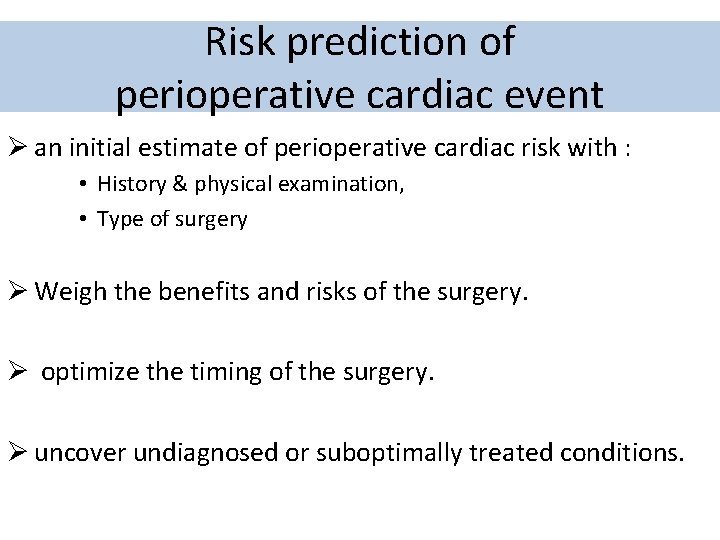
Risk prediction of perioperative cardiac event Ø an initial estimate of perioperative cardiac risk with : • History & physical examination, • Type of surgery Ø Weigh the benefits and risks of the surgery. Ø optimize the timing of the surgery. Ø uncover undiagnosed or suboptimally treated conditions.


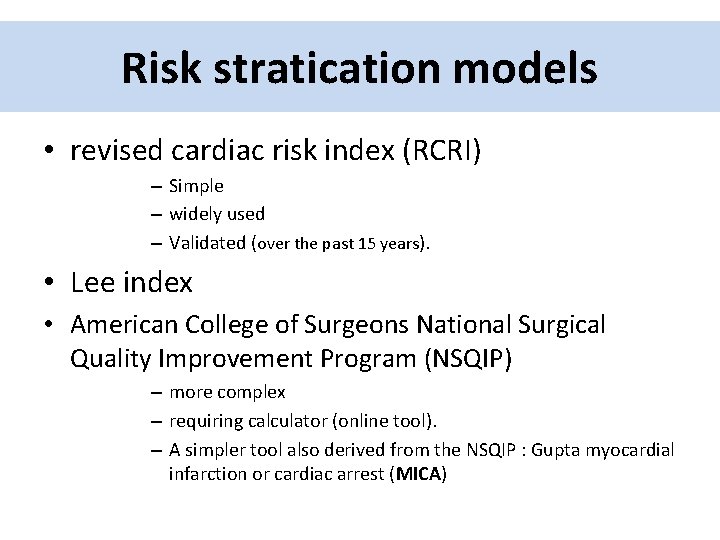
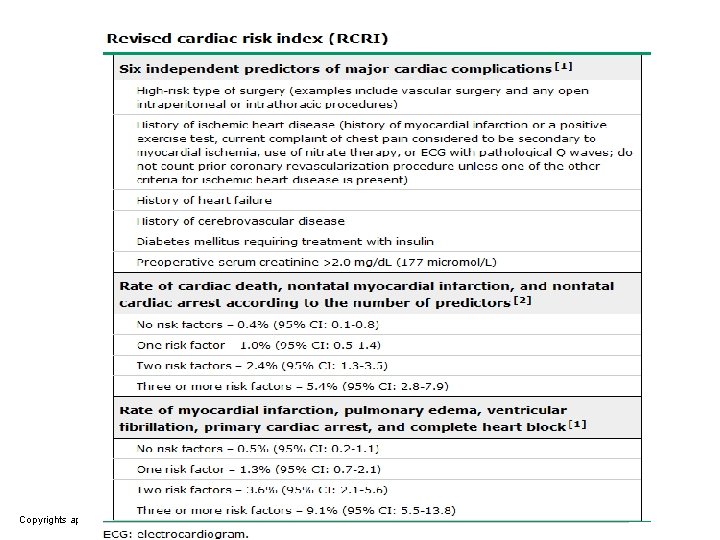
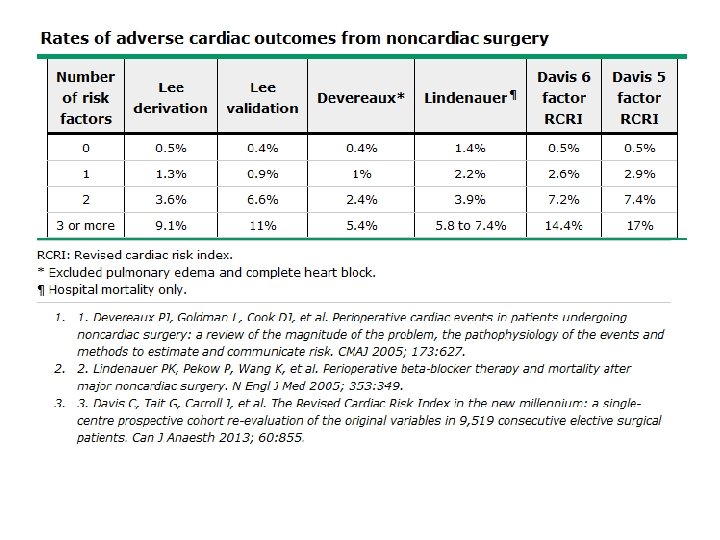
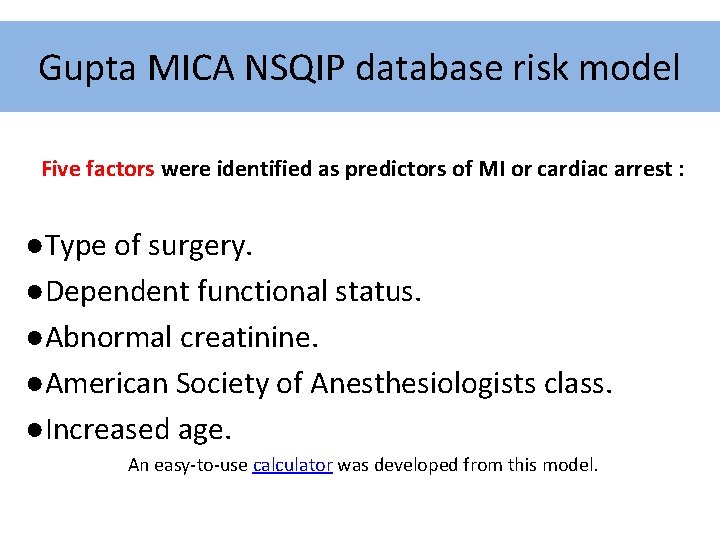
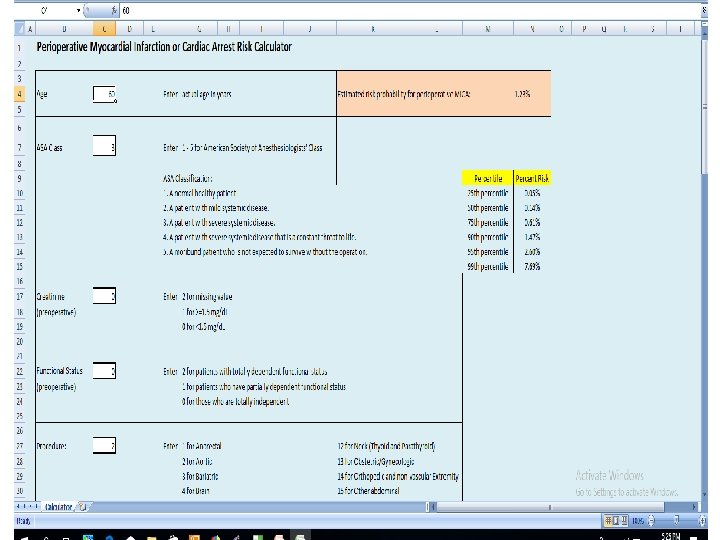
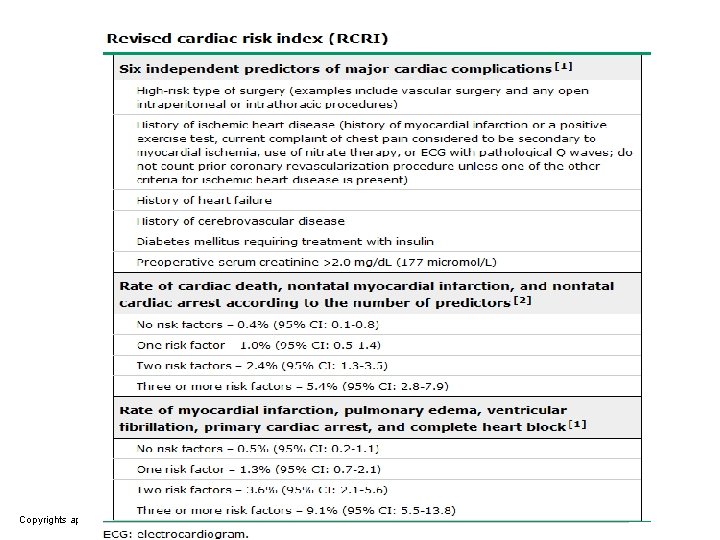
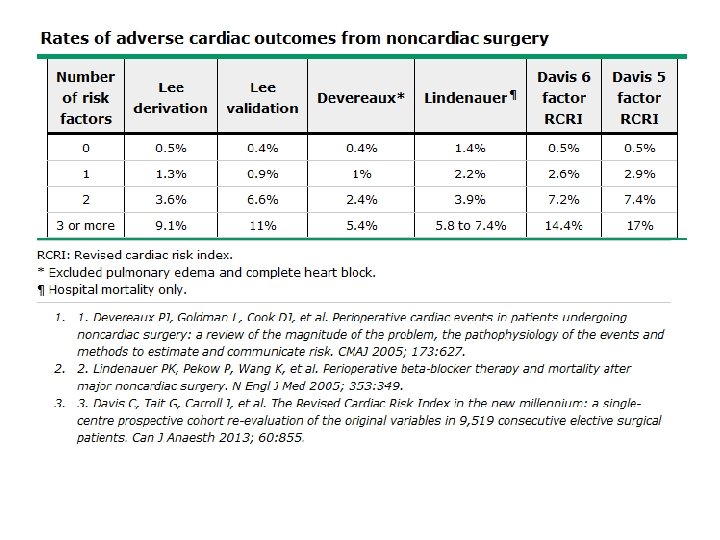
Risk stratication models • revised cardiac risk index (RCRI) – Simple – widely used – Validated (over the past 15 years). • Lee index • American College of Surgeons National Surgical Quality Improvement Program (NSQIP) – more complex – requiring calculator (online tool). – A simpler tool also derived from the NSQIP : Gupta myocardial infarction or cardiac arrest (MICA)
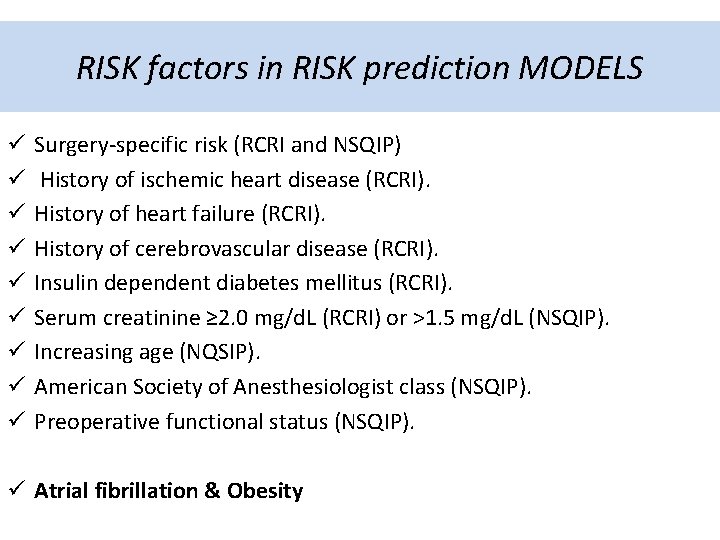
RISK factors in RISK prediction MODELS ü ü ü ü ü Surgery-specific risk (RCRI and NSQIP) History of ischemic heart disease (RCRI). History of heart failure (RCRI). History of cerebrovascular disease (RCRI). Insulin dependent diabetes mellitus (RCRI). Serum creatinine ≥ 2. 0 mg/d. L (RCRI) or >1. 5 mg/d. L (NSQIP). Increasing age (NQSIP). American Society of Anesthesiologist class (NSQIP). Preoperative functional status (NSQIP). ü Atrial fibrillation & Obesity
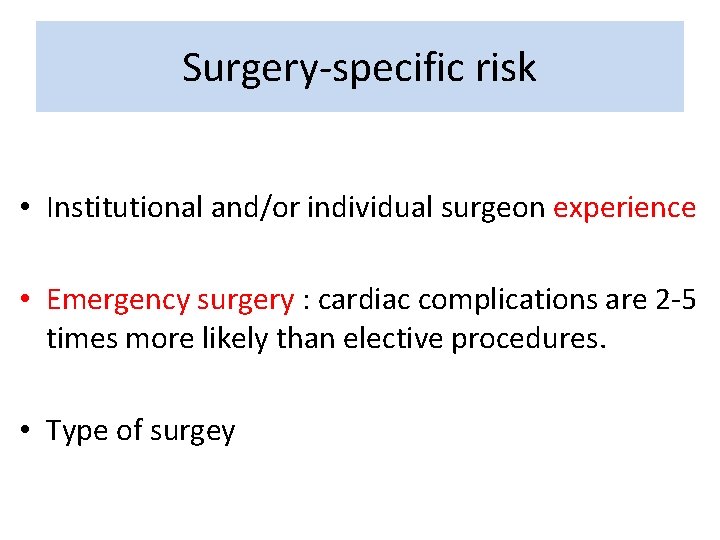
Surgery-specific risk • Institutional and/or individual surgeon experience • Emergency surgery : cardiac complications are 2 -5 times more likely than elective procedures. • Type of surgey

Copyrights apply
Copyrights apply
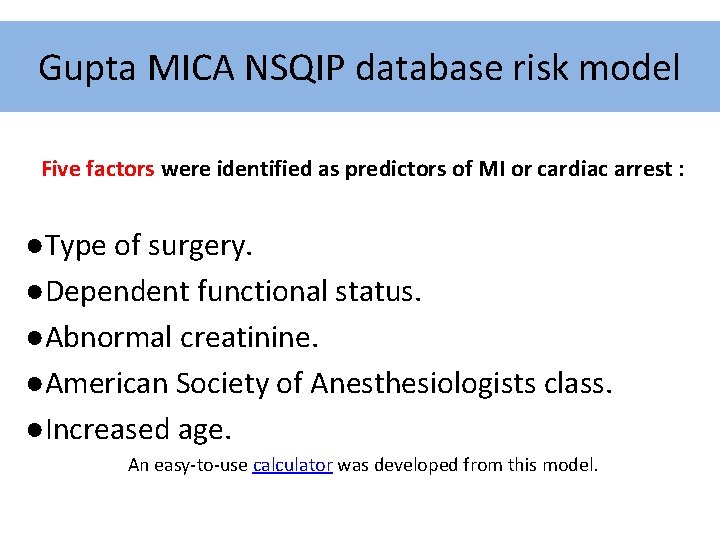
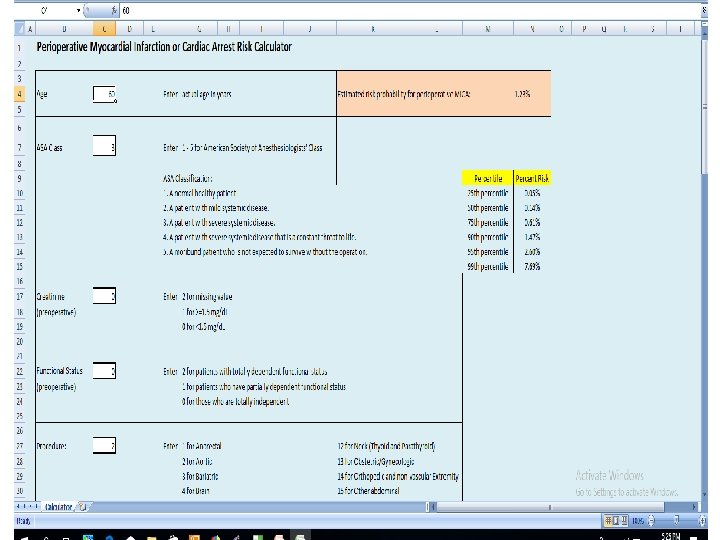
Gupta MICA NSQIP database risk model Five factors were identified as predictors of MI or cardiac arrest : ●Type of surgery. ●Dependent functional status. ●Abnormal creatinine. ●American Society of Anesthesiologists class. ●Increased age. An easy-to-use calculator was developed from this model.
Copyrights apply
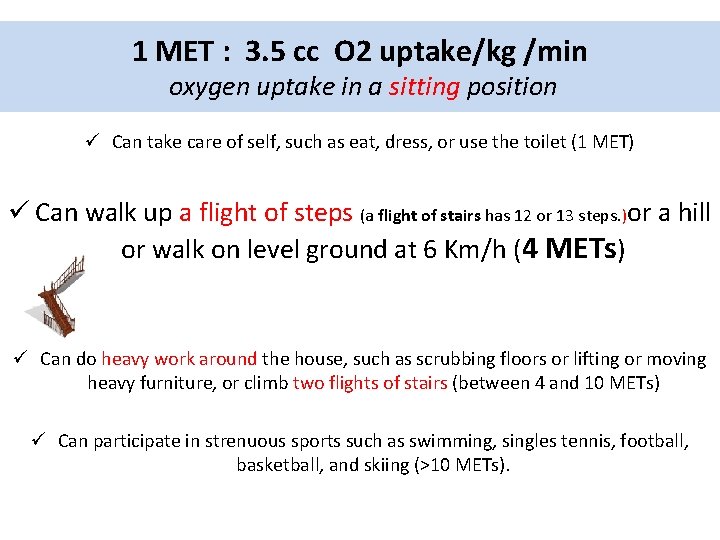
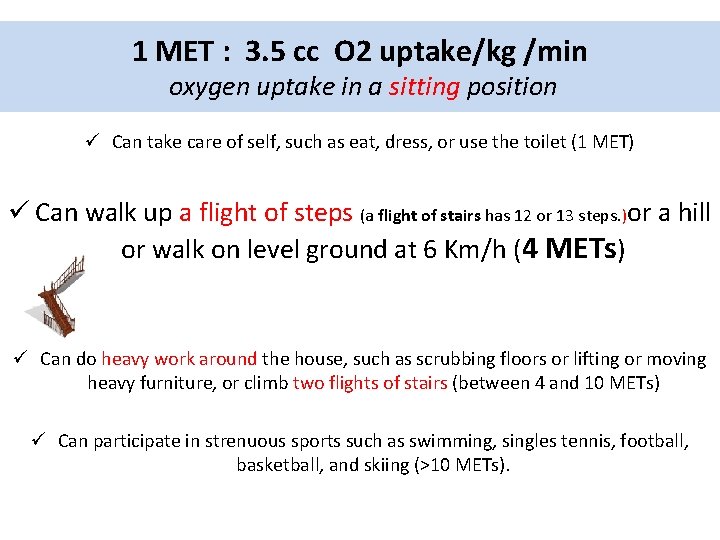
1 MET : 3. 5 cc O 2 uptake/kg /min oxygen uptake in a sitting position ü Can take care of self, such as eat, dress, or use the toilet (1 MET) ü Can walk up a flight of steps (a flight of stairs has 12 or 13 steps. )or a hill or walk on level ground at 6 Km/h (4 METs) ü Can do heavy work around the house, such as scrubbing floors or lifting or moving heavy furniture, or climb two flights of stairs (between 4 and 10 METs) ü Can participate in strenuous sports such as swimming, singles tennis, football, basketball, and skiing (>10 METs).

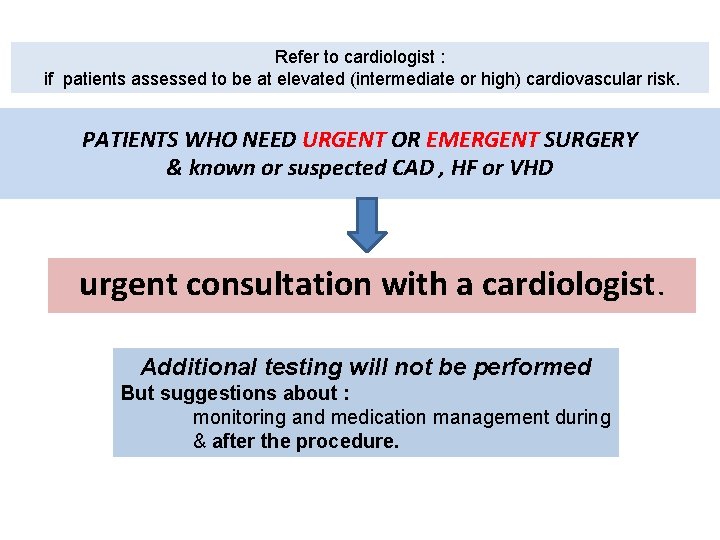
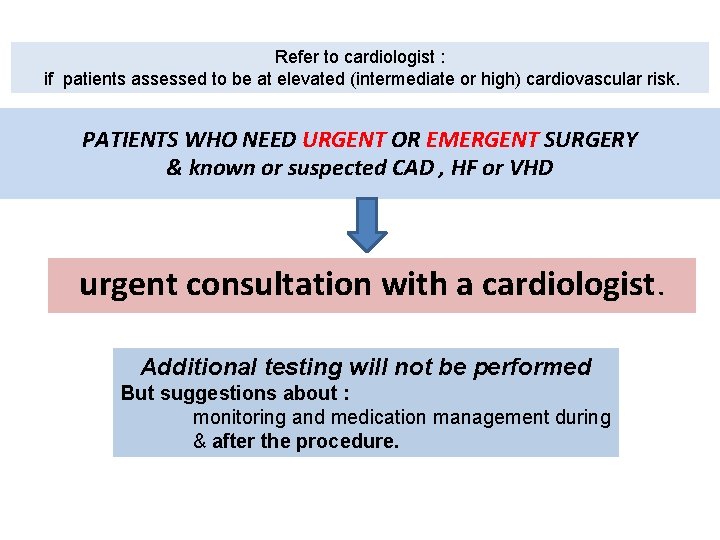
Refer to cardiologist : if patients assessed to be at elevated (intermediate or high) cardiovascular risk. PATIENTS WHO NEED URGENT OR EMERGENT SURGERY & known or suspected CAD , HF or VHD urgent consultation with a cardiologist. Additional testing will not be performed But suggestions about : monitoring and medication management during & after the procedure.
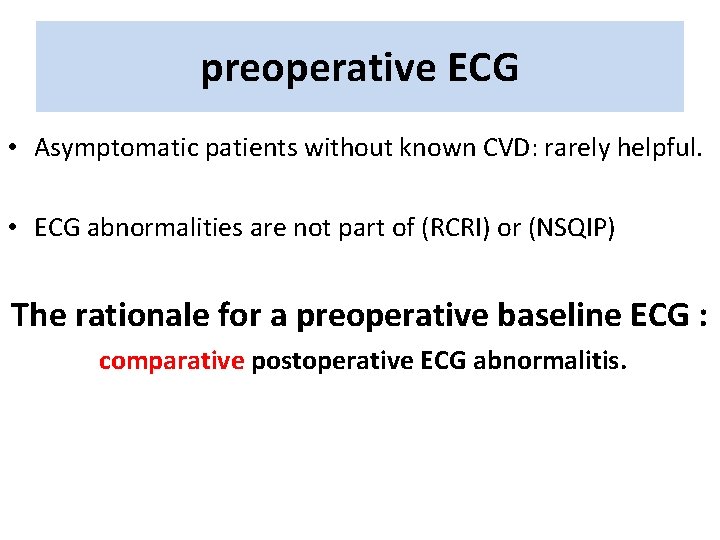
preoperative ECG • Asymptomatic patients without known CVD: rarely helpful. • ECG abnormalities are not part of (RCRI) or (NSQIP) The rationale for a preoperative baseline ECG : comparative postoperative ECG abnormalitis.
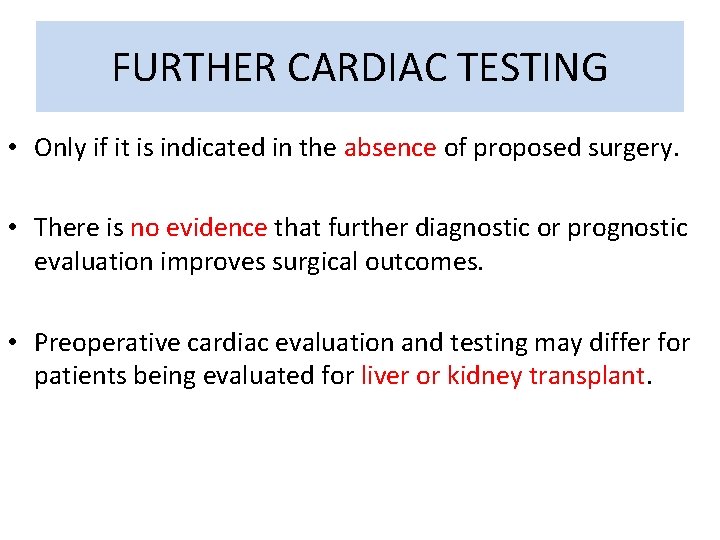
FURTHER CARDIAC TESTING • Only if it is indicated in the absence of proposed surgery. • There is no evidence that further diagnostic or prognostic evaluation improves surgical outcomes. • Preoperative cardiac evaluation and testing may differ for patients being evaluated for liver or kidney transplant.
Resting echocardiography • Is not indicated : unless there is another indication, such as : – Murmur – Dyspnea of unknown cause – Edema.
Stress testing • Is not indicated : solely because of the surgery if there is no other indication. • Some experts : routine preoperative stress imaging in major vascular surgery • No evidence for: prophylactic revascularization to prevent ischemia & improves outcomes.
Revascularization before surgery • Except in ACS : myocardial revascularization prior to noncardiac surgery is not recommended. • Patients with stable CAD do not benefit from prophylactic revascularization prior to noncardiac surgery. • only patients with unprotected left main benefited from preoperative revascularization (high risk non-invasive tests).
“ Stents “ Perioperative DAPT & Bleeding • The proinflammatory and prothrombotic condition up to 1 M. after surgery (regardless of stent type)may increase the baseline risk of stent thrombosis. • aspirin alone (20%) & with P 2 Y 12 blocker (50%) increases the risk of bleeding. • increase in PC transfusion, but not in surgical mortality or morbidity.

premature cessation of DAPT • The major predictor of stent thrombosis, irrespective of stent type. • The risk has been estimated to be 30 - to 50 -fold or greater. • In patients who stop both agents, stent thrombosis generally occurs within 10 days in the majority of patients.
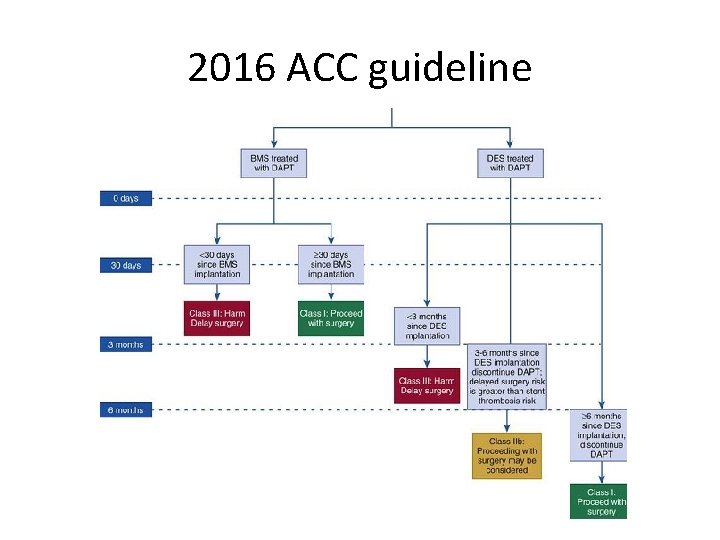
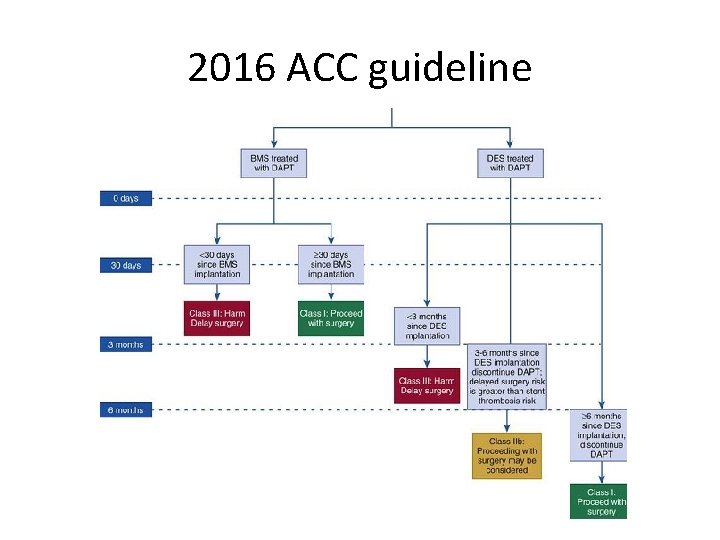
2016 ACC guideline
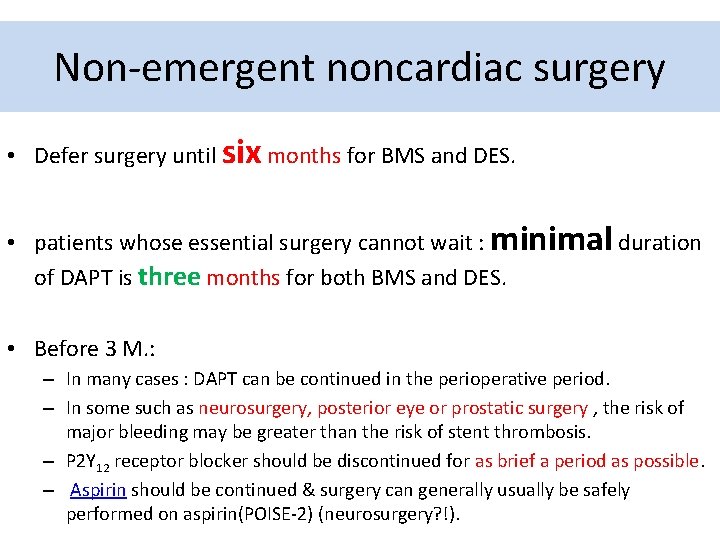
Non-emergent noncardiac surgery • Defer surgery until six months for BMS and DES. • patients whose essential surgery cannot wait : minimal duration of DAPT is three months for both BMS and DES. • Before 3 M. : – In many cases : DAPT can be continued in the perioperative period. – In some such as neurosurgery, posterior eye or prostatic surgery , the risk of major bleeding may be greater than the risk of stent thrombosis. – P 2 Y 12 receptor blocker should be discontinued for as brief a period as possible. – Aspirin should be continued & surgery can generally usually be safely performed on aspirin(POISE-2) (neurosurgery? !).
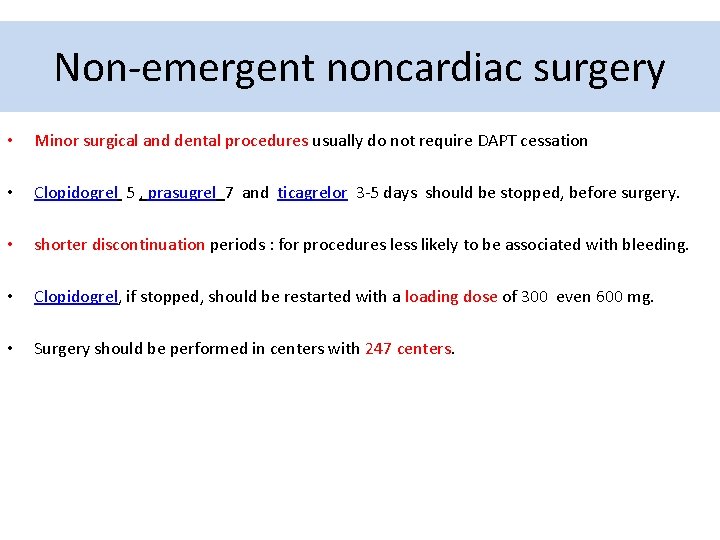
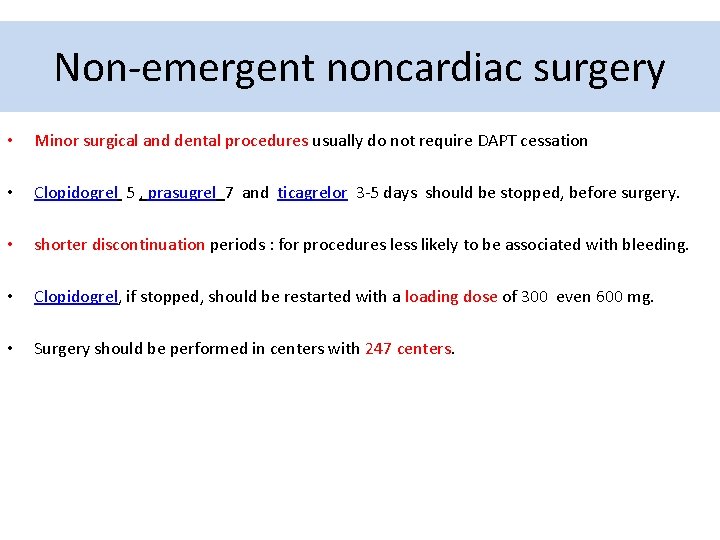
Non-emergent noncardiac surgery • Minor surgical and dental procedures usually do not require DAPT cessation • Clopidogrel 5 , prasugrel 7 and ticagrelor 3 -5 days should be stopped, before surgery. • shorter discontinuation periods : for procedures less likely to be associated with bleeding. • Clopidogrel, if stopped, should be restarted with a loading dose of 300 even 600 mg. • Surgery should be performed in centers with 247 centers.
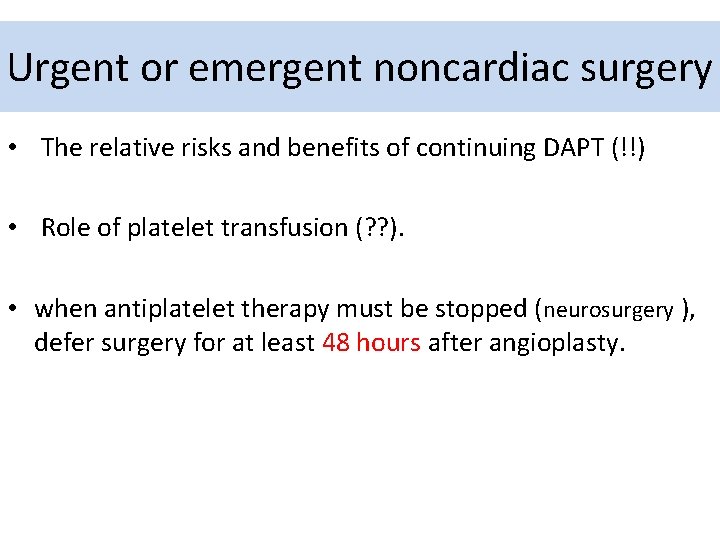
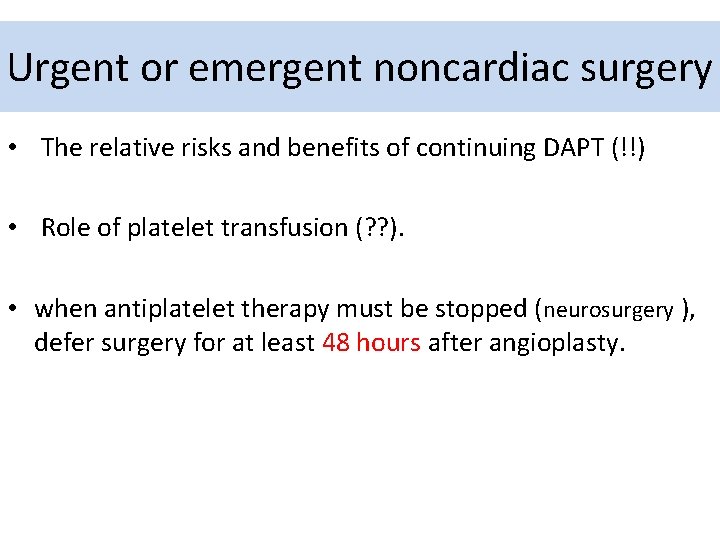
Urgent or emergent noncardiac surgery • The relative risks and benefits of continuing DAPT (!!) • Role of platelet transfusion (? ? ). • when antiplatelet therapy must be stopped (neurosurgery ), defer surgery for at least 48 hours after angioplasty.
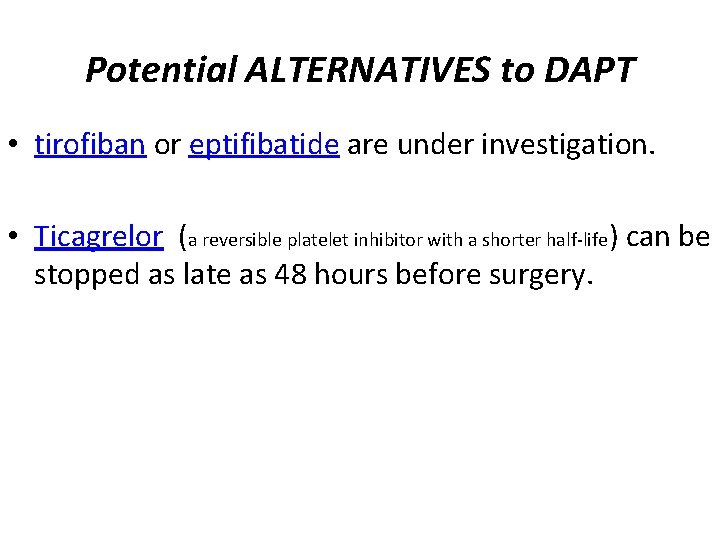
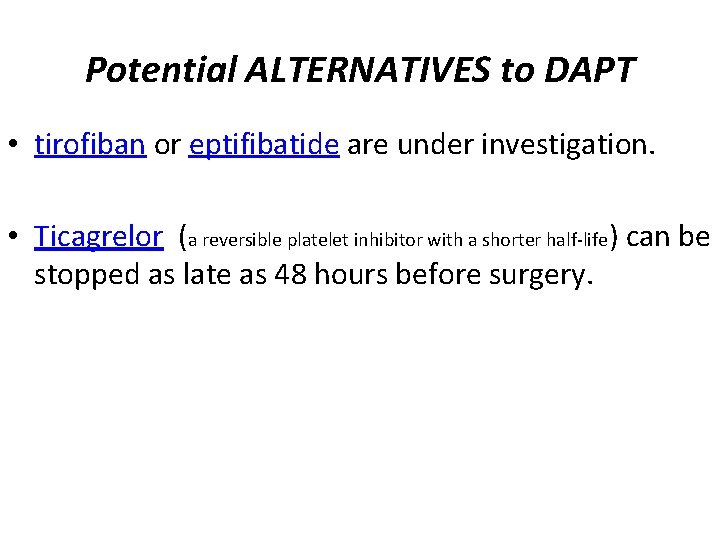
Potential ALTERNATIVES to DAPT • tirofiban or eptifibatide are under investigation. • Ticagrelor (a reversible platelet inhibitor with a shorter half-life) can be stopped as late as 48 hours before surgery.




 Ihd
Ihd Pathology
Pathology Ihd
Ihd Paradigm shift from women studies to gender studies
Paradigm shift from women studies to gender studies Diet chart for icu patients
Diet chart for icu patients Nursing diagnosis ocd
Nursing diagnosis ocd Broadmoor patients
Broadmoor patients Ethical issues in treating lgbt patients
Ethical issues in treating lgbt patients Life expectancy of sickle cell patients
Life expectancy of sickle cell patients Management of patients with neurologic trauma
Management of patients with neurologic trauma Medicare improvements for patients and providers act
Medicare improvements for patients and providers act Chapter 55 care of patients with stomach disorders
Chapter 55 care of patients with stomach disorders Health education on hepatitis ppt
Health education on hepatitis ppt Patients rights charter
Patients rights charter Pico questions for oncology patients
Pico questions for oncology patients Dealing with challenging patients
Dealing with challenging patients Periodontal management of medically compromised patients
Periodontal management of medically compromised patients Some patients shout in pain while ______ an injection.
Some patients shout in pain while ______ an injection. Leadership rounding
Leadership rounding Patients rights and responsibilities
Patients rights and responsibilities Classification of soft palate
Classification of soft palate Conclusion of position in nursing foundation
Conclusion of position in nursing foundation Dope mnemonic emt
Dope mnemonic emt Lifting and moving patients emt
Lifting and moving patients emt Safe staffing ratios: benefiting nurses and patients
Safe staffing ratios: benefiting nurses and patients Patient safety malaysia
Patient safety malaysia Safe patient handling algorithms
Safe patient handling algorithms High fowler's
High fowler's Moving and handling dementia patients
Moving and handling dementia patients Jack in the box
Jack in the box Rostering patients
Rostering patients Dr carlson advises his depressed patients
Dr carlson advises his depressed patients Andreas leischker
Andreas leischker