Using FOTO Data and Peer Review to Optimize






- Slides: 24
Using FOTO Data and Peer Review to Optimize Patient Care Julie Collins, MA, OTR/L April 6, 2014

Ohio. Health System Not-for-profit, faith-based health system West Ohio Conference of United Methodist Church Our Organization + 17, 000 associates + 30+ ambulatory sites + 2, 800 physicians + 94, 000 inpatient admissions + 3, 000 volunteers + 393, 000 ED visits + 19 hospitals + 1. 8 million outpatient visits (member and affiliated) 2 2
Ohio. Health Physical Rehabilitation 3
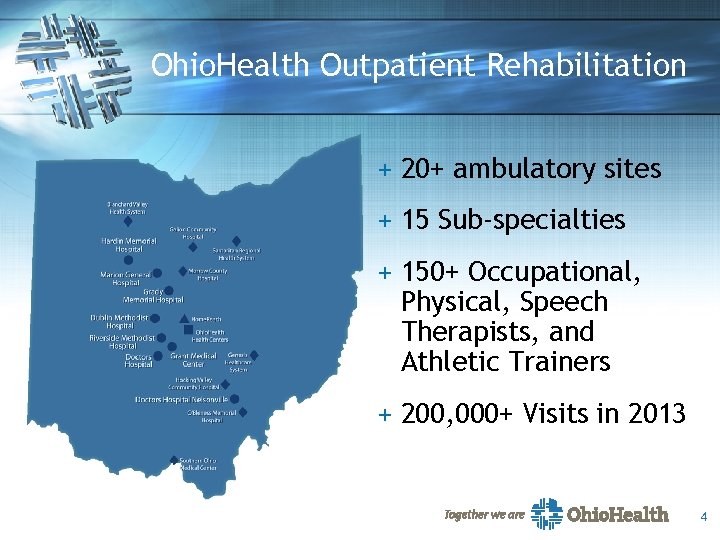
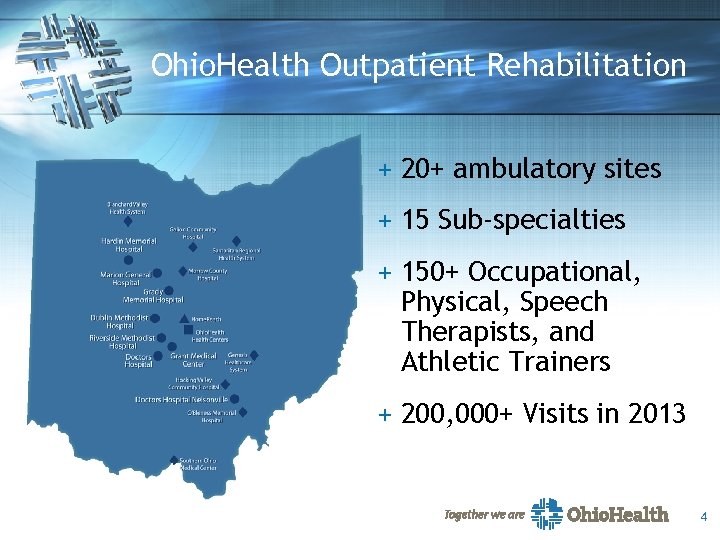
Ohio. Health Outpatient Rehabilitation + 20+ ambulatory sites + 15 Sub-specialties + 150+ Occupational, Physical, Speech Therapists, and Athletic Trainers + 200, 000+ Visits in 2013 4

Ohio. Health Outpatient Rehabilitation Outpatient Rehab Quality Management Committee (ORQMC) § Committee Membership – – – Director(s) Manager(s) Supervisor(s) Sub-committee Chairperson Specialty Therapists > 5 years per APTA Guidelines: Peer Review Training BOD G 03 -05 -15 -30 5
Clinical Quality Peer Review § What it IS: – A process to : § Improve rehabilitation’s overall quality of care § Identify clinical practice improvement opportunities § Integrate evidence based care § What it is NOT: – A historical chart review process of regulatory requirements 6

ORQMC Committee Goals Improve patient outcomes by pursuing and maintaining excellence in therapist performance Create a positive culture toward OP peer review Promote efficient resource use by assessing treatment justification, medical necessity, intervention effectiveness, and treatment duration 7
ORQMC Committee Goals Positively assist in providing therapists timely and specific feedback Support therapist educational goals, professional growth, and competence Promote efficient resource utilization (therapists, admin, quality, office support) Maximize value to patients, payer sources, and regulatory agencies 8

Committee Responsibilities Identify outlying charts and review OP Rehab Quality Management Committee Communicate and track improvement for system and individual therapists Identify opportunities for improvement and develop plan Disseminate results to management and clinicians 9
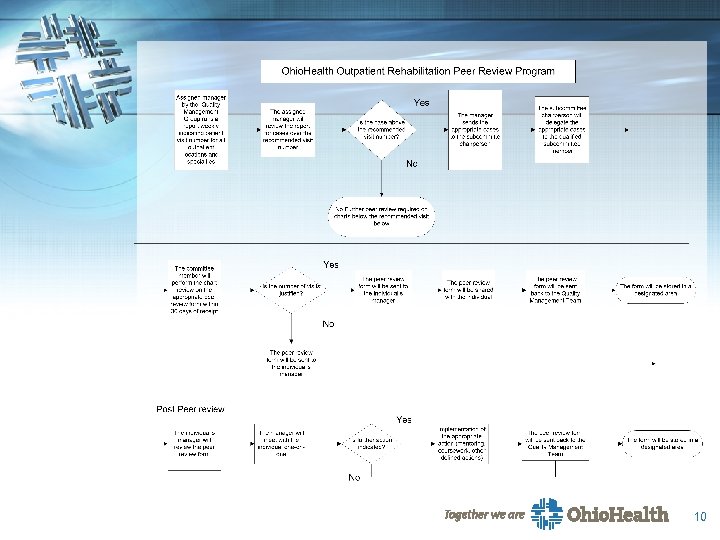
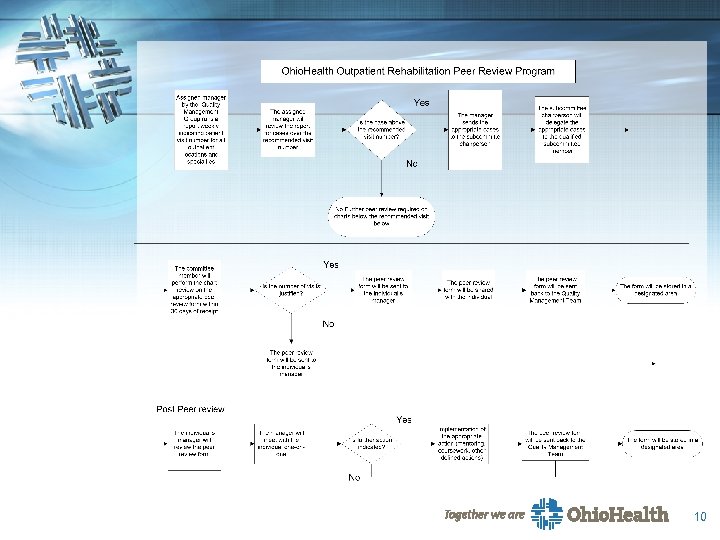
10
Clinical Quality Review Pilot review performed utilizing information on outpatients with lumbar spine involvement – Most opportunity for improvement – Most frequent diagnosis – Greatest potential for patient improvement – Robust evidence based practice literature 11
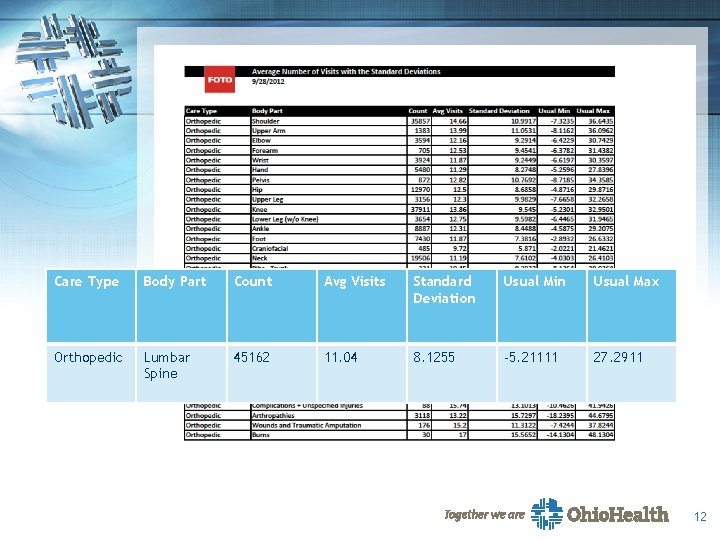
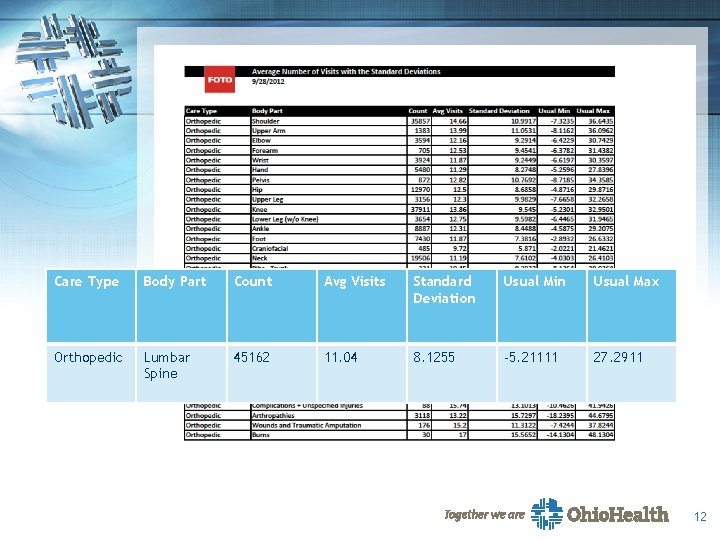
Care Type Body Part Count Avg Visits Standard Deviation Usual Min Usual Max Orthopedic Lumbar Spine 45162 11. 04 8. 1255 -5. 21111 27. 2911 12
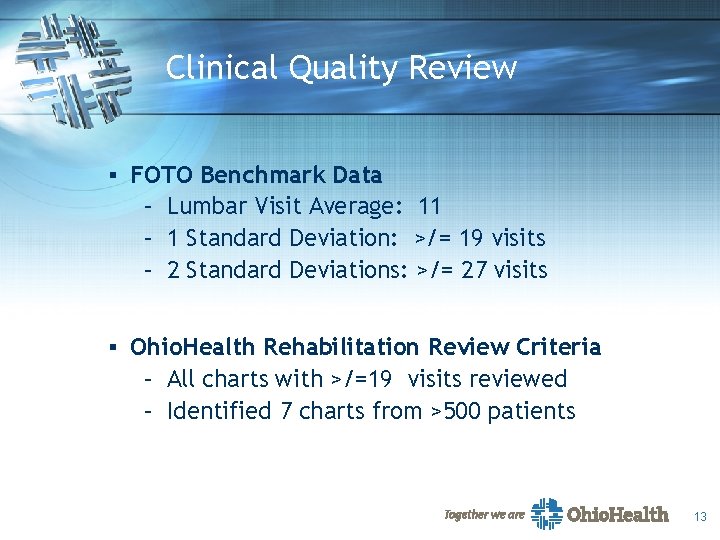
Clinical Quality Review § FOTO Benchmark Data – Lumbar Visit Average: 11 – 1 Standard Deviation: >/= 19 visits – 2 Standard Deviations: >/= 27 visits § Ohio. Health Rehabilitation Review Criteria – All charts with >/=19 visits reviewed – Identified 7 charts from >500 patients 13
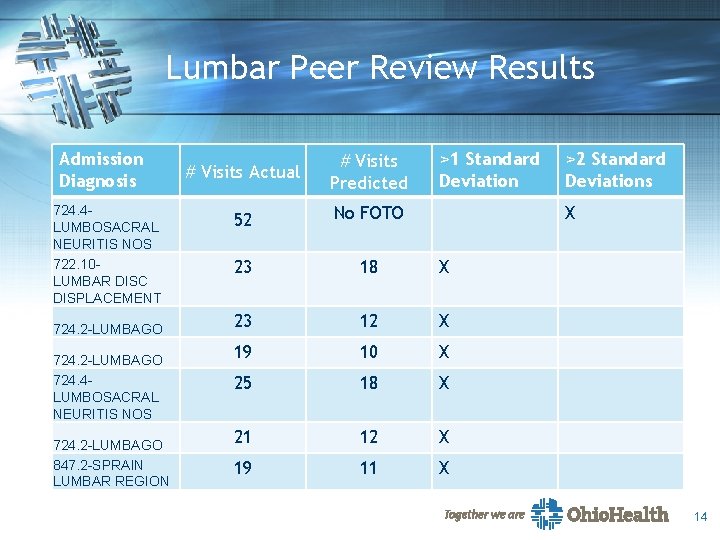
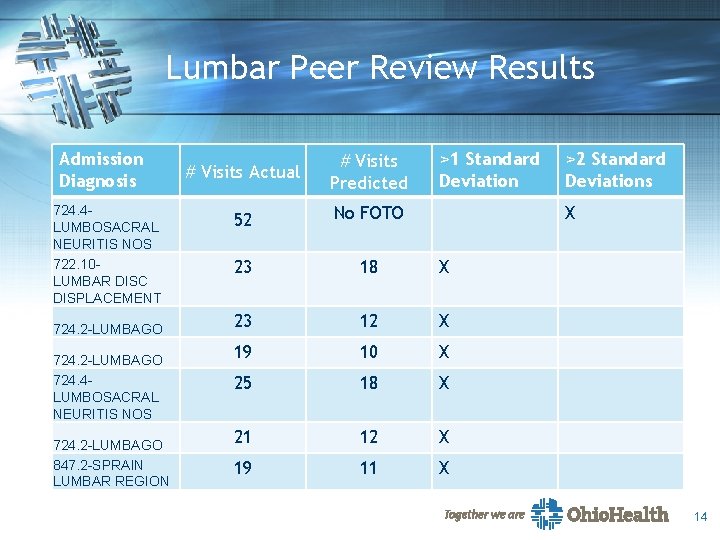
Lumbar Peer Review Results Admission Diagnosis 724. 4 LUMBOSACRAL NEURITIS NOS 722. 10 LUMBAR DISC DISPLACEMENT 724. 2 -LUMBAGO 724. 4 LUMBOSACRAL NEURITIS NOS 724. 2 -LUMBAGO 847. 2 -SPRAIN LUMBAR REGION >1 Standard Deviation # Visits Actual # Visits Predicted 52 No FOTO 23 18 X 23 12 X 19 10 X 25 18 X 21 12 X 19 11 X >2 Standard Deviations X 14
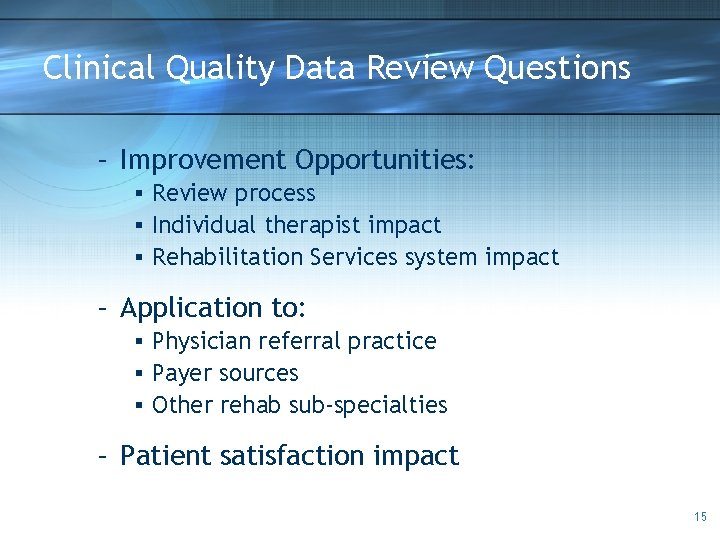
Clinical Quality Data Review Questions – Improvement Opportunities: § Review process § Individual therapist impact § Rehabilitation Services system impact – Application to: § Physician referral practice § Payer sources § Other rehab sub-specialties – Patient satisfaction impact 15

Committee Responsibilities Identify outlying charts and review OP Rehab Quality Management Committee Communicate and track improvement for system and individual therapists Identify opportunities for improvement and develop plan Disseminate results to management and clinicians 16
The Advisory Board 17
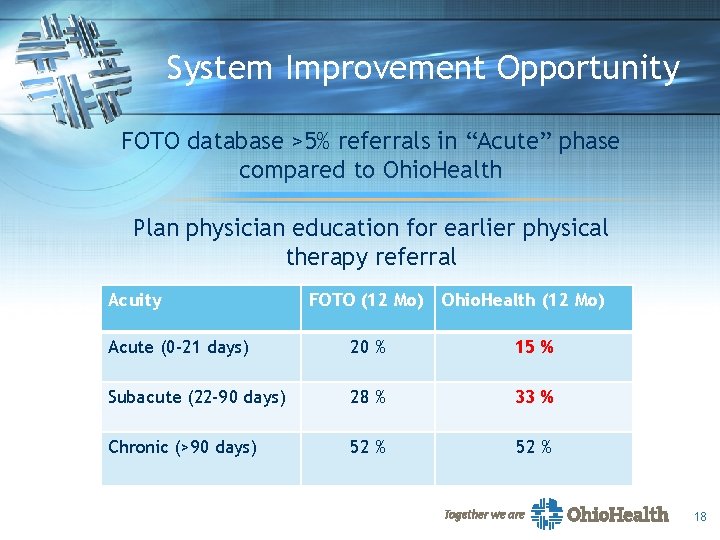
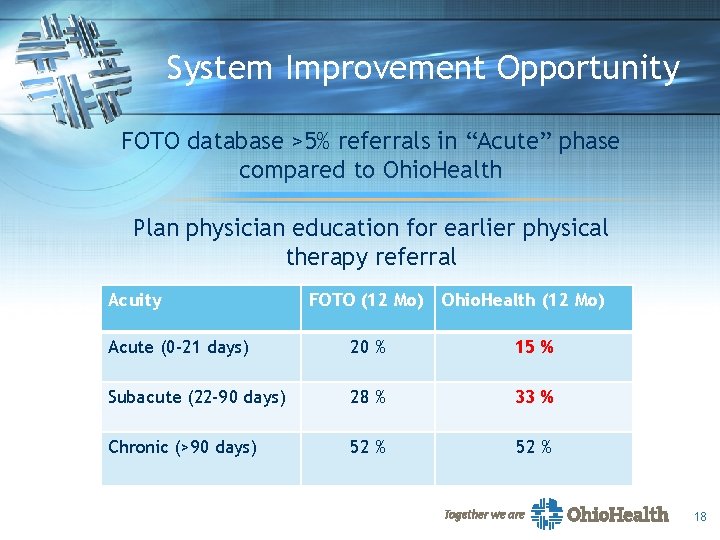
System Improvement Opportunity FOTO database >5% referrals in “Acute” phase compared to Ohio. Health Plan physician education for earlier physical therapy referral Acuity FOTO (12 Mo) Ohio. Health (12 Mo) Acute (0 -21 days) 20 % 15 % Subacute (22 -90 days) 28 % 33 % Chronic (>90 days) 52 % 18

System Improvement Opportunity § Compared with delayed physical therapy, early physical therapy timing was associated with decreased: – Risk of advanced imaging – Physician visits – Likelihood of surgery – Likelihood of injections and opioid medications – Total medical costs ($2, 736 lower) § Overall lower risk of subsequent medical service usage among patients who received PT early after and episode of acute low back pain 19
ORQMC Subcommittee Peer Review Recommendations Continue to review individual patient charts >1 SD Identify patients with best utilization Randomly review patient charts Goal to increase review to 10 per quarter 20
QUESTIONS ? ? 21
References § APTA Guidelines: Peer Review Training BOD G 03 -05 -15 -30 § Campbell SM, Braspenning J, Hutchinson A, Marshall M. Research methods used in developing and applying quality indicators in primary care. Qual Saf Health Care. 2002; 11: 358364. § Fritz JM, Childs JD, Wainner RS, Flynn TW. Primary care referral of patients with low back pain to physical therapy: impact on future health care utilization and costs. Spine. 2012; 37(25): 2114 -21. § Gellhorn AC, Chan L, Martin B, Friedly J. Management patterns in acute low back pain: the role of physical therapy. Spine. 2012; 37(9): 775 -82. 22
References Continued § Jansen MJ, Hendriks EJ, Oostendorp RAB, Dekker J, De Bie RA. Quality indicators indicate good adherence to the clinical practice guideline on “Osteoarthritis of the hip and knee” and few prognostic factors influence outcome indicators: a prospective cohort study. European Journal of Physical and Rehabilitation Medicine. 2010; 46(3); 337 -345. § Jette DU, Jewell DV. Use of Quality Indicators in Physical Therapist Practice: An Observational Study. Phys Ther. 2012; 92(4): pages unknown. Published online January 6, 2012. § Jette DU, Halbert J, Iverson C, Miceli E, Shah P. Use of Standardized Outcome Measures in Physical Therapist Practice: Perceptions and Applications. Phys Ther. 2009; 89: 125 -135. 23
References Continued § Miller PA, Nayer M, Eva KW. Psychometric Properties of a Peer- Assessment Program to Assess Continuing Competence in Physical Therapy. Phys Ther. 2010; 90(7): 1026 -1038. § Rollan T-M, Hocking C, Jones M. Physiotherapists’ Participation in Peer Review in New Zealand: Implications for the Profession. Phys Ther. Res. Int. 2010; 15: 118 -122. 24