TOOTH DISCOLORATION Classification of discoloration Intrinsic discoloration Extrinsic



- Slides: 46
TOOTH DISCOLORATION

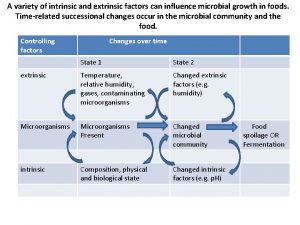
Classification of discoloration ØIntrinsic discoloration. ØExtrinsic discoloration. ØCombination of both.
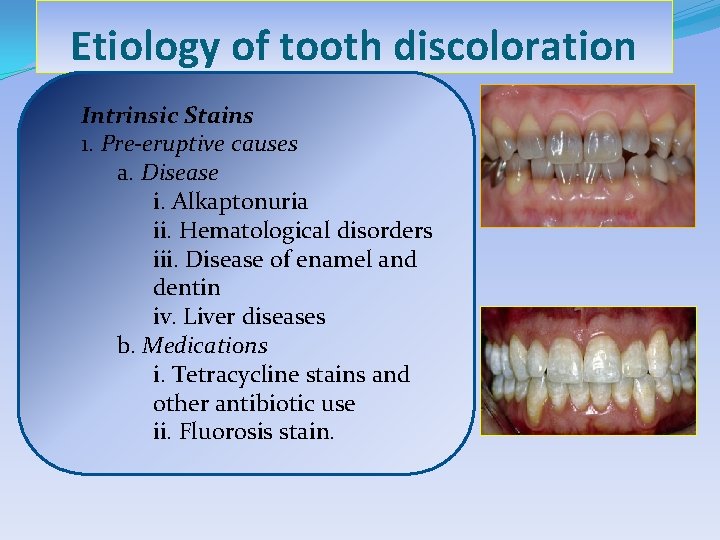
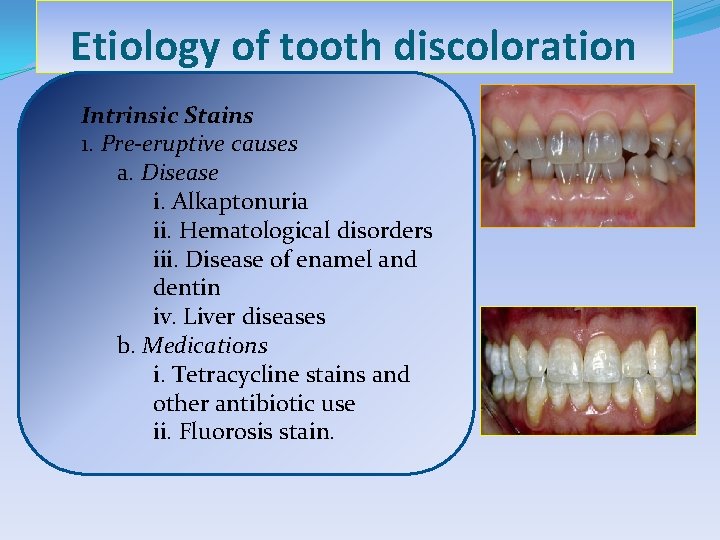
Etiology of tooth discoloration Intrinsic Stains 1. Pre-eruptive causes a. Disease i. Alkaptonuria ii. Hematological disorders iii. Disease of enamel and dentin iv. Liver diseases b. Medications i. Tetracycline stains and other antibiotic use ii. Fluorosis stain.
2. Posteruptive causes of discoloration a. Pulpal changes b. Trauma c. Dentin hypercalcification d. Dental caries e. Restorative materials and operative procedures f. Aging g. Functional and parafunctional changes
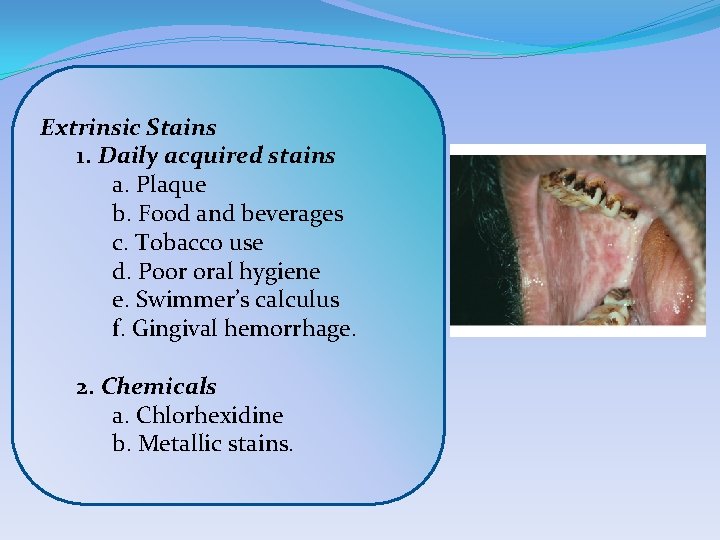
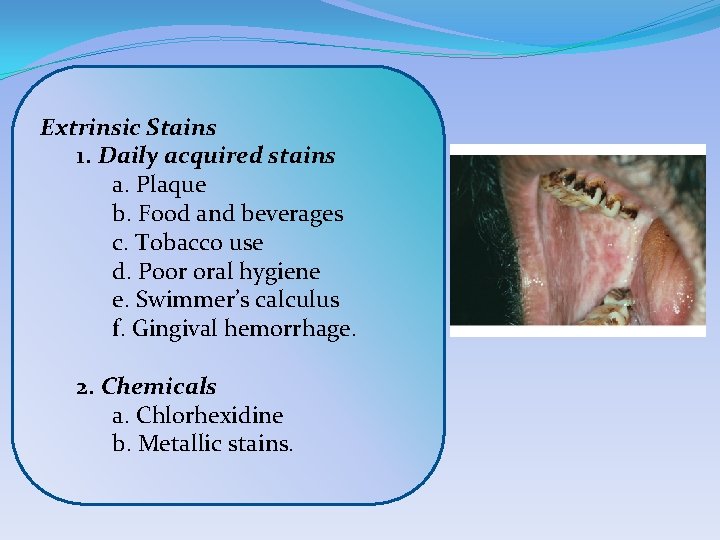
Extrinsic Stains 1. Daily acquired stains a. Plaque b. Food and beverages c. Tobacco use d. Poor oral hygiene e. Swimmer’s calculus f. Gingival hemorrhage. 2. Chemicals a. Chlorhexidine b. Metallic stains.
BLEACHING Bleaching is a procedure which involves lightening of the color of a tooth through the application of a chemical agent to oxidize the organic pigmentation in the tooth.

CONTRAINDICATIONS FOR BLEACHING �POOR CASE SELECTION �Psychologically or emotionally compromised patient �DENTIN HYPERSENSITIVITY �EXTENSIVELY RESTORED TEETH �TEETH WITH HYPOPLASTIC MARKS AND CRACKS �DEFECTIVE AND LEAKY RESTORATION �Discoloration from metallic salts particularly mercury �Defective obturation
Ideal requirements of a bleaching agent � Be easy to apply on the teeth. � Have a neutral p. H. � Lighten the teeth efficiently. � Remain in contact with oral soft tissues for short periods. � Be required in minimum quantity to achieve desired results. �Not irritate or dehydrate the oral tissues. �Not cause damage to the teeth. �Be well controlled by the dentist to customize the treatment to the patient’s need.
BLEACHING AGENTS �Constituents of bleaching gels �Carbamide peroxide. �Hydrogen peroxide and sodium hydroxide. �Sodium perborate. �Thickening agent-carbopol or carboxy polymethylene. �Urea. �Surfactant and pigment dispersants. �Preservatives. �Vehicle-glycerine and dentifrice. �Flavors. �Fluoride and 3 percent potassium nitrate.
�Carbamide Peroxide (CH 6 N 2 O 3) �It is a bifunctional derivative of carbonic acid. It is available as: 1. Home bleaching a. 5 percent carbamide peroxide. b. 10 percent carbamide peroxide. c. 15 percent carbamide peroxide. d. 20 percent carbamide peroxide. 2. In-office bleaching a. 35 percent solution or gel of carbamide peroxide.
�Hydrogen Peroxide (H 2 O 2) �H 2 O 2 breaks down to water and nascent oxygen. It also formsmfree radical perhydroxyl (HO 2) which is responsible for bleaching action. �Sodium Perborate �It comes as monohydrate, trihydrate or tetrahydrate. �It contains 95 percent perborate, providing 10 percent available oxygen.
�Thickening Agents �Carbopol (Carboxy polymethylene): Addition of carbopol in bleaching gels results in: 1. Slow release of oxygen. 2. Increased viscosity of bleaching material, which further helps in longer retention of material in tray and need of less material. 3. Delayed effervescence–thicker products stay on the teeth for longer time to provide necessary time for the carbamide peroxide to diffuse into the tooth. 4. The slow diffusion into enamel may also allow tooth to be bleached more effectively.
�Urea �It is added in bleaching solutions to: � • Stabilize the H 2 O 2 � • Elevate the p. H of solution. � • Anticariogenic effects.
�Surfactants �Surfactant acts as surface wetting agent which allows the hydrogen peroxide to pass across gel tooth boundary. �Preservatives �Commonly used preservatives are phosphoric acids, citric acid or sodium stannate. They sequestrate metals such as Fe, Cu and Mg which accelerate breakdown of H 2 O 2 and give gels better durability and stability.
�Vehicle 1. Glycerine: It is used to increase viscosity of preparation and ease of manipulation. 2. Dentifrice. �Flavors �They are added to improve patient acceptability. �Fluoride and 3 percent Potassium Nitrate �They are added to prevent sensitivity of teeth after bleaching.
Mechanism of Bleaching �Mechanism of bleaching is mainly linked to degradation of high molecular weight complex organic molecules that reflect a specific wavelength of light that is responsible for color of stain. �The resulting degradation products are of lower molecular weight and composed of less complex molecules that reflect less light, resulting in a reduction or elimination of discoloration
HOME BLEACHING TECHNIQUE/NIGHTGUARD BLEACHING �Indications for Use � Mild generalized staining. � Age related discolorations. � Mild tetracycline staining. � Mild fluorosis. � Acquired superficial staining. � Stains from smoking tobacco. � Color changes related to pulpal trauma or necrosis.
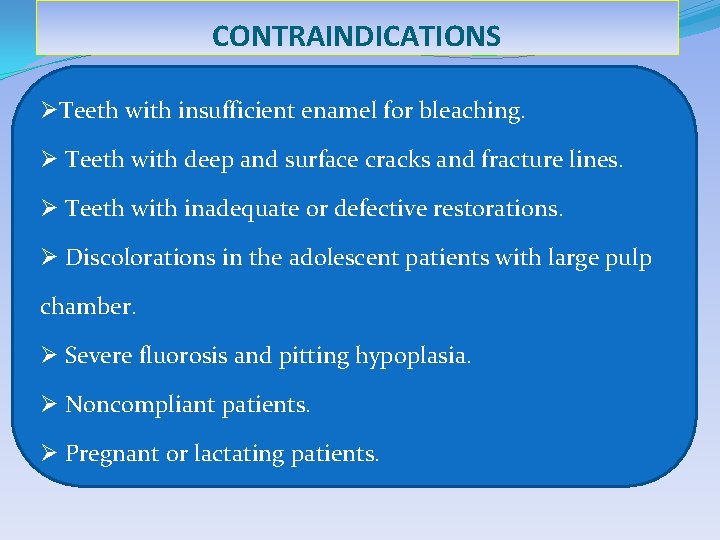
CONTRAINDICATIONS ØTeeth with insufficient enamel for bleaching. Ø Teeth with deep and surface cracks and fracture lines. Ø Teeth with inadequate or defective restorations. Ø Discolorations in the adolescent patients with large pulp chamber. Ø Severe fluorosis and pitting hypoplasia. Ø Noncompliant patients. Ø Pregnant or lactating patients.
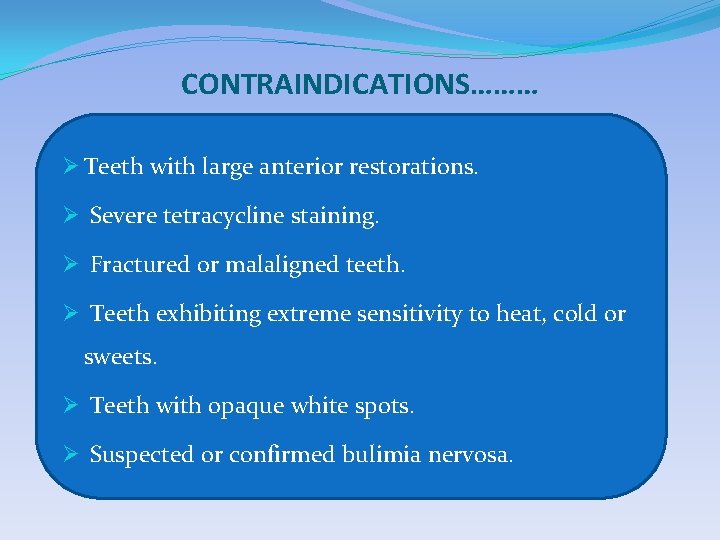
CONTRAINDICATIONS……… Ø Teeth with large anterior restorations. Ø Severe tetracycline staining. Ø Fractured or malaligned teeth. Ø Teeth exhibiting extreme sensitivity to heat, cold or sweets. Ø Teeth with opaque white spots. Ø Suspected or confirmed bulimia nervosa.
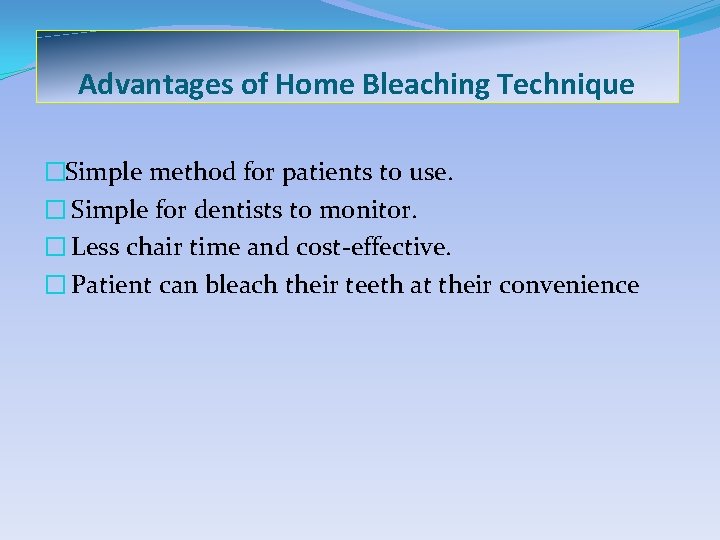
Advantages of Home Bleaching Technique �Simple method for patients to use. � Simple for dentists to monitor. � Less chair time and cost-effective. � Patient can bleach their teeth at their convenience
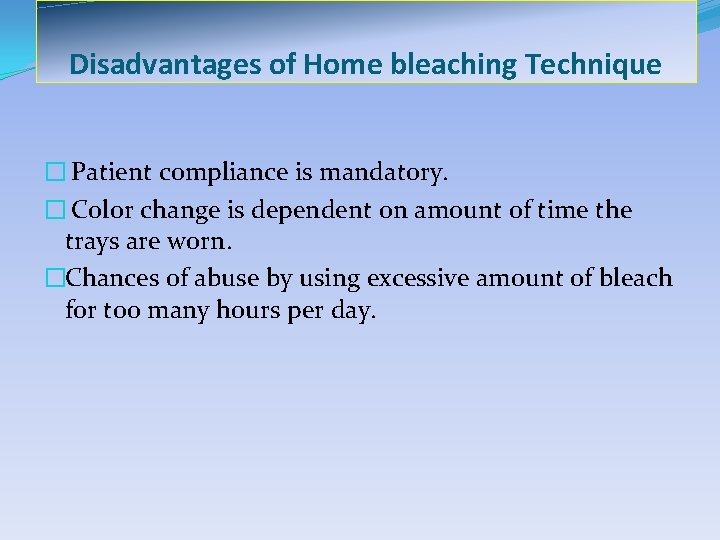
Disadvantages of Home bleaching Technique � Patient compliance is mandatory. � Color change is dependent on amount of time the trays are worn. �Chances of abuse by using excessive amount of bleach for too many hours per day.
�Commonly used solution for nightguard bleaching: � • 10 percent carbamide peroxide with or without carbopol. � • 15 percent carbamide peroxide � • Hydrogen peroxide (1 -10%).
Steps of Tray Fabrication �Take the impression and make a stone model. � Trim the model. � Place the stock out resin and cure it. � Apply separating media. � Choose the tray sheet material. � Nature of material used for fabrication of bleaching tray is flexible plastic. Most common tray material used is ethyl vinyl acetate.
�Cast the plastic in vacuum tray forming machines. � Trim and polish the tray. � Checking the tray for correct fit, retention and overextension �Demonstrate the amount of bleaching material to be placed.
�Thickness of Tray � Standard thickness of tray is 0. 035 inch. � Thicker tray, i. e. 0. 05 inch is indicated in patients with breaking habit. � Thinner tray, i. e. 0. 02 inch thick is indicated in patients who gag.
Treatment Regimen �When and how long to keep the trays in the mouth, depends on patients lifestyle preference and schedule. �Wearing the tray during day time allows replenishment of the gel after 1 -2 hours for maximum concentration. �Overnight use causes decrease in loss of material due to decreased salivary flow at night and decreased occlusal pressure. � Patient is recalled 1 -2 weeks after wearing the tray.
Side Effects of Home Bleaching �Gingival irritation—Painful gums after a few days of wearing trays. �Soft tissue irritation—From excessive wearing of the trays or applying too much bleach to the trays. �Altered taste sensation—Metallic taste immediately after removing trays. �Tooth sensitivity—Most common side effect.
IN-OFFICE BLEACHING THERMOCATALYTIC VITAL TOOTH BLEACHING �Equipment needed for in-office bleaching are: �Power bleach material. �Tissue protector. �Energizing/activating source. �Protective clothing and eye wear. �Mechanical timer.
Light Sources Used In-office Bleach �Various available light sources are: 1. Conventional bleaching light. 2. Tungsten halogen curing light. 3. Xenon plasma arc light. 4. Argon and CO 2 lasers. 5. Diode laser light.
�Indications of In-office Bleaching �Superficial stains. �Moderate to mild stains. �Contraindications of In-office Bleaching �Tetracycline stains. �Extensive restorations �Severe discolorations. �Extensive caries. �Patient sensitive to bleaching agents.
�Advantages of In-office Bleaching �Patient preference. �Less time than overall time needed for home bleaching. �Patient motivation. �Protection of soft tissues.
�Disadvantages of In-office Bleaching �More chair time. �More expensive. �Unpredictable and deterioration of color is quicker. �More frequent and longer appointment. �Dehydration of teeth. �Serious safety considerations. �Not much research to support its use. �Discomfort of rubber dam.
Procedures 1. Pumice the teeth to clean off any debris present on the tooth surface. 2. Isolate the teeth with rubber dam. 3. Saturate the cotton or gauze piece with bleaching solution (30 -35% H 2 O 2) and place it on the teeth. 4. Depending upon light, expose the tooth/teeth. 5. Change solution in between after every 4 to 5 minutes.
6. Remove solution with the help of wet gauge. 7. Repeat the procedure until desired shade is produced. 8. Remove solution and irrigate teeth thoroughly with warm water. 9. Polish teeth and apply neutral sodium fluoride gel. 10. Instruct the patient to avoid coffee, tea, etc. for 2 weeks. 11. Second and third appointment is given after 3 -6 weeks. This will allow pulp to settle.
MICROABRASION �It is a procedure in which a microscopic layer of enamel is simultaneously eroded and abraded with a special compound (usually contains 18% of hydrochloric acid) leaving a perfectly intact enamel surface behind. �Indications �Developmental intrinsic stains and discolorations limited to superficial enamel only. �Enamel discolorations as a result of hypomineralization or hypermineralization. �Decalcification lesions from stasis of plaque and from orthodontic bands. �Areas of enamel fluorosis. �Multicolored superficial stains and some irregular surface texture.

�Contraindications �Age related staining. �Deep enamel hypoplastic lesions. �Areas of deep enamel and dentin stains. �Amelogenesis imperfecta and dentinogenesi imperfecta cases. �Tetracycline staining. �Carious lesions underlying regions of decalcification.
�Advantages �Minimum discomfort to patient. �Can be easily done in less time by operator. �Useful in removing superficial stains. �The surface of treated tooth is shiny and smooth in nature. �Disadvantages �Not effective for deeper stains. �Removes enamel layer. Yellow discoloration of teeth has been reported in some cases after treatment.
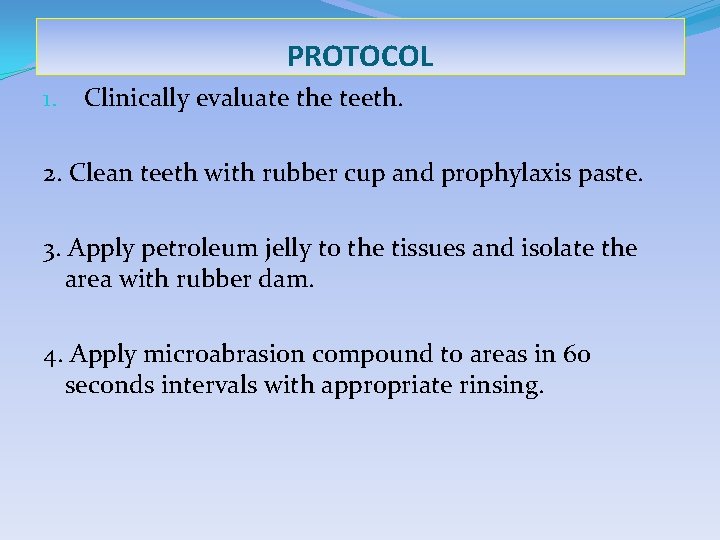
PROTOCOL 1. Clinically evaluate the teeth. 2. Clean teeth with rubber cup and prophylaxis paste. 3. Apply petroleum jelly to the tissues and isolate the area with rubber dam. 4. Apply microabrasion compound to areas in 60 seconds intervals with appropriate rinsing.
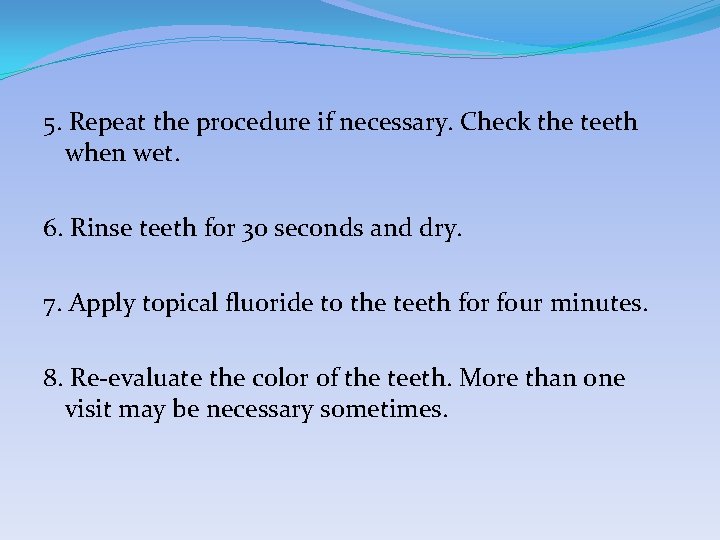
5. Repeat the procedure if necessary. Check the teeth when wet. 6. Rinse teeth for 30 seconds and dry. 7. Apply topical fluoride to the teeth for four minutes. 8. Re-evaluate the color of the teeth. More than one visit may be necessary sometimes.
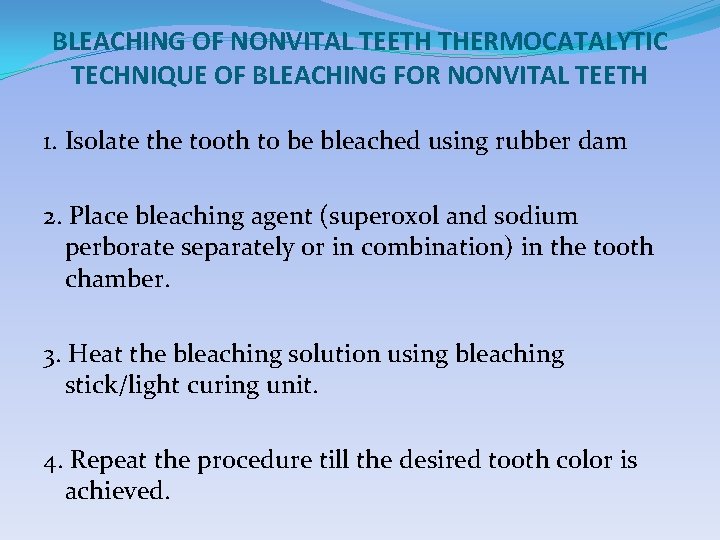
BLEACHING OF NONVITAL TEETH THERMOCATALYTIC TECHNIQUE OF BLEACHING FOR NONVITAL TEETH 1. Isolate the tooth to be bleached using rubber dam 2. Place bleaching agent (superoxol and sodium perborate separately or in combination) in the tooth chamber. 3. Heat the bleaching solution using bleaching stick/light curing unit. 4. Repeat the procedure till the desired tooth color is achieved.
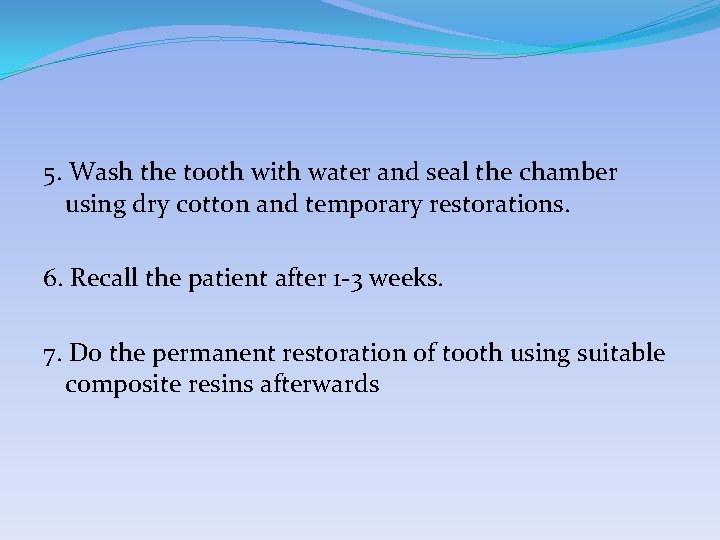
5. Wash the tooth with water and seal the chamber using dry cotton and temporary restorations. 6. Recall the patient after 1 -3 weeks. 7. Do the permanent restoration of tooth using suitable composite resins afterwards
INTRACORONAL BLEACHING/WALKING BLEACH OF NONVITAL TEETH �It involves use of chemical agents within the coronal portion of an endodontically treated tooth to remove tooth discoloration. �Indications of Intracoronal Bleaching • Discoloration of pulp chamber origin • Moderate to severe tetracycline staining. • Dentin discoloration. • Discoloration not agreeable to extracoronal bleaching. �Contraindications of Intracoronal Bleaching • Superficial enamel discoloration. • Defective enamel formation. • Presence of caries. • Unpredictable prognosis of tooth.
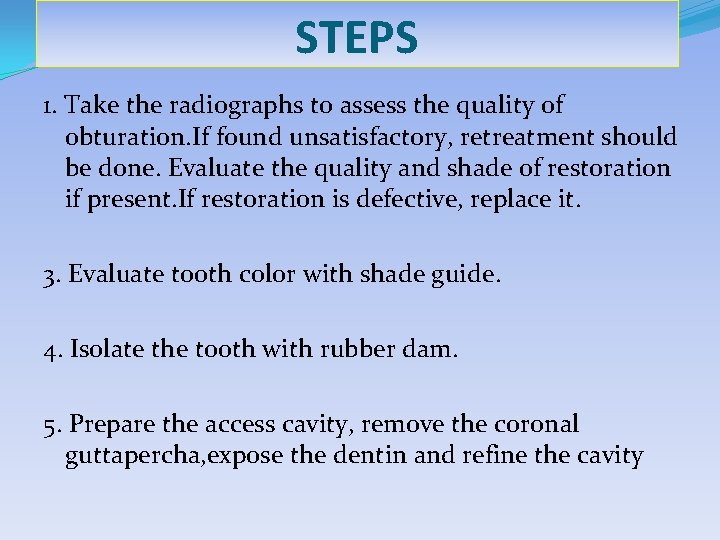
STEPS 1. Take the radiographs to assess the quality of obturation. If found unsatisfactory, retreatment should be done. Evaluate the quality and shade of restoration if present. If restoration is defective, replace it. 3. Evaluate tooth color with shade guide. 4. Isolate the tooth with rubber dam. 5. Prepare the access cavity, remove the coronal guttapercha, expose the dentin and refine the cavity
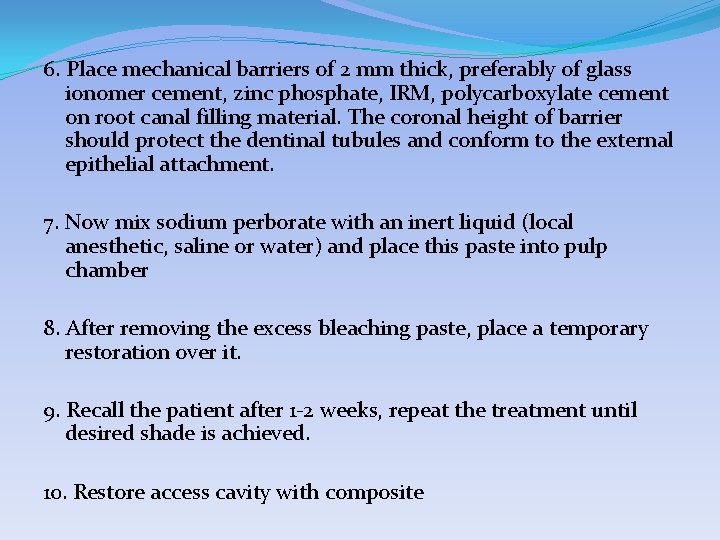
6. Place mechanical barriers of 2 mm thick, preferably of glass ionomer cement, zinc phosphate, IRM, polycarboxylate cement on root canal filling material. The coronal height of barrier should protect the dentinal tubules and conform to the external epithelial attachment. 7. Now mix sodium perborate with an inert liquid (local anesthetic, saline or water) and place this paste into pulp chamber 8. After removing the excess bleaching paste, place a temporary restoration over it. 9. Recall the patient after 1 -2 weeks, repeat the treatment until desired shade is achieved. 10. Restore access cavity with composite
�Complications of Intracoronal Bleaching � • External root resorption. � • Chemical burns if using 30 -35 percent H 2 O 2. � • Decrease bond strength of composite.
�Precautions to be Taken for Safer Nonvital Bleaching 1. Isolate tooth effectively. 2. Protect oral mucosa. 3. Verify adequate endodontic obturation. 4. Use protective barriers. 5. Avoid acid etching. 6. Avoid strong oxidizers. 7. Avoid heat. 8. Recall periodically
 Classification of tooth discoloration
Classification of tooth discoloration Lintrinsic
Lintrinsic What is expressive criticism
What is expressive criticism Extrinsic elements of poetry
Extrinsic elements of poetry Semiconductor conductivity vs temperature
Semiconductor conductivity vs temperature Intrinsic and extrinsic parameters of food
Intrinsic and extrinsic parameters of food Intrinsic property
Intrinsic property What is extrinsic elements
What is extrinsic elements Intrinsic and extrinsic character traits
Intrinsic and extrinsic character traits Extrinsic and intrinsic aids to statutory interpretation
Extrinsic and intrinsic aids to statutory interpretation Intrinsic vs extrinsic feedback
Intrinsic vs extrinsic feedback Example of motivation
Example of motivation An eye for an eye a tooth for a tooth sister act
An eye for an eye a tooth for a tooth sister act Dental mobility classification
Dental mobility classification Glickman furcation classification
Glickman furcation classification Tooth classification and numbering systems
Tooth classification and numbering systems Isthmus width is 1/4th intercuspal distance
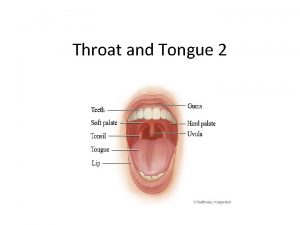
Isthmus width is 1/4th intercuspal distance Genioglossus innervation
Genioglossus innervation Muir v keay
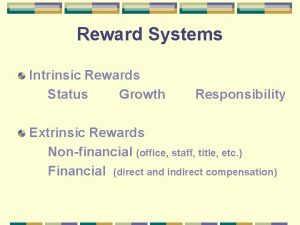
Muir v keay Extrinsic rewards
Extrinsic rewards Specialized mucosa
Specialized mucosa Genioglossus muscle
Genioglossus muscle Causes of hemolysis
Causes of hemolysis Intrinsic factors for microbial growth
Intrinsic factors for microbial growth Tapetum eye
Tapetum eye Extrinsic hemolytic anemia
Extrinsic hemolytic anemia Hard palate
Hard palate Extrinsic rewards
Extrinsic rewards Extrinsic rewards
Extrinsic rewards Extrinsic rewards
Extrinsic rewards Fibrous tunic
Fibrous tunic Appeal to kairos
Appeal to kairos Courstey
Courstey Extrinsic camera calibration
Extrinsic camera calibration Audionyms
Audionyms Dynamic model of wellbeing
Dynamic model of wellbeing Motivational cycle
Motivational cycle Superior intercostal artery
Superior intercostal artery Intrinsic value of stock formula
Intrinsic value of stock formula Intrinsic laryngeal muscle
Intrinsic laryngeal muscle Hugo van bever
Hugo van bever Ujt ppt
Ujt ppt Intrinsic impedance of lossy dielectric medium
Intrinsic impedance of lossy dielectric medium Intrinsic foot muscles
Intrinsic foot muscles Teacher feedback for students examples
Teacher feedback for students examples Intrinsic magnetic field
Intrinsic magnetic field Intrinsic carrier density
Intrinsic carrier density