Thoracic pancreatic pseudocyst presenting as a pulmonary pseudotumour
- Slides: 21
Thoracic pancreatic pseudocyst presenting as a pulmonary pseudotumour with spontaneous decompression via a pancreatico-bronchial fistula Dr Martin Lewis Sp. R 1, 2, Dr Thomas Glover Sp. R 1, 3, Dr Zybnek Stetina Consultant Radiologist 1 Kingston University Hospital NHS Trust 2 St Georges University Hospitals NHS Foundation Trust 3 Chelsea and Westminster Hospital NHS Foundation Trust 1
Clinical Information • 54 year old male of no fixed abode, attended emergency department via ambulance. • PC – One month of mild left sided abdominal pain. No other symptoms. • O/E – Intoxicated, sarcopenic and unkempt. Otherwise unremarkable examination. Afebrile. Vital signs within normal limits. • PMHx – nil. DHx – Nil. SHx – Nil. No previous presentations. GP in Luton. • Bloods - WCC 13. 9 (Neut 11. 0, Mono 1. 8, Eos 0. 1, Bas 0. 1), Lymph 0. 9. - Hb 11. 4 (MCV 92), Plts 675 - Na 135, K 4. 5, Ur 6. 0, Cr 60 - Bilirubin 13, AST 19, ALP 75, Albumin 35 - CRP 246 - Lipase 137 - Ca 2. 3 - INR 1. 3
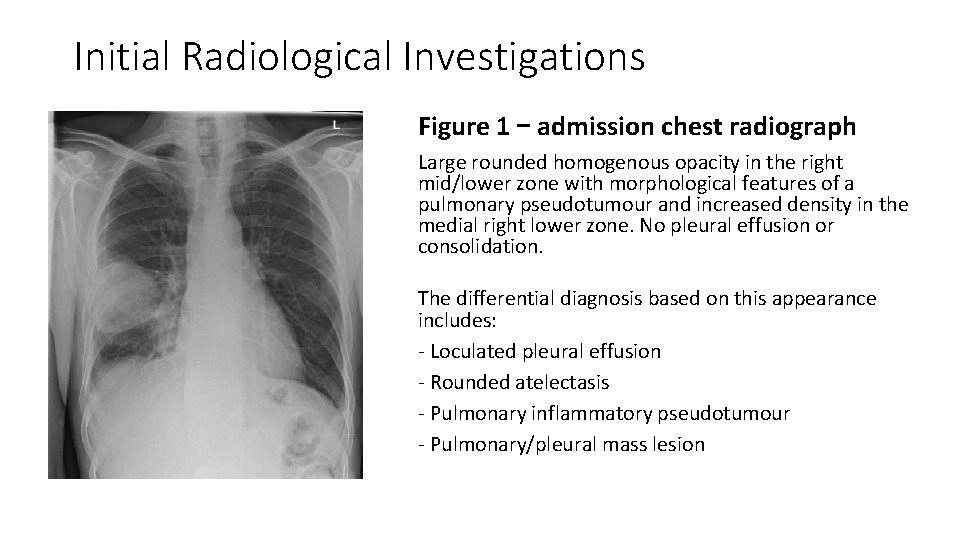
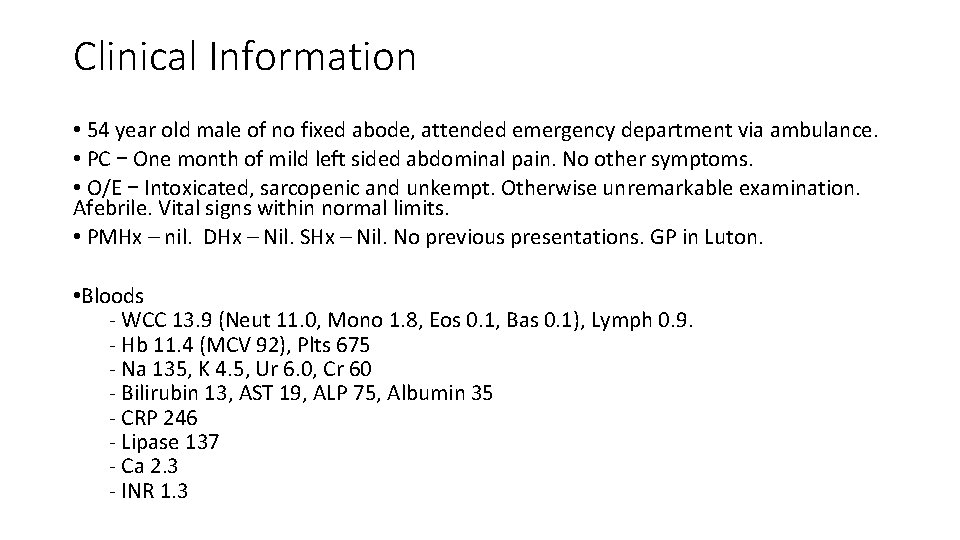
Initial Radiological Investigations Figure 1 – admission chest radiograph Large rounded homogenous opacity in the right mid/lower zone with morphological features of a pulmonary pseudotumour and increased density in the medial right lower zone. No pleural effusion or consolidation. The differential diagnosis based on this appearance includes: - Loculated pleural effusion - Rounded atelectasis - Pulmonary inflammatory pseudotumour - Pulmonary/pleural mass lesion
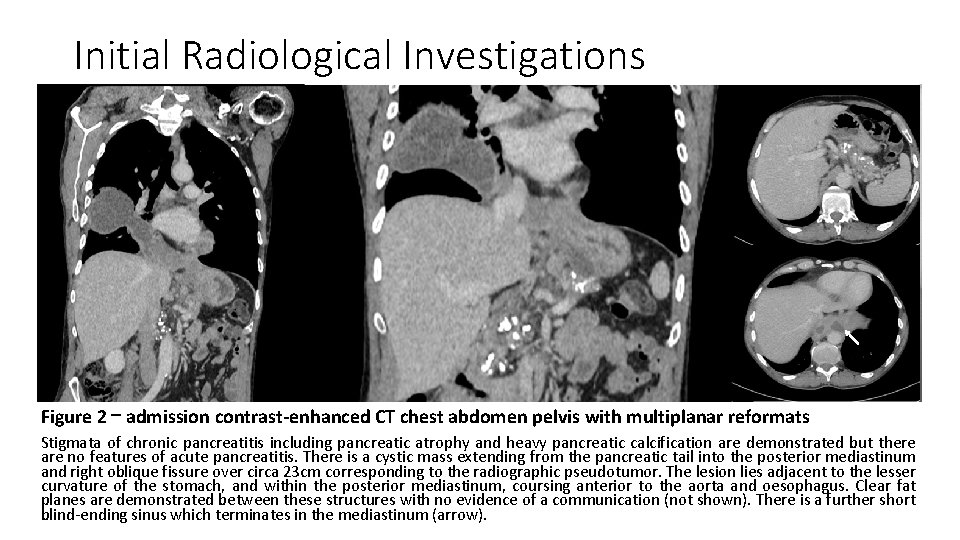
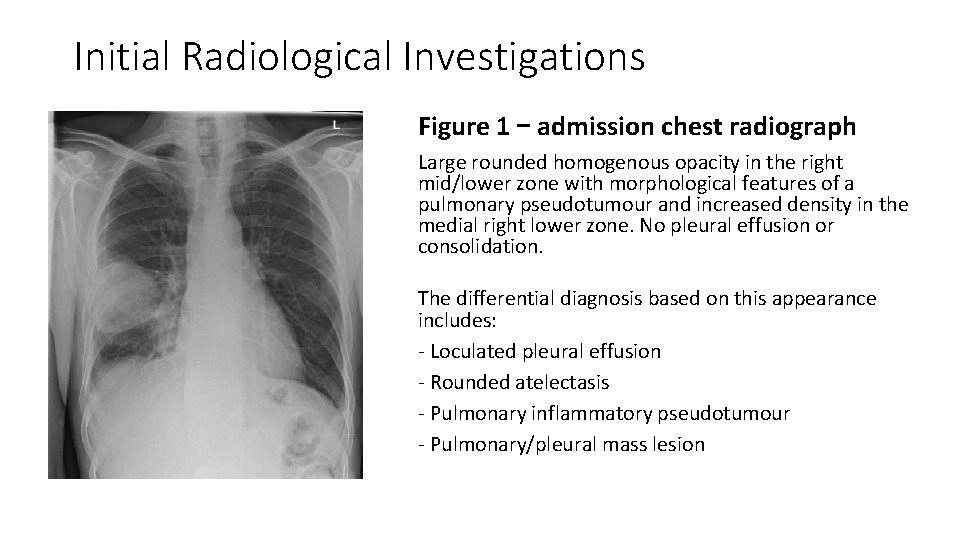
Initial Radiological Investigations Figure 2 – admission contrast-enhanced CT chest abdomen pelvis with multiplanar reformats Stigmata of chronic pancreatitis including pancreatic atrophy and heavy pancreatic calcification are demonstrated but there are no features of acute pancreatitis. There is a cystic mass extending from the pancreatic tail into the posterior mediastinum and right oblique fissure over circa 23 cm corresponding to the radiographic pseudotumor. The lesion lies adjacent to the lesser curvature of the stomach, and within the posterior mediastinum, coursing anterior to the aorta and oesophagus. Clear fat planes are demonstrated between these structures with no evidence of a communication (not shown). There is a further short blind-ending sinus which terminates in the mediastinum (arrow).
Initial Impressions • Clinical impression: • Mild acute-on-chronic pancreatitis • Infection (but patient afebrile and no systemic manifestations of sepsis) • Low lymphocyte count ? immunosuppression secondary to ETOH excess • Working radiological diagnosis: Pancreatic pseudocyst with intrathoracic extension and possible super-added infection Differential diagnosis: - Perforation of the gastro-oesophageal junction - Ulcerating malignancy of the upper GI tract with abscess formation - Tuberculous abscess • Clinical management – empirical intravenous antibiotics, fluids and bowel rest
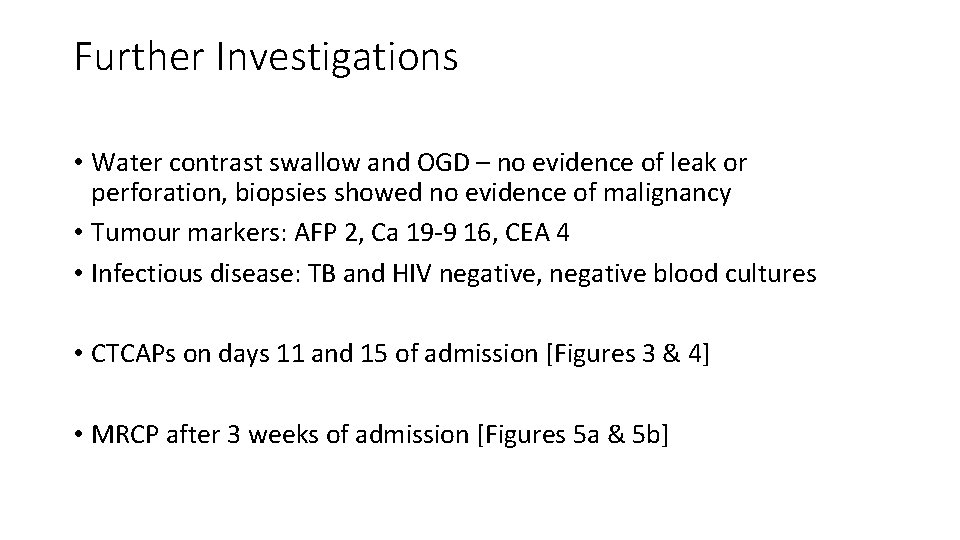
Further Investigations • Water contrast swallow and OGD – no evidence of leak or perforation, biopsies showed no evidence of malignancy • Tumour markers: AFP 2, Ca 19 -9 16, CEA 4 • Infectious disease: TB and HIV negative, negative blood cultures • CTCAPs on days 11 and 15 of admission [Figures 3 & 4] • MRCP after 3 weeks of admission [Figures 5 a & 5 b]
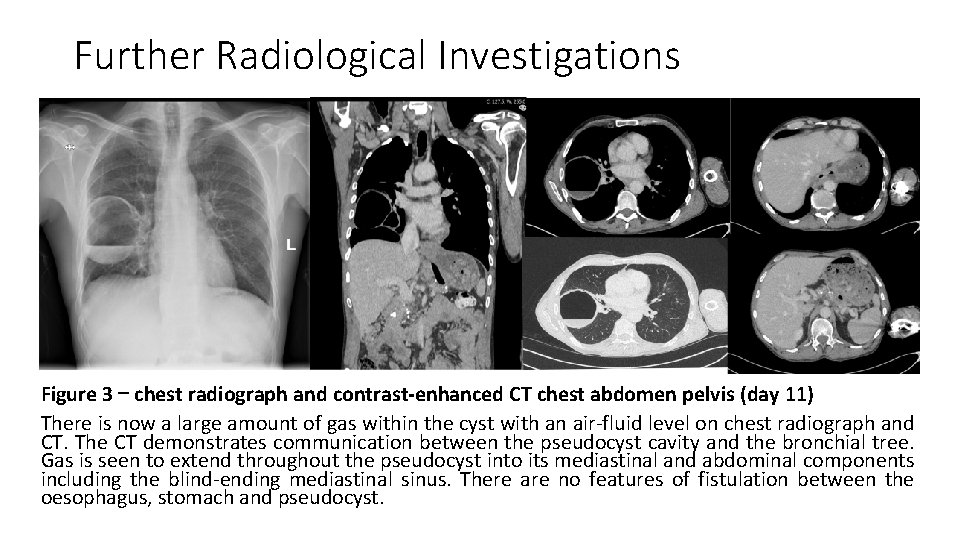
Further Radiological Investigations Figure 3 – chest radiograph and contrast-enhanced CT chest abdomen pelvis (day 11) There is now a large amount of gas within the cyst with an air-fluid level on chest radiograph and CT. The CT demonstrates communication between the pseudocyst cavity and the bronchial tree. Gas is seen to extend throughout the pseudocyst into its mediastinal and abdominal components including the blind-ending mediastinal sinus. There are no features of fistulation between the oesophagus, stomach and pseudocyst.
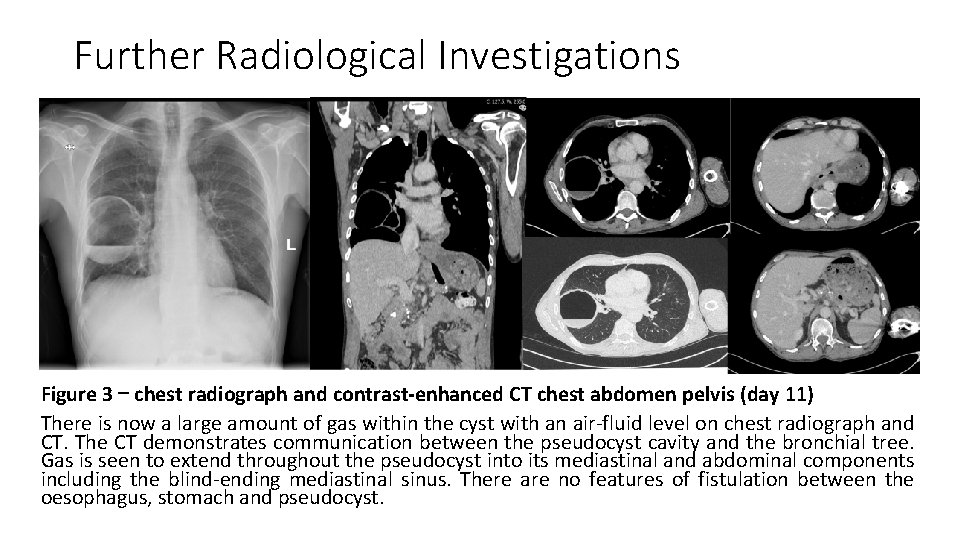
Progress during admission • The patient continued to improve on IV antibiotics • The case was discussed at regional HPB and cardiothoracic MDTs: - HPB MDT : scope for ERCP +/- stent but on risk/benefit analysis interval scanning was deemed most appropriate based on clinical improvement with IV fluids and antibiotics - Cardiothoracic MDT: little scope for intervention, sclerosing agents possible but low efficacy and not indicated given clinical improvement • A further interval CT was performed on day 15 (Figure 4) and an MRCP was performed on day 22 (Figure 5 a & 5 b) • An interval outpatient CT scan has been arranged with a view to discussion for definitive management
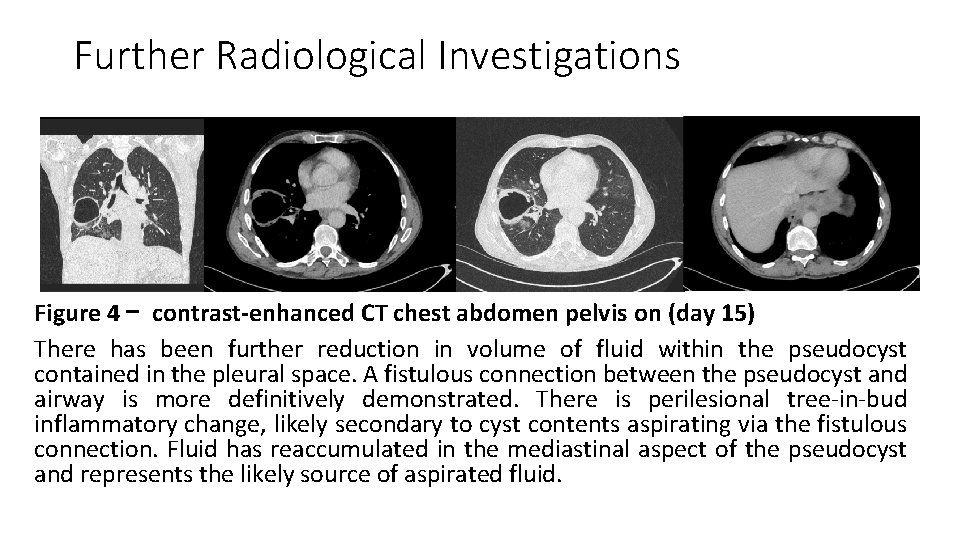
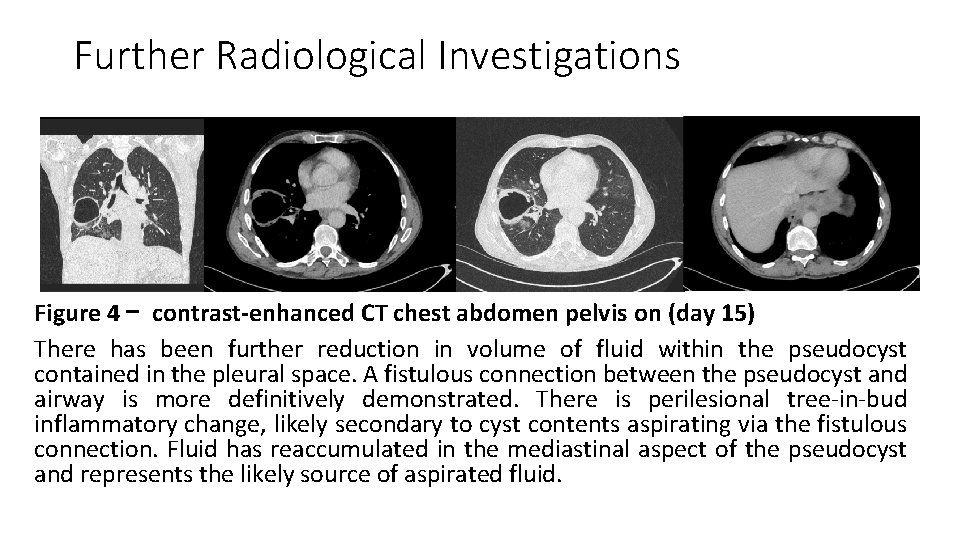
Further Radiological Investigations Figure 4 – contrast-enhanced CT chest abdomen pelvis on (day 15) There has been further reduction in volume of fluid within the pseudocyst contained in the pleural space. A fistulous connection between the pseudocyst and airway is more definitively demonstrated. There is perilesional tree-in-bud inflammatory change, likely secondary to cyst contents aspirating via the fistulous connection. Fluid has reaccumulated in the mediastinal aspect of the pseudocyst and represents the likely source of aspirated fluid.
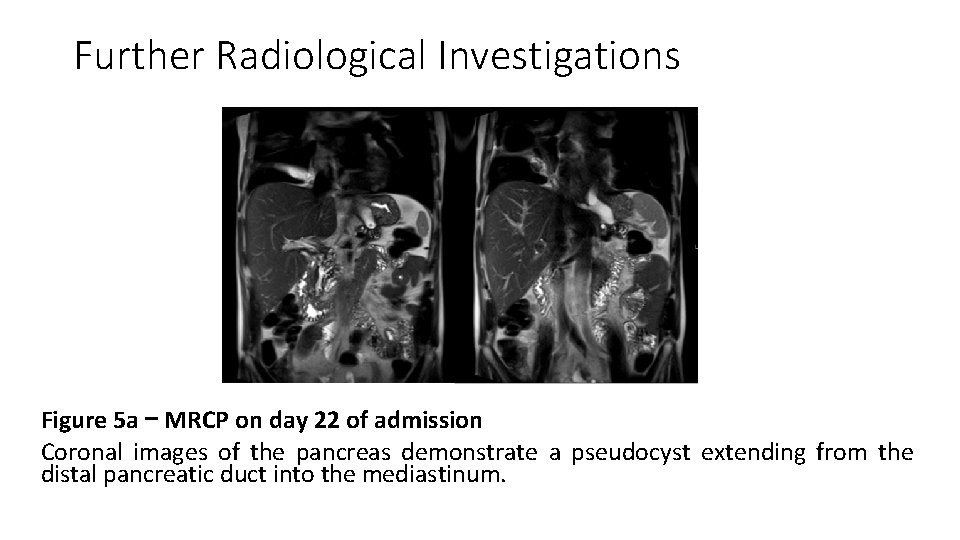
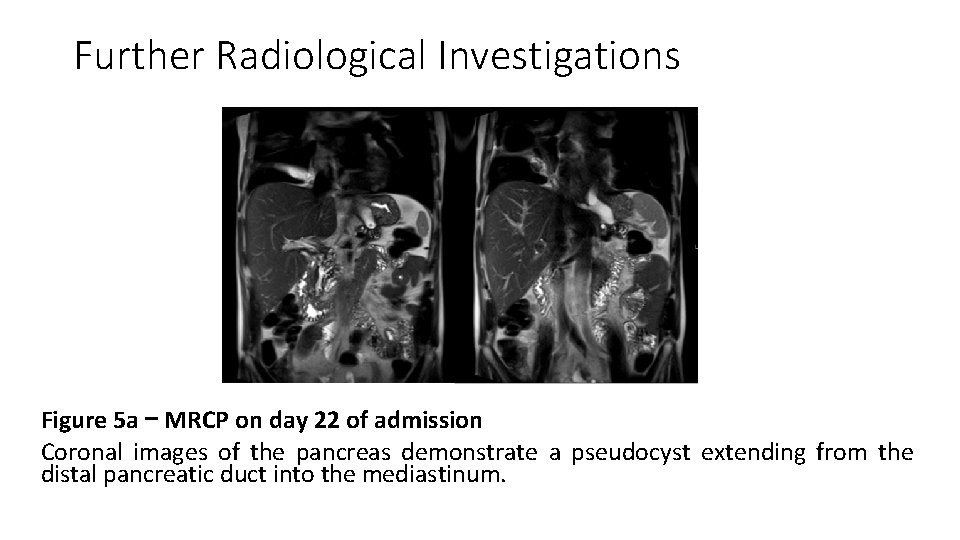
Further Radiological Investigations Figure 5 a – MRCP on day 22 of admission Coronal images of the pancreas demonstrate a pseudocyst extending from the distal pancreatic duct into the mediastinum.
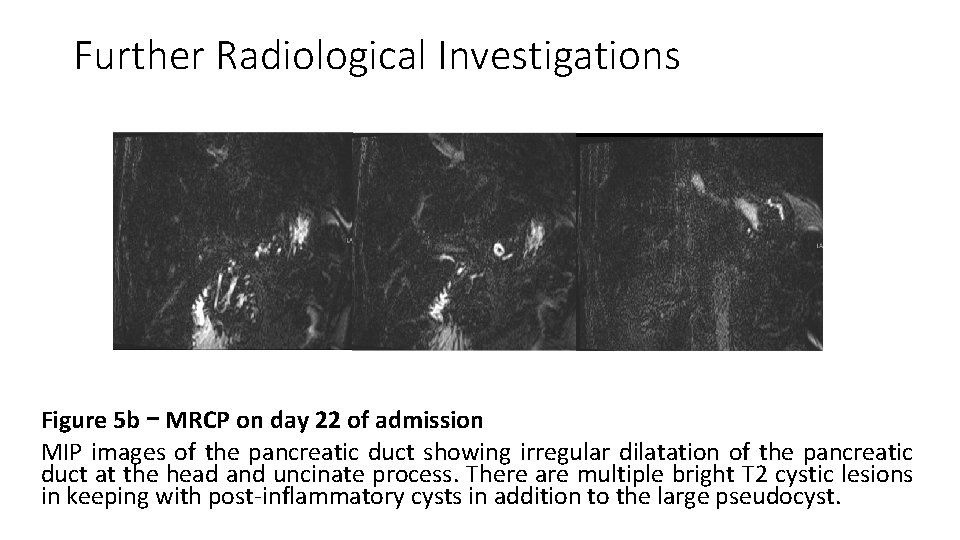
Further Radiological Investigations Figure 5 b – MRCP on day 22 of admission MIP images of the pancreatic duct showing irregular dilatation of the pancreatic duct at the head and uncinate process. There are multiple bright T 2 cystic lesions in keeping with post-inflammatory cysts in addition to the large pseudocyst.
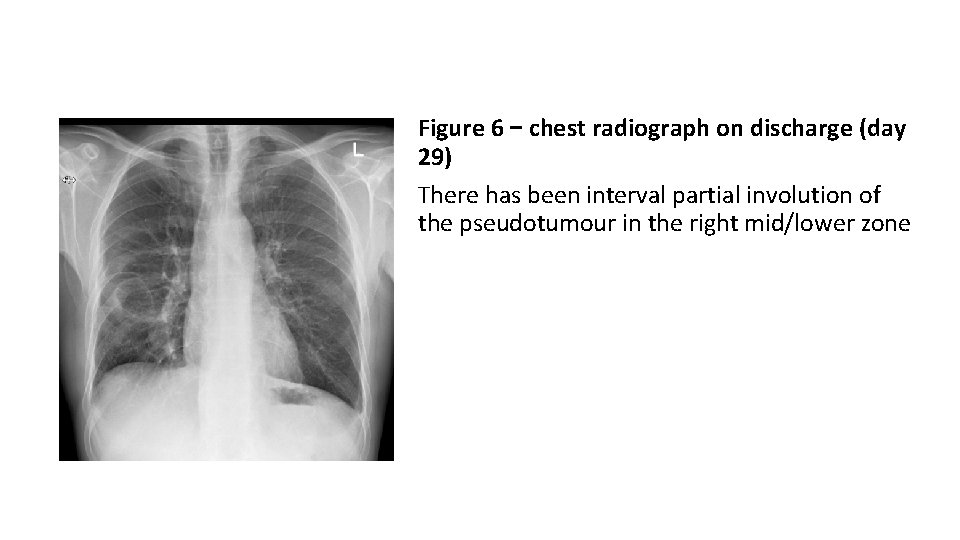
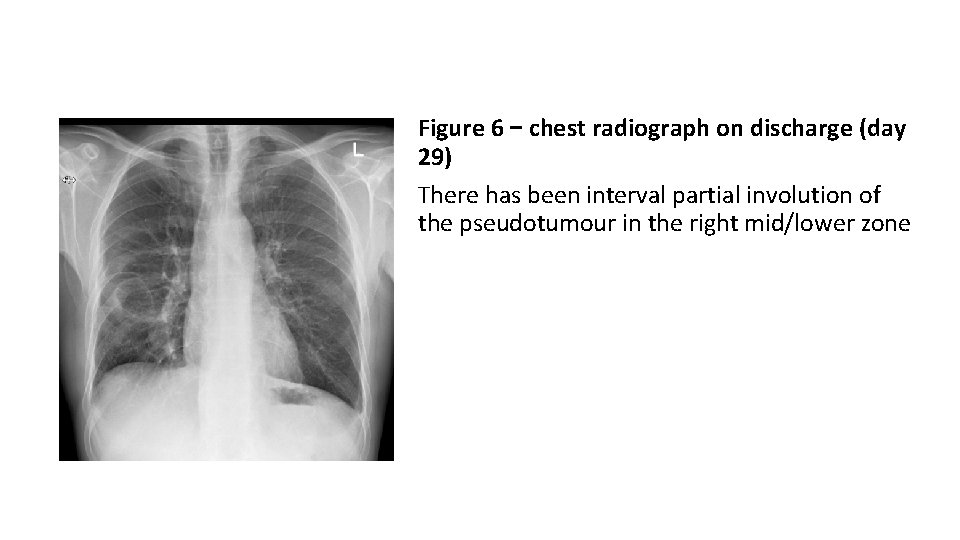
Figure 6 – chest radiograph on discharge (day 29) There has been interval partial involution of the pseudotumour in the right mid/lower zone
Final Diagnosis • Mild acute pancreatitis on background of ETOH-induced chronic pancreatitis - Classical imaging findings on CT and MRI - Biochemical pancreatitis (↑Lipase, CRP, WCC) • Mediastinal pancreatic pseudocyst with no convincing features of infection - Multiple imaging modalities demonstrating a pseudocyst extending into the mediastinum and right oblique fissure - MRCP demonstrates a connection between the pseudocyst and distal pancreatic duct - Biochemical markers aside (↑WCC & CRP), there were no physical signs of sepsis • Pancreatico-bronchial fistula - CT demonstrates a fistulous connection between pseudocyst and airway. Serial chest radiographs and CTs demonstrate gradual decompression and involution of the cavity with time, likely due to expectoration - CT and MRI excluded a fistula with the upper gastrointestinal tract
Summary • We report a very rare case of a thoracic pancreatic pseudocyst presenting as a pulmonary pseudotumour and spontaneously decompressing via a pancreatico-bronchial fistula • This was an incidental presentation after being taken to the emergency department as a result of intoxication • The patient progressed well clinically with IV antibiotics and supportive measures and was discharged without any specific intervention
Discussion (Pathophysiology) • Thoracic extension of pancreatic pseudocysts is very rare (cases < 100) • The initial pathophysiological trigger is disruption of the pancreatic duct with leakage of enzymes into the retroperitoneum and diaphragmatic hiatus 1 - The MRCP demonstrates classical imaging features with multiple pseudocysts, an irregular dilated pancreatic duct, and communication between the duct and the large mediastinal pseudocyst • Once in the mediastinum, a pseudocyst can remain as a pseudocyst or transform into a pancreaticopleural fistula - Rupture of a pseudocyst into the pleural cavity typically presents with a pleural effusion. High amylase content in aspirated pleural fluid is confirmatory. Pleural extension without effusion is a less common appearance as larger cysts are much more prone to rupture 2
Discussion (Pathophysiology) • Subsequent communication between the pancreas and the bronchial tree is the rarest of thoracic complications, and is often associated with grave consequences 3, 4. - No pleural effusion is present and therefore diagnosis most often relies on multiple imaging modalities +/- analysis of sputum. Sputum analyses for amylase were not performed during admission.
Discussion (Clinical - Symptoms) • Once the cyst is within the mediastinum a variety of compressive or lytic effects on vascular, bronchial or gastrointestinal structures may result, which along with the anatomical path taken, informs the clinical presentation and imaging findings - Aside from the pancreas, the thoracic pseudocyst did not communicate with any other organs and so the patient was asymptomatic • When fistulation with the bronchus occurs there is often clinical deterioration and features of tracheobronchitis as a result of irritation by proteolytic enzymes 5 - Although bronchial impaction was demonstrated radiologically the patient did not complain of any significant thoracic symptoms
Discussion (Clinical – Management) • The literature thus far contains only limited management suggestions for thoracic pancreatic pseudocysts without standardised guidelines • In general, the primary aim is to decompress the cystic component either surgically (via cystogastrostomy, cystojejunostomy, pancreaticoduodenectomy and pancreatojejunostomy), endoscopically (via ERCP or EUS) or by medical management (octreotide)6 • Cases of spontaneous remission have been reported after initiation of total parenteral nutrition and octreotide therapy - Our case is unique in that there was spontaneous regression of the pseudocyst and clinical improvement with intravenous fluids and antibiotics. Intervention was not required.
Unique points of this case • To our knowledge this is the first case of a mediastinal pseudocyst presenting as a radiographic pseudotumour • Spontaneous regression without intervention is vanishingly rare – to our knowledge this is the first case of such a large pseudocyst regressing with conservative measures (IV fluids & antibiotics) only • Formation of a pancreatico-bronchial fistula often results in significant respiratory symptoms and compromise – fortunately this did not occur in this case
References H. Xu, X. Zhang, A. Christe et al. , “Anatomic pathways of peripancreatic fluid draining to mediastinum in recurrent acute pancreatitis: visible human project and CT study, ” PLo. S ONE, vol. 8, no. 4, Article IDe 62025, 2013. 1 2 Ramahi A et al. “Pancreaticopleural fistula: A rare presentation and a rare complication”. Cureus 2019 Jun 24; 11(6): e 4984 3 Iglehart et al. Pancreaticobronchial fistula. Case report and review of the literatures. Gastroentrology 1986; 90: 756 -63. 4 Misare BD et al. Pancreaticobronchial fistula causing lung abscess: case report and brief discussion of the literature. Surgery 1991; 110: 549– 51. 5 Yasuda T et al. Pancreaticobronchial fistula associated with chronic pancreatitis: report of a case. Surg Today. 2007; 37(4): 338– 341. 6 Dafni M et al. Surgical Intervention for Mediastinal Pancreatic Pseudocysts. A Case Series and Review of the Literature. JOP. J Pancreas (Online) 2015 Jan 31; 16(1): 74 -77.
Note • The authors note the presentation time of 4 minutes. What we have enclosed is therefore not the final presentation but a demonstration of the key features of the case as requested in the instructions. If selected, the final presentation will be truncated in order to the fit the requirements for oral presentation, and feature higher quality images.
 Acute pancreatitis pes statement
Acute pancreatitis pes statement Which is the largest gland of the body
Which is the largest gland of the body Pancreatic calcification
Pancreatic calcification Pancreatic juice
Pancreatic juice Content of pancreatic juice
Content of pancreatic juice The hepatic portal vein empties into the ____.
The hepatic portal vein empties into the ____. The main jobs of the large intestine are _____.
The main jobs of the large intestine are _____. Stage 2b pancreatic cancer
Stage 2b pancreatic cancer Function of vitamin a
Function of vitamin a Mrcp pancreatic cyst
Mrcp pancreatic cyst Pad sign in pancreatic carcinoma
Pad sign in pancreatic carcinoma Carbohydrates
Carbohydrates Exocrine secretion
Exocrine secretion Pancreatic calcification
Pancreatic calcification Pancreas
Pancreas Moa of glucagon
Moa of glucagon Wikipedia commons
Wikipedia commons Pancreatic juice
Pancreatic juice Canine exocrine pancreatic insufficiency
Canine exocrine pancreatic insufficiency Steatorrhoea pancreatica
Steatorrhoea pancreatica Ralph steinman pancreatic cancer
Ralph steinman pancreatic cancer Pancreatic histology
Pancreatic histology