The External Ear General Compartments External Middle Inner




- Slides: 21
The External Ear
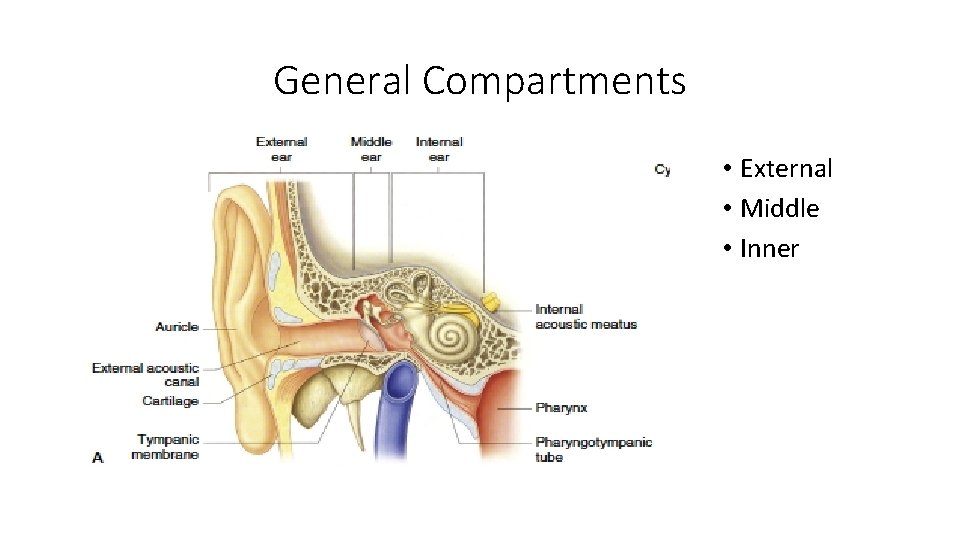
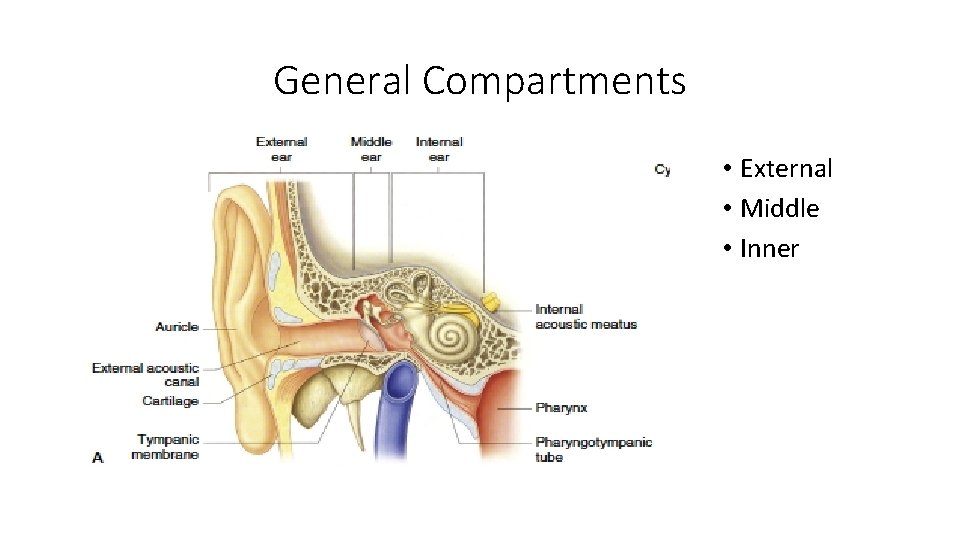
General Compartments • External • Middle • Inner

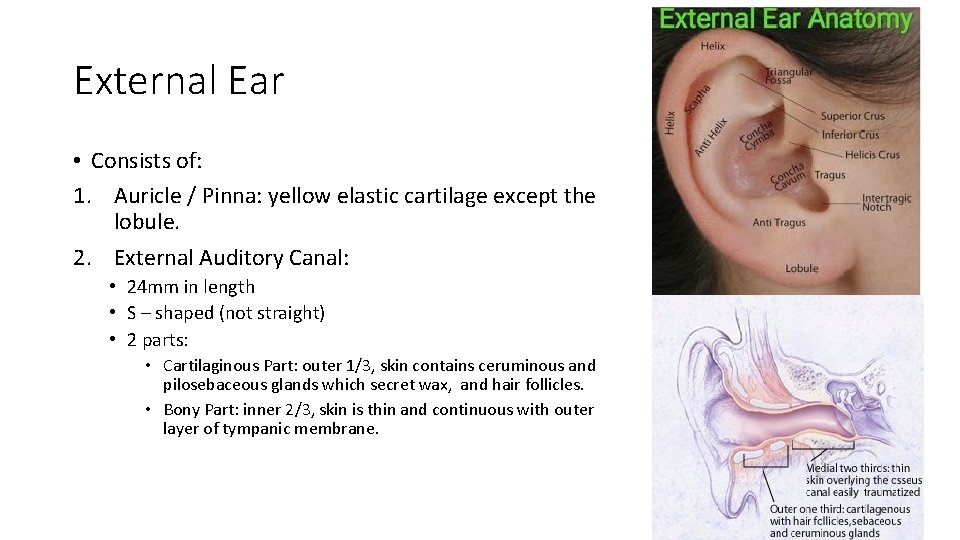
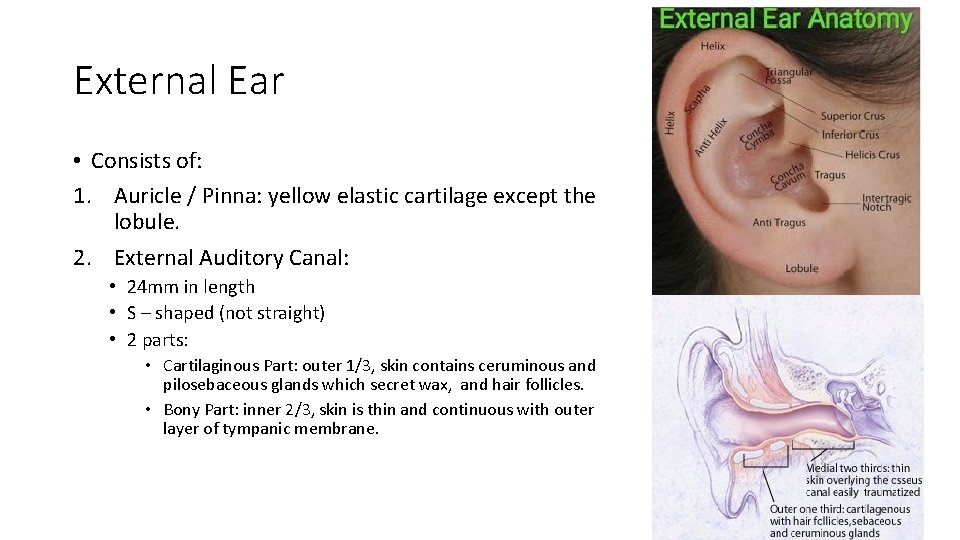
External Ear • Consists of: 1. Auricle / Pinna: yellow elastic cartilage except the lobule. 2. External Auditory Canal: • 24 mm in length • S – shaped (not straight) • 2 parts: • Cartilaginous Part: outer 1/3, skin contains ceruminous and pilosebaceous glands which secret wax, and hair follicles. • Bony Part: inner 2/3, skin is thin and continuous with outer layer of tympanic membrane.
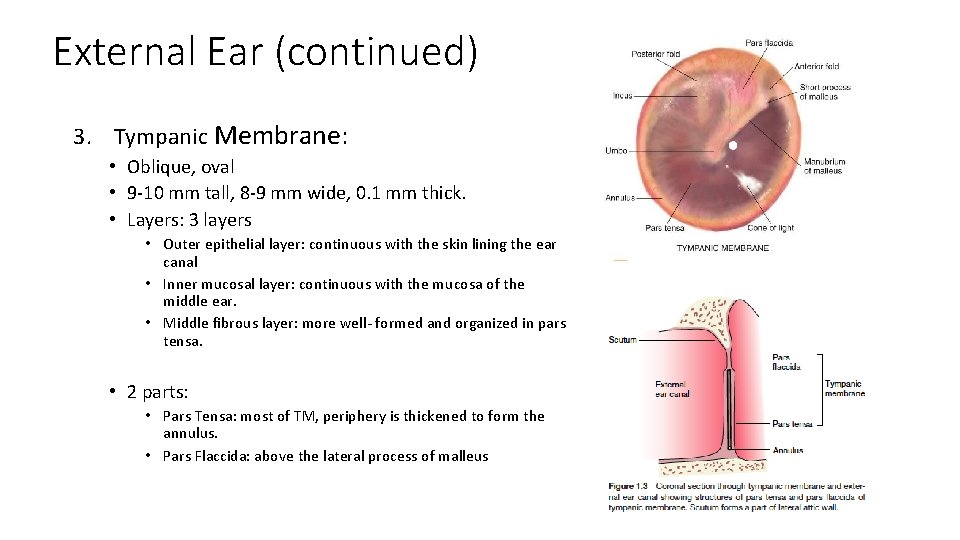
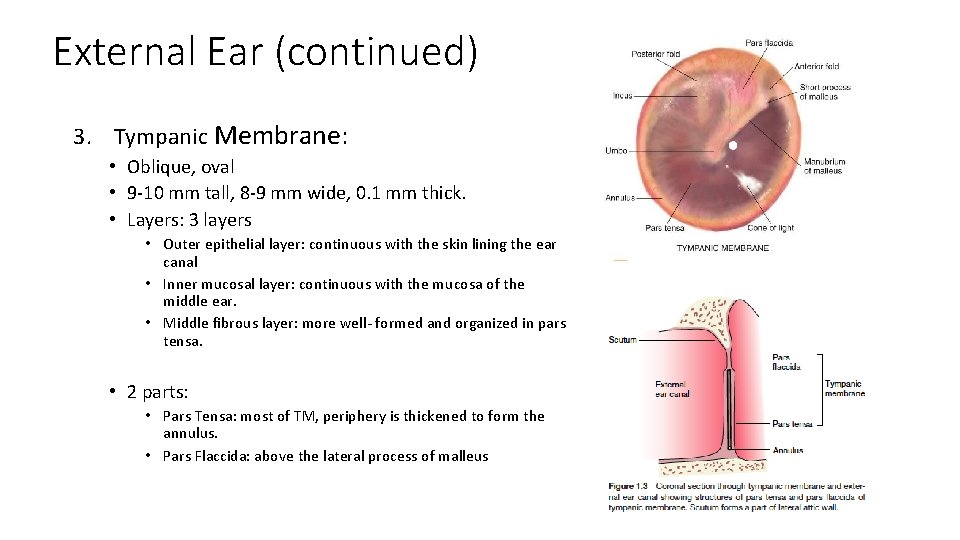
External Ear (continued) 3. Tympanic Membrane: • Oblique, oval • 9 -10 mm tall, 8 -9 mm wide, 0. 1 mm thick. • Layers: 3 layers • Outer epithelial layer: continuous with the skin lining the ear canal • Inner mucosal layer: continuous with the mucosa of the middle ear. • Middle fibrous layer: more well- formed and organized in pars tensa. • 2 parts: • Pars Tensa: most of TM, periphery is thickened to form the annulus. • Pars Flaccida: above the lateral process of malleus

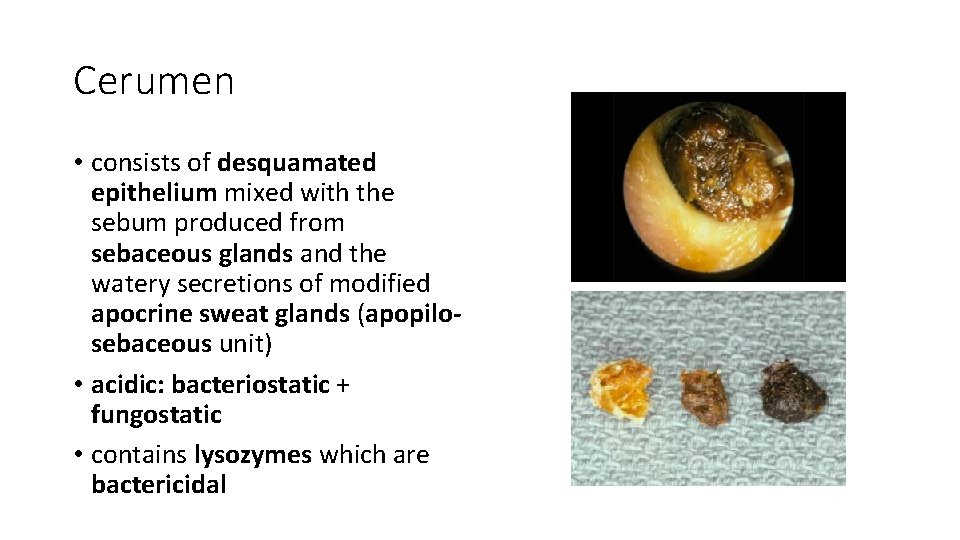
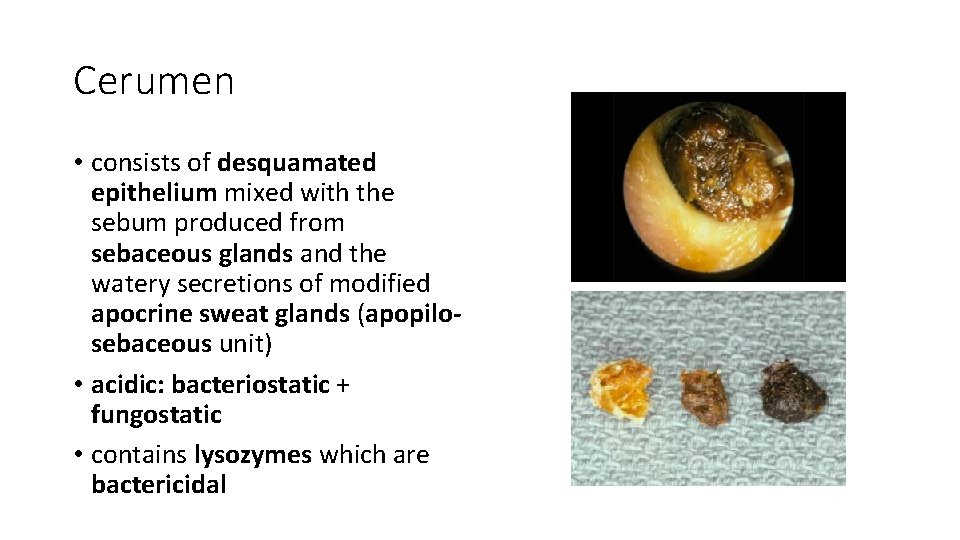
Cerumen • consists of desquamated epithelium mixed with the sebum produced from sebaceous glands and the watery secretions of modified apocrine sweat glands (apopilosebaceous unit) • acidic: bacteriostatic + fungostatic • contains lysozymes which are bactericidal
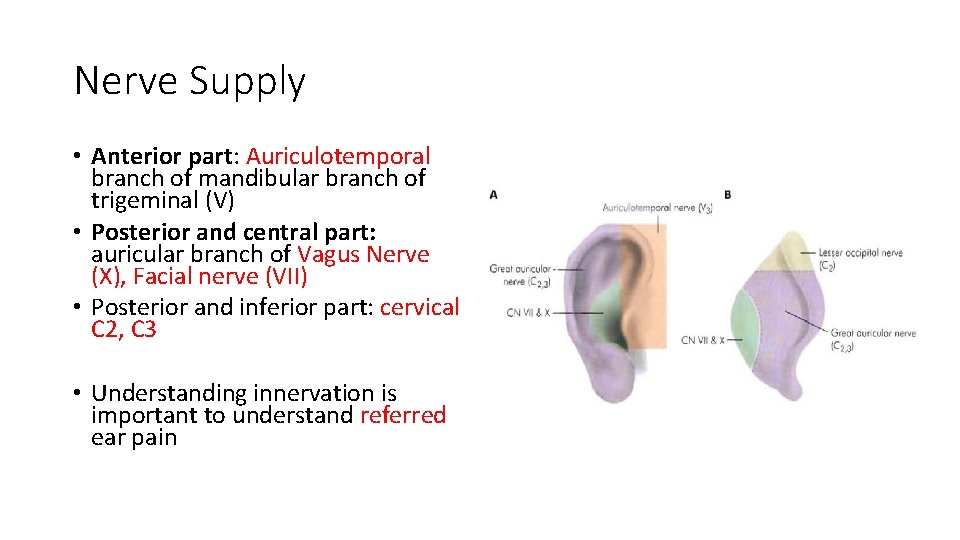
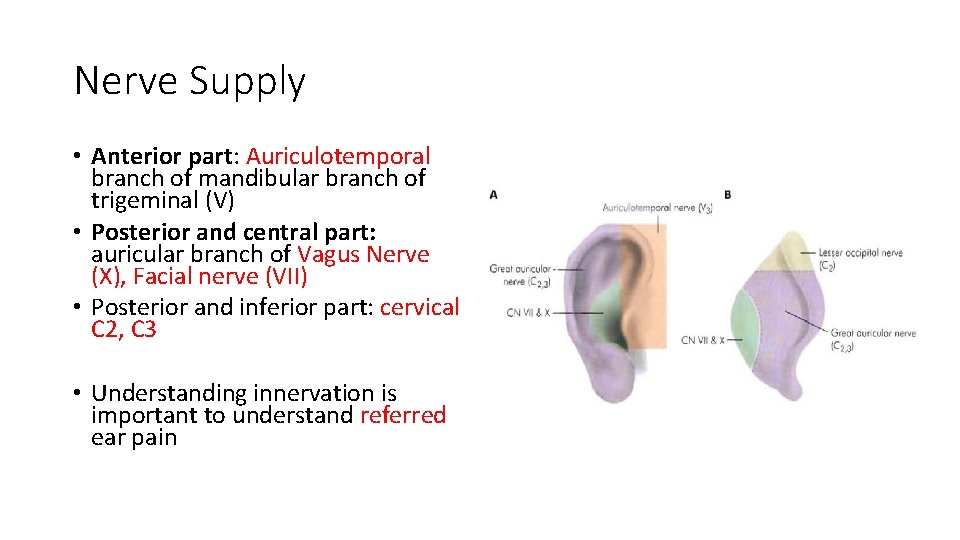
Nerve Supply • Anterior part: Auriculotemporal branch of mandibular branch of trigeminal (V) • Posterior and central part: auricular branch of Vagus Nerve (X), Facial nerve (VII) • Posterior and inferior part: cervical C 2, C 3 • Understanding innervation is important to understand referred ear pain
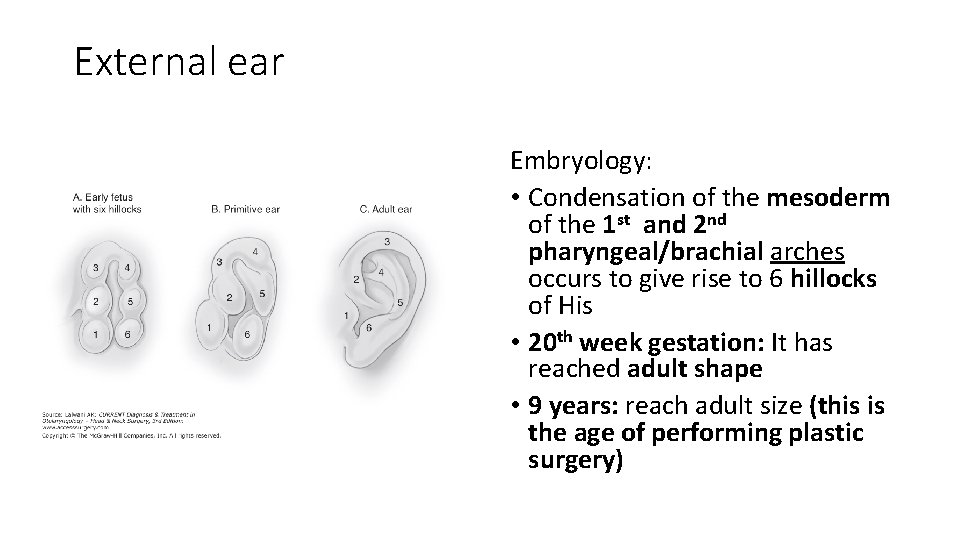
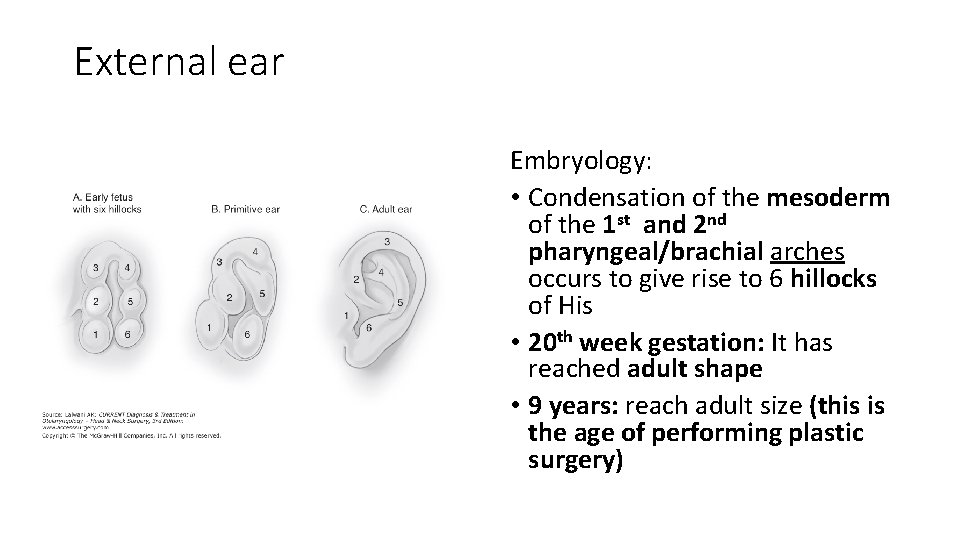
External ear Embryology: • Condensation of the mesoderm of the 1 st and 2 nd pharyngeal/brachial arches occurs to give rise to 6 hillocks of His • 20 th week gestation: It has reached adult shape • 9 years: reach adult size (this is the age of performing plastic surgery)

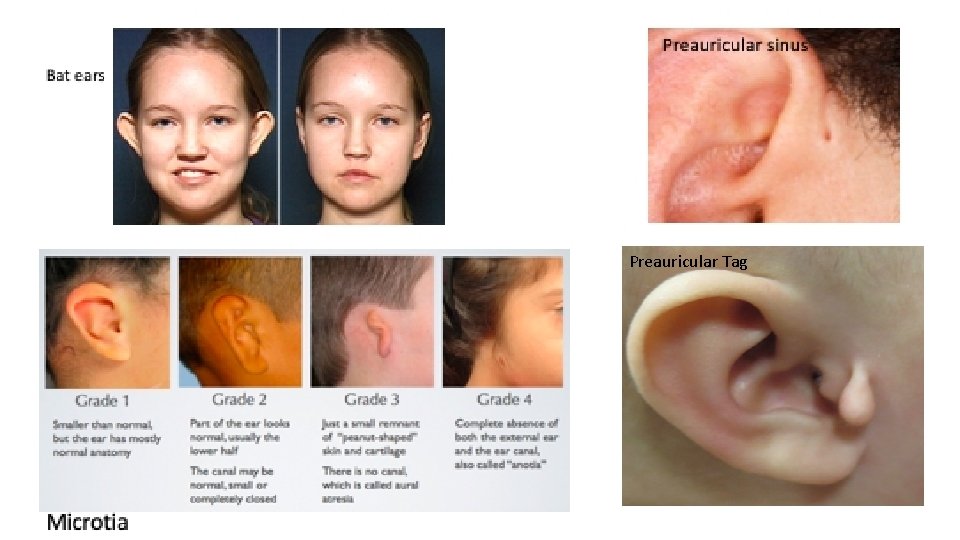
Congenintal anomalies of the Pinna • Preauricular tag • Remnant of one of the hillocks. • Uncertain risk factor for hearing loss. • Preauricular sinus • results from improper fusion of the 1 st & 2 nd brachial arches • May be associated with branchio-oto-renal syndrome • Surgery is only indicated when it is complicated by recurrent infection or abscesses • Microtia: underdeveloped ear pinna • Bat ears: protruding ears, loss of antihelix
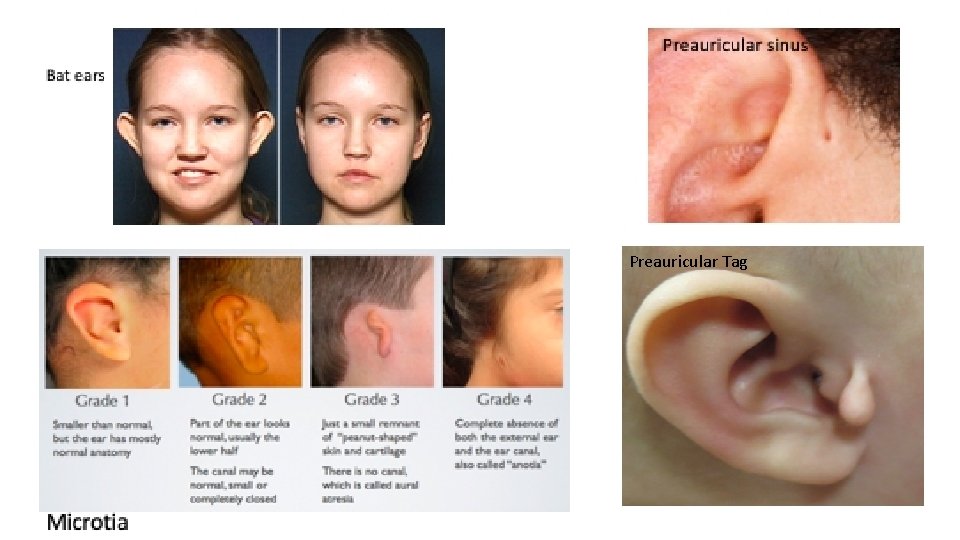
Preauricular Tag
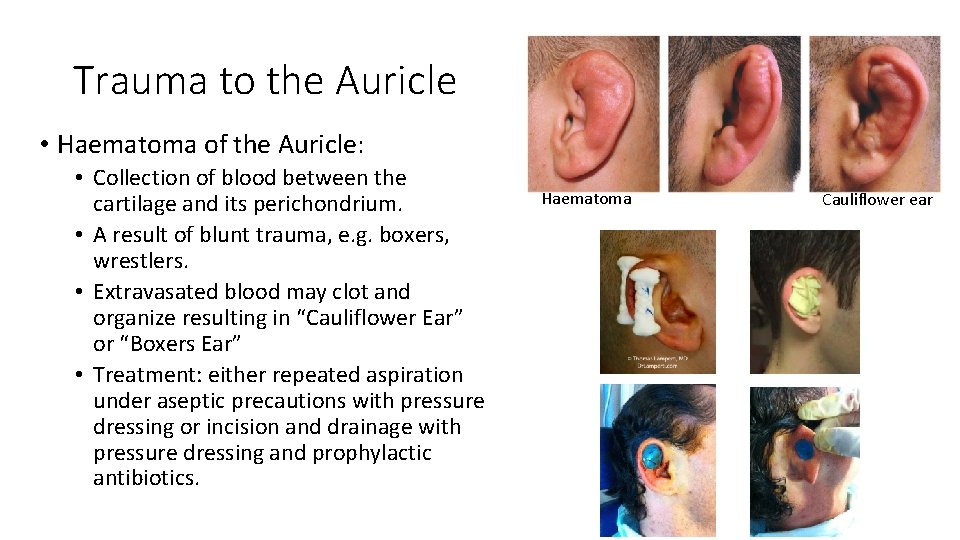
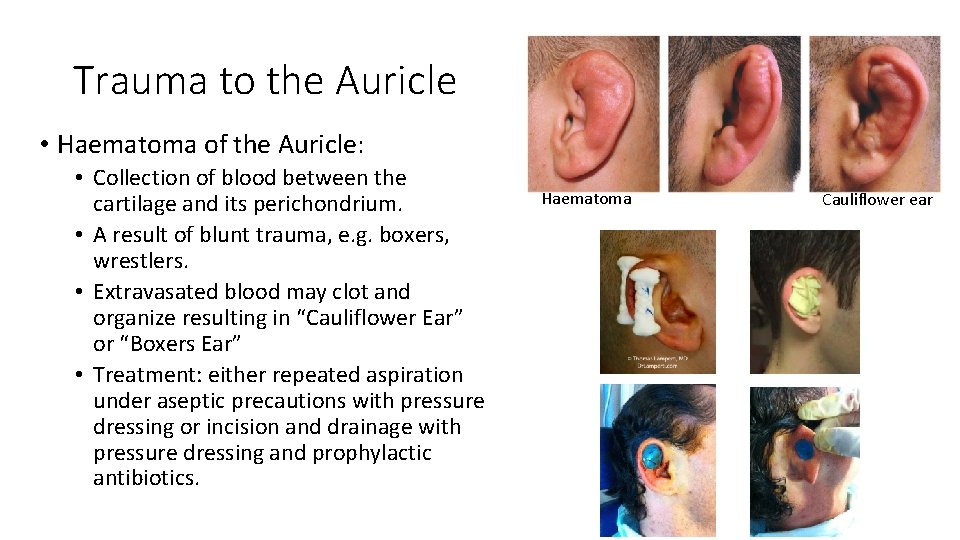
Trauma to the Auricle • Haematoma of the Auricle: • Collection of blood between the cartilage and its perichondrium. • A result of blunt trauma, e. g. boxers, wrestlers. • Extravasated blood may clot and organize resulting in “Cauliflower Ear” or “Boxers Ear” • Treatment: either repeated aspiration under aseptic precautions with pressure dressing or incision and drainage with pressure dressing and prophylactic antibiotics. Haematoma Cauliflower ear
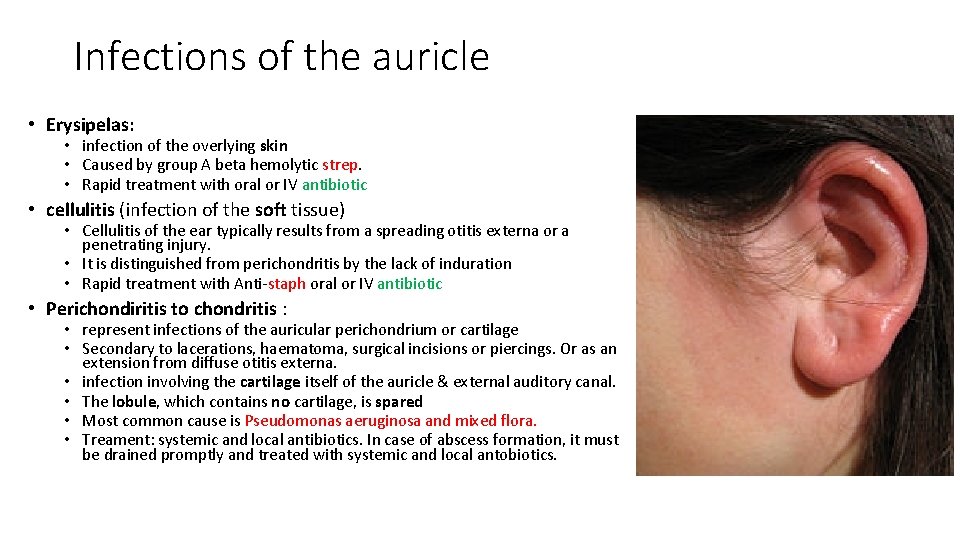
Infections of the auricle • Erysipelas: • infection of the overlying skin • Caused by group A beta hemolytic strep. • Rapid treatment with oral or IV antibiotic • cellulitis (infection of the soft tissue) • Cellulitis of the ear typically results from a spreading otitis externa or a penetrating injury. • It is distinguished from perichondritis by the lack of induration • Rapid treatment with Anti-staph oral or IV antibiotic • Perichondiritis to chondritis : • represent infections of the auricular perichondrium or cartilage • Secondary to lacerations, haematoma, surgical incisions or piercings. Or as an extension from diffuse otitis externa. • infection involving the cartilage itself of the auricle & external auditory canal. • The lobule, which contains no cartilage, is spared • Most common cause is Pseudomonas aeruginosa and mixed flora. • Treament: systemic and local antibiotics. In case of abscess formation, it must be drained promptly and treated with systemic and local antobiotics.
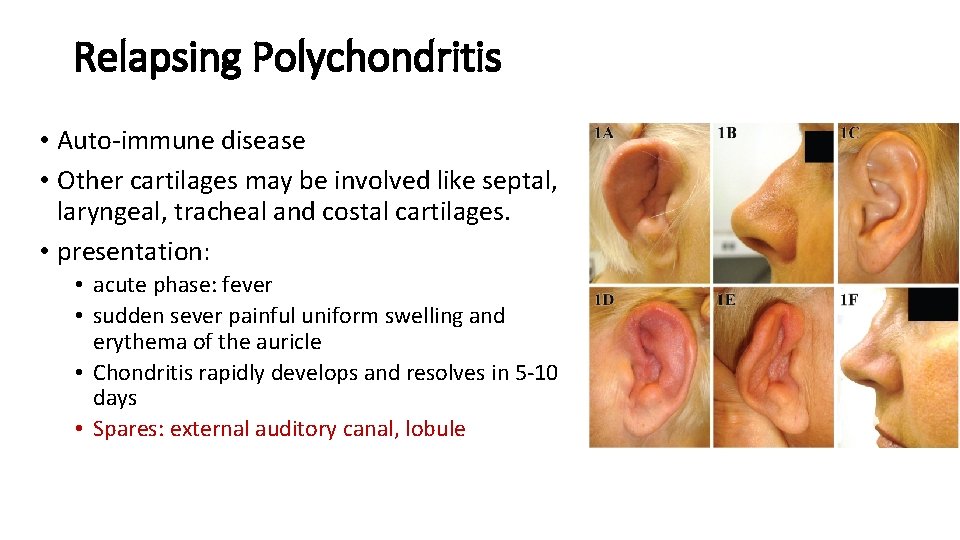
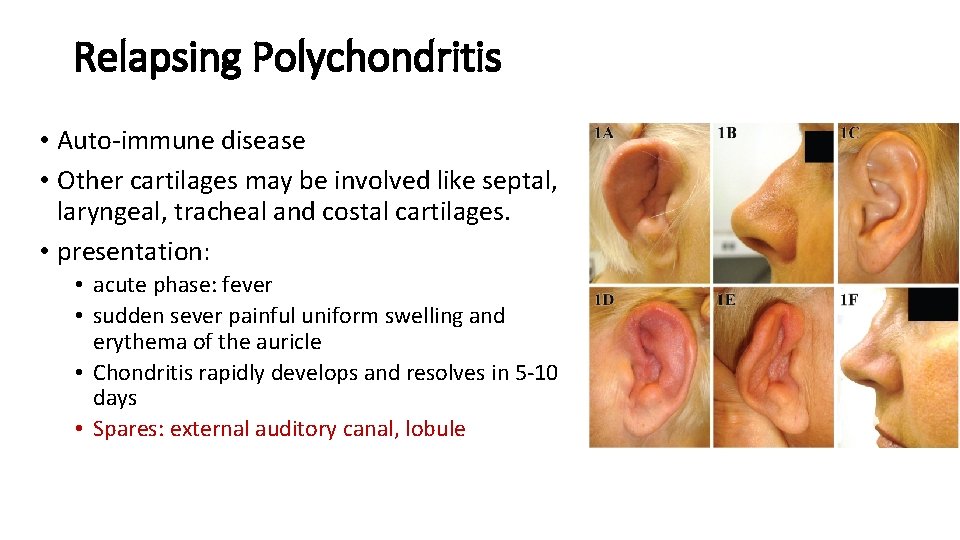
Relapsing Polychondritis • Auto-immune disease • Other cartilages may be involved like septal, laryngeal, tracheal and costal cartilages. • presentation: • acute phase: fever • sudden sever painful uniform swelling and erythema of the auricle • Chondritis rapidly develops and resolves in 5 -10 days • Spares: external auditory canal, lobule
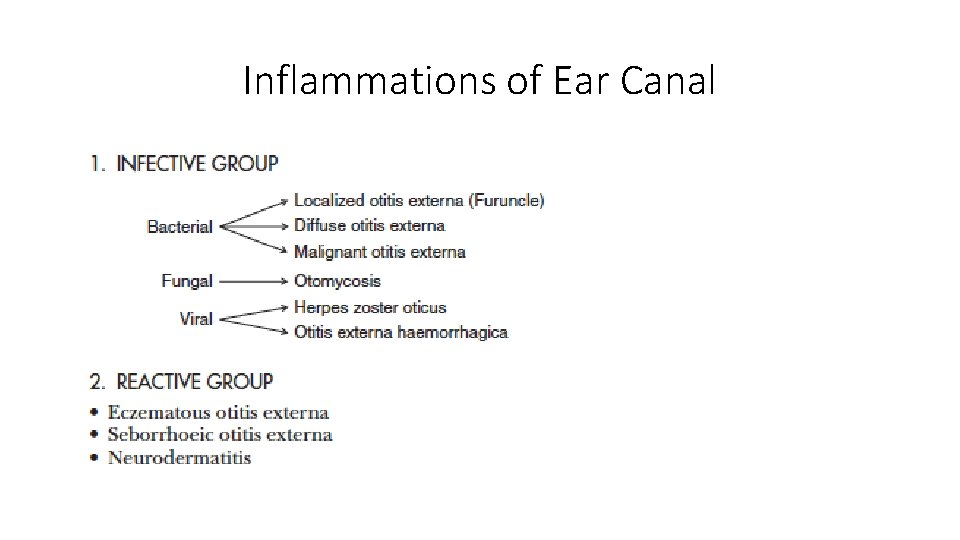
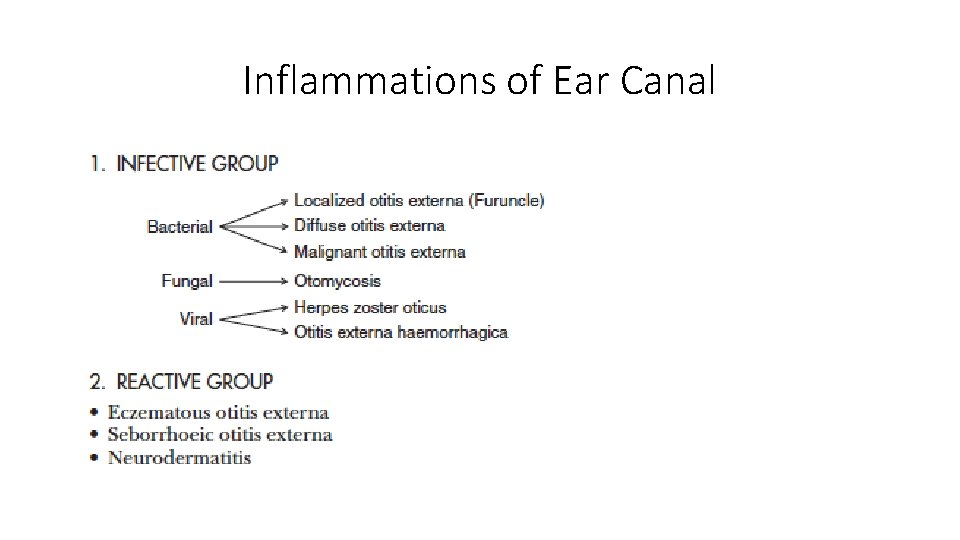
Inflammations of Ear Canal

External auditory canal infections • Furunculosis • Furuncle is a localized abscess of the apopilo-sebaceous unit • Most common organism: Staph aureus. • Confined to the outer 1/3 of the ear canal. • Symptoms: severe pain and tenderness. • Treatment: • Analgesia • Anti-staphylococcal oral and topical antibiotics should be administered. • A fluctuant lesion should be incised and drained under local anesthetic.
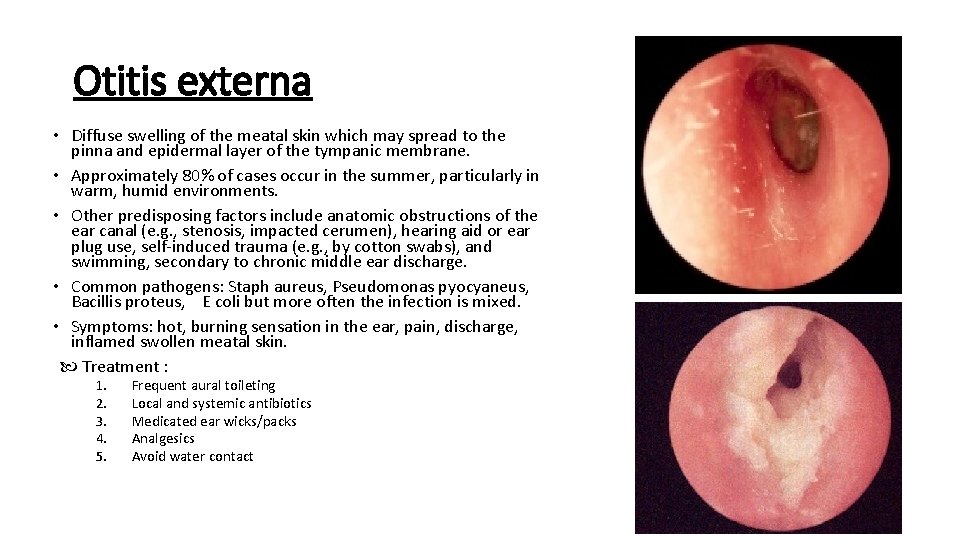
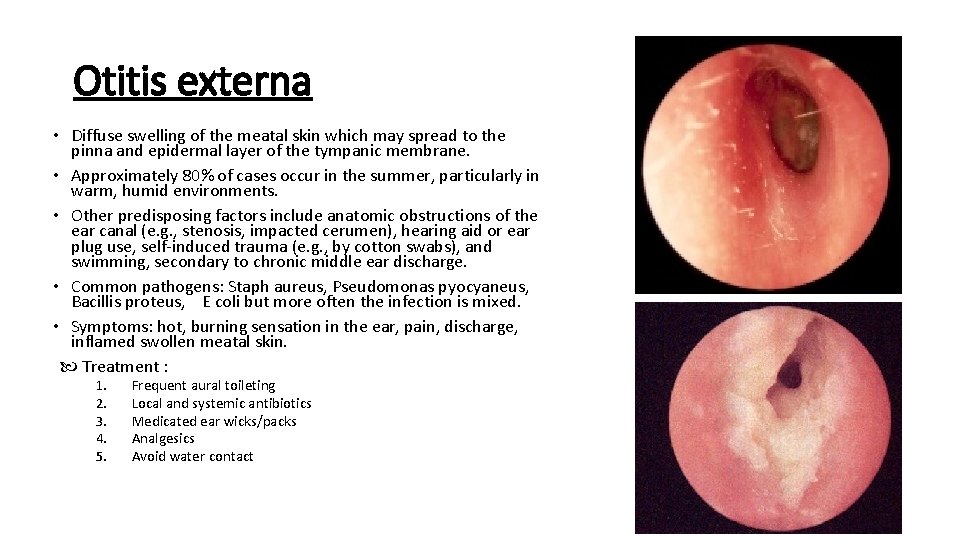
Otitis externa • Diffuse swelling of the meatal skin which may spread to the pinna and epidermal layer of the tympanic membrane. • Approximately 80% of cases occur in the summer, particularly in warm, humid environments. • Other predisposing factors include anatomic obstructions of the ear canal (e. g. , stenosis, impacted cerumen), hearing aid or ear plug use, self-induced trauma (e. g. , by cotton swabs), and swimming, secondary to chronic middle ear discharge. • Common pathogens: Staph aureus, Pseudomonas pyocyaneus, Bacillis proteus, E coli but more often the infection is mixed. • Symptoms: hot, burning sensation in the ear, pain, discharge, inflamed swollen meatal skin. Treatment : 1. 2. 3. 4. 5. Frequent aural toileting Local and systemic antibiotics Medicated ear wicks/packs Analgesics Avoid water contact
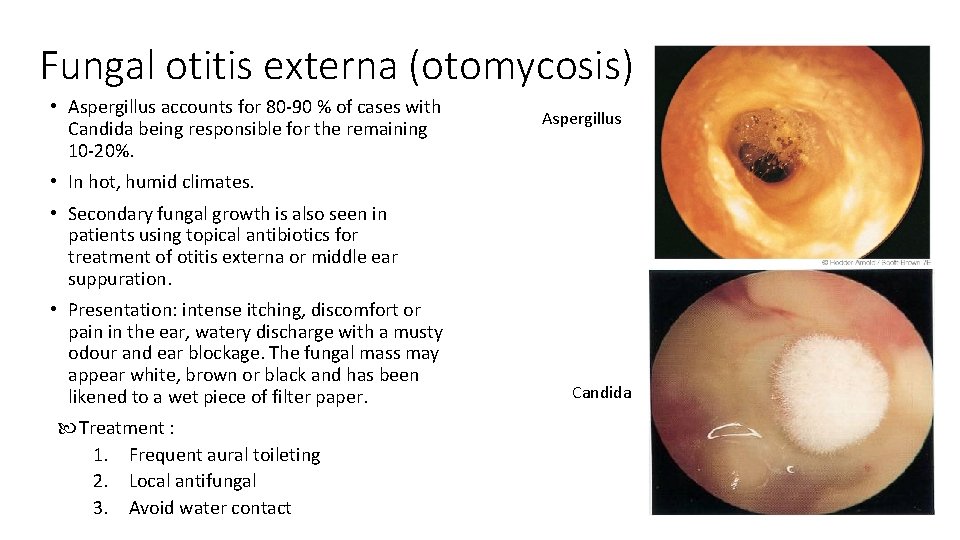
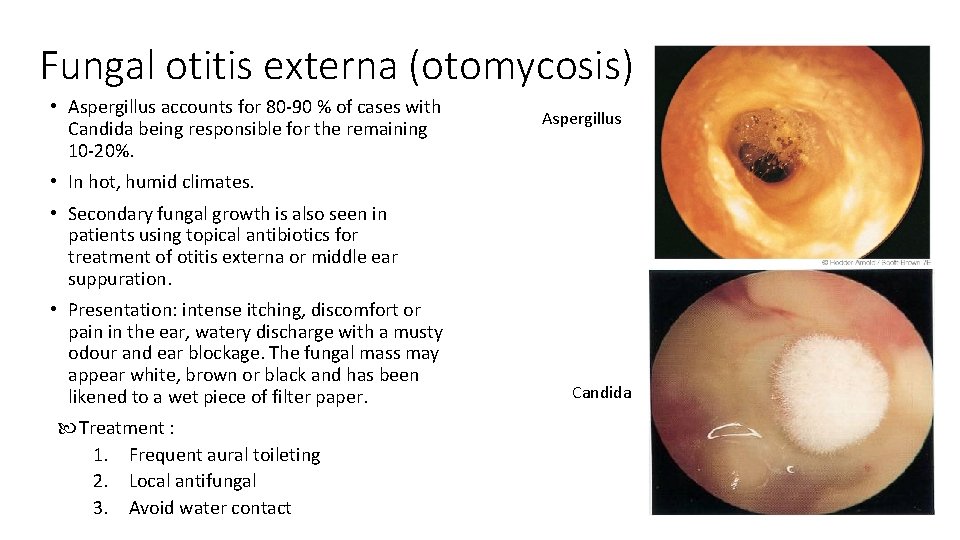
Fungal otitis externa (otomycosis) • Aspergillus accounts for 80 -90 % of cases with Candida being responsible for the remaining 10 -20%. Aspergillus • In hot, humid climates. • Secondary fungal growth is also seen in patients using topical antibiotics for treatment of otitis externa or middle ear suppuration. • Presentation: intense itching, discomfort or pain in the ear, watery discharge with a musty odour and ear blockage. The fungal mass may appear white, brown or black and has been likened to a wet piece of filter paper. Treatment : 1. Frequent aural toileting 2. Local antifungal 3. Avoid water contact Candida
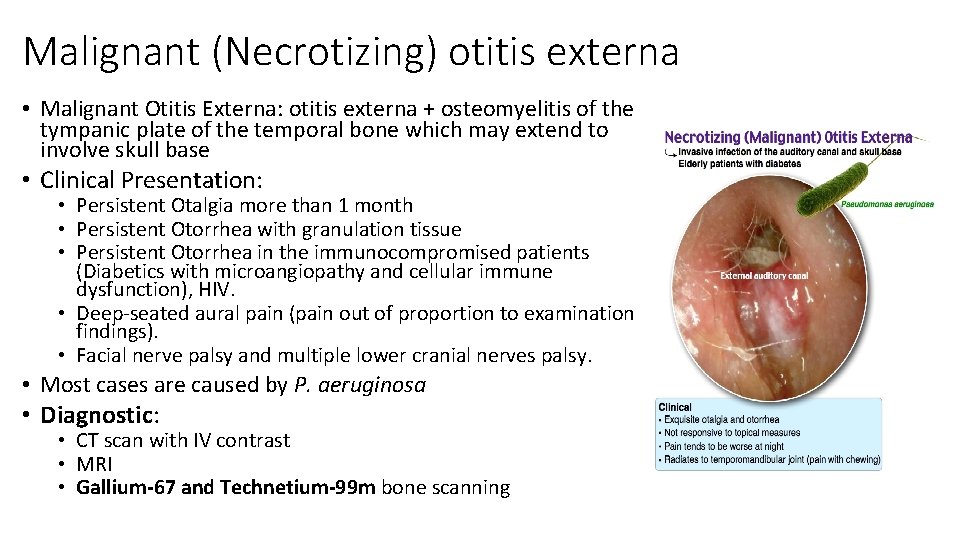
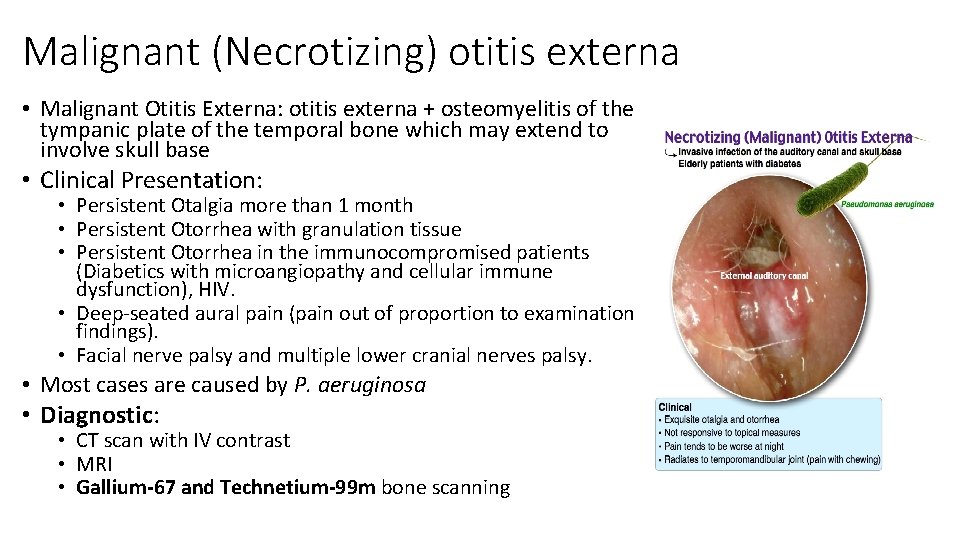
Malignant (Necrotizing) otitis externa • Malignant Otitis Externa: otitis externa + osteomyelitis of the tympanic plate of the temporal bone which may extend to involve skull base • Clinical Presentation: • Persistent Otalgia more than 1 month • Persistent Otorrhea with granulation tissue • Persistent Otorrhea in the immunocompromised patients (Diabetics with microangiopathy and cellular immune dysfunction), HIV. • Deep-seated aural pain (pain out of proportion to examination findings). • Facial nerve palsy and multiple lower cranial nerves palsy. • Most cases are caused by P. aeruginosa • Diagnostic: • CT scan with IV contrast • MRI • Gallium-67 and Technetium-99 m bone scanning
Malignant (Necrotizing) otitis externa Treatment: • • • Regular aural toilet Blood sugar control Correct immunodeficiency if possible Pain killer Infectious disease consult IV antibiotic for 6 -8 weeks, with antipseudomonal coverage (gentamicin+ticarcillin or ceftazidime+aminoglycoside or quinolones like ciprofloxacin) Prognosis: • Mortality is 5 -20%
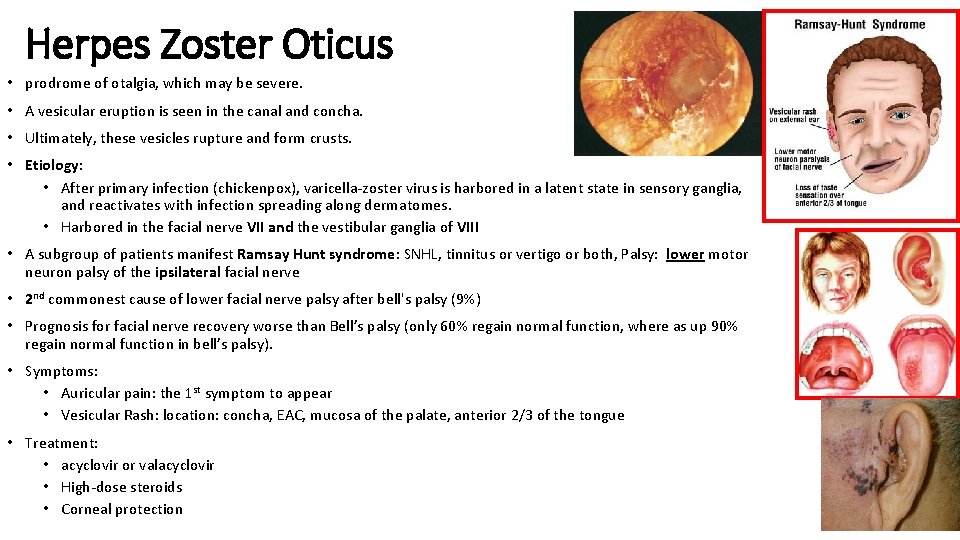
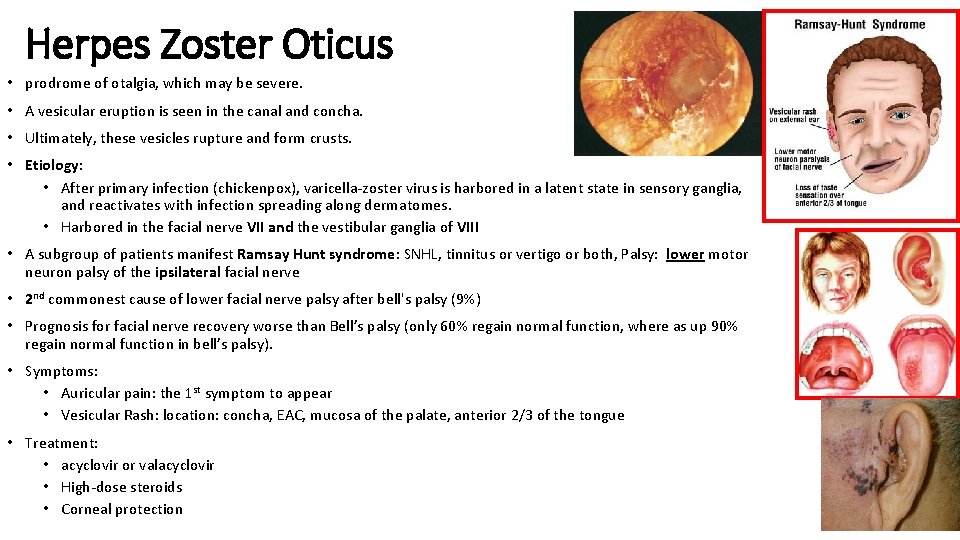
Herpes Zoster Oticus • prodrome of otalgia, which may be severe. • A vesicular eruption is seen in the canal and concha. • Ultimately, these vesicles rupture and form crusts. • Etiology: • After primary infection (chickenpox), varicella-zoster virus is harbored in a latent state in sensory ganglia, and reactivates with infection spreading along dermatomes. • Harbored in the facial nerve VII and the vestibular ganglia of VIII • A subgroup of patients manifest Ramsay Hunt syndrome: SNHL, tinnitus or vertigo or both, Palsy: lower motor neuron palsy of the ipsilateral facial nerve • 2 nd commonest cause of lower facial nerve palsy after bell's palsy (9%) • Prognosis for facial nerve recovery worse than Bell’s palsy (only 60% regain normal function, where as up 90% regain normal function in bell’s palsy). • Symptoms: • Auricular pain: the 1 st symptom to appear • Vesicular Rash: location: concha, EAC, mucosa of the palate, anterior 2/3 of the tongue • Treatment: • acyclovir or valacyclovir • High-dose steroids • Corneal protection