Teaching Residents to Use Motivational Interviewing Techniques and

- Slides: 54
“Teaching Residents to Use Motivational Interviewing Techniques and Writing Innovative Behavioral Prescriptions With Patients”
By Michelle Domanchuk, RN, MSN Georgeann Iacono-Russell, Ph. D Kenneth Blair, MD Scott Levin, MD April 28, 2007
Workshop Outline 1. Background 2. Motivational Interviewing Techniques 3. Behavioral Prescription and Prescription Steps (BPPS) 4. Review Video Role Play 5. Breakout Sessions 6. Re-group 7. Evaluation of Resident Learning (Data) 8. Conclusions
Objectives 1. Effectively teach residents about behavior-driven chronic diseases and how to increase behavior change using motivational interviewing techniques.
Objectives 2. Be able to write and model for the resident a Behavioral Prescription with Prescription Steps given a Case Study using a seven-point self-assessment guideline.
Objectives 3. Effectively implement teaching strategies, such as case-study and roleplay, with residents to increase the likelihood of adoption of the Behavioral Prescription into the residents patient panel.
Background • Supported by HRSA Residency Training Grant • Need for creative curricular topics to teach residents to more effectively educate and motivate patients towards healthy behavioral change • Increasing percentage of chronic health conditions is behavior-driven • Success rates not high
Background • Majority of adults and ever-increasing percentage of children are overweight or obese • The associated illnesses of the skeletal, cardiovascular, endocrine, and renal systems mandates success in health behavior change if they are to be successfully treated. • The burden in morbidity and mortality and dollar costs is substantial.
Chronic Care Model and the Disease Management Model • Both models focus on chronic illness and emphasize the patient’s active role in managing their illness • Education to patient and family with focus on self-management skills
Chronic Care Model • Over 700 community health centers part of a national collaborative to help patients delay or decrease complications related to chronic illness • Standardized patient assessments include self-management knowledge, skills, confidence, supports and barriers • BPPS helps teach and document selfmanagement skills
Disease Management Model • Initiated in 2005 by Center for Medicare & Medicaid Services (CMS) • Improve quality of care by communicating directly with patients rather than persuading physicians to change • Focus on educating patients and their families on patient self-management skills via telephone calls, mailings, Internet, and home visits
Background • Provider recognition of patient’s health literacy level is critical for meaningful communication between provider and patient • The Self-Efficacy Theory developed by the Social Cognitive Theorist Professor Albert Bandura was used in the development of the BPPS
Self-Efficacy Theory • Defined in healthcare as the belief that one can carry out a behavior to achieve a desired goal related to one’s health • A function of an individual’s attitudes, beliefs, characteristics, and innate abilities, as well as education, knowledge, training, and learned skills
The Science of Change: Motivational Interviewing • Originated in the chemical dependency area • Specific counseling techniques • Increasing interest to incorporate MI techniques in health care setting to influence health behavior change • Not enough data yet to prove shortened techniques work for MD’s
The Science of Change: Motivational Interviewing A patient-centered, directive method for enhancing intrinsic motivation to change by exploring and resolving ambivalence
Prochaska and Diclemente’s Stages of Change Model Emphasizes people progress through predictable cognitive stages prior to making a change in behavior
Tenets of Motivational Interviewing • Collaboration rather than Confrontation • Evocation rather than education • Autonomy rather than authority
The Motivational Interviewing Process (EDARS) • Express empathy • Develop discrepancy • Avoid argument • Roll with resistance • Support self-efficacy
Ambivalence • Rather than view ambivalence and resistance as “pathological” we need to understand that they are a normal part of the change process and work with them • Very few decisions in life are made with 100% certainty/resolve
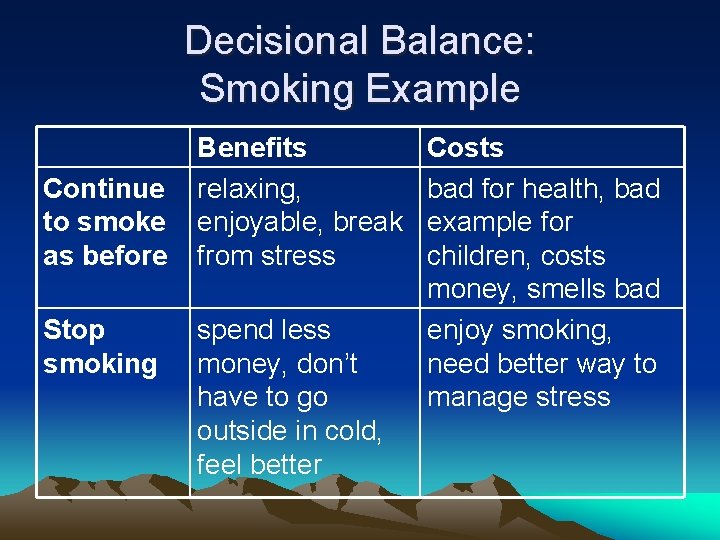
Decisional Balance: Benefits and Costs • People weigh the costs/benefits of change versus the costs/benefits of staying the same • Important to understand what the patient perceives as the costs/benefits of change versus staying the same
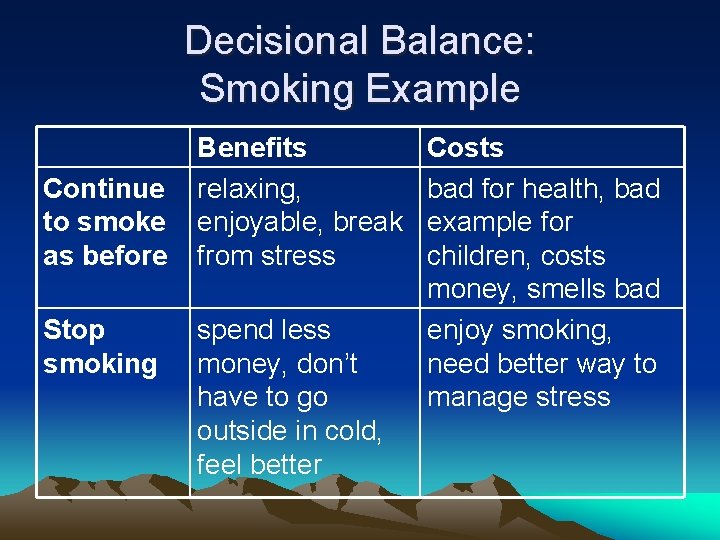
Decisional Balance: Smoking Example Continue to smoke as before Stop smoking Benefits relaxing, enjoyable, break from stress spend less money, don’t have to go outside in cold, feel better Costs bad for health, bad example for children, costs money, smells bad enjoy smoking, need better way to manage stress
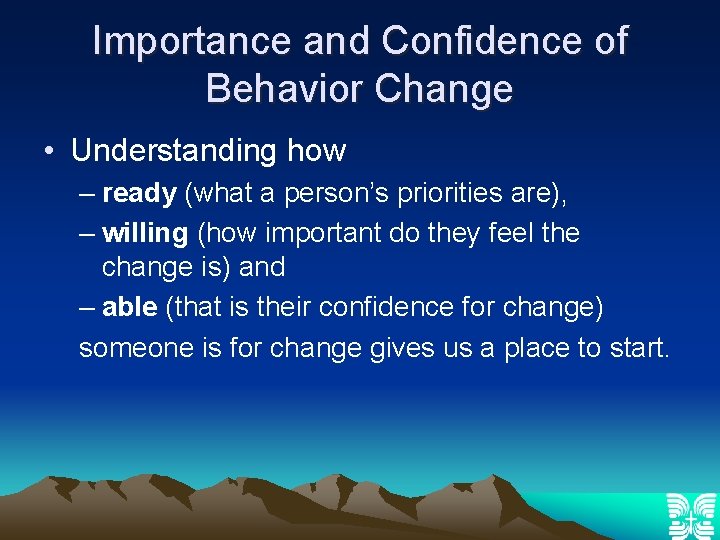
Importance and Confidence of Behavior Change • Understanding how – ready (what a person’s priorities are), – willing (how important do they feel the change is) and – able (that is their confidence for change) someone is for change gives us a place to start.
Patient-Centered Approach • Our listening and empathy skills serve to enhance patient participation, motivation and compliance
Motivational Interviewing • See sample Dialogues (handout that is used for future workshops) • See handout on “Examples of questions that evoke change talk”
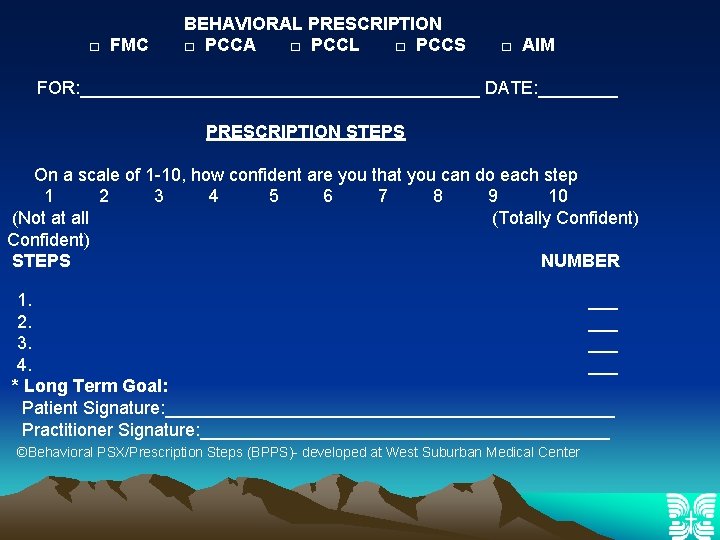
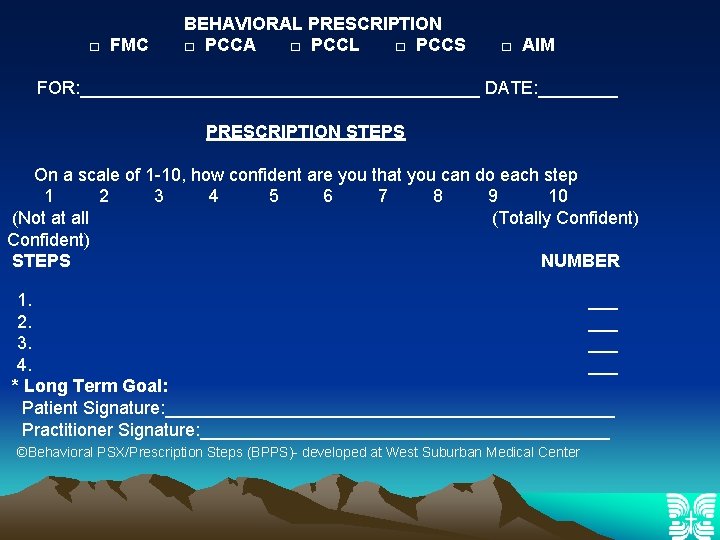
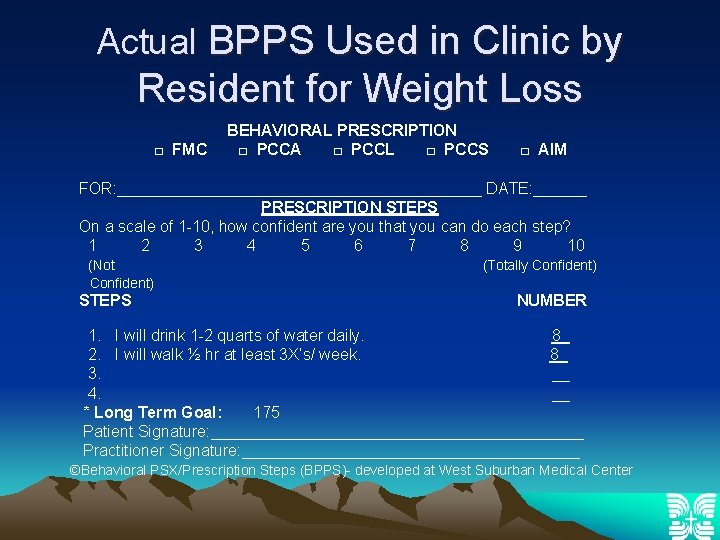
□ FMC BEHAVIORAL PRESCRIPTION □ PCCA □ PCCL □ PCCS □ AIM FOR: ____________________ DATE: ____ PRESCRIPTION STEPS On a scale of 1 -10, how confident are you that you can do each step 1 2 3 4 5 6 7 8 9 10 (Not at all (Totally Confident) STEPS NUMBER 1. ___ 2. ___ 3. ___ 4. ___ * Long Term Goal: Patient Signature: _______________________ Practitioner Signature: _____________________ ©Behavioral PSX/Prescription Steps (BPPS)- developed at West Suburban Medical Center
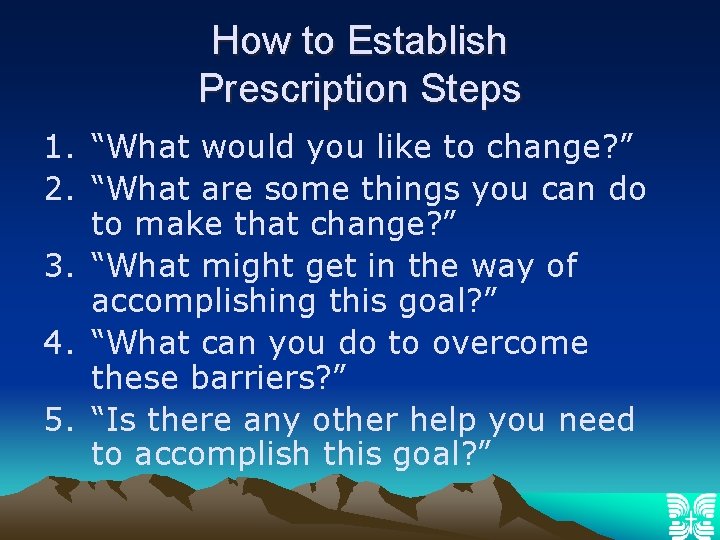
How to Establish Prescription Steps 1. “What would you like to change? ” 2. “What are some things you can do to make that change? ” 3. “What might get in the way of accomplishing this goal? ” 4. “What can you do to overcome these barriers? ” 5. “Is there any other help you need to accomplish this goal? ”
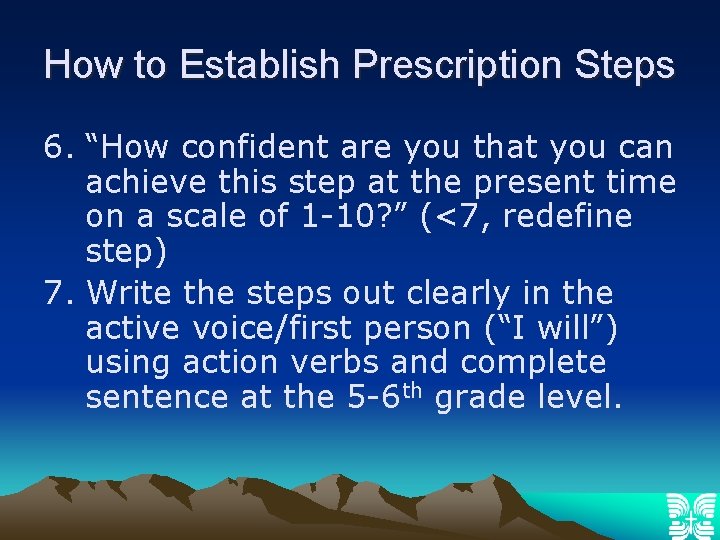
How to Establish Prescription Steps 6. “How confident are you that you can achieve this step at the present time on a scale of 1 -10? ” (<7, redefine step) 7. Write the steps out clearly in the active voice/first person (“I will”) using action verbs and complete sentence at the 5 -6 th grade level.
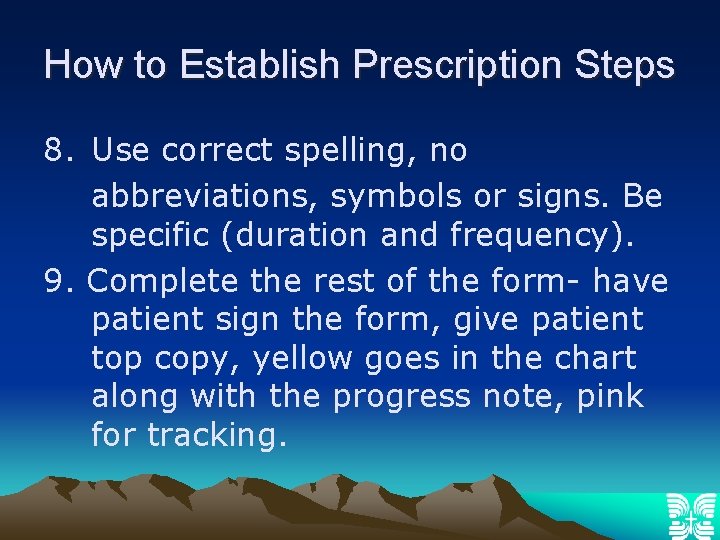
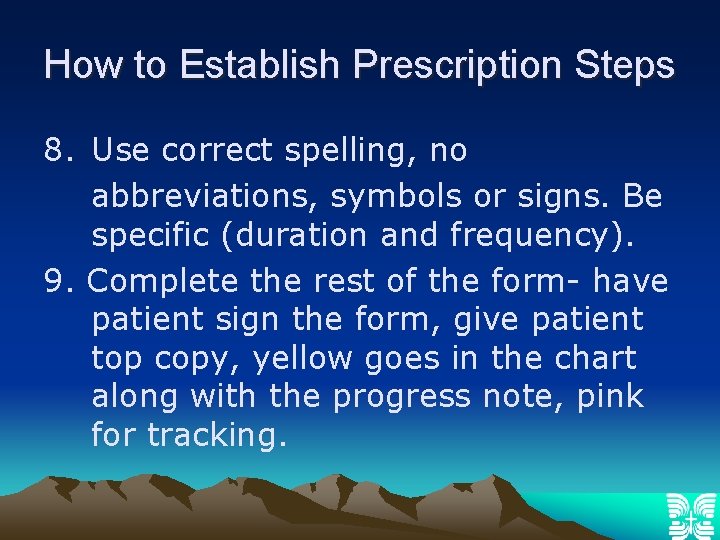
How to Establish Prescription Steps 8. Use correct spelling, no abbreviations, symbols or signs. Be specific (duration and frequency). 9. Complete the rest of the form- have patient sign the form, give patient top copy, yellow goes in the chart along with the progress note, pink for tracking.
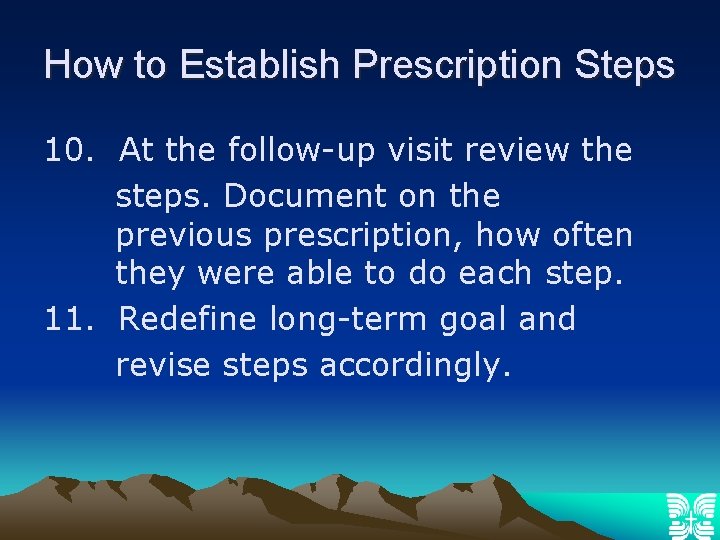
How to Establish Prescription Steps 10. At the follow-up visit review the steps. Document on the previous prescription, how often they were able to do each step. 11. Redefine long-term goal and revise steps accordingly.
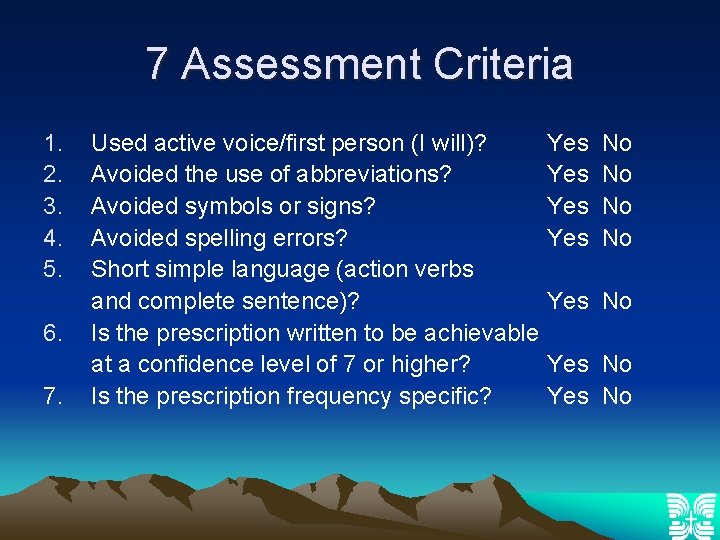
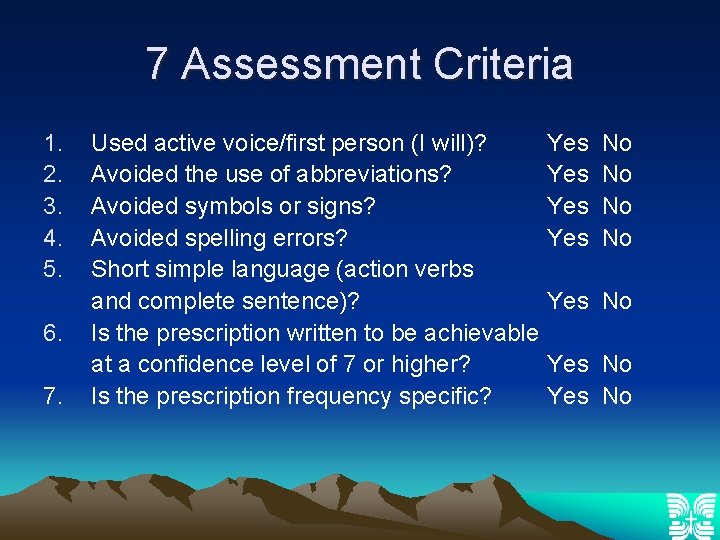
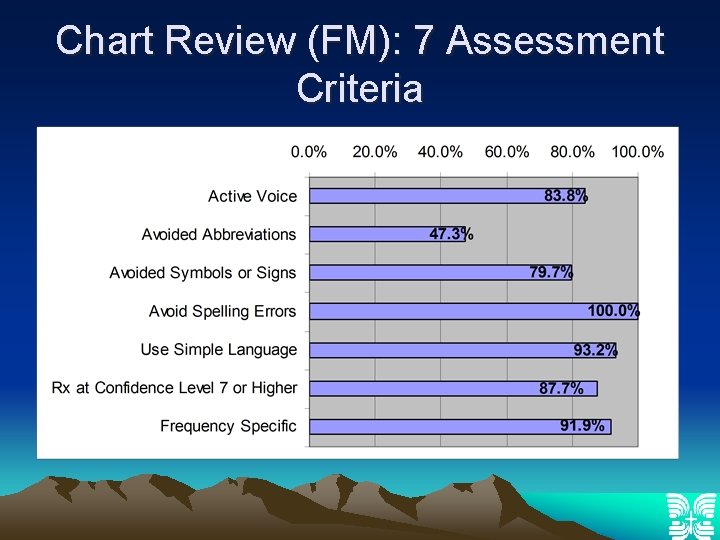
7 Assessment Criteria 1. 2. 3. 4. 5. 6. 7. Used active voice/first person (I will)? Avoided the use of abbreviations? Avoided symbols or signs? Avoided spelling errors? Short simple language (action verbs and complete sentence)? Is the prescription written to be achievable at a confidence level of 7 or higher? Is the prescription frequency specific? Yes Yes No No Yes No
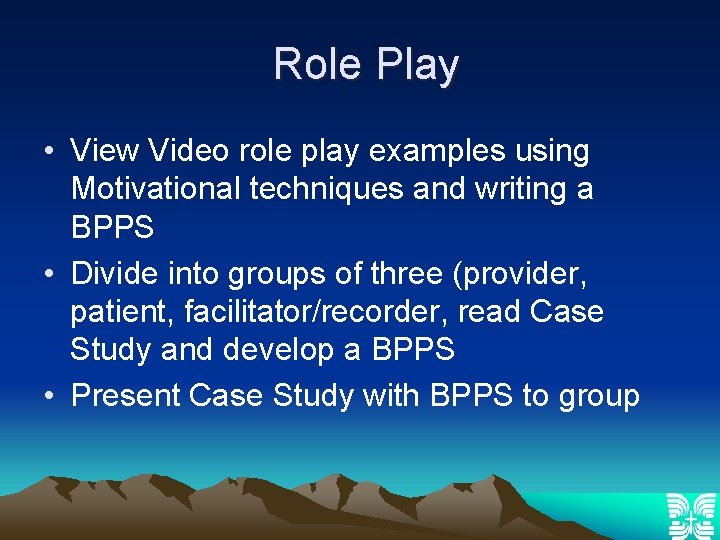
Role Play • View Video role play examples using Motivational techniques and writing a BPPS • Divide into groups of three (provider, patient, facilitator/recorder, read Case Study and develop a BPPS • Present Case Study with BPPS to group
Problem Solving Techniques to Use When Patients Do Not Meet Their Set Goals • Listen to what the person is telling you about why they did not meet their goals – “Tell me how it went…. ” – “What did you find got in your way? ” • Emphasize that the inability to meet the goal can provide useful information rather than indicating a failure. – In many ways it is more important to learn what was difficult and problem solve than to be able to perfectly meet a goal.
Evaluation of Resident Learning 1. One hour Workshop with Motivational Interviewing techniques and case study/role play developing a BPPS 2. Health Literacy Computer Exercise II developing a BPPS 3. Retrospective Chart review and scoring system 4. Faculty and Residents asked to write their own BPPS that they will write 2 BPPS’s a month with their patients (recent greatest impact)
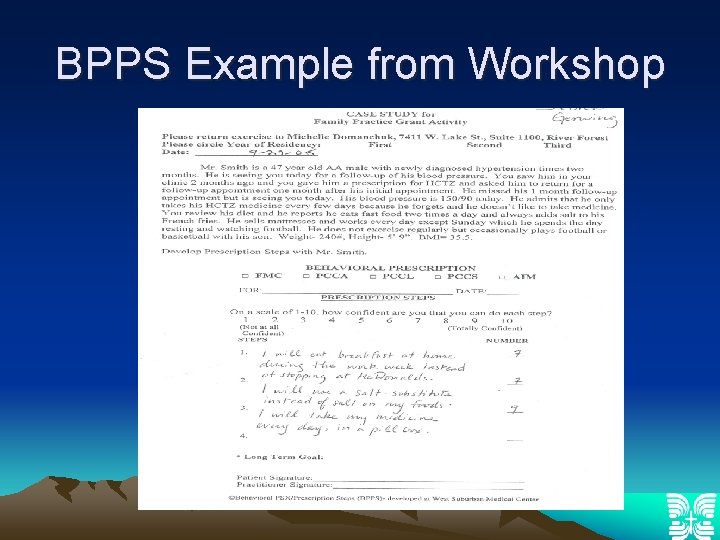
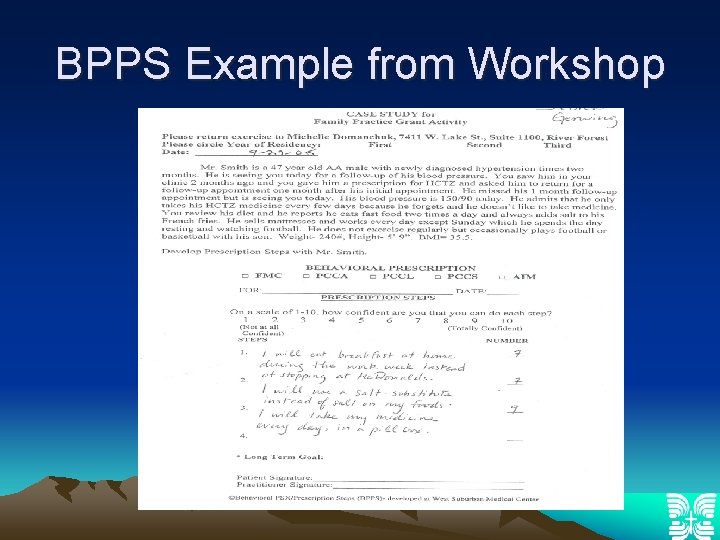
BPPS Example from Workshop
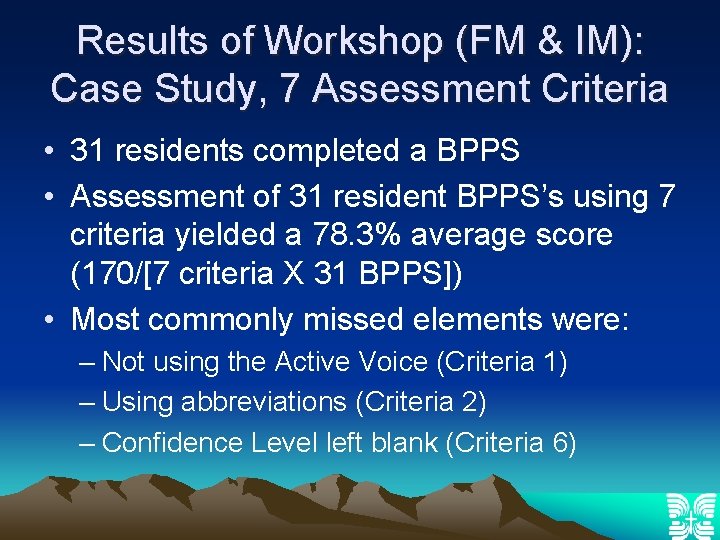
Results of Workshop (FM & IM): Case Study, 7 Assessment Criteria • 31 residents completed a BPPS • Assessment of 31 resident BPPS’s using 7 criteria yielded a 78. 3% average score (170/[7 criteria X 31 BPPS]) • Most commonly missed elements were: – Not using the Active Voice (Criteria 1) – Using abbreviations (Criteria 2) – Confidence Level left blank (Criteria 6)
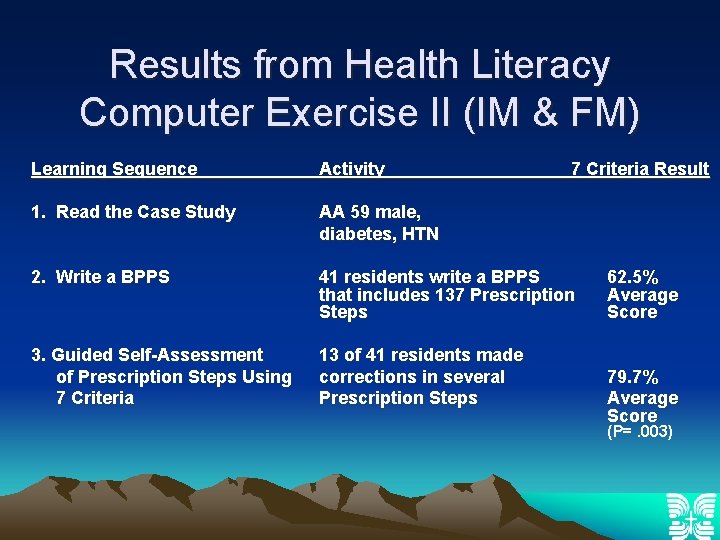
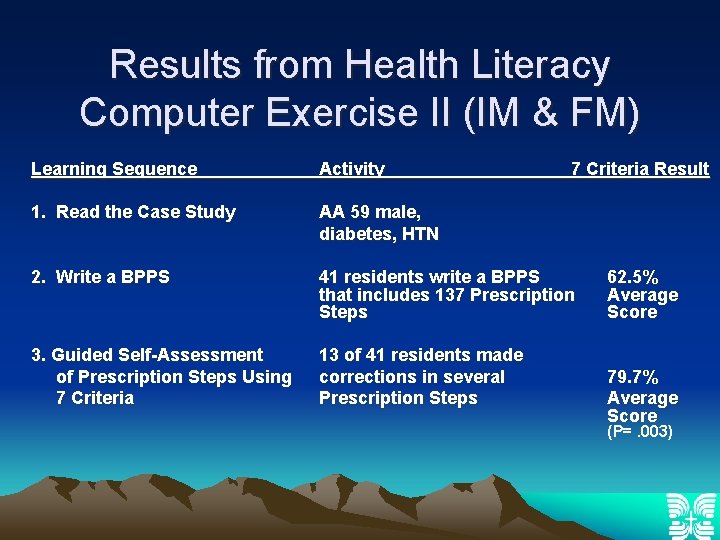
Results from Health Literacy Computer Exercise II (IM & FM) Learning Sequence Activity 7 Criteria Result 1. Read the Case Study AA 59 male, diabetes, HTN 2. Write a BPPS 41 residents write a BPPS that includes 137 Prescription Steps 3. Guided Self-Assessment of Prescription Steps Using 7 Criteria 13 of 41 residents made corrections in several Prescription Steps 62. 5% Average Score 79. 7% Average Score (P=. 003)
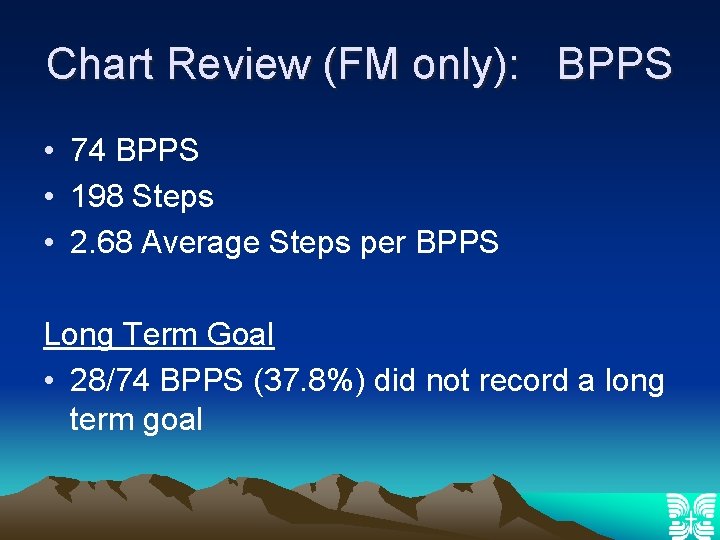
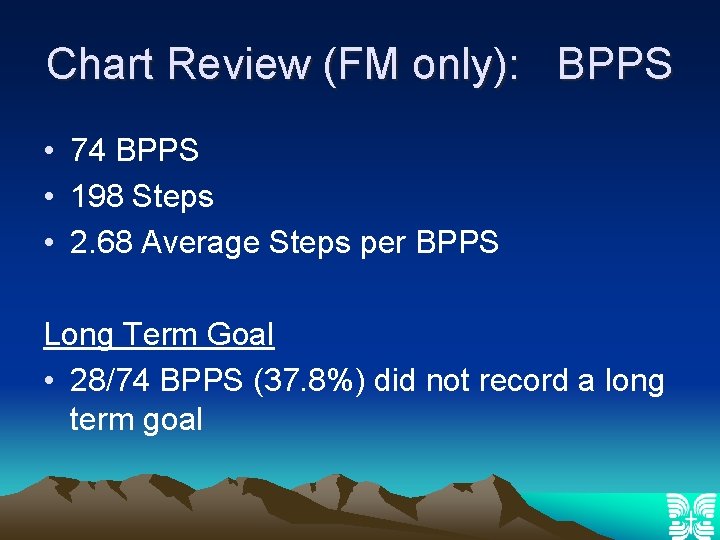
Chart Review (FM only): BPPS • 74 BPPS • 198 Steps • 2. 68 Average Steps per BPPS Long Term Goal • 28/74 BPPS (37. 8%) did not record a long term goal
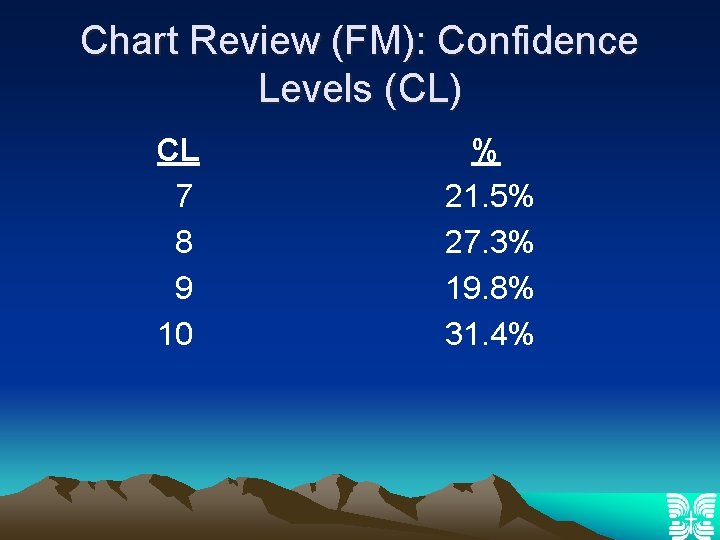
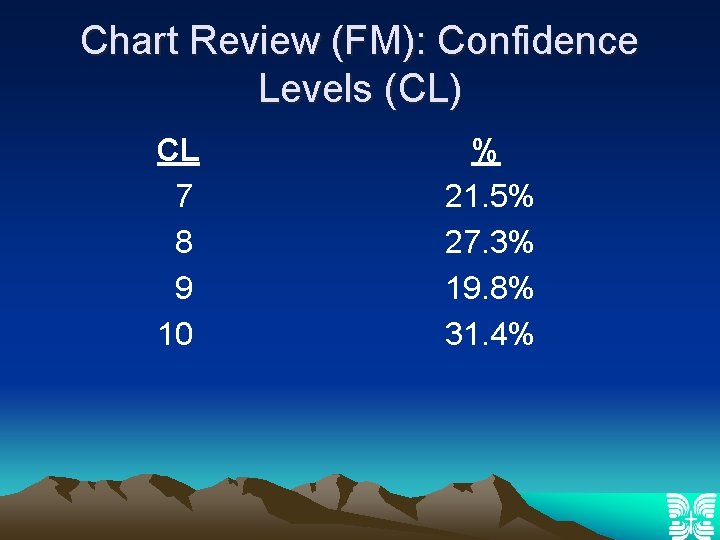
Chart Review (FM): Confidence Levels (CL) CL 7 8 9 10 % 21. 5% 27. 3% 19. 8% 31. 4%
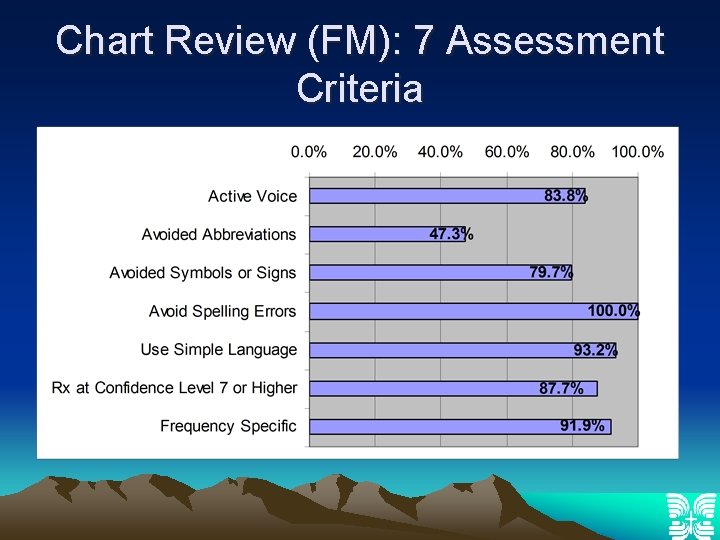
Chart Review (FM): 7 Assessment Criteria
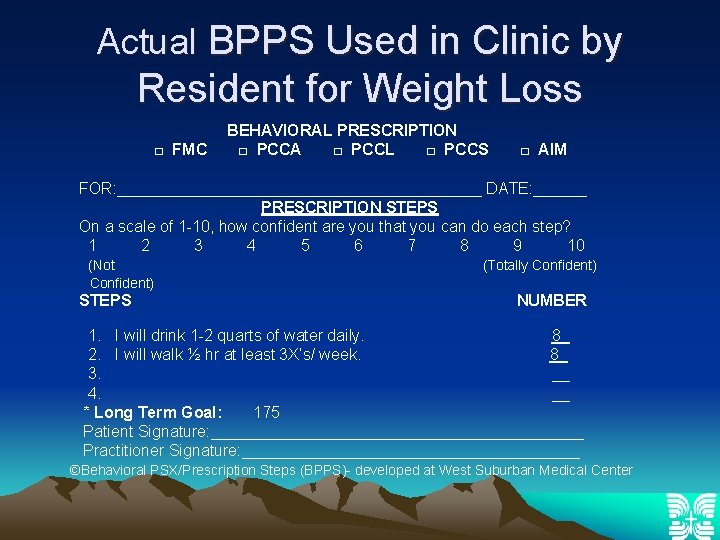
Actual BPPS Used in Clinic by Resident for Weight Loss □ FMC BEHAVIORAL PRESCRIPTION □ PCCA □ PCCL □ PCCS □ AIM FOR: _____________________ DATE: ______ PRESCRIPTION STEPS On a scale of 1 -10, how confident are you that you can do each step? 1 2 3 4 5 6 7 8 9 10 (Not Confident) STEPS (Totally Confident) NUMBER 1. I will drink 1 -2 quarts of water daily. 8_ 2. I will walk ½ hr at least 3 X’s/ week. 8_ 3. __ 4. __ * Long Term Goal: 175 Patient Signature: _____________________ Practitioner Signature: ___________________ ©Behavioral PSX/Prescription Steps (BPPS)- developed at West Suburban Medical Center
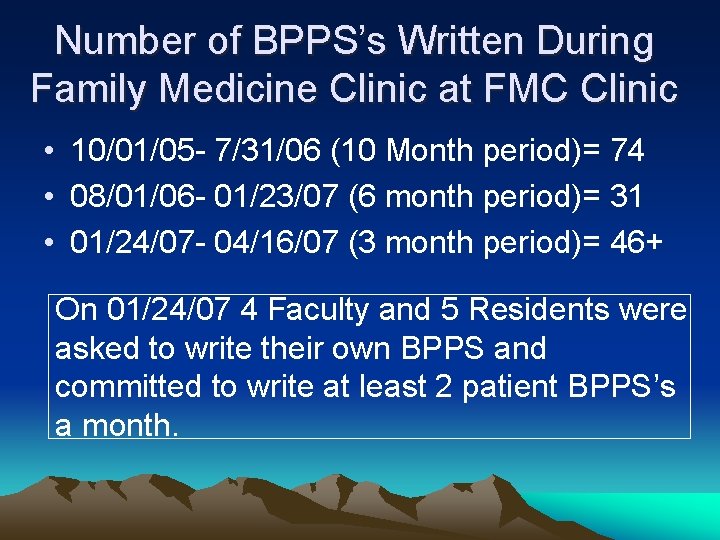
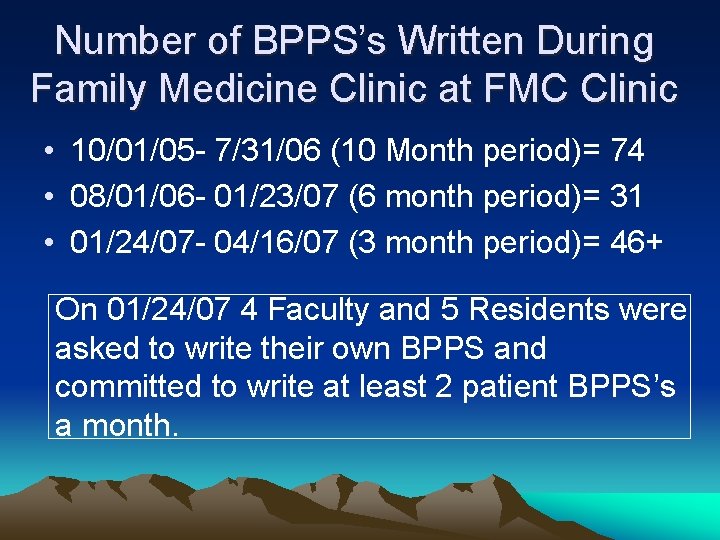
Number of BPPS’s Written During Family Medicine Clinic at FMC Clinic • 10/01/05 - 7/31/06 (10 Month period)= 74 • 08/01/06 - 01/23/07 (6 month period)= 31 • 01/24/07 - 04/16/07 (3 month period)= 46+ On 01/24/07 4 Faculty and 5 Residents were asked to write their own BPPS and committed to write at least 2 patient BPPS’s a month.
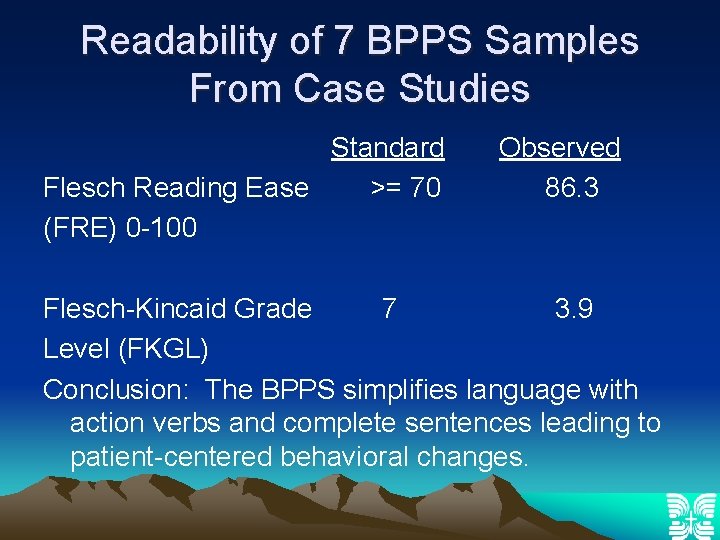
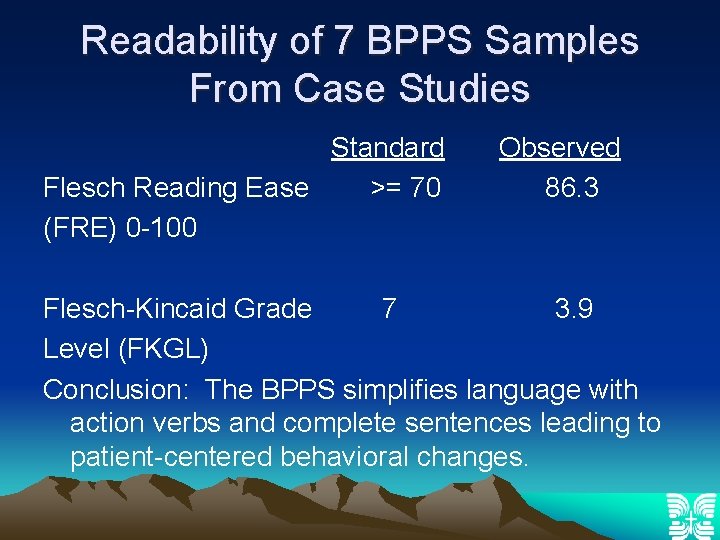
Readability of 7 BPPS Samples From Case Studies Standard Flesch Reading Ease >= 70 (FRE) 0 -100 Observed 86. 3 Flesch-Kincaid Grade 7 3. 9 Level (FKGL) Conclusion: The BPPS simplifies language with action verbs and complete sentences leading to patient-centered behavioral changes.
Conclusions • A one-hour workshop is sufficient to learn to appropriately write a BPPS • Using Motivational Interviewing techniques with a patient-centered approach along with the BPPS helps residents to assess patient readiness for change and increases patient behavioral changes • Patient readability, which is essential, is enhanced with a BPPS
Conclusions • BPPS encourages realistic goal-setting with the patient in the office • Residents are able to self-assess the appropriateness of Prescription Steps and make necessary adjustments in the BPPS • A Chart Review indicated adoption of BPPS in resident’s patient panel • Future research to focus on reviewing patient charts to assess patient behavioral changes and health outcomes attributed to the BPPS
Famous Quotes • “Self Confidence is the first requisite to great undertakings” Samuel Johnson • “Nothing can be done without hope and confidence” Helen Keller • “They are able who think they are able. ” Virgil
Famous Quotes • “Whether you think that you can or you can’t, you’re usually right. ” Henry Ford • “If I have a belief that I can do it, I shall surely acquire the capacity to do it even if I may not have it at the beginning. ” Mahatma Gandhi
Famous Quotes If you treat an individual as he is, he will stay as he is, but if you treat him as if he were what he ought to be and could be, he will become what he ought to be and could be. Johann Wolfgang von Goethe
References Information on self-efficacy: a community of scholars, On-line links, Nov. 9, 2004. Paone, D. Self-efficacy/self-health care among older adults: a literature review, National Chronic Care Consortium, 1999. Safeer, R. S. , Keenan, J. , Health literacy: the gap between physicians and patients, Am Fam Physician 2005; 72: 463 -8.
References S. Rollnick, P. Mason, C. Butler. Healthy behavior change: a guide for practitioners, New York: Churchill Livingstone, 1999 W. R. Miller, S. Rollnick. Motivational interviewing: preparing people for change. New York: Guildford Press, 2002
Resources • Handley, M. , Mac. Gregor, K. , Schillinger, D. , Sharifi, C. , Wong, S. , Bodenheimer, T. Using action plans to help primary care patients adopt healthy behaviors: a descriptive study. JABFM (2006); 19: 224 -231. • Holt, J. , Warren, L. , Wallace, R. What behavioral interventions are safe and effective for treating obesity? J Fam Med (2006); 55; 536 -538. • Mac. Gregor, K. , Handley, M. , Wong, S. , Sharifi, C. , Gjeltema, K. , Schillinger, D. , Bodenheimer, T. Behaviorchange action plans in primary care: a feasibility study of clinicians. JABFM (2006); 19: 215 -223.
Resources • Michelle Domanchuk, RN, MSN michelle. domanchuk@reshealthcare. org 708 -763 -2193 • Georgeann Iacono-Russell, Ph. D georgeannrussell@sbcglobal. net 708 -763 -2120 Kenneth Blair, MD 708 -488 -1490 Scott Levin, MD 708 -488 -1490 Margaret Z. (Peggy) Cassey, MPH, RN, BC mcassey@uic. edu
Resources • Motivational Interviewing and Behavioral Prescriptions: Tools for the Health Care Professional Video, Direct Link http: //westsuburbanmedicalcenter. reshealth. org/educatio n/wsmcfamily/residencyvideo. cfm • FMRDL-Search for Domanchuk (Lecture handout to residents, BPPS, Pocket Cards, Posters from STFM Conferences, STFM Seminar April 2007). Search for Cassey (Health Literacy Computer Exercise Part I and II • UCLA Center for Human Nutrition: Sample Scripts for Stages of Change www. cellinteractive. com/ucla/physician_ed/scripts_for_c hange. html
Acknowledgements • Thanks to Z. Harry Piotrowski, Ph. D for writing and obtaining the HRSA Grant to develop innovative curricula for the Family Medicine Residency Program. • Thanks to Margaret Z. (Peggy) Cassey for her encouragement and expertise in the development of the Web-based computer exercises integrating health literacy, cultural humility, and use of the BPPS.
