MOTIVATIONAL INTERVIEWING S 4 S Teaching Shannon Hilton



- Slides: 15

MOTIVATIONAL INTERVIEWING S 4 S Teaching Shannon Hilton
AIMS To define Motivational Interviewing To understand key concepts and structure of a MI conversation
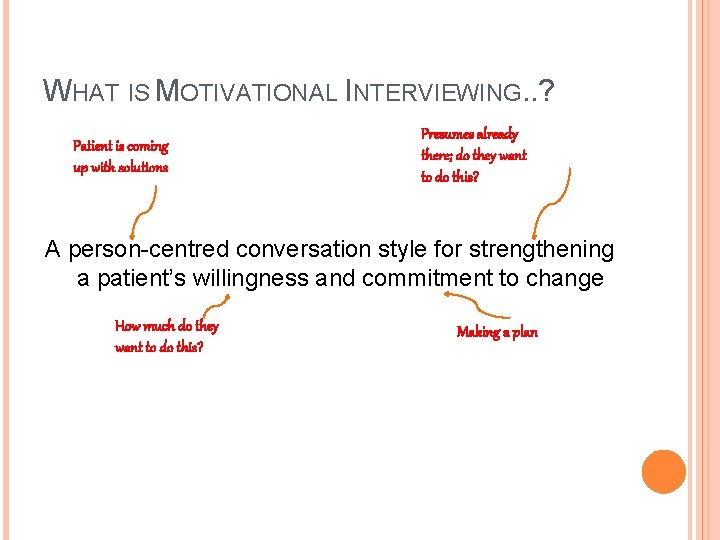
WHAT IS MOTIVATIONAL INTERVIEWING. . ? Patient is coming up with solutions Presumes already there; do they want to do this? A person-centred conversation style for strengthening a patient’s willingness and commitment to change How much do they want to do this? Making a plan
Quit smoking Encouraging social interaction Addiction Exercise Looking for work Reduce alcohol Medication compliance Stress management Healthy eating Coping with depression Understanding about an illness
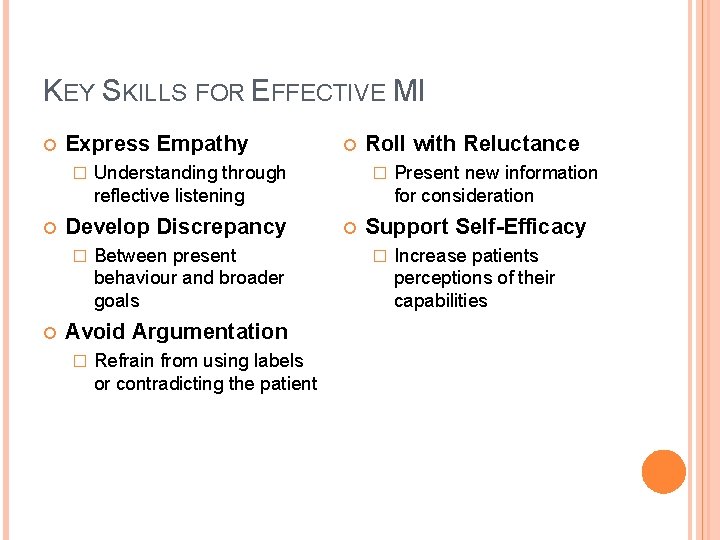
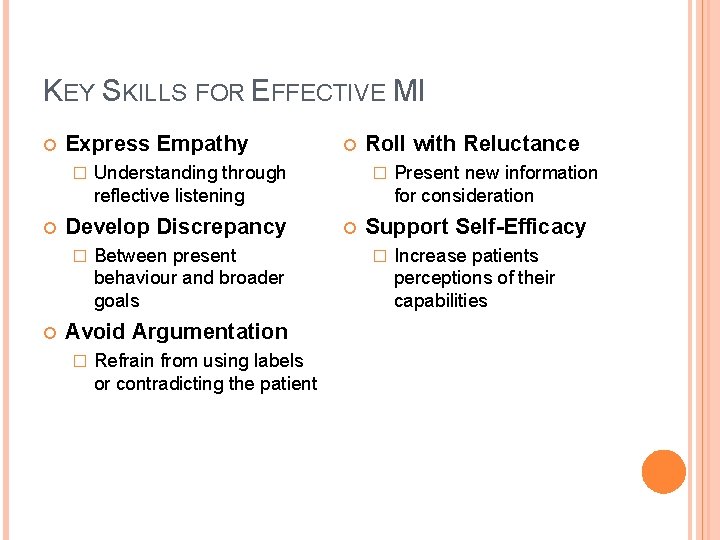
KEY SKILLS FOR EFFECTIVE MI Express Empathy � Understanding through reflective listening Develop Discrepancy � Between present behaviour and broader goals Avoid Argumentation � Refrain from using labels or contradicting the patient Roll with Reluctance � Present new information for consideration Support Self-Efficacy � Increase patients perceptions of their capabilities
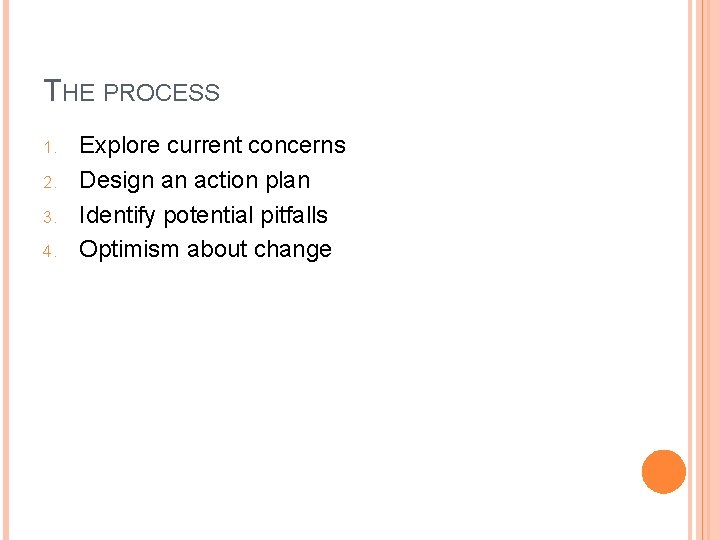
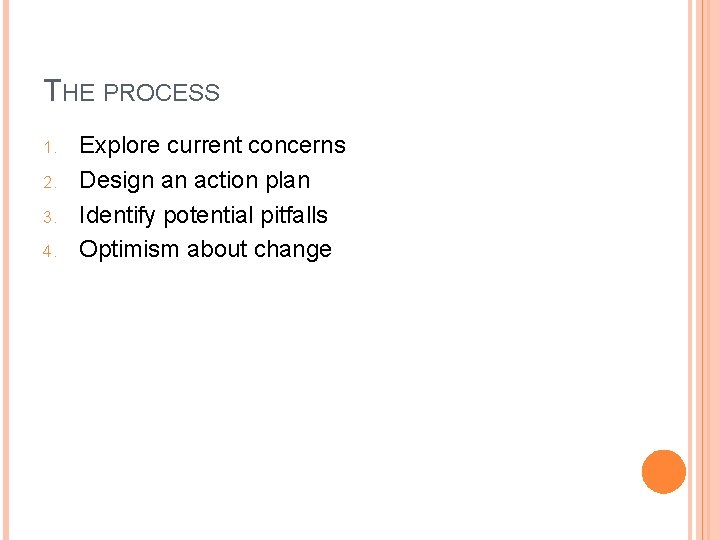
THE PROCESS 1. 2. 3. 4. Explore current concerns Design an action plan Identify potential pitfalls Optimism about change

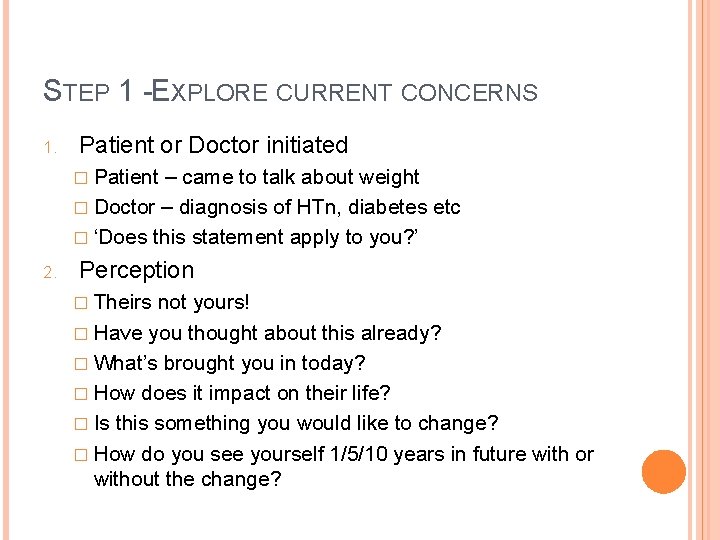
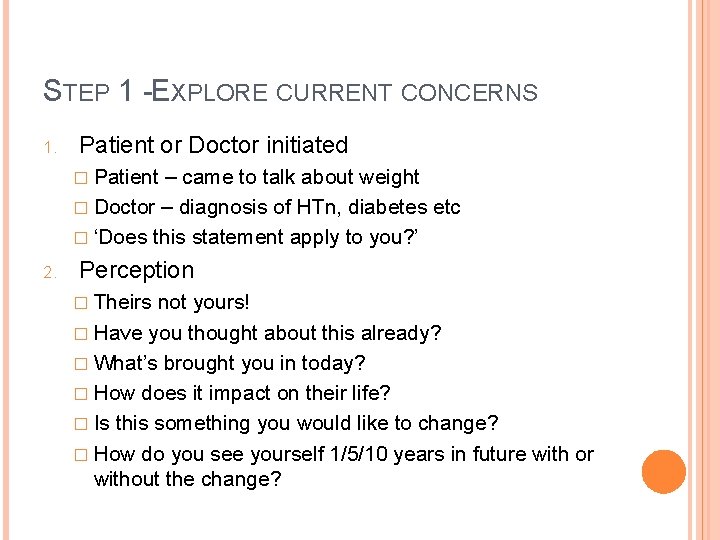
STEP 1 -EXPLORE CURRENT CONCERNS 1. Patient or Doctor initiated � Patient – came to talk about weight � Doctor – diagnosis of HTn, diabetes etc � ‘Does this statement apply to you? ’ 2. Perception � Theirs not yours! � Have you thought about this already? � What’s brought you in today? � How does it impact on their life? � Is this something you would like to change? � How do you see yourself 1/5/10 years in future with or without the change?

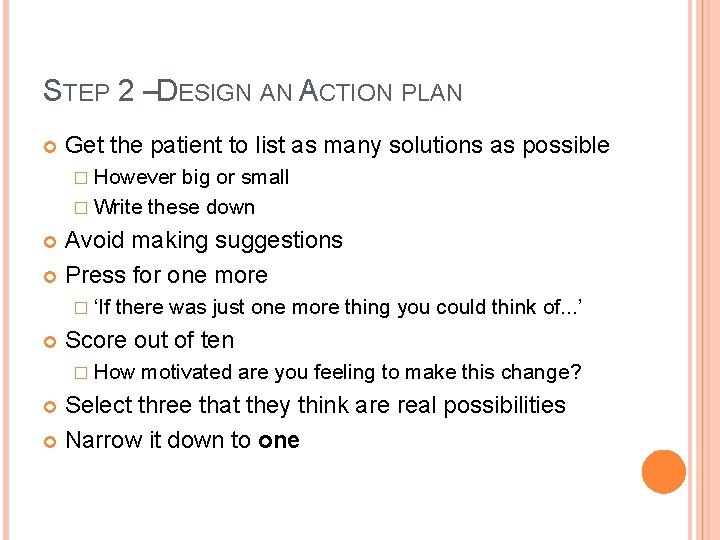
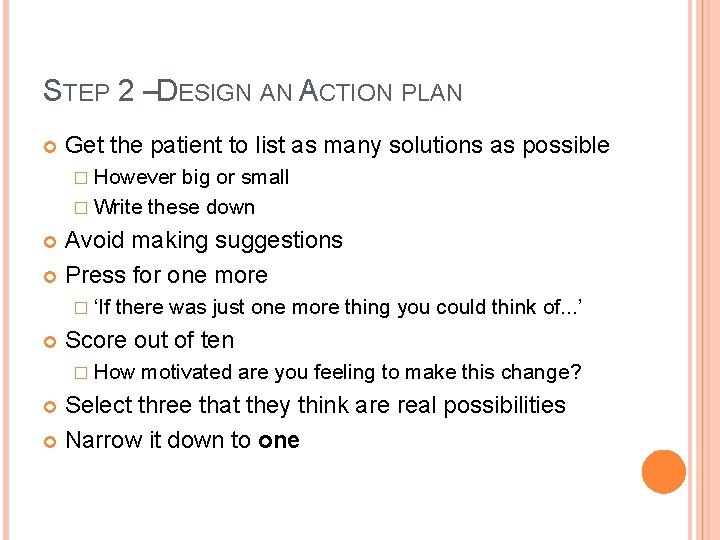
STEP 2 –DESIGN AN ACTION PLAN Get the patient to list as many solutions as possible � However big or small � Write these down Avoid making suggestions Press for one more � ‘If there was just one more thing you could think of. . . ’ Score out of ten � How motivated are you feeling to make this change? Select three that they think are real possibilities Narrow it down to one
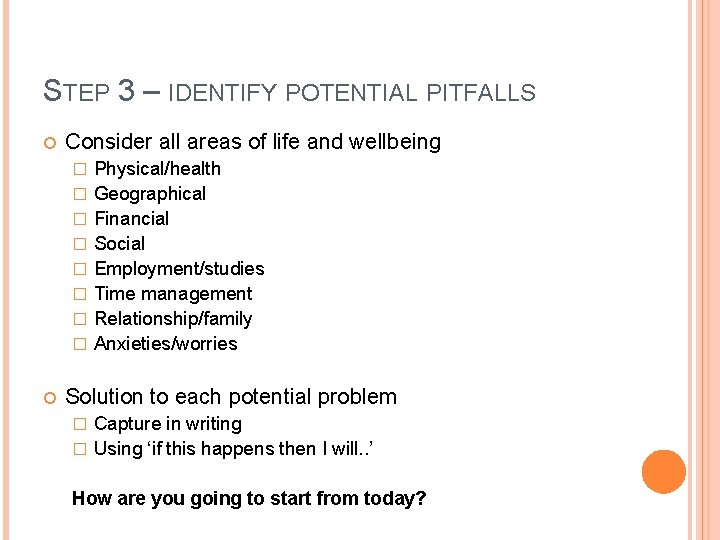
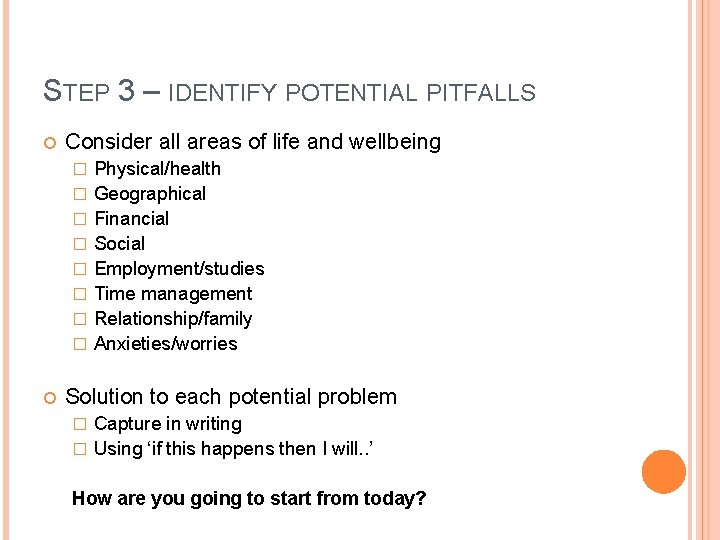
STEP 3 – IDENTIFY POTENTIAL PITFALLS Consider all areas of life and wellbeing � � � � Physical/health Geographical Financial Social Employment/studies Time management Relationship/family Anxieties/worries Solution to each potential problem Capture in writing � Using ‘if this happens then I will. . ’ � How are you going to start from today?
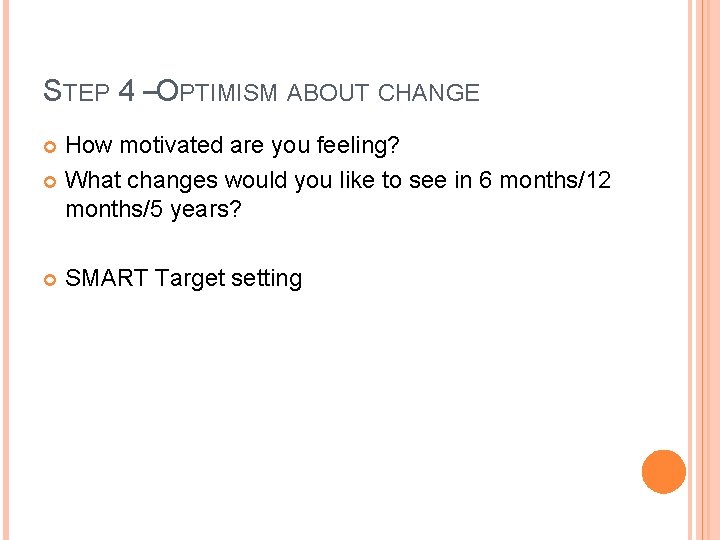
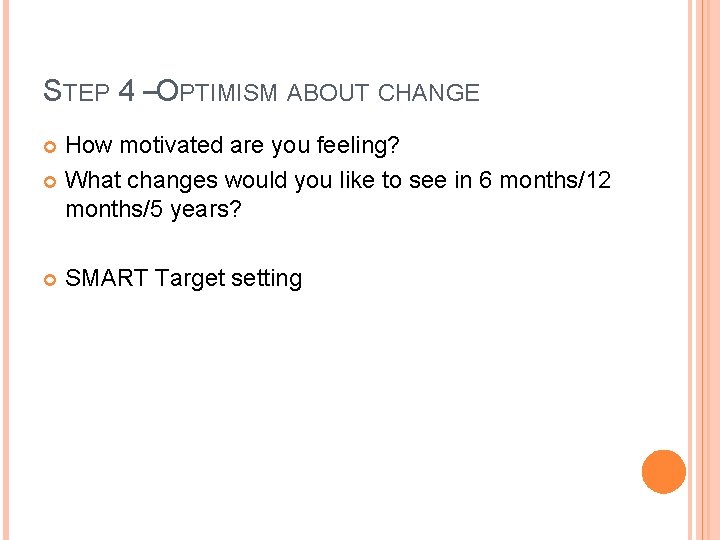
STEP 4 –OPTIMISM ABOUT CHANGE How motivated are you feeling? What changes would you like to see in 6 months/12 months/5 years? SMART Target setting
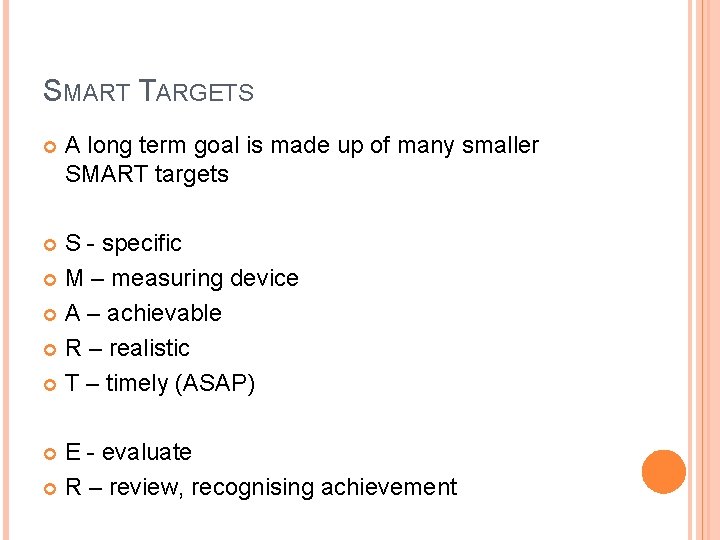
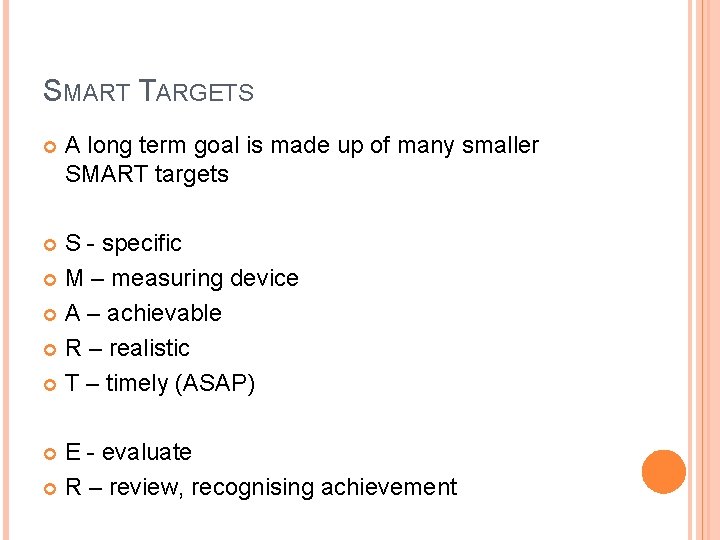
SMART TARGETS A long term goal is made up of many smaller SMART targets S - specific M – measuring device A – achievable R – realistic T – timely (ASAP) E - evaluate R – review, recognising achievement
KEY POINTS 1. 2. 3. 4. Patient-centred approach Explore current concerns Design action plan Think about potential pitfalls SMARTER targets/leave optimistic
ANY QUESTIONS? Thanks for listening!
 Motivational interviewing case management
Motivational interviewing case management Reds motivational interviewing
Reds motivational interviewing Motivational interviewing
Motivational interviewing Mi readiness ruler
Mi readiness ruler Change talk worksheet
Change talk worksheet Dears motivational interviewing
Dears motivational interviewing Darn cat motivational interviewing
Darn cat motivational interviewing Motivational interviewing
Motivational interviewing Darn cat motivational interviewing
Darn cat motivational interviewing Dears motivational interviewing
Dears motivational interviewing Motivational interviewing
Motivational interviewing Motivational interviewing traps
Motivational interviewing traps Ears motivational interviewing
Ears motivational interviewing Motivational interviewing
Motivational interviewing Motivational interviewing preparing people for change
Motivational interviewing preparing people for change Motivational interviewing schizophrenia
Motivational interviewing schizophrenia