Teaching Residents Clinical Leadership and Teamwork Through an


![Didactics: Context Curricular Goals Implementation Didactics [Patient care and medical knowledge] - 1 hr Didactics: Context Curricular Goals Implementation Didactics [Patient care and medical knowledge] - 1 hr](https://slidetodoc.com/presentation_image/322c69f84e2f28af172a966229f3db10/image-15.jpg)
![Team meetings: Context Curricular Goals Implementation Didactics Case-based Team meetings [Professionalism, systems based learning] Team meetings: Context Curricular Goals Implementation Didactics Case-based Team meetings [Professionalism, systems based learning]](https://slidetodoc.com/presentation_image/322c69f84e2f28af172a966229f3db10/image-22.jpg)

- Slides: 32
Teaching Residents Clinical Leadership and Teamwork Through an Outpatient Chronic Disease Curriculum Carla Ainsworth, MD, MPH Elizabeth Hutchinson, MD Swedish Family Medicine-First Hill , Seattle WA
PCMH = The future of primary care
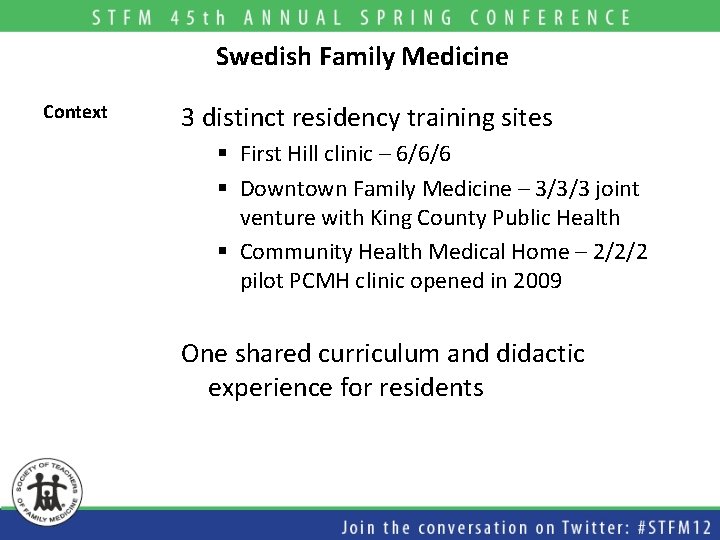
Swedish Family Medicine Context 3 distinct residency training sites § First Hill clinic – 6/6/6 § Downtown Family Medicine – 3/3/3 joint venture with King County Public Health § Community Health Medical Home – 2/2/2 pilot PCMH clinic opened in 2009 One shared curriculum and didactic experience for residents

First Hill clinic Context 32 providers – residents/fellows/faculty RN/MD teams Pharm/Social Work/Behavioral Health
2009 – Time for a curricular change Context Reasons for change Outpatient clinic experience was unpopular § Experience felt unstructured § Residents felt unsupported § Residents lacked confidence Didactic model felt outdated § Treatment focused, not outcome focused § Needed a way to translate teaching to clinic processes and patient panels
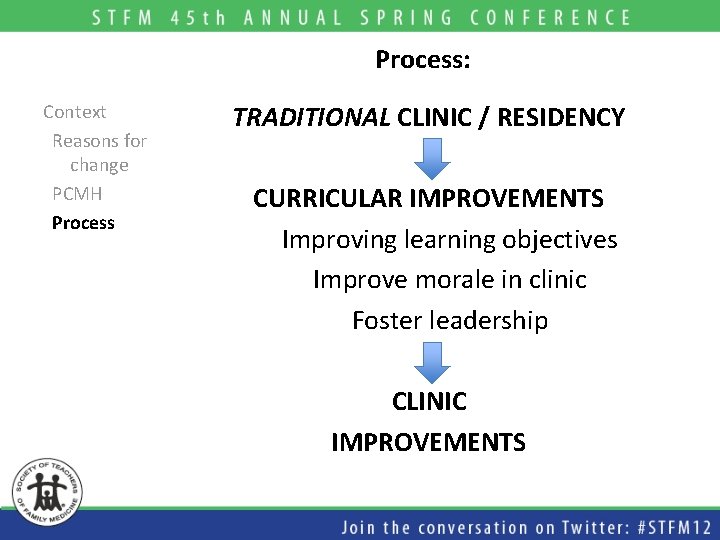
Process: Context Reasons for change PCMH Process TRADITIONAL CLINIC / RESIDENCY CURRICULAR IMPROVEMENTS Improving learning objectives Improve morale in clinic Foster leadership CLINIC IMPROVEMENTS
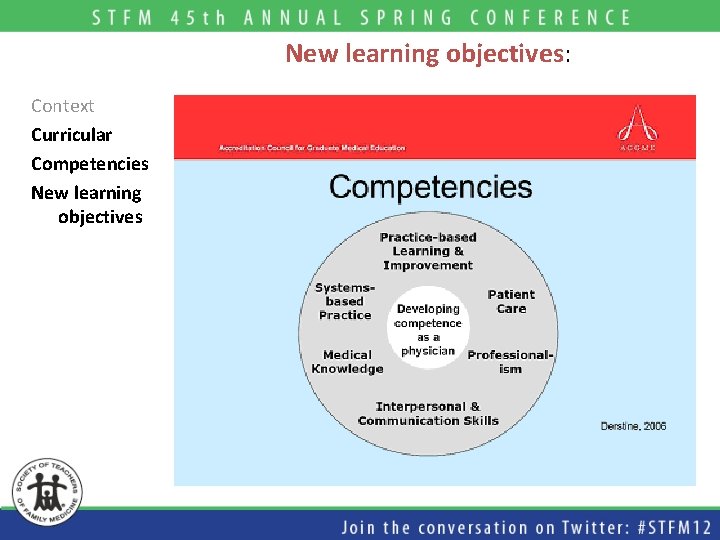
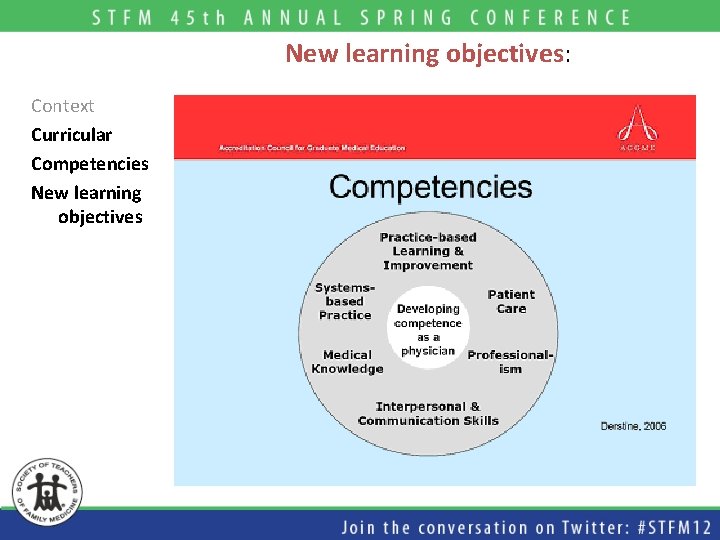
New learning objectives: Context Curricular Competencies New learning objectives
Patient care Context Curricular Competencies New learning objectives Power of the relationship Physician role Continuity of care
Medical knowledge Context Curricular Competencies New learning objectives Chronic disease care: Illness progression Effective interventions Resources for patients Management principles Preventative care Patient centered
Practice based learning Context Curricular Competencies New learning objectives Determine clinically relevant standards Follow patient panels Adapt clinical practice

Interpersonal and communication skills Context Curricular Competencies New learning objectives Communication Patients Nurses Social worker, psychologist pharmacist Consultants Community agencies
Professionalism Context Curricular Competencies New learning objectives Develop leadership skills Function with confidence in clinic Preparation for future practice Foundation for growth after residency
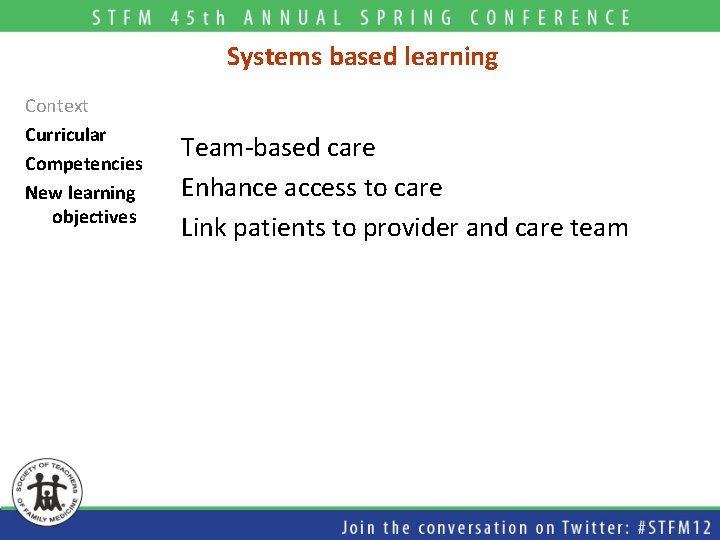
Systems based learning Context Curricular Competencies New learning objectives Team-based care Enhance access to care Link patients to provider and care team
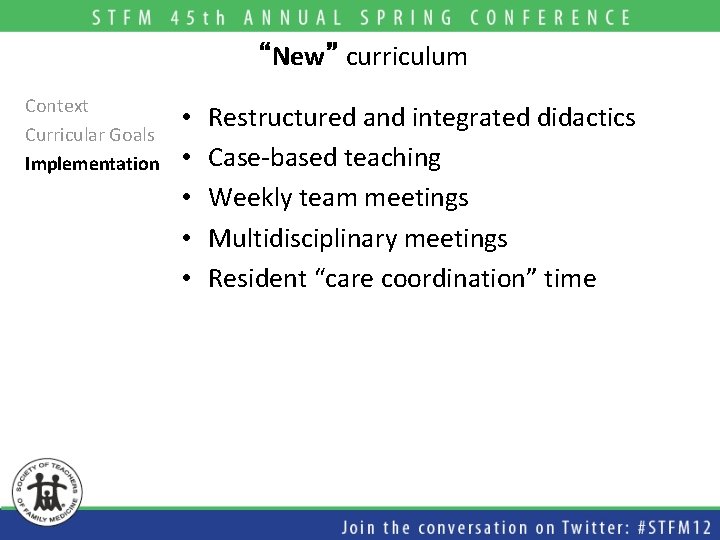
“New” curriculum Context Curricular Goals Implementation • • • Restructured and integrated didactics Case-based teaching Weekly team meetings Multidisciplinary meetings Resident “care coordination” time
![Didactics Context Curricular Goals Implementation Didactics Patient care and medical knowledge 1 hr Didactics: Context Curricular Goals Implementation Didactics [Patient care and medical knowledge] - 1 hr](https://slidetodoc.com/presentation_image/322c69f84e2f28af172a966229f3db10/image-15.jpg)
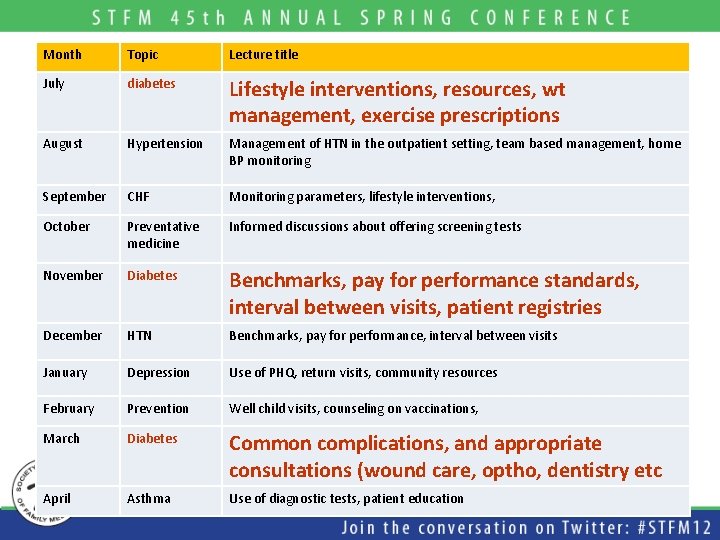
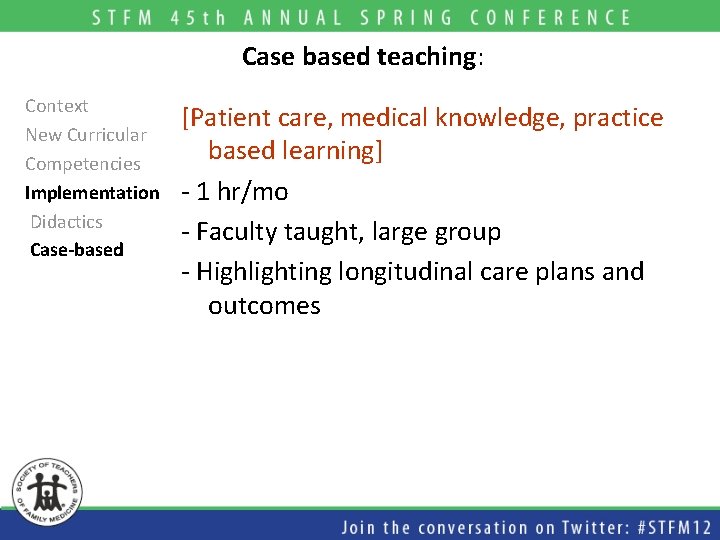
Didactics: Context Curricular Goals Implementation Didactics [Patient care and medical knowledge] - 1 hr / month outpatient topics - Topics chronic disease and preventive medicine [DM, HTN, CHF, asthma, preventative care, care of immigrant populations, depression] - Coordinated with general family medicine didactic schedule
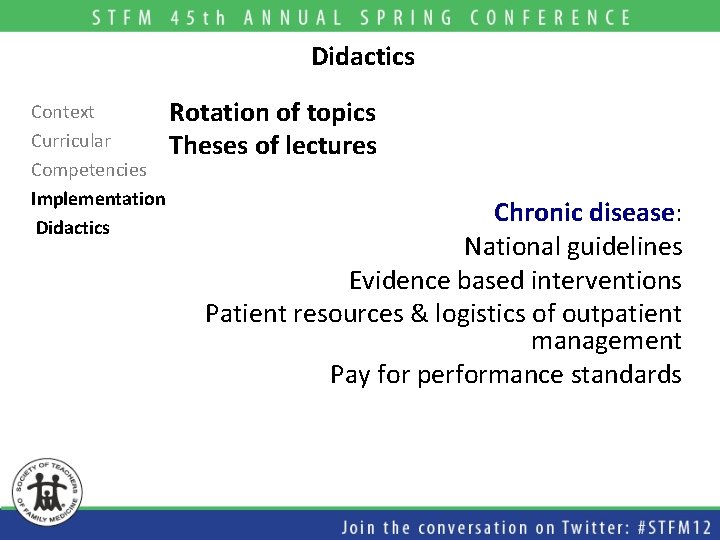
Didactics Context Rotation of topics Curricular Theses of lectures Competencies Implementation Didactics Chronic disease: National guidelines Evidence based interventions Patient resources & logistics of outpatient management Pay for performance standards
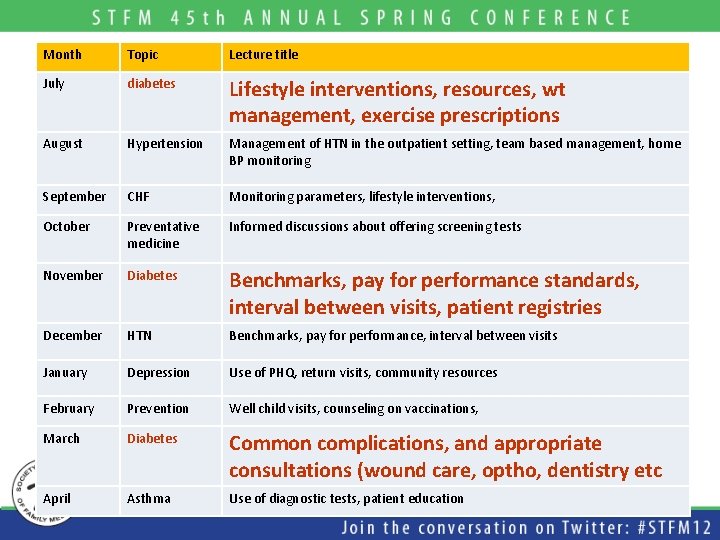
Month Topic Lecture title July diabetes Lifestyle interventions, resources, wt management, exercise prescriptions August Hypertension Management of HTN in the outpatient setting, team based management, home BP monitoring September CHF Monitoring parameters, lifestyle interventions, October Preventative medicine Informed discussions about offering screening tests November Diabetes Benchmarks, pay for performance standards, interval between visits, patient registries December HTN Benchmarks, pay for performance, interval between visits January Depression Use of PHQ, return visits, community resources February Prevention Well child visits, counseling on vaccinations, March Diabetes Common complications, and appropriate consultations (wound care, optho, dentistry etc April Asthma Use of diagnostic tests, patient education
Didactics Context Curricular Competencies Implementation Didactics Preventative medicine: Patient centered Evidenced based
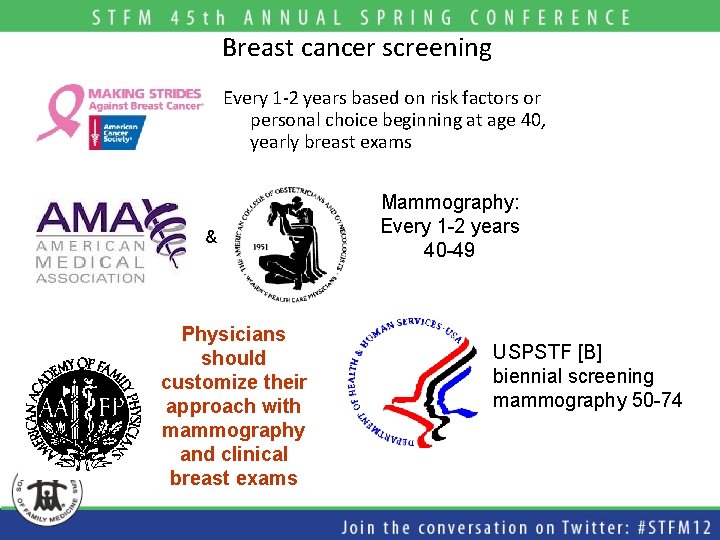
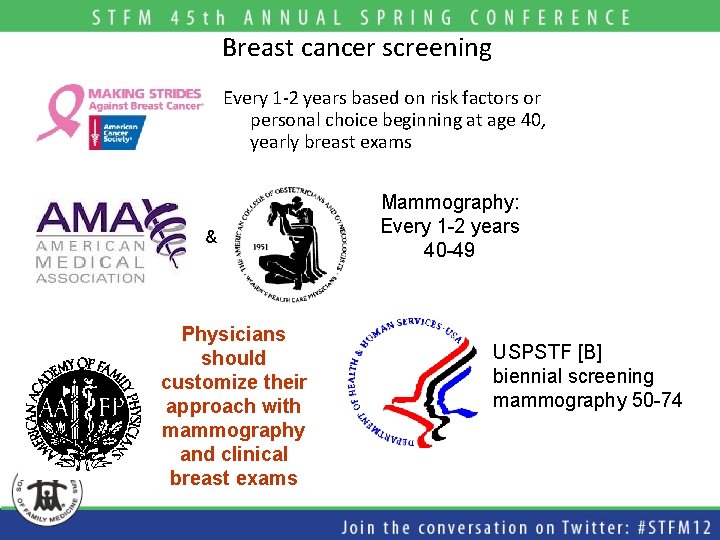
Breast cancer screening Every 1 -2 years based on risk factors or personal choice beginning at age 40, yearly breast exams & Physicians should customize their approach with mammography and clinical breast exams Mammography: Every 1 -2 years 40 -49 USPSTF [B] biennial screening mammography 50 -74
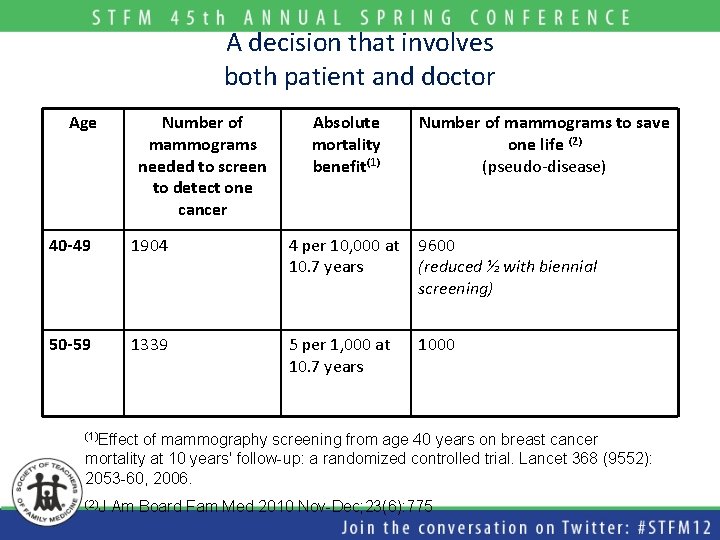
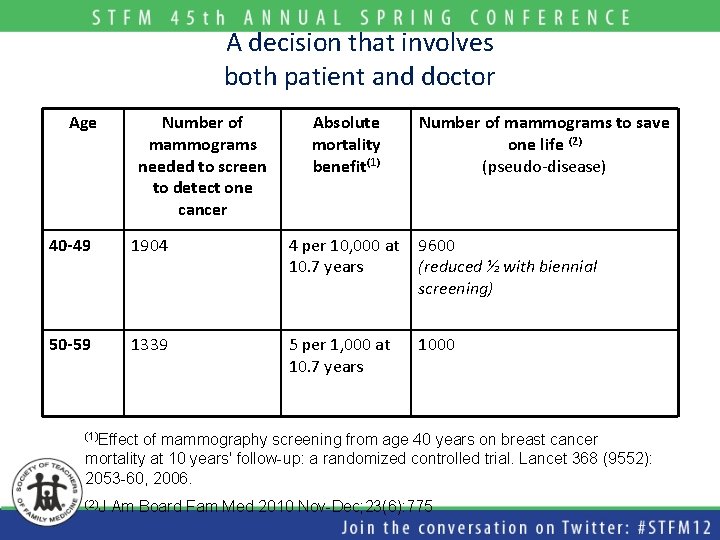
A decision that involves both patient and doctor Age Number of mammograms needed to screen to detect one cancer Absolute mortality benefit(1) Number of mammograms to save one life (2) (pseudo-disease) 40 -49 1904 4 per 10, 000 at 10. 7 years 9600 (reduced ½ with biennial screening) 50 -59 1339 5 per 1, 000 at 10. 7 years 1000 (1)Effect of mammography screening from age 40 years on breast cancer mortality at 10 years' follow-up: a randomized controlled trial. Lancet 368 (9552): 2053 -60, 2006. (2)J Am Board Fam Med 2010 Nov-Dec; 23(6): 775
Case based teaching: Context New Curricular Competencies Implementation Didactics Case-based [Patient care, medical knowledge, practice based learning] - 1 hr/mo - Faculty taught, large group - Highlighting longitudinal care plans and outcomes
![Team meetings Context Curricular Goals Implementation Didactics Casebased Team meetings Professionalism systems based learning Team meetings: Context Curricular Goals Implementation Didactics Case-based Team meetings [Professionalism, systems based learning]](https://slidetodoc.com/presentation_image/322c69f84e2f28af172a966229f3db10/image-22.jpg)
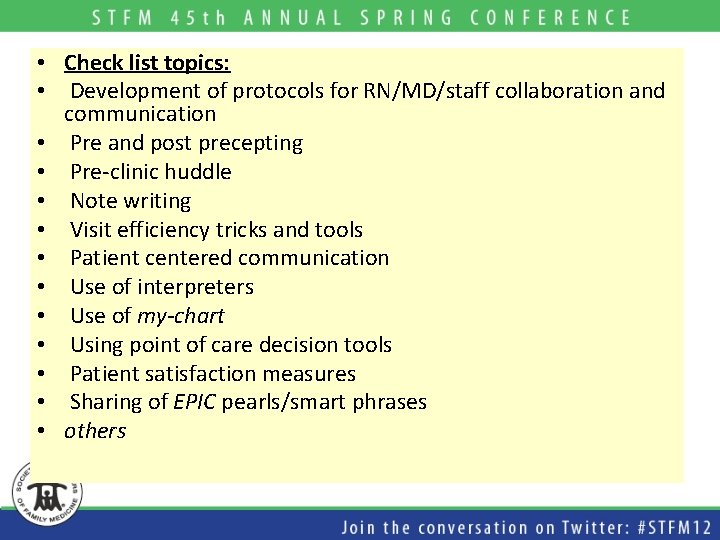
Team meetings: Context Curricular Goals Implementation Didactics Case-based Team meetings [Professionalism, systems based learning] - 30 min/week, delayed clinic start - Monthly panel review, coordinated with didactic teaching - Sharing /creating Epic tools - Topical discussion - Check-list topics
• Check list topics: • Development of protocols for RN/MD/staff collaboration and communication • Pre and post precepting • Pre-clinic huddle • Note writing • Visit efficiency tricks and tools • Patient centered communication • Use of interpreters • Use of my-chart • Using point of care decision tools • Patient satisfaction measures • Sharing of EPIC pearls/smart phrases • others
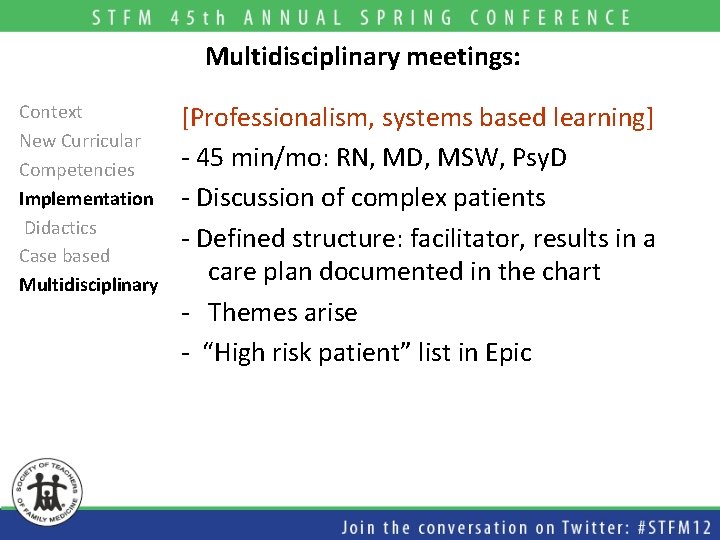
Multidisciplinary meetings: Context New Curricular Competencies Implementation Didactics Case based Multidisciplinary [Professionalism, systems based learning] - 45 min/mo: RN, MD, MSW, Psy. D - Discussion of complex patients - Defined structure: facilitator, results in a care plan documented in the chart - Themes arise - “High risk patient” list in Epic
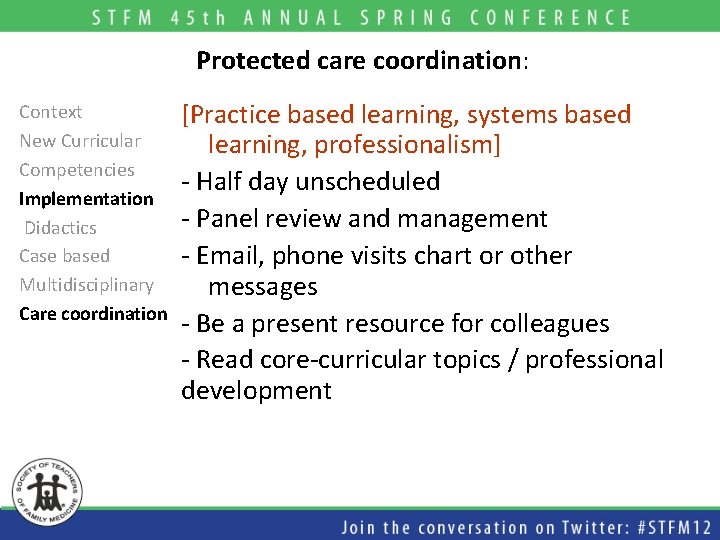
Protected care coordination: Context New Curricular Competencies Implementation Didactics Case based Multidisciplinary Care coordination [Practice based learning, systems based learning, professionalism] - Half day unscheduled - Panel review and management - Email, phone visits chart or other messages - Be a present resource for colleagues - Read core-curricular topics / professional development
Two years later – How did it go? Outcome – resident experience and competence § What worked? § What didn’t? § What should we do next?
Successes Context Curricular Goals Implementation Changes Outcomes Improvement 1. Medical knowledge: more comfortable managing diabetes & HTN 2. Teamwork: more likely to incorporate clinic staff in patient care plans 3. Enhance access to care: gaining skills with asynchronous communication 4. Care coordination: improvement in population management 5. Morale: improved
Areas that need work Context Curricular Goals Implementation Changes Outcomes Improvement Improving 1. Leadership: residents struggle with applying principles of the “medical home” 2. Care coordination: lack of incentive to actively manage a population
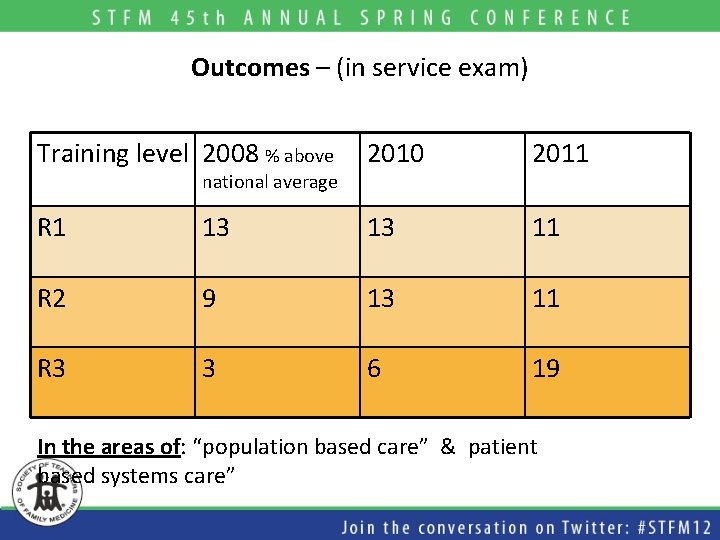
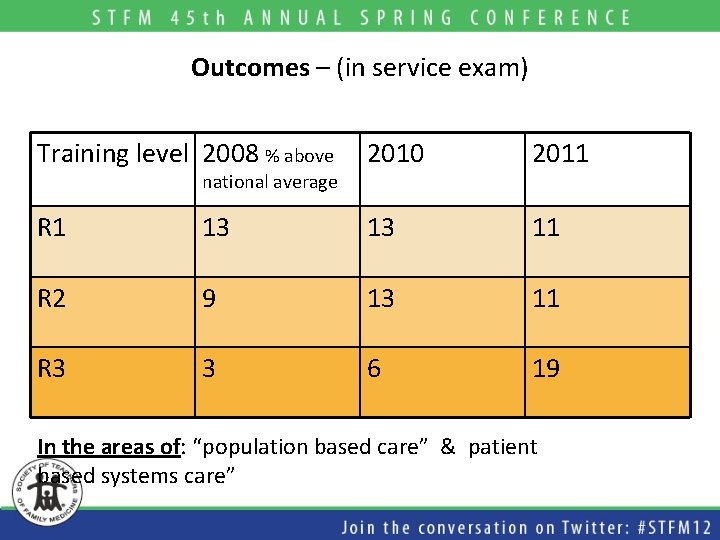
Outcomes – (in service exam) Training level 2008 % above 2010 2011 R 1 13 13 11 R 2 9 13 11 R 3 3 6 19 national average In the areas of: “population based care” & patient based systems care”
Questions we have Context Curricular Goals Implementation Changes Outcomes Discussion How do you support resident morale in clinic? How have you changed how you teach outpatient medicine to your learners in the past 5 years? How do you train learners to work in multidisciplinary teams? How does that change over the course of their training?

Next steps for us Context Curricular Goals Implementati on Changes Outcomes Discussion Barriers Next steps Better outcomes data to support panel management Improved ability to match patient with PCP
Lessons learned • Curriculum redesign can be the driver of practice transformation • We can increase residents’ competence in and enjoyment of clinic at the same time
 Make an acrostic poem using the word teamwork.
Make an acrostic poem using the word teamwork. Chapter 14 teamwork and leadership
Chapter 14 teamwork and leadership Teamwork
Teamwork Disadvantages of tangential sawing
Disadvantages of tangential sawing Set dialogue closure
Set dialogue closure Rcn clinical leadership programme
Rcn clinical leadership programme Definitions of microteaching
Definitions of microteaching Transactional vs transformational leadership
Transactional vs transformational leadership Amy lee plastic surgery
Amy lee plastic surgery Umass pharmacy residency
Umass pharmacy residency Dr kirk kleinfeld
Dr kirk kleinfeld Dr sarah gernhart
Dr sarah gernhart Uihc internal medicine residency
Uihc internal medicine residency Tufts anesthesiology residency
Tufts anesthesiology residency Unmc obgyn residents
Unmc obgyn residents Paro call stipend
Paro call stipend Informed delivery for business mailers
Informed delivery for business mailers Unm emergency medicine residents
Unm emergency medicine residents Uthscsa family medicine residency
Uthscsa family medicine residency Karl suure tähtsaim residents
Karl suure tähtsaim residents Tourism involving non-residents of the given area.
Tourism involving non-residents of the given area. How can an na best help residents with eating?
How can an na best help residents with eating? Cna chapter 6 personal care skills
Cna chapter 6 personal care skills Famous yonkers residents
Famous yonkers residents St louis family medicine residency
St louis family medicine residency Uf neurology residency
Uf neurology residency Transforming teacher education through clinical practice
Transforming teacher education through clinical practice Sin entered through one man
Sin entered through one man Furcation involvement
Furcation involvement Summary of the poem night of the scorpion by nissim ezekiel
Summary of the poem night of the scorpion by nissim ezekiel Adaptive leadership theory
Adaptive leadership theory Situational leadership vs adaptive leadership
Situational leadership vs adaptive leadership Alicia burdess teaching through problem solving
Alicia burdess teaching through problem solving