Surgical Protocol for External Ventricular Catheter EVD Placement
- Slides: 25
Surgical Protocol for External Ventricular Catheter (EVD) Placement for CLEAR III Trial Surgical Coordinating Center for CLEAR III North. Shore University Health. System Evanston, Illinois Revised May 12, 2009
General Principles • All EVD placements are performed under full sterile technique (cap, gown, gloves, mask, full draping), and by the most senior skilled surgeon (housestaff or attending) immediately available to perform the EVD procedure. • When more than two passes are required for EVD placement, additional stabilization of catheter site will be determined with a CT performed at 24 hours after placement before proceeding with CLEAR. • Suboptimal catheter placements are all too frequent, and are associated with less efficient IVH clearance. Hence it is important to optimize surgical technique for EVD placement in every case and to consider image guided insertion whenever possible
Emergent versus Image Guided Techniques of EVD Placement • Emergent EVD Placement is typically performed using the twist drill and external landmarks in the ICU or Emergency Department setting for the first catheter placement, whenever intracranial pressure (ICP) control is an issue and per the surgeon’s clinical judgment. • Image guided EVD Placement is considered for placement of the second EVD (clot producing trapped ventricles, clinically important shifts, or panventricular enlargement with effacement/ischemia-- typically with larger IVH > 40 cc), or for elective catheter replacement (infection, obstruction, malposition, unplanned migration or withdrawal of previous EVD).
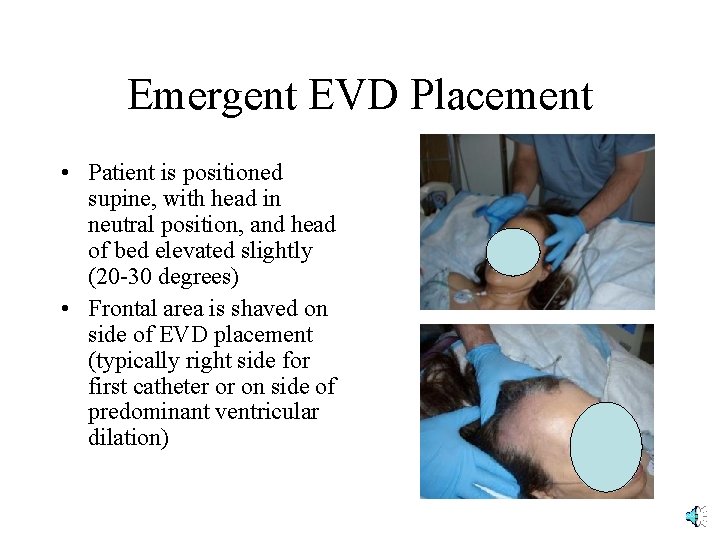
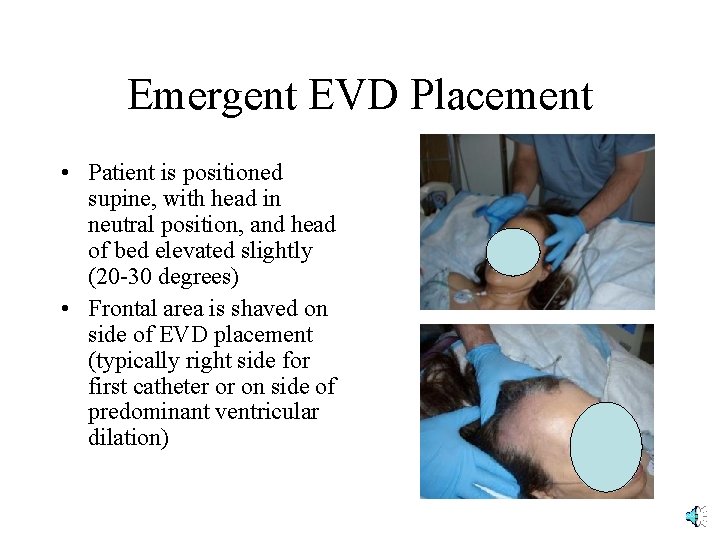
Emergent EVD Placement • Patient is positioned supine, with head in neutral position, and head of bed elevated slightly (20 -30 degrees) • Frontal area is shaved on side of EVD placement (typically right side for first catheter or on side of predominant ventricular dilation)
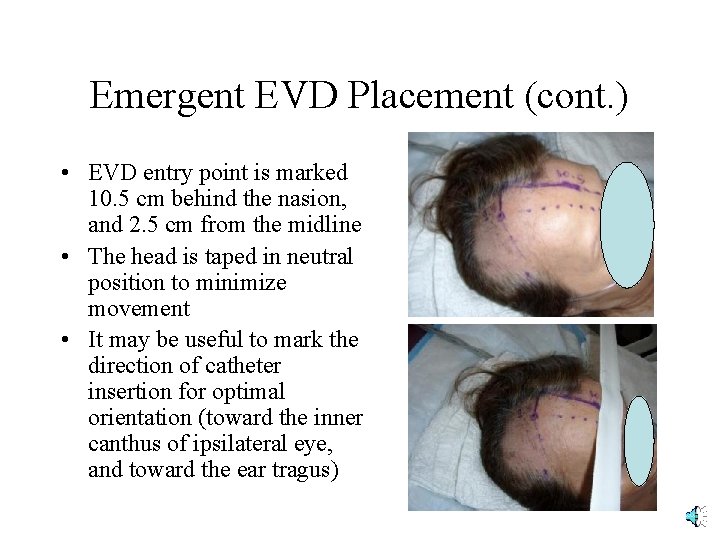
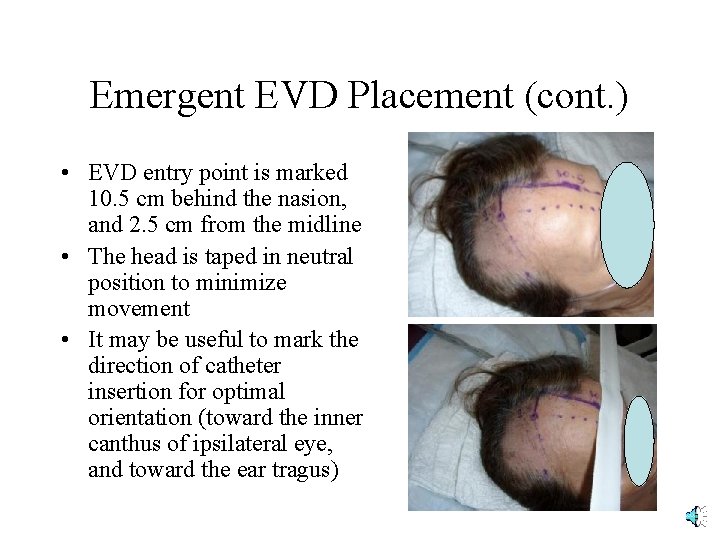
Emergent EVD Placement (cont. ) • EVD entry point is marked 10. 5 cm behind the nasion, and 2. 5 cm from the midline • The head is taped in neutral position to minimize movement • It may be useful to mark the direction of catheter insertion for optimal orientation (toward the inner canthus of ipsilateral eye, and toward the ear tragus)
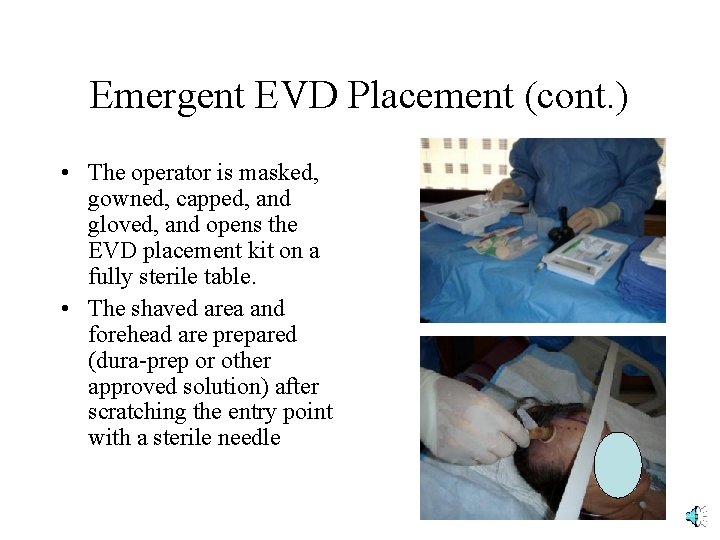
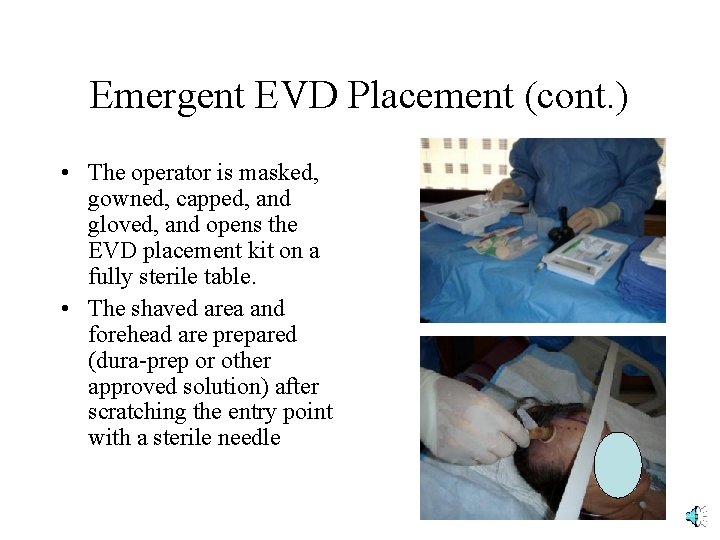
Emergent EVD Placement (cont. ) • The operator is masked, gowned, capped, and gloved, and opens the EVD placement kit on a fully sterile table. • The shaved area and forehead are prepared (dura-prep or other approved solution) after scratching the entry point with a sterile needle
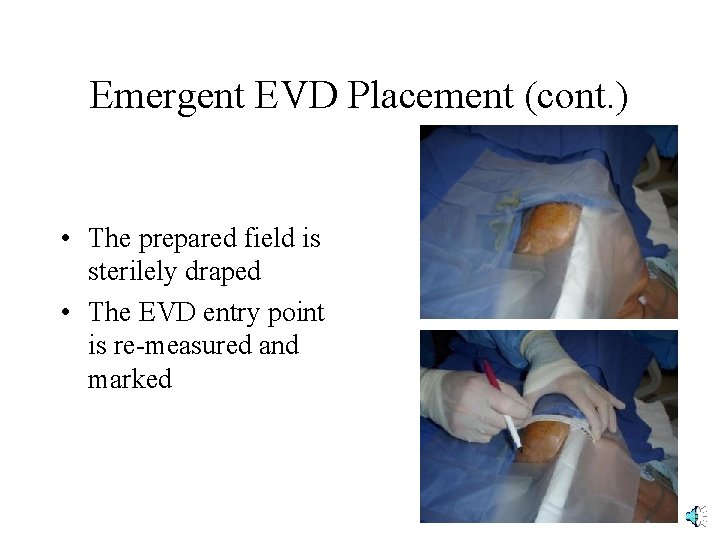
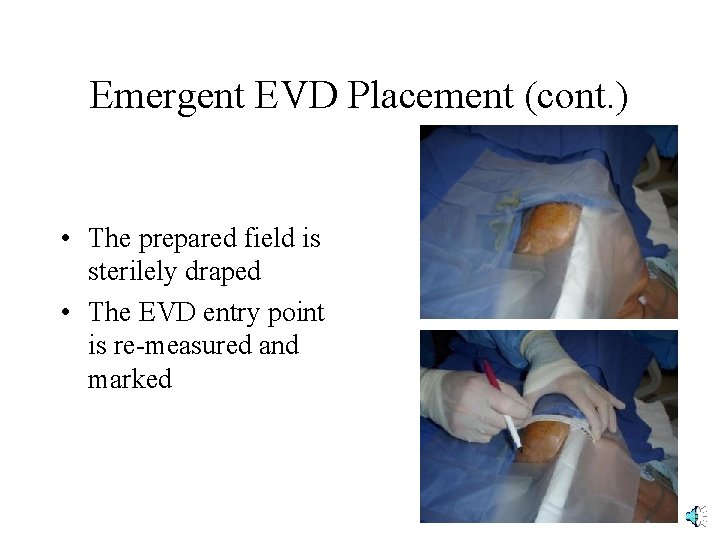
Emergent EVD Placement (cont. ) • The prepared field is sterilely draped • The EVD entry point is re-measured and marked
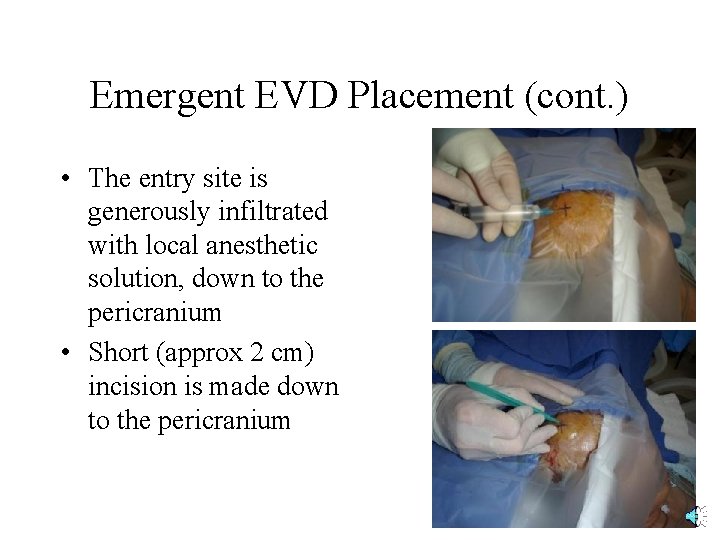
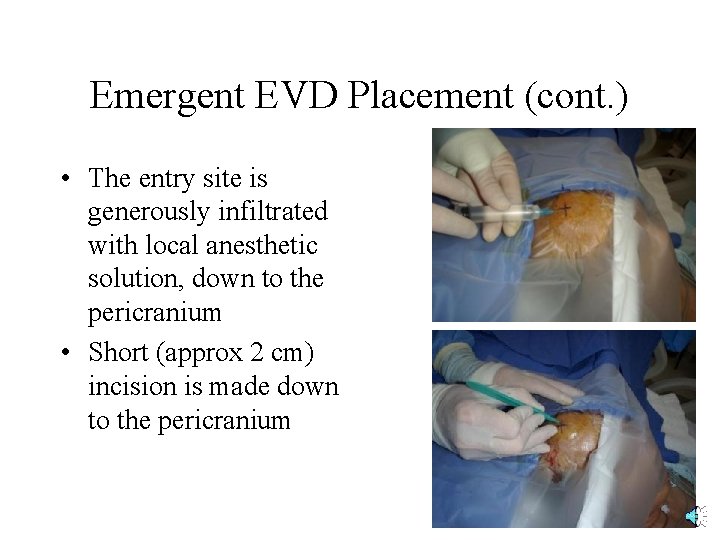
Emergent EVD Placement (cont. ) • The entry site is generously infiltrated with local anesthetic solution, down to the pericranium • Short (approx 2 cm) incision is made down to the pericranium
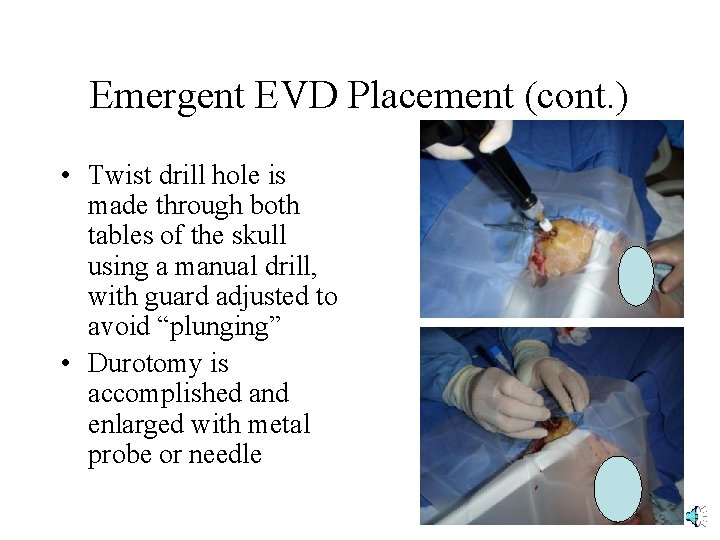
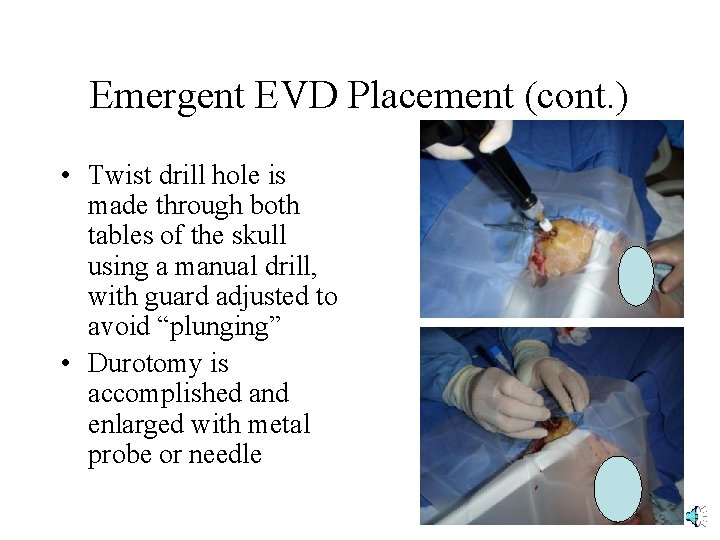
Emergent EVD Placement (cont. ) • Twist drill hole is made through both tables of the skull using a manual drill, with guard adjusted to avoid “plunging” • Durotomy is accomplished and enlarged with metal probe or needle
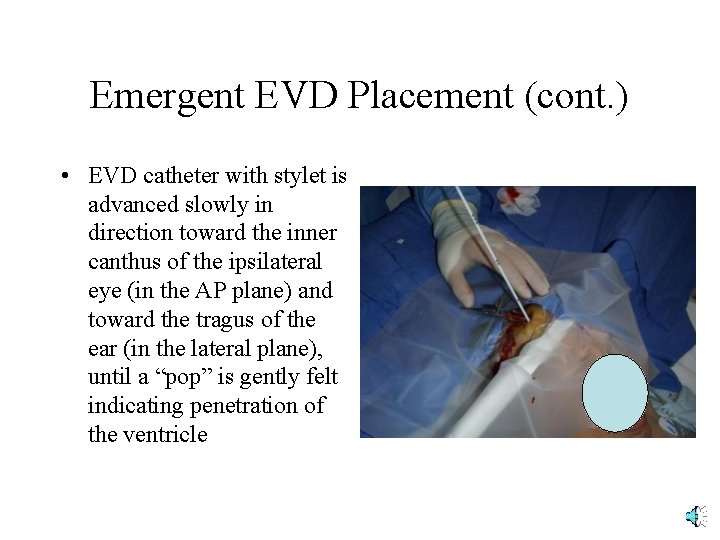
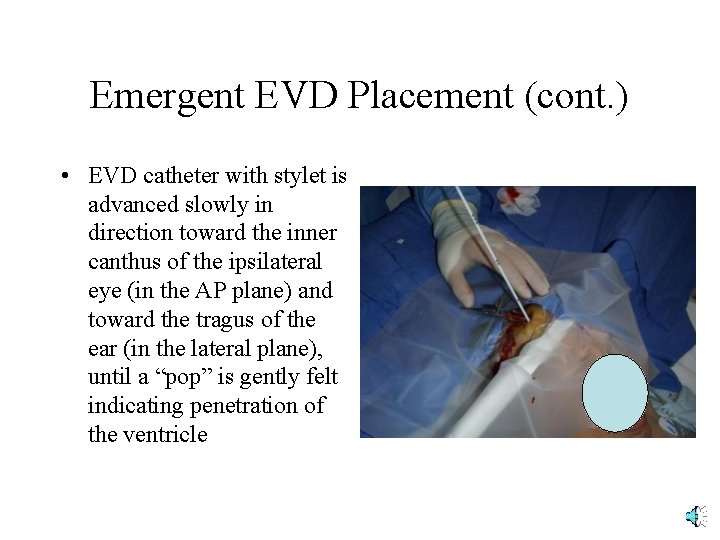
Emergent EVD Placement (cont. ) • EVD catheter with stylet is advanced slowly in direction toward the inner canthus of the ipsilateral eye (in the AP plane) and toward the tragus of the ear (in the lateral plane), until a “pop” is gently felt indicating penetration of the ventricle
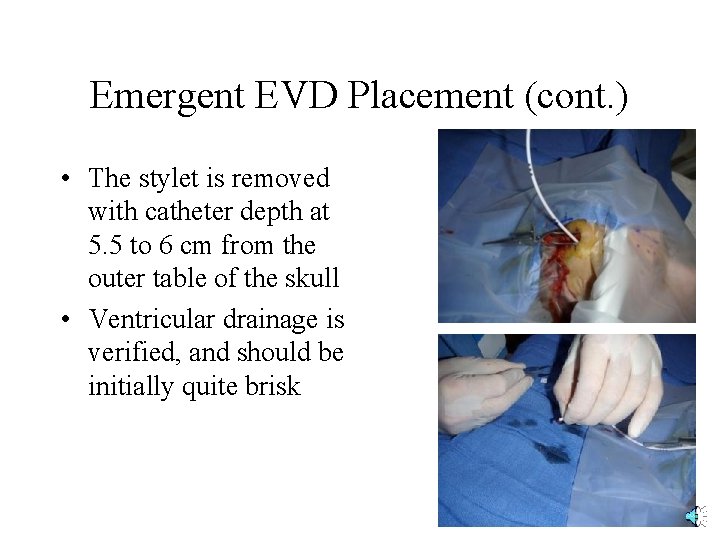
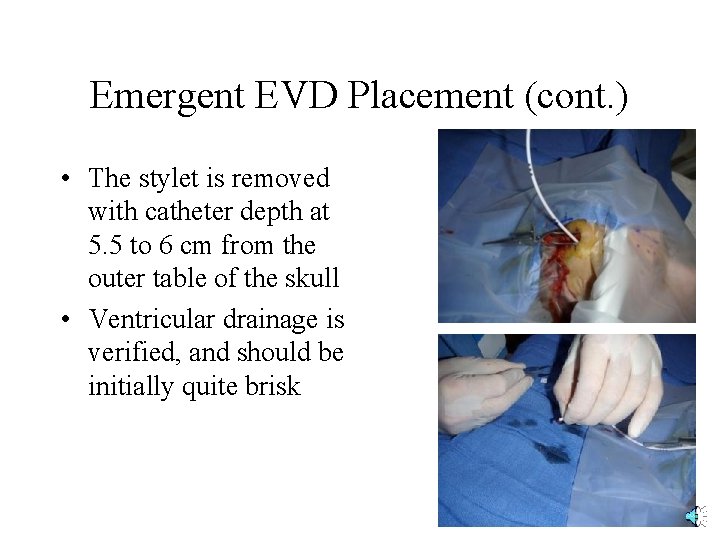
Emergent EVD Placement (cont. ) • The stylet is removed with catheter depth at 5. 5 to 6 cm from the outer table of the skull • Ventricular drainage is verified, and should be initially quite brisk
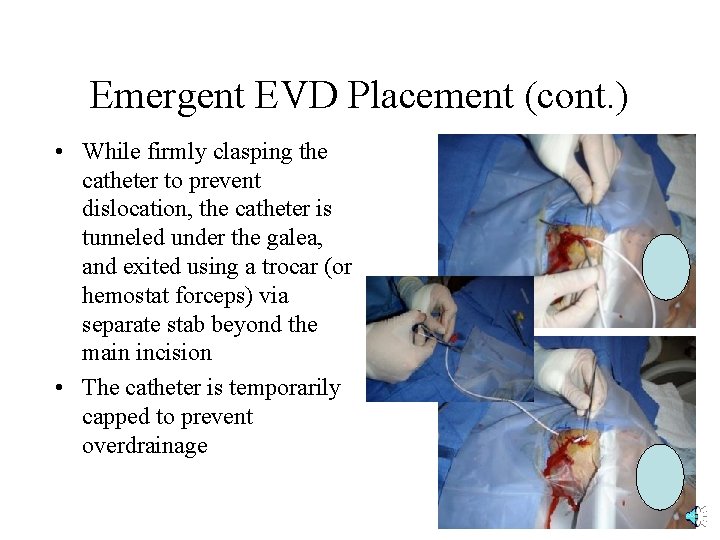
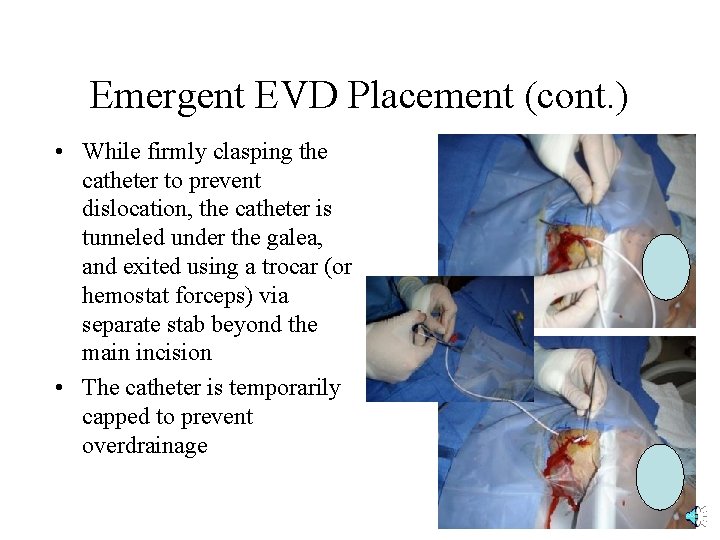
Emergent EVD Placement (cont. ) • While firmly clasping the catheter to prevent dislocation, the catheter is tunneled under the galea, and exited using a trocar (or hemostat forceps) via separate stab beyond the main incision • The catheter is temporarily capped to prevent overdrainage
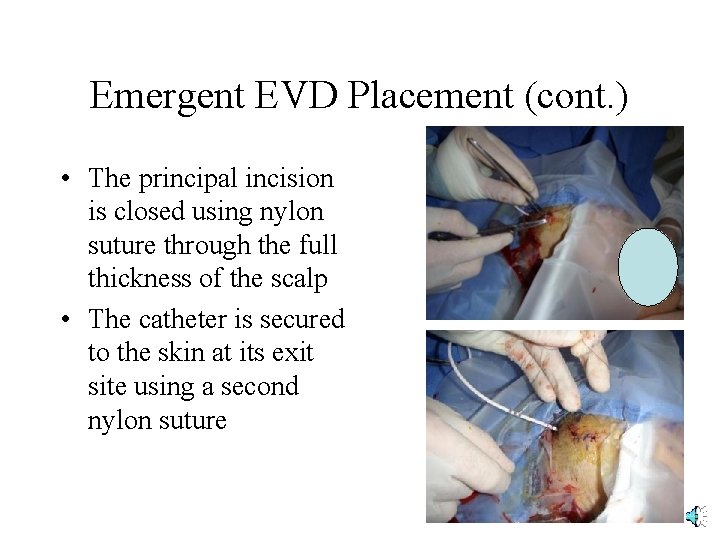
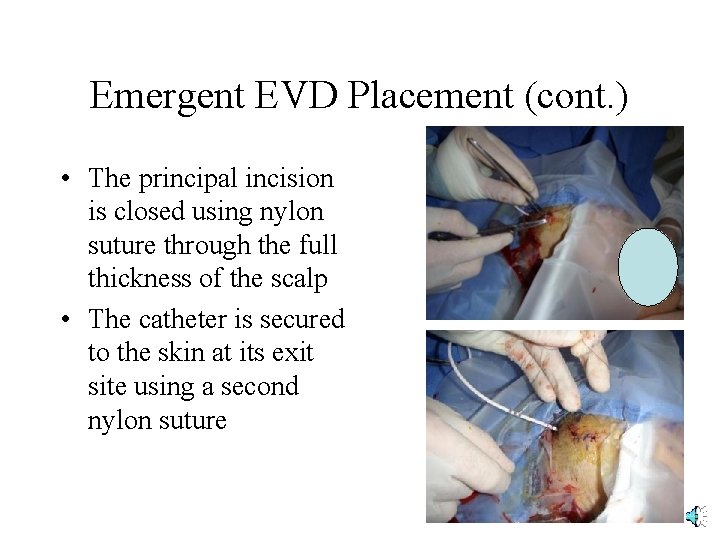
Emergent EVD Placement (cont. ) • The principal incision is closed using nylon suture through the full thickness of the scalp • The catheter is secured to the skin at its exit site using a second nylon suture
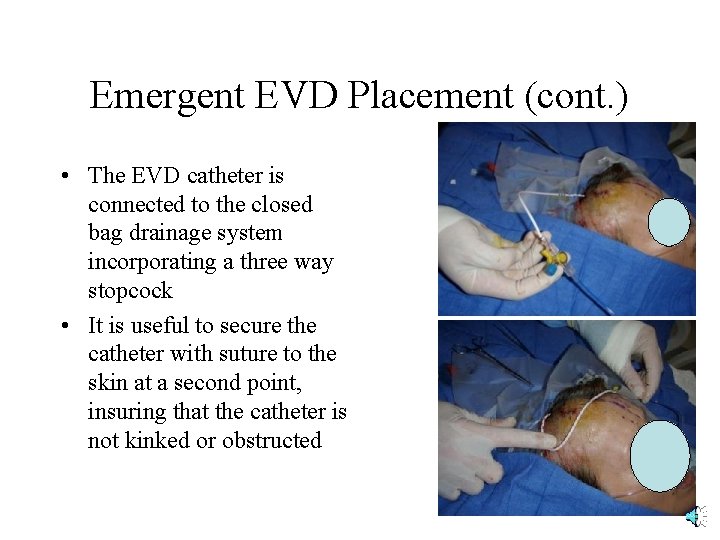
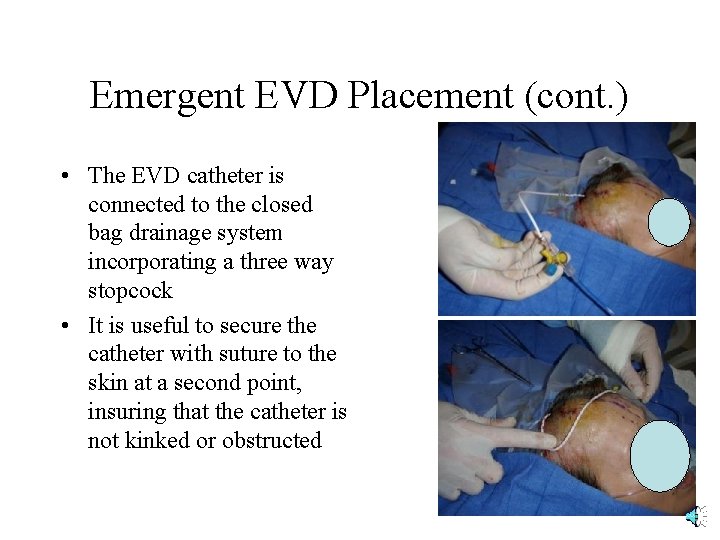
Emergent EVD Placement (cont. ) • The EVD catheter is connected to the closed bag drainage system incorporating a three way stopcock • It is useful to secure the catheter with suture to the skin at a second point, insuring that the catheter is not kinked or obstructed
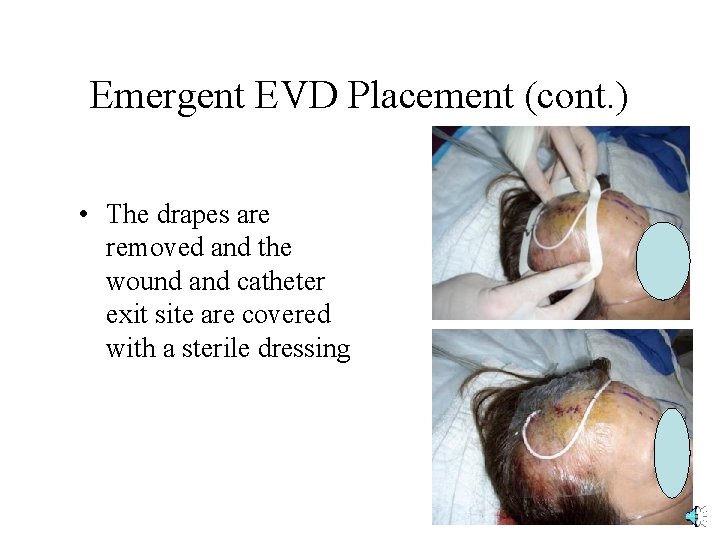
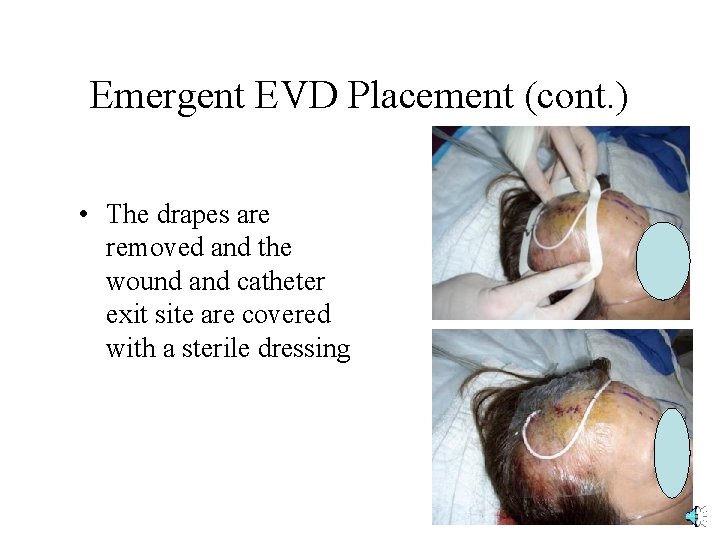
Emergent EVD Placement (cont. ) • The drapes are removed and the wound and catheter exit site are covered with a sterile dressing
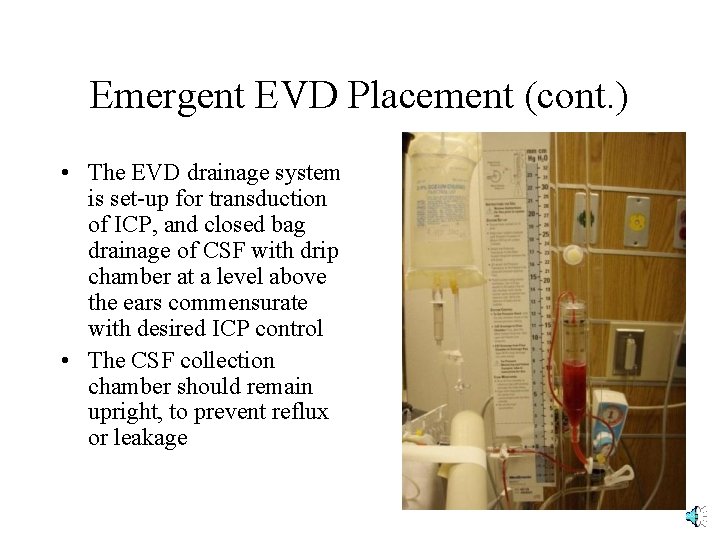
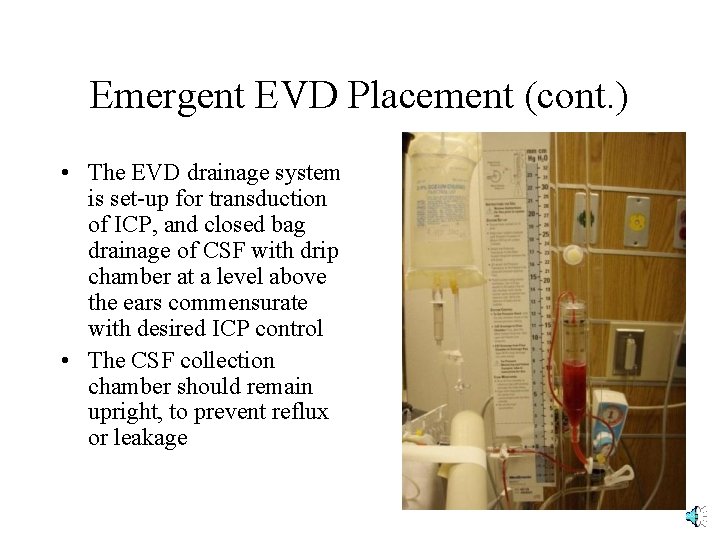
Emergent EVD Placement (cont. ) • The EVD drainage system is set-up for transduction of ICP, and closed bag drainage of CSF with drip chamber at a level above the ears commensurate with desired ICP control • The CSF collection chamber should remain upright, to prevent reflux or leakage
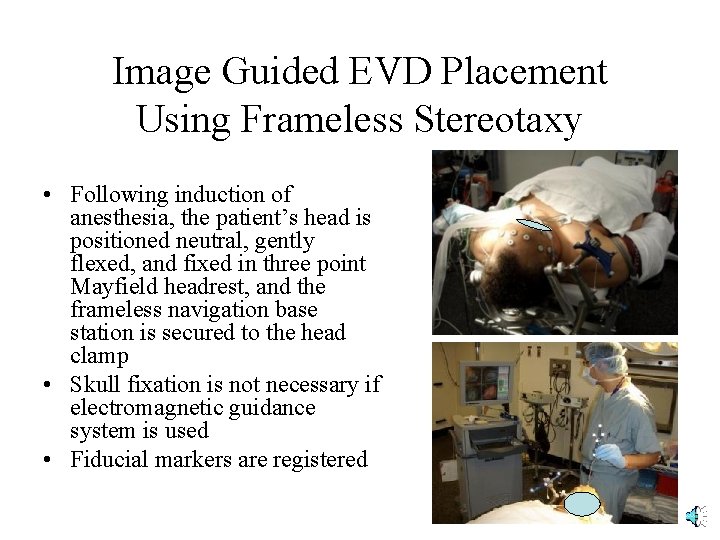
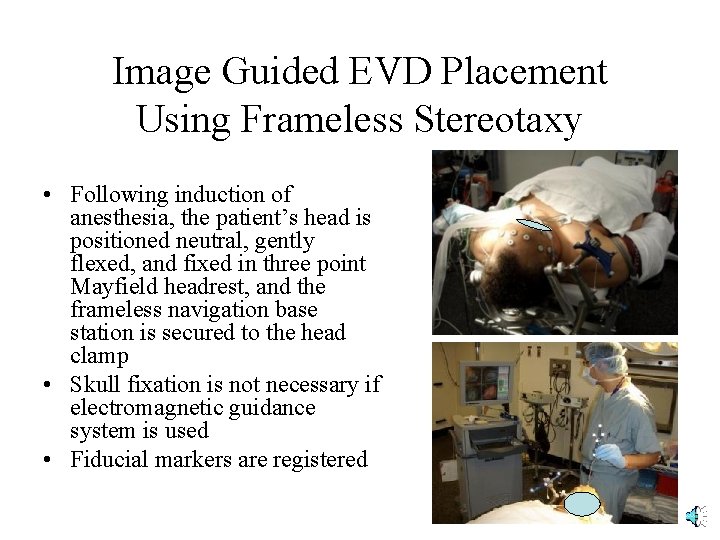
Image Guided EVD Placement Using Frameless Stereotaxy • Following induction of anesthesia, the patient’s head is positioned neutral, gently flexed, and fixed in three point Mayfield headrest, and the frameless navigation base station is secured to the head clamp • Skull fixation is not necessary if electromagnetic guidance system is used • Fiducial markers are registered
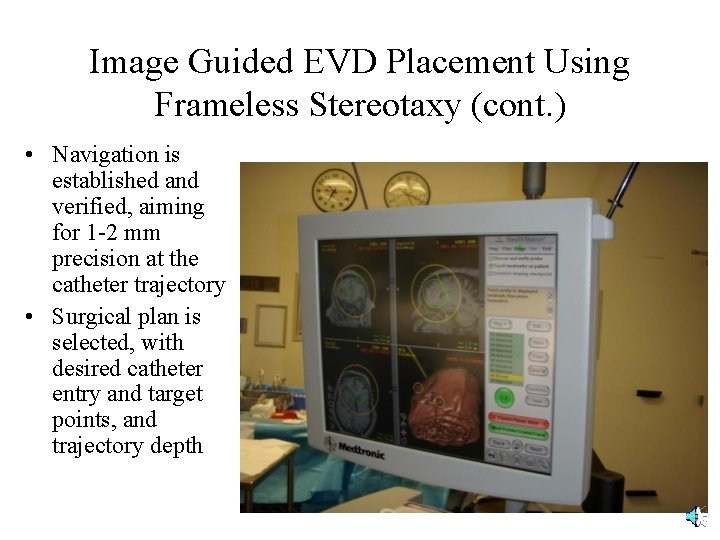
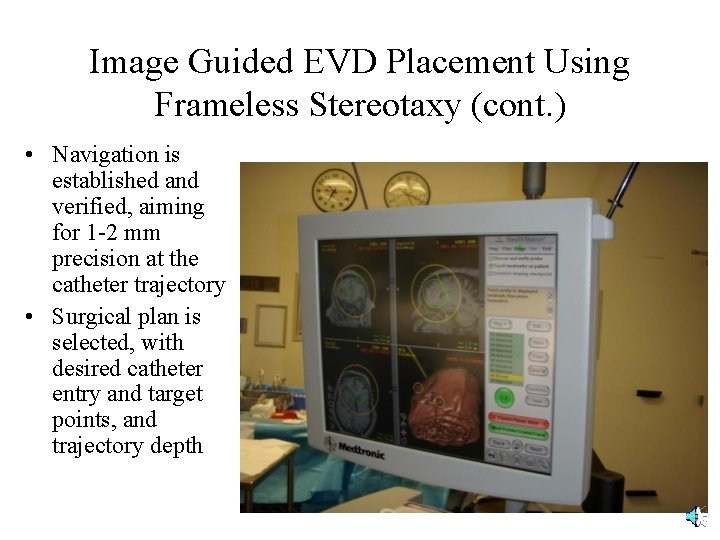
Image Guided EVD Placement Using Frameless Stereotaxy (cont. ) • Navigation is established and verified, aiming for 1 -2 mm precision at the catheter trajectory • Surgical plan is selected, with desired catheter entry and target points, and trajectory depth
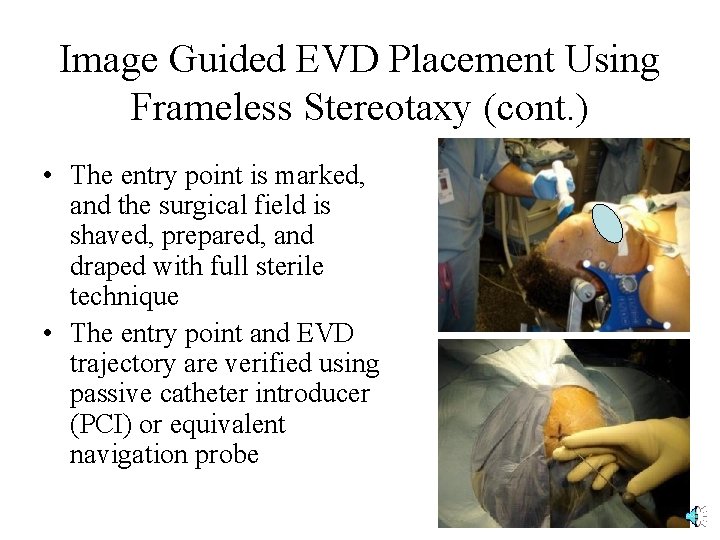
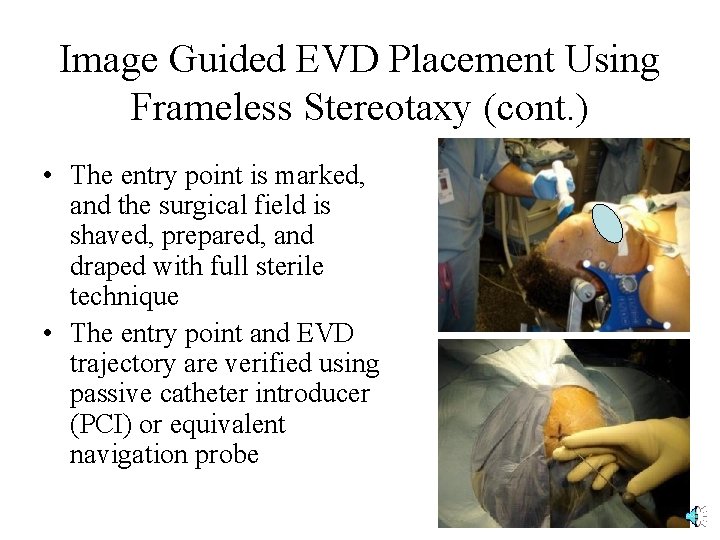
Image Guided EVD Placement Using Frameless Stereotaxy (cont. ) • The entry point is marked, and the surgical field is shaved, prepared, and draped with full sterile technique • The entry point and EVD trajectory are verified using passive catheter introducer (PCI) or equivalent navigation probe
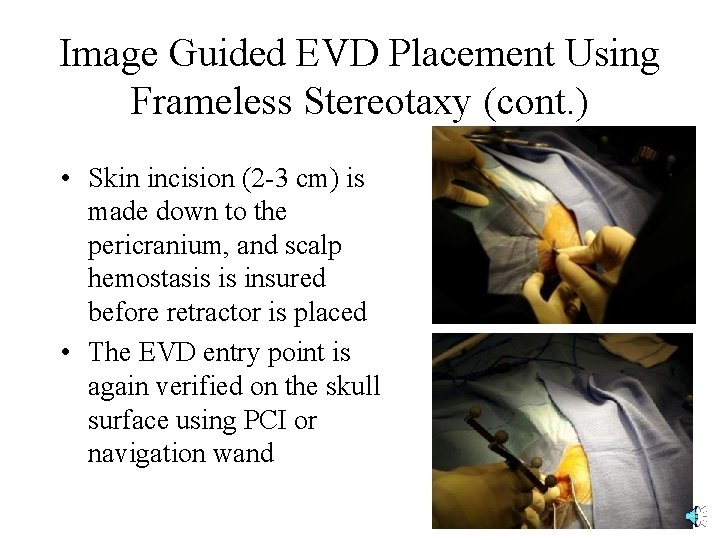
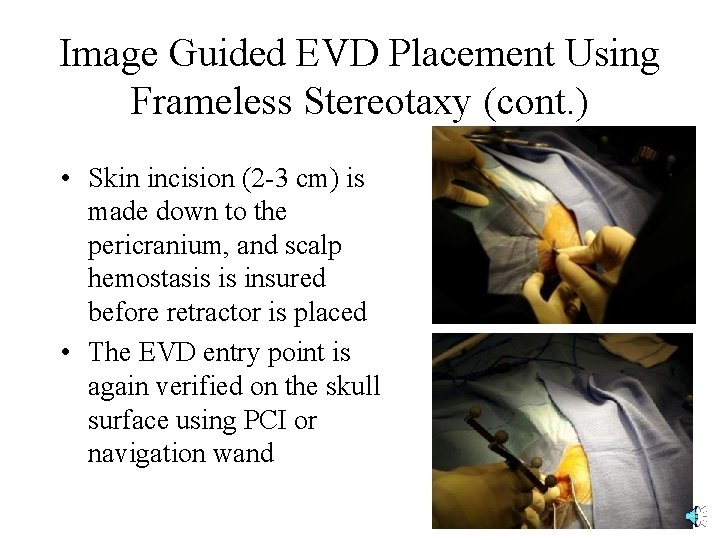
Image Guided EVD Placement Using Frameless Stereotaxy (cont. ) • Skin incision (2 -3 cm) is made down to the pericranium, and scalp hemostasis is insured before retractor is placed • The EVD entry point is again verified on the skull surface using PCI or navigation wand
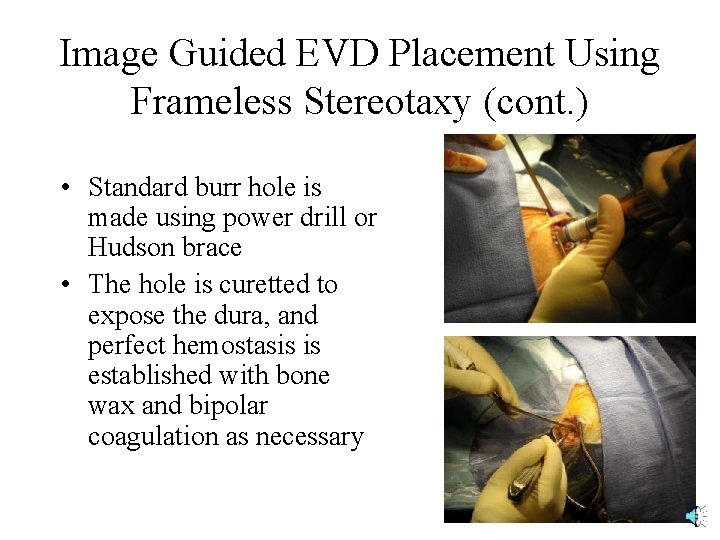
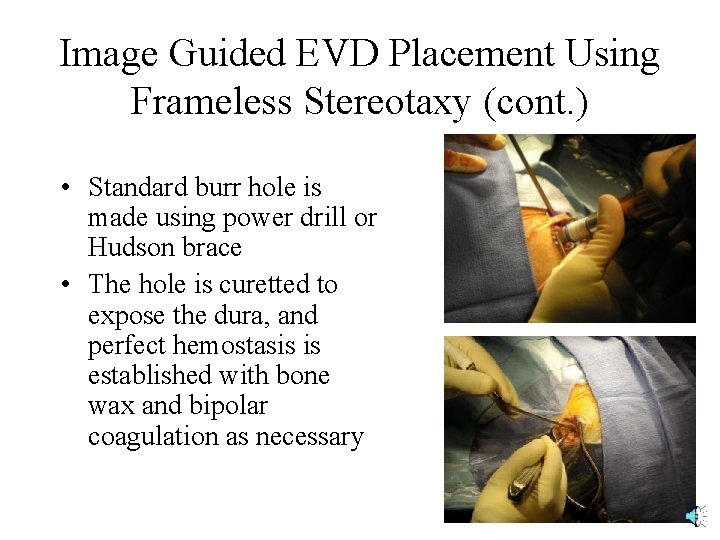
Image Guided EVD Placement Using Frameless Stereotaxy (cont. ) • Standard burr hole is made using power drill or Hudson brace • The hole is curetted to expose the dura, and perfect hemostasis is established with bone wax and bipolar coagulation as necessary
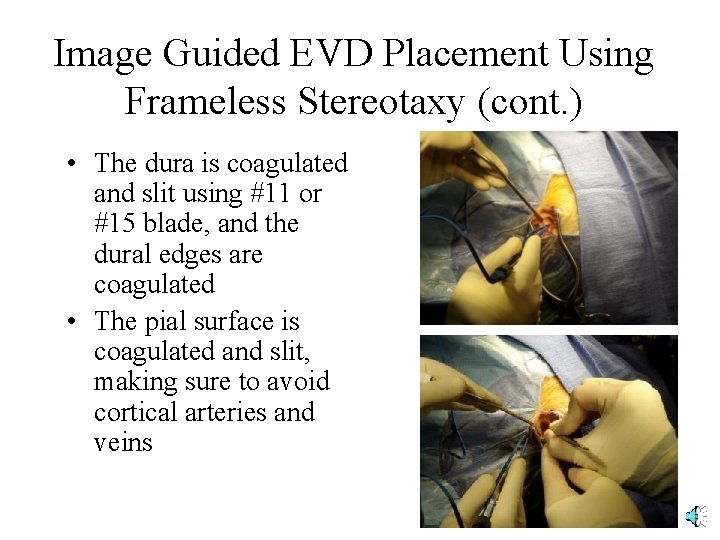
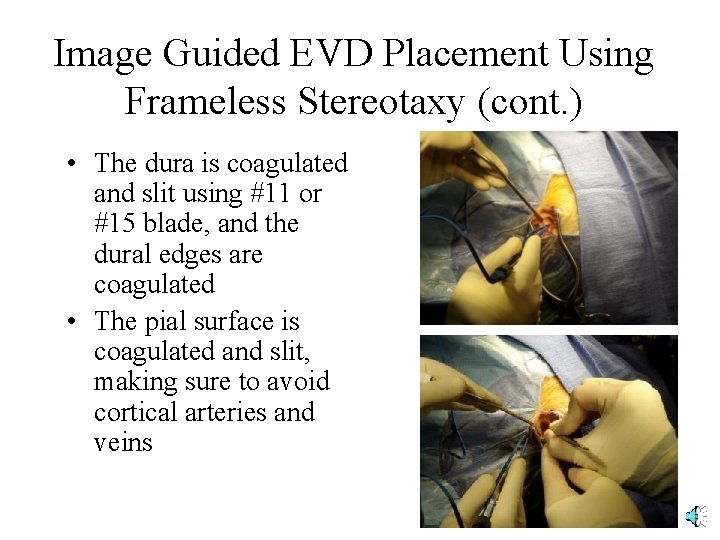
Image Guided EVD Placement Using Frameless Stereotaxy (cont. ) • The dura is coagulated and slit using #11 or #15 blade, and the dural edges are coagulated • The pial surface is coagulated and slit, making sure to avoid cortical arteries and veins
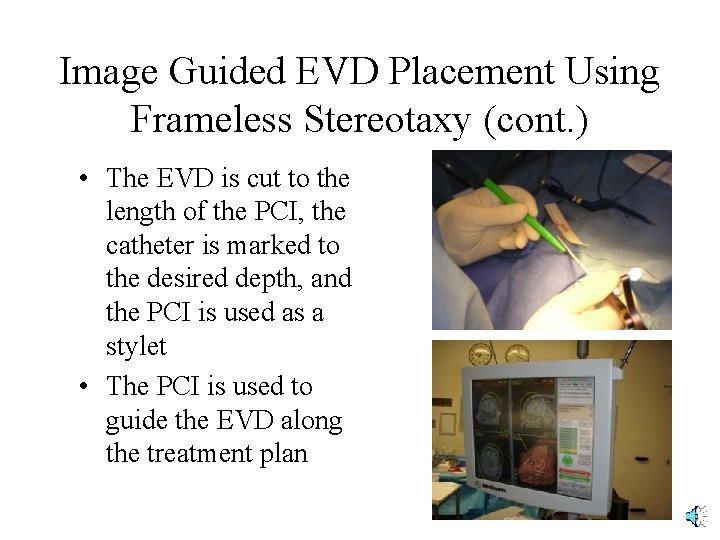
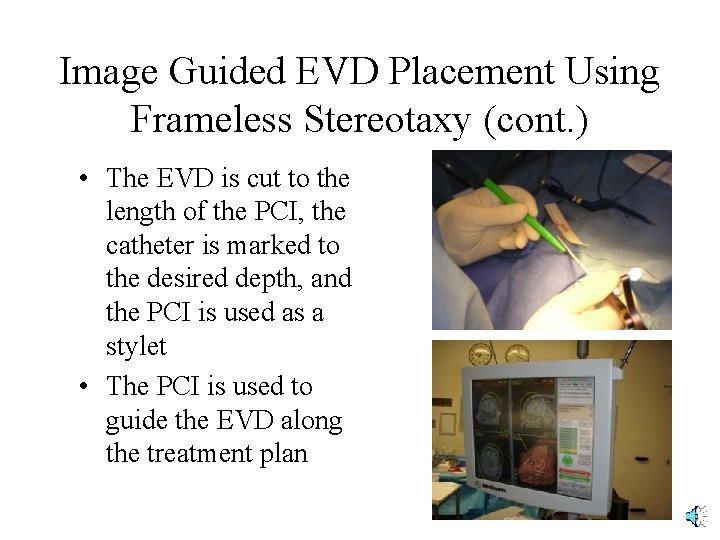
Image Guided EVD Placement Using Frameless Stereotaxy (cont. ) • The EVD is cut to the length of the PCI, the catheter is marked to the desired depth, and the PCI is used as a stylet • The PCI is used to guide the EVD along the treatment plan
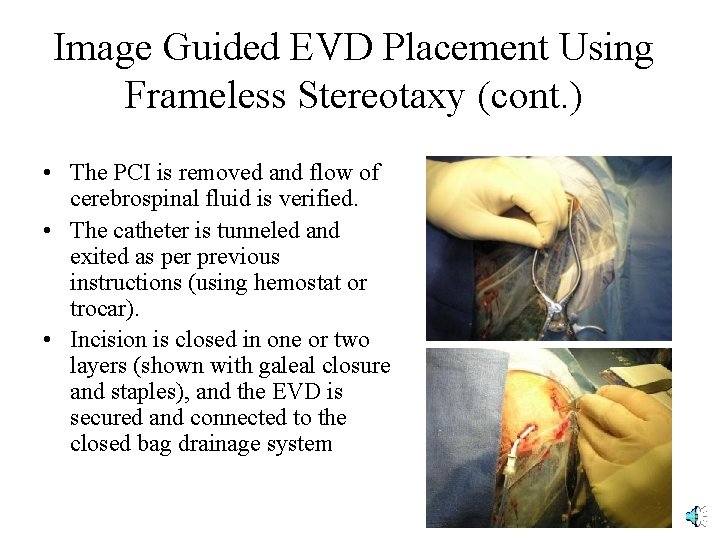
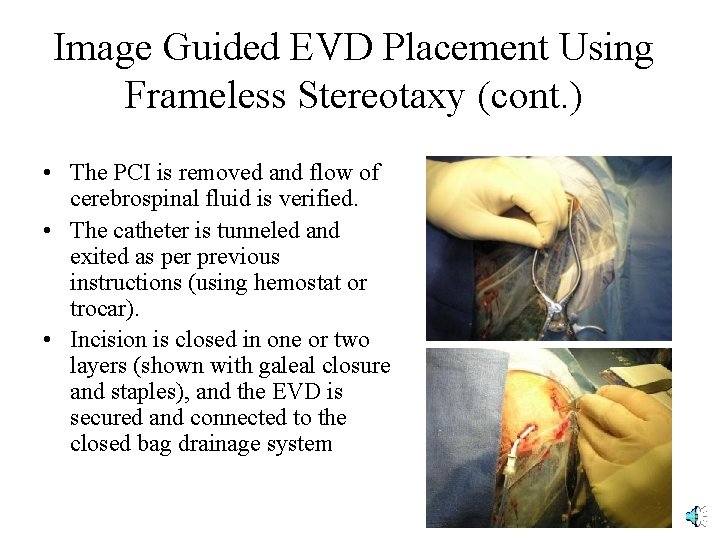
Image Guided EVD Placement Using Frameless Stereotaxy (cont. ) • The PCI is removed and flow of cerebrospinal fluid is verified. • The catheter is tunneled and exited as per previous instructions (using hemostat or trocar). • Incision is closed in one or two layers (shown with galeal closure and staples), and the EVD is secured and connected to the closed bag drainage system
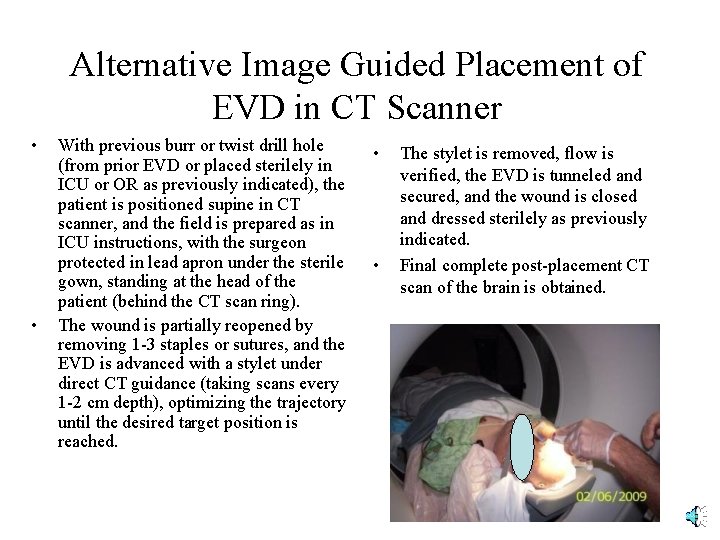
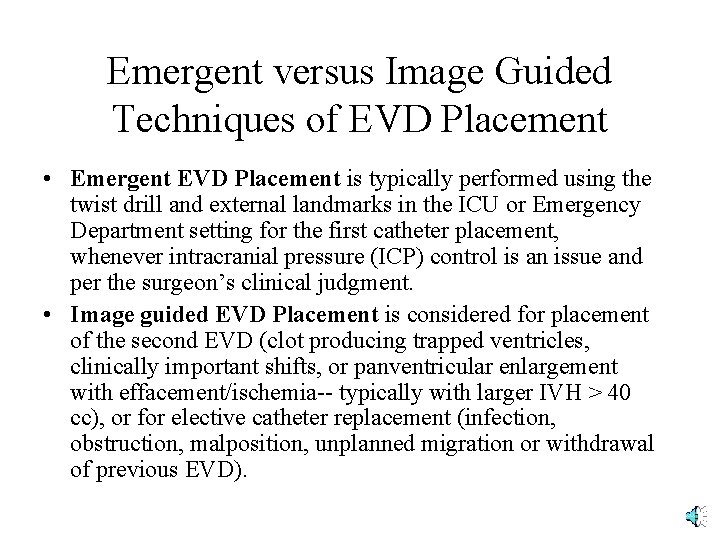
Alternative Image Guided Placement of EVD in CT Scanner • • With previous burr or twist drill hole (from prior EVD or placed sterilely in ICU or OR as previously indicated), the patient is positioned supine in CT scanner, and the field is prepared as in ICU instructions, with the surgeon protected in lead apron under the sterile gown, standing at the head of the patient (behind the CT scan ring). The wound is partially reopened by removing 1 -3 staples or sutures, and the EVD is advanced with a stylet under direct CT guidance (taking scans every 1 -2 cm depth), optimizing the trajectory until the desired target position is reached. • • The stylet is removed, flow is verified, the EVD is tunneled and secured, and the wound is closed and dressed sterilely as previously indicated. Final complete post-placement CT scan of the brain is obtained.