Skin integrity and Wound care Spring Semester 2016


- Slides: 48
Skin integrity and Wound care Spring Semester 2016 1
Skin integrity • Intact skin: presence of normal skin layers uninterrupted by wounds. • Impaired skin integrity is a threat to: - Elders Client with restricted mobility Chronic illness Trauma Those undergoing invasive health care procedure 2
Skin integrity • The skin is the body’s largest organ and the primary defense against pathogenic invasion. • The skin also contributes to temperature regulation, prevents loss of internal fluids, and provides sensory awareness. • The appearance of skin and skin integrity are influenced by: - Internal factors( genetics, age and status of person’s health, malnutrition) - External ( activity, sun and medications as AB and chemotherapy, corticosteroids) 3
Types of wound • Intentional: trauma occurs during therapy as operation, vein puncture and tumor excision • Unintentional: are accidental as fracture from car accident and § Closed: tissue trauma without a break in the skin § Open: when the skin or mucous membrane surface is broken 4
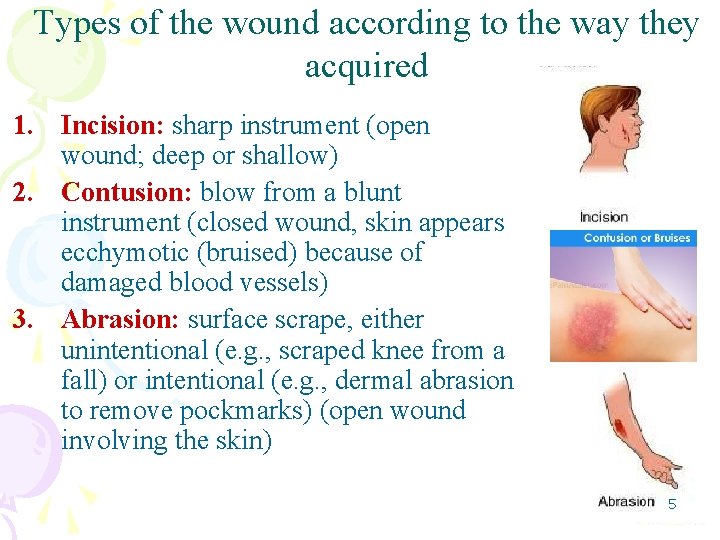
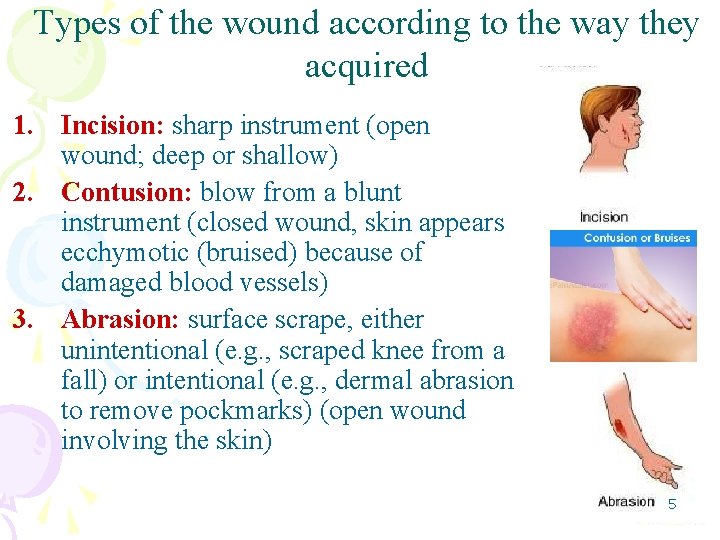
Types of the wound according to the way they acquired 1. Incision: sharp instrument (open wound; deep or shallow) 2. Contusion: blow from a blunt instrument (closed wound, skin appears ecchymotic (bruised) because of damaged blood vessels) 3. Abrasion: surface scrape, either unintentional (e. g. , scraped knee from a fall) or intentional (e. g. , dermal abrasion to remove pockmarks) (open wound involving the skin) 5
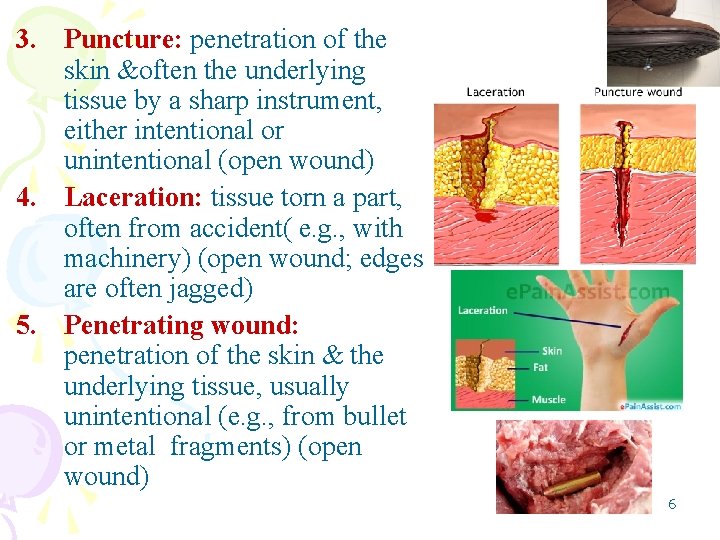
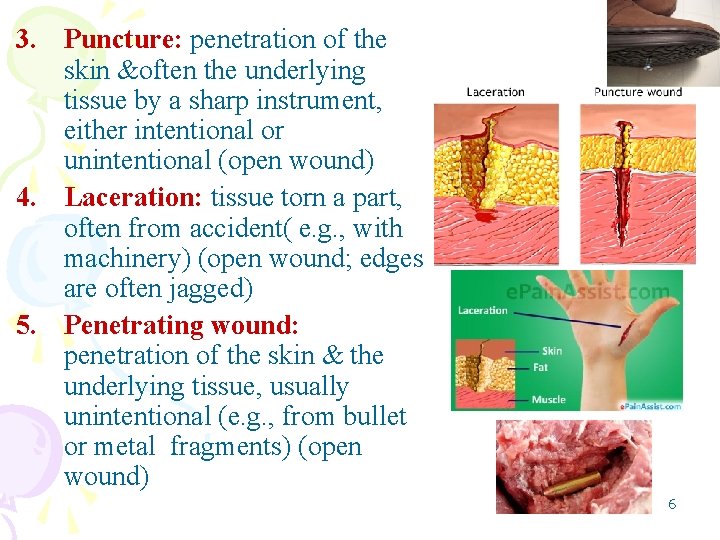
3. Puncture: penetration of the skin &often the underlying tissue by a sharp instrument, either intentional or unintentional (open wound) 4. Laceration: tissue torn a part, often from accident( e. g. , with machinery) (open wound; edges are often jagged) 5. Penetrating wound: penetration of the skin & the underlying tissue, usually unintentional (e. g. , from bullet or metal fragments) (open wound) 6
Wound description according to degree of contamination Clean wound: are uninfected wound in which minimal inflammation is encountered and the respiratory, genital, urinary tract are not entered. Clean wound are primarily closed wound Clean-contaminated wounds: are surgical wounds in which respiratory, alimentary, genital or urinary tract has been entered, such wounds show no evidence of infection (high risk of infection) Contaminated wounds: include open, fresh, accidental wounds & surgical wounds involving a major break in sterile technique there is an evidence of inflammation Dirty or infected wounds: wounds containing dead tissue & wounds with evidence of a clinical infection, such as purulent drainage (old, accidental wounds) 7
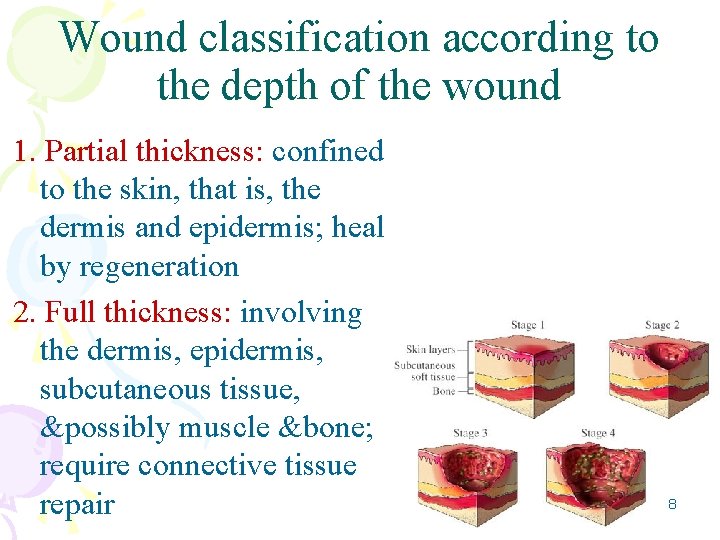
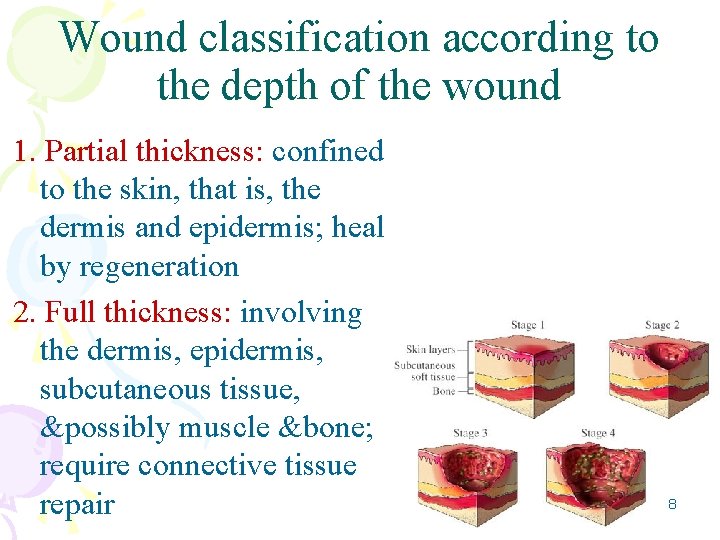
Wound classification according to the depth of the wound 1. Partial thickness: confined to the skin, that is, the dermis and epidermis; heal by regeneration 2. Full thickness: involving the dermis, epidermis, subcutaneous tissue, &possibly muscle &bone; require connective tissue repair 8
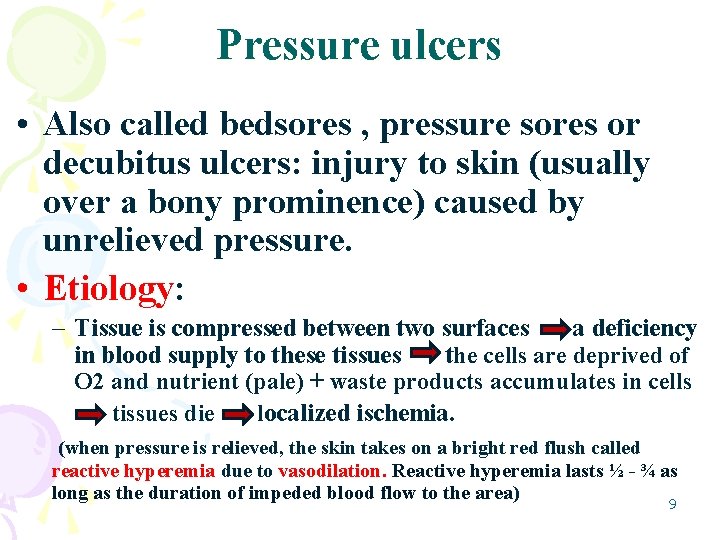
Pressure ulcers • Also called bedsores , pressure sores or decubitus ulcers: injury to skin (usually over a bony prominence) caused by unrelieved pressure. • Etiology: – Tissue is compressed between two surfaces a deficiency in blood supply to these tissues the cells are deprived of O 2 and nutrient (pale) + waste products accumulates in cells tissues die localized ischemia. (when pressure is relieved, the skin takes on a bright red flush called reactive hyperemia due to vasodilation. Reactive hyperemia lasts ½ - ¾ as long as the duration of impeded blood flow to the area) 9
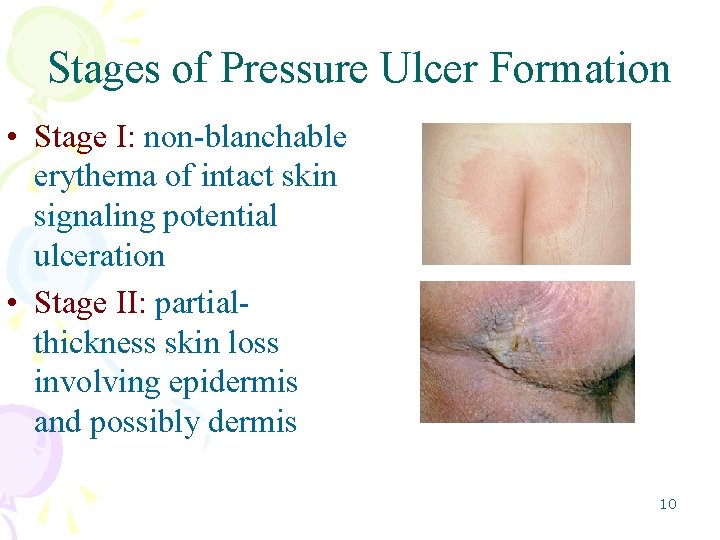
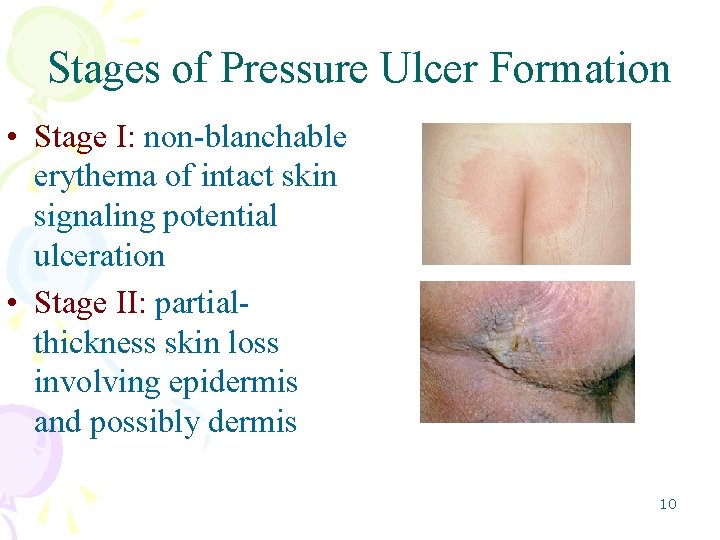
Stages of Pressure Ulcer Formation • Stage I: non-blanchable erythema of intact skin signaling potential ulceration • Stage II: partialthickness skin loss involving epidermis and possibly dermis 10
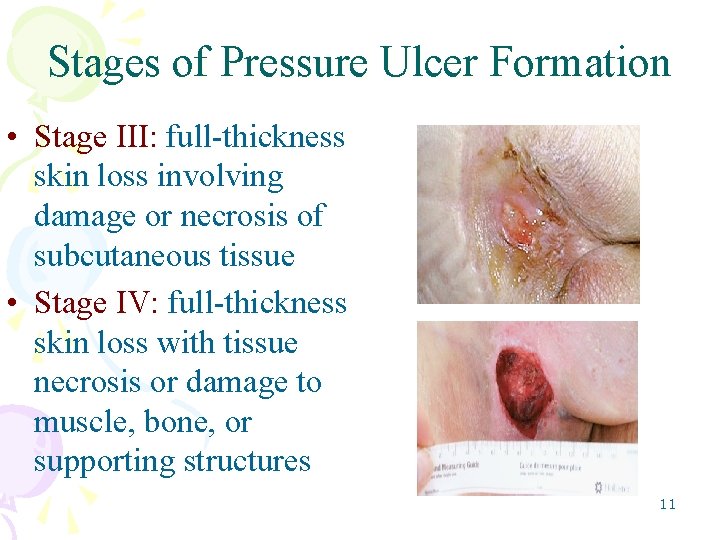
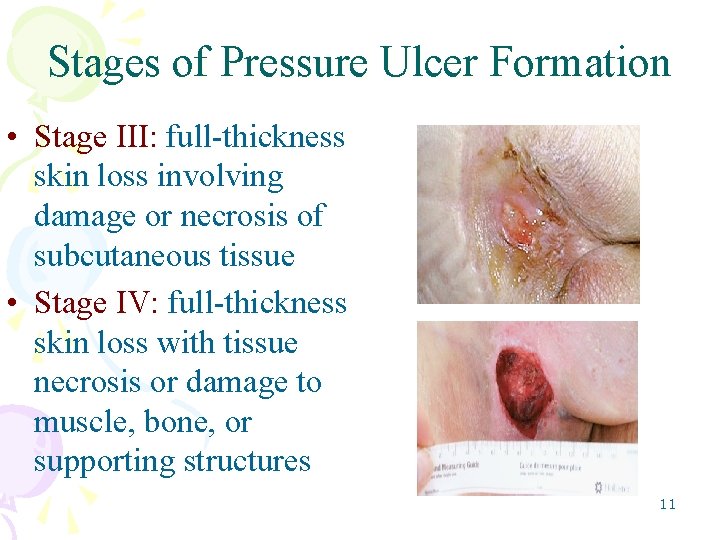
Stages of Pressure Ulcer Formation • Stage III: full-thickness skin loss involving damage or necrosis of subcutaneous tissue • Stage IV: full-thickness skin loss with tissue necrosis or damage to muscle, bone, or supporting structures 11
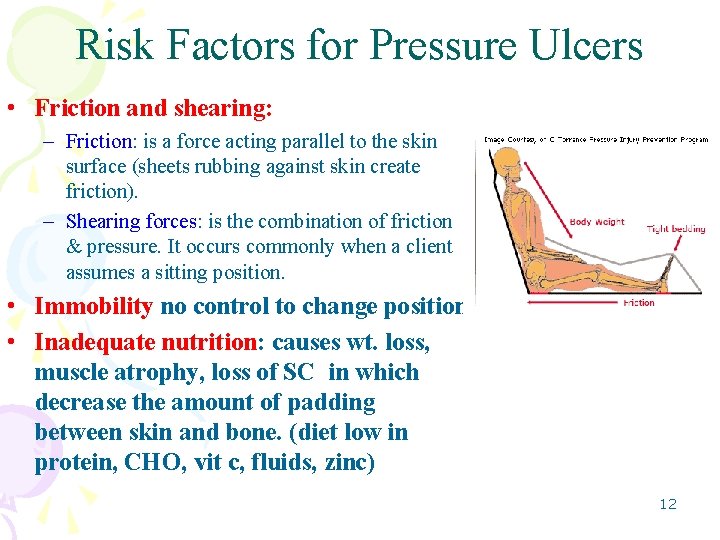
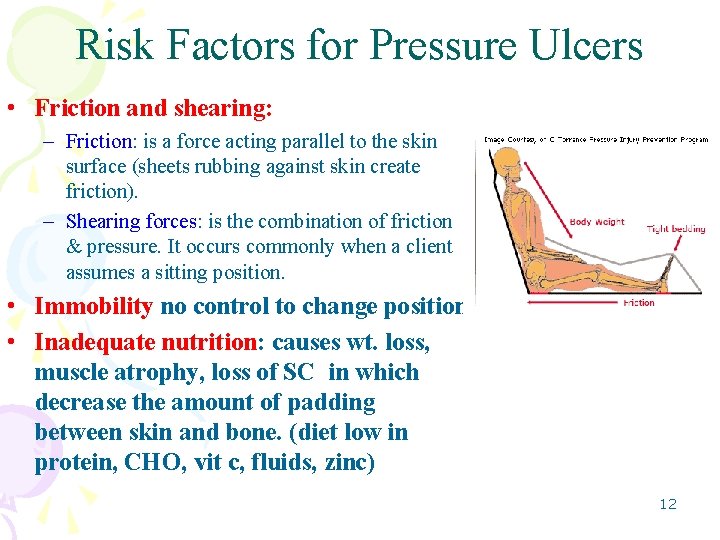
Risk Factors for Pressure Ulcers • Friction and shearing: – Friction: is a force acting parallel to the skin surface (sheets rubbing against skin create friction). – Shearing forces: is the combination of friction & pressure. It occurs commonly when a client assumes a sitting position. • Immobility no control to change position • Inadequate nutrition: causes wt. loss, muscle atrophy, loss of SC in which decrease the amount of padding between skin and bone. (diet low in protein, CHO, vit c, fluids, zinc) 12
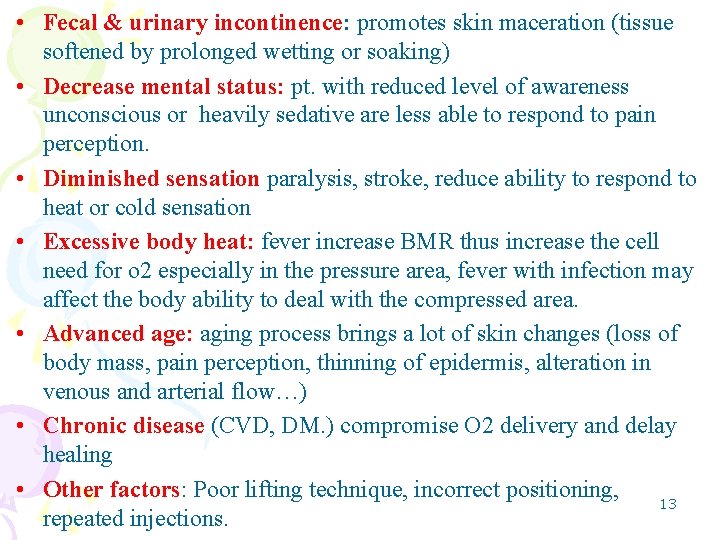
• Fecal & urinary incontinence: promotes skin maceration (tissue softened by prolonged wetting or soaking) • Decrease mental status: pt. with reduced level of awareness unconscious or heavily sedative are less able to respond to pain perception. • Diminished sensation paralysis, stroke, reduce ability to respond to heat or cold sensation • Excessive body heat: fever increase BMR thus increase the cell need for o 2 especially in the pressure area, fever with infection may affect the body ability to deal with the compressed area. • Advanced age: aging process brings a lot of skin changes (loss of body mass, pain perception, thinning of epidermis, alteration in venous and arterial flow…) • Chronic disease (CVD, DM. ) compromise O 2 delivery and delay healing • Other factors: Poor lifting technique, incorrect positioning, 13 repeated injections.
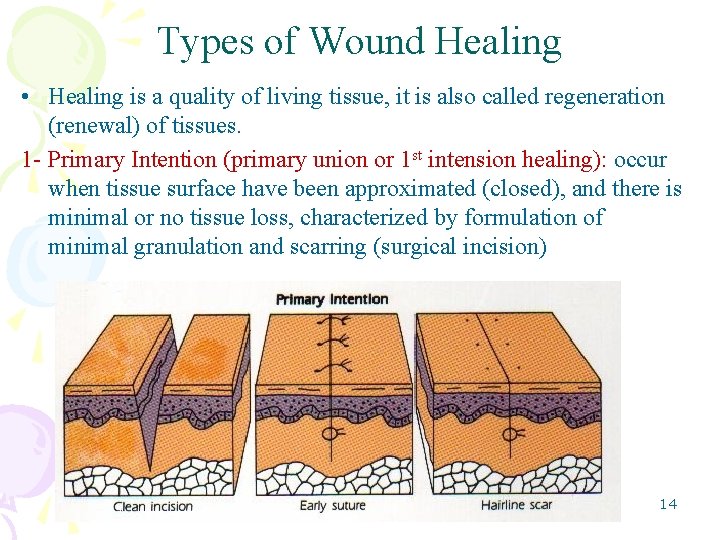
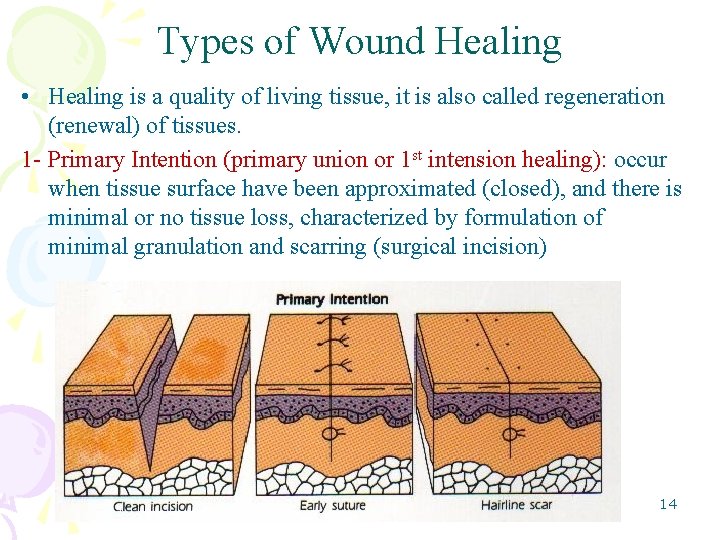
Types of Wound Healing • Healing is a quality of living tissue, it is also called regeneration (renewal) of tissues. 1 - Primary Intention (primary union or 1 st intension healing): occur when tissue surface have been approximated (closed), and there is minimal or no tissue loss, characterized by formulation of minimal granulation and scarring (surgical incision) 14
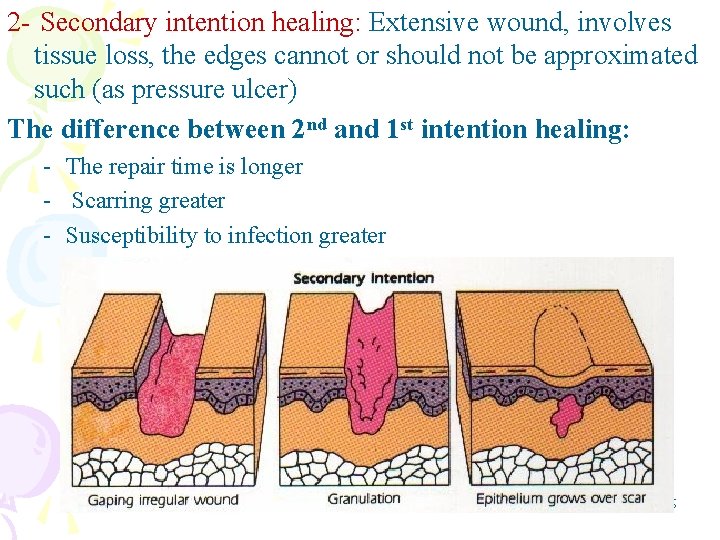
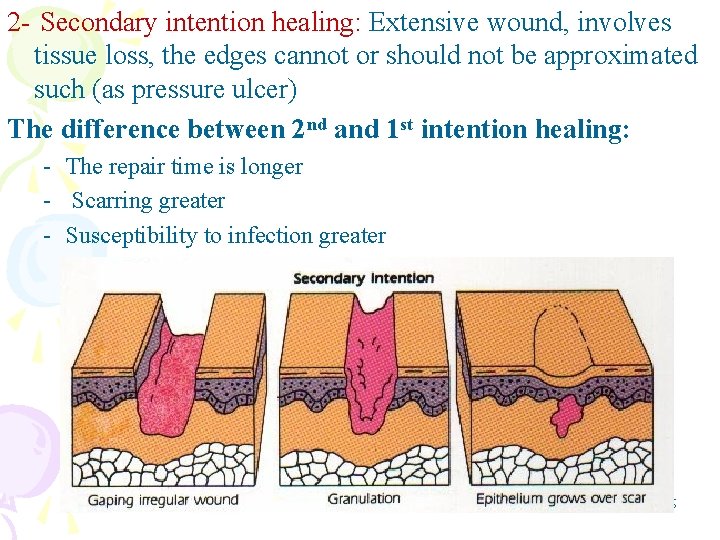
2 - Secondary intention healing: Extensive wound, involves tissue loss, the edges cannot or should not be approximated such (as pressure ulcer) The difference between 2 nd and 1 st intention healing: - The repair time is longer - Scarring greater - Susceptibility to infection greater 15
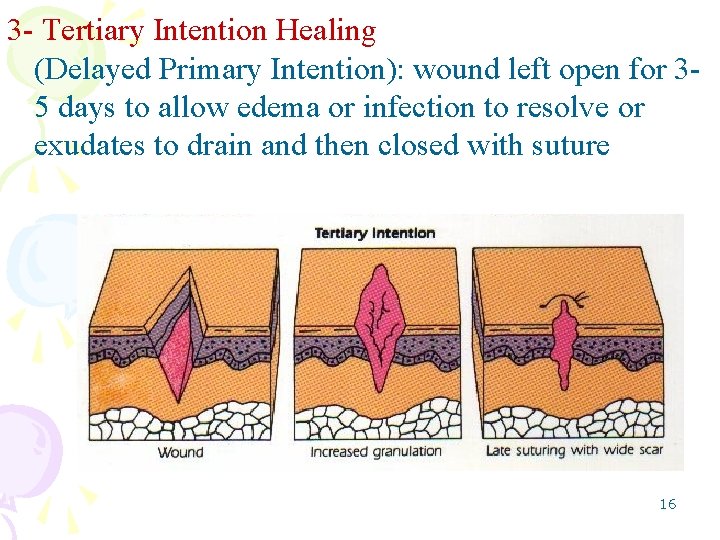
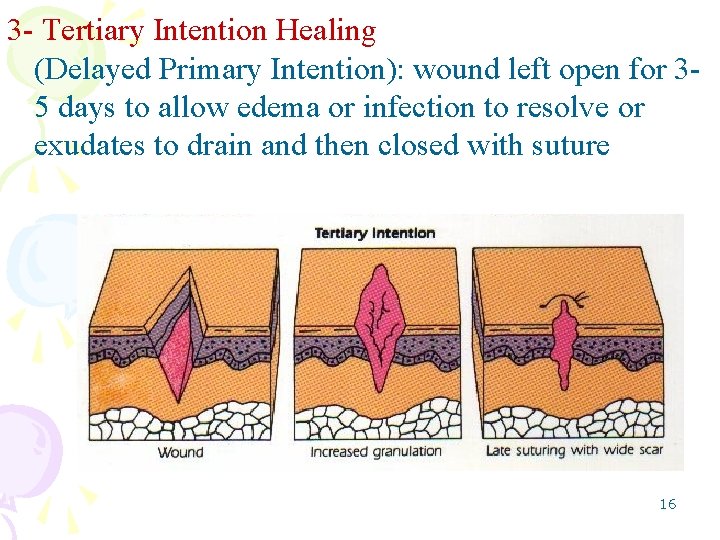
3 - Tertiary Intention Healing (Delayed Primary Intention): wound left open for 35 days to allow edema or infection to resolve or exudates to drain and then closed with suture 16
Phases of Wound Healing • It is the same for all wound but the rate of healing depend on: - Type of healing - Location and size of wound - Client health status Phases of wound healing: • Inflammatory Phase • Proliferative Phase • Maturation Phase 17
Inflammatory Phase • Immediately after injury; lasts 3 to 6 days. Two processes occur during this phase: • Hemostasis (cessation of bleeding): results from vasoconstriction of larger vessels in affected area, retraction of injured blood vessels, the deposition of fibrin (connective tissue) and the formation of blood clots which provide a matrix of fibrin that becomes the framework for cell repair. • Phagocytosis: arise from bld monocytes to engulf microorganisms 18
Proliferative Phase • From post injury day 3 or 4 until day 21 q. Fibroblasts in wound start to synthesize collagen (a whitish protein substance adds strength to wound q. Capillaries grow across wound increasing Bld supply and fibrin deposits in wound. q. The capillary network develops tissue becomes red color called granulation tissue. q. Epithelization: proliferation of epithelial tissue over the granulation, if failed dried plasma proteins and dead cells formed eschar. 19
Maturation Phase • • From day 21 until 1 or 2 years post injury Fibroblasts continue to produce collagen Remodeling of the wound occur Scar formation occur which is strong 20
Types of wound exudates • Exudates: is a fluid that are escaped from blood during inflammatory process and deposited in the tissue or in the tissue surface. 3 types: A- Serous Exudates: consist of serum (clear protein of blood) derived from blood & serous membrane of body (watery& has few cells)(e. g. fluid in the blister from burn) B- Purulent exudates: is thicker, presence of pus (leukocytes, dead tissue debris & dead living bacteria) blue, green, or yellow color depend on causative agents C- Sanguineous (hemorrhagic) exudates: large amount of RBC indicate damage to capillaries (in open wounds, may be bright (fresh bleeding) or dark (old bleeding) 21
Mixed Exudate • Serosanguineous – Clear and blood-tinged drainage, commonly seen in surgical incision • Purosanguineous – Pus and blood, commonly seen in new wound that is infected 22
Complications of Wound Healing v. Hemorrhage: due to removal of clot, slipped stitch, erosion of blood vessel, risks increase in the 1 st 48 hr’s after surgery - Internal (swelling and distension under skin, may called hematoma, if it large may cause compression in the blood vessels) - External (blood appear under dressing or escape. So apply sterile pressure dressing + check V/S) v. Infection: impaired skin healing, become apparent 2 -11 day post operative, cause change in wound color, pain, exudates, fever, increase WBC’s, hotness, tenderness 23 and redness, foul odor.

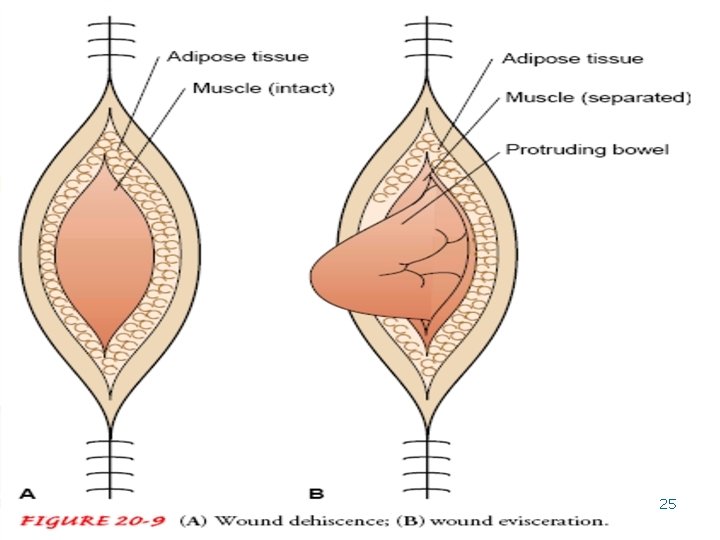
v. Dehiscence: Partial or total rupturing of sutured wound, occur 4 -5 day post op, it is due to obesity, poor nutrition, multiple trauma, excessive coughing and sneezing, sudden straining and dehydration, it is managed by (large sterile dressing soaked in N|S, place pt in bed with knee bent, then notify doctor v. Evisceration: Protrusion of the intestines through the incision. 24
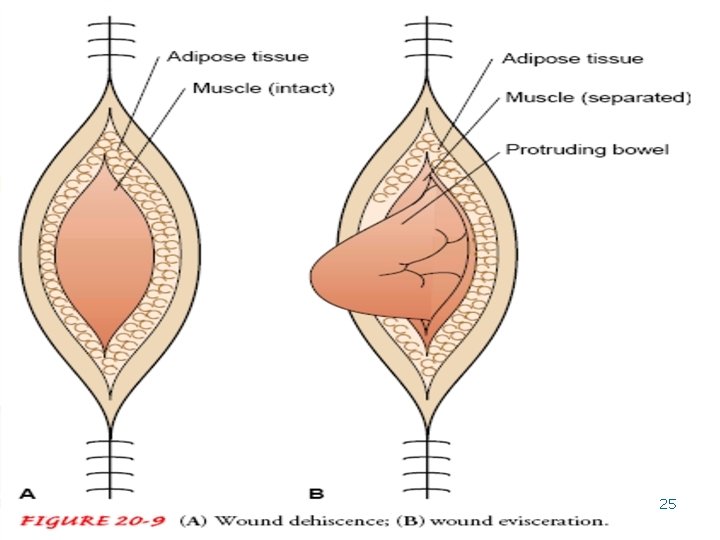
25
Factors Affecting Wound Healing • • Age: young, adult, or elderly Nutritional status: diet, obesity Lifestyle: exercise, smoking, poor hygiene Medications: anti-inflammatory drugs (steroids, aspirin) AB interfere with MO resistance. • Contamination or infection 26
Nursing Process: Assessment • Nursing history – Review of systems – Skin diseases – Previous bruising – General skin condition – Skin lesions – Usual healing of sores 27
• Inspection and palpation – – – Skin color distribution Skin turgor Presence of edema Characteristics of any skin lesions Particular attention paid to areas that are most likely to break down • Untreated wounds – – – – Location Extent of tissue damage Wound length, width, and depth Bleeding Foreign bodies Associated injuries Last tetanus toxoid injection 28
• Treated wounds – – – Appearance Size Drainage Presence of swelling Pain Status of drains or tubes • Pressure Ulcers - Location of the ulcer related to a bony prominence - Size of ulcer in centimeters including length (head to toe), width (side to side), and depth - Presence of undermining or sinus tracts - Stage of the ulcer - Color of the wound bed - Location of necrosis or Eschar - Condition of the wound margins - Integrity of surrounding skin 29 - Clinical signs of infection
Laboratory Data: q Leukocyte count: decrease LEUKOCYTE COUNT delay healing increase risk for infection. • Hemoglobin level: Low Hgb poor O 2 delivery to tissue q Blood coagulation: prolonged coagulation times result in severe bleeding, while hypercoagulability lead to intravascular clotting while intra-arterial clotting decrease bld supply to wound q Serum protein indicates nutritional status serum albumin indicate nutritional status less than 3. 5 g/dl increase risk for infection, and delay healing q Wound culture : rule out presences of infection q Sensitivity tests: to select the proper AB 30
Nursing Diagnoses – Risk for Impaired Skin Integrity – Impaired Skin Integrity: – Impaired Tissue Integrity – Risk for Infection – Pain 31
Goals in Planning Client Care • Risk for Impaired Skin Integrity – Maintain skin integrity – Avoid or reduce risk factors • Impaired Skin Integrity – Progressive wound healing – Regain intact skin • Client and family education – Assess and treat existing wound – Prevention of pressure ulcers 32
Implementation • Supporting wound healing : maintain moist wound healing, nutrition and fluid, preventing infection and positioning • Preventing pressure ulcer • Treating pressure ulcer : RYB ( Red, Yellow, Black) • Dressing wound • Cleaning wound • Supporting and immobilizing wound • Heat and cold application 33
Dressing wound • - Purposes: To protect the wound from mechanical injury To protect the wound from infection To maintain moist wound healing To absorb drainage To prevent hemorrhage To splint or immobilize the wound 34
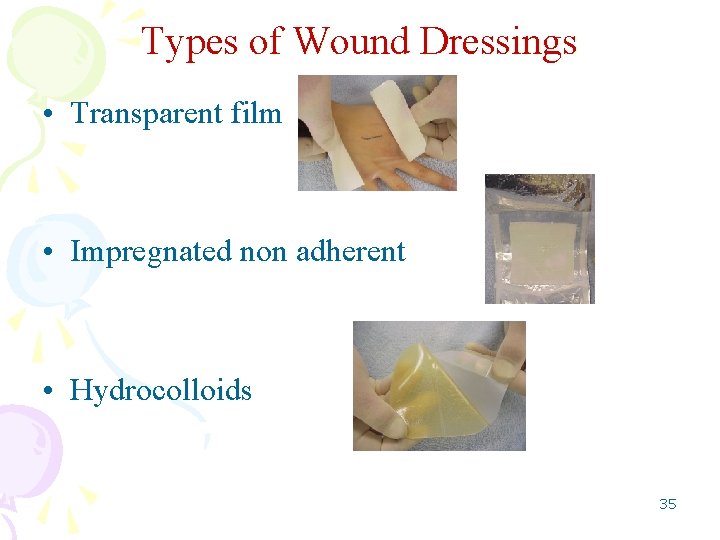
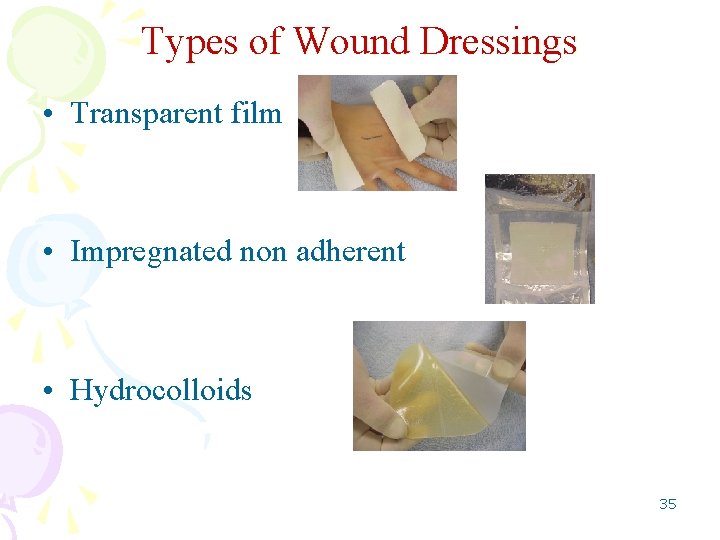
Types of Wound Dressings • Transparent film • Impregnated non adherent • Hydrocolloids 35
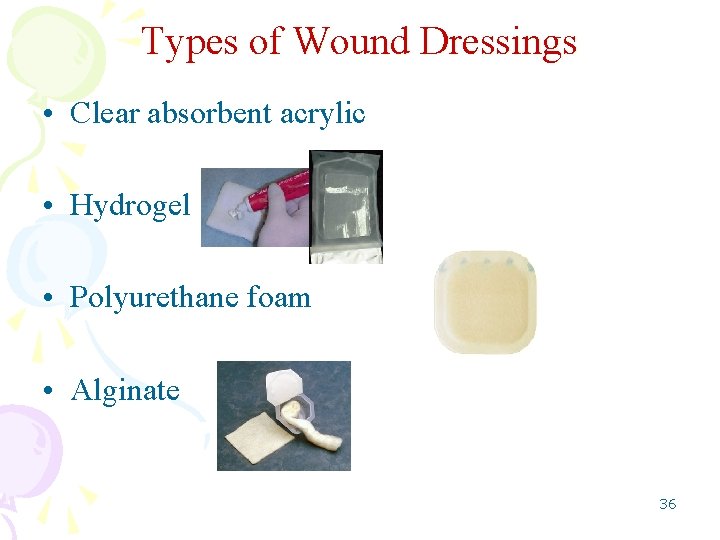
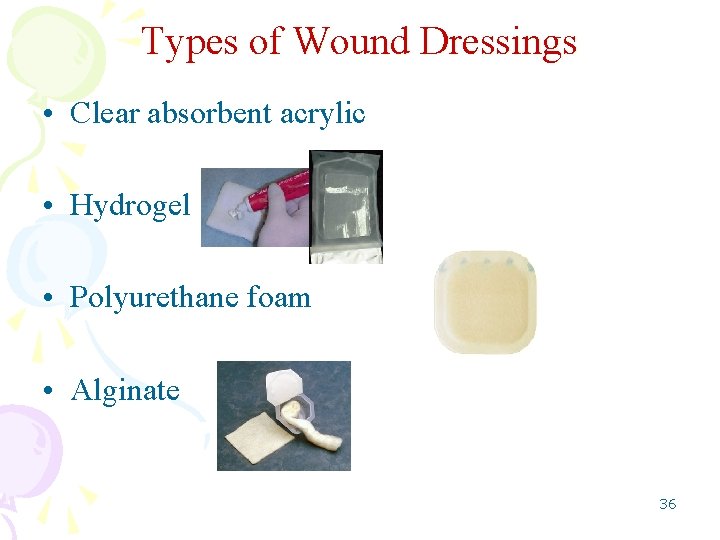
Types of Wound Dressings • Clear absorbent acrylic • Hydrogel • Polyurethane foam • Alginate 36
Types of Bandages • Gauze – Restrain dressings on wounds – Bandage hands and feet • Elasticized – Provide pressure to an area – Improve venous circulation in legs • Binders – Support large areas of body • Triangular arm sling; straight abdominal binder 37
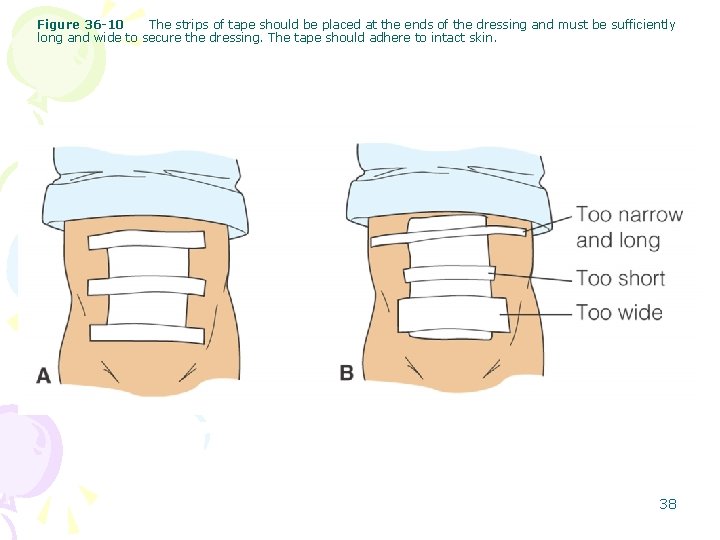
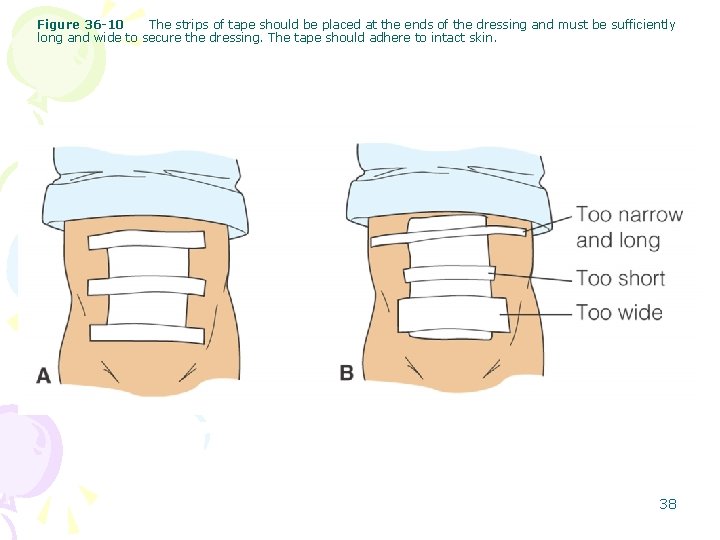
Figure 36 -10 The strips of tape should be placed at the ends of the dressing and must be sufficiently long and wide to secure the dressing. The tape should adhere to intact skin. 38
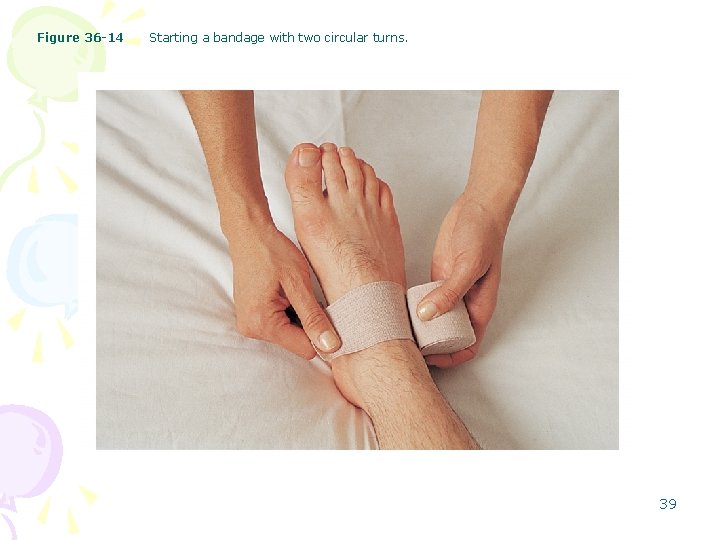
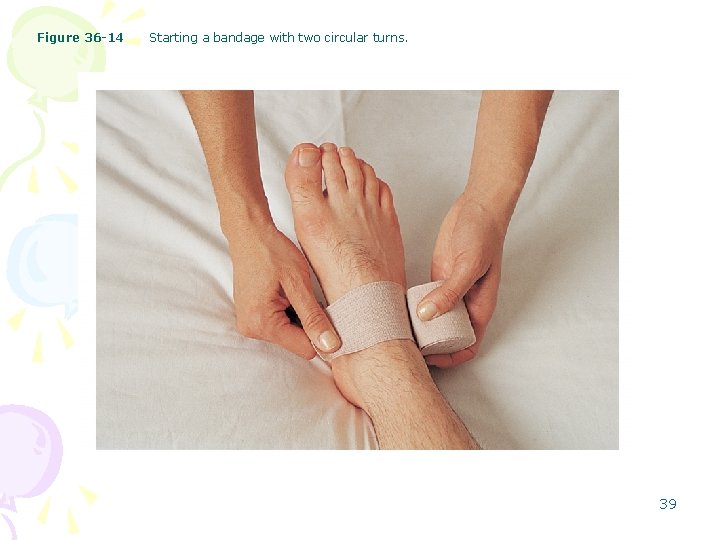
Figure 36 -14 Starting a bandage with two circular turns. 39

Figure 36 -15 Applying spiral turns. 40
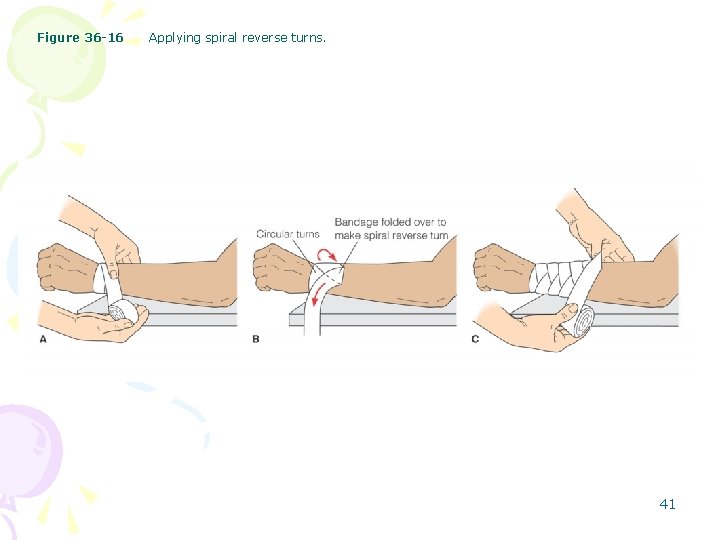
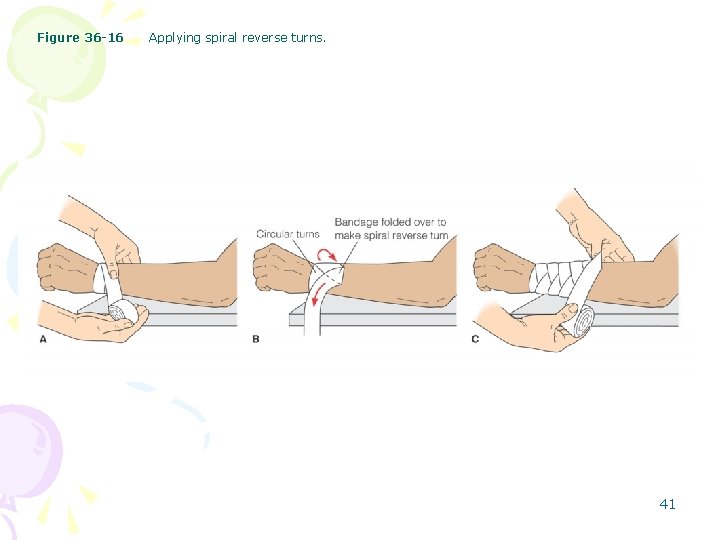
Figure 36 -16 Applying spiral reverse turns. 41
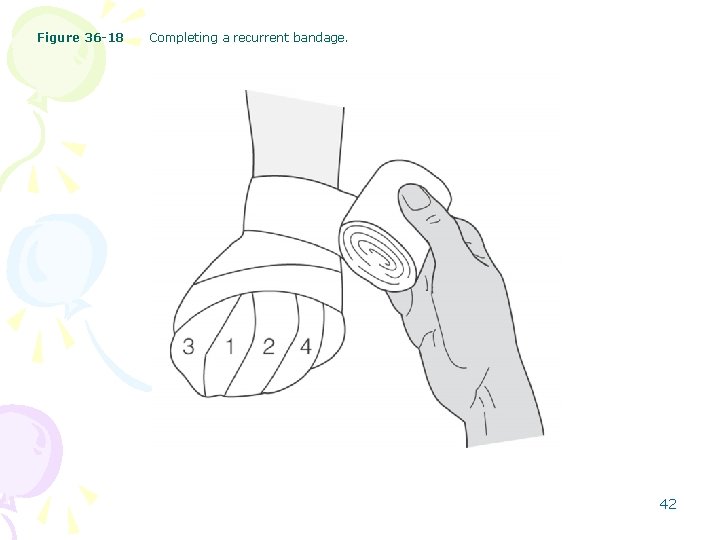
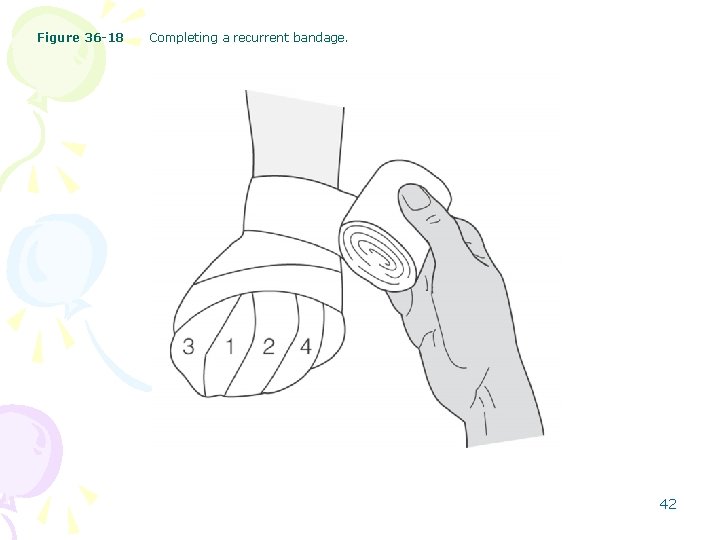
Figure 36 -18 Completing a recurrent bandage. 42
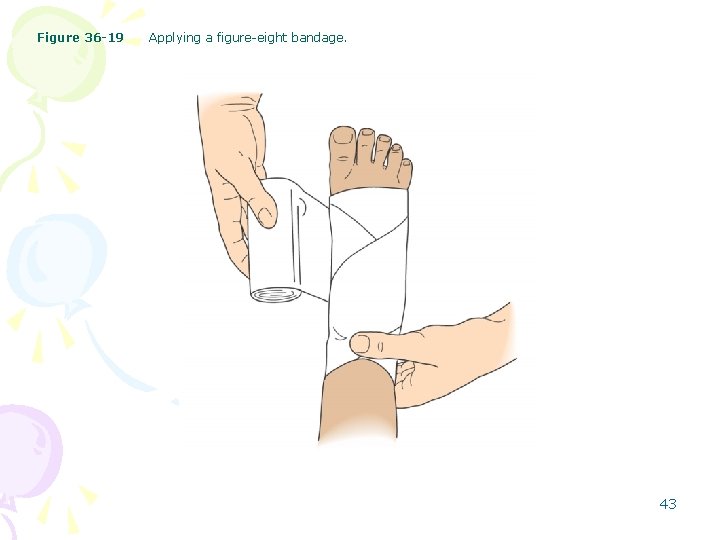
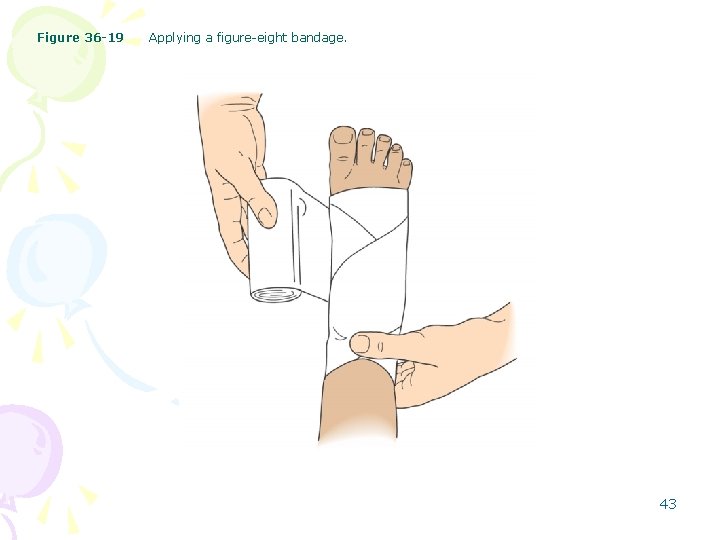
Figure 36 -19 Applying a figure-eight bandage. 43
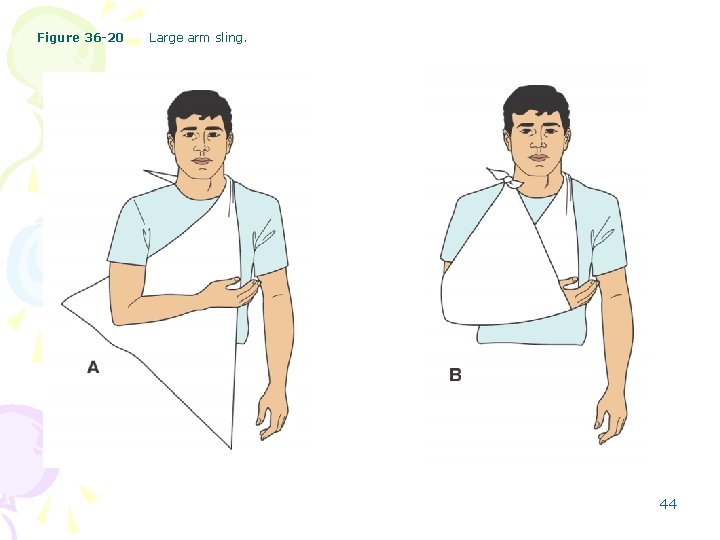
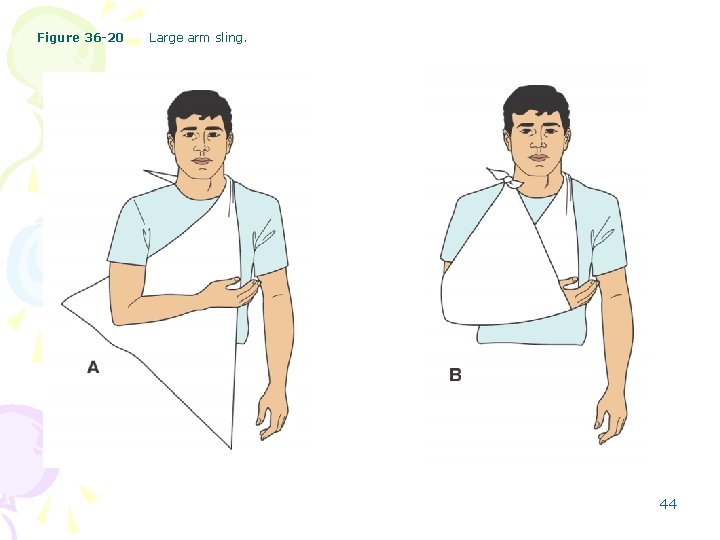
Figure 36 -20 Large arm sling. 44
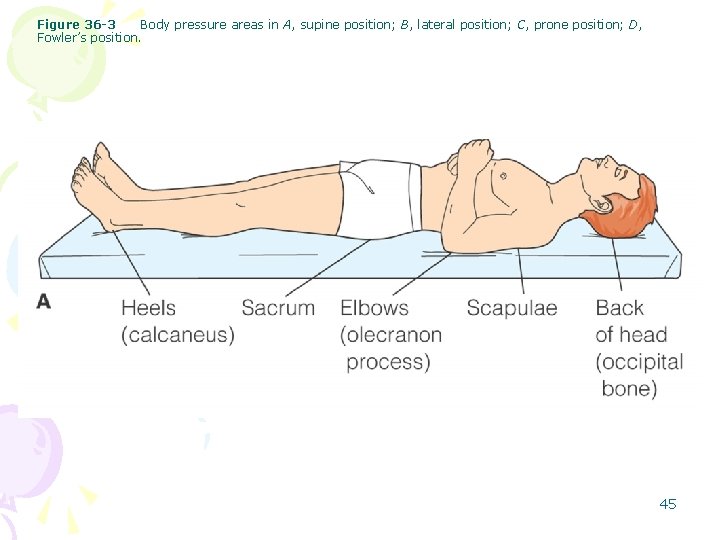
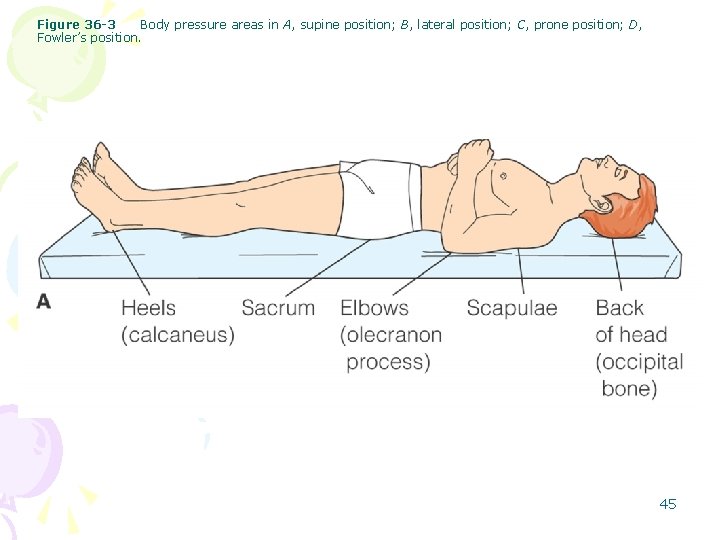
Figure 36 -3 Body pressure areas in A, supine position; B, lateral position; C, prone position; D, Fowler’s position. 45
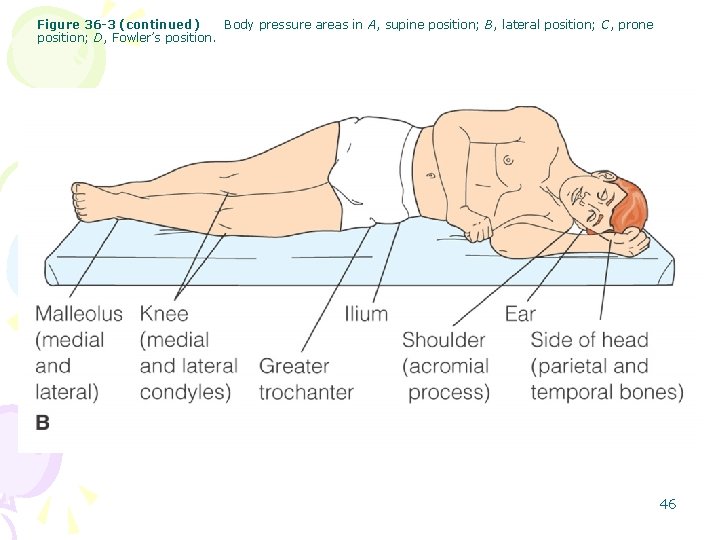
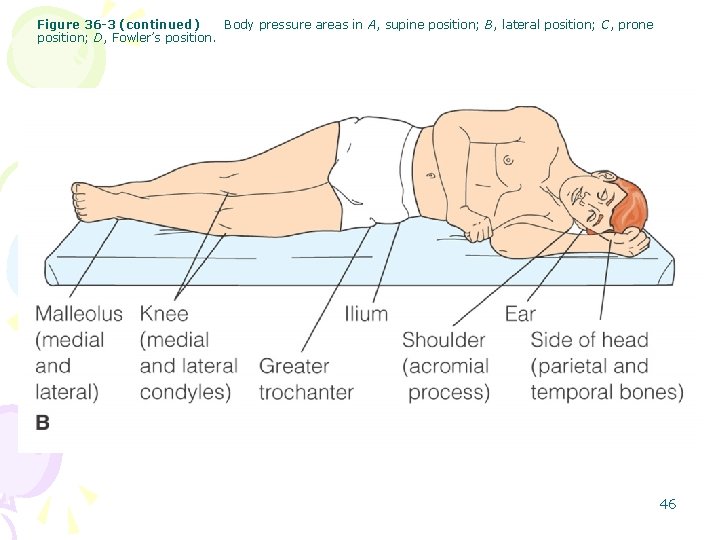
Figure 36 -3 (continued) Body pressure areas in A, supine position; B, lateral position; C, prone position; D, Fowler’s position. 46
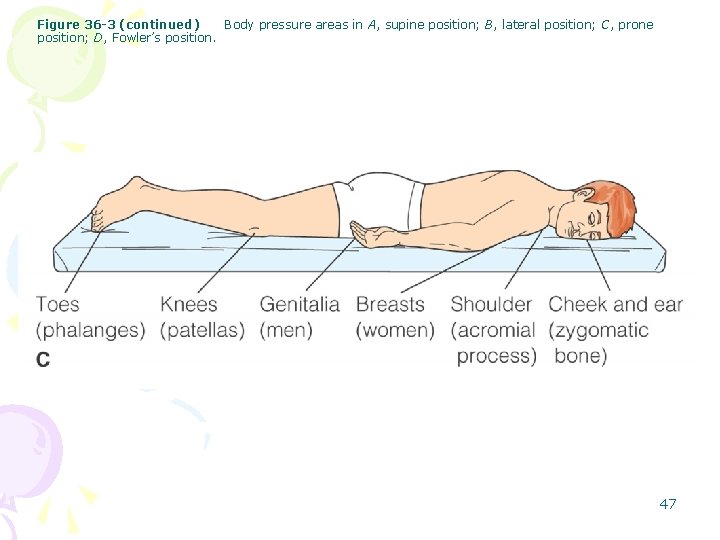
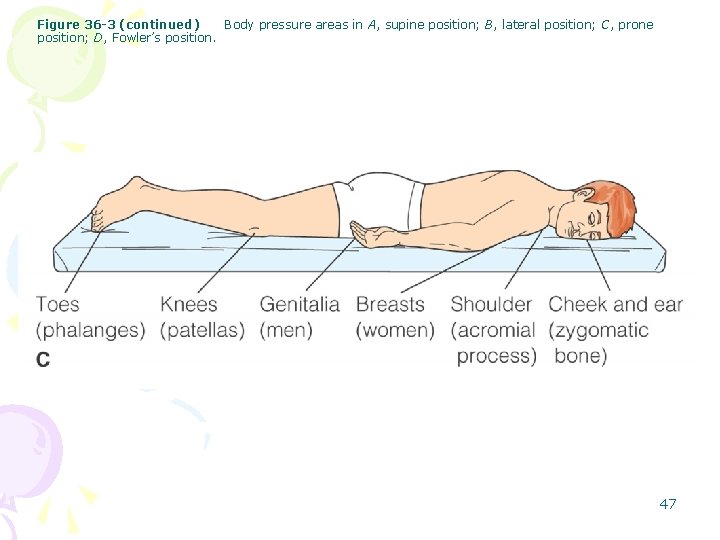
Figure 36 -3 (continued) Body pressure areas in A, supine position; B, lateral position; C, prone position; D, Fowler’s position. 47
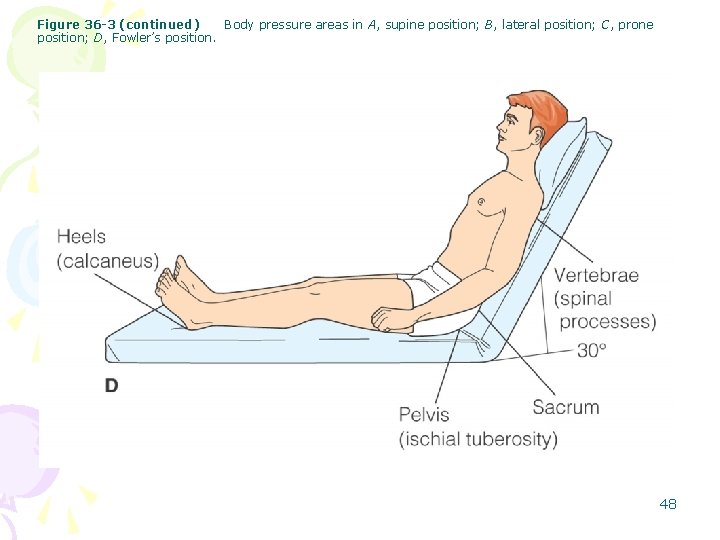
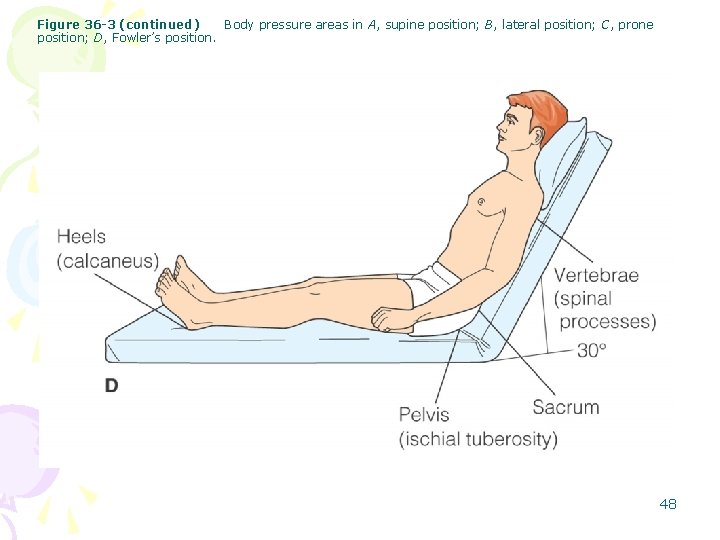
Figure 36 -3 (continued) Body pressure areas in A, supine position; B, lateral position; C, prone position; D, Fowler’s position. 48
 Chapter 32 skin integrity and wound care
Chapter 32 skin integrity and wound care Chapter 48 skin integrity and wound care
Chapter 48 skin integrity and wound care Chapter 48 skin integrity and wound care
Chapter 48 skin integrity and wound care Wolters kluwer
Wolters kluwer Skin wound
Skin wound Stratum lucidum
Stratum lucidum Skin integrity assessment
Skin integrity assessment Sskin bundle
Sskin bundle Anatomical location
Anatomical location Altered skin integrity
Altered skin integrity Spring, summer, fall, winter... and spring (2003)
Spring, summer, fall, winter... and spring (2003) Months in spring
Months in spring Thin skin vs thick skin
Thin skin vs thick skin Milady chapter 23 facial review questions
Milady chapter 23 facial review questions Ryb color code wound care
Ryb color code wound care Doylestown wound care center
Doylestown wound care center Shasta regional wound center
Shasta regional wound center Torrance memorial wound care center
Torrance memorial wound care center Wound care study days
Wound care study days Wound care pretest
Wound care pretest Wound care near freedom
Wound care near freedom Aqucel foam
Aqucel foam Primary secondary tertiary care
Primary secondary tertiary care Truescience skin care
Truescience skin care Basic skin care definition
Basic skin care definition Best skin care clinic in coimbatore
Best skin care clinic in coimbatore Royal skin care
Royal skin care Milady chapter 23 review questions
Milady chapter 23 review questions Youth rejuvenator
Youth rejuvenator Chlitina
Chlitina Conclusion of skin care
Conclusion of skin care Furnucles
Furnucles North spring primary school student care
North spring primary school student care Wound healing definition
Wound healing definition Local and systemic factors affecting wound healing
Local and systemic factors affecting wound healing Tidy and untidy wound
Tidy and untidy wound A wind up toy is fully wound and at rest
A wind up toy is fully wound and at rest Concealed puncture wound
Concealed puncture wound Health and social care unit 2
Health and social care unit 2 Type of wound
Type of wound Wound tracking software
Wound tracking software Wound infection continuum
Wound infection continuum Incised wound
Incised wound Screw driver wheel and axle
Screw driver wheel and axle Chapter 15 hunger games questions
Chapter 15 hunger games questions Jacob's ladder wound closure
Jacob's ladder wound closure Is a watch a simple machine
Is a watch a simple machine An inclined plane wound around a post
An inclined plane wound around a post Warna dasar luka
Warna dasar luka