Single Ventricle Physiology with Pulmonary Hypertension Decisions and








- Slides: 22
Single Ventricle Physiology with Pulmonary Hypertension: Decisions and Challenges Xinwei Du M. D. Shanghai Children’s Medical Center
Single Ventricle Physiology • With restrictive pulmonary blood flow • With neither restrictive pulmonary nor systemic blood flow • W/O restrictive pulmonary blood flow but with restrictive systemic blood flow
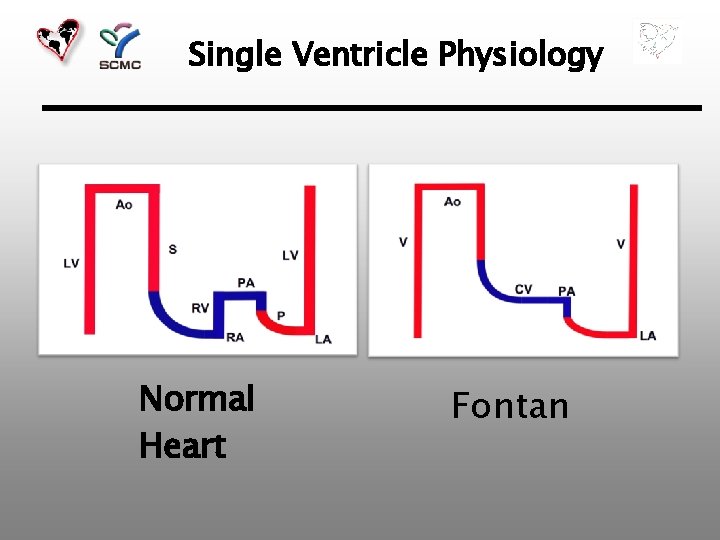
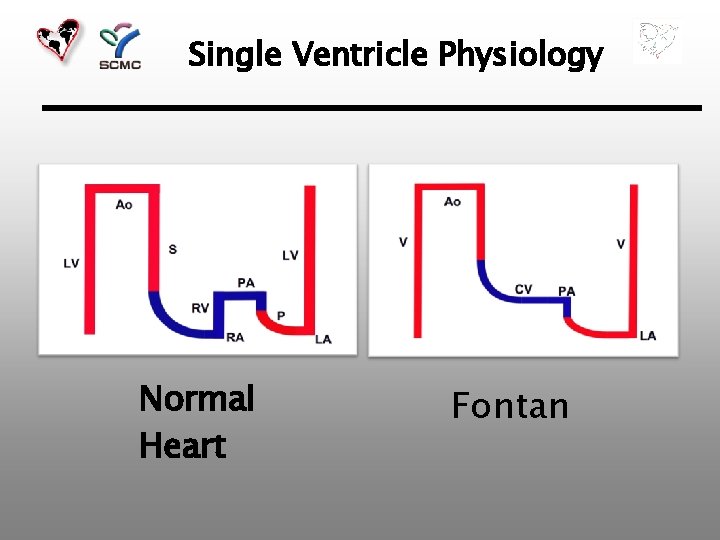
Single Ventricle Physiology Normal Heart Fontan
PVR • Success of Fontan operation depends on lower PVR • Even slight increases in PVR sig. reduce the transpulmonary blood flow → failing Fontan • Pulmonary arteries • Pulmonary vascular bed • Pulmonary venous return • Atrial septum
Surgical Techniques in Stage I Palliation • PA Banding • DKS or Norwood • Palliative Switch

PA Banding • Must have an obstructionfree SVOT anatomy R. A. Jonas
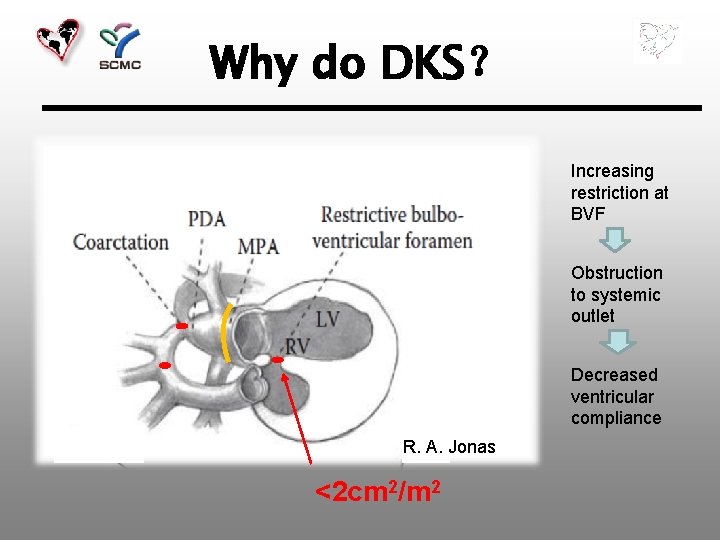
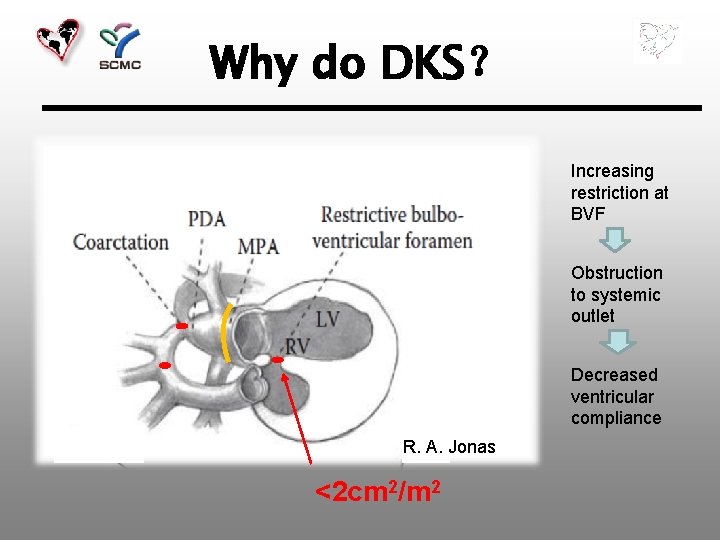
Why do DKS? Increasing restriction at BVF Obstruction to systemic outlet Decreased ventricular compliance R. A. Jonas <2 cm 2/m 2
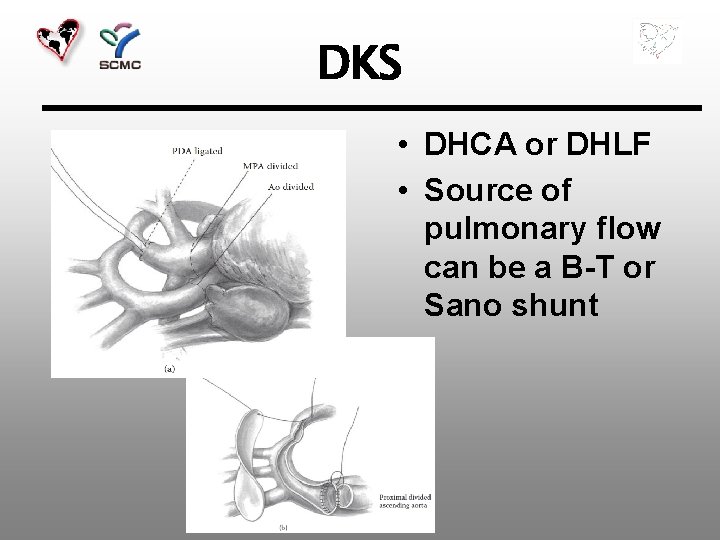
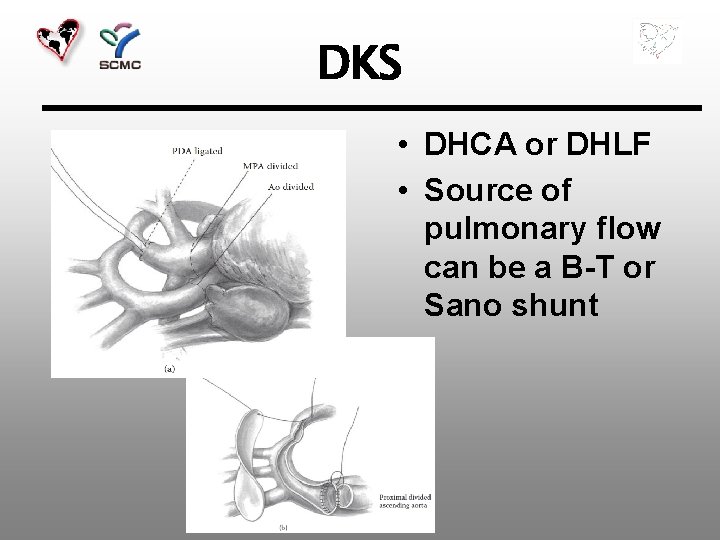
DKS • DHCA or DHLF • Source of pulmonary flow can be a B-T or Sano shunt

Lesions with Obstruction at BVF • DILV with discordant ventriculoarterial connection • TA with discordant ventriculoarterial connection • DORV with MA
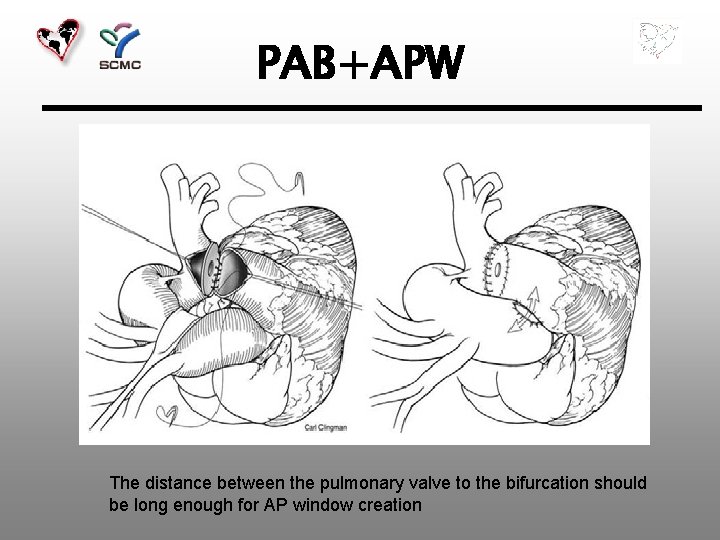
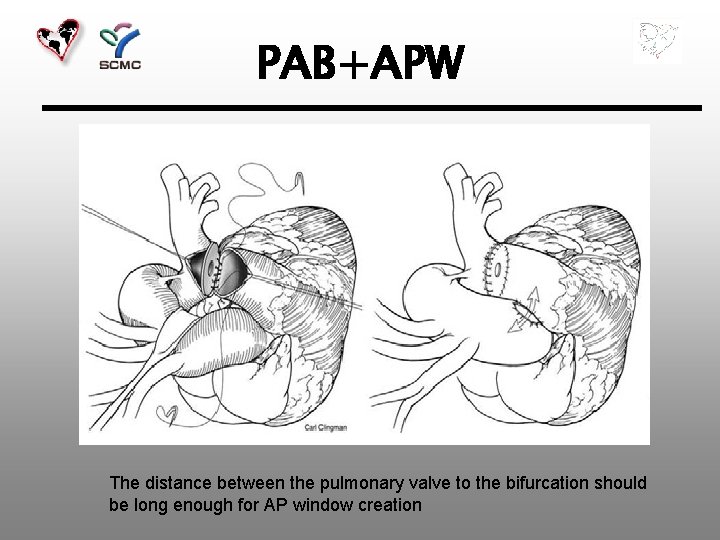
PAB+APW The distance between the pulmonary valve to the bifurcation should be long enough for AP window creation
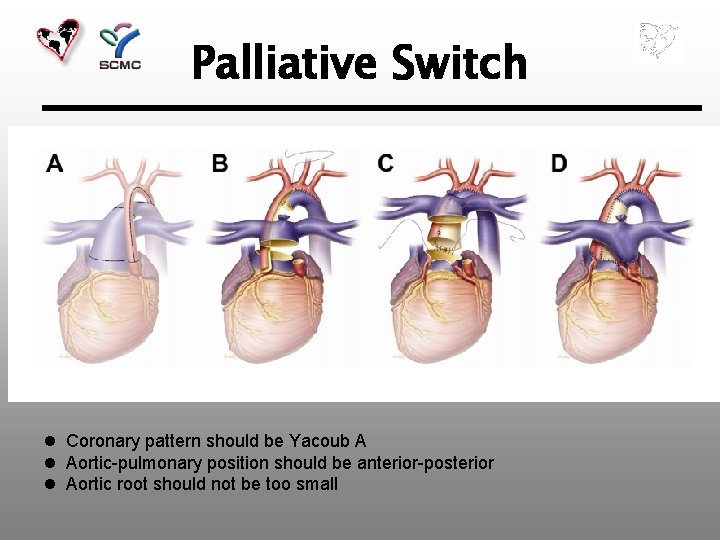
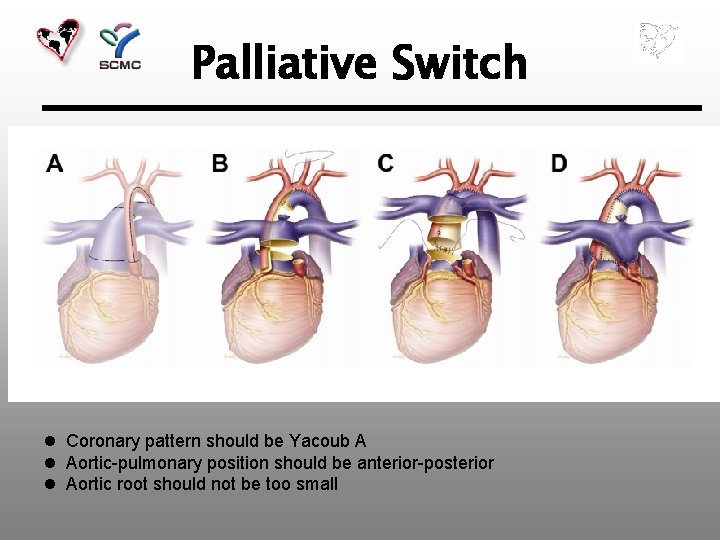
Palliative Switch l Coronary pattern should be Yacoub A l Aortic-pulmonary position should be anterior-posterior l Aortic root should not be too small

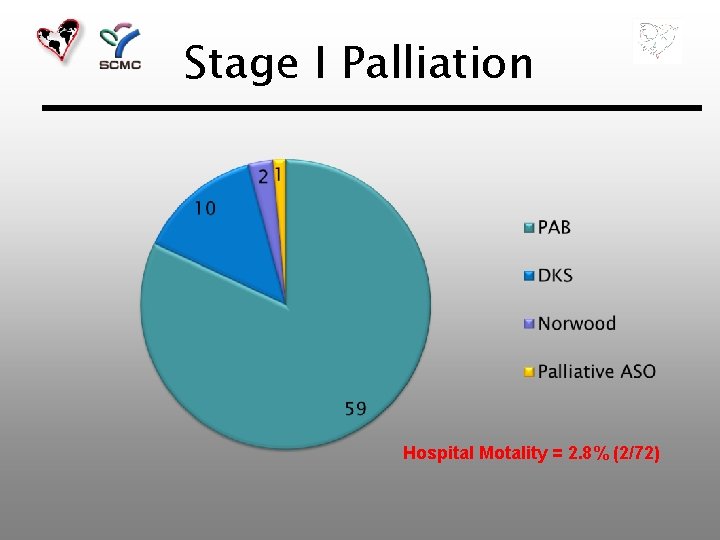
SCMC Data • 2002. 1 – 2014. 12 • 72 patients
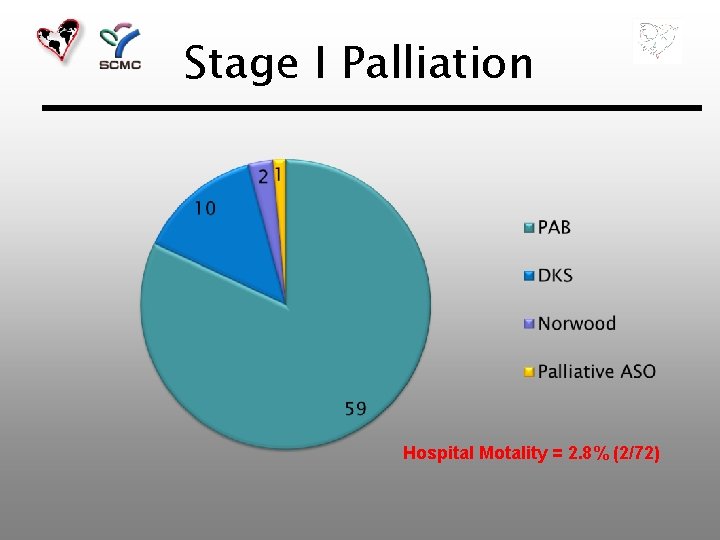
Stage I Palliation Hospital Motality = 2. 8% (2/72)


Re-operation before Stage II Glenn Rebanding 5 8. 4% (5/59 ) Shunt Revision 1 7. 6 (1/13) Other (Bleeding, Chylothorax) 2

9 Patients Failed at stage I Palliation n 2 hospital motality n 7 fail to pursue Glenn • Present late (after 6 m) • Post-op. AV valve regurgitation • Heterotaxy • m. PAP > 25 mm. Hg 5 4 5 6
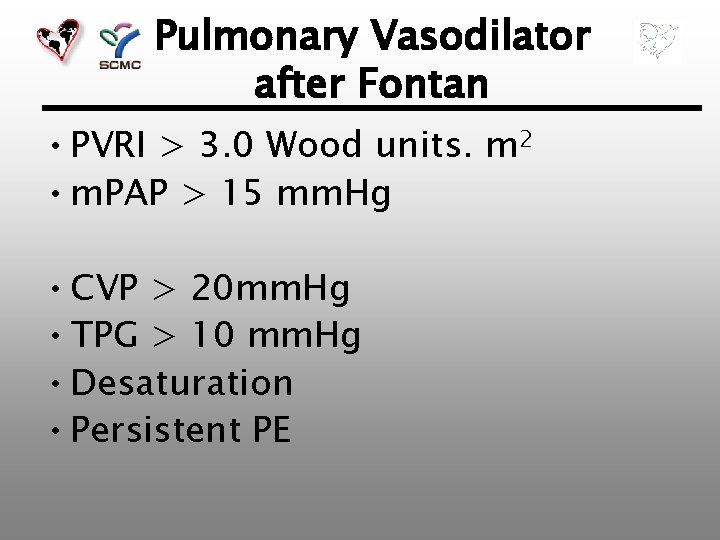
Pulmonary Vasodilator after Fontan • PVRI > 3. 0 Wood units. m 2 • m. PAP > 15 mm. Hg • CVP > 20 mm. Hg • TPG > 10 mm. Hg • Desaturation • Persistent PE
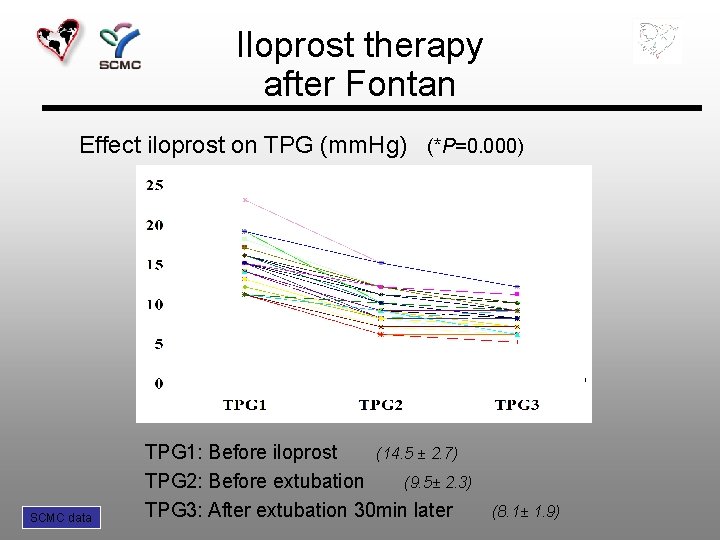
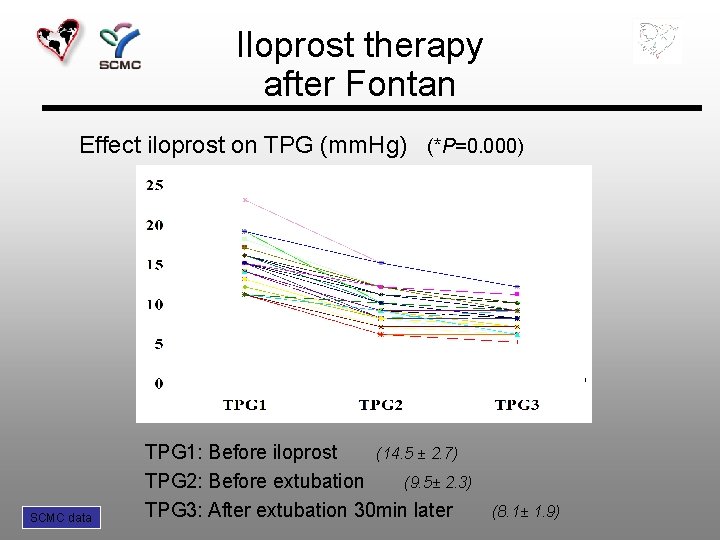
Iloprost therapy after Fontan Effect iloprost on TPG (mm. Hg) (*P=0. 000) SCMC data TPG 1: Before iloprost (14. 5 ± 2. 7) TPG 2: Before extubation (9. 5± 2. 3) TPG 3: After extubation 30 min later (8. 1± 1. 9)
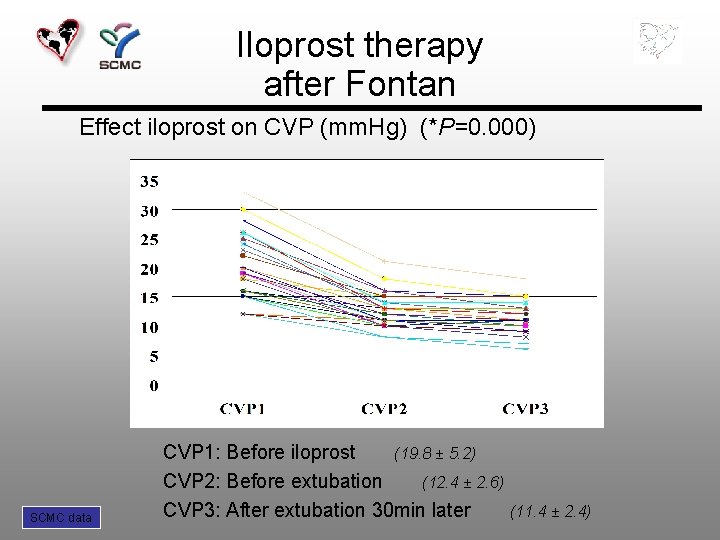
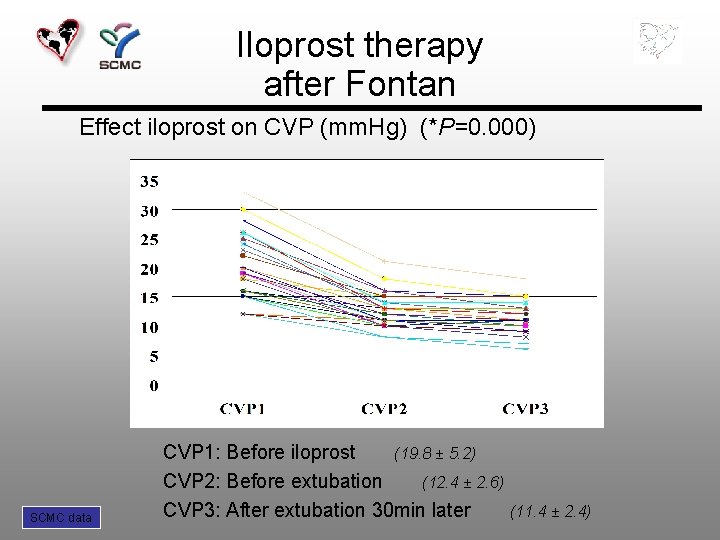
Iloprost therapy after Fontan Effect iloprost on CVP (mm. Hg) (*P=0. 000) SCMC data CVP 1: Before iloprost (19. 8 ± 5. 2) CVP 2: Before extubation (12. 4 ± 2. 6) CVP 3: After extubation 30 min later (11. 4 ± 2. 4)
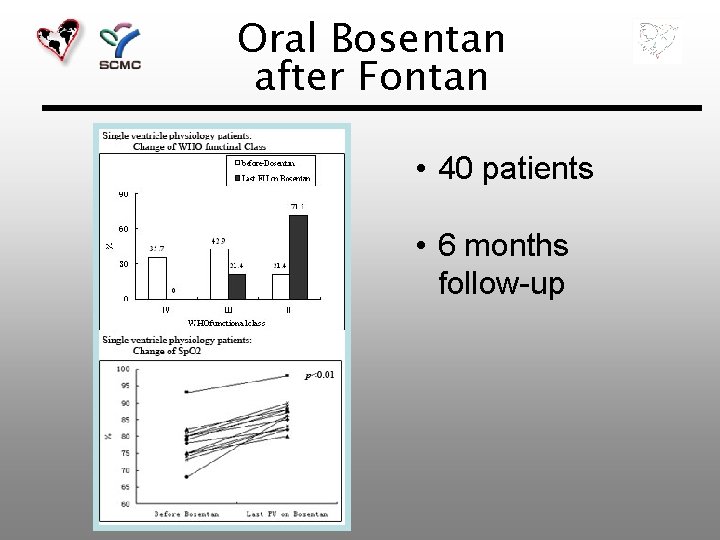
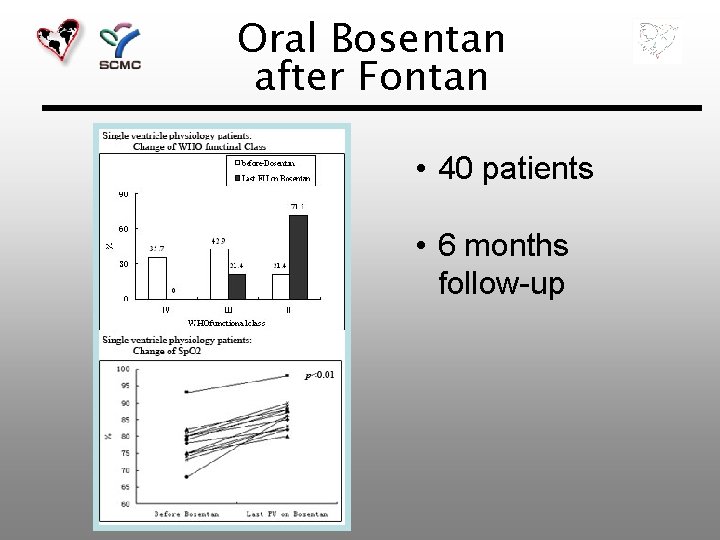
Oral Bosentan after Fontan • 40 patients • 6 months follow-up

Conclusion • Stage I palliation is the key point to treat single ventricle physiology with unrestricted pulmonary blood flow • Early diagnosis ensure a good long term outcome • Pulmonary vasodilators help to improve cardiac performance in patients with high PVR postoperatively

Thank you !
 Good decision making poster
Good decision making poster Med
Med Rvsp calculation
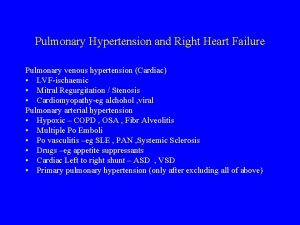
Rvsp calculation Pulmonary hypertension differential diagnosis
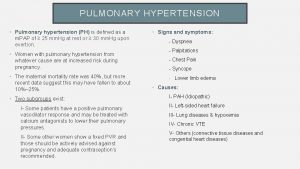
Pulmonary hypertension differential diagnosis Pulmonary hypertension definition
Pulmonary hypertension definition Bmpr gene
Bmpr gene Mitral stenosis pulmonary hypertension
Mitral stenosis pulmonary hypertension Pulmonary hypertension
Pulmonary hypertension Chd pulmonary hypertension
Chd pulmonary hypertension Pneumotrieste
Pneumotrieste Stages of pulmonary hypertension
Stages of pulmonary hypertension Pulmonary hypertension
Pulmonary hypertension Pathophysiology of pulmonary hypertension
Pathophysiology of pulmonary hypertension Screening decisions and preference decisions
Screening decisions and preference decisions Surfaces of heart
Surfaces of heart Intermediate mass
Intermediate mass Google image
Google image Muscular pectinati
Muscular pectinati Transverse fissure sheep brain
Transverse fissure sheep brain Crista terminalis
Crista terminalis Aorticopulmonary septum development
Aorticopulmonary septum development Septum secondum
Septum secondum Comissura habenularum
Comissura habenularum