Pulmonary Hypertension and the Right Ventricle UCSF Congenital
- Slides: 15
Pulmonary Hypertension and the Right Ventricle UCSF Congenital Cardiac Anesthesia Tutorials William C. K. Ng Division of Congenital Cardiac Anesthesia 2017
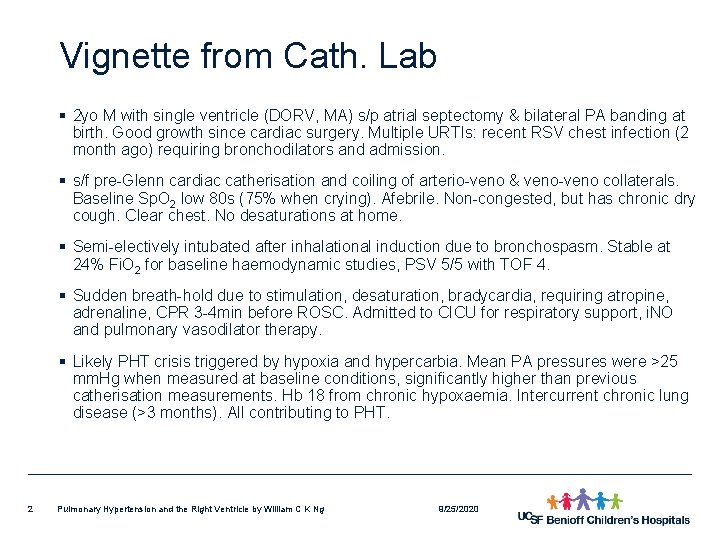
Vignette from Cath. Lab § 2 yo M with single ventricle (DORV, MA) s/p atrial septectomy & bilateral PA banding at birth. Good growth since cardiac surgery. Multiple URTIs: recent RSV chest infection (2 month ago) requiring bronchodilators and admission. § s/f pre-Glenn cardiac catherisation and coiling of arterio-veno & veno-veno collaterals. Baseline Sp. O 2 low 80 s (75% when crying). Afebrile. Non-congested, but has chronic dry cough. Clear chest. No desaturations at home. § Semi-electively intubated after inhalational induction due to bronchospasm. Stable at 24% Fi. O 2 for baseline haemodynamic studies, PSV 5/5 with TOF 4. § Sudden breath-hold due to stimulation, desaturation, bradycardia, requiring atropine, adrenaline, CPR 3 -4 min before ROSC. Admitted to CICU for respiratory support, i. NO and pulmonary vasodilator therapy. § Likely PHT crisis triggered by hypoxia and hypercarbia. Mean PA pressures were >25 mm. Hg when measured at baseline conditions, significantly higher than previous catherisation measurements. Hb 18 from chronic hypoxaemia. Intercurrent chronic lung disease (>3 months). All contributing to PHT. 2 Pulmonary Hypertension and the Right Ventricle by William C K Ng 9/25/2020
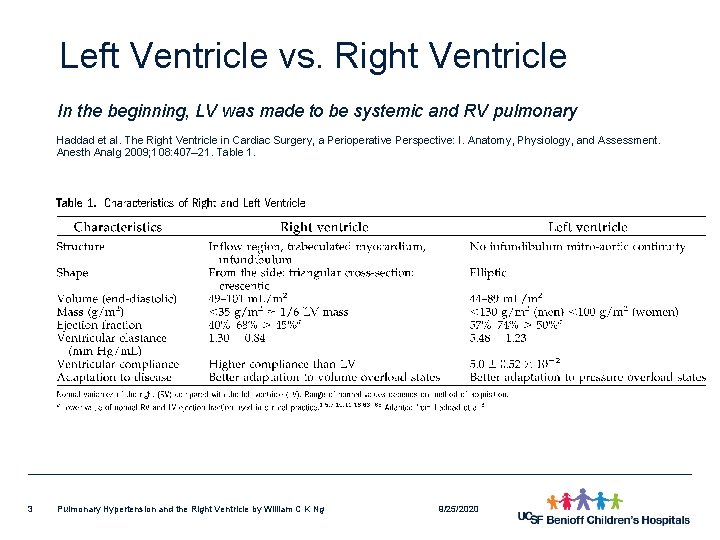
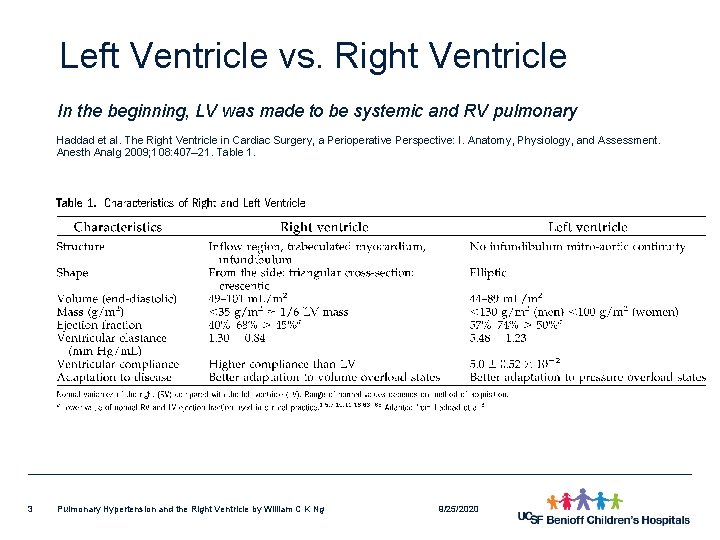
Left Ventricle vs. Right Ventricle In the beginning, LV was made to be systemic and RV pulmonary Haddad et al. The Right Ventricle in Cardiac Surgery, a Perioperative Perspective: I. Anatomy, Physiology, and Assessment. Anesth Analg 2009; 108: 407– 21. Table 1. 3 Pulmonary Hypertension and the Right Ventricle by William C K Ng 9/25/2020
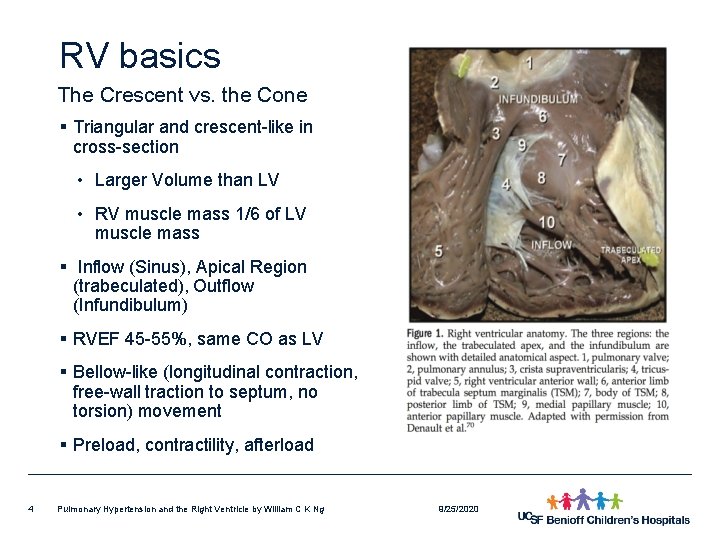
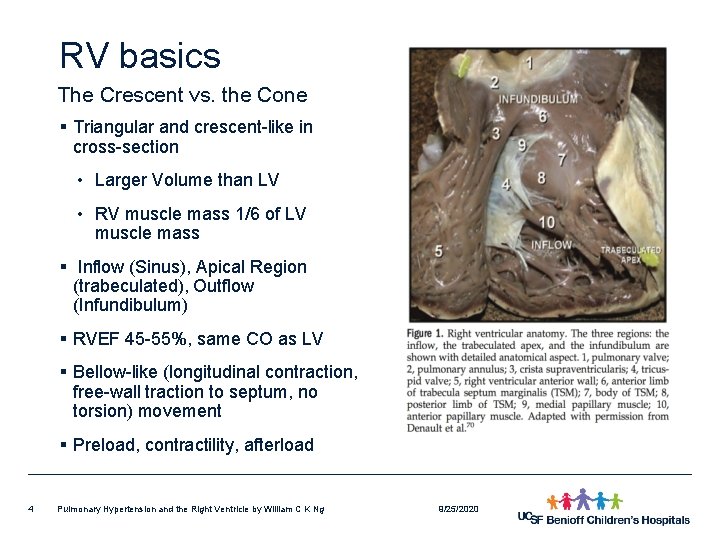
RV basics The Crescent vs. the Cone § Triangular and crescent-like in cross-section • Larger Volume than LV • RV muscle mass 1/6 of LV muscle mass § Inflow (Sinus), Apical Region (trabeculated), Outflow (Infundibulum) § RVEF 45 -55%, same CO as LV § Bellow-like (longitudinal contraction, free-wall traction to septum, no torsion) movement § Preload, contractility, afterload 4 Pulmonary Hypertension and the Right Ventricle by William C K Ng 9/25/2020
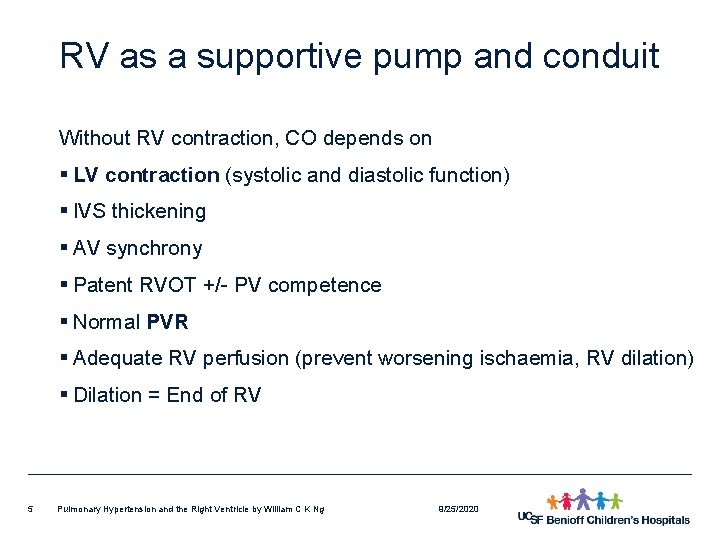
RV as a supportive pump and conduit Without RV contraction, CO depends on § LV contraction (systolic and diastolic function) § IVS thickening § AV synchrony § Patent RVOT +/- PV competence § Normal PVR § Adequate RV perfusion (prevent worsening ischaemia, RV dilation) § Dilation = End of RV 5 Pulmonary Hypertension and the Right Ventricle by William C K Ng 9/25/2020
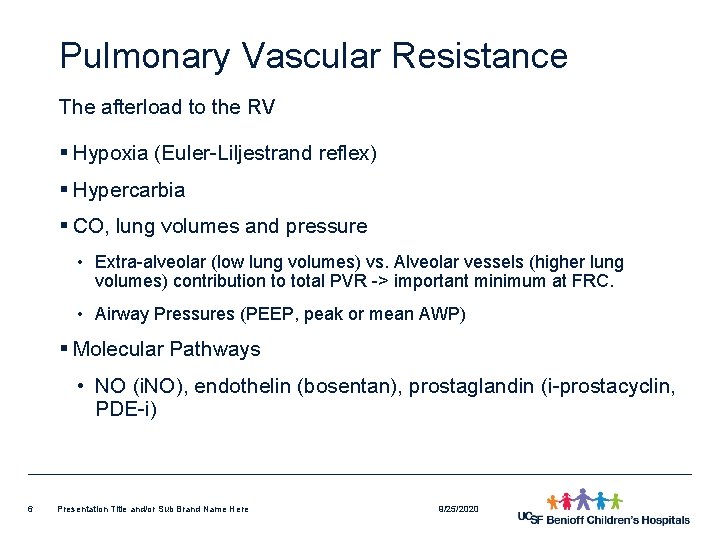
Pulmonary Vascular Resistance The afterload to the RV § Hypoxia (Euler-Liljestrand reflex) § Hypercarbia § CO, lung volumes and pressure • Extra-alveolar (low lung volumes) vs. Alveolar vessels (higher lung volumes) contribution to total PVR -> important minimum at FRC. • Airway Pressures (PEEP, peak or mean AWP) § Molecular Pathways • NO (i. NO), endothelin (bosentan), prostaglandin (i-prostacyclin, PDE-i) 6 Presentation Title and/or Sub Brand Name Here 9/25/2020
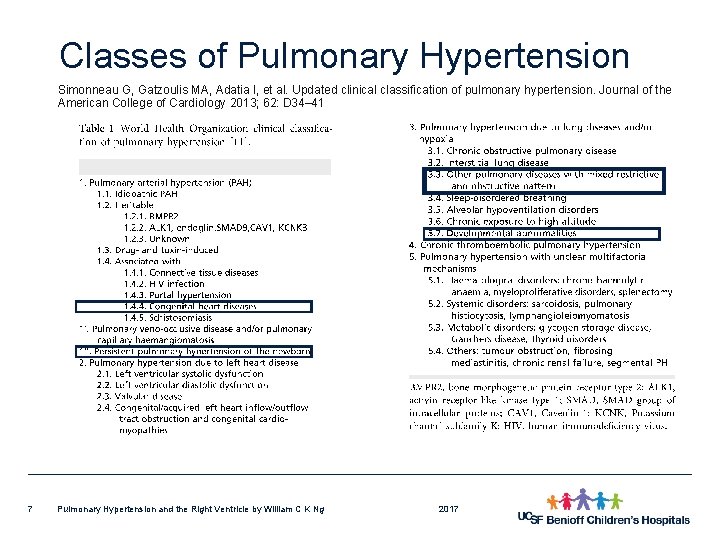
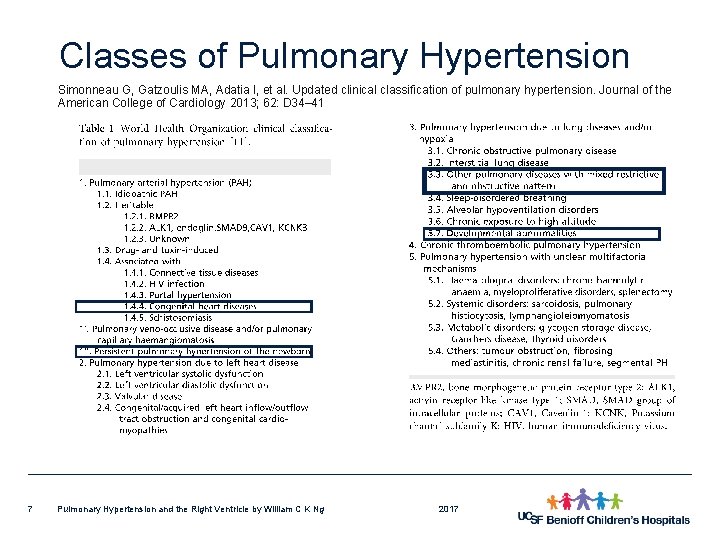
Classes of Pulmonary Hypertension Simonneau G, Gatzoulis MA, Adatia I, et al. Updated clinical classification of pulmonary hypertension. Journal of the American College of Cardiology 2013; 62: D 34– 41 7 Pulmonary Hypertension and the Right Ventricle by William C K Ng 2017
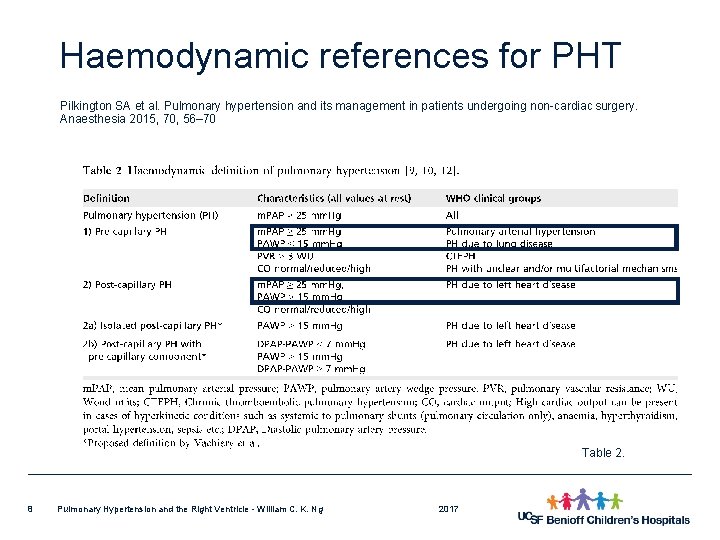
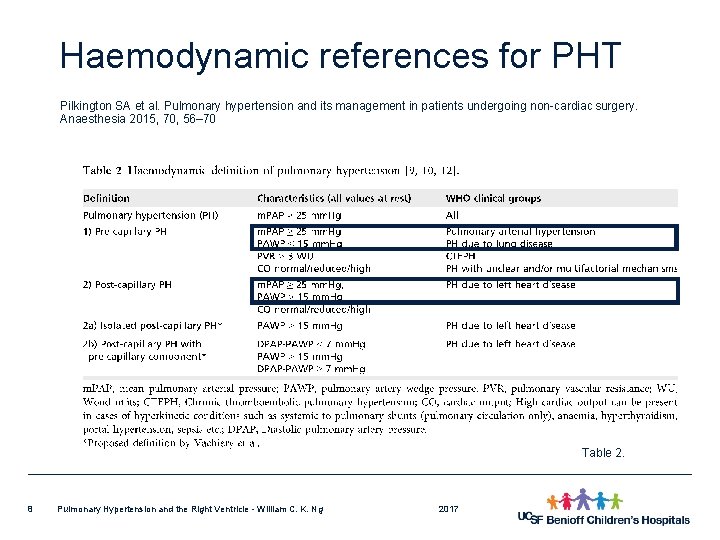
Haemodynamic references for PHT Pilkington SA et al. Pulmonary hypertension and its management in patients undergoing non-cardiac surgery. Anaesthesia 2015, 70, 56– 70 Table 2. 8 Pulmonary Hypertension and the Right Ventricle - William C. K. Ng 2017
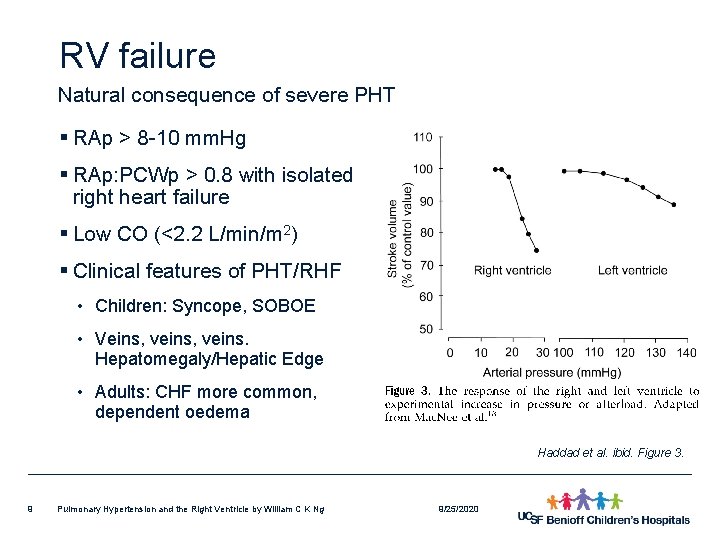
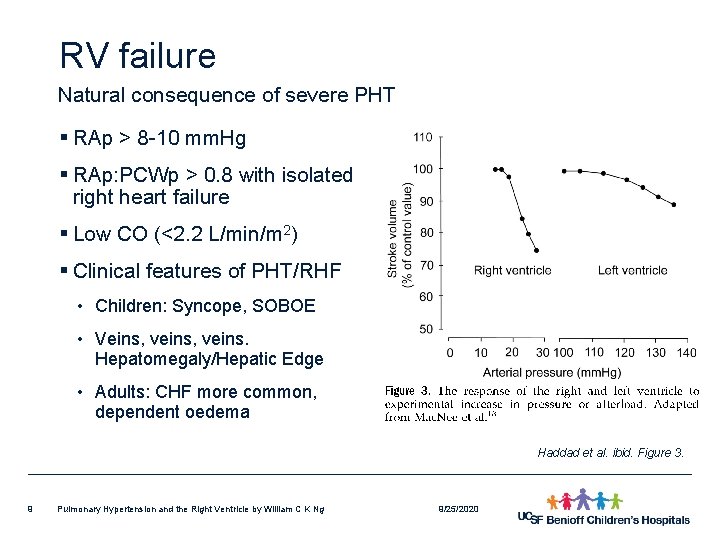
RV failure Natural consequence of severe PHT § RAp > 8 -10 mm. Hg § RAp: PCWp > 0. 8 with isolated right heart failure § Low CO (<2. 2 L/min/m 2) § Clinical features of PHT/RHF • Children: Syncope, SOBOE • Veins, veins. Hepatomegaly/Hepatic Edge • Adults: CHF more common, dependent oedema Haddad et al. ibid. Figure 3. 9 Pulmonary Hypertension and the Right Ventricle by William C K Ng 9/25/2020
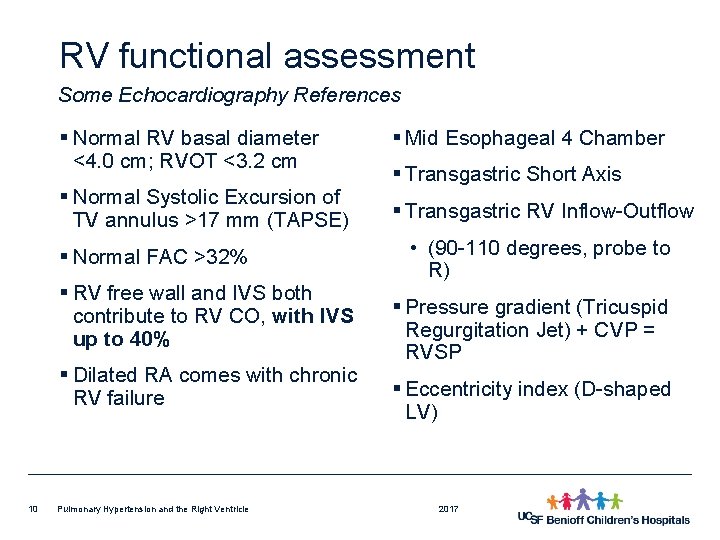
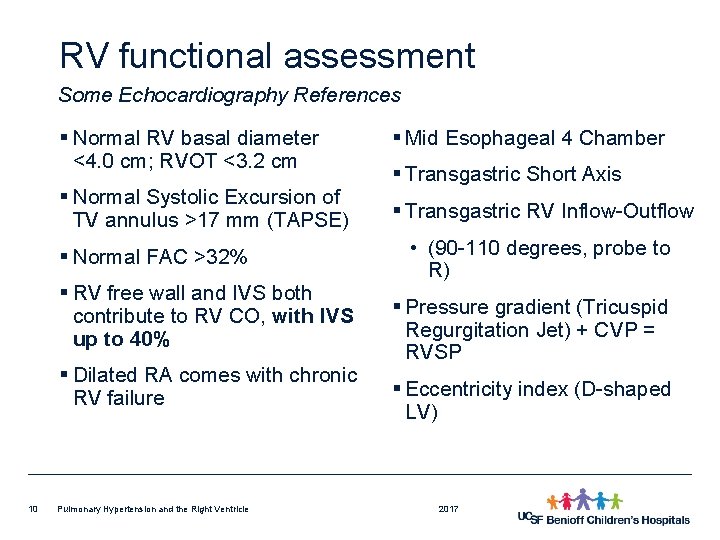
RV functional assessment Some Echocardiography References § Normal RV basal diameter <4. 0 cm; RVOT <3. 2 cm § Normal Systolic Excursion of TV annulus >17 mm (TAPSE) § Normal FAC >32% § RV free wall and IVS both contribute to RV CO, with IVS up to 40% § Dilated RA comes with chronic RV failure 10 Pulmonary Hypertension and the Right Ventricle § Mid Esophageal 4 Chamber § Transgastric Short Axis § Transgastric RV Inflow-Outflow • (90 -110 degrees, probe to R) § Pressure gradient (Tricuspid Regurgitation Jet) + CVP = RVSP § Eccentricity index (D-shaped LV) 2017
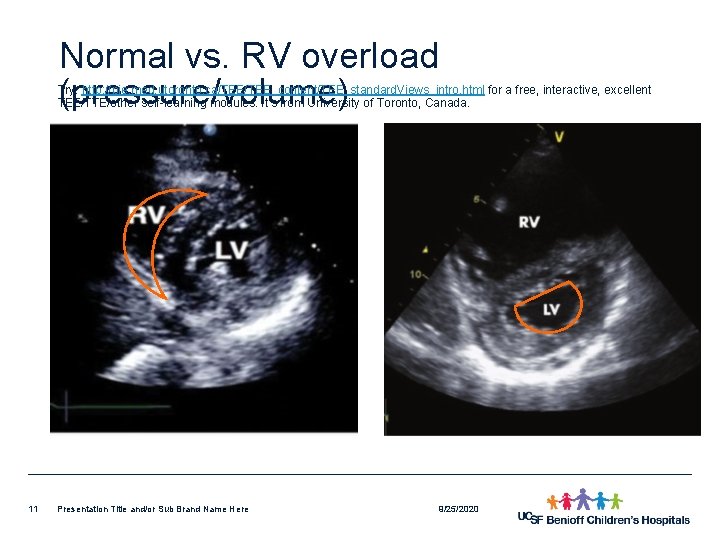
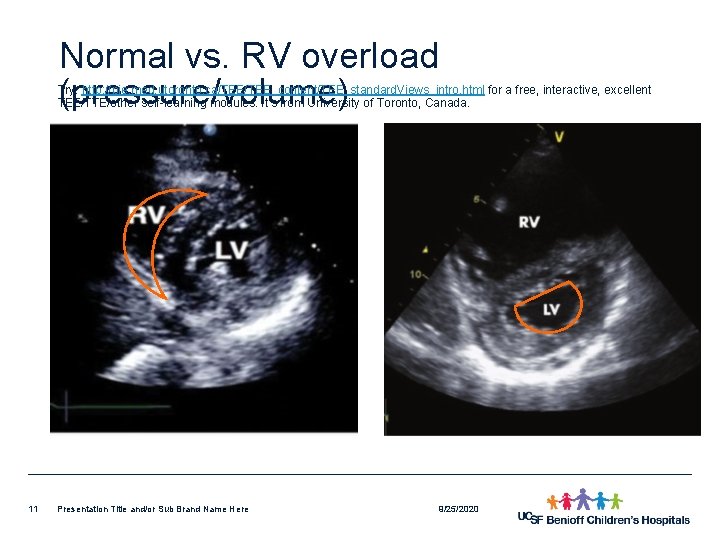
Normal vs. RV overload (pressure/volume) Try: http: //pie. med. utoronto. ca/TEE_content/TEE_standard. Views_intro. html for a free, interactive, excellent TEE/TTE/other self-learning modules. It’s from University of Toronto, Canada. 11 Presentation Title and/or Sub Brand Name Here 9/25/2020
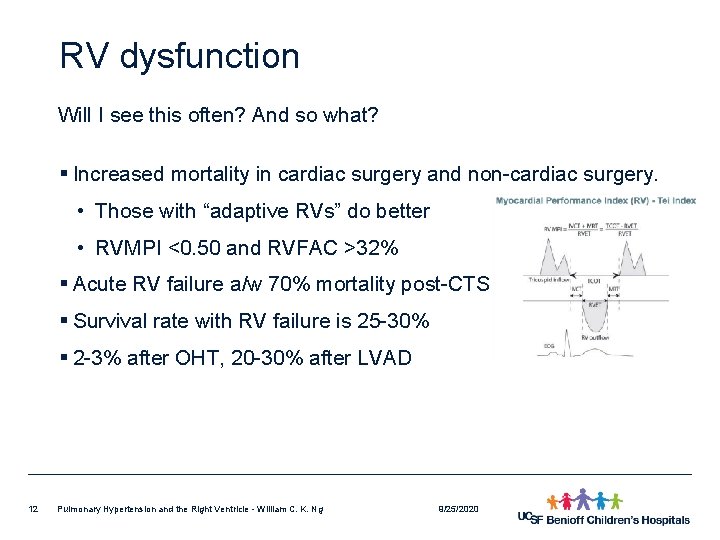
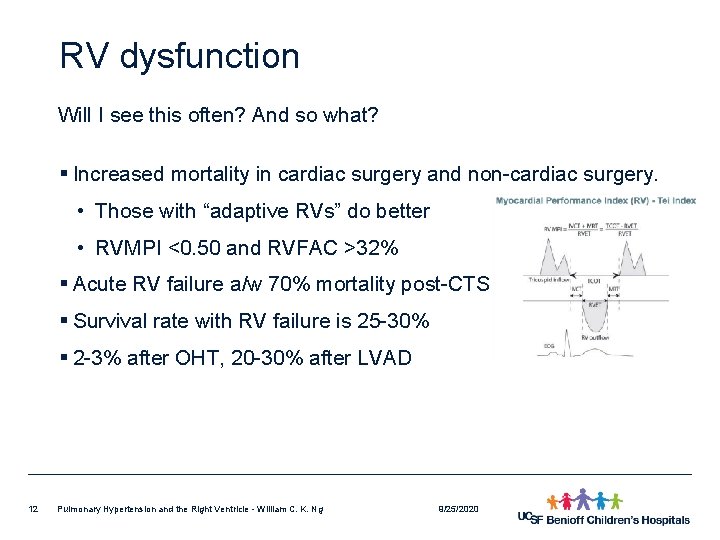
RV dysfunction Will I see this often? And so what? § Increased mortality in cardiac surgery and non-cardiac surgery. • Those with “adaptive RVs” do better • RVMPI <0. 50 and RVFAC >32% § Acute RV failure a/w 70% mortality post-CTS § Survival rate with RV failure is 25 -30% § 2 -3% after OHT, 20 -30% after LVAD 12 Pulmonary Hypertension and the Right Ventricle - William C. K. Ng 9/25/2020
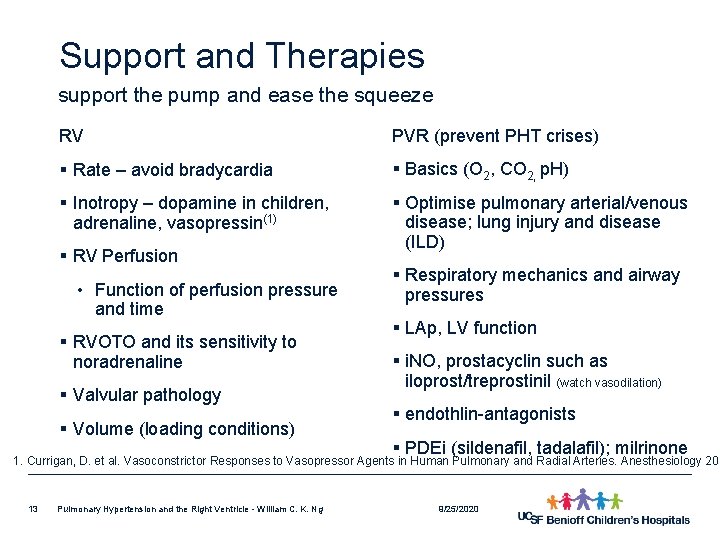
Support and Therapies support the pump and ease the squeeze RV PVR (prevent PHT crises) § Rate – avoid bradycardia § Basics (O 2, CO 2, p. H) § Inotropy – dopamine in children, adrenaline, vasopressin(1) § Optimise pulmonary arterial/venous disease; lung injury and disease (ILD) § RV Perfusion • Function of perfusion pressure and time § RVOTO and its sensitivity to noradrenaline § Valvular pathology § Volume (loading conditions) § Respiratory mechanics and airway pressures § LAp, LV function § i. NO, prostacyclin such as iloprost/treprostinil (watch vasodilation) § endothlin-antagonists § PDEi (sildenafil, tadalafil); milrinone 1. Currigan, D. et al. Vasoconstrictor Responses to Vasopressor Agents in Human Pulmonary and Radial Arteries. Anesthesiology 201 13 Pulmonary Hypertension and the Right Ventricle - William C. K. Ng 9/25/2020
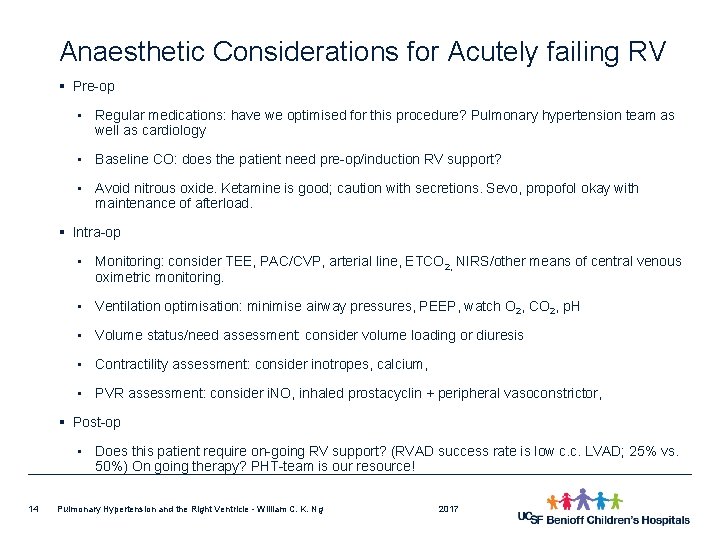
Anaesthetic Considerations for Acutely failing RV § Pre-op • Regular medications: have we optimised for this procedure? Pulmonary hypertension team as well as cardiology • Baseline CO: does the patient need pre-op/induction RV support? • Avoid nitrous oxide. Ketamine is good; caution with secretions. Sevo, propofol okay with maintenance of afterload. § Intra-op • Monitoring: consider TEE, PAC/CVP, arterial line, ETCO 2, NIRS/other means of central venous oximetric monitoring. • Ventilation optimisation: minimise airway pressures, PEEP, watch O 2, CO 2, p. H • Volume status/need assessment: consider volume loading or diuresis • Contractility assessment: consider inotropes, calcium, • PVR assessment: consider i. NO, inhaled prostacyclin + peripheral vasoconstrictor, § Post-op • Does this patient require on-going RV support? (RVAD success rate is low c. c. LVAD; 25% vs. 50%) On going therapy? PHT-team is our resource! 14 Pulmonary Hypertension and the Right Ventricle - William C. K. Ng 2017
References Selected reviews § Haddad, F. et al. The Right Ventricle in Cardiac Surgery, a Perioperative Perspective I & II. Anesth Analg 2009; 108: 407– 21 & Anesth Analg 2009; 108: 422– 33. DOI: 10. 1213/ane. 0 b 013 e 31818 f 8623 & 10. 1213/ane. 0 b 013 e 31818 d 8 b 92 § Galante, D. Intraoperative management of pulmonary arterial hypertension in infants and children. Curr Opin Anesthesiol 2011; 24: 468– 471. DOI: 10. 1213/ane. 0 b 013 e 31818 f 8623 § Pilkington, S. A. Pulmonary hypertension and its management in patients undergoing non-cardiac surgery. Anaesthesia 2015, 70, 56– 70. DOI: 10. 1111/anae. 12831 § Peacock, A. Pulmonary hypertension. Eur Respir Rev 2013; 22: 127, 20– 25. DOI: 10. 1183/09059180. 00006912 § Schillcutt, S. Evaluation of Right Ventricular Function in Simple Steps. 2015 http: //www. scahq. org/Portals/0/uploads/ECHO 15/mon/Evaluation_of_RV. pdf 15 Pulmonary Hypertension and the Right Ventricle - William C. K. Ng 2017
 Right product right place right time right price
Right product right place right time right price Family time
Family time Med
Med Pulmonary hypertension severity
Pulmonary hypertension severity Nt pro brain natriuretic peptide
Nt pro brain natriuretic peptide Pulmonary hypertension definition
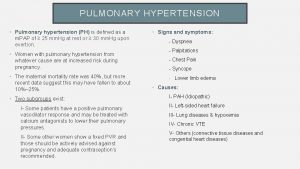
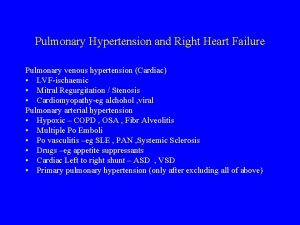
Pulmonary hypertension definition Pah groups
Pah groups Mitral stenosis pulmonary hypertension
Mitral stenosis pulmonary hypertension Pulmonary hypertension
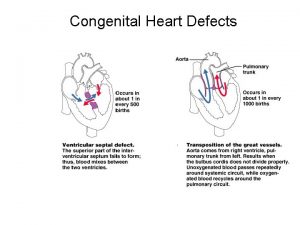
Pulmonary hypertension Chd pulmonary hypertension
Chd pulmonary hypertension Pulmonary hypertension
Pulmonary hypertension Stages of pulmonary hypertension
Stages of pulmonary hypertension Pulmonary hypertension
Pulmonary hypertension Nervous mechanism for regulation of blood pressure
Nervous mechanism for regulation of blood pressure Heart apex base
Heart apex base Muscular pectinati
Muscular pectinati