Sex Hormones ALLPPT com Free Power Point Templates






- Slides: 36
Sex Hormones ALLPPT. com _ Free Power. Point Templates, Diagrams and Charts
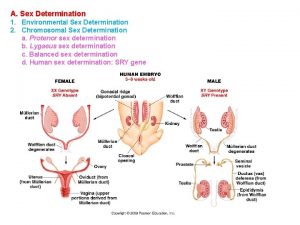
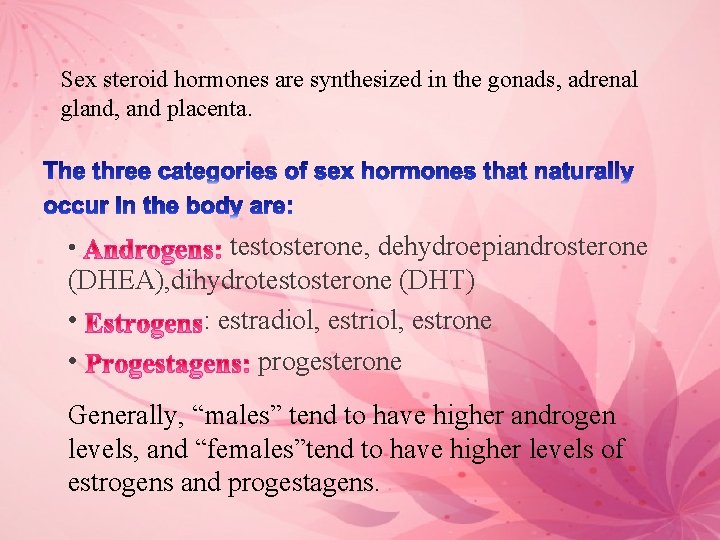
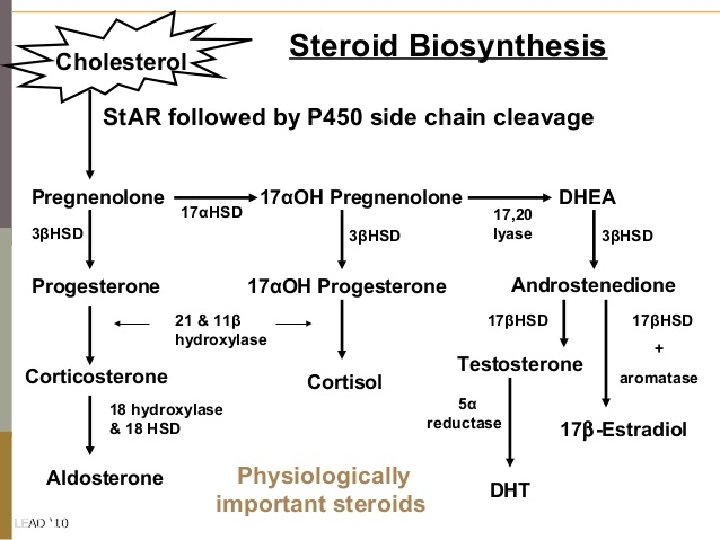
Sex steroid hormones are synthesized in the gonads, adrenal gland, and placenta. testosterone, dehydroepiandrosterone (DHEA), dihydrotestosterone (DHT) • : estradiol, estrone • progesterone • Generally, “males” tend to have higher androgen levels, and “females”tend to have higher levels of estrogens and progestagens.
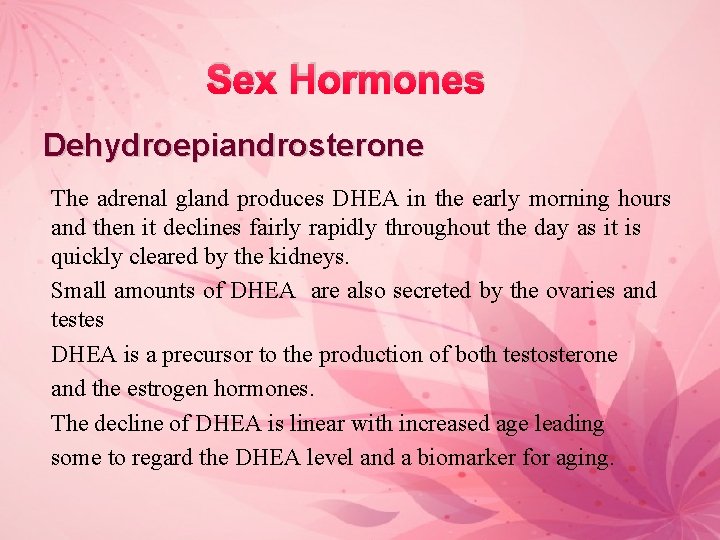
Sex Hormones Dehydroepiandrosterone The adrenal gland produces DHEA in the early morning hours and then it declines fairly rapidly throughout the day as it is quickly cleared by the kidneys. Small amounts of DHEA are also secreted by the ovaries and testes DHEA is a precursor to the production of both testosterone and the estrogen hormones. The decline of DHEA is linear with increased age leading some to regard the DHEA level and a biomarker for aging.
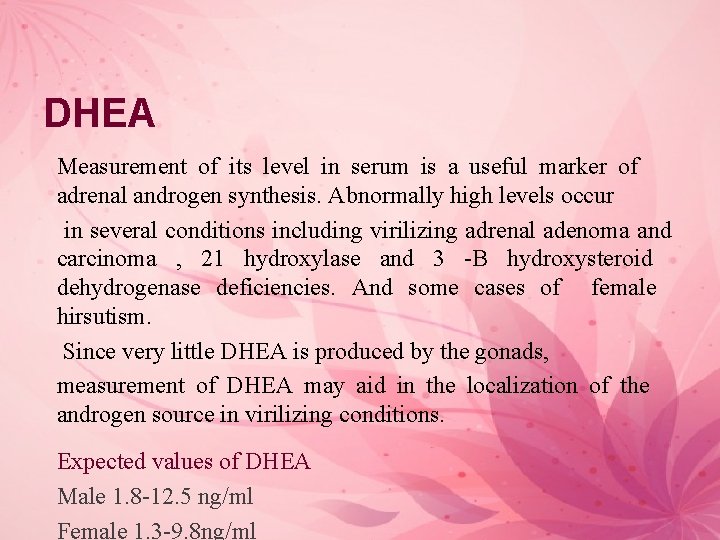
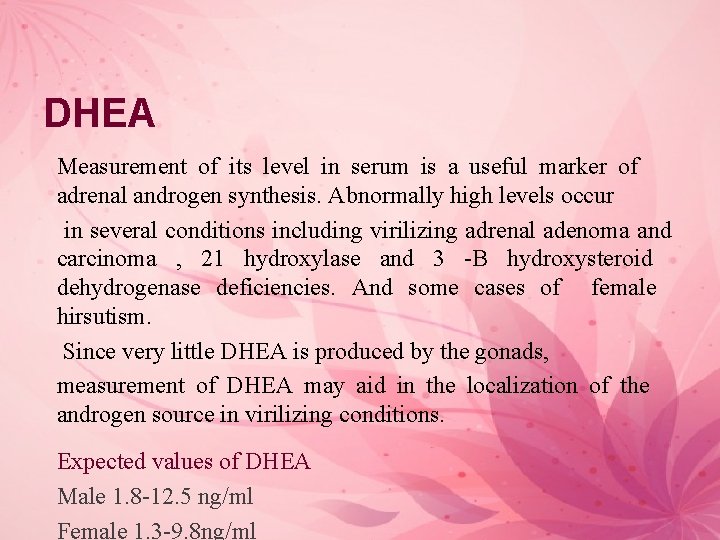
DHEA Measurement of its level in serum is a useful marker of adrenal androgen synthesis. Abnormally high levels occur in several conditions including virilizing adrenal adenoma and carcinoma , 21 hydroxylase and 3 -B hydroxysteroid dehydrogenase deficiencies. And some cases of female hirsutism. Since very little DHEA is produced by the gonads, measurement of DHEA may aid in the localization of the androgen source in virilizing conditions. Expected values of DHEA Male 1. 8 -12. 5 ng/ml Female 1. 3 -9. 8 ng/ml
Sex Hormones
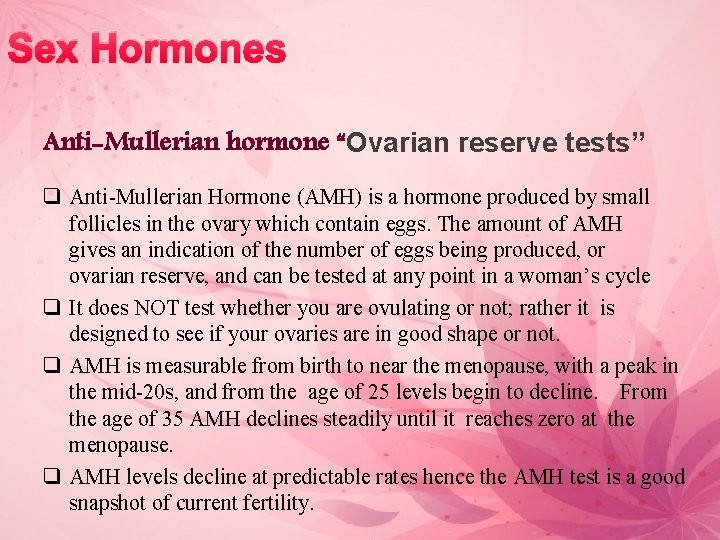
Sex Hormones Anti-Mullerian hormone “Ovarian reserve tests” q Anti-Mullerian Hormone (AMH) is a hormone produced by small follicles in the ovary which contain eggs. The amount of AMH gives an indication of the number of eggs being produced, or ovarian reserve, and can be tested at any point in a woman’s cycle q It does NOT test whether you are ovulating or not; rather it is designed to see if your ovaries are in good shape or not. q AMH is measurable from birth to near the menopause, with a peak in the mid-20 s, and from the age of 25 levels begin to decline. From the age of 35 AMH declines steadily until it reaches zero at the menopause. q AMH levels decline at predictable rates hence the AMH test is a good snapshot of current fertility.

• One recent article described continuous use of combined contraception (i. e. without monthly breaks) was associated with a reduction of AMH levels. • Women under the age of 35 may be tested to determine ovarian reserve which may assist to determine optimal timing to start a family. The test can also be helpful in determining the fertility status of patients at risk of diminished ovarian reserve e. g. women with a history of ovarian failure, family history of early onset menopause, auto immune disease, women who have undergone chemotherapy or had ovarian surgery. It is also helpful for Polycystic Ovary Syndrome patients.
It is a single blood test that can be done at any time during the menstrual cycle, used to: § Determine fertility status § Determine a patient’s response to fertility medication § It can also help to predict how many eggs you are likely to obtain in an IVF cycle. § It may also identify women who may undergo early menopause, and therefore who may lose their fertility earlier than average.
Each month at ovulation, chance of conception is based upon both the health of the egg and the ovarian environment in which the egg developed. Ovarian reserve is another fundamental factor linked to fertility. Ovarian reserve refers to a woman’s current supply of eggs within her ovaries and is closely associated with reproductive potential. In general, the greater the number of eggs remaining, the better the chance for conception. As a woman ages, her supply diminishes over time, reducing her fertility, until all of the eggs are depleted at menopause. Determining Ovarian Reserve Through FSH and AMH Clinical discordance in serum AMH and FSH values thus was frequent and was age dependent. FSH mostly reflects the last two weeks of follicular maturation when follicles become gonadotropin sensitive, while AMH is mostly representative of the young, post-primordial to preantral follicle pool going through earlier stages of folliculogenesis.

Menstruation (From day 1 to 5) Ø Follicular phase (From day 1 to 13) Ø Ovulation phase (Day 14) Ø Luteal phase (From day 15 to 28)
Follicular Phase. The follicular phase begins with the first day of menstrual bleeding: At the start of the follicular phase, estrogen and progesterone levels are at their lowest point. This causes the uterine lining to break down and shed. At the same time, the hypothalamus produces Gn. RH, which stimulates the production of follicle-stimulating hormone (FSH) and luteinizing hormone (LH). FSH and LH trigger the production of estrogen. As FSH levels increase, it stimulate the growth and maturation of eggs in the follicles. About 15 - 20 follicles are stimulated, but only one follicle continues to mature. The dominant follicle produces estrogen. The other follicles stop growing and disintegrate.

Ovulation is when a mature egg is released from the ovary, pushed down the fallopian tube, and is available to be fertilized. Approximately every month an egg will mature within one of your ovaries. As it reaches maturity, the egg is released by the ovary where it enters the fallopian tube to make its way towards the uterus. As soon as the fertilized egg has implanted, your body starts producing the pregnancy hormone, human Chorionic Gonadotrophin (h. CG), which will keep the empty follicle active. It continues to produce the hormones estrogen and progesterone to prevent the lining of the womb from being shed, until the placenta (which contains all the nutrients the embryo needs) is mature enough to maintain the pregnancy.
Ovulatory Phase. The ovulatory phase occurs halfway through the menstrual cycle (about 14 days after the start of the follicular phase. ) Ovulation, the critical process for conception, occurs during the ovulatory phase. A woman’s fertile period starts about 3 - 5 days before ovulation and ends 24 - 48 hours after it. During the ovulatory phase: The increase in estrogen from the dominant follicle triggers a surge in LH. As estrogen levels rise, they also prompt the cervix to secrete more mucus to help nourish and propel sperm to the egg. The LH surge signals the dominant follicle to burst and release the developed egg into the fallopian tube. The release of the egg is called ovulation. Once in the fallopian tube, the egg is in place for fertilization. The egg can live for 24 - 48 hours after being released. (Sperm can live for 3 - 5 days. ) A woman is most likely to get pregnant if sex occurs in the 3 - 5 days before ovulation or on the day of ovulation.
Luteal Phase. The luteal phase begins immediately after ovulation and ends when the next menstrual period starts. The luteal phase lasts about 12 - 16 days. During the luteal phase: After releasing the egg, the ruptured follicle closes and forms corpus luteum, a yellow mass of cells that provide a source of estrogen and progesterone during pregnancy. These hormones help the uterine lining to thicken and prepare for the egg’s implantation. If the egg is fertilized by a sperm cell, it implants in the uterus and pregnancy begins. If fertilization does not occur, the egg breaks apart. The corpus luteum degenerates, and estrogen and progesterone levels drop. Finally, the thickened uterine lining sloughs off and is shed along with the unfertilized egg during menstruation. The menstrual cycle begins again.
FSH and LH Luteinizing hormone (LH) and follicle-stimulating hormone (FSH) are called gonadotropins because stimulate the gonads (in males, the testes, and in females, the ovaries). They are not necessary for life, but are essential for reproduction. Measuring the gonadotropic hormones FSH & LH help determine whether a gonadal deficiency is of primary origin or is due to insufficient stimulation by the pituitary hormones. Measuring the levels of FSH and LH is of value in studying children with endocrine problems related to precocious puberty. In the case of anovulatory fertility problems, the presence or absence of the mid cycle peak can be established through a series of daily blood specimens.
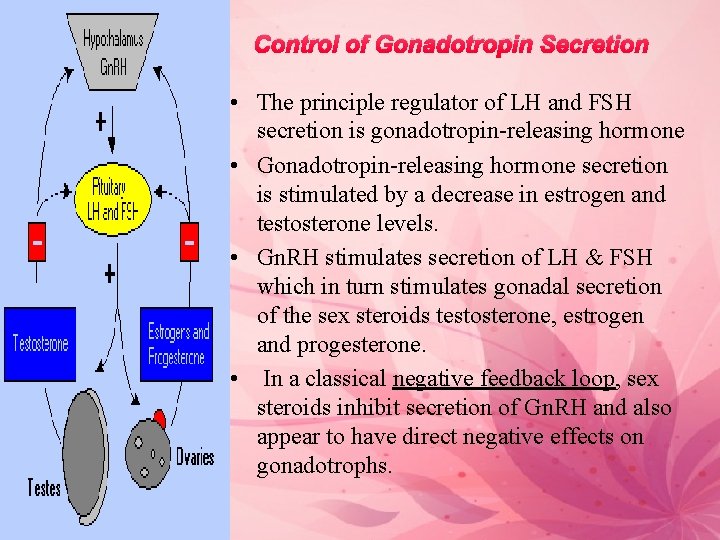
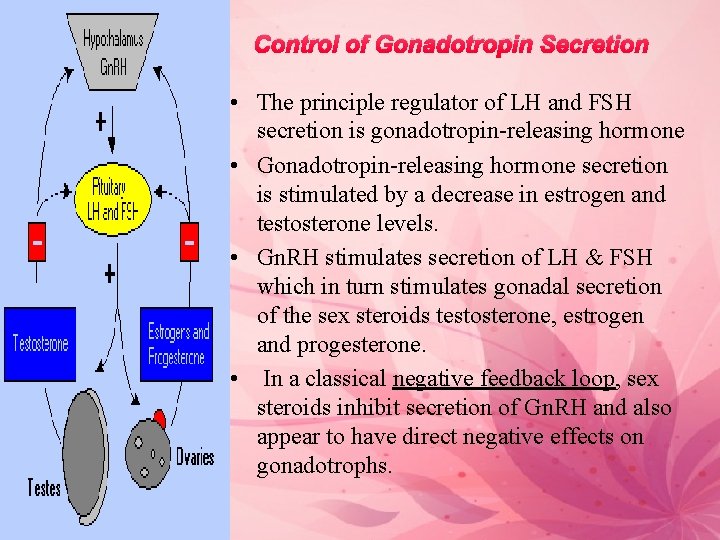
Control of Gonadotropin Secretion • The principle regulator of LH and FSH secretion is gonadotropin-releasing hormone • Gonadotropin-releasing hormone secretion is stimulated by a decrease in estrogen and testosterone levels. • Gn. RH stimulates secretion of LH & FSH which in turn stimulates gonadal secretion of the sex steroids testosterone, estrogen and progesterone. • In a classical negative feedback loop, sex steroids inhibit secretion of Gn. RH and also appear to have direct negative effects on gonadotrophs.
FSH is a glycoprotein hormone, produced in the anterior pituitary and released into the blood in response to Gn. RH (Gn. RH is released from the hypothalamus). FSH regulates the development, growth, pubertal maturation, and reproductive processes of the human body. In both males and females, FSH stimulates the maturation of germ cells. In males, FSH controls spermatogenesis In females, FSH stimulate the growth and maturation of eggs in the follicles
In female, the FSH is transported to the ovary, enters the developing follicle, and stimulates the granulosa cells to produce estrogen. Granulosa cells are a type of cells lining the follicle FSH is also responsible for growth of the follicle, involving both an increase in the number of granulosa cells and secretion of follicular fluid. As the follicle grows, the granulosa cells secrete a hormone called inhibin into the follicular fluid. This hormone is carried, through the vascular system, back to the anterior pituitary where it suppresses the secretion of FSH. • In men, FSH partially controls spermatogenesis, but the presence of testosterone is also necessary.
• The test is usually performed on cycle day 3 but it can also be performed on day 2, 3, or 4 of a woman's menstrual cycle. • FSH test is usually carried out on the 3 rd day of your menstrual cycle as this gives the most accurate reading of your ovarian reserve (number of eggs within your ovaries). • FSH levels fluctuate throughout your cycle and peak at ovulation • Your FSH level is measured along with your LH and estradiol. • Day 3 estradiol test is exactly the same as the Day 3 FSH test. • High levels of FSH/estradiol ratio mean poor quality ovarian reserve. Low levels are better, say 3 m. IU/ml to 10 m. UI/ml. More than 12 m. UI/ml indicates a problem and 25 m. UI/ml means ovarian failure. • You may be asked to stop taking medicines (including birth control pills) that contain estrogen or progesterone or both for up to 4 weeks before having a follicle-stimulating hormone (FSH) test.
Because your FSH levels rise when your ovaries stop producing enough estrogen, high FSH levels can signal that your body is entering menopause. As women approach menopause, their baseline FSH level will gradually increase. When a woman goes into menopause she is essentially running out of eggs and estrogen production in her ovaries. Sensing a low estrogen environment, the brain releases more FSH from the pituitary gland in an attempt to stimulate the ovaries to produce a mature follicle and more estrogen.
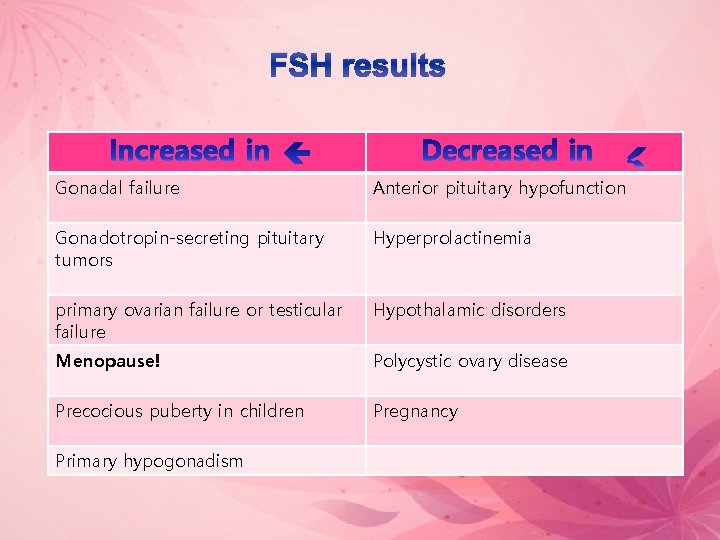
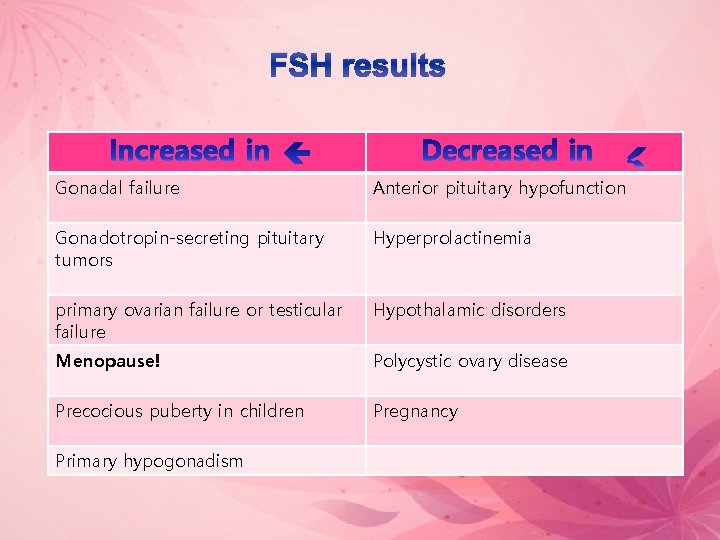
FSH results Gonadal failure Anterior pituitary hypofunction Gonadotropin-secreting pituitary tumors Hyperprolactinemia primary ovarian failure or testicular failure Hypothalamic disorders Menopause! Polycystic ovary disease Precocious puberty in children Pregnancy Primary hypogonadism
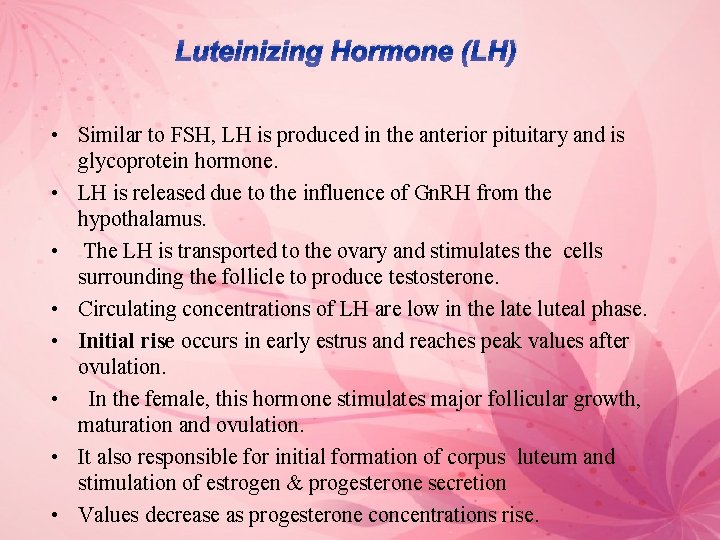
Luteinizing Hormone (LH) • Similar to FSH, LH is produced in the anterior pituitary and is glycoprotein hormone. • LH is released due to the influence of Gn. RH from the hypothalamus. • The LH is transported to the ovary and stimulates the cells surrounding the follicle to produce testosterone. • Circulating concentrations of LH are low in the late luteal phase. • Initial rise occurs in early estrus and reaches peak values after ovulation. • In the female, this hormone stimulates major follicular growth, maturation and ovulation. • It also responsible for initial formation of corpus luteum and stimulation of estrogen & progesterone secretion • Values decrease as progesterone concentrations rise.
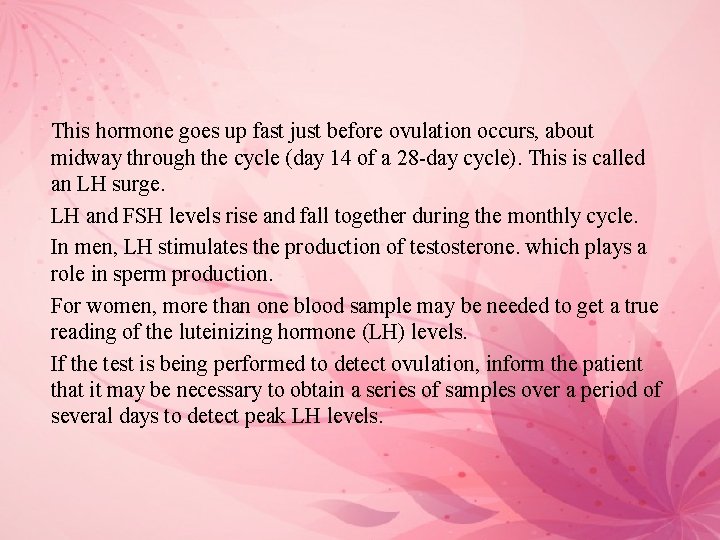
This hormone goes up fast just before ovulation occurs, about midway through the cycle (day 14 of a 28 -day cycle). This is called an LH surge. LH and FSH levels rise and fall together during the monthly cycle. In men, LH stimulates the production of testosterone. which plays a role in sperm production. For women, more than one blood sample may be needed to get a true reading of the luteinizing hormone (LH) levels. If the test is being performed to detect ovulation, inform the patient that it may be necessary to obtain a series of samples over a period of several days to detect peak LH levels.
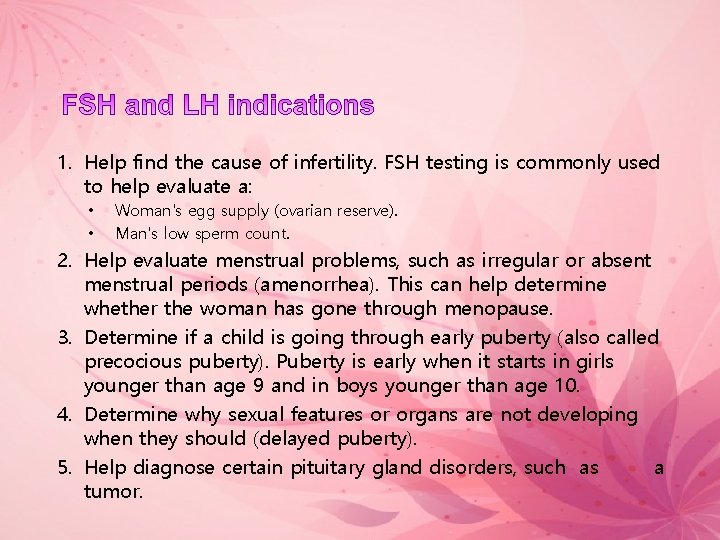
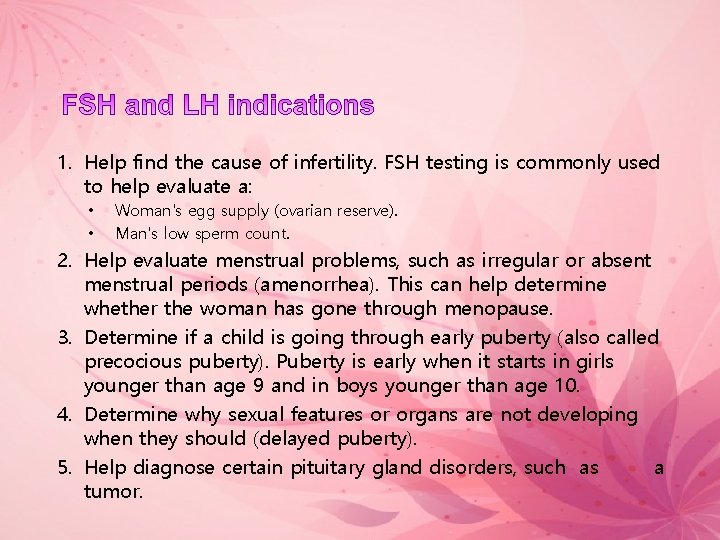
1. Help find the cause of infertility. FSH testing is commonly used to help evaluate a: • • Woman's egg supply (ovarian reserve). Man's low sperm count. 2. Help evaluate menstrual problems, such as irregular or absent menstrual periods (amenorrhea). This can help determine whether the woman has gone through menopause. 3. Determine if a child is going through early puberty (also called precocious puberty). Puberty is early when it starts in girls younger than age 9 and in boys younger than age 10. 4. Determine why sexual features or organs are not developing when they should (delayed puberty). 5. Help diagnose certain pituitary gland disorders, such as a tumor.
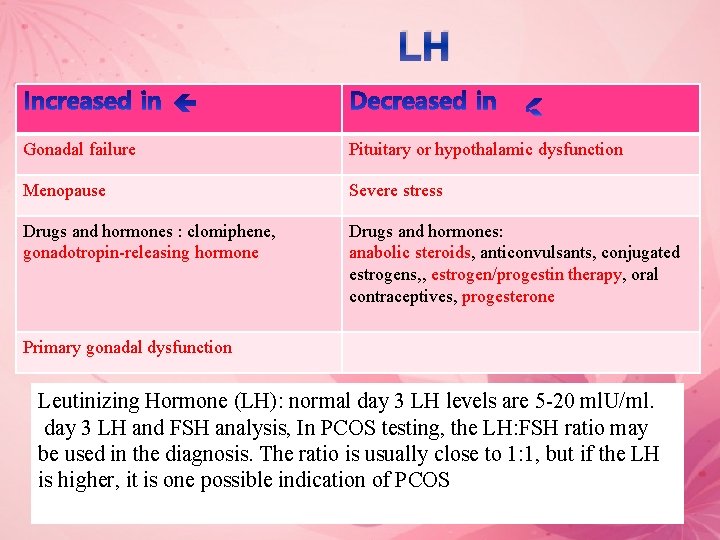
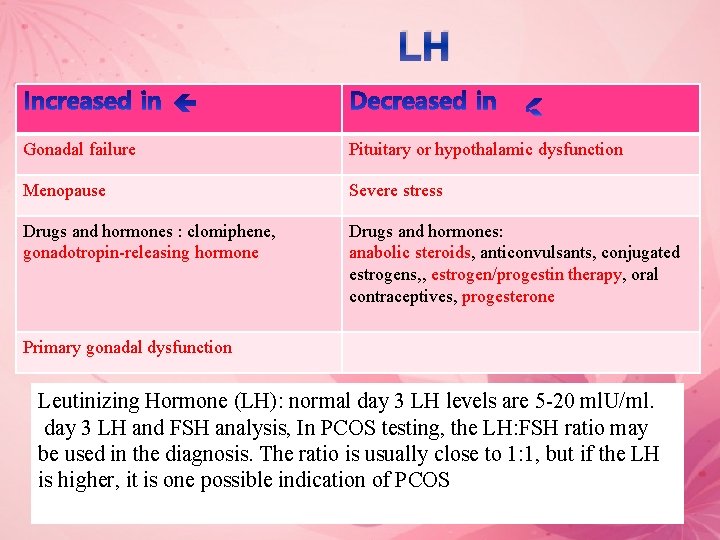
LH Gonadal failure Pituitary or hypothalamic dysfunction Menopause Severe stress Drugs and hormones : clomiphene, gonadotropin-releasing hormone Drugs and hormones: anabolic steroids, anticonvulsants, conjugated estrogens, , estrogen/progestin therapy, oral contraceptives, progesterone Primary gonadal dysfunction Leutinizing Hormone (LH): normal day 3 LH levels are 5 -20 ml. U/ml. day 3 LH and FSH analysis, In PCOS testing, the LH: FSH ratio may be used in the diagnosis. The ratio is usually close to 1: 1, but if the LH is higher, it is one possible indication of PCOS

Hormones time of collection ØFSH, At 5, 6, 7 days of cycle ØLH At 13, 14 days of cycle ØEstradiol At 9, 10, 11 days of cycle Øprogesterone 21 of cycle
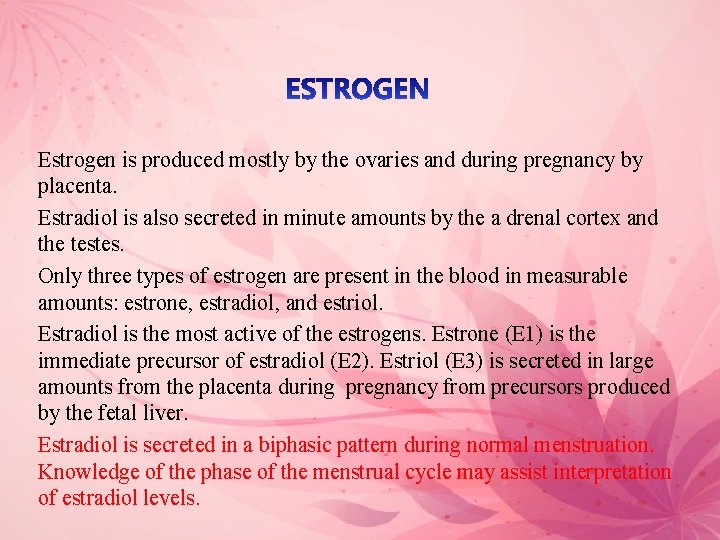
Estrogen is produced mostly by the ovaries and during pregnancy by placenta. Estradiol is also secreted in minute amounts by the a drenal cortex and the testes. Only three types of estrogen are present in the blood in measurable amounts: estrone, estradiol, and estriol. Estradiol is the most active of the estrogens. Estrone (E 1) is the immediate precursor of estradiol (E 2). Estriol (E 3) is secreted in large amounts from the placenta during pregnancy from precursors produced by the fetal liver. Estradiol is secreted in a biphasic pattern during normal menstruation. Knowledge of the phase of the menstrual cycle may assist interpretation of estradiol levels.
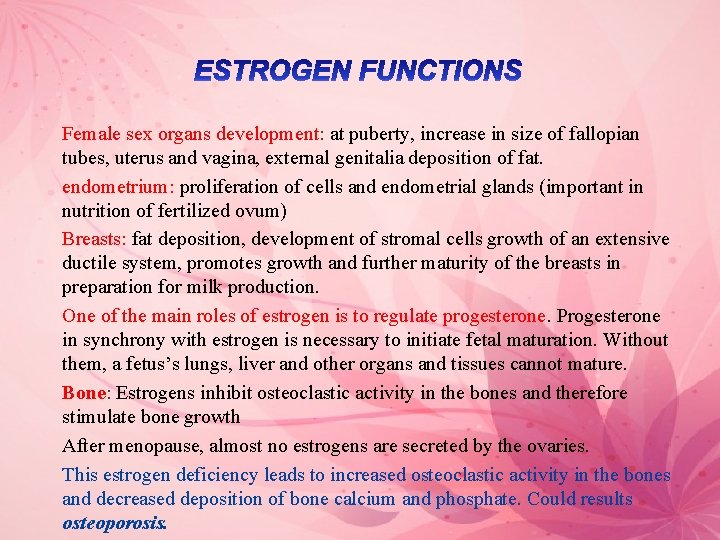
Female sex organs development: at puberty, increase in size of fallopian tubes, uterus and vagina, external genitalia deposition of fat. endometrium: proliferation of cells and endometrial glands (important in nutrition of fertilized ovum) Breasts: fat deposition, development of stromal cells growth of an extensive ductile system, promotes growth and further maturity of the breasts in preparation for milk production. One of the main roles of estrogen is to regulate progesterone. Progesterone in synchrony with estrogen is necessary to initiate fetal maturation. Without them, a fetus’s lungs, liver and other organs and tissues cannot mature. Bone: Estrogens inhibit osteoclastic activity in the bones and therefore stimulate bone growth After menopause, almost no estrogens are secreted by the ovaries. This estrogen deficiency leads to increased osteoclastic activity in the bones and decreased deposition of bone calcium and phosphate. Could results osteoporosis.
• Progesterone is a female sex hormone, is primarily involved in the preparation of the uterus for pregnancy and its maintenance during pregnancy. • The placenta begins producing progesterone at 12 weeks of gestation. • Levels of progesterone in twin pregnancy are higher than in a single pregnancy. • Progesterone level peaks in the midluteal phase of the menstrual cycle produced by the corpus luteum and levels are low during the follicular (first) phase of the menstrual cycle “corpus luteum regresses, progesterone levels fall. • After ovulation, progesterone levels rise for 4 to 5 days, the lining of the uterus has thickened to prepare for the fertilized egg. If no conception occurs, the uterine lining, as well as blood, will be shed, the shedding of an unfertilized egg and the uterine wall “Menstruation
Ø Progesterone function is to: • Prepare the uterus for pregnancy and the breasts for lactation. • Stimulate uterine glands secretion • Growth of the breast alveoli • Inhibition of uterine muscles contractions during pregnancy to prevent expulsion of the fetus Ø Uses: • To confirm that ovulation has occurred and to assess the functioning of the corpus luteum. • Serial measurements can be performed to help determine the day of ovulation. • Monitor patients receiving progesterone-replacement therapy • Assist the diagnosis of luteal phase defects (performed in conjunction with endometrial biopsy) • Evaluate patients at risk for early or spontaneous abortion • Identify patients at risk for ectopic pregnancy “along with h. CG” and assessment of corpus luteum function


The End
 Www.allppt.com free
Www.allppt.com free Sex sex sex
Sex sex sex Sex snv
Sex snv Sex sex sex
Sex sex sex Sex sex sex
Sex sex sex Secondary sexual characters
Secondary sexual characters Allppt.com.
Allppt.com. Allppt free powerpoint
Allppt free powerpoint Allppt.com free
Allppt.com free Allppt free
Allppt free Allppt.com _ free powerpoint templates diagrams and charts
Allppt.com _ free powerpoint templates diagrams and charts Dậy thổi cơm mua thịt cá
Dậy thổi cơm mua thịt cá Cơm
Cơm Octopomine
Octopomine Sex
Sex Sex determination in drosophilla
Sex determination in drosophilla Sex determination and sex linkage
Sex determination and sex linkage Once a sex offender always a sex offender
Once a sex offender always a sex offender Islamic presentation template
Islamic presentation template Free call to action templates
Free call to action templates Free real estate presentation templates
Free real estate presentation templates Http://www.free-powerpoint-templates-design.com
Http://www.free-powerpoint-templates-design.com Elearning powerpoint templates
Elearning powerpoint templates Powerpoint templates free
Powerpoint templates free Http://www.free-powerpoint-templates-design.com
Http://www.free-powerpoint-templates-design.com Power pointtemplates
Power pointtemplates Allppt.com free
Allppt.com free Free ppt
Free ppt Ppt pengantar akuntansi 2
Ppt pengantar akuntansi 2 Template ppt magang
Template ppt magang The real lesson 21
The real lesson 21 Informsu
Informsu Point point power
Point point power Free sex phohe chat 48071 maine
Free sex phohe chat 48071 maine Gibbs free energy of formation
Gibbs free energy of formation Gibbs energy and equilibrium
Gibbs energy and equilibrium Ln ksp vs 1/t
Ln ksp vs 1/t