SEIZURES IN CHILDREN Rashmi Kumar Prof Head Pediatrics




- Slides: 47
SEIZURES IN CHILDREN Rashmi Kumar Prof & Head, Pediatrics King George Medical University Lucknow
• • • Prevalence Definition Conditions that mimic seizures Pathophysiology Etiology Age wise etiology Classification Assessment Febrile seizures Management
SEIZURES • One of the most common life threatening events in childhood, more than adults • Paroxysmal electrical activity in brain --> motor/sensory/autonomic disturbance with /without alteration of consciousness • Convulsion – seizure with motor activity • Epilepsy – recurrent (2 or more) unprovoked seizures beyond newborn period 0. 5% 5%
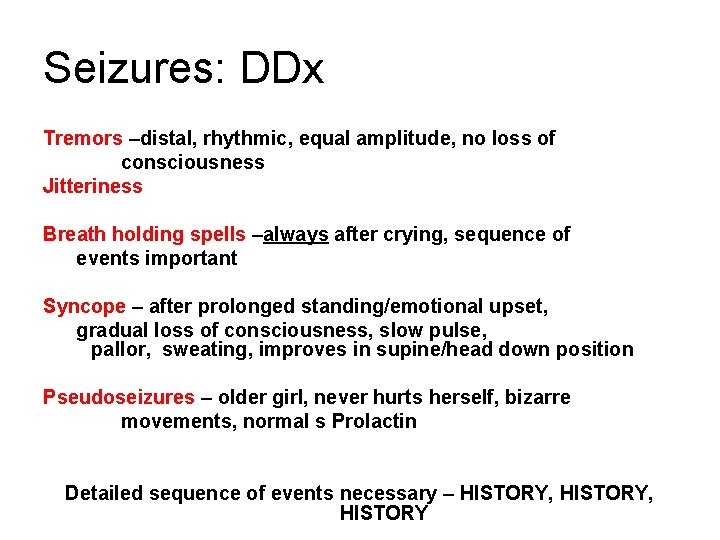
Seizures: DDx Tremors –distal, rhythmic, equal amplitude, no loss of consciousness Jitteriness Breath holding spells –always after crying, sequence of events important Syncope – after prolonged standing/emotional upset, gradual loss of consciousness, slow pulse, pallor, sweating, improves in supine/head down position Pseudoseizures – older girl, never hurts herself, bizarre movements, normal s Prolactin Detailed sequence of events necessary – HISTORY, HISTORY
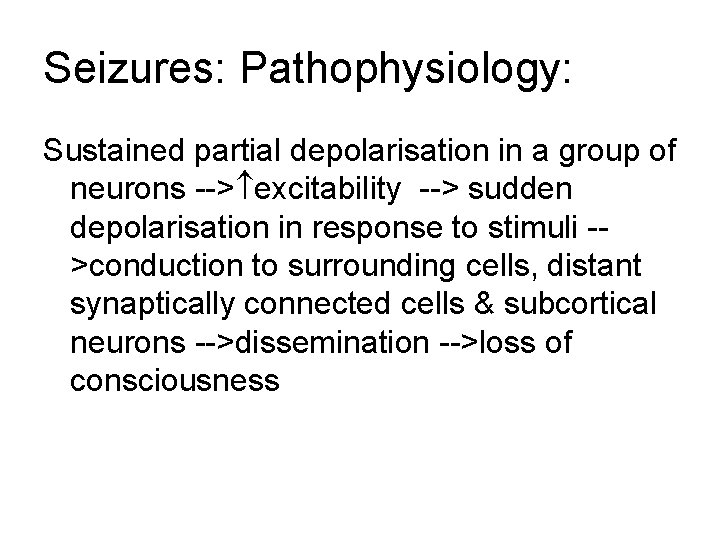
Seizures: Pathophysiology: Sustained partial depolarisation in a group of neurons --> excitability --> sudden depolarisation in response to stimuli ->conduction to surrounding cells, distant synaptically connected cells & subcortical neurons -->dissemination -->loss of consciousness
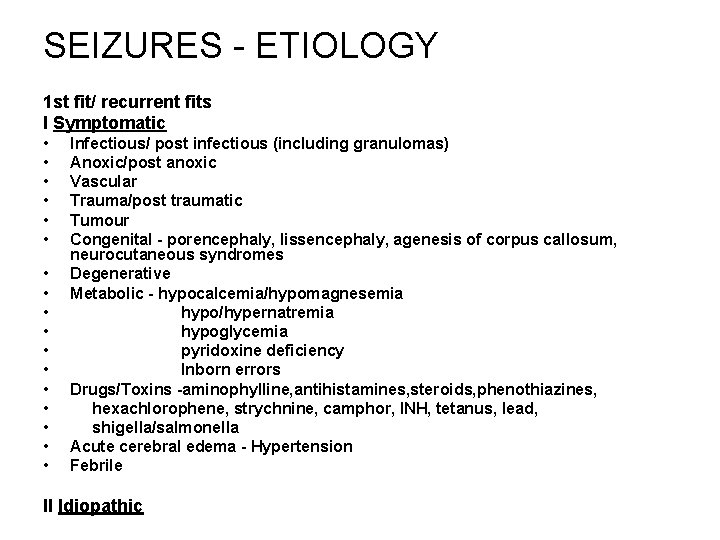
SEIZURES - ETIOLOGY 1 st fit/ recurrent fits I Symptomatic • • • • • Infectious/ post infectious (including granulomas) Anoxic/post anoxic Vascular Trauma/post traumatic Tumour Congenital - porencephaly, lissencephaly, agenesis of corpus callosum, neurocutaneous syndromes Degenerative Metabolic - hypocalcemia/hypomagnesemia hypo/hypernatremia hypoglycemia pyridoxine deficiency Inborn errors Drugs/Toxins -aminophylline, antihistamines, steroids, phenothiazines, hexachlorophene, strychnine, camphor, INH, tetanus, lead, shigella/salmonella Acute cerebral edema - Hypertension Febrile II Idiopathic
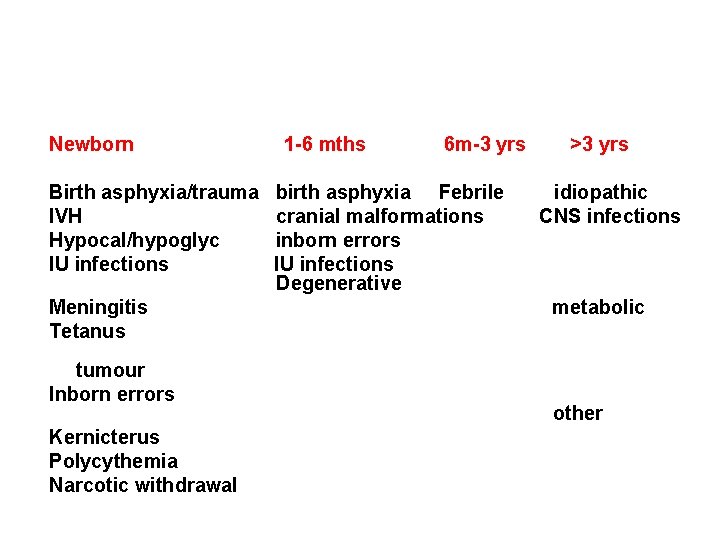
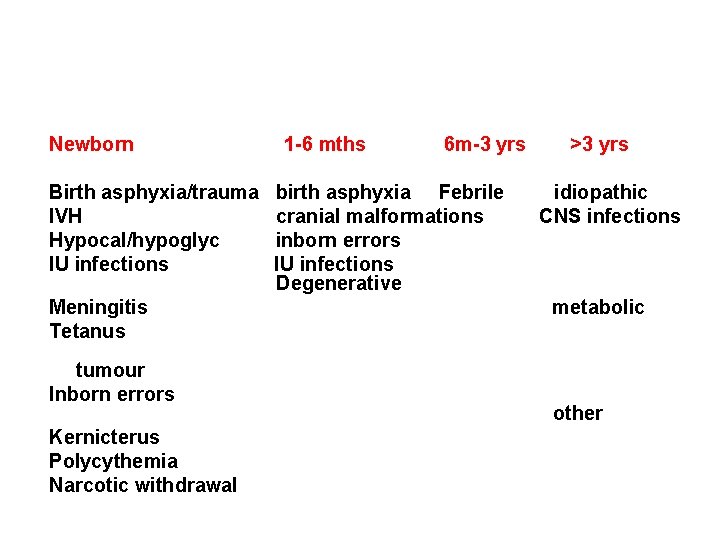
Newborn Birth asphyxia/trauma IVH Hypocal/hypoglyc IU infections Meningitis Tetanus tumour Inborn errors Kernicterus Polycythemia Narcotic withdrawal 1 -6 mths 6 m-3 yrs birth asphyxia Febrile cranial malformations inborn errors IU infections Degenerative >3 yrs idiopathic CNS infections metabolic other
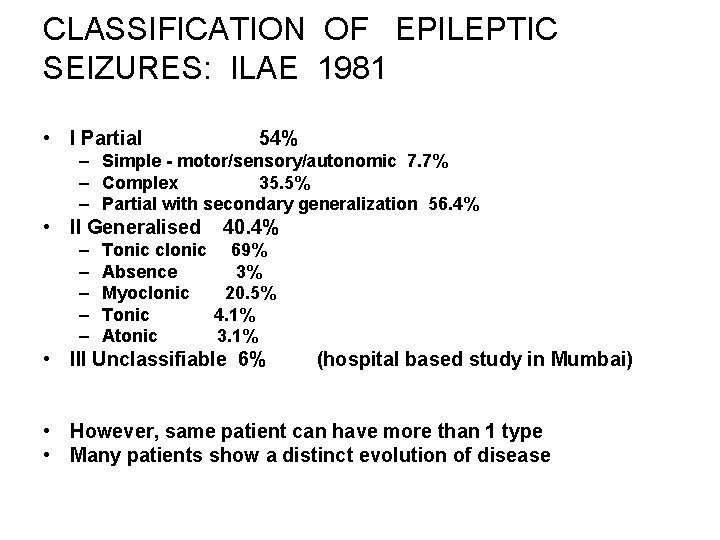
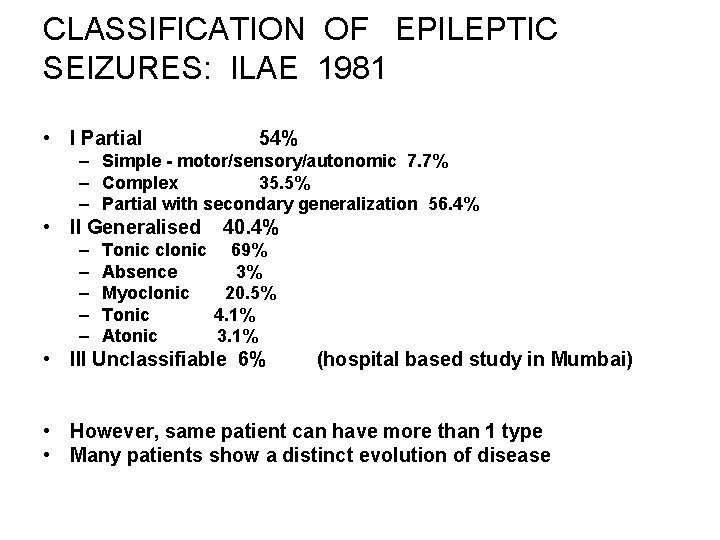
CLASSIFICATION OF EPILEPTIC SEIZURES: ILAE 1981 • I Partial 54% – Simple - motor/sensory/autonomic 7. 7% – Complex 35. 5% – Partial with secondary generalization 56. 4% • II Generalised – – – 40. 4% Tonic clonic 69% Absence 3% Myoclonic 20. 5% Tonic 4. 1% Atonic 3. 1% • III Unclassifiable 6% (hospital based study in Mumbai) • However, same patient can have more than 1 type • Many patients show a distinct evolution of disease
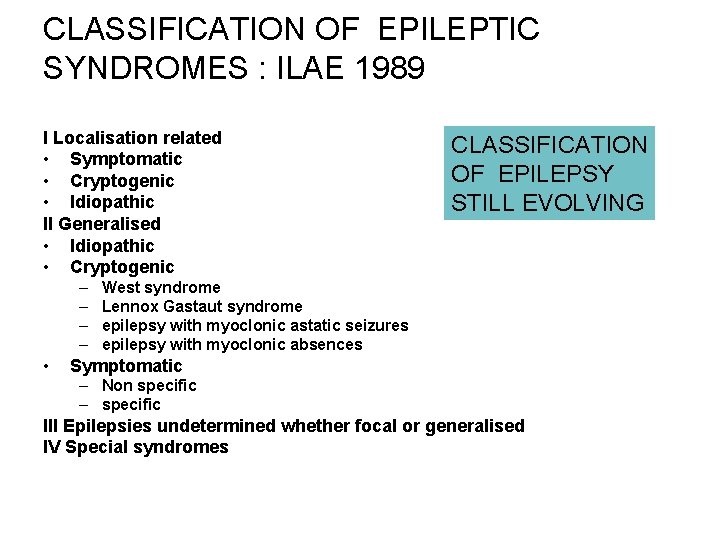
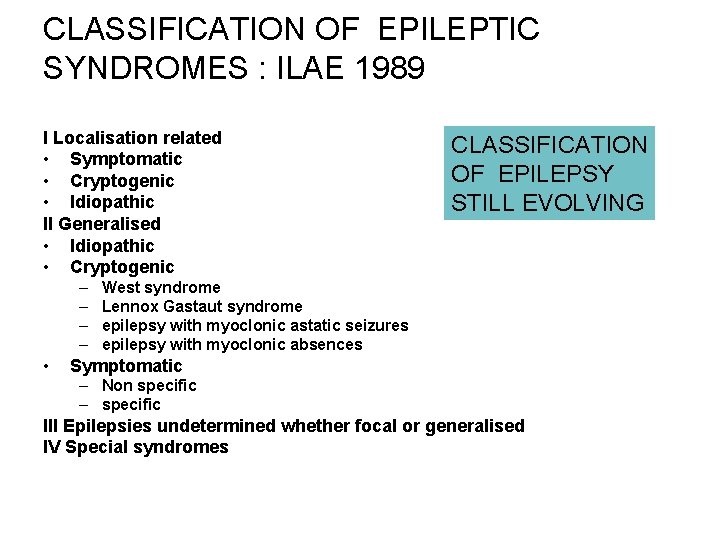
CLASSIFICATION OF EPILEPTIC SYNDROMES : ILAE 1989 I Localisation related • Symptomatic • Cryptogenic • Idiopathic II Generalised • Idiopathic • Cryptogenic – – • CLASSIFICATION OF EPILEPSY STILL EVOLVING West syndrome Lennox Gastaut syndrome epilepsy with myoclonic astatic seizures epilepsy with myoclonic absences Symptomatic – Non specific – specific III Epilepsies undetermined whether focal or generalised IV Special syndromes
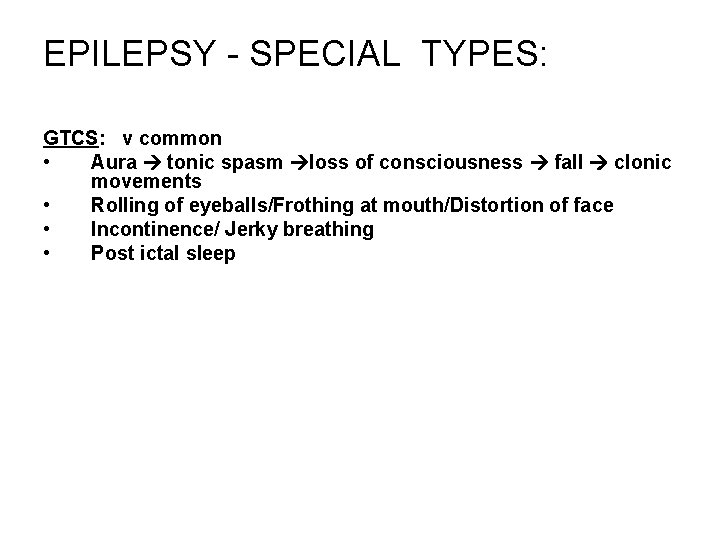
EPILEPSY - SPECIAL TYPES: GTCS: v common • Aura tonic spasm loss of consciousness fall clonic movements • Rolling of eyeballs/Frothing at mouth/Distortion of face • Incontinence/ Jerky breathing • Post ictal sleep
Absence epilepsy • • • 2 -4% of childhood idiopathic epilepsy Girls 3 -7 yrs, normal IQ Transient loss of consciousness for few secs No loss of tone Ppted by hyperventilation - • • • Treatment – Ethosuximide, valproate May develop GTCS EEG - 3/sec spike & wave activity

EPILEPSY - SPECIAL TYPES: Infantile spasms: Onset in 1 st year • Sudden flexion/extension in series esp on awakening • Upto 100 times /day • 60% secondary, 30% cryptogenic • Treatment - ACTH/steroids/ vigabatrin • Associated with mental regression • EEG - hypsarrhythmic • May develop GTCS Lennox Gastaut: • 1 -8 yrs, • tonic/absence type • EEG - diffuse 2 Hz spike-waves • Very difficult to control

EPILEPSY - SPECIAL TYPES: Psychomotor (Temporal lobe) seizures: Complex partial seizures with origin in temporal lobe. • Purposeful but inappropriate acts 'automatisms' • Associated with behavioral problems • Difficult to diagnose or treat. Benign epilepsy with centrotemporal spikes: Partial, idiopathic, • orofacial/hemifacial, 3 -13 yrs, often during sleep. Easy to control Myoclonic: heterogenous, multiple causes Juvenile myoclonic: myoclonic jerks esp after awakening • EEG - 4 -6 Hz polyspike, photosensitivity, GTCS may occur • Good response to Valproate
FEBRILE SEIZURES: • • • 2 -4% of children 3 m - 5 yr age Assn with fever due to extracranial infection Generalised, Short lasting, only one sz per illness No mental/neurological/EEG abnormality Typical vs Atypical (complex) Focal Prolonged >1 seizure during illness 1/3 have at least 1 recurrence 1/6 have multiple recurrences Risk of epilepsy: – Fh/o epilepsy – Atypical – Abnormal neurologic/mental status
Febrile Seizures: Management • • • Exclude CNS infection Control fever Look for & treat cause of fever Rectal diazepam Explain to parents, reassure If multiple - intermittent oral diazepam by 80% • If high risk for epilepsy long term phenobarb/valproate.
Seizures: ASSESSMENT History: • • • 1 st seizure/ recurrent seizures Fever Precipitating factors – diarrhea/ vomiting/ drug/ toxin/ metabolic Headache/vomiting/visual loss Duration Age at onset No of attacks Frequency / , change in seizure type, last seizure when? Exact description – – – – • • Aura partial/generalised onset Loss of consciousness Tonic/clonic phase Associated events - bed wetting/fall/tongue bite Duration Post ictal Precipitating factors Diurnal Family history Antecedant events - trauma/CNS infection/asphyxia Personality change/intellectual deterioration Failure to thrive Developmental milestones Treatment
Seizures: ASSESSMENT Examination: • BP • Head circumference • Skin lesions • Facial features • Organomegaly • Fundus • Meningeal signs • Neurological deficit • Development
Seizures: Investigations • • • • If features of CNS infection - CSF examination Glucose, Ca, Mg - low yield Skull Xray - calcification/ ICT - low yield EEG: Always diagnostic during a seizure Interictal record : normal in 40 -50% of epileptics (spikes/sharp waves & spikes –slow wave complexes) yield with sleep, sleep deprivation, hyperventilation, photic stimulation 2 -10% normal population may have epileptic changes EEG indicated in all cases of epilepsy for: -confirmation of diagnosis & syndrome -type of seizures - absence vs temporal lobe, primary generalised vs secondarily generalised -presence of underlying lesion/ idiopathic vs symptomatic -follow up -before withdrawal of AEDs -localisation of focus before surgery Video EEG
Seizures: Imaging - CT/MRI Has revolutionised the management of epilepsy Indications: focal features on exam, EEG Features of ICT Intractable However, now indicated in every case with unknown cause Not necessary in febrile/absence/BETS/ JME etc. Western studies - 30% abnormal (30 -50% of focal) -only 3% treatable Indian studies: Very high prevalence of granuloma like lesions –recent onset partial seizures in child/young adult 40% abn even after 1 st seizure indicated in every case


MCQ • The following are features of benign (typical) febrile seizures except: • They are short lasting • They are always generalised • They only occur within 4 hours of fever onset • They do not recur in the same febrile illness
The typical EEG pattern in absence epilepsy is: • Intermittent spike and slow waves • Hypsarrythmia • Burst suppression • 3 per second spike and waves
The following is true about absence epilepsy • It occurs more commonly in boys • There is loss of tone • It is precipitated by hyperventilation • Imaging is usually abnormal
Definition of epilepsy includes: • • At least 3 seizures EEG is abnormal Imaging is abnormal Beyond neonatal period
The following is true about breath holding spells: • • It is usually preceded by crying Child is always blue There is no loss of consciousness EEG may show spikes
The following is true about infantile spasms except: • • They occur in clusters They may appear like ‘startling’ They usually occur during sleep They are also called ‘salaam attacks’
West syndrome usually has the following features except: • • Infantile spasms Onset in newborn period Hypsarrythmia on EEG Psychomotor retardation or regression
Imaging in seizures is not indicated in: • • Generalised tonic clonic seizures Absence seizures Temporal lobe seizures Infantile spasms
Prevention of febrile seizures can be achieved by: • • Intermittent phenobarb Long term phenytoin Intermittent diazepam Long term carbamazepine
Emergency dose of IV diazepam for seizure control is: • • 1 mg/kg 0. 5 mg/kg 0. 1 mg/kg 0. 3 mg/kg
Seizures - Management • • • I Management of acute attack: Calm down Head down lateral position Prevent hurt If does'nt stop convulsing in 3 -5 min, Inj Diazepam 0. 3 mg/kg slow iv bolus Maybe repeated after 20 min Effect lasts 0. 5 -3 hrs SE- hypotension, respiratory depression, secretions • or • Rectal diazepam 0. 5 mg/kg dose/ nasal midzolam 0. 2 mg/kg/dose
Domiciliary Mx • Rectal Diazepam 0. 5 mg/kg • Intranasal midzolam 0. 2 mg/kg
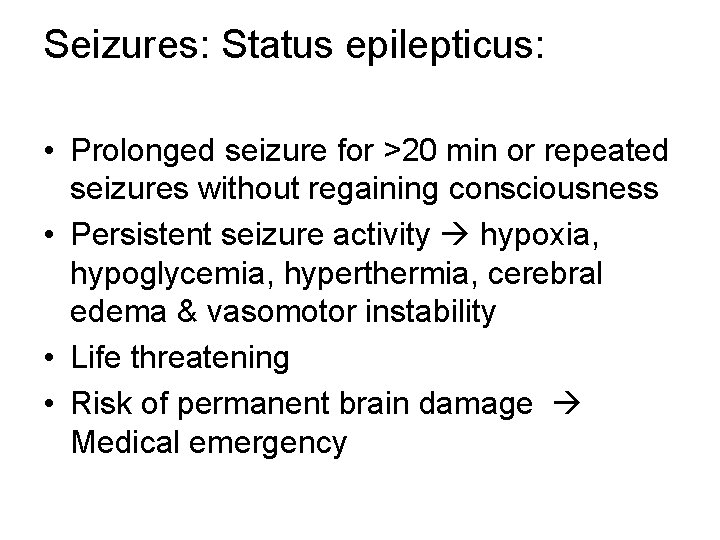
Seizures: Status epilepticus: • Prolonged seizure for >20 min or repeated seizures without regaining consciousness • Persistent seizure activity hypoxia, hypoglycemia, hyperthermia, cerebral edema & vasomotor instability • Life threatening • Risk of permanent brain damage Medical emergency
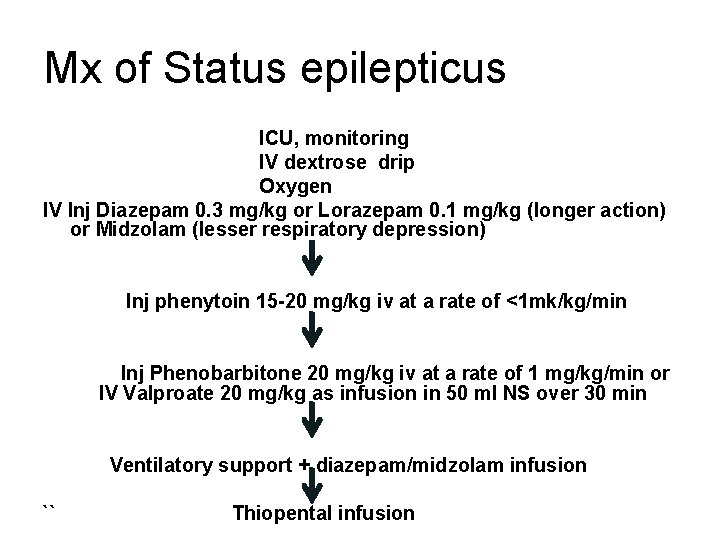
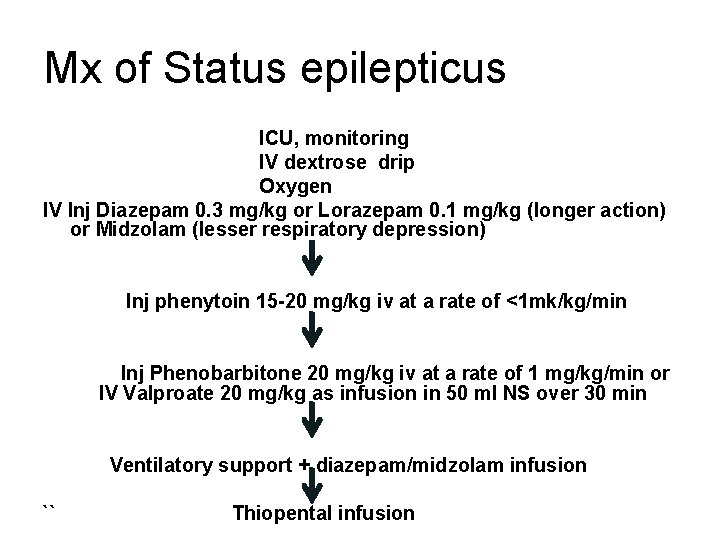
Mx of Status epilepticus ICU, monitoring IV dextrose drip Oxygen IV Inj Diazepam 0. 3 mg/kg or Lorazepam 0. 1 mg/kg (longer action) or Midzolam (lesser respiratory depression) Inj phenytoin 15 -20 mg/kg iv at a rate of <1 mk/kg/min Inj Phenobarbitone 20 mg/kg iv at a rate of 1 mg/kg/min or IV Valproate 20 mg/kg as infusion in 50 ml NS over 30 min Ventilatory support + diazepam/midzolam infusion `` Thiopental infusion
LONG TERM MANAGEMENT OF EPILEPSY: I General advice: • As normal a life style as possible • No swimming/cycling on road/driving • Inform teacher • First aid • Seizure dairy • Regularity
LONG TERM MANAGEMENT OF EPILEPSY: Drugs: • When to start? If 2 or more seizures within a 12 month period • Monotherapy: • Start at lower limit & build up gradually till toxicity/control • If no effect at maximum dose, taper off while introducing 2 nd drug • 4 first line drugs - Carbamazepine, phenytoin, valproate and phenobarbitone • No drug completely safe • 70% can be controlled
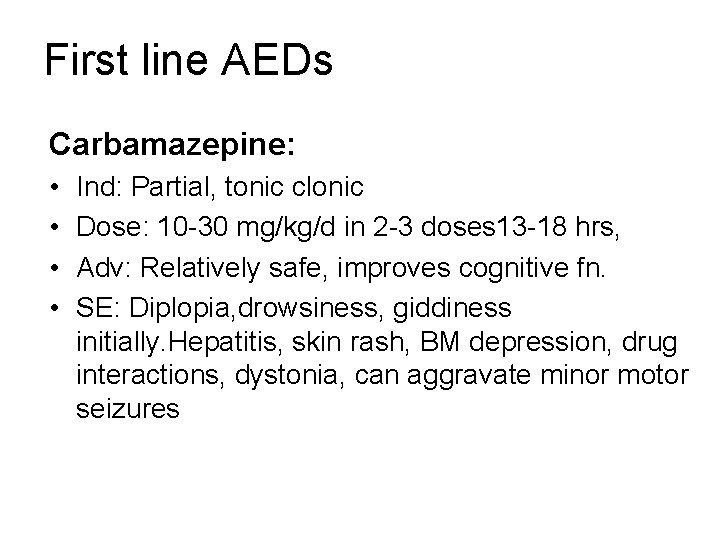
First line AEDs Carbamazepine: • • Ind: Partial, tonic clonic Dose: 10 -30 mg/kg/d in 2 -3 doses 13 -18 hrs, Adv: Relatively safe, improves cognitive fn. SE: Diplopia, drowsiness, giddiness initially. Hepatitis, skin rash, BM depression, drug interactions, dystonia, can aggravate minor motor seizures
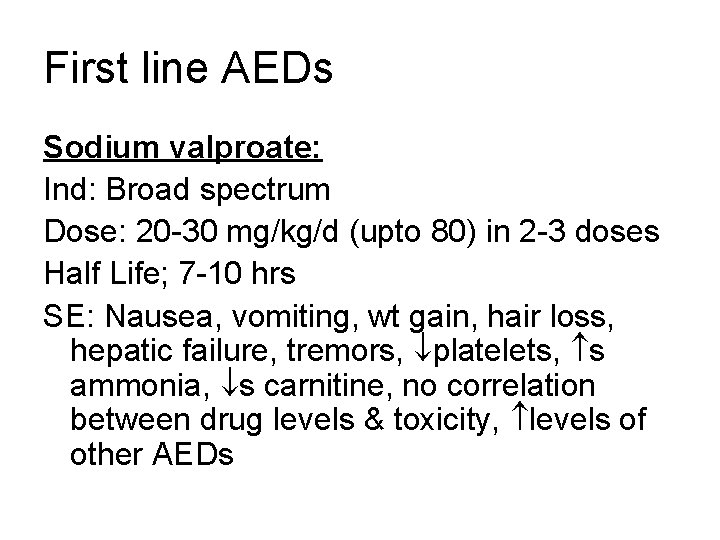
First line AEDs Sodium valproate: Ind: Broad spectrum Dose: 20 -30 mg/kg/d (upto 80) in 2 -3 doses Half Life; 7 -10 hrs SE: Nausea, vomiting, wt gain, hair loss, hepatic failure, tremors, platelets, s ammonia, s carnitine, no correlation between drug levels & toxicity, levels of other AEDs
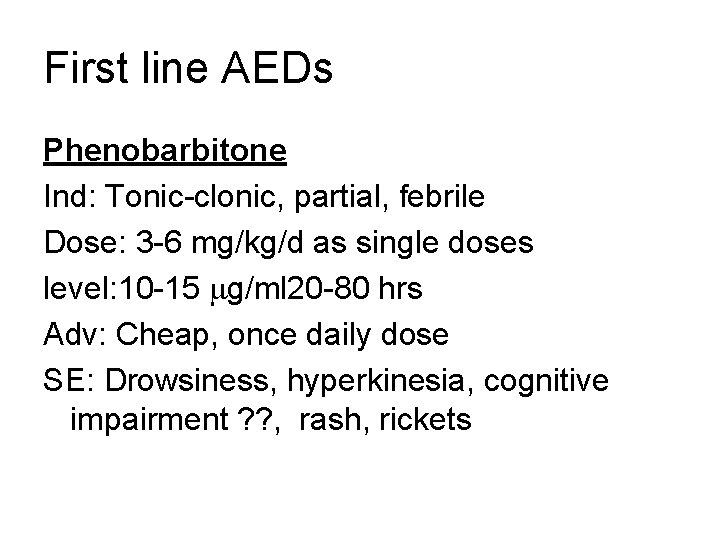
First line AEDs Phenobarbitone Ind: Tonic-clonic, partial, febrile Dose: 3 -6 mg/kg/d as single doses level: 10 -15 g/ml 20 -80 hrs Adv: Cheap, once daily dose SE: Drowsiness, hyperkinesia, cognitive impairment ? ? , rash, rickets
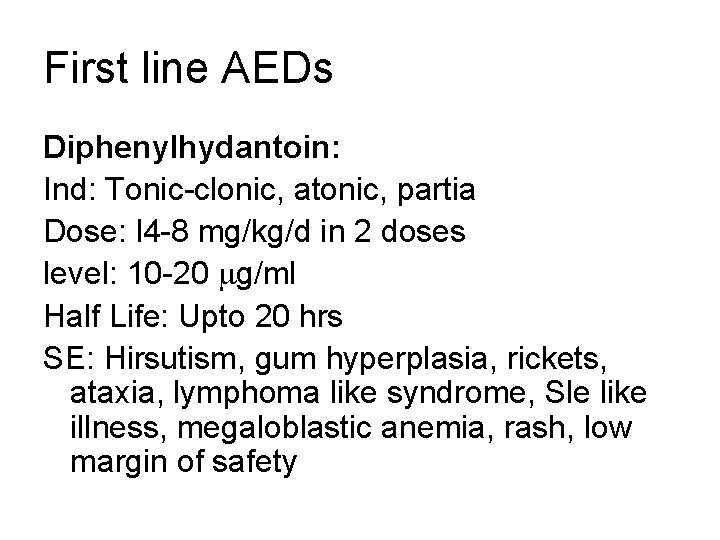
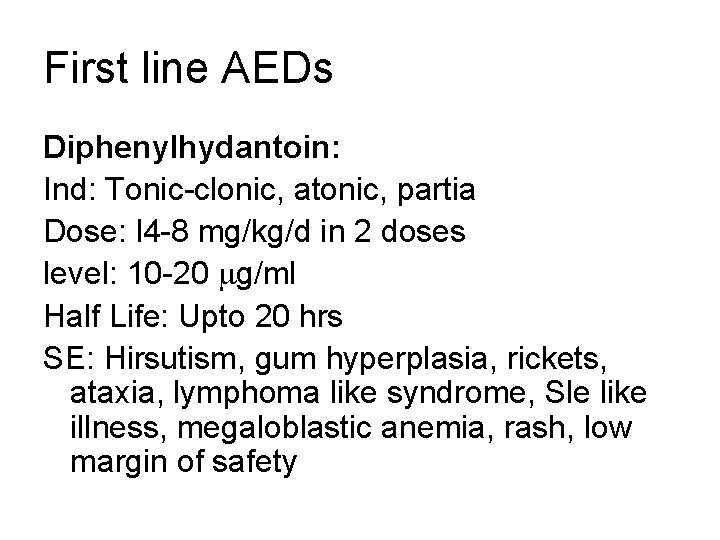
First line AEDs Diphenylhydantoin: Ind: Tonic-clonic, atonic, partia Dose: l 4 -8 mg/kg/d in 2 doses level: 10 -20 g/ml Half Life: Upto 20 hrs SE: Hirsutism, gum hyperplasia, rickets, ataxia, lymphoma like syndrome, Sle like illness, megaloblastic anemia, rash, low margin of safety
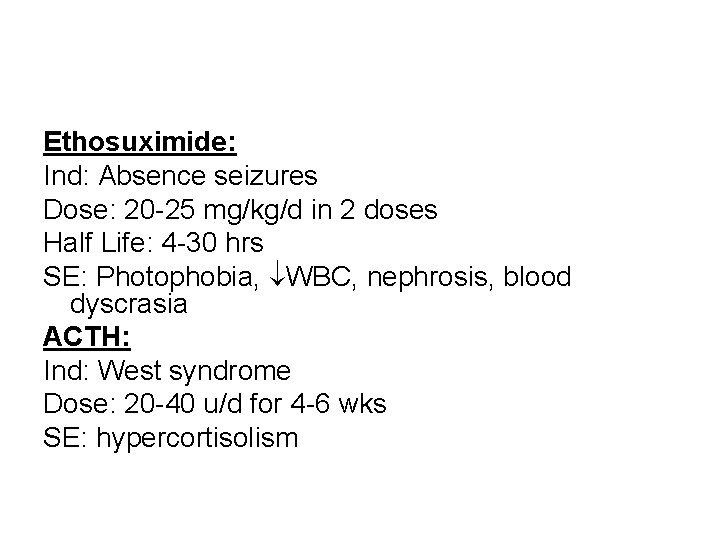
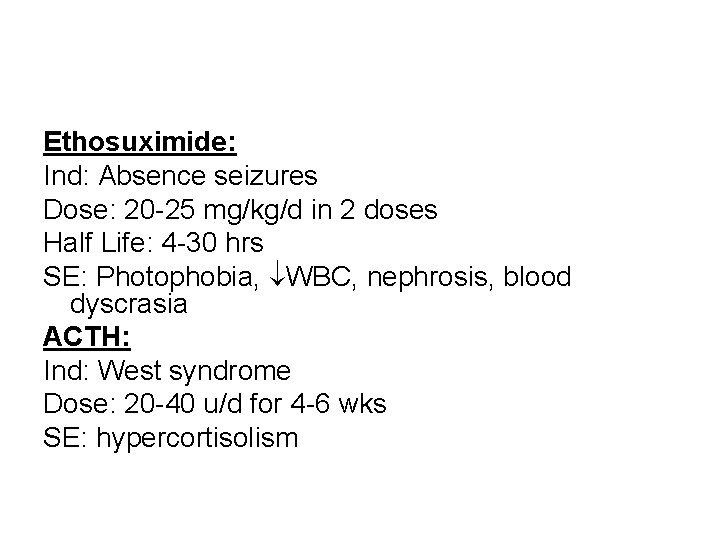
Ethosuximide: Ind: Absence seizures Dose: 20 -25 mg/kg/d in 2 doses Half Life: 4 -30 hrs SE: Photophobia, WBC, nephrosis, blood dyscrasia ACTH: Ind: West syndrome Dose: 20 -40 u/d for 4 -6 wks SE: hypercortisolism
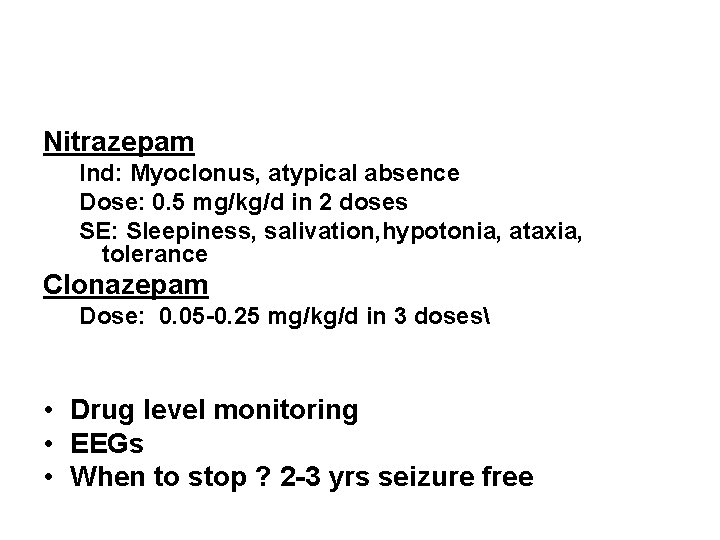
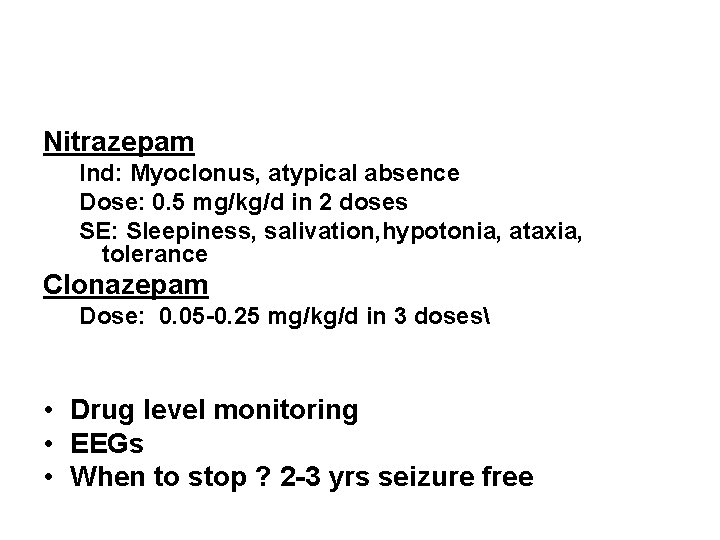
Nitrazepam Ind: Myoclonus, atypical absence Dose: 0. 5 mg/kg/d in 2 doses SE: Sleepiness, salivation, hypotonia, ataxia, tolerance Clonazepam Dose: 0. 05 -0. 25 mg/kg/d in 3 doses • Drug level monitoring • EEGs • When to stop ? 2 -3 yrs seizure free
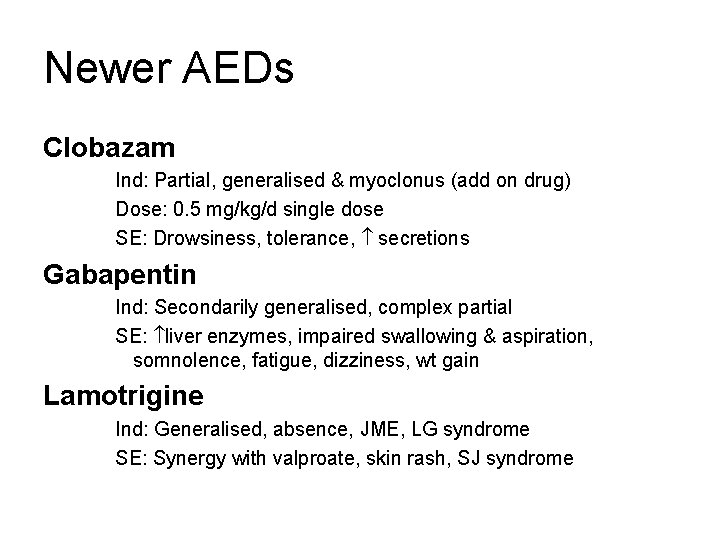
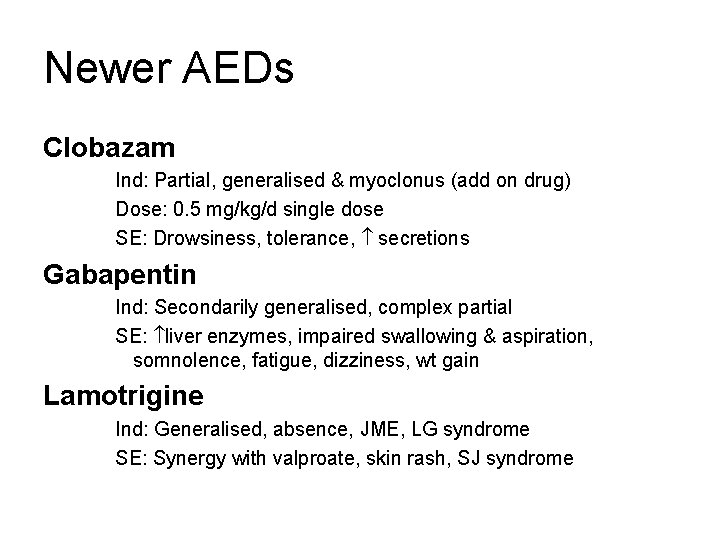
Newer AEDs Clobazam Ind: Partial, generalised & myoclonus (add on drug) Dose: 0. 5 mg/kg/d single dose SE: Drowsiness, tolerance, secretions Gabapentin Ind: Secondarily generalised, complex partial SE: liver enzymes, impaired swallowing & aspiration, somnolence, fatigue, dizziness, wt gain Lamotrigine Ind: Generalised, absence, JME, LG syndrome SE: Synergy with valproate, skin rash, SJ syndrome
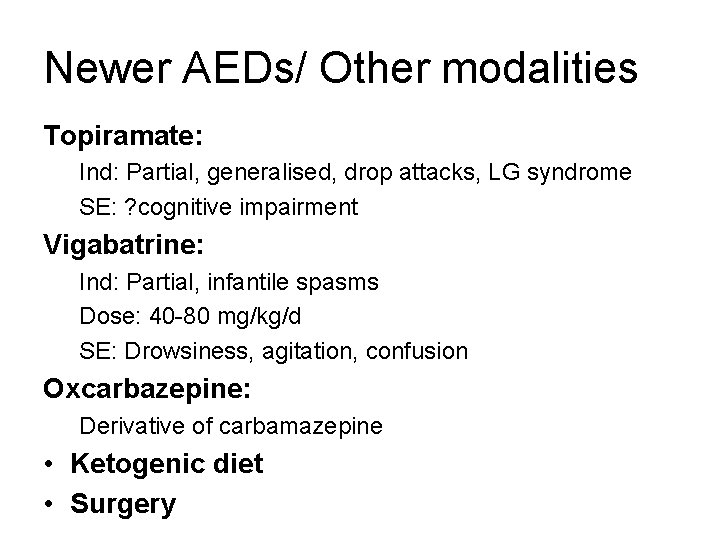
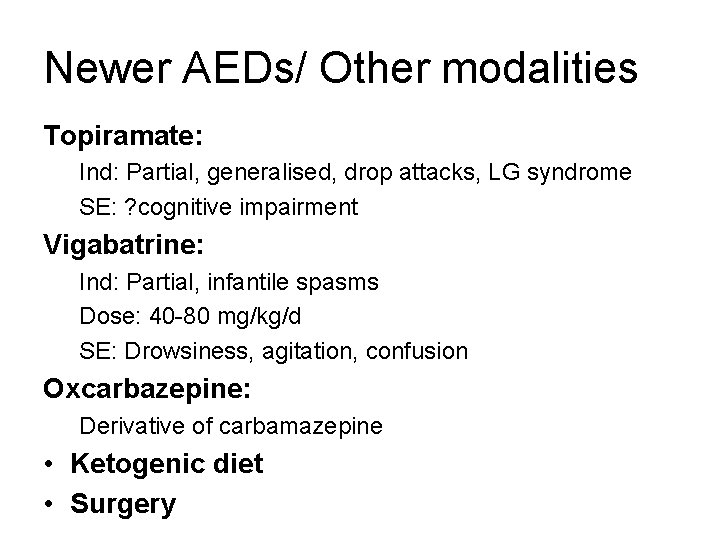
Newer AEDs/ Other modalities Topiramate: Ind: Partial, generalised, drop attacks, LG syndrome SE: ? cognitive impairment Vigabatrine: Ind: Partial, infantile spasms Dose: 40 -80 mg/kg/d SE: Drowsiness, agitation, confusion Oxcarbazepine: Derivative of carbamazepine • Ketogenic diet • Surgery
 Cholegogue
Cholegogue Rashmi halker singh
Rashmi halker singh Rashmi kohli
Rashmi kohli Dr rashmi saxena
Dr rashmi saxena Palmar crease pallor
Palmar crease pallor Rashmi choudhary presenter
Rashmi choudhary presenter Dhuryodhana
Dhuryodhana Dr rashmi choudhary
Dr rashmi choudhary Non epileptic seizures
Non epileptic seizures Epilepsy
Epilepsy Basic mechanisms underlying seizures and epilepsy
Basic mechanisms underlying seizures and epilepsy Seizures
Seizures Pediatric seizures
Pediatric seizures Simple febrile seizure
Simple febrile seizure Psychomotor seizures
Psychomotor seizures Pimidone
Pimidone Ptsd seizures
Ptsd seizures Simple partial seizures vs complex
Simple partial seizures vs complex Abdominal ultrasound scan glasgow
Abdominal ultrasound scan glasgow Psychomotor seizures
Psychomotor seizures Shaking vs seizure
Shaking vs seizure Classification of anticonvulsant drug
Classification of anticonvulsant drug What is a seizure
What is a seizure Spina bifida occulta
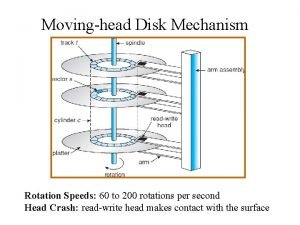
Spina bifida occulta The head of moving head disk
The head of moving head disk Positive suction head and negative suction head
Positive suction head and negative suction head 40/8 is the indexing for the divisions of
40/8 is the indexing for the divisions of Neck part of body
Neck part of body Biceps femoris innervation
Biceps femoris innervation The attacking firm goes head-to-head with its competitor.
The attacking firm goes head-to-head with its competitor. The tone unit
The tone unit Pre-head head tonic syllable tail
Pre-head head tonic syllable tail Html tagi
Html tagi The head of moving head disk with 100 tracks
The head of moving head disk with 100 tracks Tlc pediatrics flint
Tlc pediatrics flint Newborn care definition
Newborn care definition Practical approach pediatrics
Practical approach pediatrics Duke pediatrics durham nc
Duke pediatrics durham nc N-pass pain scale
N-pass pain scale Normal vitals
Normal vitals Combivent para bebes
Combivent para bebes Lsu new orleans pediatric residency
Lsu new orleans pediatric residency Im injection sites and volumes pediatrics
Im injection sites and volumes pediatrics When administering ear drops to adults the pinna is pulled
When administering ear drops to adults the pinna is pulled Nn pediatrics
Nn pediatrics Disease xxx
Disease xxx Randall neustaedter
Randall neustaedter 11yo
11yo