Safety and quality of neuraxial analgesia Ulla Sipilinen





- Slides: 29

Safety and quality of neuraxial analgesia Ulla Sipiläinen 6. 10. 2011 HUCS Jorvi hospital
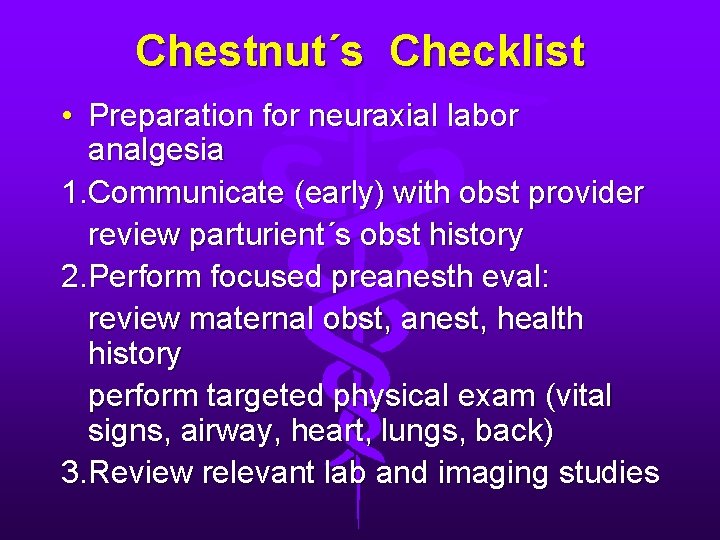
Chestnut´s Checklist • Preparation for neuraxial labor analgesia 1. Communicate (early) with obst provider review parturient´s obst history 2. Perform focused preanesth eval: review maternal obst, anest, health history perform targeted physical exam (vital signs, airway, heart, lungs, back) 3. Review relevant lab and imaging studies
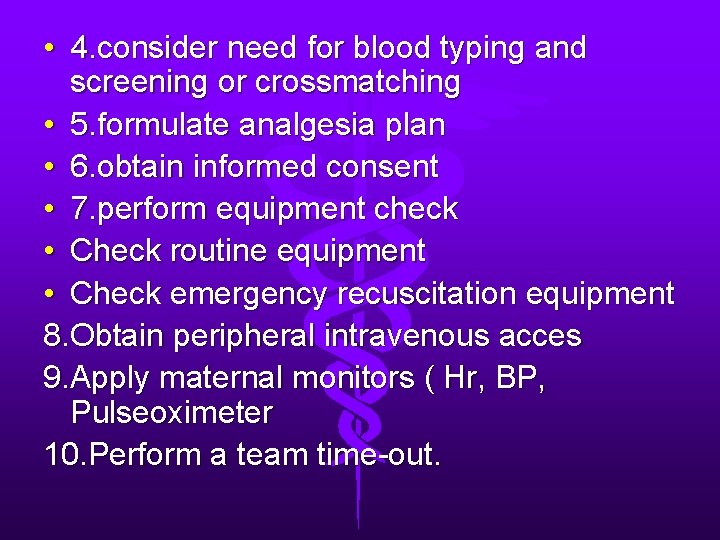
• 4. consider need for blood typing and screening or crossmatching • 5. formulate analgesia plan • 6. obtain informed consent • 7. perform equipment check • Check routine equipment • Check emergency recuscitation equipment 8. Obtain peripheral intravenous acces 9. Apply maternal monitors ( Hr, BP, Pulseoximeter 10. Perform a team time-out.

Real life checklist • Airway, airway! • Trombosytes, if symptoms of preechlampsia • Position: BMI • Allergies
maintain your skills • wet tap rate / dural puncture rate • teaching problematic • formal training programme for epidural analgesia? • simulator?

Position • sitting/ on side • weight>height-100, examp, 170 cm, 80 kg • consider sitting position
Skin preparation • • • meningitis epidural infection wear mask, sterile gloves, hat skin preparation infections are very rare st viridans
early vs late epidural • cervical dilatation less than 4 cm • with low-dose local anesthetic technique • no difference in cs rates • C. Wong 2005 and 2009
CSE vs epidural analgesia • CSE when it is really needed • multiparous patients in advanced, rapidly progressing labour • even single-shot spinal • risk of cs, obese, very painful
Air vs Saline • • saline is recommended saline with small air bubble in Finland air is most popular no differences in the incidence if PDPH between saline or air
Continous vs intermittent • pressure in loss of resistance syringe • no difference • personal preferences
Volume • high-volume • low concentration solutions • better analgesia with 20 ml epidural than 13 ml or 15 ml • if one-sided or in-adequate analgesia, volume addition ad 5 ml before replacement
PCEA, infusion, bolus? • maintaining • volume! • second dose intructions for midwife: 20 ml • PCEA best, large bolus are needed to spread widely
Intra-venous epidural • test dose!! • catether migrate into veins very easily and often • saline -injektion, aspiration • important to detect

Obese partiturent • • greater risk for cs epidural space? lumbar space? position: sitting G 18/G 27 120 mm needle CSE or epidural favour early analgesia
Taping • flexed position minimizes the distance between skin and epidural space • the catether can move up to 4 cm • leave the catether 5 -6 cm into the epidural space
Routines • • • routines protect from mistakes variation between phycisians analgesia similar undependantly from person on call
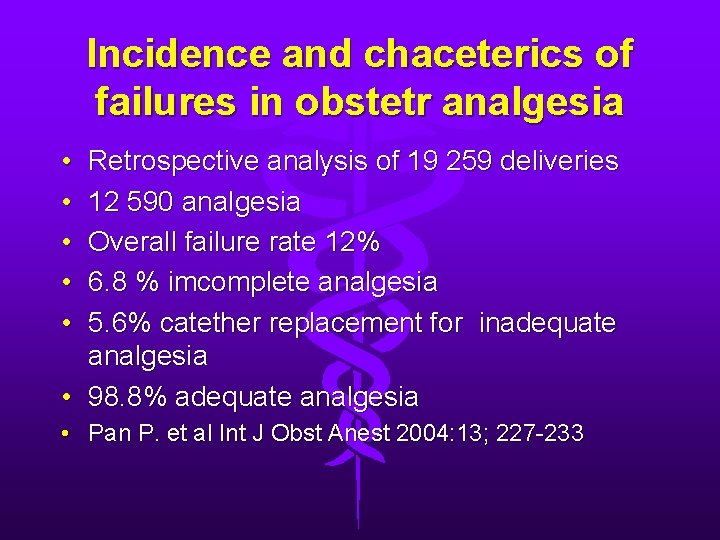
Incidence and chaceterics of failures in obstetr analgesia • • • Retrospective analysis of 19 259 deliveries 12 590 analgesia Overall failure rate 12% 6. 8 % imcomplete analgesia 5. 6% catether replacement for inadequate analgesia • 98. 8% adequate analgesia • Pan P. et al Int J Obst Anest 2004: 13; 227 -233
Inadequate analgesia • Consider other causes of pain: distended bladder, ruptured uterus • Evaluation: catether in epidural space? > not-> replacement or consider CSE • Inadequate analgesia, asymmetric block -> inject saline 5 ml • CSE has lower failure rate than epidural
Intrathecal catether • • important to detect test dose always via catether immediate analgesia total spinal anaesthesia may be disasterous
Accidental dural puncture • earlier: catether placed for 24 hrs • now: new epidural analgesia from another lumbar space and epidural blood patch if needed after 24 -36 hrs • delayd application of EBP may cause problems, be aware!
Neuraxial analgesia and neuraxial injury • common claim • indirect injury: longer second stage of labour • relaxation of pelvic muscles -> delays rotation of head • no pain-> encourage to push without changing body position
Adverse delivery outcomes • weakened desire to push • increases the risk of instrumental delivery • risk of vaginal/ perineal trauma • back pain is common
Recommendations • • instructions also for potential complications iv line, hydration hypotension anesthesia for CS fasting dural puncture
Conclusion 1 • ”Unreasonable to expect, that neuroblocade of the half lower body NOT have any affect on labour process. . ” • Chestnut`s
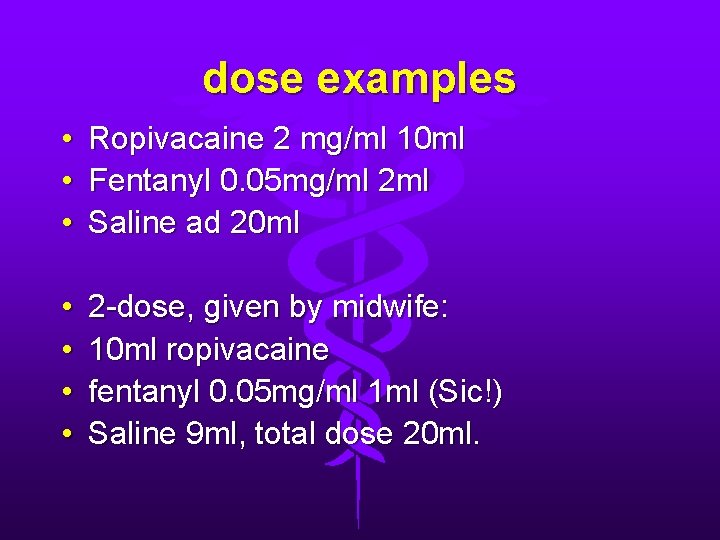
dose examples • • • Ropivacaine 2 mg/ml 10 ml Fentanyl 0. 05 mg/ml 2 ml Saline ad 20 ml • • 2 -dose, given by midwife: 10 ml ropivacaine fentanyl 0. 05 mg/ml 1 ml (Sic!) Saline 9 ml, total dose 20 ml.
dose examples • • CSE: Bupivacain 2. 5 mg Fentanyl 25 mcg saline ad 2 ml
Conclusion • Instructions for own hospital • Analgesia should be given early enough • Does not increase cs rate

Thank you!
 Analgesia sistemica
Analgesia sistemica Elastomero morfina effetti collaterali
Elastomero morfina effetti collaterali Quality control and quality assurance
Quality control and quality assurance Concept of quality assurance
Concept of quality assurance Megan childers
Megan childers Chapter 27 patient safety and quality
Chapter 27 patient safety and quality Safety quality productivity
Safety quality productivity Quality and safety education for nurses
Quality and safety education for nurses What is qsen
What is qsen Ndis quality safety and you
Ndis quality safety and you Food quality importance
Food quality importance Patient safety and quality care movement
Patient safety and quality care movement Qsen ksa
Qsen ksa Blood safety and quality regulations
Blood safety and quality regulations Pmp quality management
Pmp quality management Pmbok quality assurance vs quality control
Pmbok quality assurance vs quality control Quality assurance model in nursing
Quality assurance model in nursing Quality improvement vs quality assurance
Quality improvement vs quality assurance Tqm guru
Tqm guru Crosby quality is free
Crosby quality is free What is tqm
What is tqm Ihi basic certificate
Ihi basic certificate Sormimurtumat
Sormimurtumat Ulla hahn: nie mehr gedicht text
Ulla hahn: nie mehr gedicht text Ulla hahn ein gedicht für dich
Ulla hahn ein gedicht für dich Halv v-fog
Halv v-fog Ulla knuuti
Ulla knuuti Ulla licandro
Ulla licandro Ulla serup thomsen
Ulla serup thomsen Aufbau des natriumchloridkristalls
Aufbau des natriumchloridkristalls