RETROVIROLOGY ONCONOVIRUSES LENTIVIRUSES Retrovirus Family Taxonomy Retrovirus Structure



- Slides: 52
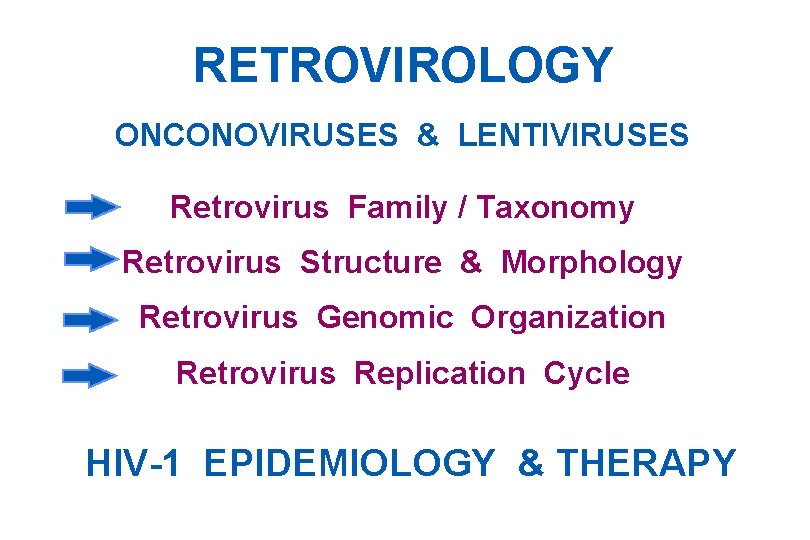
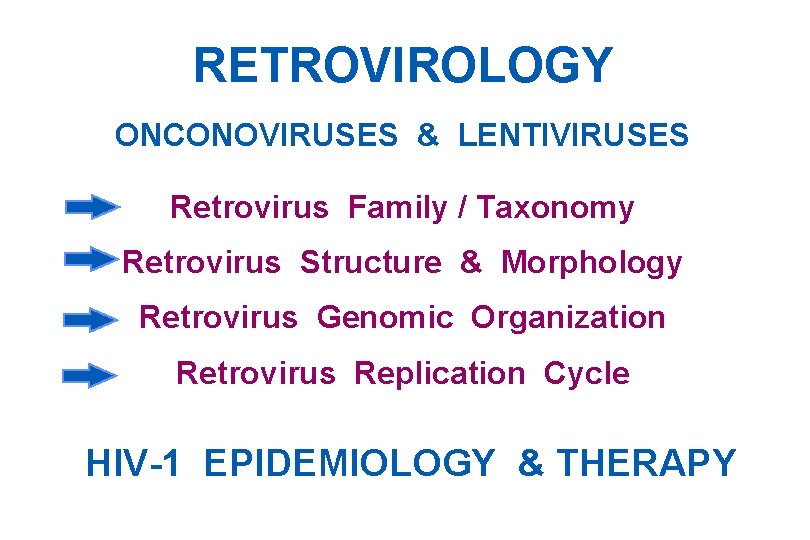
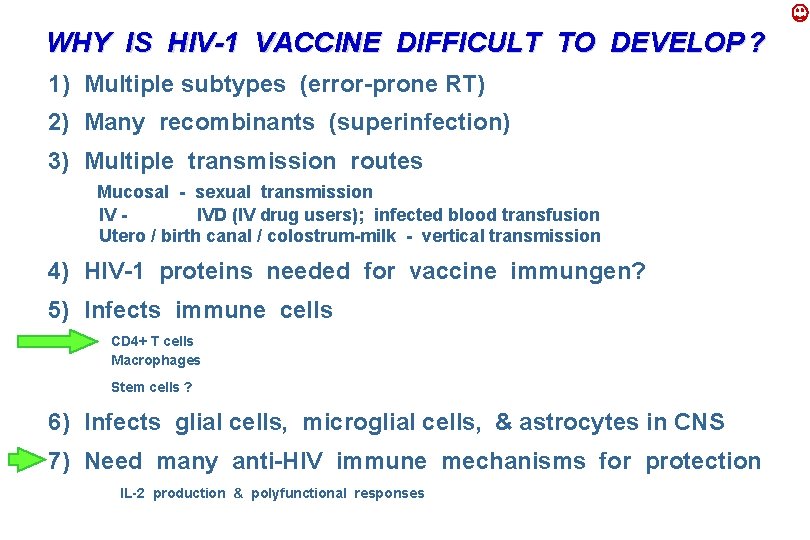
RETROVIROLOGY ONCONOVIRUSES & LENTIVIRUSES Retrovirus Family / Taxonomy Retrovirus Structure & Morphology Retrovirus Genomic Organization Retrovirus Replication Cycle HIV-1 EPIDEMIOLOGY & THERAPY
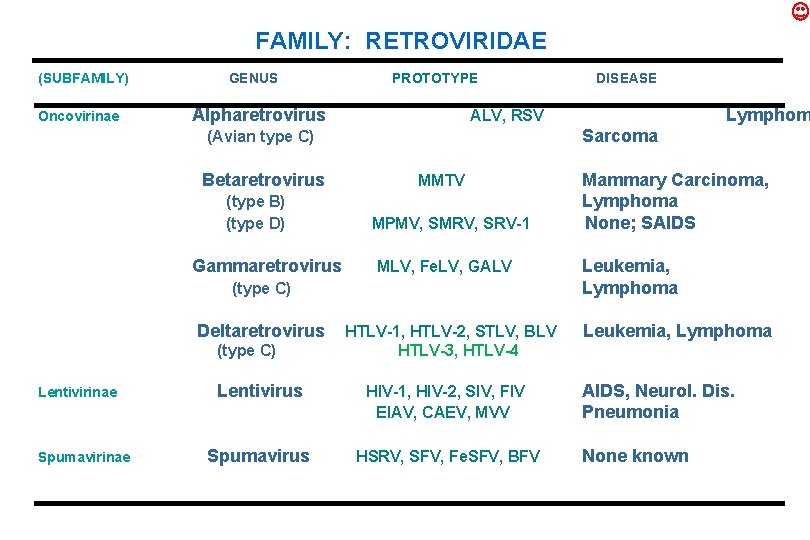
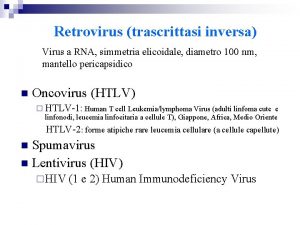
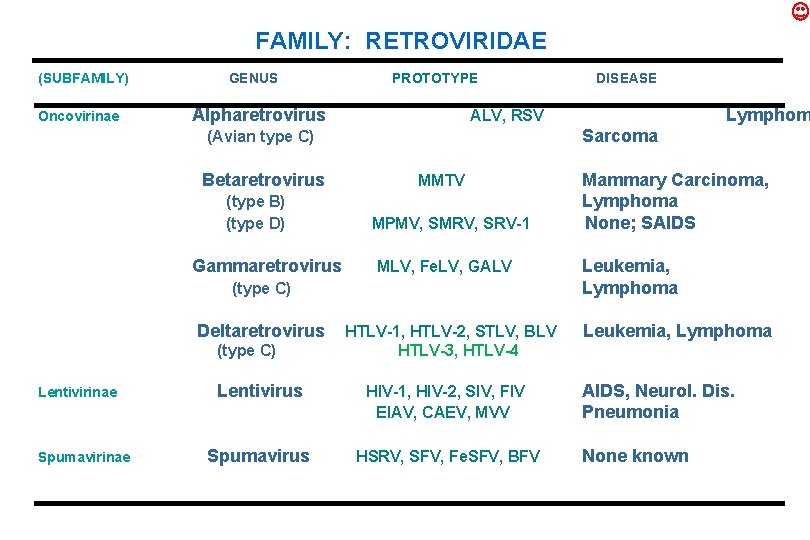
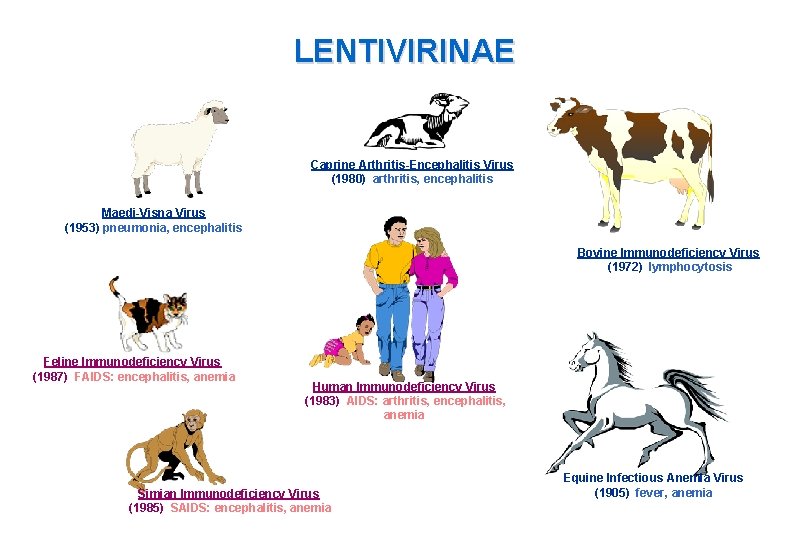
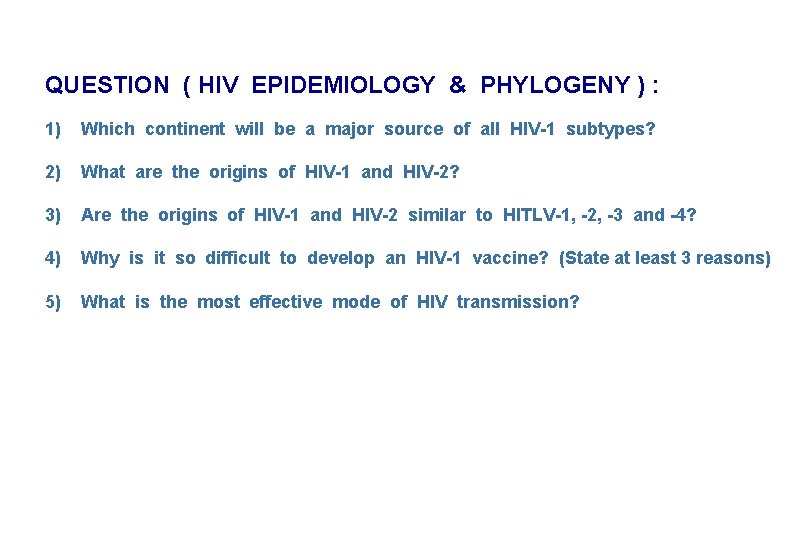
FAMILY: RETROVIRIDAE (SUBFAMILY) Oncovirinae GENUS PROTOTYPE Alpharetrovirus (type B) (type D) Gammaretrovirus Sarcoma MMTV MPMV, SMRV, SRV-1 MLV, Fe. LV, GALV (type C) Deltaretrovirus (type C) Lentivirinae Spumavirinae Lymphom ALV, RSV (Avian type C) Betaretrovirus DISEASE HTLV-1, HTLV-2, STLV, BLV HTLV-3, HTLV-4 Lentivirus HIV-1, HIV-2, SIV, FIV EIAV, CAEV, MVV Spumavirus HSRV, SFV, Fe. SFV, BFV Mammary Carcinoma, Lymphoma None; SAIDS Leukemia, Lymphoma AIDS, Neurol. Dis. Pneumonia None known
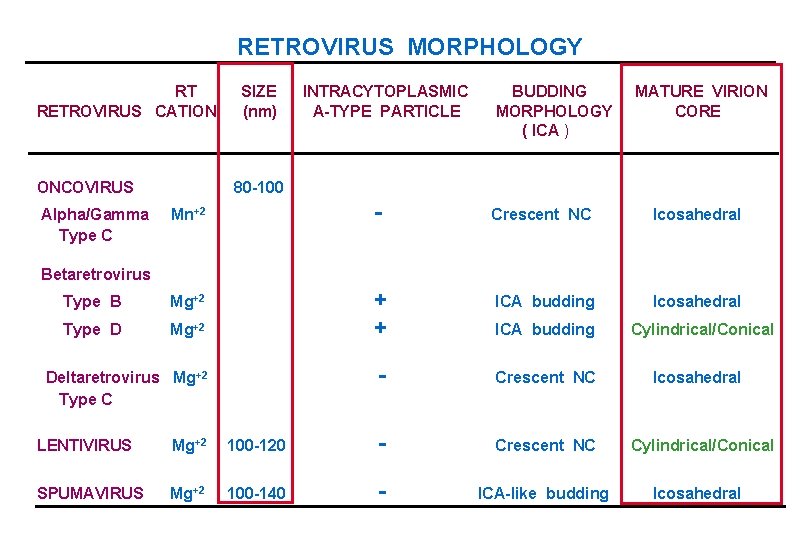
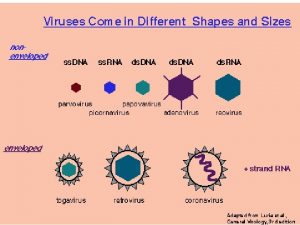
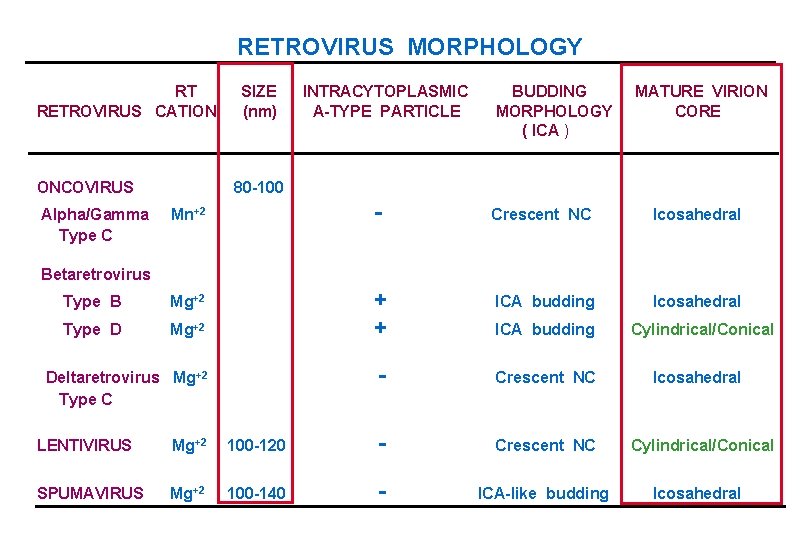
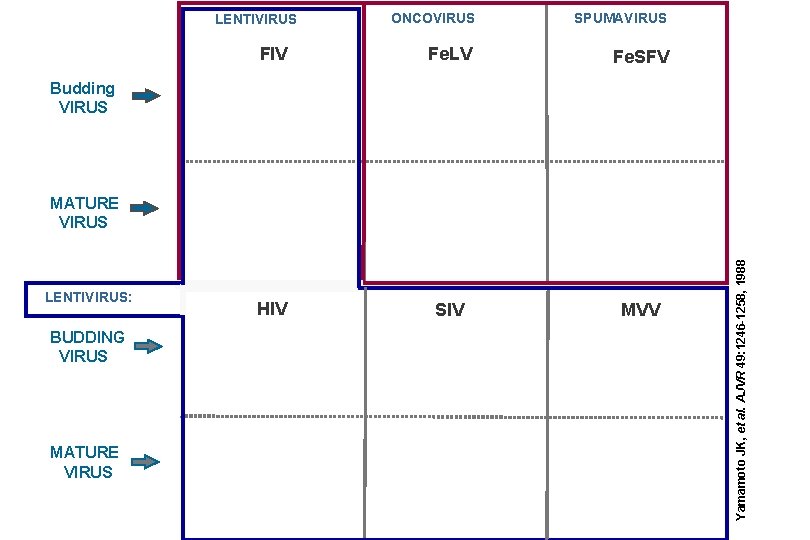
RETROVIRUS MORPHOLOGY RT RETROVIRUS CATION ONCOVIRUS SIZE (nm) INTRACYTOPLASMIC A-TYPE PARTICLE BUDDING MORPHOLOGY ( ICA ) MATURE VIRION CORE 80 -100 Mn+2 - Crescent NC Icosahedral Type B Mg+2 ICA budding Icosahedral Type D Mg+2 + + - Crescent NC Alpha/Gamma Type C Betaretrovirus Deltaretrovirus Mg+2 Type C ICA budding LENTIVIRUS Mg+2 100 -120 - Crescent NC SPUMAVIRUS Mg+2 100 -140 - ICA-like budding Cylindrical/Conical Icosahedral
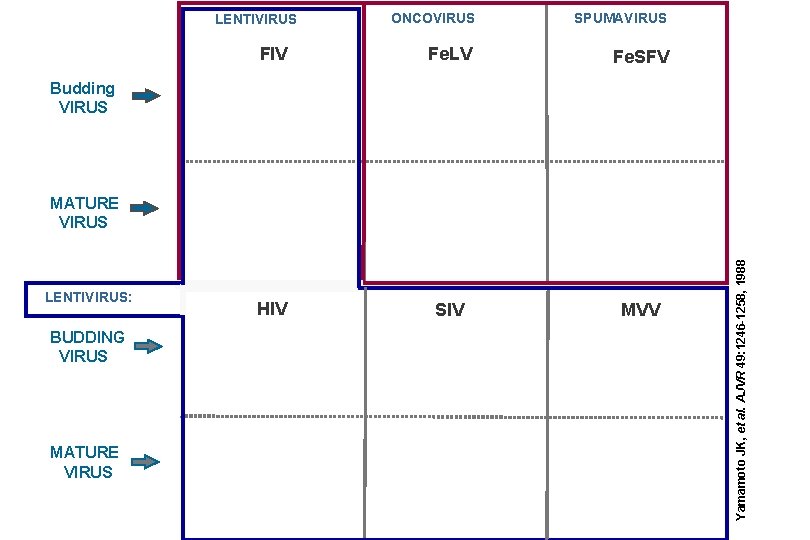
ONCOVIRUS SPUMAVIRUS FIV Fe. LV Fe. SFV HIV SIV MVV LENTIVIRUS Budding VIRUS LENTIVIRUS: BUDDING VIRUS MATURE VIRUS Yamamoto JK, et al. AJVR 49: 1246 -1258, 1988 MATURE VIRUS
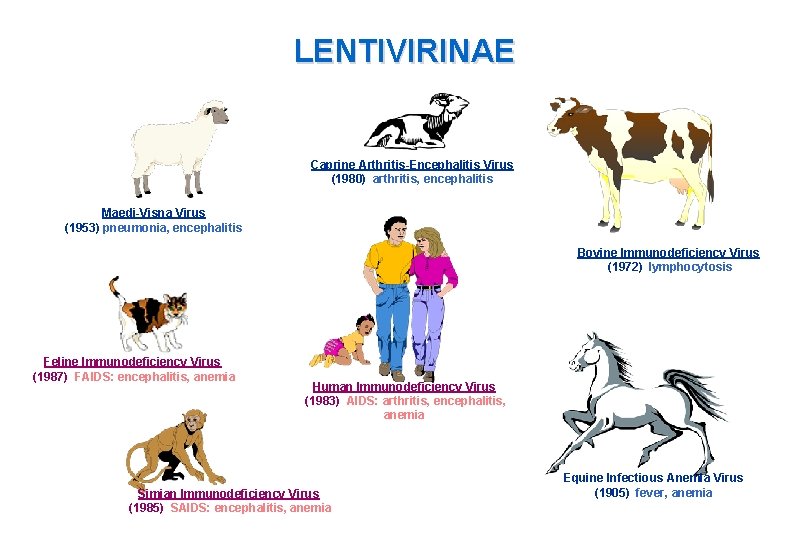
LENTIVIRINAE Caprine Arthritis-Encephalitis Virus (1980) arthritis, encephalitis Maedi-Visna Virus (1953) pneumonia, encephalitis Bovine Immunodeficiency Virus (1972) lymphocytosis Feline Immunodeficiency Virus (1987) FAIDS: encephalitis, anemia Human Immunodeficiency Virus (1983) AIDS: arthritis, encephalitis, anemia Simian Immunodeficiency Virus (1985) SAIDS: encephalitis, anemia Equine Infectious Anemia Virus (1905) fever, anemia
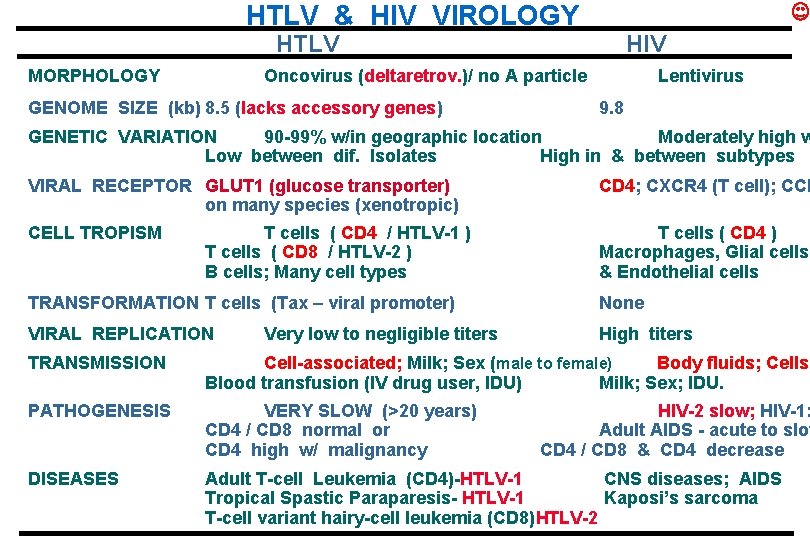
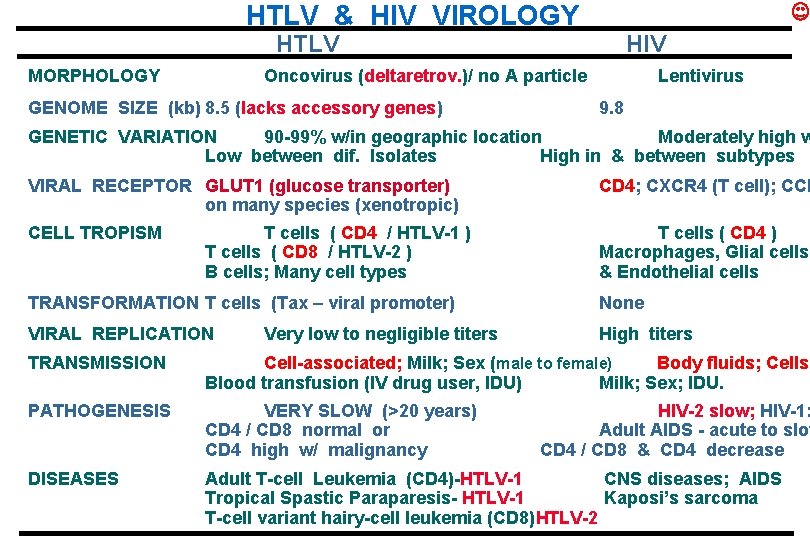
HTLV & HIV VIROLOGY HTLV MORPHOLOGY HIV Oncovirus (deltaretrov. )/ no A particle GENOME SIZE (kb) 8. 5 (lacks accessory genes) Lentivirus 9. 8 GENETIC VARIATION 90 -99% w/in geographic location Moderately high w Low between dif. Isolates High in & between subtypes VIRAL RECEPTOR GLUT 1 (glucose transporter) on many species (xenotropic) CD 4; CXCR 4 (T cell); CCR CELL TROPISM T cells ( CD 4 ) Macrophages, Glial cells, & Endothelial cells T cells ( CD 4 / HTLV-1 ) T cells ( CD 8 / HTLV-2 ) B cells; Many cell types TRANSFORMATION T cells (Tax – viral promoter) None VIRAL REPLICATION High titers Very low to negligible titers TRANSMISSION Cell-associated; Milk; Sex (male to female) Body fluids; Cells; Blood transfusion (IV drug user, IDU) Milk; Sex; IDU. PATHOGENESIS VERY SLOW (>20 years) CD 4 / CD 8 normal or CD 4 high w/ malignancy DISEASES Adult T-cell Leukemia (CD 4)-HTLV-1 CNS diseases; AIDS Tropical Spastic Paraparesis- HTLV-1 Kaposi’s sarcoma T-cell variant hairy-cell leukemia (CD 8)HTLV-2 HIV-2 slow; HIV-1: Adult AIDS - acute to slow CD 4 / CD 8 & CD 4 decrease
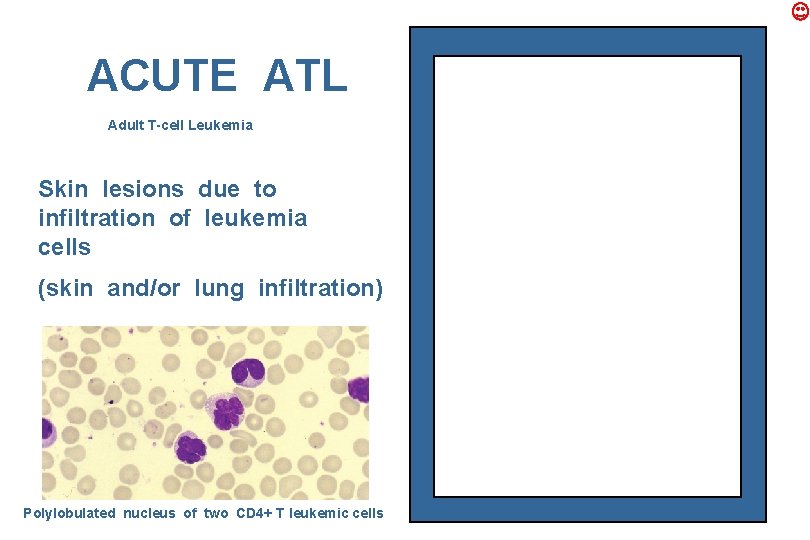
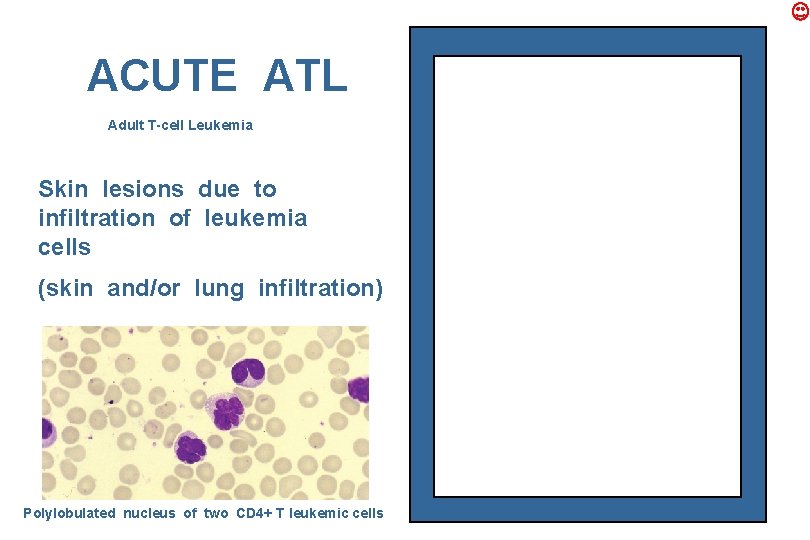
ACUTE ATL Adult T-cell Leukemia Skin lesions due to infiltration of leukemia cells (skin and/or lung infiltration) Polylobulated nucleus of two CD 4+ T leukemic cells
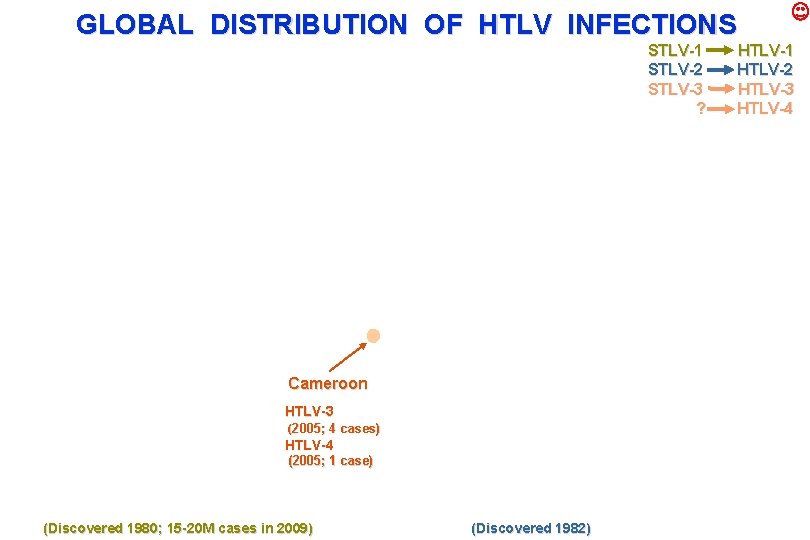
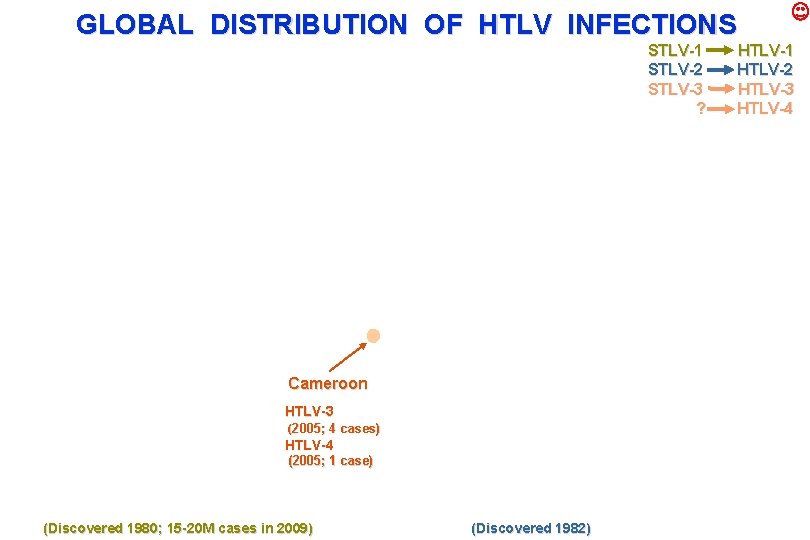
GLOBAL DISTRIBUTION OF HTLV INFECTIONS STLV-1 STLV-2 STLV-3 ? Cameroon HTLV-3 (2005; 4 cases) HTLV-4 (2005; 1 case) (Discovered 1980; 15 -20 M cases in 2009) (Discovered 1982) HTLV-1 HTLV-2 HTLV-3 HTLV-4
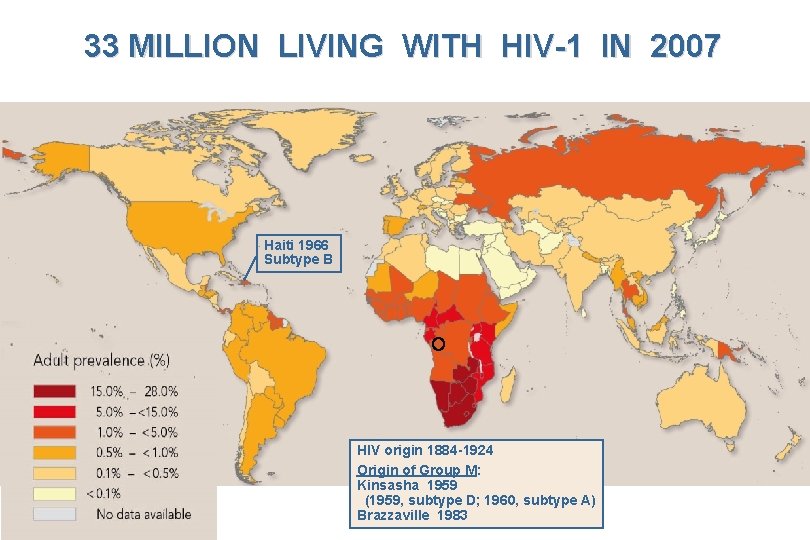
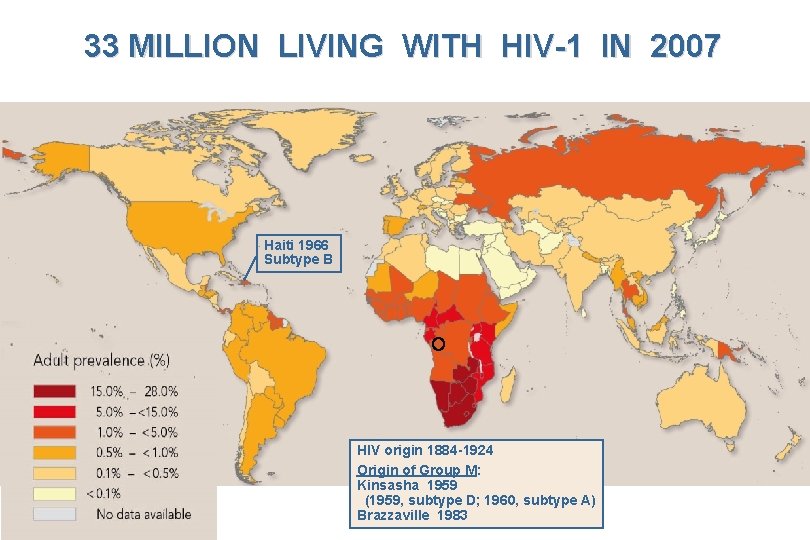
33 MILLION LIVING WITH HIV-1 IN 2007 Haiti 1966 Subtype B HIV origin 1884 -1924 Origin of Group M: Kinsasha 1959 (1959, subtype D; 1960, subtype A) Brazzaville 1983
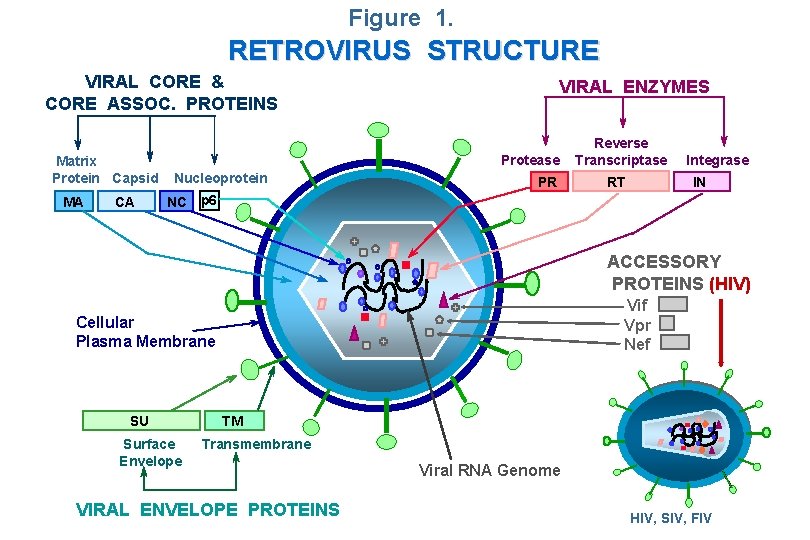
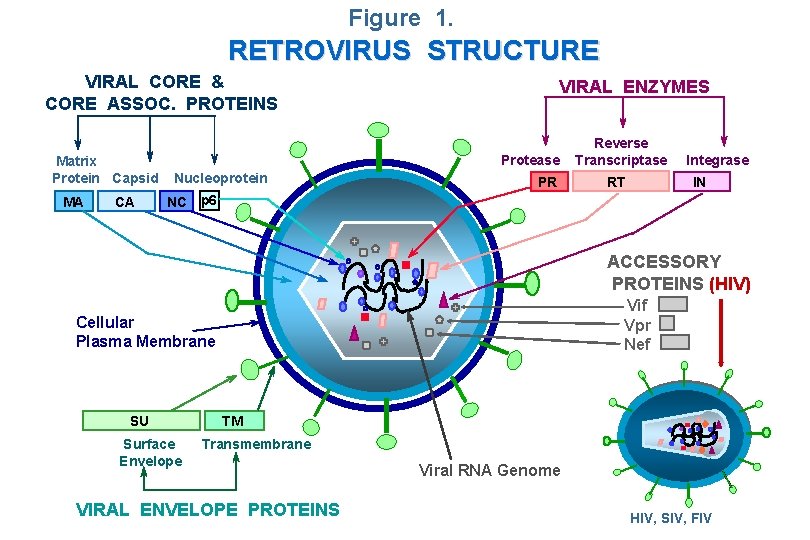
Figure 1. RETROVIRUS STRUCTURE VIRAL CORE & CORE ASSOC. PROTEINS Matrix Protein Capsid MA CA VIRAL ENZYMES Protease Nucleoprotein PR Reverse Transcriptase RT Integrase IN NC p 6 ACCESSORY PROTEINS (HIV) Vif Vpr Nef Cellular Plasma Membrane SU Surface Envelope TM Transmembrane VIRAL ENVELOPE PROTEINS Viral RNA Genome HIV, SIV, FIV
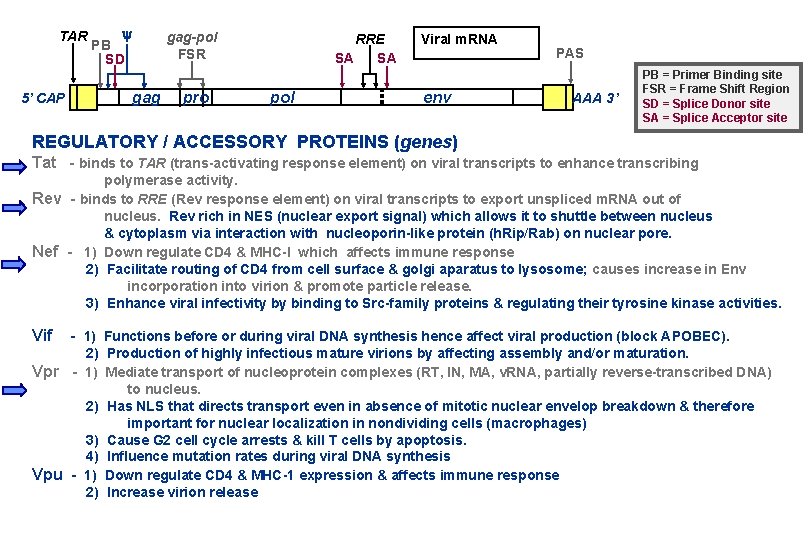
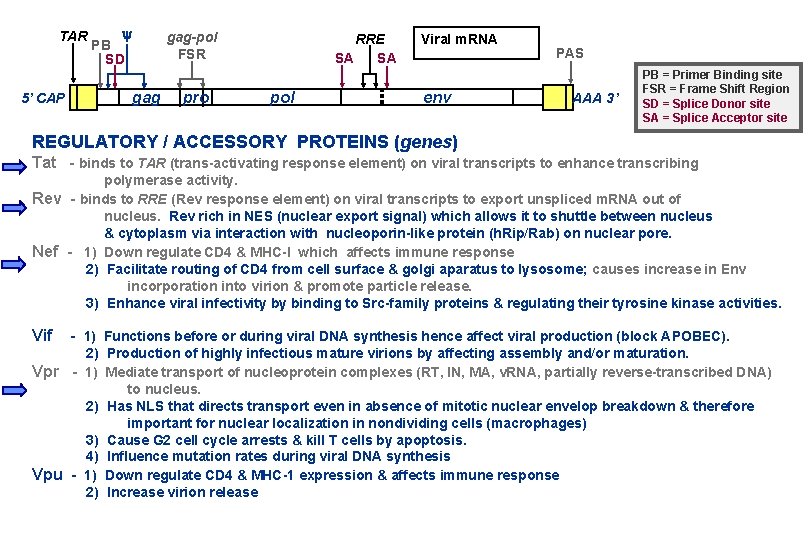
TAR 5’ CAP y PB SD gag-pol FSR gag pro RRE SA SA pol Viral m. RNA env PAS AAA 3’ PB = Primer Binding site FSR = Frame Shift Region SD = Splice Donor site SA = Splice Acceptor site REGULATORY / ACCESSORY PROTEINS (genes) Tat - binds to TAR (trans-activating response element) on viral transcripts to enhance transcribing polymerase activity. Rev - binds to RRE (Rev response element) on viral transcripts to export unspliced m. RNA out of nucleus. Rev rich in NES (nuclear export signal) which allows it to shuttle between nucleus & cytoplasm via interaction with nucleoporin-like protein (h. Rip/Rab) on nuclear pore. Nef - 1) Down regulate CD 4 & MHC-I which affects immune response 2) Facilitate routing of CD 4 from cell surface & golgi aparatus to lysosome; causes increase in Env incorporation into virion & promote particle release. 3) Enhance viral infectivity by binding to Src-family proteins & regulating their tyrosine kinase activities. Vif - 1) Functions before or during viral DNA synthesis hence affect viral production (block APOBEC). 2) Production of highly infectious mature virions by affecting assembly and/or maturation. Vpr - 1) Mediate transport of nucleoprotein complexes (RT, IN, MA, v. RNA, partially reverse-transcribed DNA) to nucleus. 2) Has NLS that directs transport even in absence of mitotic nuclear envelop breakdown & therefore important for nuclear localization in nondividing cells (macrophages) 3) Cause G 2 cell cycle arrests & kill T cells by apoptosis. 4) Influence mutation rates during viral DNA synthesis Vpu - 1) Down regulate CD 4 & MHC-1 expression & affects immune response 2) Increase virion release
COMPARISON OF RETROVIRAL GENOMES ( kilobases ) 0 1 2 3 4 5 6 7 8 9 10

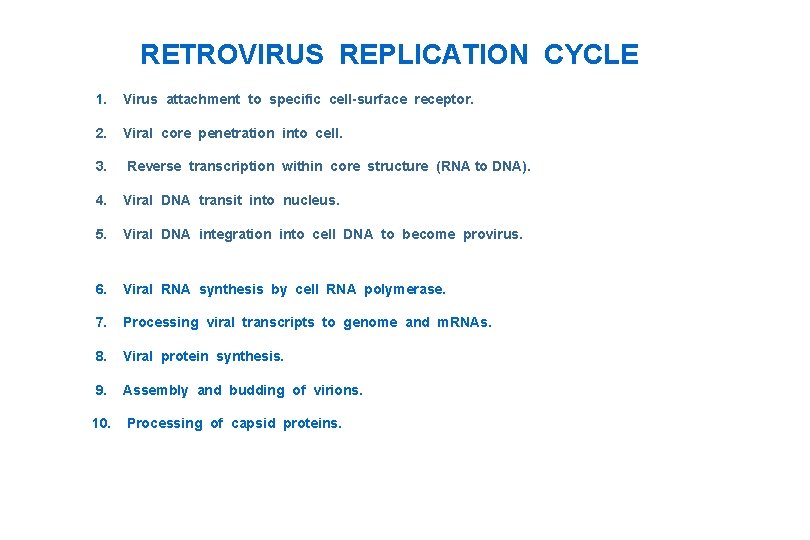
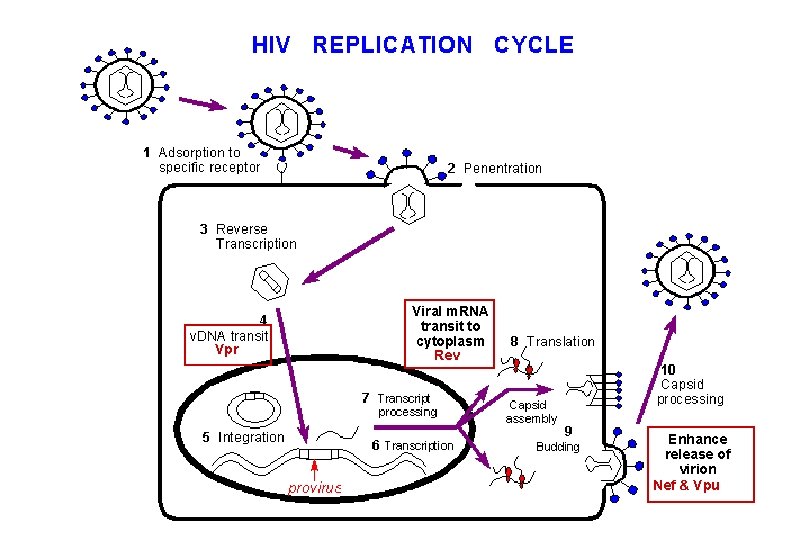
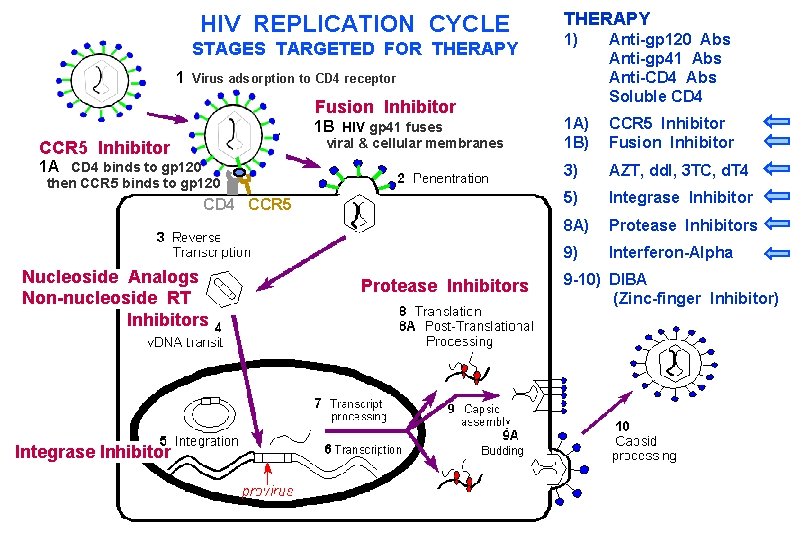
RETROVIRUS REPLICATION CYCLE 1. Virus attachment to specific cell-surface receptor. 2. Viral core penetration into cell. 3. Reverse transcription within core structure (RNA to DNA). 4. Viral DNA transit into nucleus. 5. Viral DNA integration into cell DNA to become provirus. 6. Viral RNA synthesis by cell RNA polymerase. 7. Processing viral transcripts to genome and m. RNAs. 8. Viral protein synthesis. 9. Assembly and budding of virions. 10. Processing of capsid proteins.
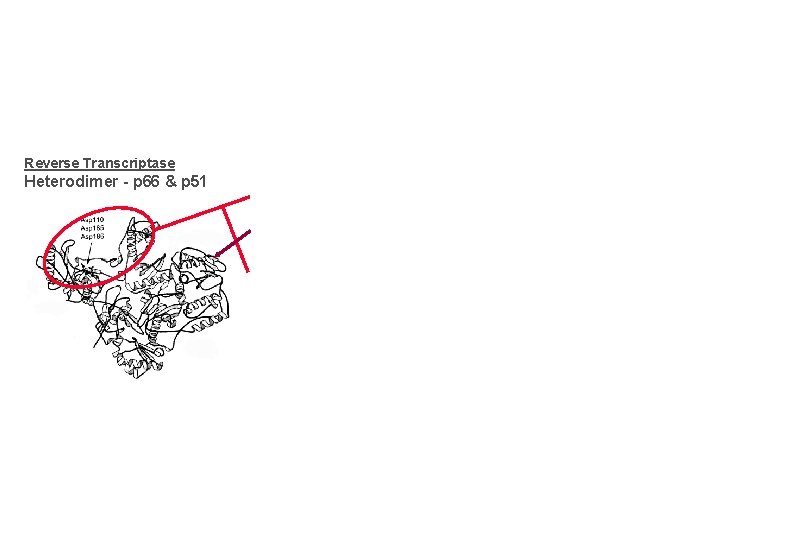
Reverse Transcriptase Heterodimer - p 66 & p 51
VIRAL DNA SYNTHESIS ( Stage 1 - Cell Cytoplasm )
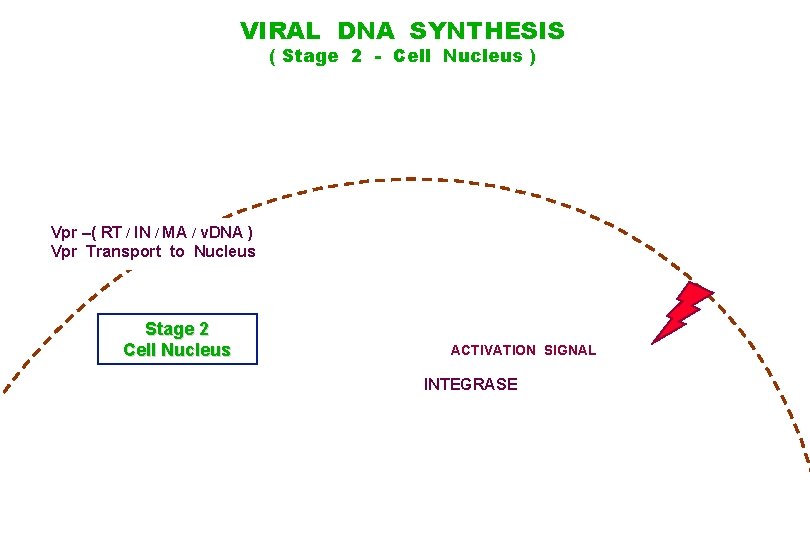
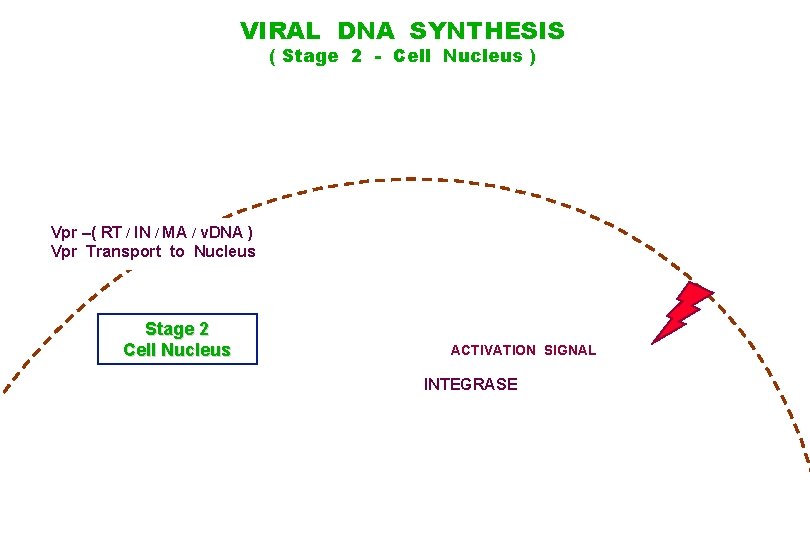
VIRAL DNA SYNTHESIS ( Stage 2 - Cell Nucleus ) Vpr –( RT / IN / MA / v. DNA ) Vpr Transport to Nucleus Stage 2 Cell Nucleus ACTIVATION SIGNAL INTEGRASE
0 Tat 1 2 3 4 5 6 7 8 9 10
0 1 2 3 4 5 in 6 7 8 9 10
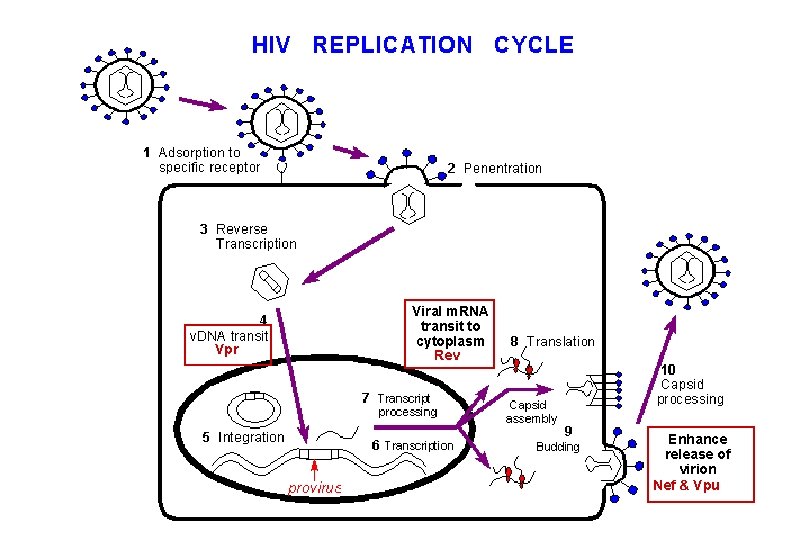
Vpr Viral m. RNA transit to cytoplasm Rev Enhance release of virion Nef & Vpu
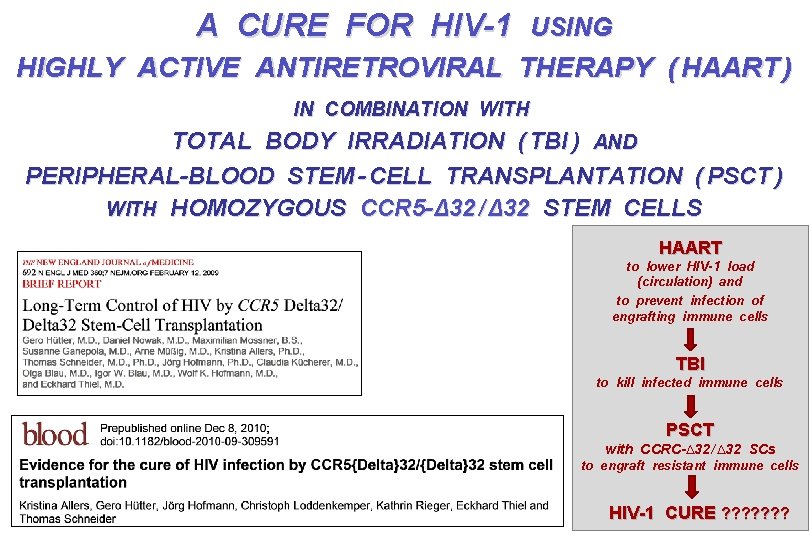
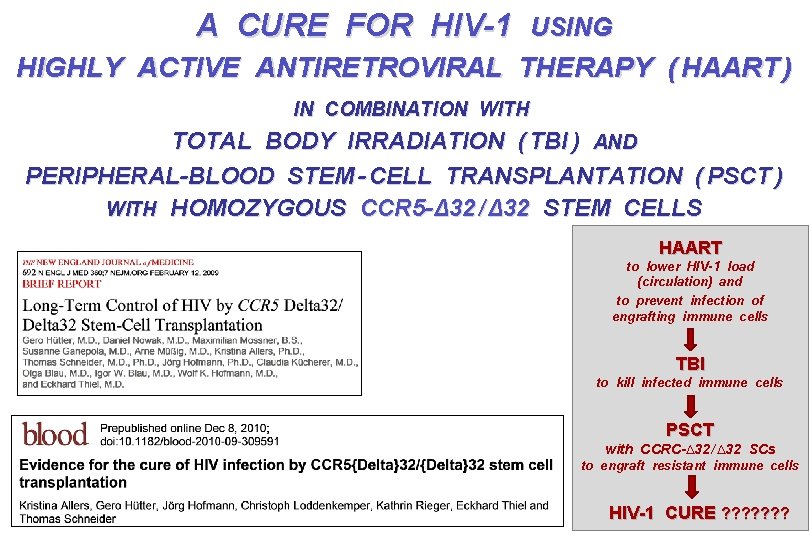
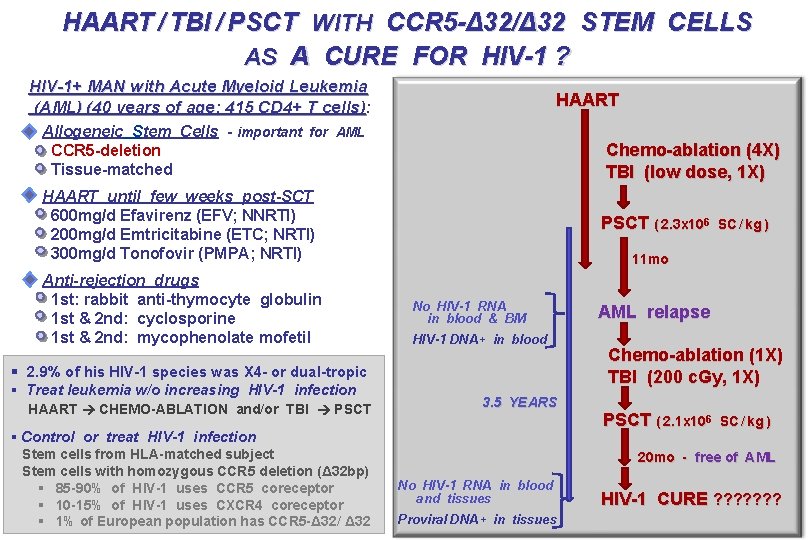
A CURE FOR HIV-1 USING HIGHLY ACTIVE ANTIRETROVIRAL THERAPY ( HAART ) IN COMBINATION WITH TOTAL BODY IRRADIATION ( TBI ) AND PERIPHERAL-BLOOD STEM - CELL TRANSPLANTATION ( PSCT ) WITH HOMOZYGOUS CCR 5 -Δ 32 / Δ 32 STEM CELLS HAART to lower HIV-1 load (circulation) and to prevent infection of engrafting immune cells TBI to kill infected immune cells PSCT with CCRC-∆32 / ∆32 SCs to engraft resistant immune cells HIV-1 CURE ? ? ? ?
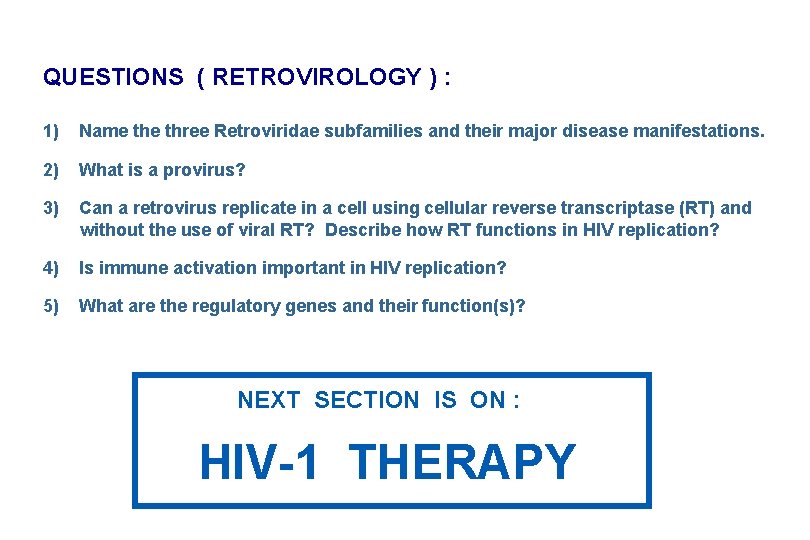
QUESTIONS ( RETROVIROLOGY ) : 1) Name three Retroviridae subfamilies and their major disease manifestations. 2) What is a provirus? 3) Can a retrovirus replicate in a cell using cellular reverse transcriptase (RT) and without the use of viral RT? Describe how RT functions in HIV replication? 4) Is immune activation important in HIV replication? 5) What are the regulatory genes and their function(s)? NEXT SECTION IS ON : HIV-1 THERAPY
HIV-1 AND AIDS HIV THERAPY HIV EPIDEMIOLOGY & PHYLOGENY HIV PATHOGENESIS & HIV VACCINE
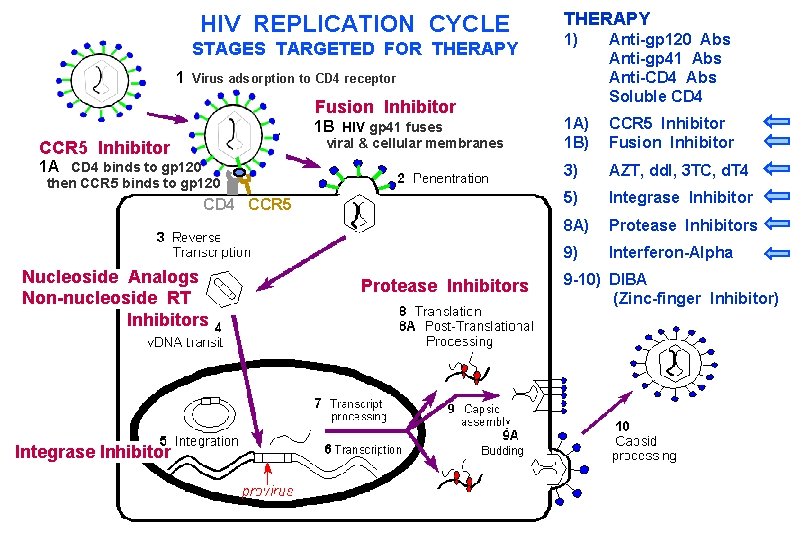
HIV REPLICATION CYCLE STAGES TARGETED FOR THERAPY 1) Anti-gp 120 Abs Anti-gp 41 Abs Anti-CD 4 Abs Soluble CD 4 1 A) 1 B) CCR 5 Inhibitor Fusion Inhibitor 3) AZT, dd. I, 3 TC, d. T 4 5) Integrase Inhibitor 8 A) Protease Inhibitors 9) Interferon-Alpha 1 Virus adsorption to CD 4 receptor Fusion Inhibitor 1 B HIV gp 41 fuses viral & cellular membranes CCR 5 Inhibitor 1 A CD 4 binds to gp 120 then CCR 5 binds to gp 120 CD 4 CCR 5 Nucleoside Analogs Non-nucleoside RT Inhibitors Integrase Inhibitor Protease Inhibitors 9 -10) DIBA (Zinc-finger Inhibitor)
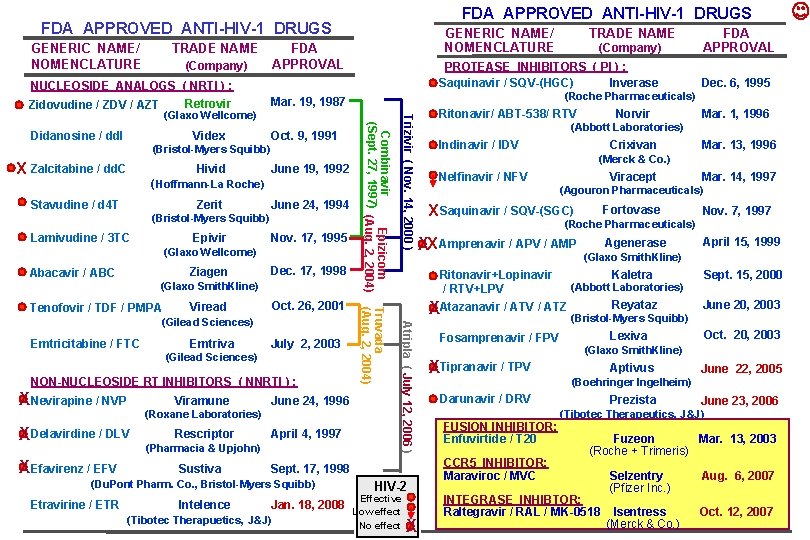
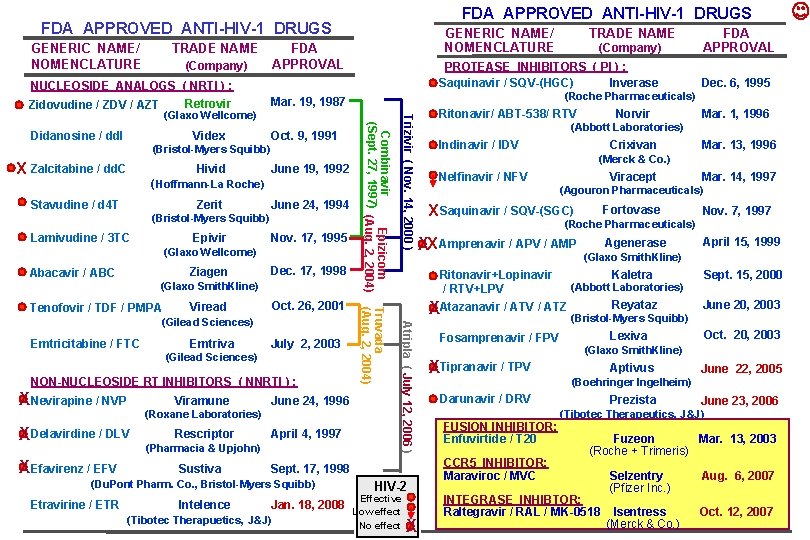
FDA APPROVED ANTI-HIV-1 DRUGS GENERIC NAME/ NOMENCLATURE TRADE NAME GENERIC NAME/ NOMENCLATURE FDA APPROVAL (Company) NUCLEOSIDE ANALOGS ( NRTI ) : Retrovir / AZT Retrovir Zidovudine / ZDV / AZT Х Zalcitabine / dd. C Hivid June 19, 1992 ( Hoffmann-La Roche) Stavudine / d 4 T Zerit June 24, 1994 (Bristol-Myers Squibb) Lamivudine / 3 TC Epivir Nov. 17, 1995 (Glaxo Wellcome) Ziagen Abacavir / ABC Dec. 17, 1998 (Glaxo Smith. Kline) Oct. 26, 2001 Viread Emtricitabine / FTC Emtriva July 2, 2003 (Gilead Sciences) NON-NUCLEOSIDE RT INHIBITORS ( NNRTI ) : XNevirapine / NVP Viramune (Roxane Laboratories) XDelavirdine / DLV XEfavirenz / EFV June 24, 1996 Rescriptor April 4, 1997 (Pharmacia & Upjohn) Sustiva Sept. 17, 1998 (Du. Pont Pharm. Co. , Bristol-Myers Squibb) Etravirine / ETR Intelence Jan. 18, 2008 (Tibotec Therapuetics, J&J) Ritonavir/ ABT-538/ RTV Dec. 6, 1995 HIV-2 Effective Low effect No effect X Norvir Mar. 1, 1996 (Abbott Laboratories) Indinavir / IDV Crixivan Mar. 13, 1996 (Merck & Co. ) Nelfinavir / NFV Viracept Mar. 14, 1997 (Agouron Pharmaceuticals) Х Saquinavir / SQV-(SGC) Fortovase Nov. 7, 1997 (Roche Pharmaceuticals) XХ Amprenavir / APV / AMP Ritonavir+Lopinavir / RTV+LPV Atripla ( July 12, 2006 ) (Gilead Sciences) Truvada (Aug. 2, 2004) Tenofovir / TDF / PMPA Trizivir ( Nov. 14, 2000 ) (Bristol-Myers Squibb) Combinavir Epizicom (Sept. 27, 1997) (Aug. 2, 2004) Oct. 9, 1991 FDA APPROVAL (Roche Pharmaceuticals) Mar. 19, 1987 Videx (Company) PROTEASE INHIBITORS ( PI ) : Saquinavir / SQV-(HGC) Inverase (Glaxo Wellcome) Didanosine / dd. I TRADE NAME Agenerase (Glaxo Smith. Kline) Kaletra (Abbott Laboratories) Reyataz XAtazanavir / ATV / ATZ (Bristol-Myers Squibb) Fosamprenavir / FPV XTipranavir / TPV Lexiva CCR 5 INHIBITOR: Maraviroc / MVC Sept. 15, 2000 June 20, 2003 Oct. 20, 2003 (Glaxo Smith. Kline) Aptivus June 22, 2005 (Boehringer Ingelheim) Darunavir / DRV FUSION INHIBITOR: Enfuvirtide / T 20 April 15, 1999 Prezista June 23, 2006 (Tibotec Therapeutics, J&J) Fuzeon Mar. 13, 2003 (Roche + Trimeris) INTEGRASE INHIBTOR: Raltegravir / RAL / MK-0518 Selzentry (Pfizer Inc. ) Aug. 6, 2007 Isentress (Merck & Co. ) Oct. 12, 2007
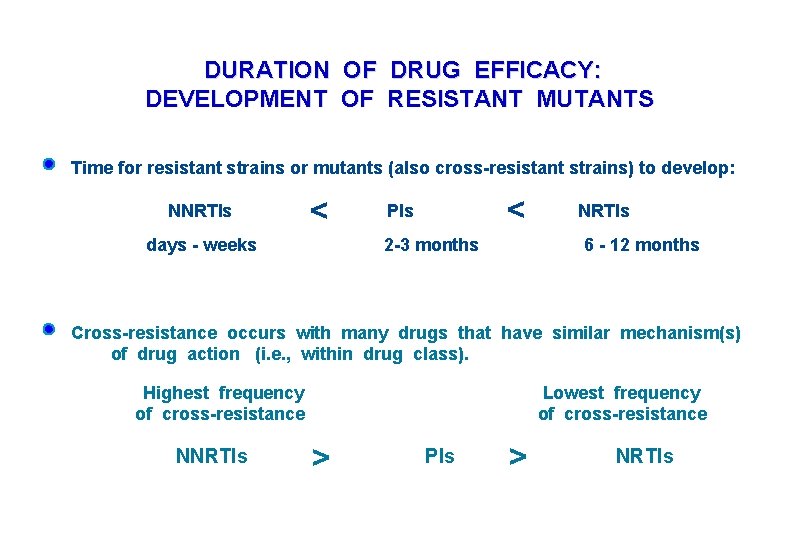
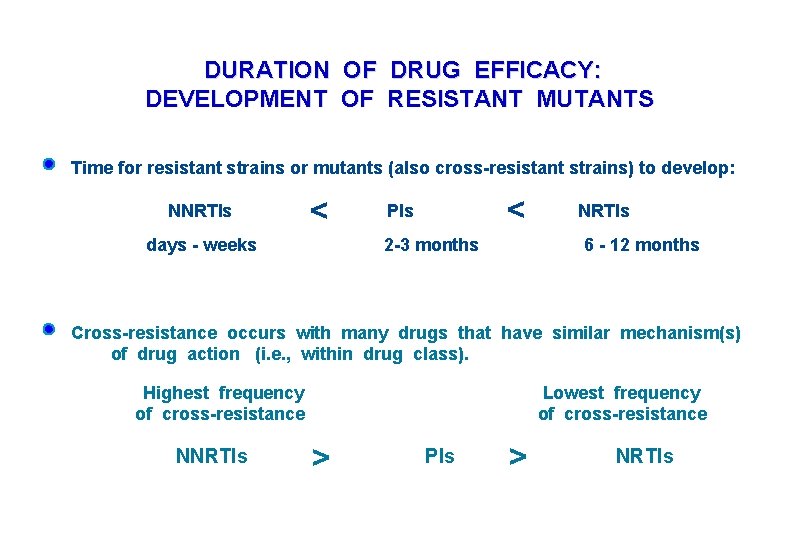
DURATION OF DRUG EFFICACY: DEVELOPMENT OF RESISTANT MUTANTS Time for resistant strains or mutants (also cross-resistant strains) to develop: NNRTIs < days - weeks < PIs 2 -3 months NRTIs 6 - 12 months Cross-resistance occurs with many drugs that have similar mechanism(s) of drug action (i. e. , within drug class). Highest frequency of cross-resistance NNRTIs Lowest frequency of cross-resistance > PIs > NRTIs
( d 4 T ) ( 3 TC ) ( PMPA ) ( ABC ) deoxyguanosine
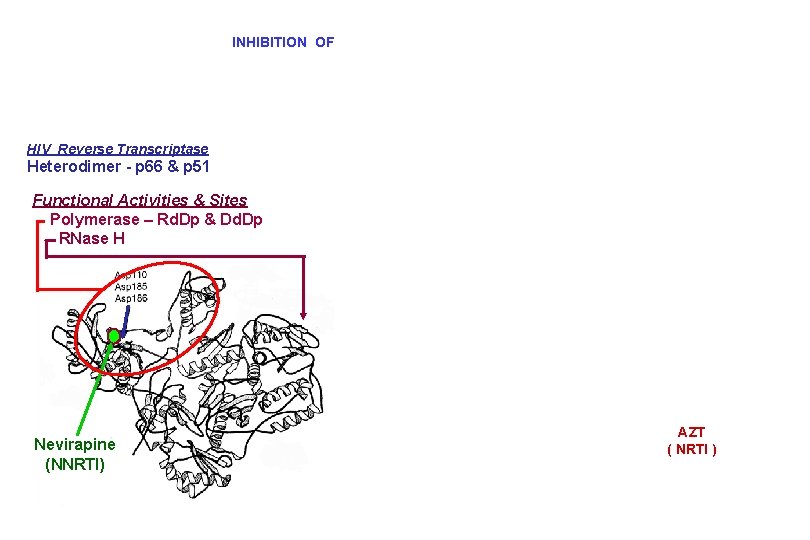
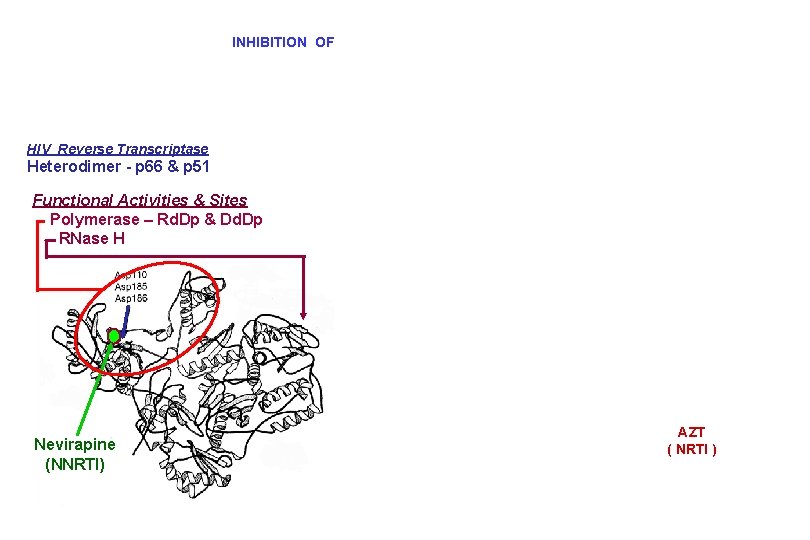
INHIBITION OF HIV Reverse Transcriptase Heterodimer - p 66 & p 51 Functional Activities & Sites Polymerase – Rd. Dp & Dd. Dp RNase H Nevirapine (NNRTI) AZT ( NRTI )

HIV PROTEASE INHIBITORS RT IN

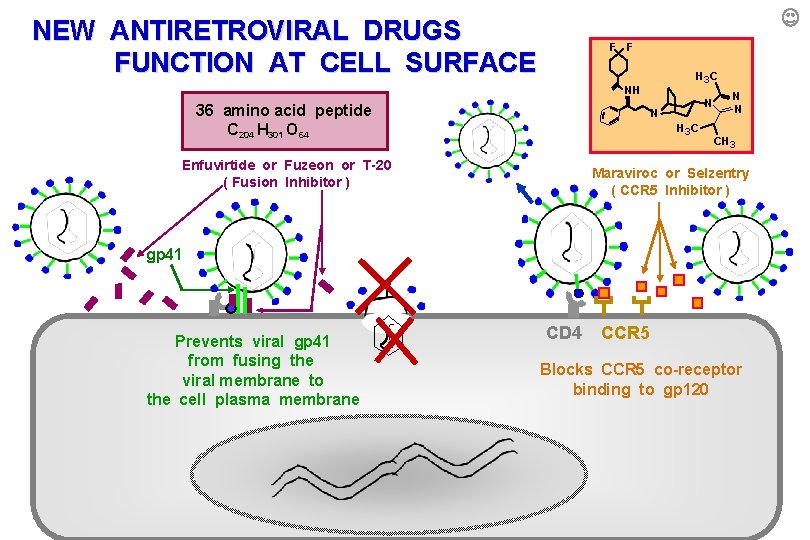
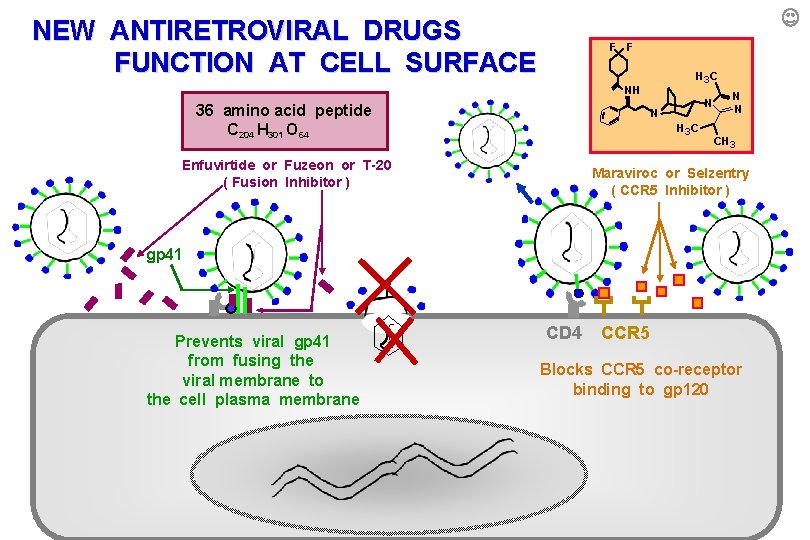
NEW ANTIRETROVIRAL DRUGS FUNCTION AT CELL SURFACE F F H 3 C NH 36 amino acid peptide C 204 H 301 O 64 N N H 3 C Enfuvirtide or Fuzeon or T-20 ( Fusion Inhibitor ) N N CH 3 Maraviroc or Selzentry ( CCR 5 Inhibitor ) gp 41 Prevents viral gp 41 from fusing the viral membrane to the cell plasma membrane CD 4 CCR 5 Blocks CCR 5 co-receptor binding to to gp 120
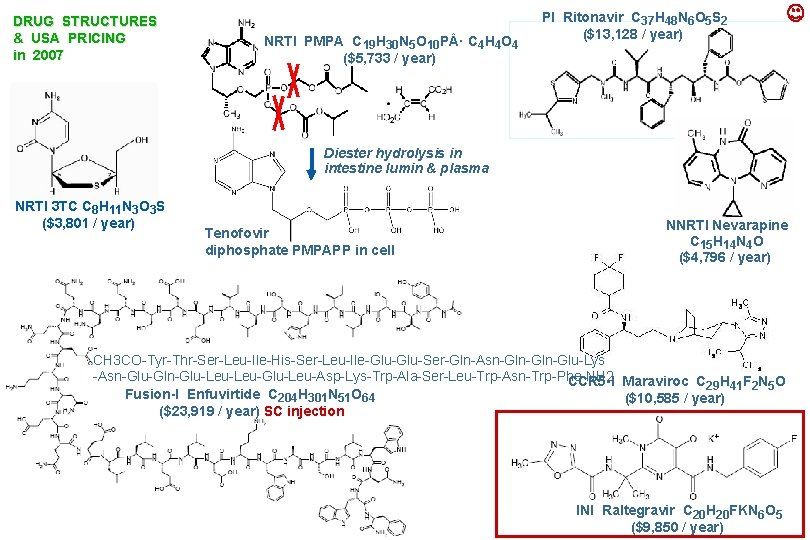
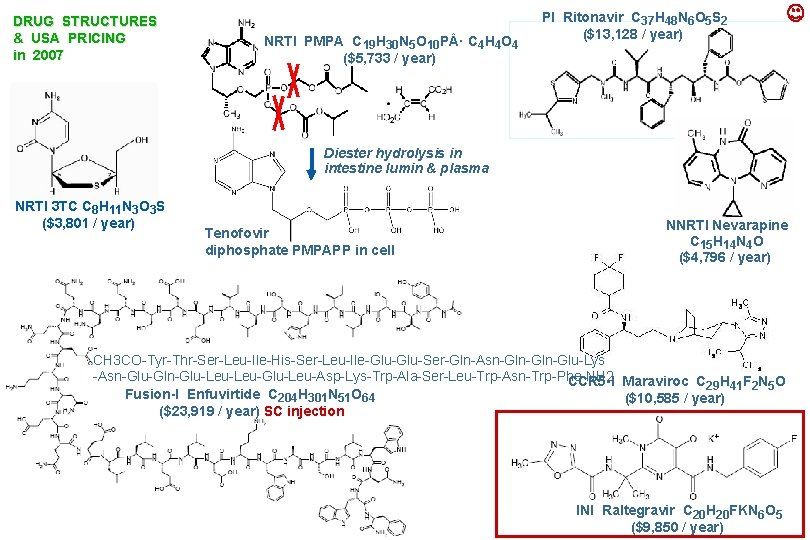
DRUG STRUCTURES & USA PRICING in 2007 NRTI PMPA C 19 H 30 N 5 O 10 P · C 4 H 4 O 4 ($5, 733 / year) PI Ritonavir C 37 H 48 N 6 O 5 S 2 ($13, 128 / year) Diester hydrolysis in intestine lumin & plasma NRTI 3 TC C 8 H 11 N 3 O 3 S ($3, 801 / year) Tenofovir diphosphate PMPAPP in cell NNRTI Nevarapine C 15 H 14 N 4 O ($4, 796 / year) CH 3 CO-Tyr-Thr-Ser-Leu-Ile-His-Ser-Leu-Ile-Glu-Ser-Gln-Asn-Gln-Glu-Lys -Asn-Glu-Gln-Glu-Leu-Glu-Leu-Asp-Lys-Trp-Ala-Ser-Leu-Trp-Asn-Trp-Phe-NH 2 CCR 5 -I Maraviroc C 29 H 41 F 2 N 5 O Fusion-I Enfuvirtide C 204 H 301 N 51 O 64 ($10, 585 / year) ($23, 919 / year) SC injection INI Raltegravir C 20 H 20 FKN 6 O 5 ($9, 850 / year)
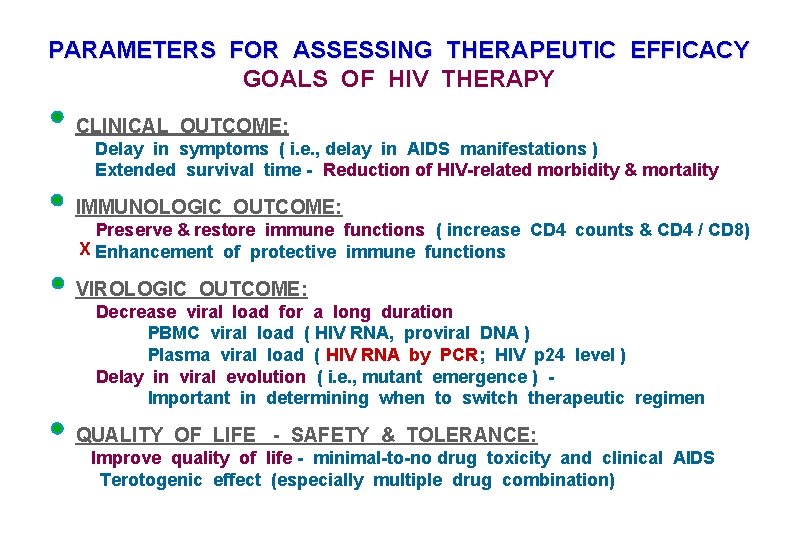
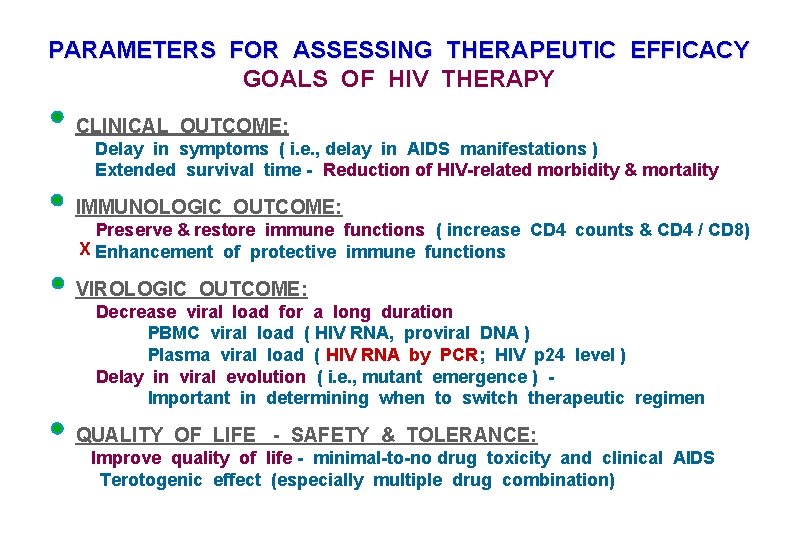
PARAMETERS FOR ASSESSING THERAPEUTIC EFFICACY GOALS OF HIV THERAPY CLINICAL OUTCOME: Delay in symptoms ( i. e. , delay in AIDS manifestations ) Extended survival time - Reduction of HIV-related morbidity & mortality IMMUNOLOGIC OUTCOME: Preserve & restore immune functions ( increase CD 4 counts & CD 4 / CD 8) X Enhancement of protective immune functions VIROLOGIC OUTCOME: Decrease viral load for a long duration PBMC viral load ( HIV RNA, proviral DNA ) Plasma viral load ( HIV RNA by PCR; HIV p 24 level ) Delay in viral evolution ( i. e. , mutant emergence ) Important in determining when to switch therapeutic regimen QUALITY OF LIFE - SAFETY & TOLERANCE: Improve quality of life - minimal-to-no drug toxicity and clinical AIDS Terotogenic effect (especially multiple drug combination)
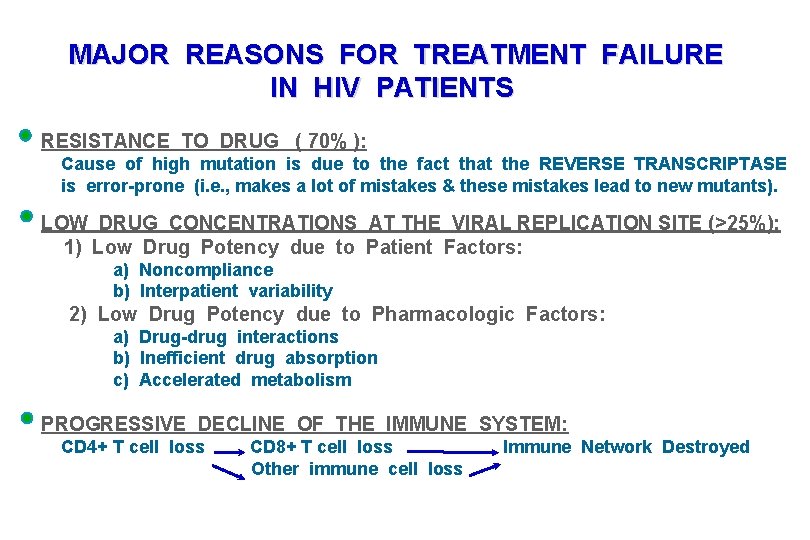
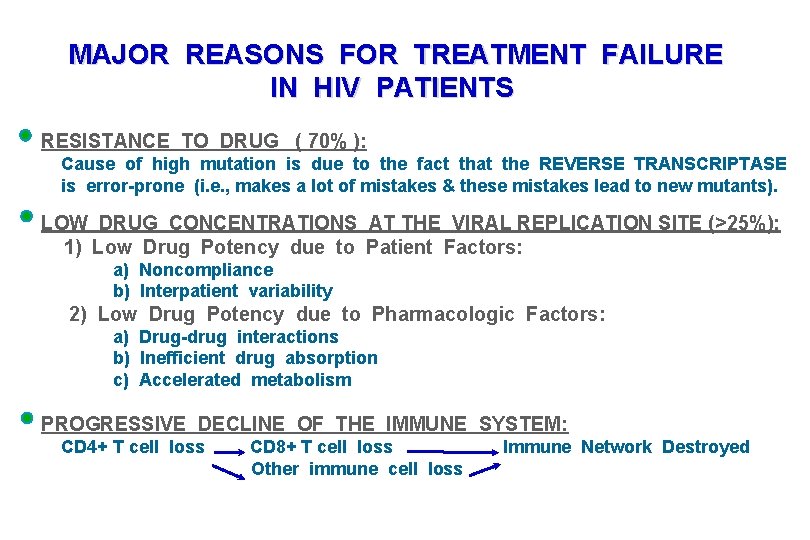
MAJOR REASONS FOR TREATMENT FAILURE IN HIV PATIENTS RESISTANCE TO DRUG ( 70% ): Cause of high mutation is due to the fact that the REVERSE TRANSCRIPTASE is error-prone (i. e. , makes a lot of mistakes & these mistakes lead to new mutants). LOW DRUG CONCENTRATIONS AT THE VIRAL REPLICATION SITE (>25%): 1) Low Drug Potency due to Patient Factors: a) Noncompliance b) Interpatient variability 2) Low Drug Potency due to Pharmacologic Factors: a) Drug-drug interactions b) Inefficient drug absorption c) Accelerated metabolism PROGRESSIVE DECLINE OF THE IMMUNE SYSTEM: CD 4+ T cell loss CD 8+ T cell loss Other immune cell loss Immune Network Destroyed
QUESTIONS ( HIV THERAPY ) : 1) What is HAART or ART? 2) An unsuccessful treatment with a protease inhibitor will often cause the subsequent therapy with another protease inhibitor to be less effective. Why? Would a therapy with nucleoside analogs be more successful in this patient?
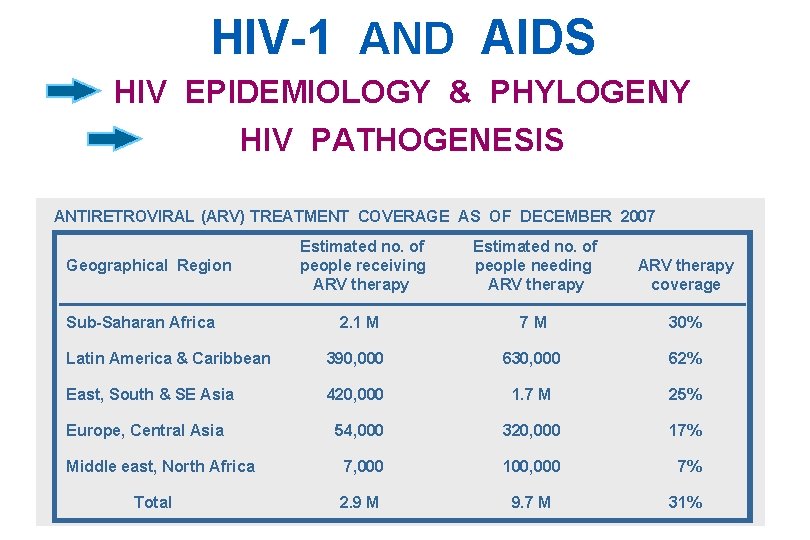
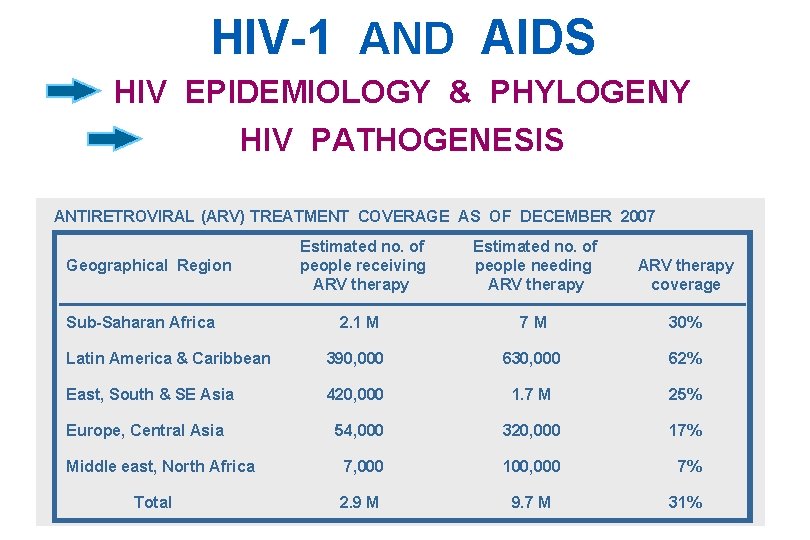
HIV-1 AND AIDS HIV EPIDEMIOLOGY & PHYLOGENY HIV PATHOGENESIS ANTIRETROVIRAL (ARV) TREATMENT COVERAGE AS OF DECEMBER 2007 Estimated no. of people receiving ARV therapy Estimated no. of people needing ARV therapy coverage 2. 1 M 7 M 30% Latin America & Caribbean 390, 000 630, 000 62% East, South & SE Asia 420, 000 1. 7 M 25% 54, 000 320, 000 17% 7, 000 100, 000 7% 2. 9 M 9. 7 M 31% Geographical Region Sub-Saharan Africa Europe, Central Asia Middle east, North Africa Total
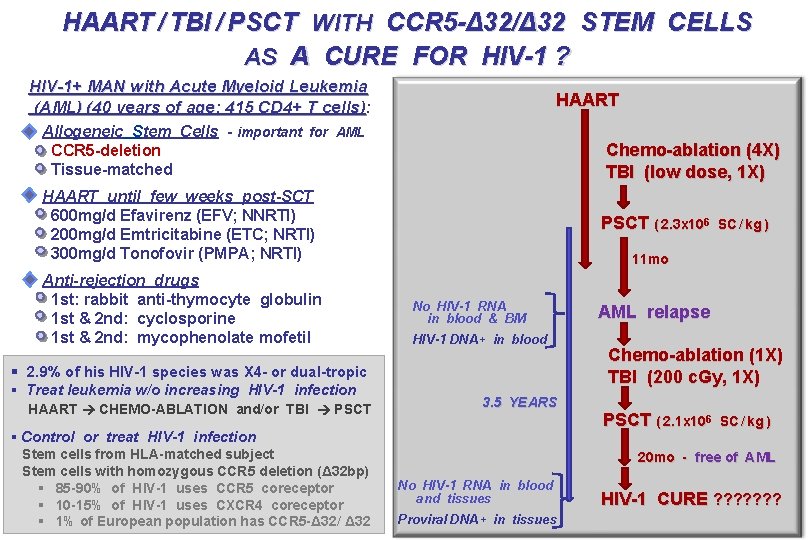
HAART / TBI / PSCT WITH CCR 5 -Δ 32/Δ 32 STEM CELLS AS A CURE FOR HIV-1 ? HIV-1+ MAN with Acute Myeloid Leukemia (AML) (40 years of age; 415 CD 4+ T cells): HAART Allogeneic Stem Cells - important for AML CCR 5 -deletion Tissue-matched Chemo-ablation (4 X) TBI (low dose, 1 X) HAART until few weeks post-SCT 600 mg/d Efavirenz (EFV; NNRTI) 200 mg/d Emtricitabine (ETC; NRTI) 300 mg/d Tonofovir (PMPA; NRTI) Anti-rejection drugs 1 st: rabbit anti-thymocyte globulin 1 st & 2 nd: cyclosporine 1 st & 2 nd: mycophenolate mofetil PSCT ( 2. 3 x 106 11 mo No HIV-1 RNA in blood & BM HIV-1 DNA+ in blood § 2. 9% of his HIV-1 species was X 4 - or dual-tropic § Treat leukemia w/o increasing HIV-1 infection HAART CHEMO-ABLATION and/or TBI PSCT § Control or treat HIV-1 infection Stem cells from HLA-matched subject Stem cells with homozygous CCR 5 deletion (Δ 32 bp) § 85 -90% of HIV-1 uses CCR 5 coreceptor § 10 -15% of HIV-1 uses CXCR 4 coreceptor § 1% of European population has CCR 5 -Δ 32/ Δ 32 SC / kg ) 3. 5 YEARS AML relapse Chemo-ablation (1 X) TBI (200 c. Gy, 1 X) PSCT ( 2. 1 x 106 SC / kg ) 20 mo - free of AML No HIV-1 RNA in blood and tissues Proviral DNA+ in tissues HIV-1 CURE ? ? ? ?
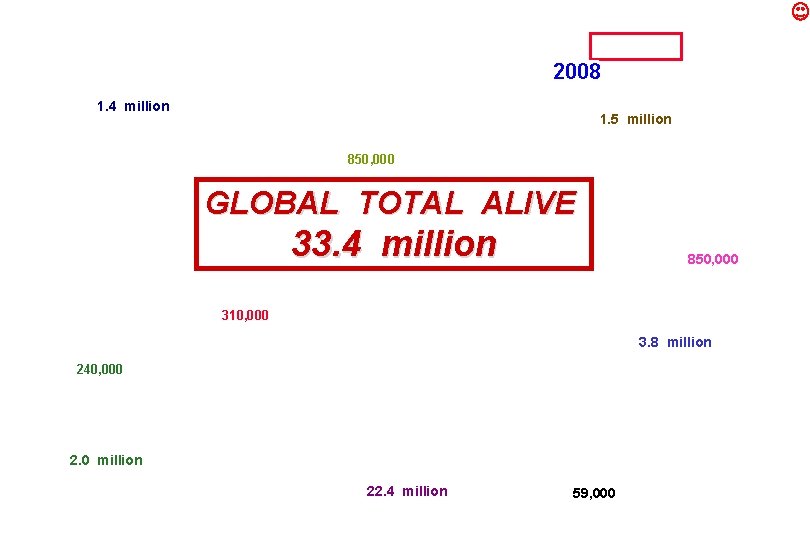
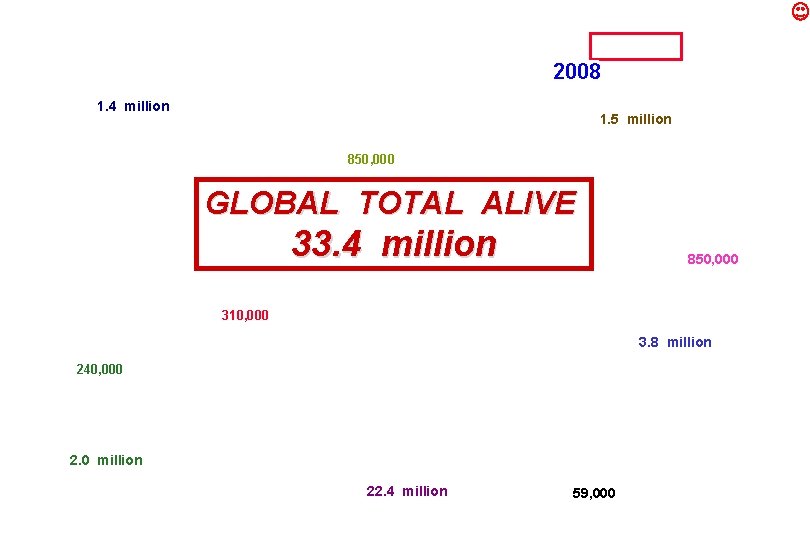
2008 1. 4 million 1. 5 million 850, 000 GLOBAL TOTAL ALIVE 33. 4 million 850, 000 310, 000 3. 8 million 240, 000 2. 0 million 22. 4 million 59, 000
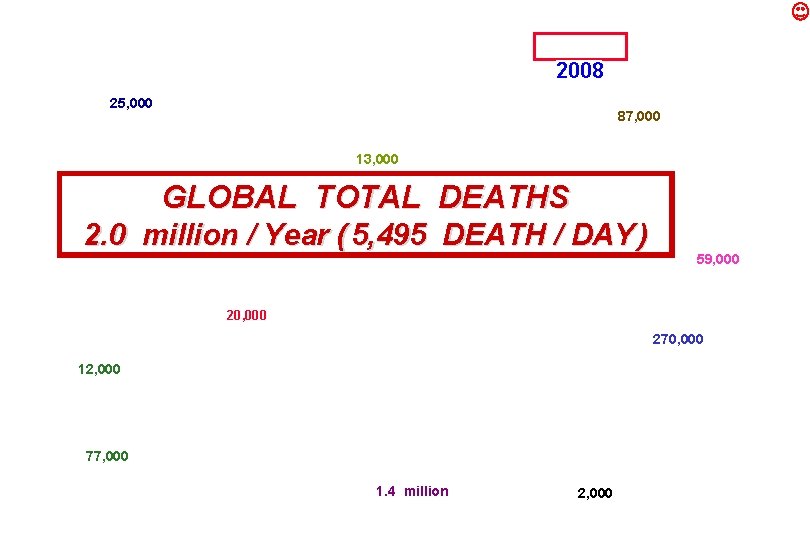
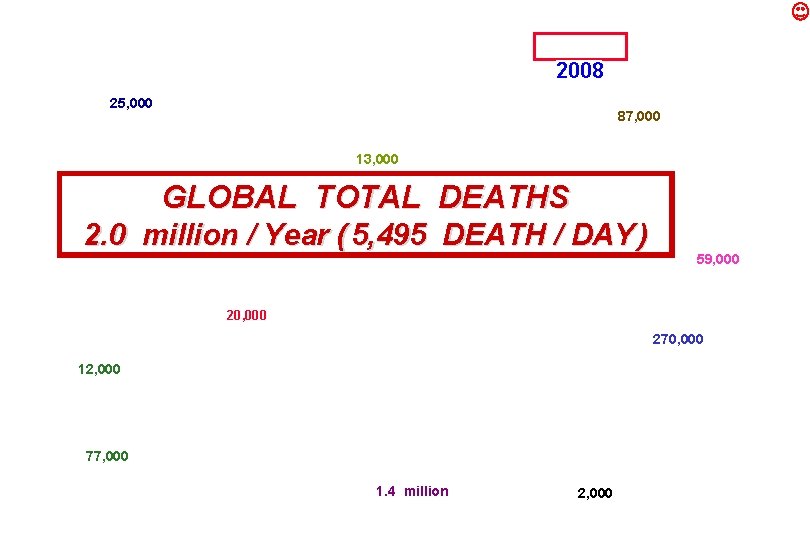
2008 25, 000 87, 000 13, 000 GLOBAL TOTAL DEATHS 2. 0 million / Year ( 5, 495 DEATH / DAY ) 59, 000 20, 000 270, 000 12, 000 77, 000 1. 4 million 2, 000
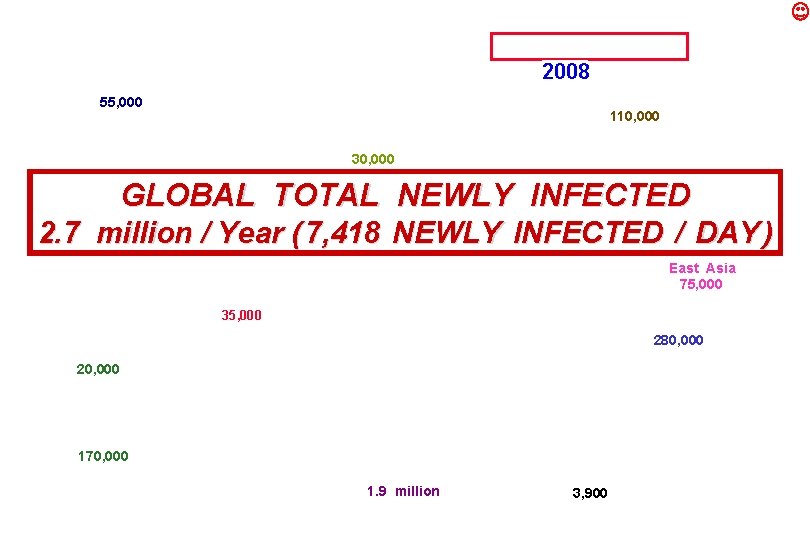
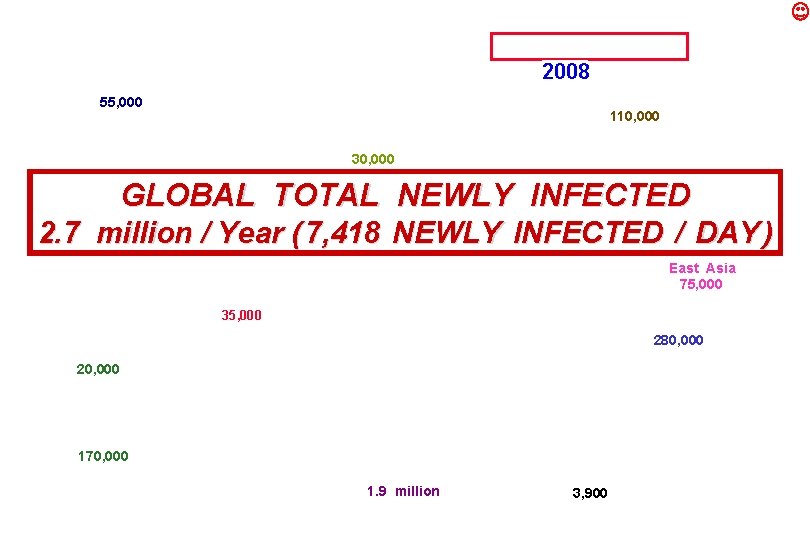
2008 55, 000 110, 000 30, 000 GLOBAL TOTAL NEWLY INFECTED 2. 7 million / Year ( 7, 418 NEWLY INFECTED / DAY ) East Asia 75, 000 35, 000 280, 000 20, 000 170, 000 1. 9 million 3, 900
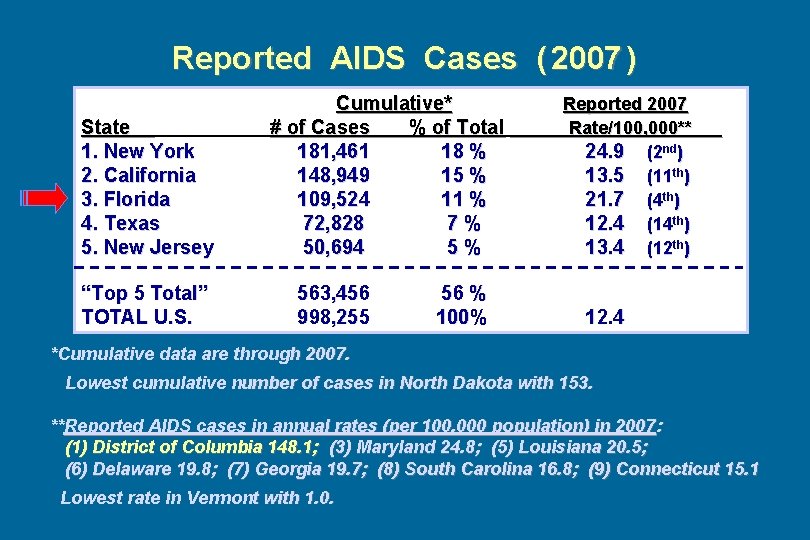
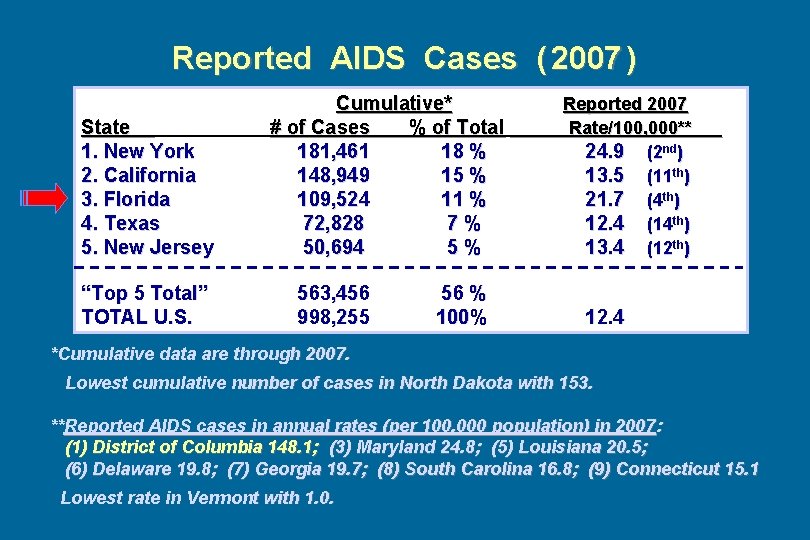
Reported AIDS Cases ( 2007 ) State 1. New York 2. California 3. Florida 4. Texas 5. New Jersey “Top 5 Total” TOTAL U. S. Cumulative* # of Cases % of Total 181, 461 18 % 148, 949 15 % 109, 524 11 % 72, 828 7% 50, 694 5% 563, 456 998, 255 56 % 100% Reported 2007 Rate/100, 000** 24. 9 (2 nd) 13. 5 (11 th) 21. 7 (4 th) 12. 4 (14 th) 13. 4 (12 th) . 12. 4 *Cumulative data are through 2007. Lowest cumulative number of cases in North Dakota with 153. **Reported AIDS cases in annual rates (per 100, 000 population) in 2007 : (1) District of Columbia 148. 1; (3) Maryland 24. 8; (5) Louisiana 20. 5; (6) Delaware 19. 8; (7) Georgia 19. 7; (8) South Carolina 16. 8; (9) Connecticut 15. 1 Lowest rate in Vermont with 1. 0.
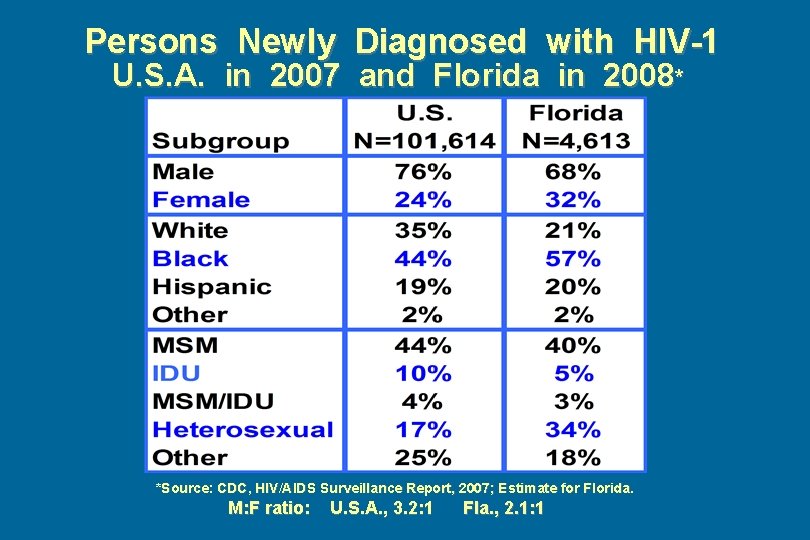
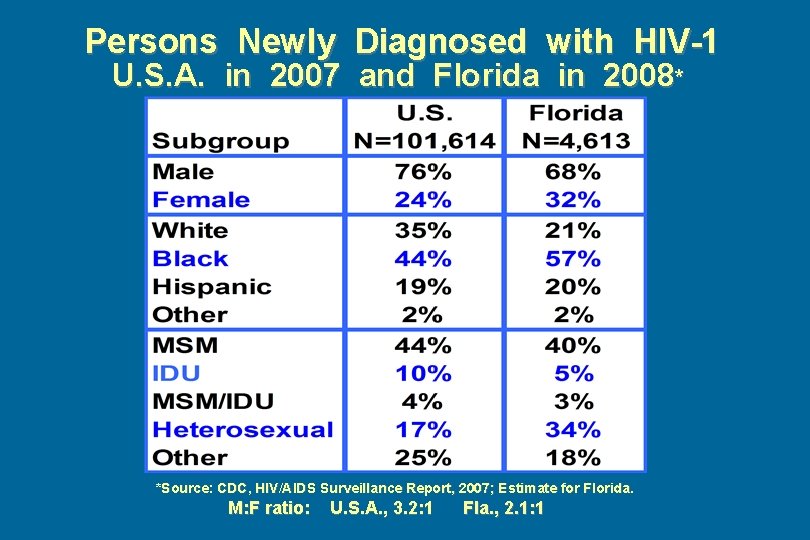
Persons Newly Diagnosed with HIV-1 U. S. A. in 2007 and Florida in 2008* *Source: CDC, HIV/AIDS Surveillance Report, 2007; Estimate for Florida. M: F ratio: U. S. A. , 3. 2: 1 Fla. , 2. 1: 1
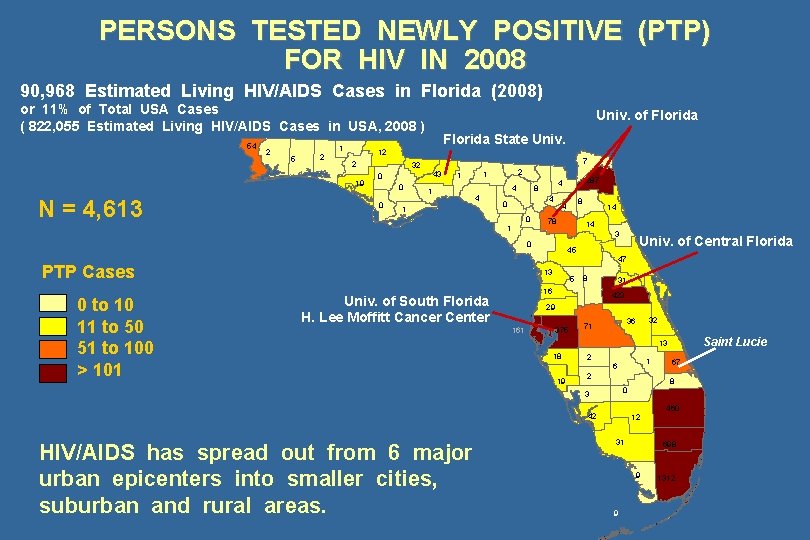
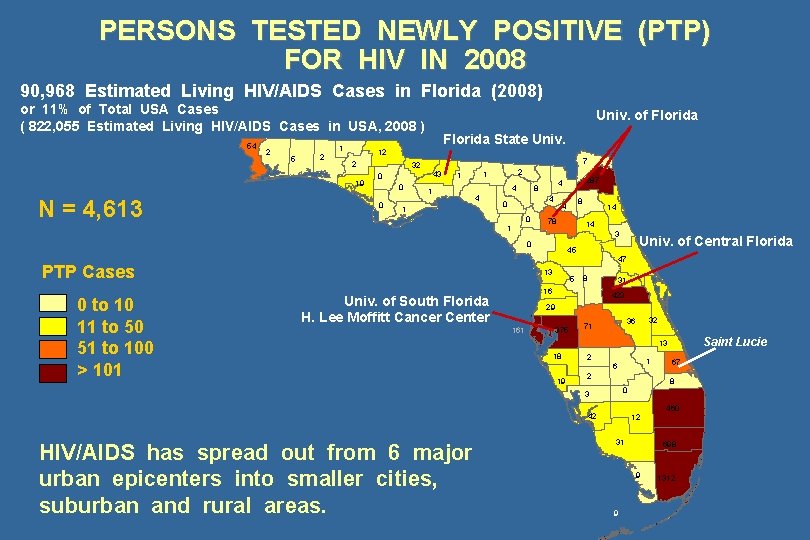
PERSONS TESTED NEWLY POSITIVE (PTP) FOR HIV IN 2008 90, 968 Estimated Living HIV/AIDS Cases in Florida (2008) or 11% of Total USA Cases ( 822, 055 Estimated Living HIV/AIDS Cases in USA, 2008 ) 54 2 5 2 1 Florida State Univ. 12 2 19 N = 4, 613 Univ. of Florida 7 32 43 0 0 0 1 2 1 1 4 4 1 4 0 0 1 287 4 8 78 14 14 3 0 PTP Cases 0 to 10 11 to 50 51 to 100 > 101 8 4 45 13 5 47 8 31 16 Univ. of South Florida H. Lee Moffitt Cancer Center Univ. of Central Florida 423 29 161 375 Saint Lucie 13 18 2 1 6 19 2 67 8 0 3 42 HIV/AIDS has spread out from 6 major urban epicenters into smaller cities, suburban and rural areas. 32 36 71 12 31 698 9 9 460 1312
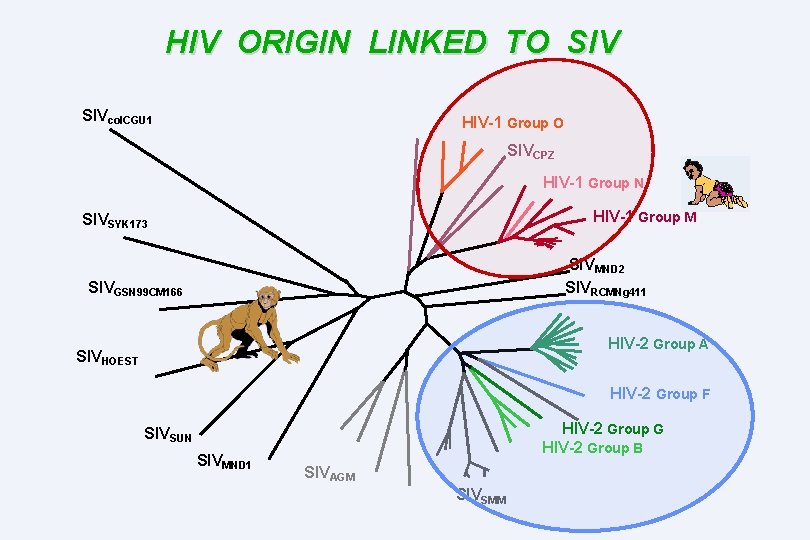
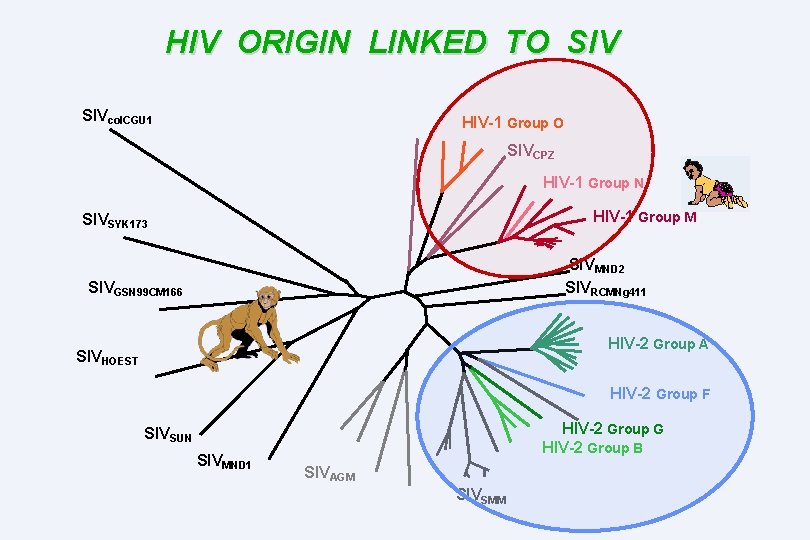
HIV ORIGIN LINKED TO SIVcol. CGU 1 HIV-1 Group O SIVCPZ HIV-1 Group N HIV-1 Group M SIVSYK 173 SIVMND 2 SIVRCMNg 411 SIVGSN 99 CM 166 HIV-2 Group A SIVHOEST HIV-2 Group F HIV-2 Group G HIV-2 Group B SIVSUN SIVMND 1 SIVAGM SIVSMM
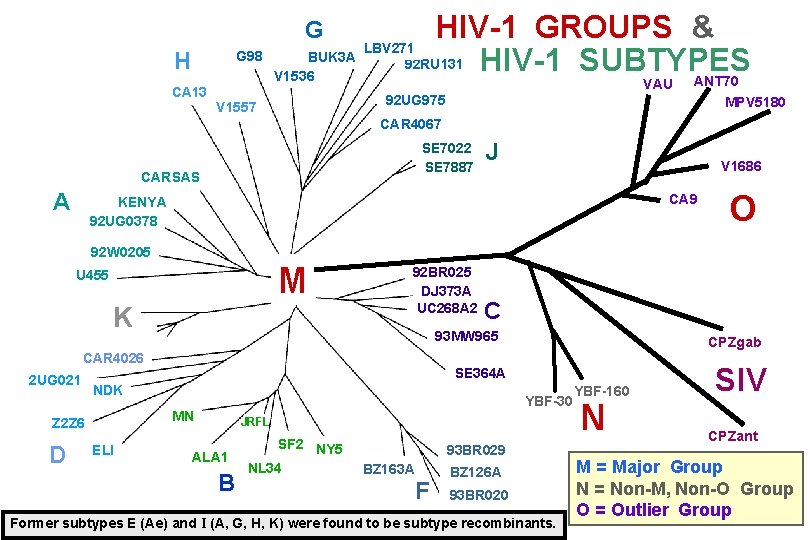
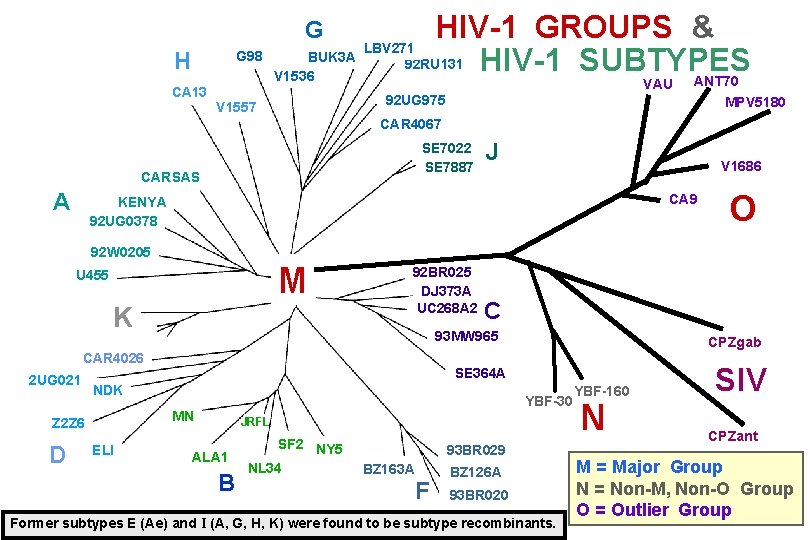
HIV-1 GROUPS & LBV 271 BUK 3 A 92 RU 131 HIV-1 SUBTYPES V 1536 ANT 70 G H G 98 CA 13 VAU 92 UG 975 V 1557 MPV 5180 CAR 4067 SE 7022 SE 7887 CARSAS A V 1686 CA 9 KENYA 92 UG 0378 92 W 0205 M U 455 K 92 BR 025 DJ 373 A UC 268 A 2 2 UG 021 YBF-30 MN ELI CPZgab SE 364 A NDK Z 2 Z 6 JRFL ALA 1 B SF 2 NY 5 NL 34 93 BR 029 BZ 163 A F O C 93 MW 965 CAR 4026 D J BZ 126 A 93 BR 020 Former subtypes E (Ae) and I (A, G, H, K) were found to be subtype recombinants. YBF-160 N SIV CPZant M = Major Group N = Non-M, Non-O Group O = Outlier Group
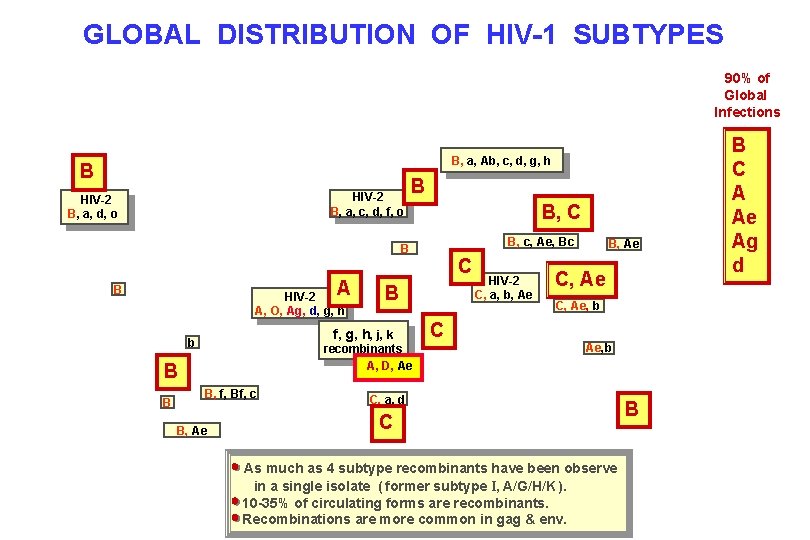
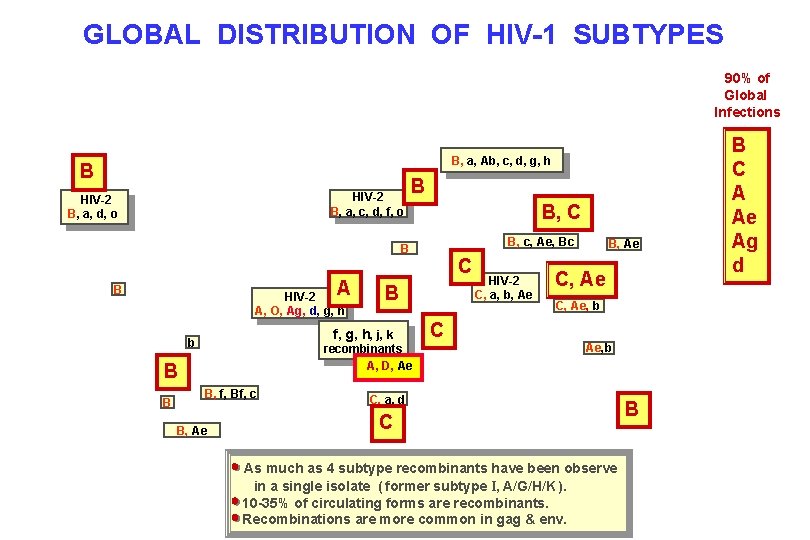
GLOBAL DISTRIBUTION OF HIV-1 SUBTYPES 90% of Global Infections B, a, Ab, c, d, g, h B HIV-2 B, a, c, d, f, o HIV-2 B, a, d, o B B, C B, c, Ae, Bc B A B HIV-2 A, O, Ag, d, g, h recombinants A, D, Ae B B f, g, h, j, k b B, f, Bf, c B, Ae C HIV-2 C, a, b, Ae B, Ae C, Ae, b CC Ae, b C, a, d C As much as 4 subtype recombinants have been observe in a single isolate ( former subtype I, A/G/H/K ). 10 -35% of circulating forms are recombinants. Recombinations are more common in gag & env. B B B C A Ae Ag d
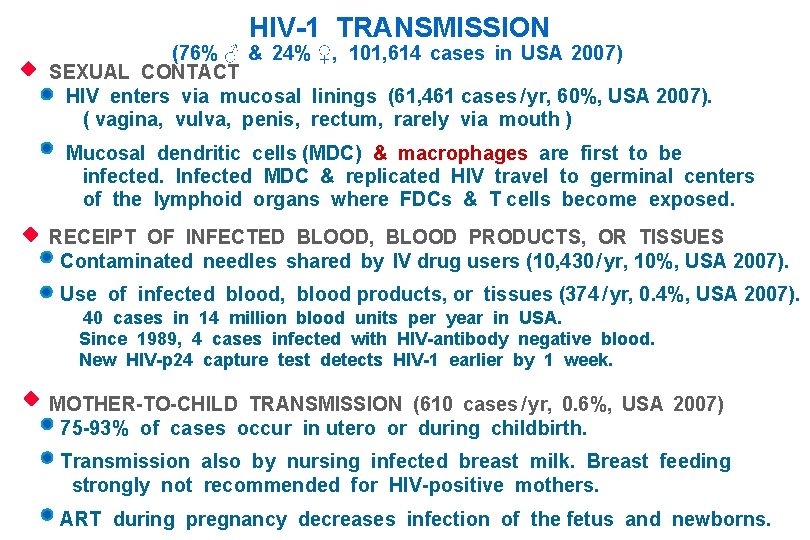
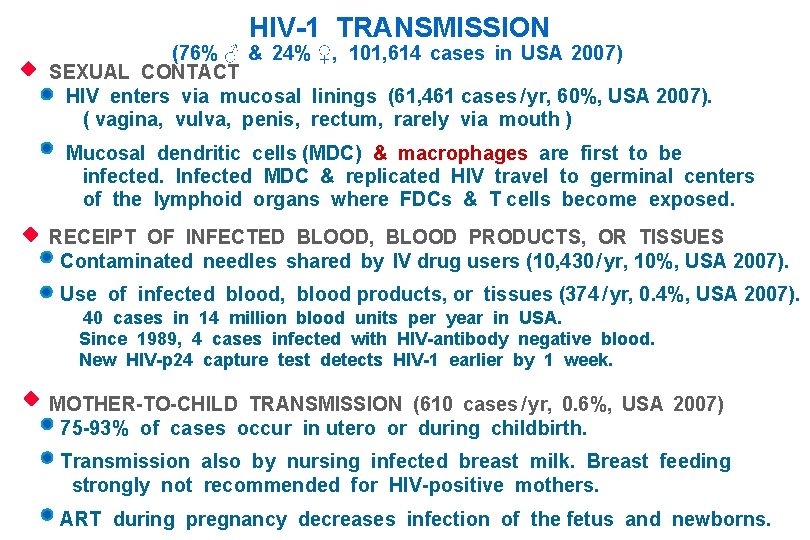
HIV-1 TRANSMISSION (76% ♂ & 24% ♀, 101, 614 cases in USA 2007) SEXUAL CONTACT HIV enters via mucosal linings (61, 461 cases / yr, 60%, USA 2007). ( vagina, vulva, penis, rectum, rarely via mouth ) Mucosal dendritic cells (MDC) & macrophages are first to be infected. Infected MDC & replicated HIV travel to germinal centers of the lymphoid organs where FDCs & T cells become exposed. RECEIPT OF INFECTED BLOOD, BLOOD PRODUCTS, OR TISSUES Contaminated needles shared by IV drug users (10, 430 / yr, 10%, USA 2007). Use of infected blood, blood products, or tissues (374 / yr, 0. 4%, USA 2007). 40 cases in 14 million blood units per year in USA. Since 1989, 4 cases infected with HIV-antibody negative blood. New HIV-p 24 capture test detects HIV-1 earlier by 1 week. MOTHER-TO-CHILD TRANSMISSION (610 cases / yr, 0. 6%, USA 2007) 75 -93% of cases occur in utero or during childbirth. Transmission also by nursing infected breast milk. Breast feeding strongly not recommended for HIV-positive mothers. ART during pregnancy decreases infection of the fetus and newborns.
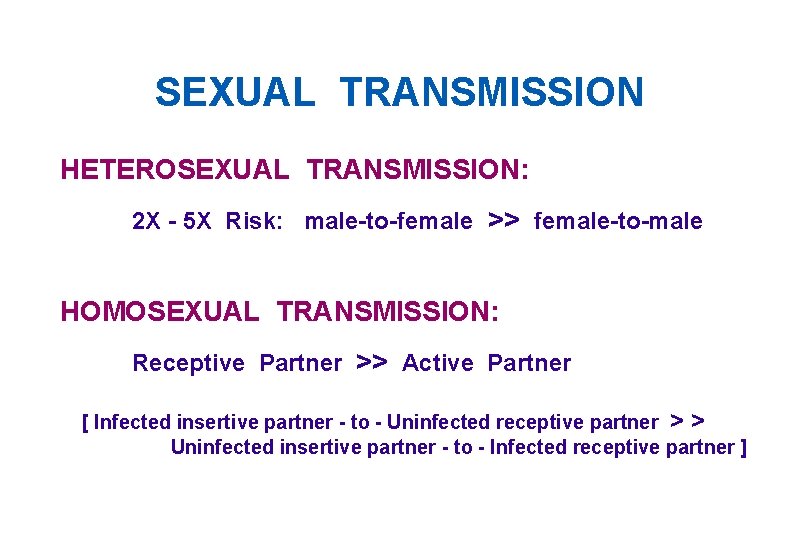
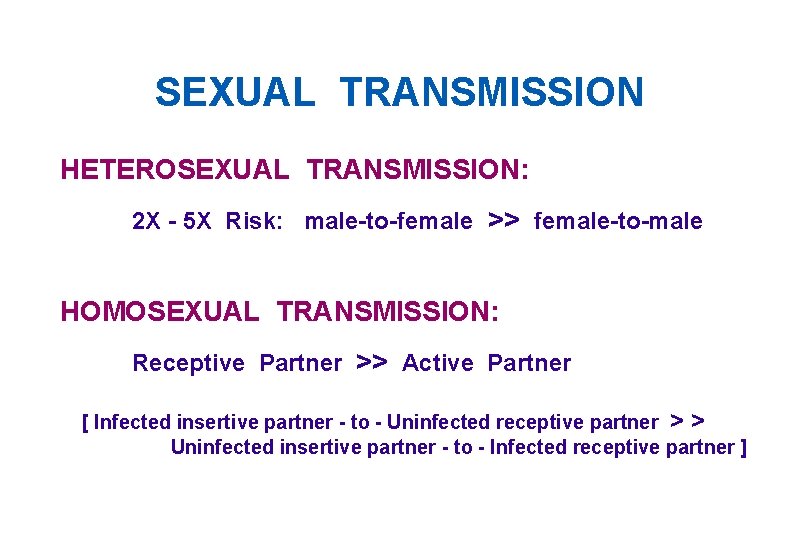
SEXUAL TRANSMISSION HETEROSEXUAL TRANSMISSION: 2 X - 5 X Risk: male-to-female >> female-to-male HOMOSEXUAL TRANSMISSION: Receptive Partner >> Active Partner [ Infected insertive partner - to - Uninfected receptive partner > > Uninfected insertive partner - to - Infected receptive partner ]
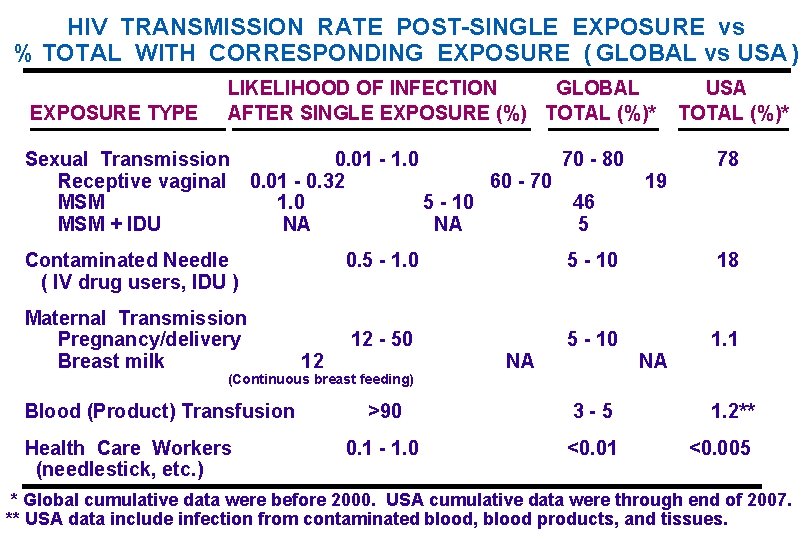
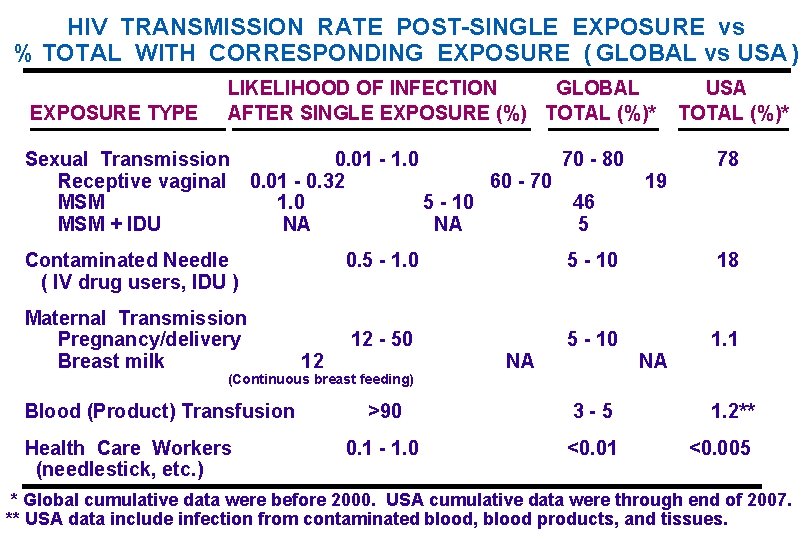
HIV TRANSMISSION RATE POST-SINGLE EXPOSURE vs % TOTAL WITH CORRESPONDING EXPOSURE ( GLOBAL vs USA ) EXPOSURE TYPE LIKELIHOOD OF INFECTION GLOBAL AFTER SINGLE EXPOSURE (%) TOTAL (%)* Sexual Transmission 0. 01 - 1. 0 70 - 80 Receptive vaginal 0. 01 - 0. 32 60 - 70 MSM 1. 0 5 - 10 46 MSM + IDU NA NA 5 Contaminated Needle ( IV drug users, IDU ) Maternal Transmission Pregnancy/delivery Breast milk 12 Health Care Workers (needlestick, etc. ) 78 0. 5 - 1. 0 5 - 10 18 12 - 50 5 - 10 1. 1 (Continuous breast feeding) Blood (Product) Transfusion 19 USA TOTAL (%)* NA NA >90 3 -5 1. 2** 0. 1 - 1. 0 <0. 01 <0. 005 * Global cumulative data were before 2000. USA cumulative data were through end of 2007. ** USA data include infection from contaminated blood, blood products, and tissues.
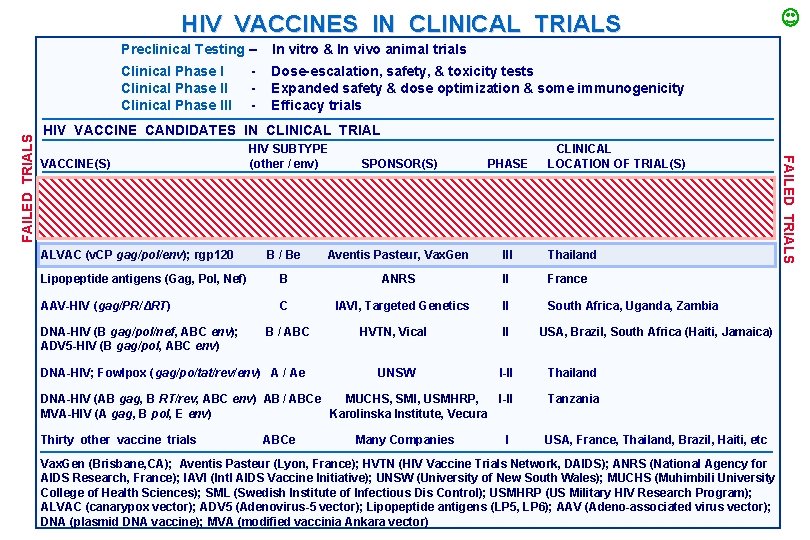
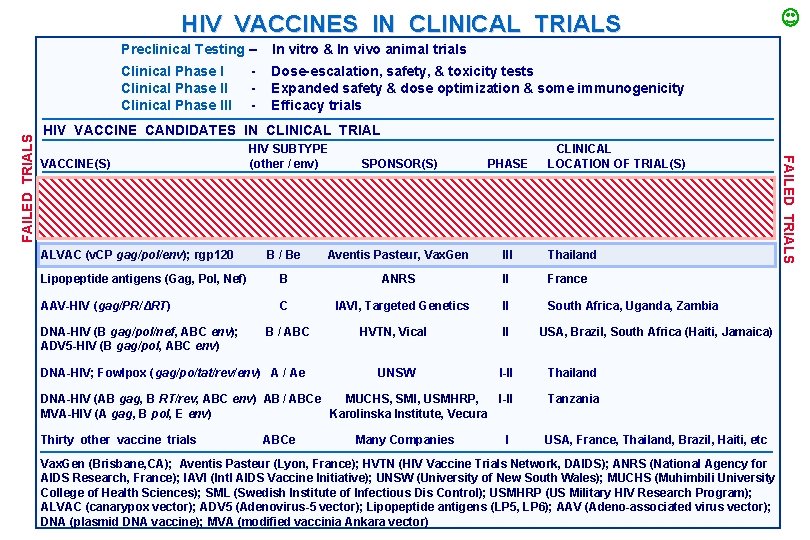
Preclinical Testing – In vitro & In vivo animal trials Clinical Phase III Dose-escalation, safety, & toxicity tests Expanded safety & dose optimization & some immunogenicity Efficacy trials - HIV VACCINE CANDIDATES IN CLINICAL TRIAL VACCINE(S) HIV SUBTYPE (other / env) CLINICAL LOCATION OF TRIAL(S) SPONSOR(S) PHASE BB Vax. Gen III USA B Merck, HVTN IIb USA, Canada, Peru, Haiti, Porto Rico, Dominican Republic, Australia B / Be Aventis Pasteur, Vax. Gen III Thailand Lipopeptide antigens (Gag, Pol, Nef) B ANRS II France AAV-HIV (gag/PR/ΔRT) C II South Africa, Uganda, Zambia rgp 120 Adenovirus 5 -gag/pol/nef ALVAC (v. CP gag/pol/env); rgp 120 DNA-HIV (B gag/pol/nef, ABC env); ADV 5 -HIV (B gag/pol, ABC env) B / ABC IAVI, Targeted Genetics HVTN, Vical II UNSW I-II Thailand DNA-HIV (AB gag, B RT/rev, ABC env) AB / ABCe MUCHS, SMI, USMHRP, I-II MVA-HIV (A gag, B pol, E env) Karolinska Institute, Vecura Tanzania Thirty other vaccine trials USA, France, Thailand, Brazil, Haiti, etc DNA-HIV; Fowlpox (gag/po/tat/rev/env) A / Ae ABCe Many Companies I USA, Brazil, South Africa (Haiti, Jamaica) Vax. Gen (Brisbane, CA); Aventis Pasteur (Lyon, France); HVTN (HIV Vaccine Trials Network, DAIDS); ANRS (National Agency for AIDS Research, France); IAVI (Intl AIDS Vaccine Initiative); UNSW (University of New South Wales); MUCHS (Muhimbili University College of Health Sciences); SML (Swedish Institute of Infectious Dis Control); USMHRP (US Military HIV Research Program); ALVAC (canarypox vector); ADV 5 (Adenovirus-5 vector); Lipopeptide antigens (LP 5, LP 6); AAV (Adeno-associated virus vector); DNA (plasmid DNA vaccine); MVA (modified vaccinia Ankara vector) FAILED TRIALS HIV VACCINES IN CLINICAL TRIALS
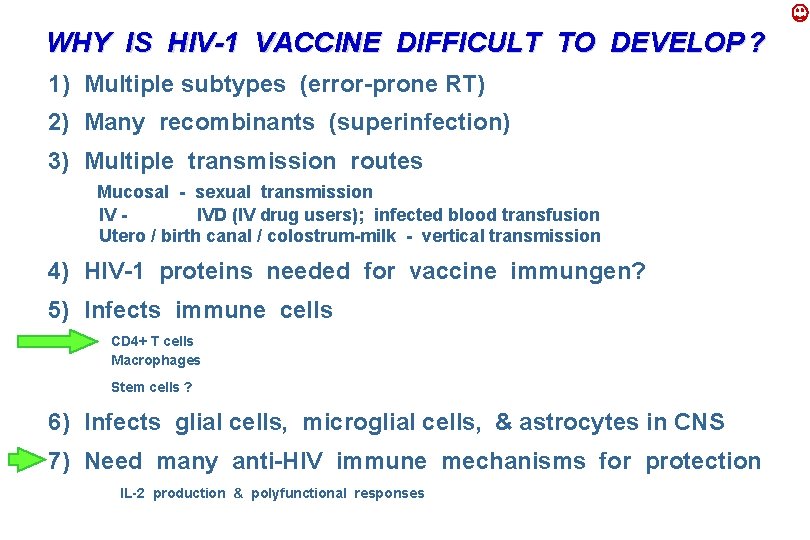
WHY IS HIV-1 VACCINE DIFFICULT TO DEVELOP ? 1) Multiple subtypes (error-prone RT) 2) Many recombinants (superinfection) 3) Multiple transmission routes Mucosal - sexual transmission IV IVD (IV drug users); infected blood transfusion Utero / birth canal / colostrum-milk - vertical transmission 4) HIV-1 proteins needed for vaccine immungen? 5) Infects immune cells CD 4+ T cells Macrophages Stem cells ? 6) Infects glial cells, microglial cells, & astrocytes in CNS 7) Need many anti-HIV immune mechanisms for protection IL-2 production & polyfunctional responses
QUESTION ( HIV EPIDEMIOLOGY & PHYLOGENY ) : 1) Which continent will be a major source of all HIV-1 subtypes? 2) What are the origins of HIV-1 and HIV-2? 3) Are the origins of HIV-1 and HIV-2 similar to HITLV-1, -2, -3 and -4? 4) Why is it so difficult to develop an HIV-1 vaccine? (State at least 3 reasons) 5) What is the most effective mode of HIV transmission?
 Kendall and marzano
Kendall and marzano Virus replication
Virus replication Characteristics of retrovirus
Characteristics of retrovirus Trascrittasi inversa retrovirus
Trascrittasi inversa retrovirus Kromatinstruktur
Kromatinstruktur Arborovirus
Arborovirus Retrovirus
Retrovirus Hiv retrovirus
Hiv retrovirus Gemmazione virus
Gemmazione virus Cell structure and taxonomy
Cell structure and taxonomy Conclusion on topic family
Conclusion on topic family Varies from family to family on the periodic table.
Varies from family to family on the periodic table. Blended family vs binuclear
Blended family vs binuclear Igbo family structure
Igbo family structure Yeast taxonomy
Yeast taxonomy Mnemonic for taxonomy
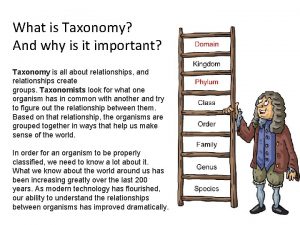
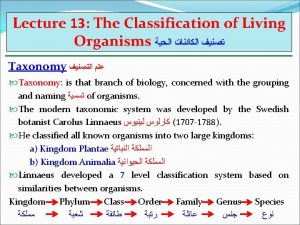
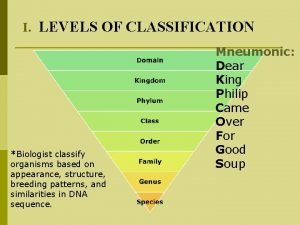
Mnemonic for taxonomy What is taxonomy and why is it important
What is taxonomy and why is it important Pros and cons of virtualization
Pros and cons of virtualization Mnemonic for taxonomy
Mnemonic for taxonomy Builder vs buyer in stm
Builder vs buyer in stm Thermodynamics is the branch of science that deals with
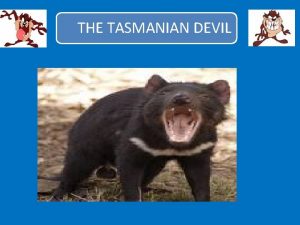
Thermodynamics is the branch of science that deals with Tasmanian devil habitat
Tasmanian devil habitat Technology business management council
Technology business management council Human order taxonomy
Human order taxonomy Genus order family
Genus order family Dear king phillip came over
Dear king phillip came over What genus do dogs belong to
What genus do dogs belong to Taxonomy project
Taxonomy project Structural bugs
Structural bugs What are the kingdoms in biology
What are the kingdoms in biology Harrows taxonomy
Harrows taxonomy Taxonomy of bugs
Taxonomy of bugs Taxonomy foldable
Taxonomy foldable Fink's taxonomy
Fink's taxonomy Systematics vs taxonomy
Systematics vs taxonomy Taxonomy vs systematics
Taxonomy vs systematics Zoology taxonomy
Zoology taxonomy Gri taxonomy
Gri taxonomy 18-2 modern evolutionary classification
18-2 modern evolutionary classification Flynn's classical taxonomy
Flynn's classical taxonomy Bloom taxonomy questions examples
Bloom taxonomy questions examples Marzano's taxonomy
Marzano's taxonomy Bloom's taxonomy ppt
Bloom's taxonomy ppt Apg system of classification
Apg system of classification Classification order of plants
Classification order of plants Unit 15 plant structures and taxonomy
Unit 15 plant structures and taxonomy Taxa biology
Taxa biology Metacognition bloom's taxonomy
Metacognition bloom's taxonomy Levels of questions in bloom's taxonomy
Levels of questions in bloom's taxonomy Thermoneutral
Thermoneutral Binomial nomenclature consists of two names *
Binomial nomenclature consists of two names * Nursing intervention examples
Nursing intervention examples What are the 8 levels of classification
What are the 8 levels of classification