Recent Developments in Patient Safety and Scope of

- Slides: 30
Recent Developments in Patient Safety and Scope of Patient Safety Special Interest Group Ali Rashidee, MD. MS. Co-Chair, Patient Safety SIG
PATIENT SAFETY: Estimates of medical errors The Harvard Medical Practice Study (Brennan TA et al. and Leape LL et al. Results of the Harvard Medical Practice Study. New England Journal of Medicine 324(6): 370 -376, and 377384 respectively, 1991. – adverse events in 3. 7% of hospitalization, and about 28% of these attributable to negligence. Although about 71% of these caused disabling injuries that lasted less than six months, 2. 6% caused permanent disability and 13. 6 percent lead to death. The Colorado and Utah Hospital Discharge Study (Thomas EJ et al. Incidence and Types of Adverse Events and Negligent Care in Utah and Colorado. Medical Care, Spring 2000) – adverse events in 2. 9% of hospitalizations, and 6. 6 % of these lead to death, and over half assessed to be preventable. When extrapolated to 33. 6 million admissions to US hospitals in 1997, the results of a study in Colorado and Utah conducted by Thomas E J et al. imply that at least 44, 000 Americans die each year as a result of medical errors. Another study by Leape L L et al. . at Harvard Medical Practice Study, 1991 suggests 98, 000 deaths due to medical errors- AHA Hospital Statistics.
Burden of medical errors § Even when using the lower estimate, deaths due to medical errors exceed the number attributable to the 8 th leading cause of death. Death: Final data for 1997. CDC-National Vital Statistics Reports. 47(19): 27, 1999. § More people die in a given year as a result of medical errors than from motor vehicle accidents (~44, 000), breast cancer (~43, 000) or AIDS(~16, 500). Births and Deaths: Preliminary data for 1998. CDC, National Vital Statistics Reports. 47(25): 6, 1999. § Medication error along, occurring either in or out of hospitals, are estimated to account for 7000 deaths annually. Phillips DP et al. Increase in US medication error deaths between 1983 and 1993. The Lancet, 351: 643 -44, 1998. § Total national cost of preventable adverse events are estimated between 17 billion of which health care costs represent one half. Thomas EJ et al. Cost of Medical Injuries in Utah and Colorado. Inquiry 36: 225 -264, 1999 and Johnson WJ et al. The economic consequences of medical injuries, JAMA. 267: 2487 -2492, 1992. § The Quality in Australian Health Care Study (Wilson RM et al. The Quality in Australian Health Care Study. The Medical Journal of Australia. 163(9): 458 -71, 1995 – 16. 6 percent of hospital admissions involved adverse events, half of those considered preventable. About 14 percent of adverse events were found to have resulted in permanent disability, with 4. 9 percent resulting in death.
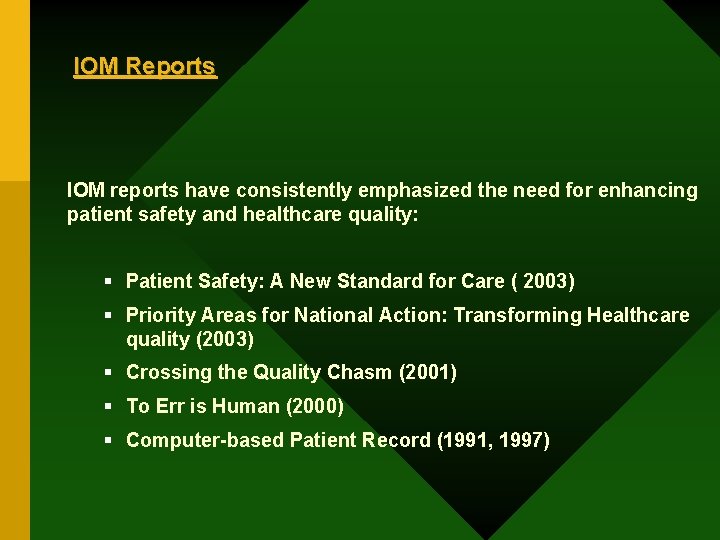
IOM Reports IOM reports have consistently emphasized the need for enhancing patient safety and healthcare quality: § Patient Safety: A New Standard for Care ( 2003) § Priority Areas for National Action: Transforming Healthcare quality (2003) § Crossing the Quality Chasm (2001) § To Err is Human (2000) § Computer-based Patient Record (1991, 1997)
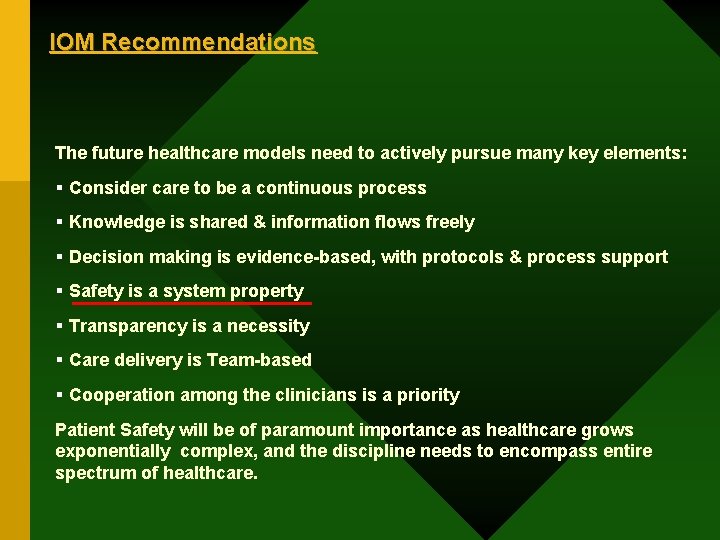
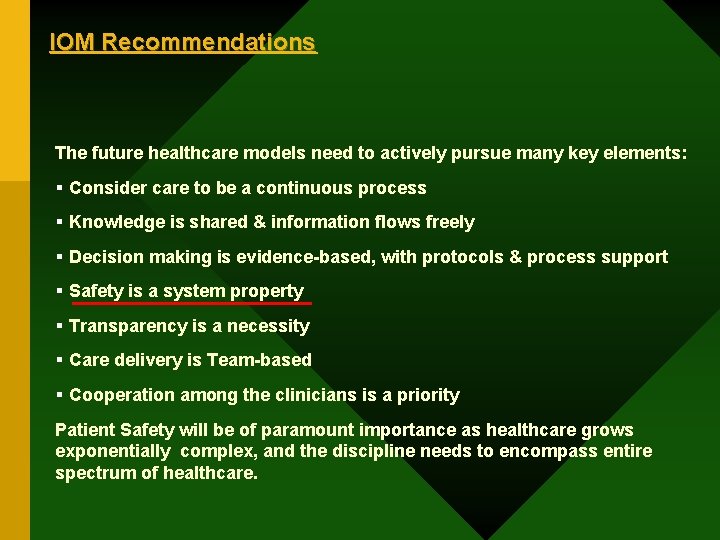
IOM Recommendations The future healthcare models need to actively pursue many key elements: § Consider care to be a continuous process § Knowledge is shared & information flows freely § Decision making is evidence-based, with protocols & process support § Safety is a system property § Transparency is a necessity § Care delivery is Team-based § Cooperation among the clinicians is a priority Patient Safety will be of paramount importance as healthcare grows exponentially complex, and the discipline needs to encompass entire spectrum of healthcare.
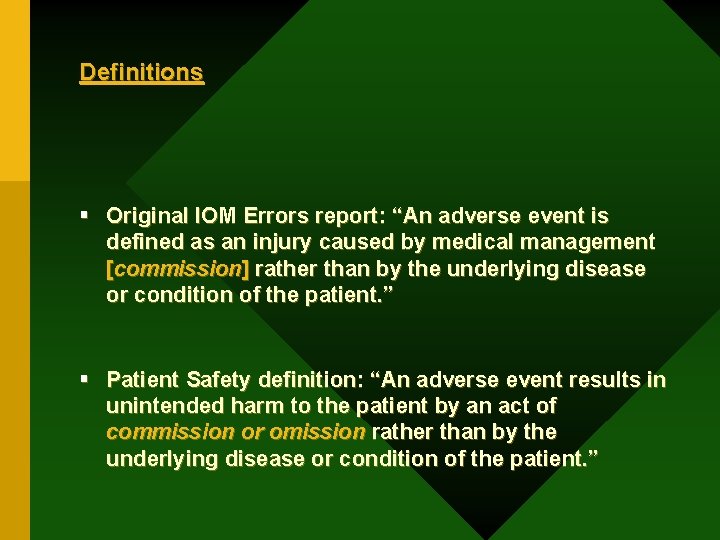
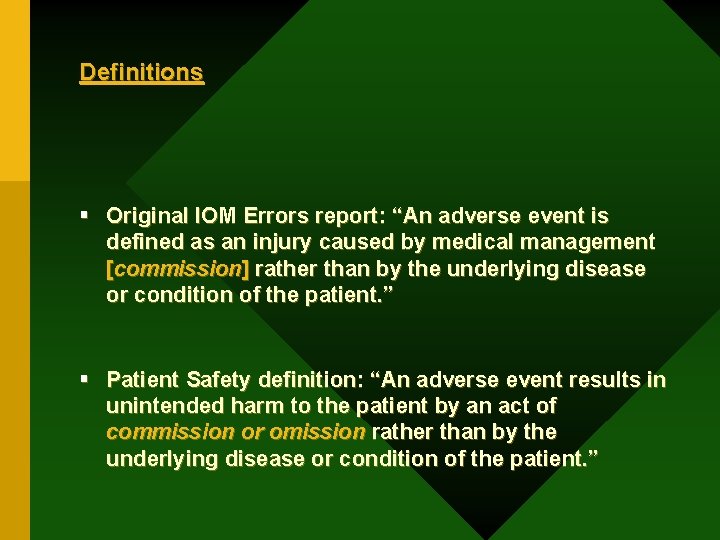
Definitions § Original IOM Errors report: “An adverse event is defined as an injury caused by medical management [commission] rather than by the underlying disease or condition of the patient. ” § Patient Safety definition: “An adverse event results in unintended harm to the patient by an act of commission or omission rather than by the underlying disease or condition of the patient. ”
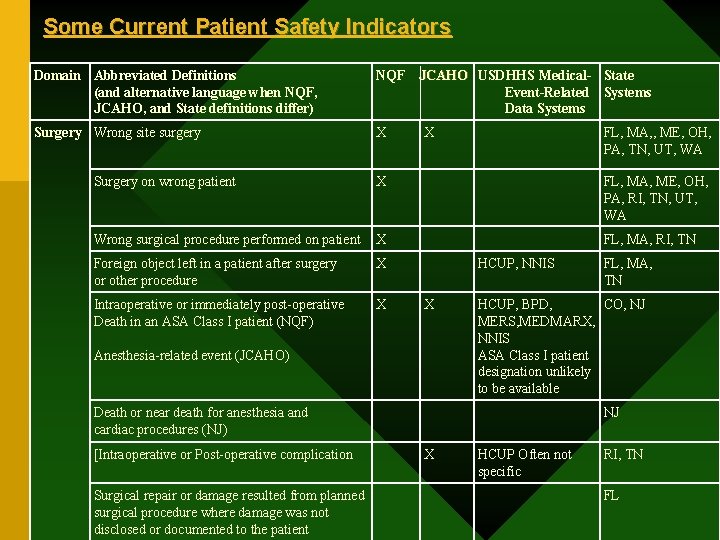
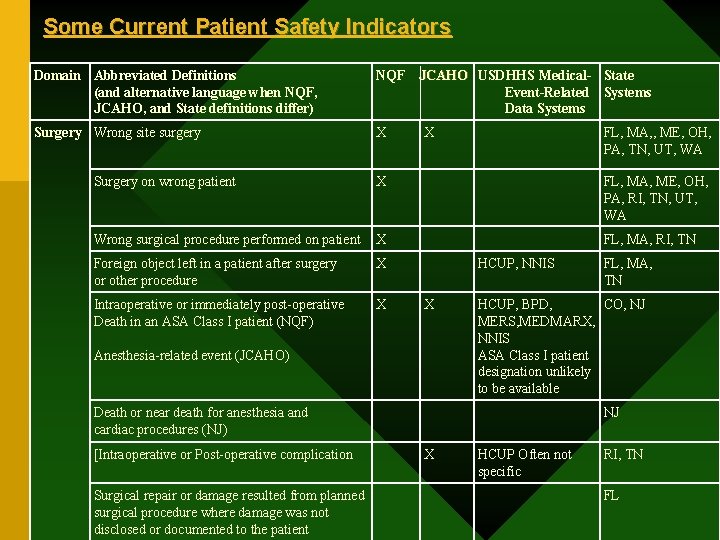
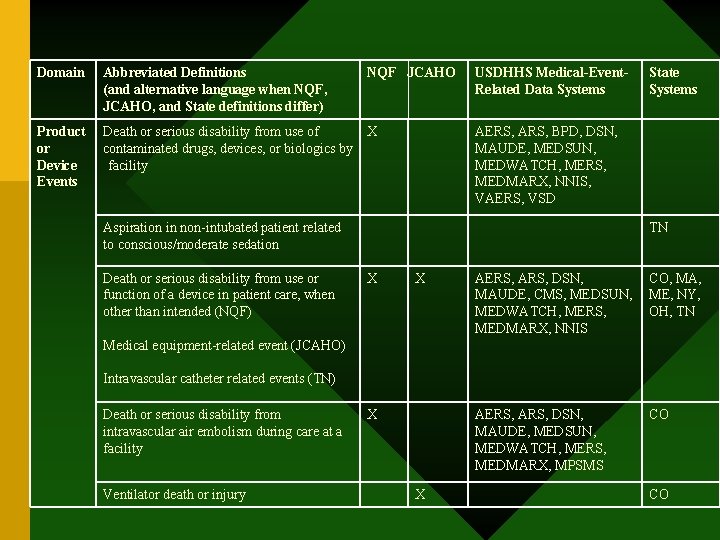
Some Current Patient Safety Indicators Domain Abbreviated Definitions (and alternative language when NQF, JCAHO, and State definitions differ) NQF JCAHO USDHHS Medical- State Event-Related Systems Data Systems Surgery Wrong site surgery X X FL, MA, , ME, OH, PA, TN, UT, WA Surgery on wrong patient X FL, MA, ME, OH, PA, RI, TN, UT, WA Wrong surgical procedure performed on patient X FL, MA, RI, TN Foreign object left in a patient after surgery or other procedure X Intraoperative or immediately post-operative Death in an ASA Class I patient (NQF) X HCUP, NNIS X Anesthesia-related event (JCAHO) HCUP, BPD, CO, NJ MERS, MEDMARX, NNIS ASA Class I patient designation unlikely to be available Death or near death for anesthesia and cardiac procedures (NJ) [Intraoperative or Post-operative complication Surgical repair or damage resulted from planned surgical procedure where damage was not disclosed or documented to the patient FL, MA, TN NJ X HCUP Often not specific RI, TN FL
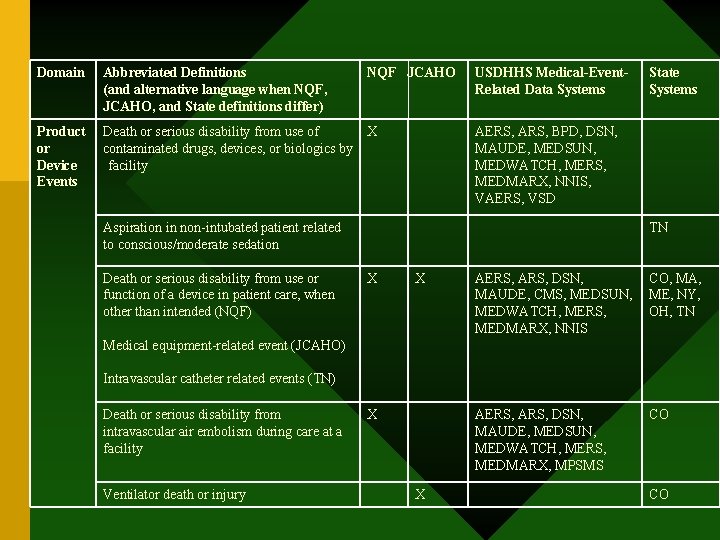
Domain Abbreviated Definitions (and alternative language when NQF, JCAHO, and State definitions differ) NQF JCAHO USDHHS Medical-Event. Related Data Systems Product or Device Events Death or serious disability from use of contaminated drugs, devices, or biologics by facility X AERS, ARS, BPD, DSN, MAUDE, MEDSUN, MEDWATCH, MERS, MEDMARX, NNIS, VAERS, VSD Aspiration in non-intubated patient related to conscious/moderate sedation Death or serious disability from use or function of a device in patient care, when other than intended (NQF) State Systems TN X X AERS, ARS, DSN, MAUDE, CMS, MEDSUN, MEDWATCH, MERS, MEDMARX, NNIS CO, MA, ME, NY, OH, TN AERS, ARS, DSN, MAUDE, MEDSUN, MEDWATCH, MERS, MEDMARX, MPSMS CO Medical equipment-related event (JCAHO) Intravascular catheter related events (TN) Death or serious disability from intravascular air embolism during care at a facility Ventilator death or injury X X CO
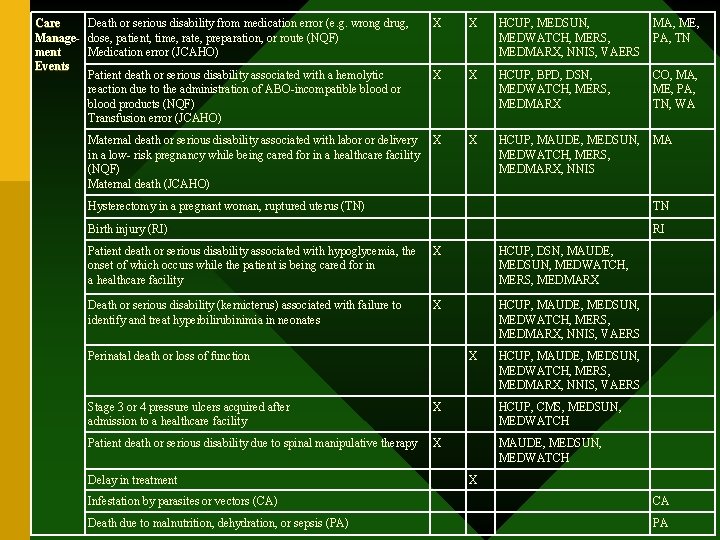
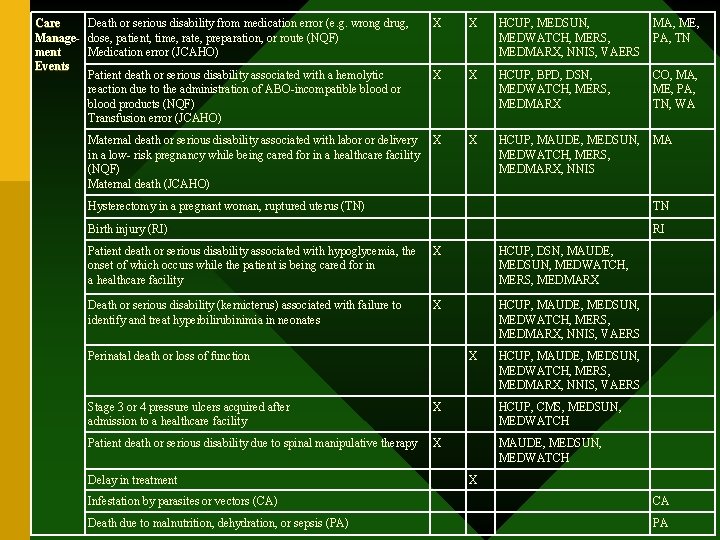
Care Death or serious disability from medication error (e. g. wrong drug, Manage- dose, patient, time, rate, preparation, or route (NQF) ment Medication error (JCAHO) Events Patient death or serious disability associated with a hemolytic reaction due to the administration of ABO-incompatible blood or blood products (NQF) Transfusion error (JCAHO) Maternal death or serious disability associated with labor or delivery in a low- risk pregnancy while being cared for in a healthcare facility (NQF) Maternal death (JCAHO) X X HCUP, MEDSUN, MEDWATCH, MERS, MEDMARX, NNIS, VAERS MA, ME, PA, TN X X HCUP, BPD, DSN, MEDWATCH, MERS, MEDMARX CO, MA, ME, PA, TN, WA X X HCUP, MAUDE, MEDSUN, MEDWATCH, MERS, MEDMARX, NNIS MA Hysterectomy in a pregnant woman, ruptured uterus (TN) TN Birth injury (RI) RI Patient death or serious disability associated with hypoglycemia, the onset of which occurs while the patient is being cared for in a healthcare facility X HCUP, DSN, MAUDE, MEDSUN, MEDWATCH, MERS, MEDMARX Death or serious disability (kernicterus) associated with failure to identify and treat hyperbilirubinimia in neonates X HCUP, MAUDE, MEDSUN, MEDWATCH, MERS, MEDMARX, NNIS, VAERS Perinatal death or loss of function X HCUP, MAUDE, MEDSUN, MEDWATCH, MERS, MEDMARX, NNIS, VAERS Stage 3 or 4 pressure ulcers acquired after admission to a healthcare facility X HCUP, CMS, MEDSUN, MEDWATCH Patient death or serious disability due to spinal manipulative therapy X MAUDE, MEDSUN, MEDWATCH Delay in treatment X Infestation by parasites or vectors (CA) CA Death due to malnutrition, dehydration, or sepsis (PA) PA
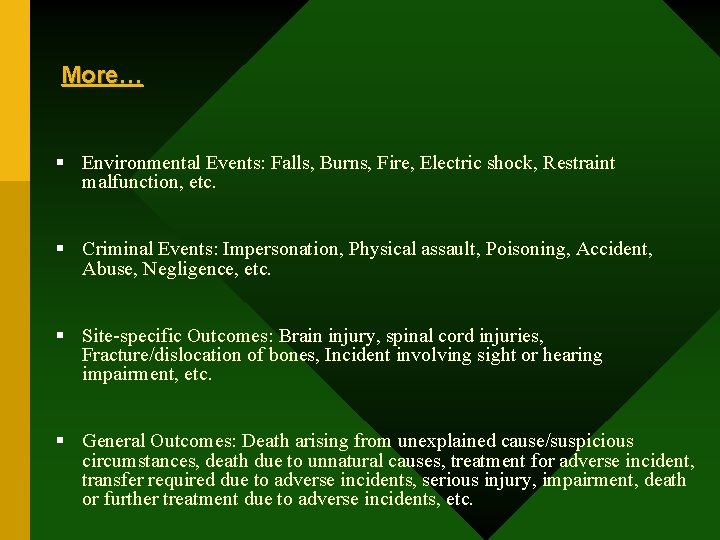
More… § Environmental Events: Falls, Burns, Fire, Electric shock, Restraint malfunction, etc. § Criminal Events: Impersonation, Physical assault, Poisoning, Accident, Abuse, Negligence, etc. § Site-specific Outcomes: Brain injury, spinal cord injuries, Fracture/dislocation of bones, Incident involving sight or hearing impairment, etc. § General Outcomes: Death arising from unexplained cause/suspicious circumstances, death due to unnatural causes, treatment for adverse incident, transfer required due to adverse incidents, serious injury, impairment, death or further treatment due to adverse incidents, etc.
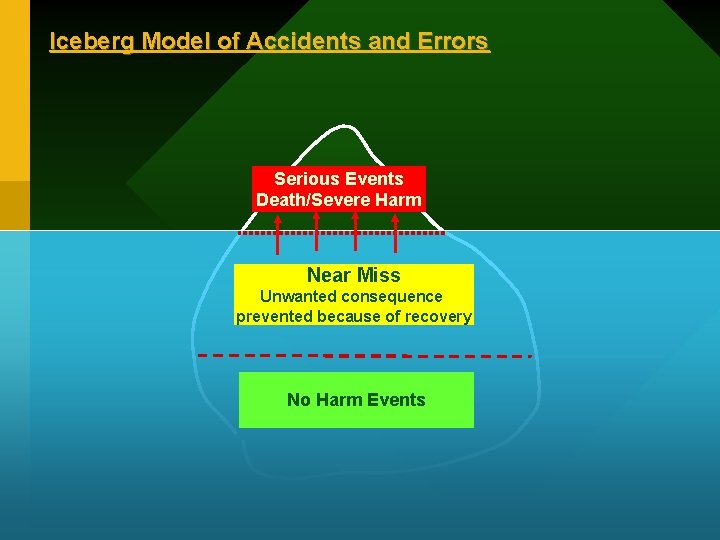
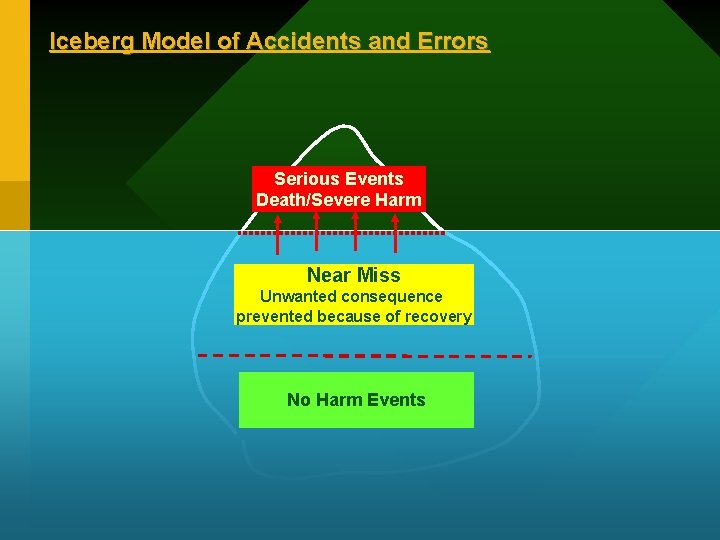
Iceberg Model of Accidents and Errors Serious Events Death/Severe Harm Near Miss Unwanted consequence prevented because of recovery No Harm Events
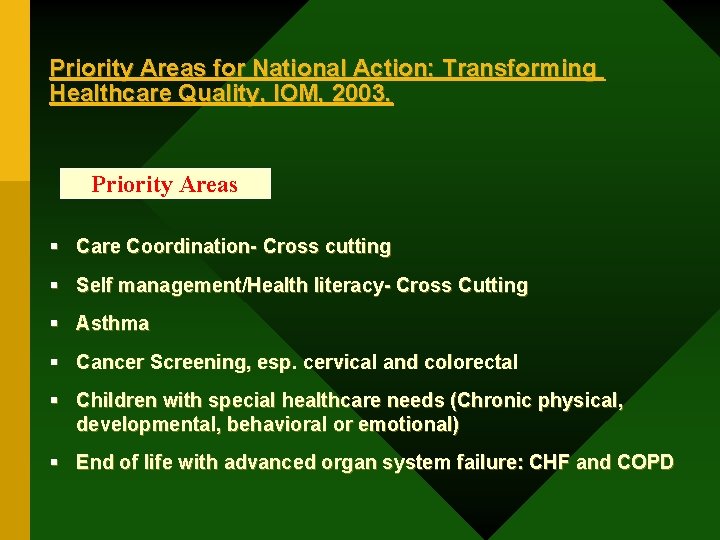
Priority Areas for National Action: Transforming Healthcare Quality, IOM, 2003. Priority Areas § Care Coordination- Cross cutting § Self management/Health literacy- Cross Cutting § Asthma § Cancer Screening, esp. cervical and colorectal § Children with special healthcare needs (Chronic physical, developmental, behavioral or emotional) § End of life with advanced organ system failure: CHF and COPD
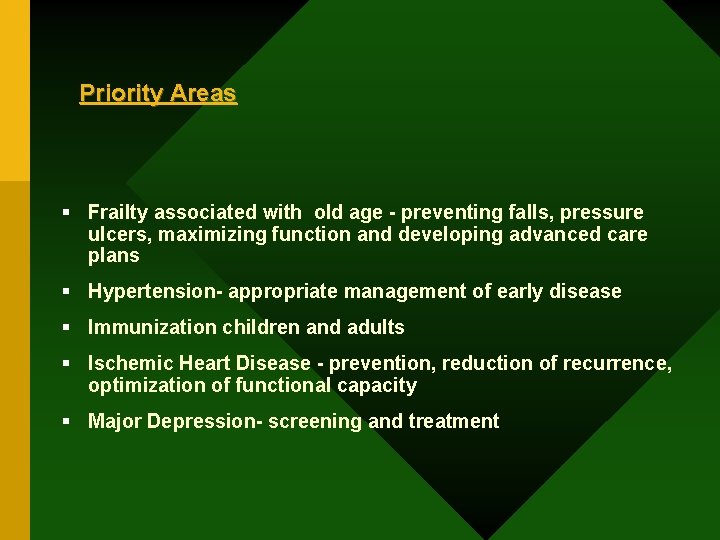
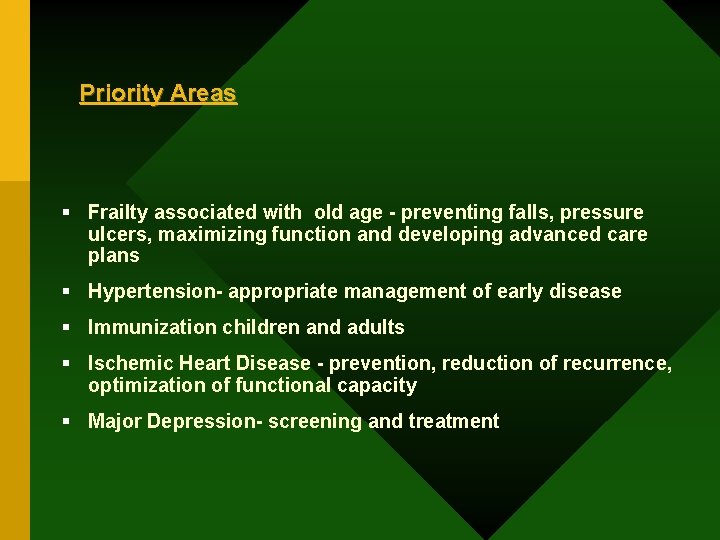
Priority Areas § Frailty associated with old age - preventing falls, pressure ulcers, maximizing function and developing advanced care plans § Hypertension- appropriate management of early disease § Immunization children and adults § Ischemic Heart Disease - prevention, reduction of recurrence, optimization of functional capacity § Major Depression- screening and treatment
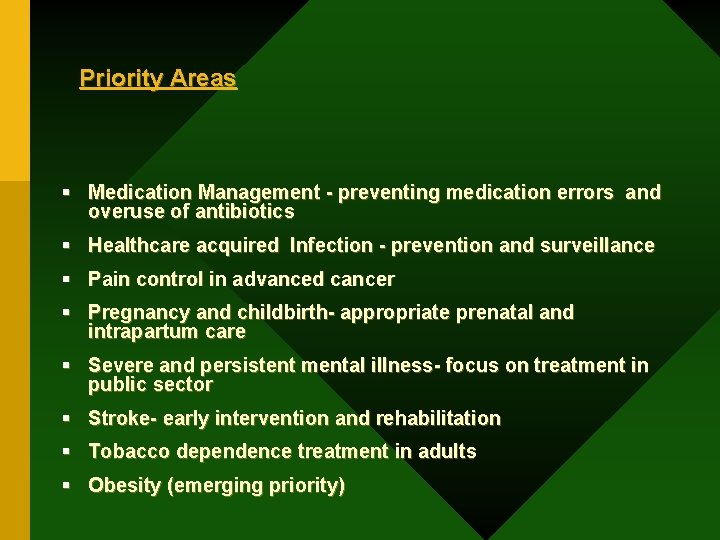
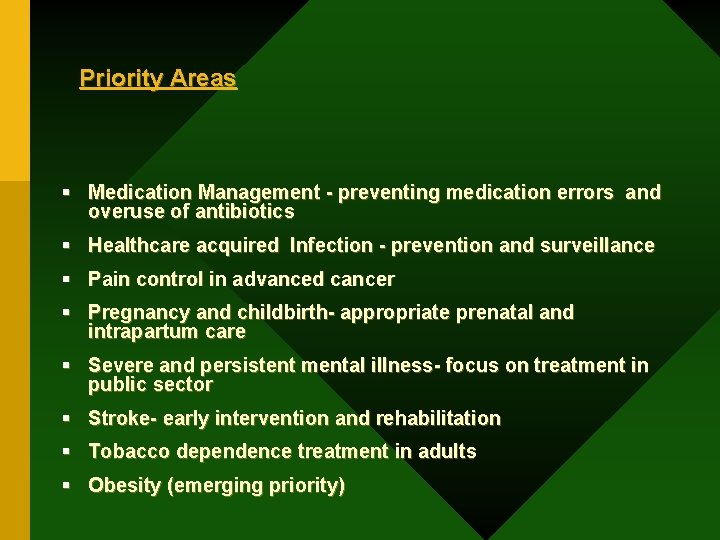
Priority Areas § Medication Management - preventing medication errors and overuse of antibiotics § Healthcare acquired Infection - prevention and surveillance § Pain control in advanced cancer § Pregnancy and childbirth- appropriate prenatal and intrapartum care § Severe and persistent mental illness- focus on treatment in public sector § Stroke- early intervention and rehabilitation § Tobacco dependence treatment in adults § Obesity (emerging priority)
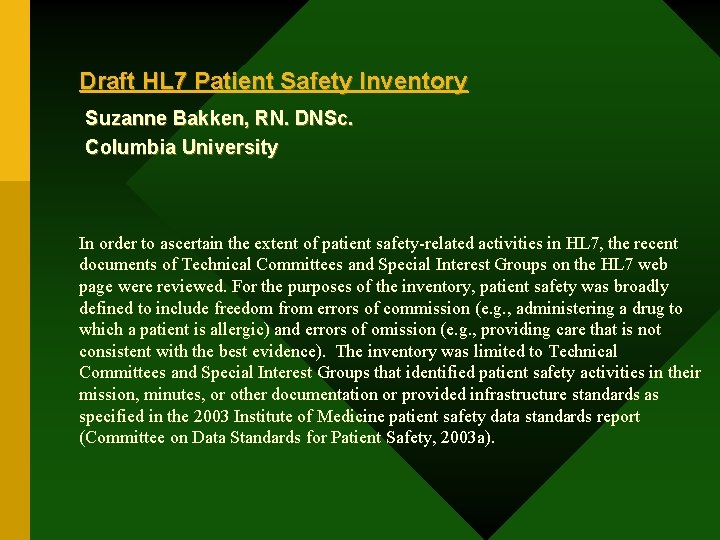
Draft HL 7 Patient Safety Inventory Suzanne Bakken, RN. DNSc. Columbia University In order to ascertain the extent of patient safety-related activities in HL 7, the recent documents of Technical Committees and Special Interest Groups on the HL 7 web page were reviewed. For the purposes of the inventory, patient safety was broadly defined to include freedom from errors of commission (e. g. , administering a drug to which a patient is allergic) and errors of omission (e. g. , providing care that is not consistent with the best evidence). The inventory was limited to Technical Committees and Special Interest Groups that identified patient safety activities in their mission, minutes, or other documentation or provided infrastructure standards as specified in the 2003 Institute of Medicine patient safety data standards report (Committee on Data Standards for Patient Safety, 2003 a).
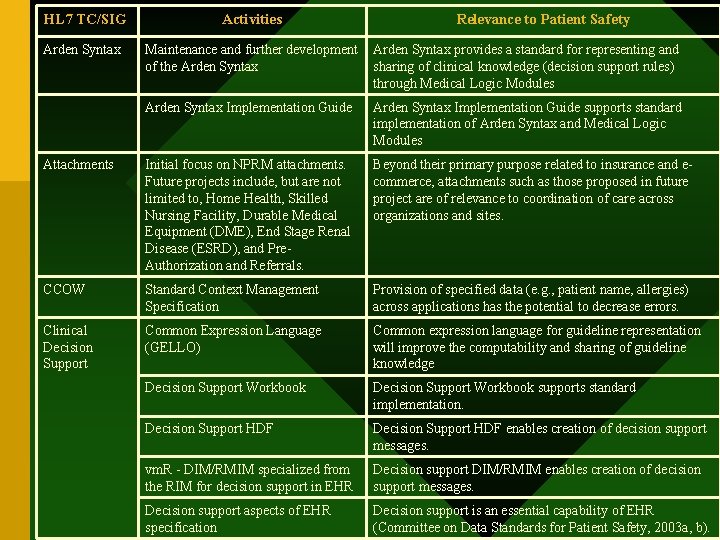
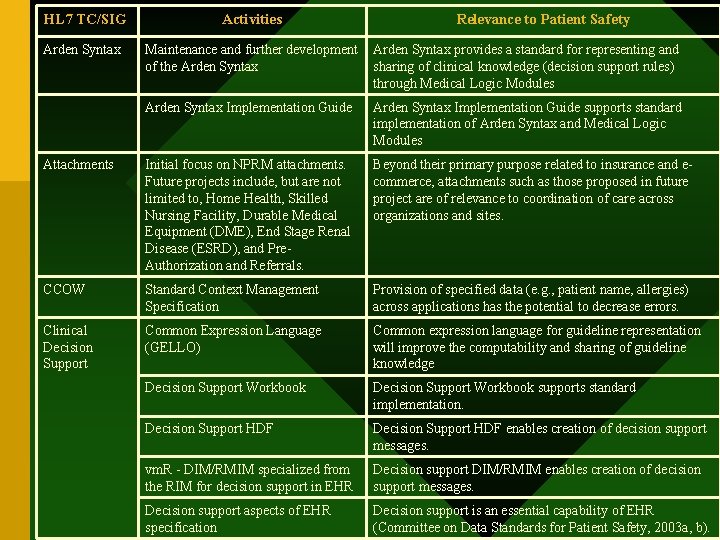
HL 7 TC/SIG Activities Relevance to Patient Safety Arden Syntax Maintenance and further development of the Arden Syntax provides a standard for representing and sharing of clinical knowledge (decision support rules) through Medical Logic Modules Arden Syntax Implementation Guide supports standard implementation of Arden Syntax and Medical Logic Modules Attachments Initial focus on NPRM attachments. Future projects include, but are not limited to, Home Health, Skilled Nursing Facility, Durable Medical Equipment (DME), End Stage Renal Disease (ESRD), and Pre. Authorization and Referrals. Beyond their primary purpose related to insurance and ecommerce, attachments such as those proposed in future project are of relevance to coordination of care across organizations and sites. CCOW Standard Context Management Specification Provision of specified data (e. g. , patient name, allergies) across applications has the potential to decrease errors. Clinical Decision Support Common Expression Language (GELLO) Common expression language for guideline representation will improve the computability and sharing of guideline knowledge Decision Support Workbook supports standard implementation. Decision Support HDF enables creation of decision support messages. vm. R - DIM/RMIM specialized from the RIM for decision support in EHR Decision support DIM/RMIM enables creation of decision support messages. Decision support aspects of EHR specification Decision support is an essential capability of EHR (Committee on Data Standards for Patient Safety, 2003 a, b).
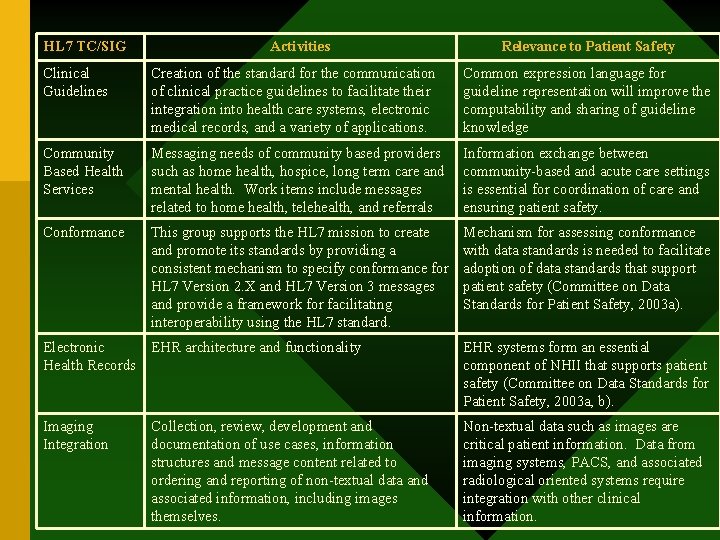
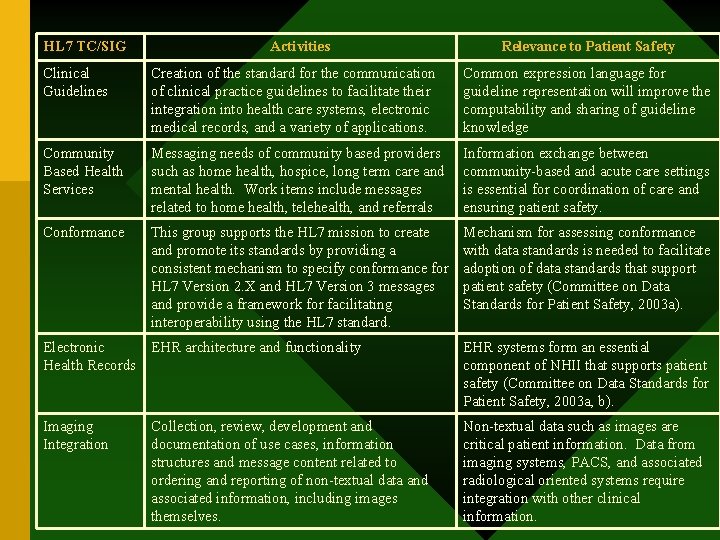
HL 7 TC/SIG Activities Relevance to Patient Safety Clinical Guidelines Creation of the standard for the communication of clinical practice guidelines to facilitate their integration into health care systems, electronic medical records, and a variety of applications. Common expression language for guideline representation will improve the computability and sharing of guideline knowledge Community Based Health Services Messaging needs of community based providers such as home health, hospice, long term care and mental health. Work items include messages related to home health, telehealth, and referrals Information exchange between community-based and acute care settings is essential for coordination of care and ensuring patient safety. Conformance This group supports the HL 7 mission to create and promote its standards by providing a consistent mechanism to specify conformance for HL 7 Version 2. X and HL 7 Version 3 messages and provide a framework for facilitating interoperability using the HL 7 standard. Mechanism for assessing conformance with data standards is needed to facilitate adoption of data standards that support patient safety (Committee on Data Standards for Patient Safety, 2003 a). Electronic Health Records EHR architecture and functionality EHR systems form an essential component of NHII that supports patient safety (Committee on Data Standards for Patient Safety, 2003 a, b). Imaging Integration Collection, review, development and documentation of use cases, information structures and message content related to ordering and reporting of non-textual data and associated information, including images themselves. Non-textual data such as images are critical patient information. Data from imaging systems, PACS, and associated radiological oriented systems require integration with other clinical information.
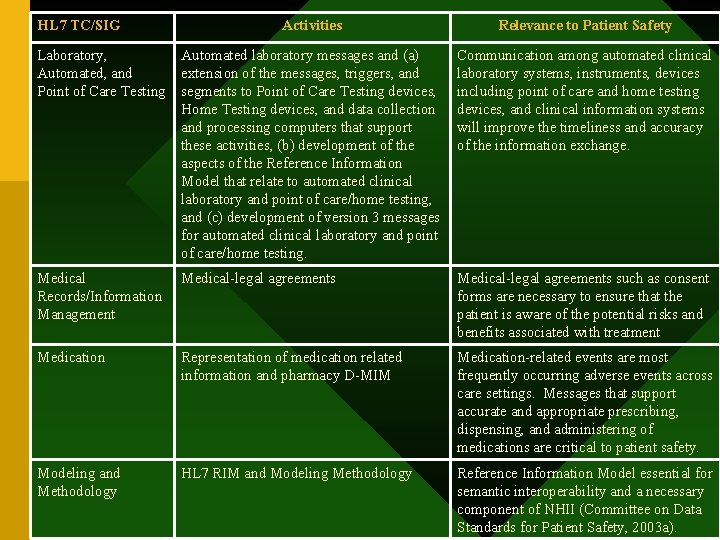
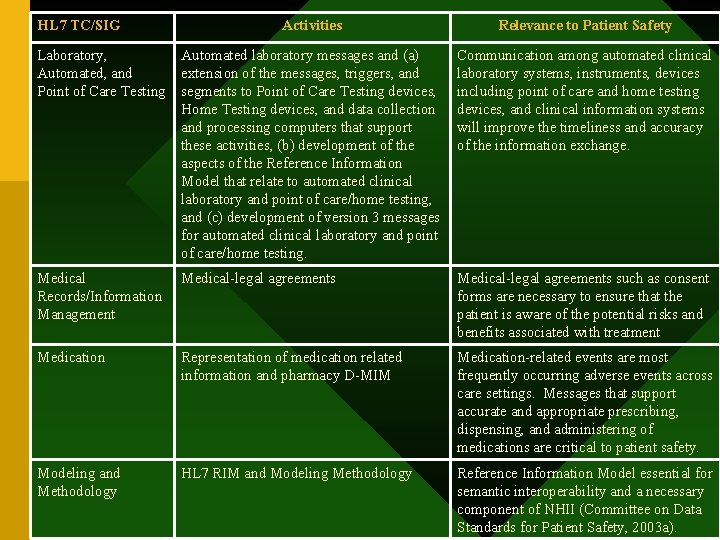
HL 7 TC/SIG Activities Relevance to Patient Safety Laboratory, Automated, and Point of Care Testing Automated laboratory messages and (a) extension of the messages, triggers, and segments to Point of Care Testing devices, Home Testing devices, and data collection and processing computers that support these activities, (b) development of the aspects of the Reference Information Model that relate to automated clinical laboratory and point of care/home testing, and (c) development of version 3 messages for automated clinical laboratory and point of care/home testing. Communication among automated clinical laboratory systems, instruments, devices including point of care and home testing devices, and clinical information systems will improve the timeliness and accuracy of the information exchange. Medical Records/Information Management Medical-legal agreements such as consent forms are necessary to ensure that the patient is aware of the potential risks and benefits associated with treatment Medication Representation of medication related information and pharmacy D-MIM Medication-related events are most frequently occurring adverse events across care settings. Messages that support accurate and appropriate prescribing, dispensing, and administering of medications are critical to patient safety. Modeling and Methodology HL 7 RIM and Modeling Methodology Reference Information Model essential for semantic interoperability and a necessary component of NHII (Committee on Data Standards for Patient Safety, 2003 a).
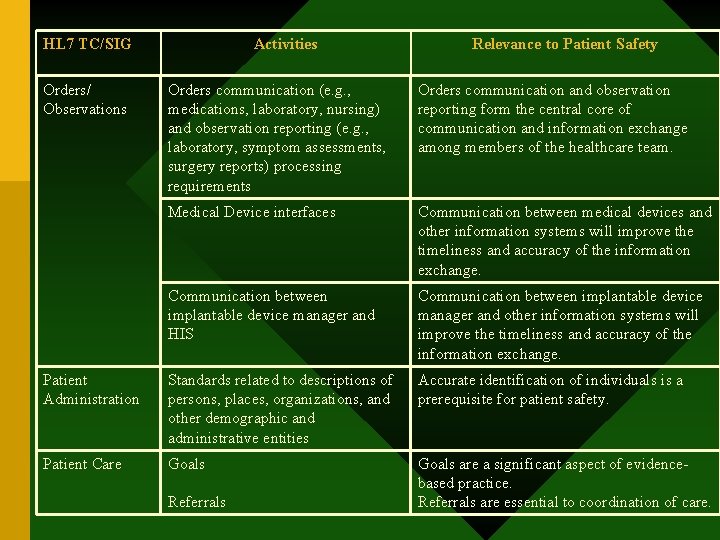
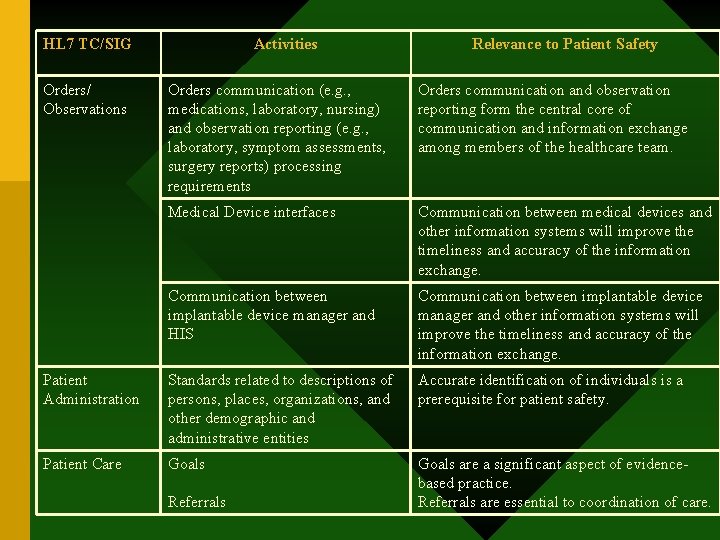
HL 7 TC/SIG Orders/ Observations Activities Relevance to Patient Safety Orders communication (e. g. , medications, laboratory, nursing) and observation reporting (e. g. , laboratory, symptom assessments, surgery reports) processing requirements Orders communication and observation reporting form the central core of communication and information exchange among members of the healthcare team. Medical Device interfaces Communication between medical devices and other information systems will improve the timeliness and accuracy of the information exchange. Communication between implantable device manager and HIS Communication between implantable device manager and other information systems will improve the timeliness and accuracy of the information exchange. Patient Administration Standards related to descriptions of persons, places, organizations, and other demographic and administrative entities Accurate identification of individuals is a prerequisite for patient safety. Patient Care Goals are a significant aspect of evidencebased practice. Referrals are essential to coordination of care. Referrals
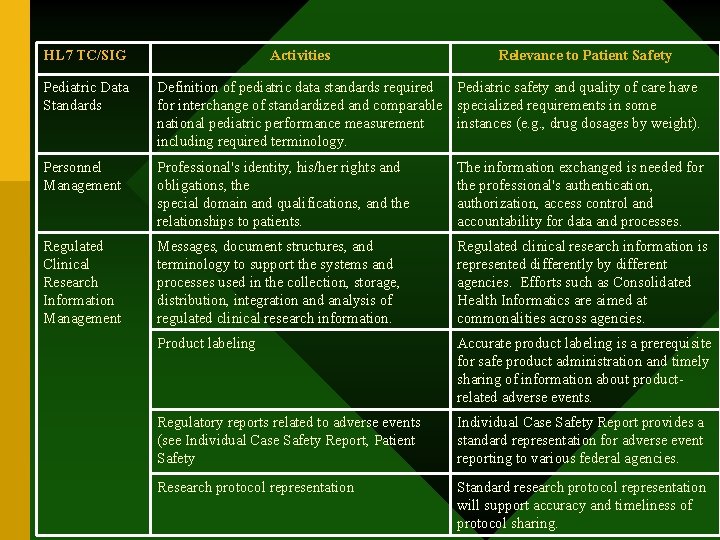
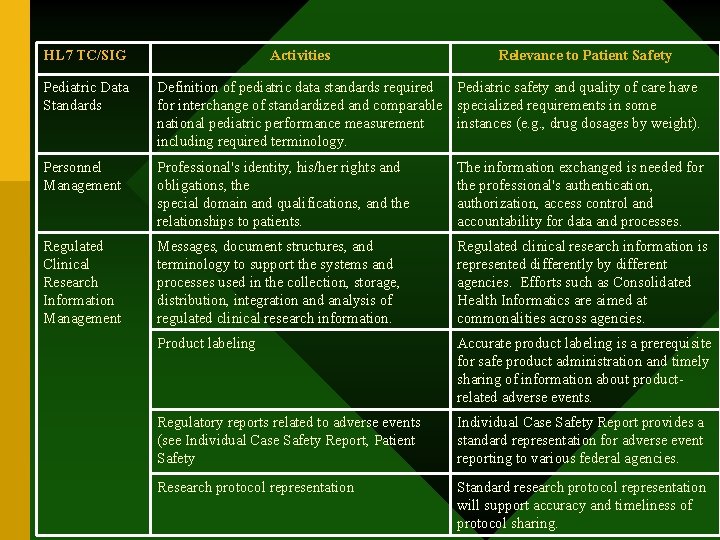
HL 7 TC/SIG Activities Relevance to Patient Safety Pediatric Data Standards Definition of pediatric data standards required Pediatric safety and quality of care have for interchange of standardized and comparable specialized requirements in some national pediatric performance measurement instances (e. g. , drug dosages by weight). including required terminology. Personnel Management Professional's identity, his/her rights and obligations, the special domain and qualifications, and the relationships to patients. The information exchanged is needed for the professional's authentication, authorization, access control and accountability for data and processes. Regulated Clinical Research Information Management Messages, document structures, and terminology to support the systems and processes used in the collection, storage, distribution, integration and analysis of regulated clinical research information. Regulated clinical research information is represented differently by different agencies. Efforts such as Consolidated Health Informatics are aimed at commonalities across agencies. Product labeling Accurate product labeling is a prerequisite for safe product administration and timely sharing of information about productrelated adverse events. Regulatory reports related to adverse events (see Individual Case Safety Report, Patient Safety Individual Case Safety Report provides a standard representation for adverse event reporting to various federal agencies. Research protocol representation Standard research protocol representation will support accuracy and timeliness of protocol sharing.
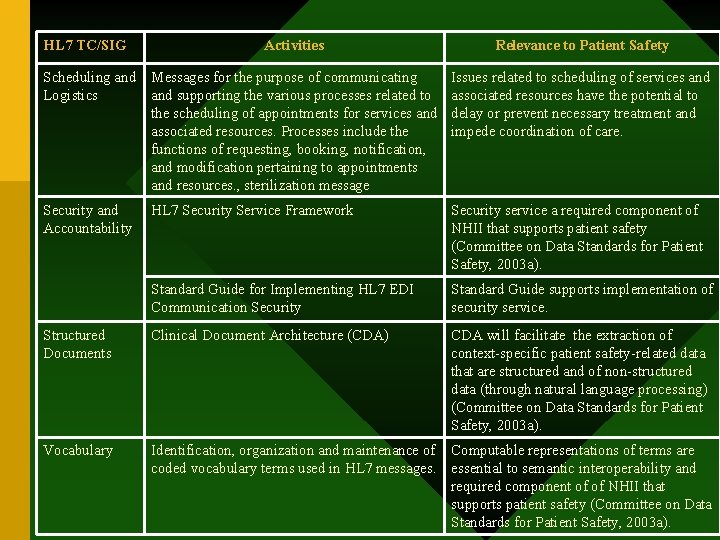
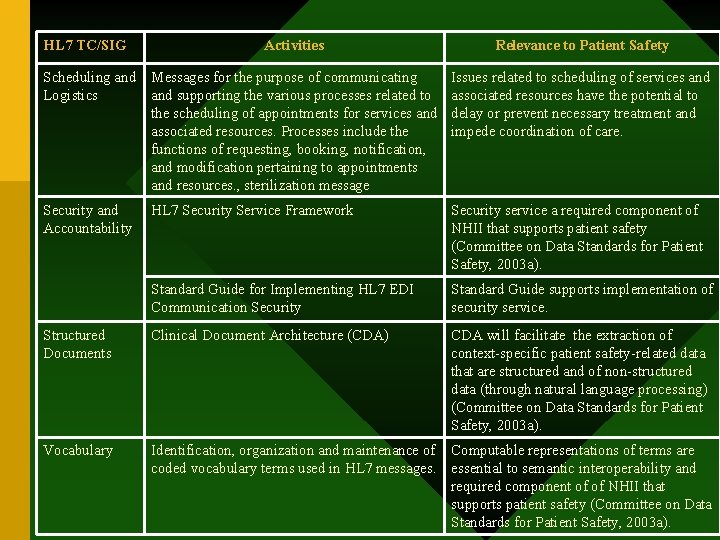
HL 7 TC/SIG Activities Relevance to Patient Safety Scheduling and Logistics Messages for the purpose of communicating and supporting the various processes related to the scheduling of appointments for services and associated resources. Processes include the functions of requesting, booking, notification, and modification pertaining to appointments and resources. , sterilization message Issues related to scheduling of services and associated resources have the potential to delay or prevent necessary treatment and impede coordination of care. Security and Accountability HL 7 Security Service Framework Security service a required component of NHII that supports patient safety (Committee on Data Standards for Patient Safety, 2003 a). Standard Guide for Implementing HL 7 EDI Communication Security Standard Guide supports implementation of security service. Structured Documents Clinical Document Architecture (CDA) CDA will facilitate the extraction of context-specific patient safety-related data that are structured and of non-structured data (through natural language processing) (Committee on Data Standards for Patient Safety, 2003 a). Vocabulary Identification, organization and maintenance of Computable representations of terms are coded vocabulary terms used in HL 7 messages. essential to semantic interoperability and required component of of NHII that supports patient safety (Committee on Data Standards for Patient Safety, 2003 a).
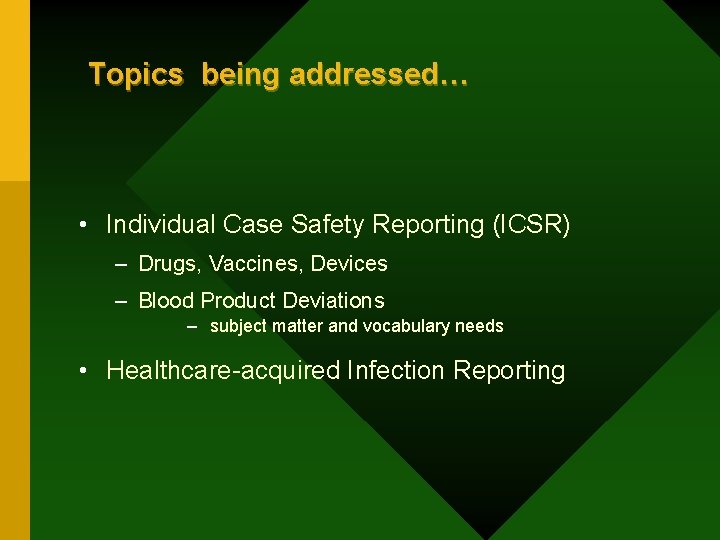
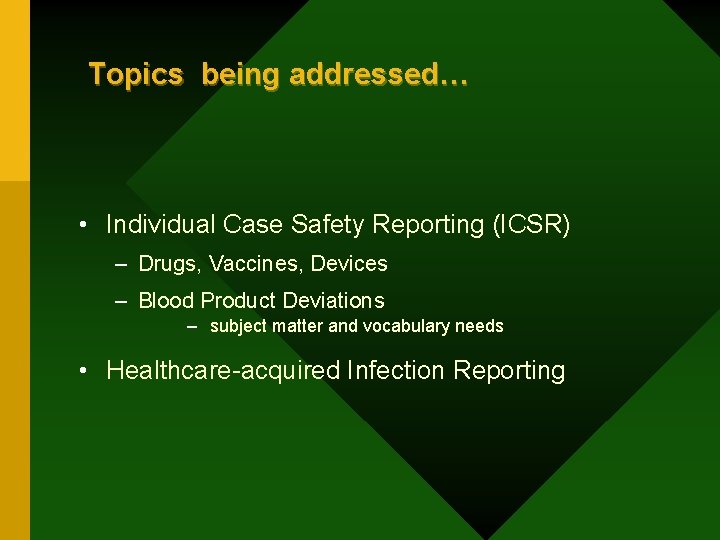
Topics being addressed… • Individual Case Safety Reporting (ICSR) – Drugs, Vaccines, Devices – Blood Product Deviations – subject matter and vocabulary needs • Healthcare-acquired Infection Reporting
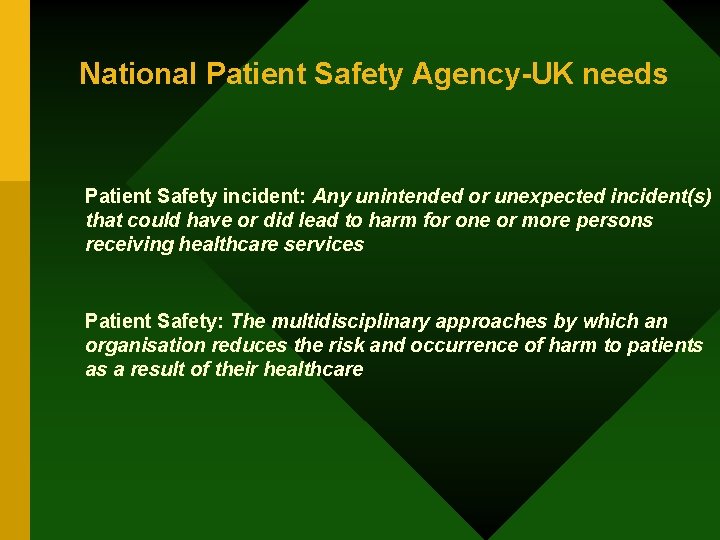
National Patient Safety Agency-UK needs Patient Safety incident: Any unintended or unexpected incident(s) that could have or did lead to harm for one or more persons receiving healthcare services Patient Safety: The multidisciplinary approaches by which an organisation reduces the risk and occurrence of harm to patients as a result of their healthcare
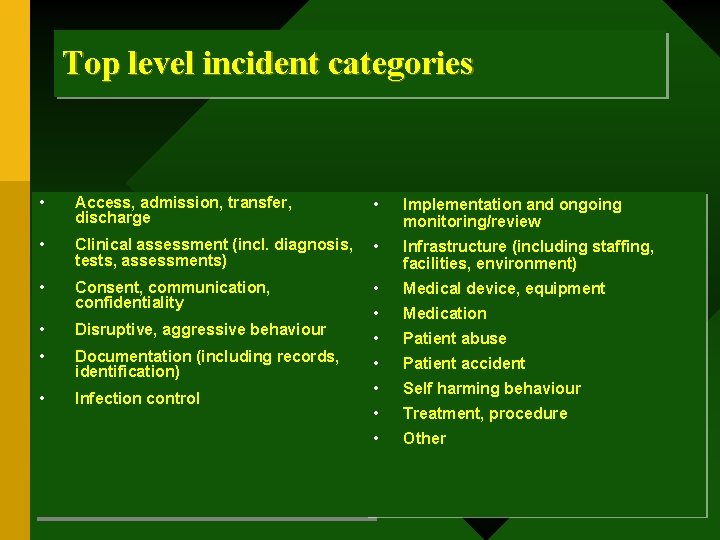
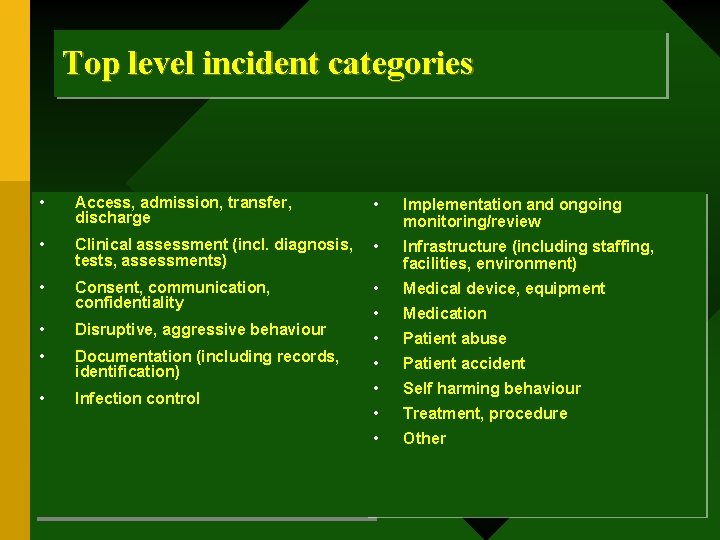
Top level incident categories • Access, admission, transfer, discharge • Implementation and ongoing monitoring/review • Clinical assessment (incl. diagnosis, tests, assessments) • Infrastructure (including staffing, facilities, environment) • Consent, communication, confidentiality • Medical device, equipment • Medication • Patient abuse • Patient accident • Self harming behaviour • Treatment, procedure • Other • Disruptive, aggressive behaviour • Documentation (including records, identification) • Infection control
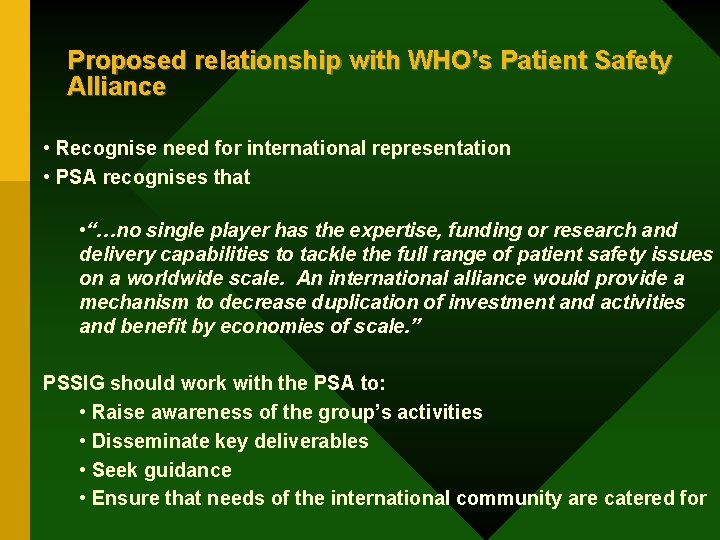
Proposed relationship with WHO’s Patient Safety Alliance • Recognise need for international representation • PSA recognises that • “…no single player has the expertise, funding or research and delivery capabilities to tackle the full range of patient safety issues on a worldwide scale. An international alliance would provide a mechanism to decrease duplication of investment and activities and benefit by economies of scale. ” PSSIG should work with the PSA to: • Raise awareness of the group’s activities • Disseminate key deliverables • Seek guidance • Ensure that needs of the international community are catered for

Australian Participation • Working with HL 7 Australia • Multiple needs in different settings • Different groups have long-term experience, and have developed methodologies and tools Japanese Participation…
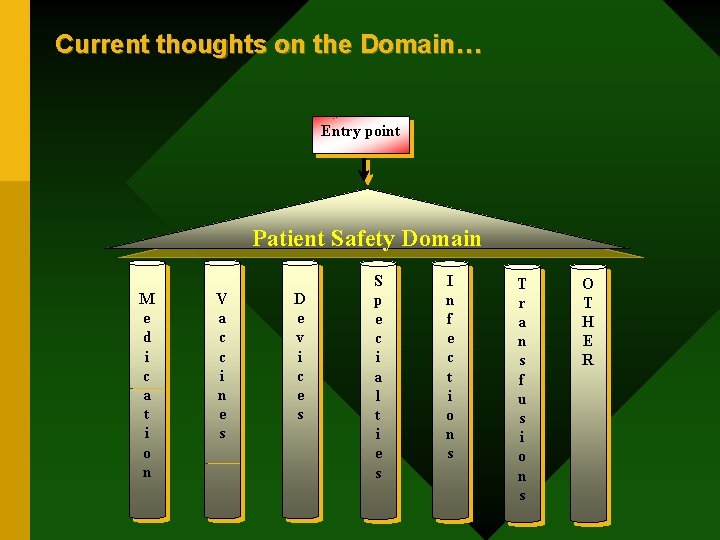
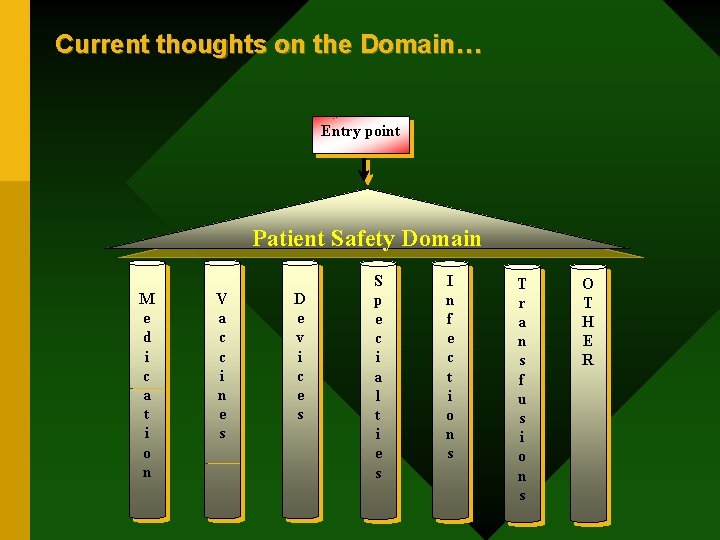
Current thoughts on the Domain… Entry point Patient Safety Domain M e d i c a t i o n V a c c i n e s D e v i c e s S p e c i a l t i e s I n f e c t i o n s T r a n s f u s i o n s O T H E R
Vision, Mission, Principles, Charter, Decision Making Process, Prioritization, Interaction with other TCs and SIGs, etc.
Interactions with other TCs and SIGs Patient Care TC to define settings and processes in medical care that and the related clinical/other information needs effect patient safety Electronic Health Record TC to identify and develop patient safety related functionalities within electronic medical record environment Pharmacy SIG to ensure proper medication usage (drug-drug interaction, contraindications, drug concentration and dosing, dispensing, AE reporting etc. ) Structured Document TC to accommodate the patient safety related information needs within structured technical documents Clinical Decision Support TC to address patient safety needs at the point-of-care from a evidence-based healthcare practice perspective, and Vocabulary TC to improve patient safety related vocabularies (coding for HL 7 internal codes, diseases, drugs, vaccines, medical devices/procedures, blood products, clinical terminology, regulatory terminology, etc. ) and promote the usage of appropriate controlled vocabularies. PHER… CBHS…
What is needed • Finding ‘Natural Home’ for different topics • Coordination of efforts where overlaps are identified – Friday Q 1 meeting with PC • Harmonization of domains and work products • Ensuring that the HL 7 standard as a whole reflects the patient safety perspectives