Pulmonary atelectasis in anaesthesia and critical care Damian




- Slides: 28
+ Pulmonary atelectasis in anaesthesia and critical care Damian Laba
+ Types: n Obstructive – tumor, mucus plug, FB n Non-obstructive -Compressive – tumor, bullae, air trapping -Passive/relaxation –parietal and visceral pleaura -Adhesive -surfactant -Cicatrizing – scar Risks: Obesity, lung disease, smoking, pregnancy
+ Atelectasis related to GA n Common n Critically ill n Mechanisms -Compression: FRC, relaxant, GA, surgical manipulation +obesity, laparoscopy, OLV -Absorption occlusion or high Fi 02 -Inflammatory response – ALI, neutrophil activation, fluid, mediators -Surfactant depletion- smoke inhalation, Laplace’s law
+ Pathophysiological effects of atelectasis n Decreased compliance - Less effective pressure –volume curve , increase WOB n Impaired oxygenation -V/Q mismatch n Increased pulmonary vascular resistance -hypoxic pulmonary vasoconstriction
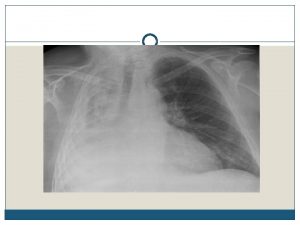
+ Clinical presentation n Asymtomatic n Non-productive cough n Hypoxia/Respiratory failure n PE: chest expansion, dullness, no breath sounds, trachea Investigations: CXR – direct and indirect signs CT US
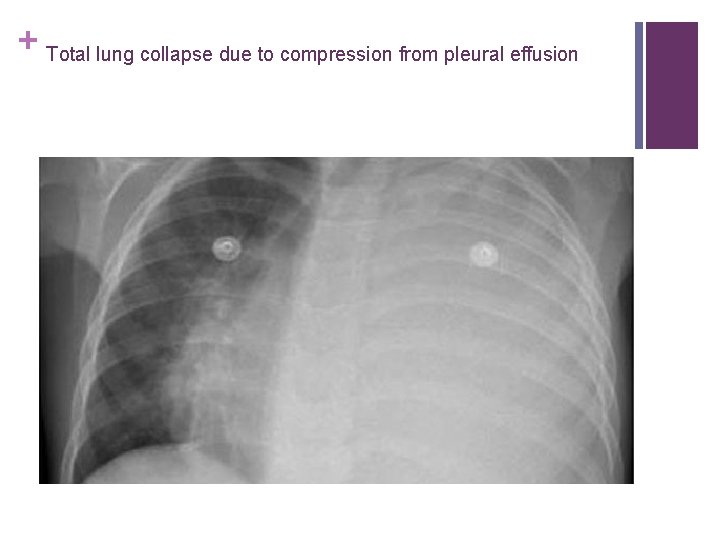
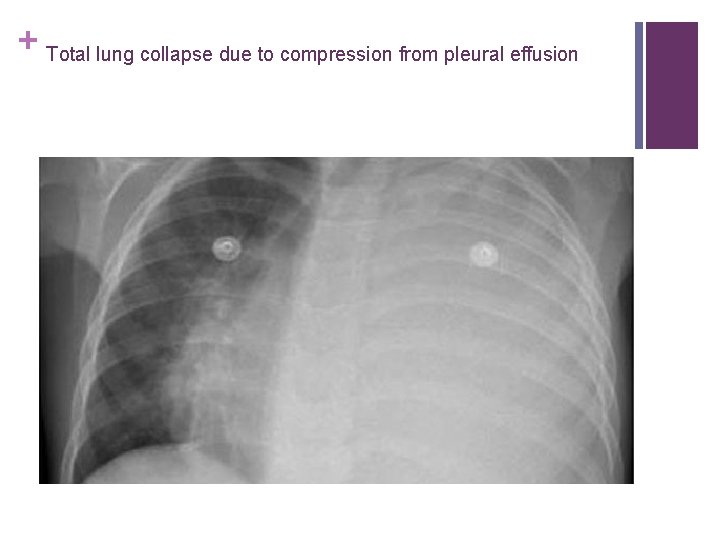
+ Total lung collapse due to compression from pleural effusion
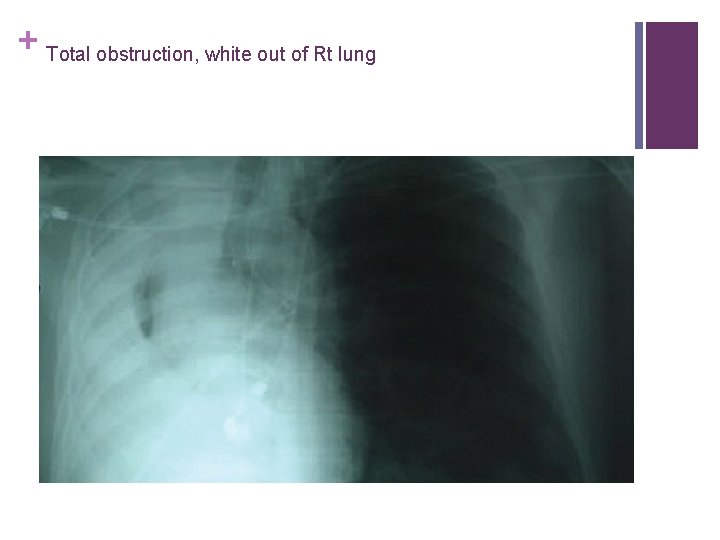
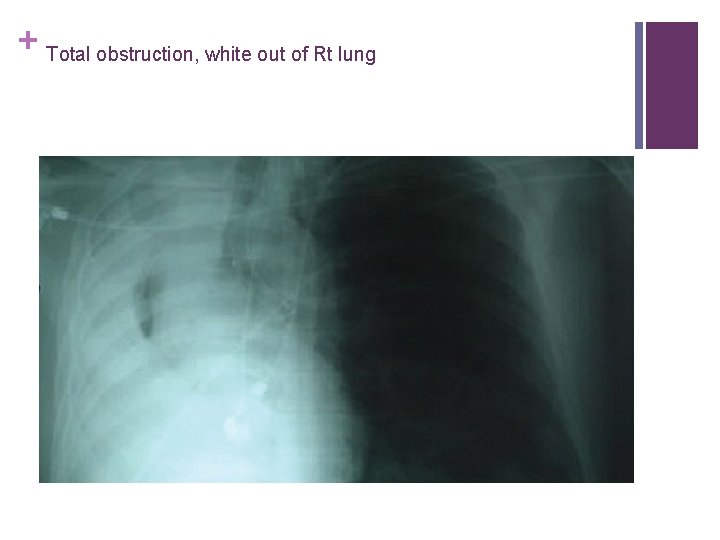
+ Total obstruction, white out of Rt lung
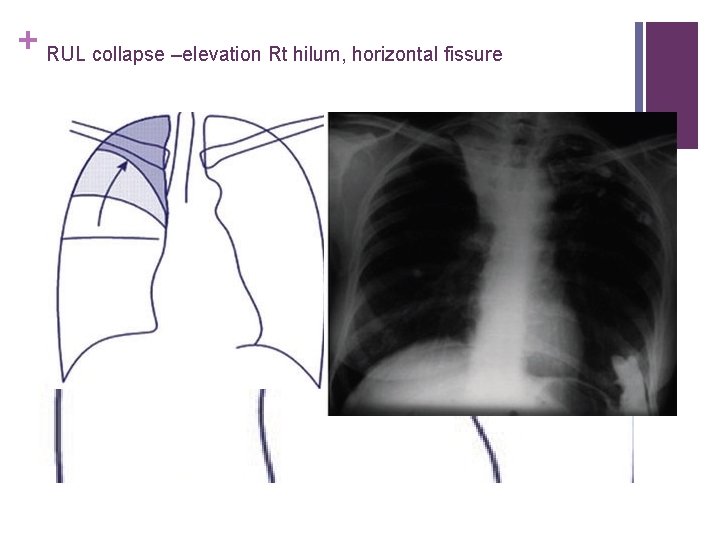
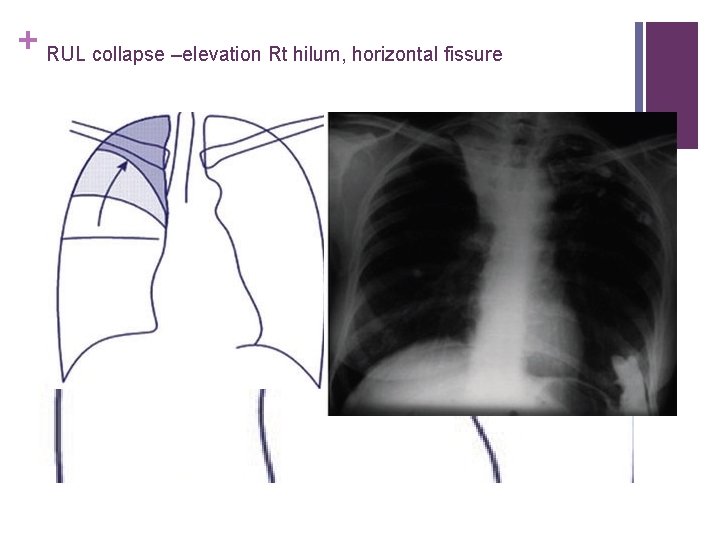
+ RUL collapse –elevation Rt hilum, horizontal fissure

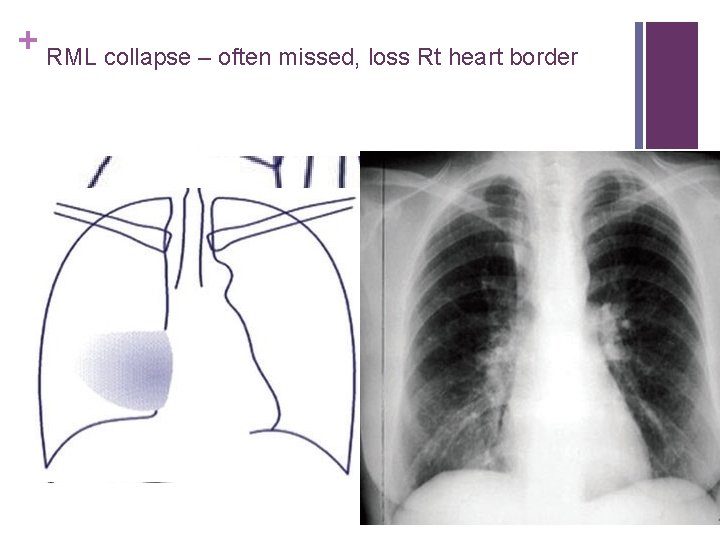
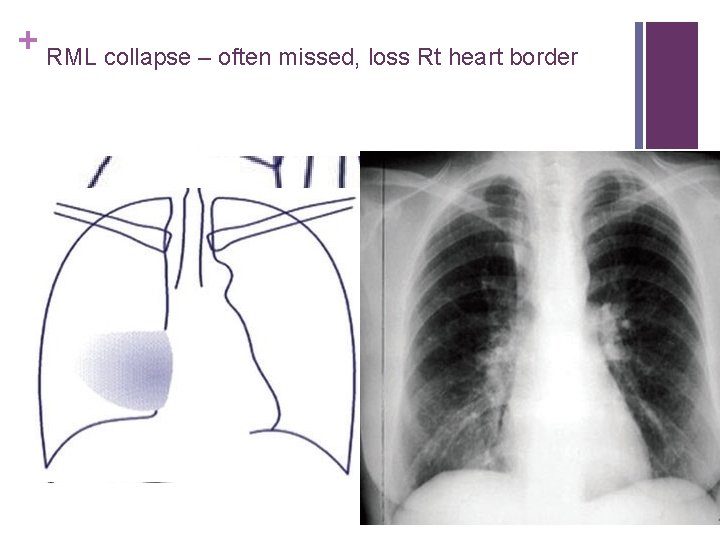
+ RML collapse – often missed, loss Rt heart border

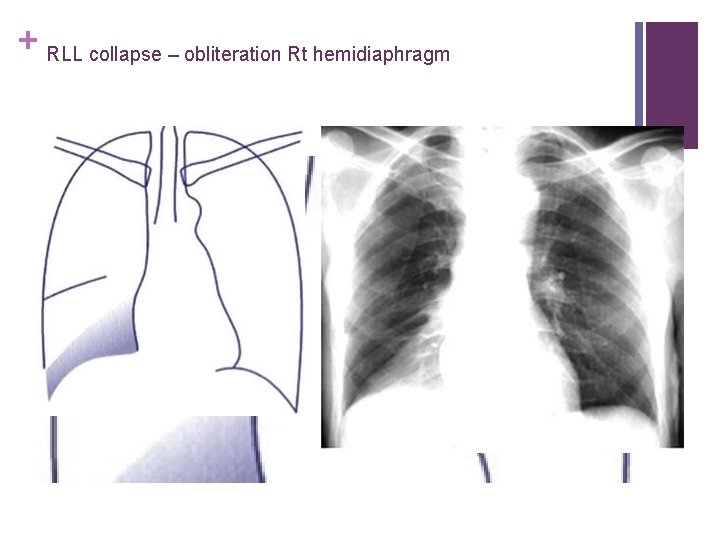
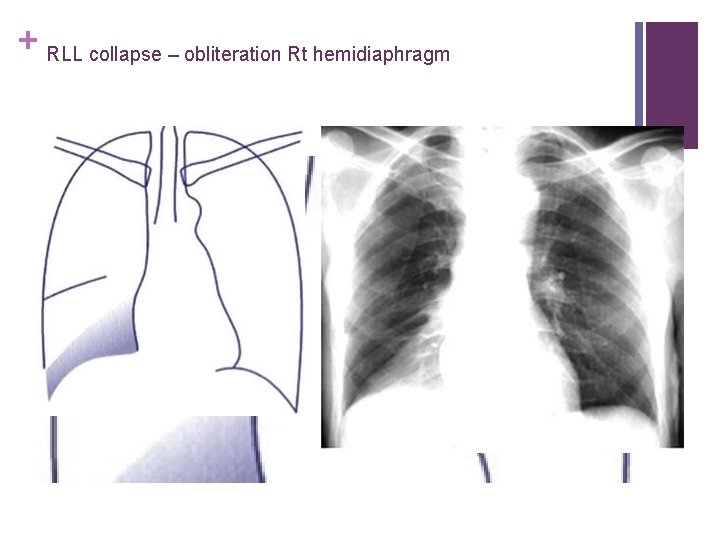
+ RLL collapse – obliteration Rt hemidiaphragm

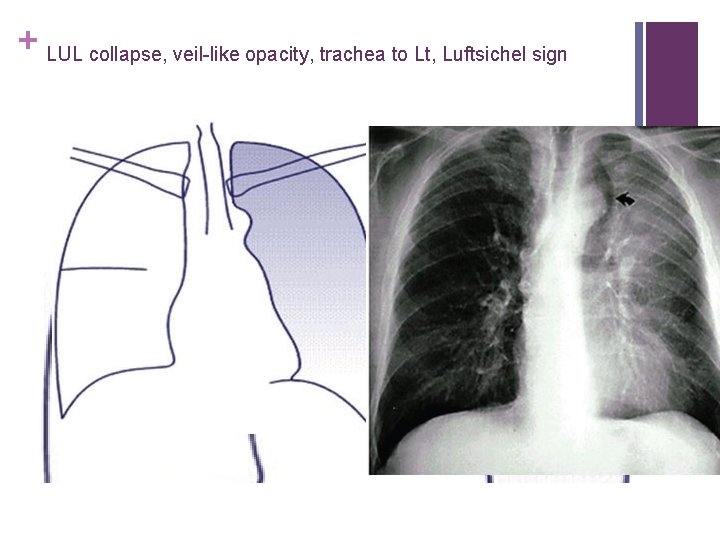
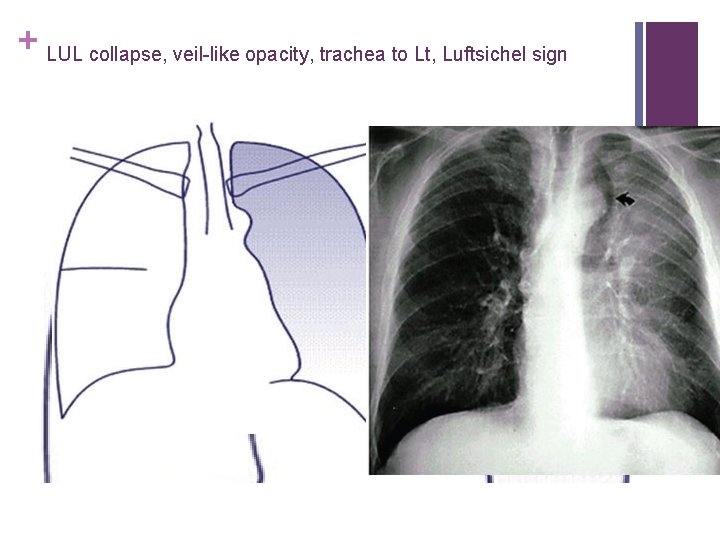
+ LUL collapse, veil-like opacity, trachea to Lt, Luftsichel sign
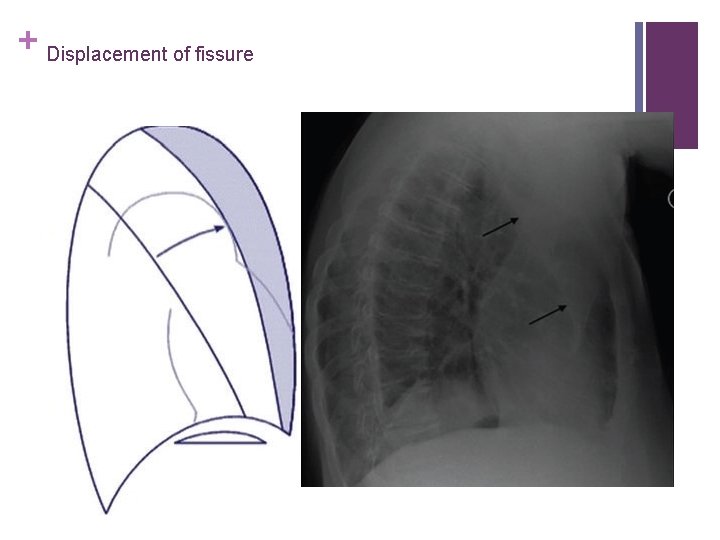
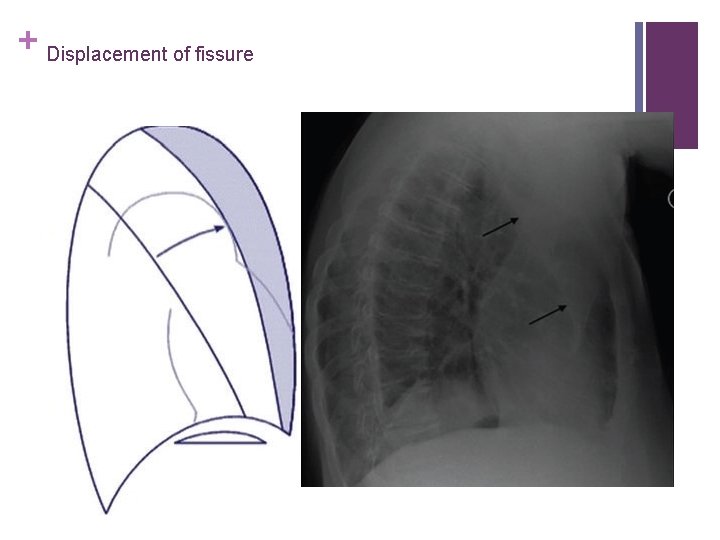
+ Displacement of fissure
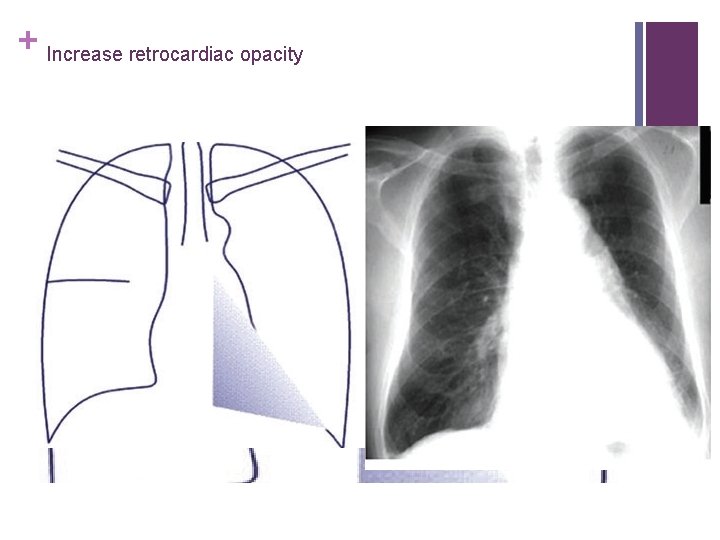
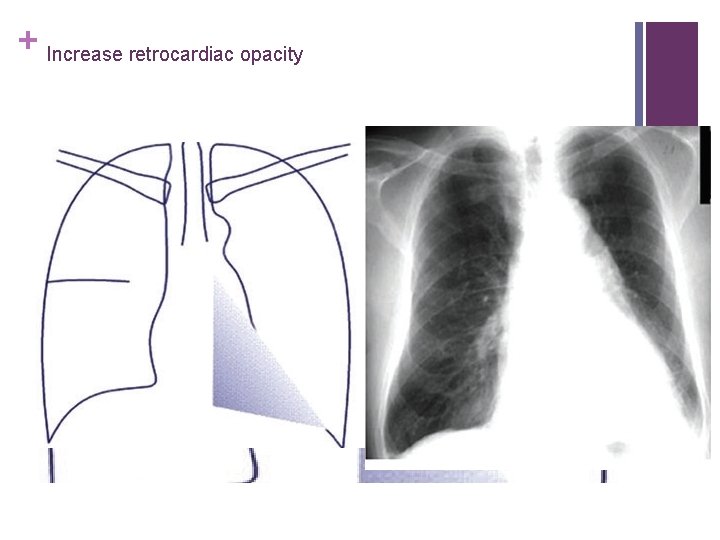
+ Increase retrocardiac opacity
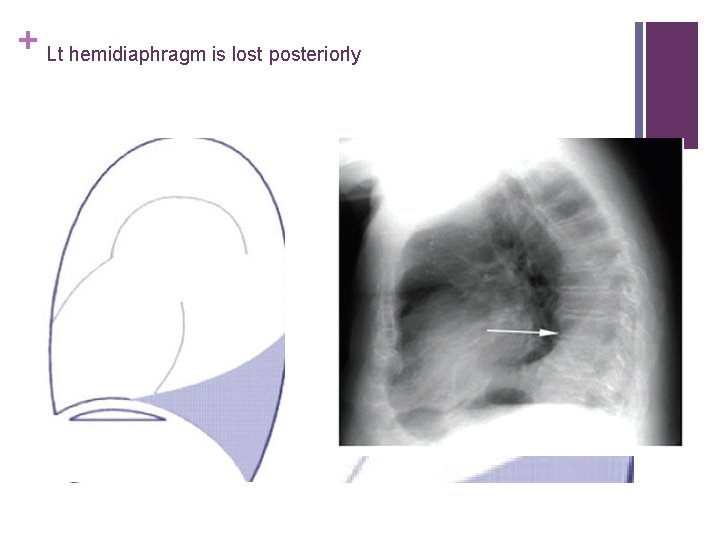
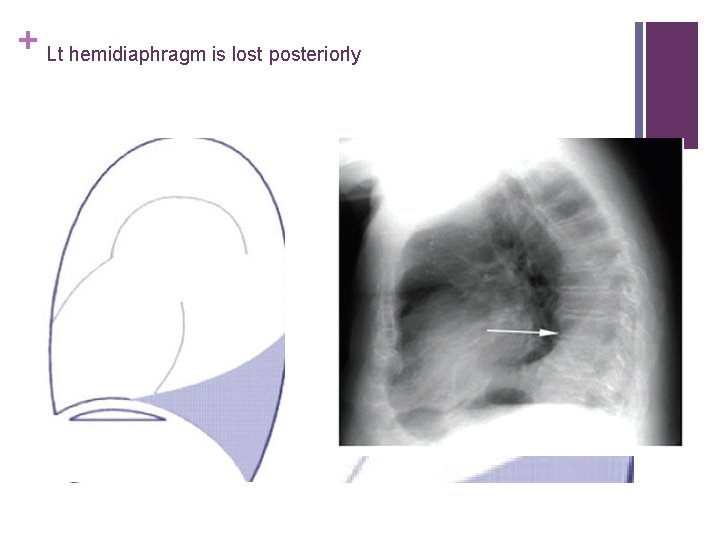
+ Lt hemidiaphragm is lost posteriorly

+ Hounsfield units -100 - +100
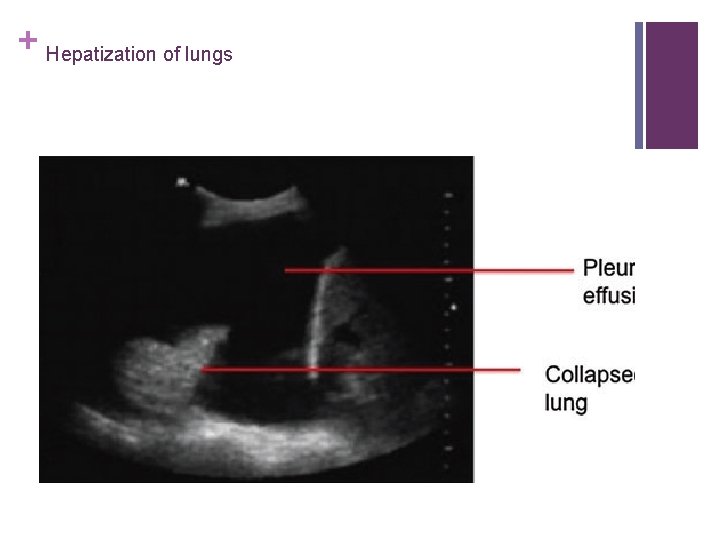
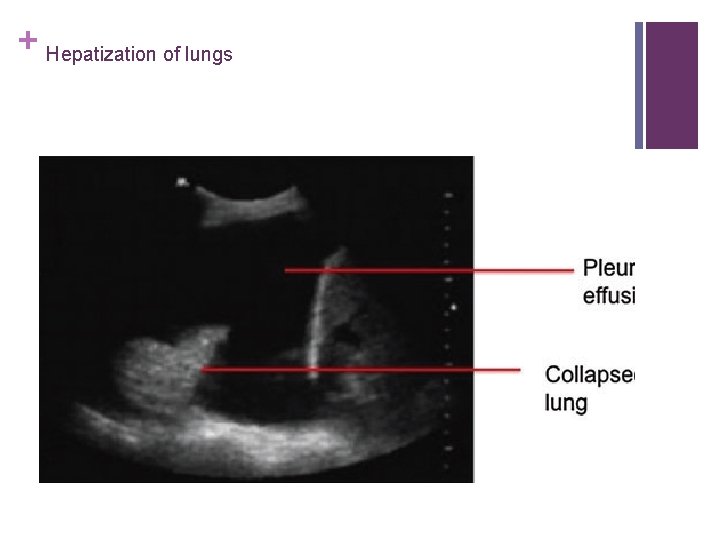
+ Hepatization of lungs
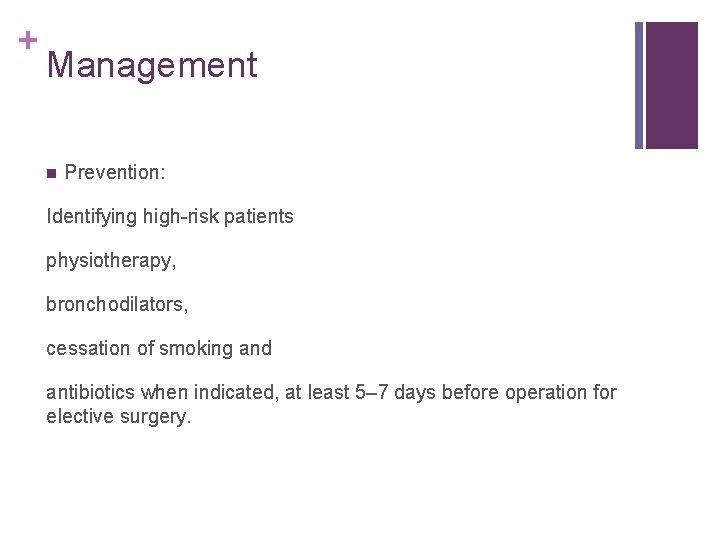
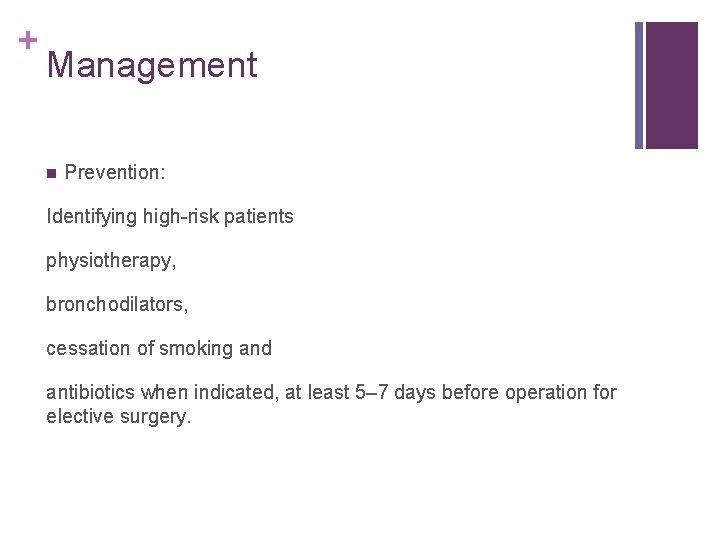
+ Management n Prevention: Identifying high-risk patients physiotherapy, bronchodilators, cessation of smoking and antibiotics when indicated, at least 5– 7 days before operation for elective surgery.
+ n Baseline X-rays, blood gases, and lung function tests for patients with moderate to severe respiratory and cardiovascular disease for more major procedures. n Lung function test are not recommended as part of routine preoperative for ASA I with no comorbidities undergoing surgery of any severity.
+ On Inductions n Fi. O 2 0. 8 n Recruitments n CPAP
+ Maintaince n PEEP n Recruitments: 1) Vital capacity manoeuvre using an inflation pressure of 40 cm. H 2 O sustained for 10– 15 s. 2) Increasing PEEP to 15 cm H 2 O and then increasing tidal volumes to achieve peak inspiratory pressure of 40 cm H 2 O for 10 breaths before then returning to standard ventilator settings.
+ Post op n Pain control n CPAP n Deep breath exercise n physiotherapy
+ ITU settings n Ventilation strategies: - CPAP - PEEP - Vt 6 -8 ml/kg - P plateau < 35 cm. H 2 O - Recruitments - Fi. O 2 - ? HFOV
+ Other strategies which may be used in the management of artificial ventilation in patients with atelectasis. Prone position Promotes ventilation–perfusion matching, increase FRC, decrease shunt Kinetic bed (40 degrees rotation on each side with pause of 10 min on each side and 5 min in the supine position) Prevents collection of secretions, ventilator-associated pneumonia, redistribution of pressure to allow lung expansion Chest physiotherapy Aids airway clearance and improves ventilation Bronchoscopy Aids airway clearance in patients with poor cough, e. g. neuromuscular disease Mucolytics or Dnase Clears tenacious secretions, good results in paediatrics Surfactant Surface tension to allow alveoli stability and prevent collapse Fluorocarbons Facilitates lung recruitment by separating adherent lung surfaces by virtue of their low equilibrium surface tension and positive spreading coefficient
+ Conclusions: n Atelectasis common cause of hypoxia or respiratory failure in anaesthesia and ITU settings n Prevention better than cure n Timely diagnosis and management is crucial for good outcome
+ Thank you n Contin Educ Anaesth Crit Care Pain (2014) 14 (5): 236 -245. First published online: December 23, 2013
 Critical semi critical and non critical instruments
Critical semi critical and non critical instruments Principle of sterilization
Principle of sterilization Derive adjective
Derive adjective Invaginasi usg
Invaginasi usg Absorption atelectasis
Absorption atelectasis Glottic opening
Glottic opening Hafoe mask
Hafoe mask Atelectasis tactile fremitus
Atelectasis tactile fremitus Absorptive atelectasis
Absorptive atelectasis Bulbous enlargement of the distal segments of the fingers
Bulbous enlargement of the distal segments of the fingers Mosby items and derived items
Mosby items and derived items Absorptive atelectasis
Absorptive atelectasis Bronchitis alergi icd 10
Bronchitis alergi icd 10 Lll atelectasis
Lll atelectasis Denitrogenation atelectasis
Denitrogenation atelectasis Nursing care plan for pulmonary embolism
Nursing care plan for pulmonary embolism Nursing management of pulmonary tuberculosis
Nursing management of pulmonary tuberculosis Primary secondary tertiary medical care
Primary secondary tertiary medical care Stop maid intubation
Stop maid intubation Anesthesia hose
Anesthesia hose Spinal anesthesia structures pierced
Spinal anesthesia structures pierced Spinal anesthesia ligaments
Spinal anesthesia ligaments Minimum alveolar concentration
Minimum alveolar concentration Balanced anesthesia components
Balanced anesthesia components Dr pradnya joshi
Dr pradnya joshi Dizepam
Dizepam What is regional anesthesia
What is regional anesthesia Appherensive
Appherensive Local anaesthesia
Local anaesthesia