Proximal humerus simple twopart fracture Case for small

- Slides: 22
Proximal humerus: simple twopart fracture Case for small group discussion: Upper extremity fractures—decision making and methods of stabilization AO Trauma Advanced Principles Course
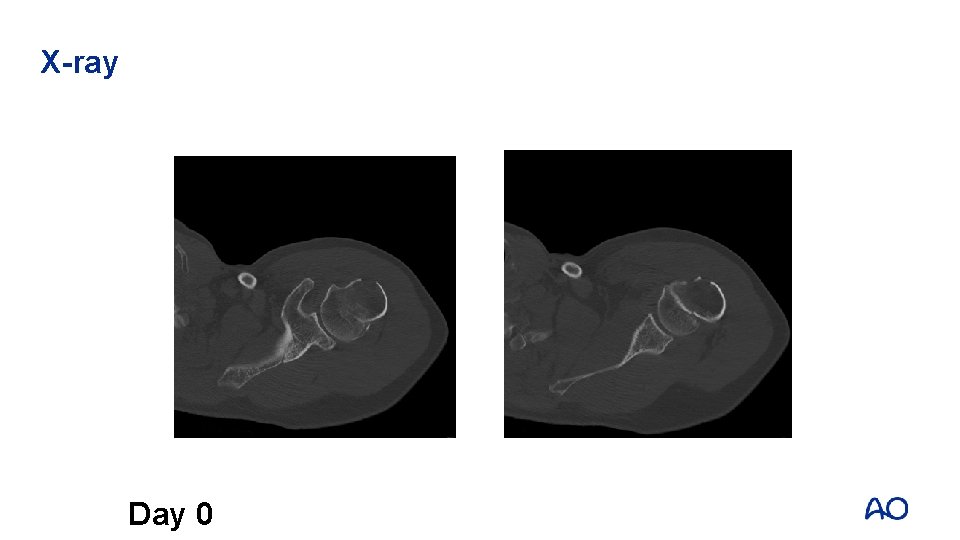
Case history • 52 -year-old male patient • Trauma mechanism: – The patient did fall from an about 2 -meter height (stairs) with a direct impact on the left shoulder – He cannot move the shoulder and is in severe pain – The skin is intact, we note bruising over the deltoid area and the left hemithorax – There are no neurovascular disturbances, especially not concerning the axillary – There is no clinical indication of other traumatic injuries Day 0
Case history • Medical history: – 06/2007: large cell bladder carcinoma with important post-renal failure – 01/2008: cystectomy with orthotopic bladder replacement – 10/2009: radial head fracture on right elbow – 10/2009: scaphoid fracture left wrist Day 0
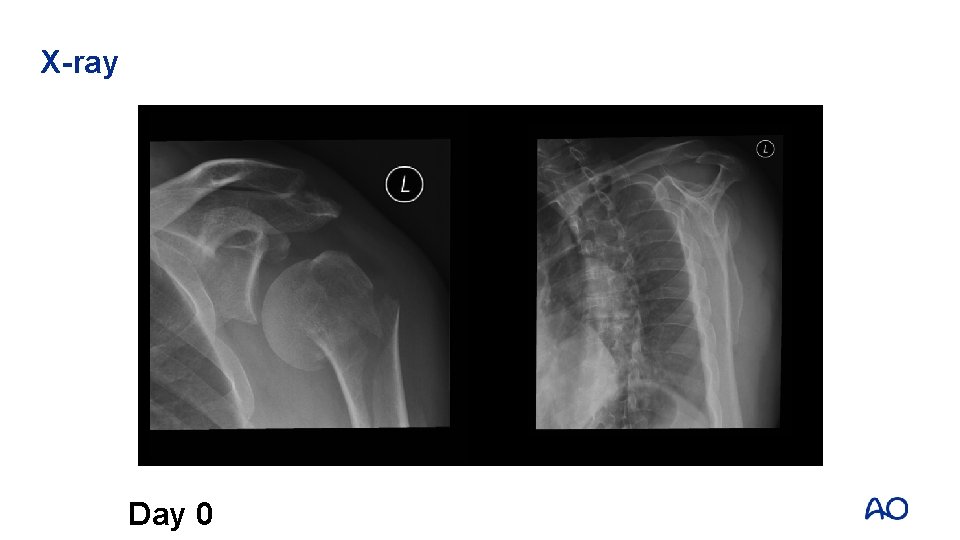
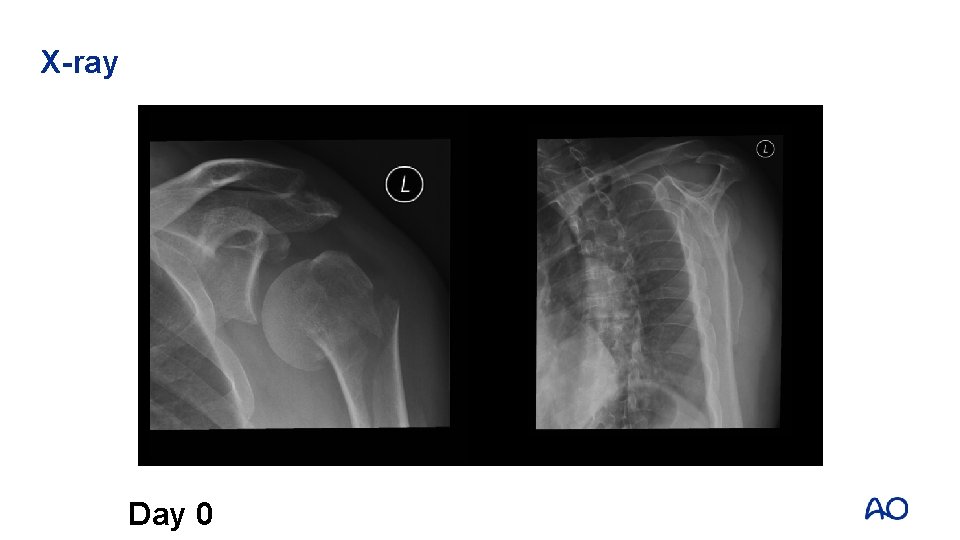
X-ray Day 0
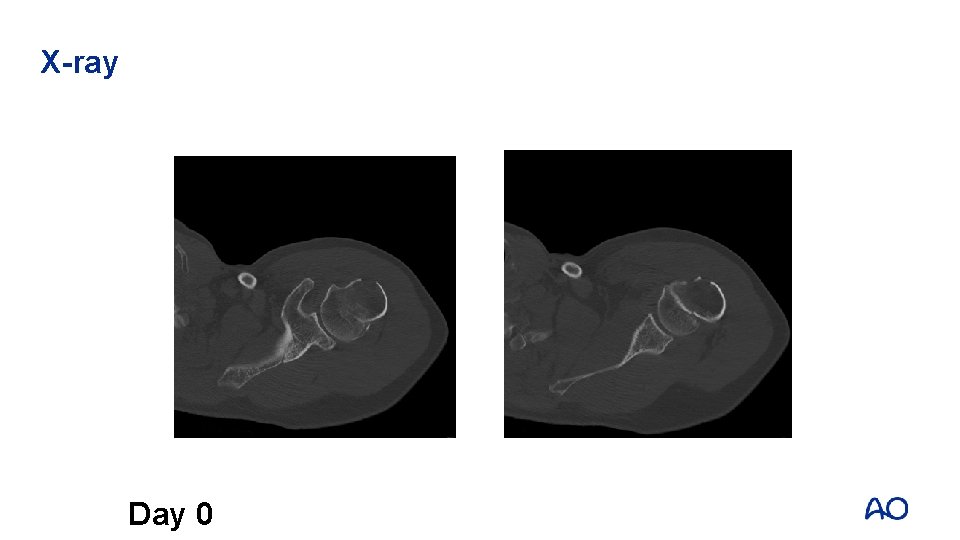
X-ray Day 0
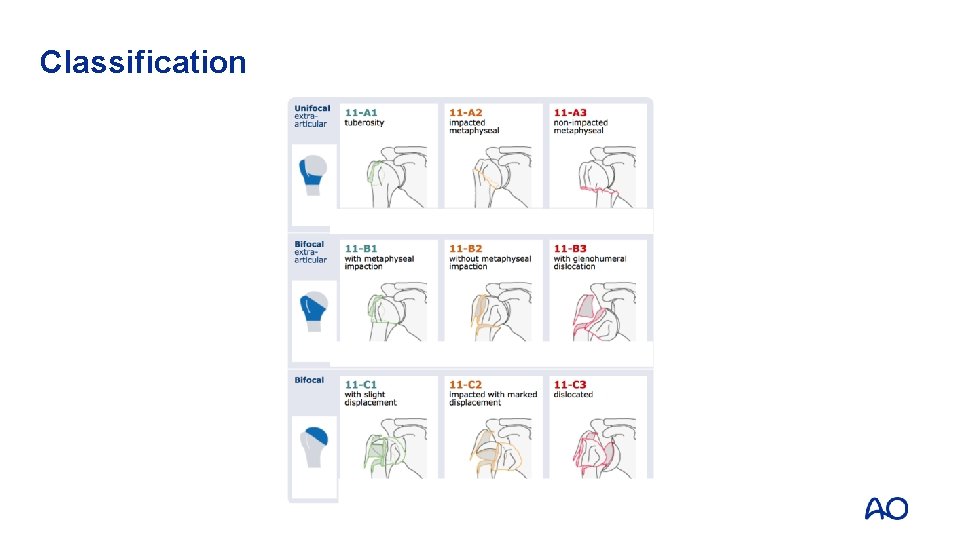
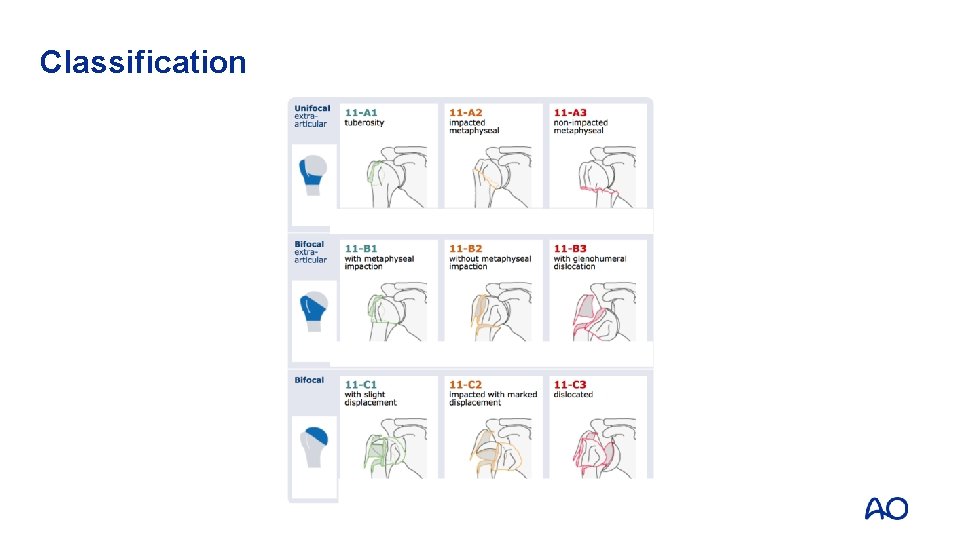
Classification
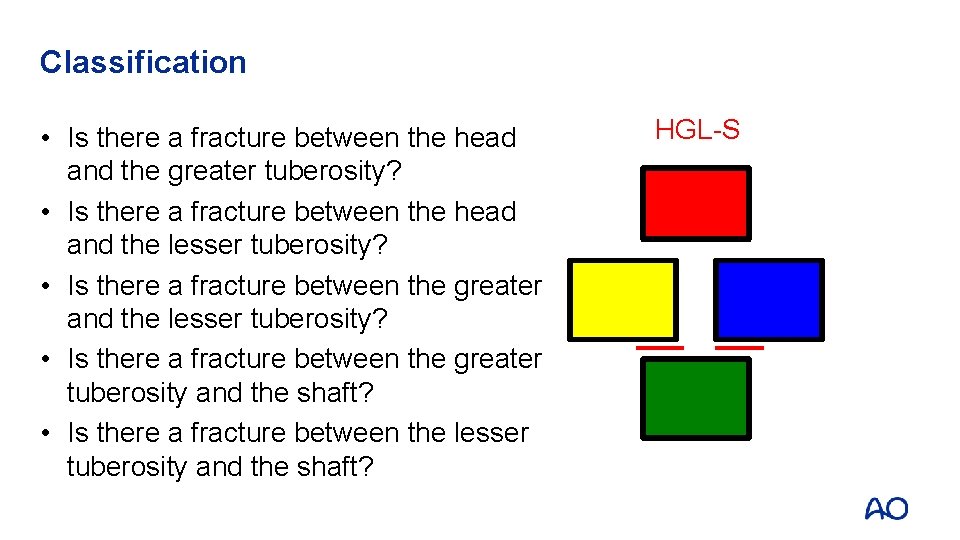
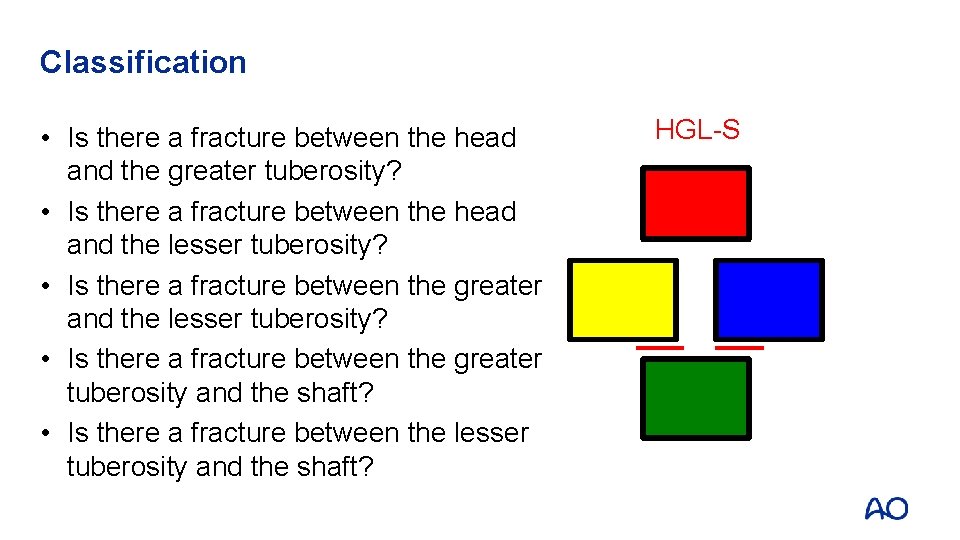
Classification • Is there a fracture between the head and the greater tuberosity? • Is there a fracture between the head and the lesser tuberosity? • Is there a fracture between the greater tuberosity and the shaft? • Is there a fracture between the lesser tuberosity and the shaft? HGL-S
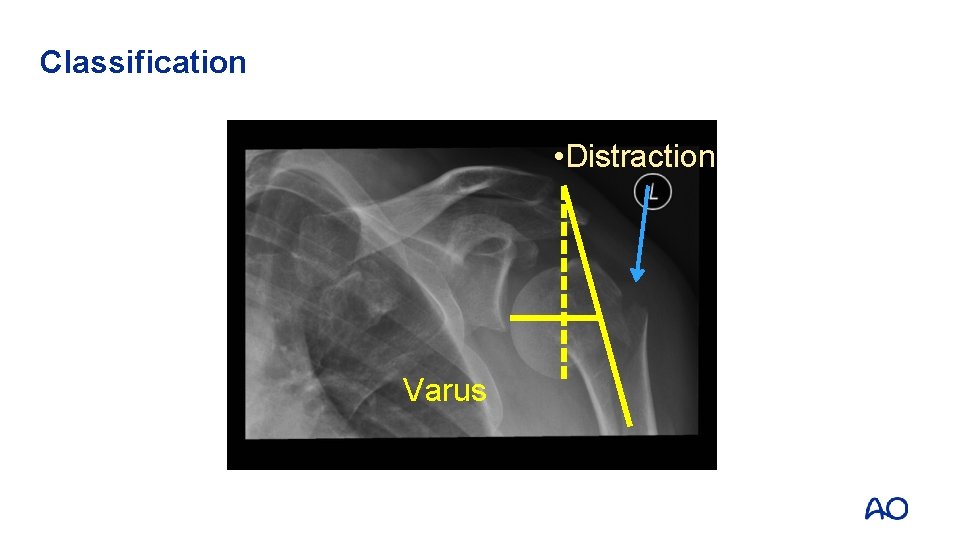
Classification • Distraction Varus
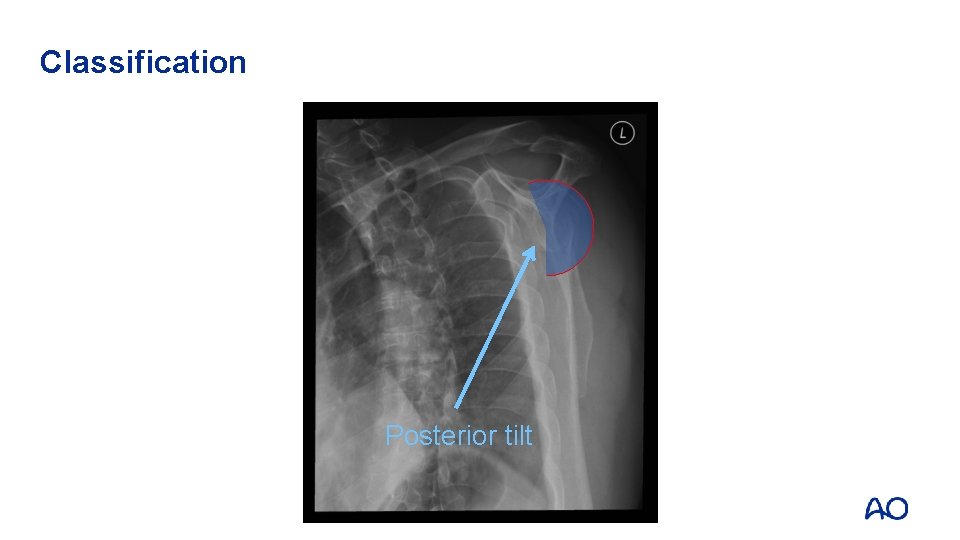
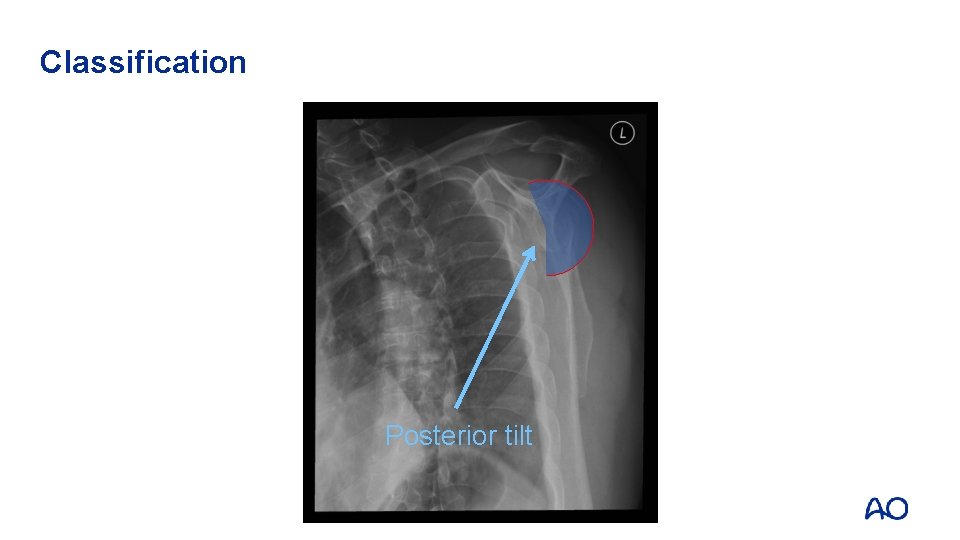
Classification Posterior tilt
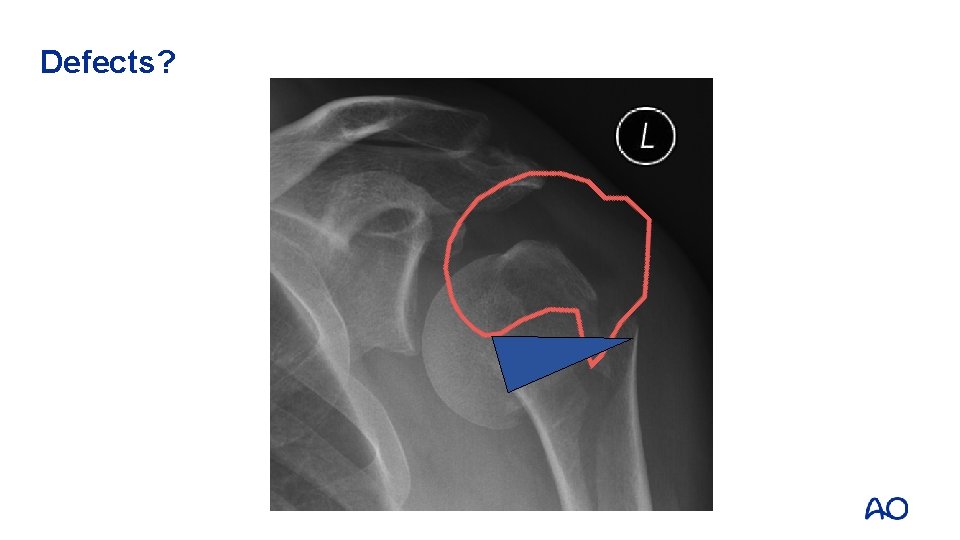
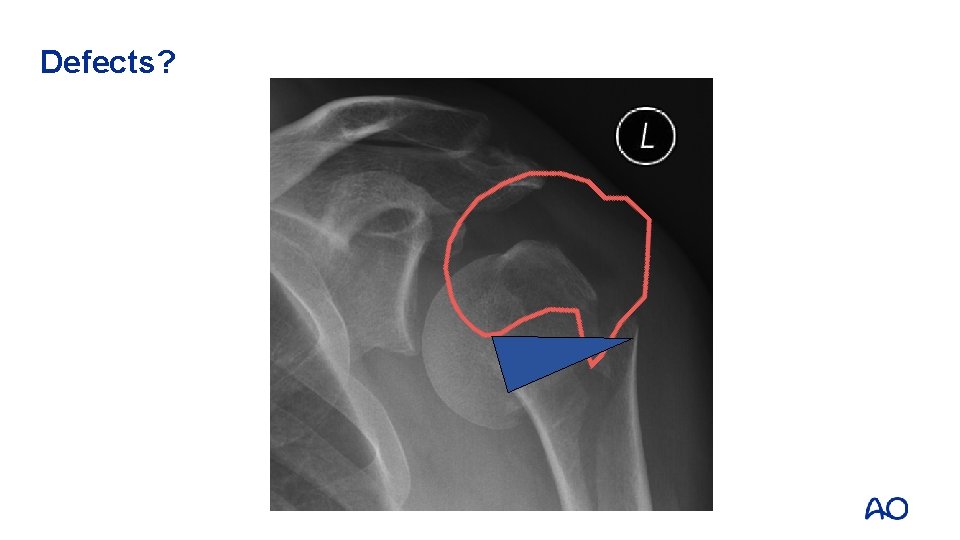
Defects?
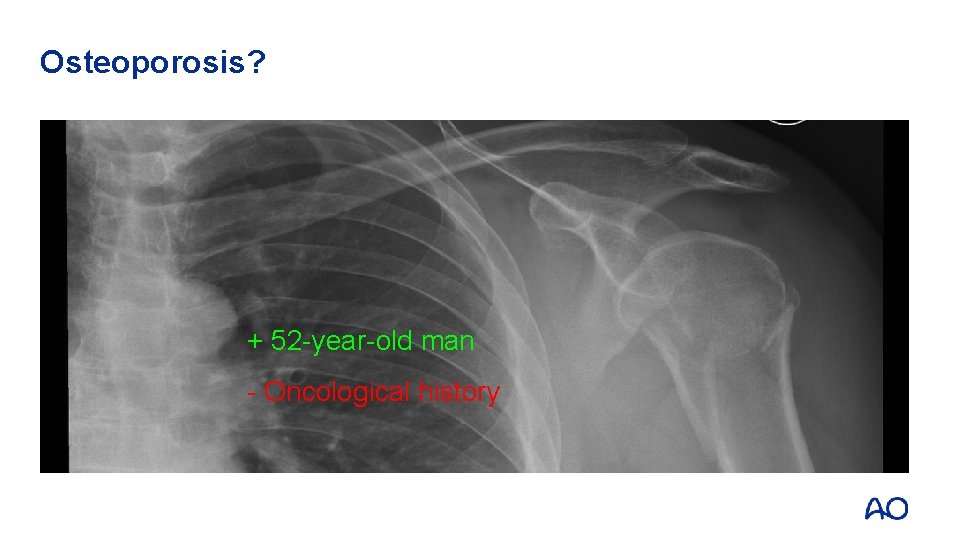
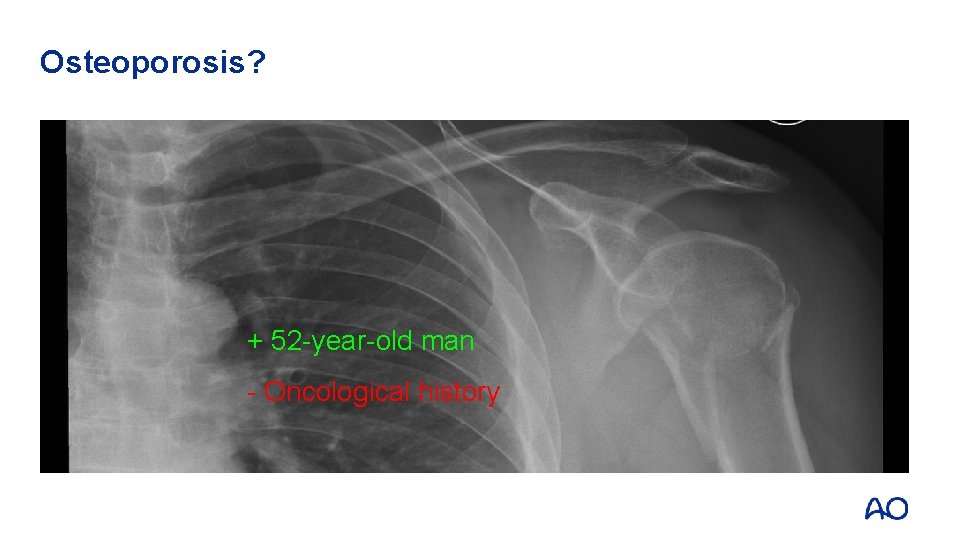
Osteoporosis? + 52 -year-old man - Oncological history
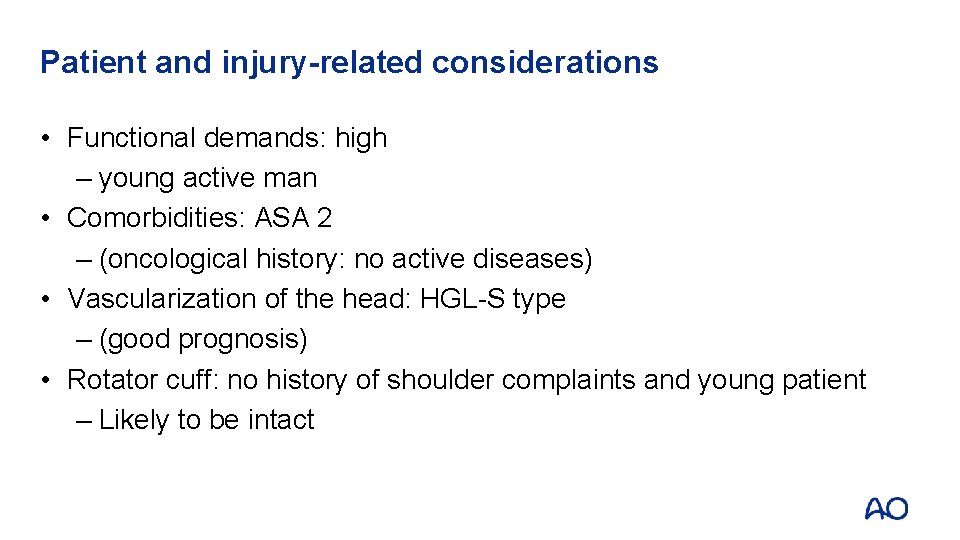
Patient and injury-related considerations • Functional demands: high – young active man • Comorbidities: ASA 2 – (oncological history: no active diseases) • Vascularization of the head: HGL-S type – (good prognosis) • Rotator cuff: no history of shoulder complaints and young patient – Likely to be intact
Treatment options • Nonoperative treatment • Fixation: – Closed nailing – Minimally invasive percutaneous plate osteosynthesis (MIPPO) – Open reduction internal fixation (ORIF)
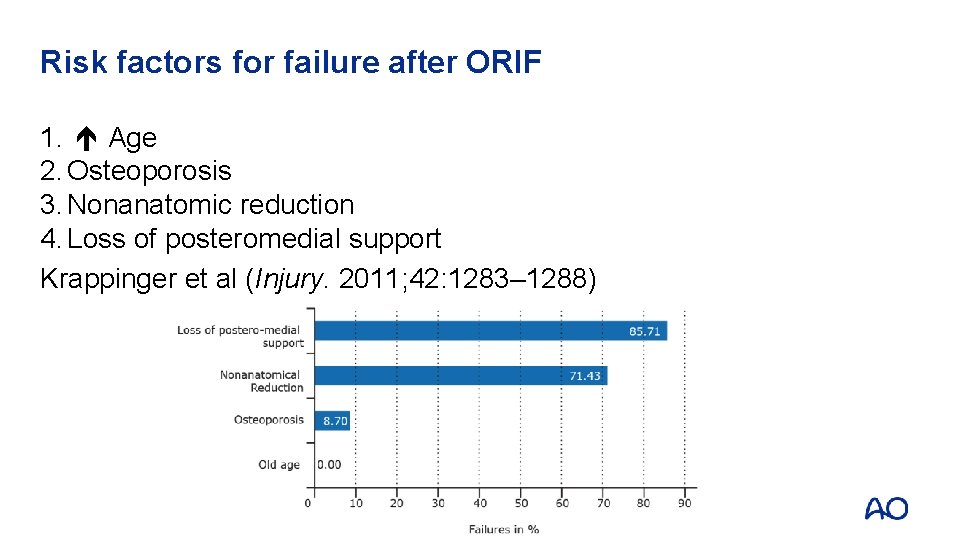
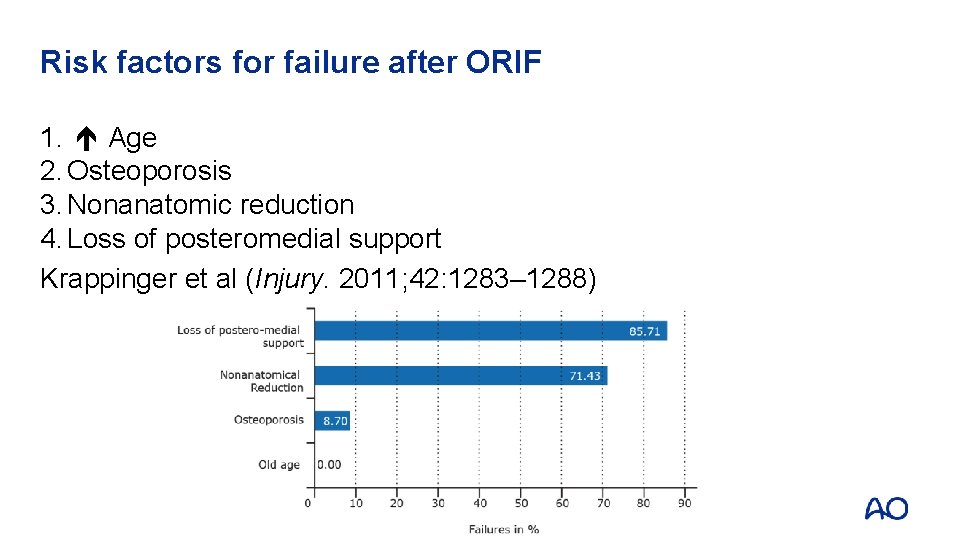
Risk factors for failure after ORIF 1. Age 2. Osteoporosis 3. Nonanatomic reduction 4. Loss of posteromedial support Krappinger et al (Injury. 2011; 42: 1283– 1288)
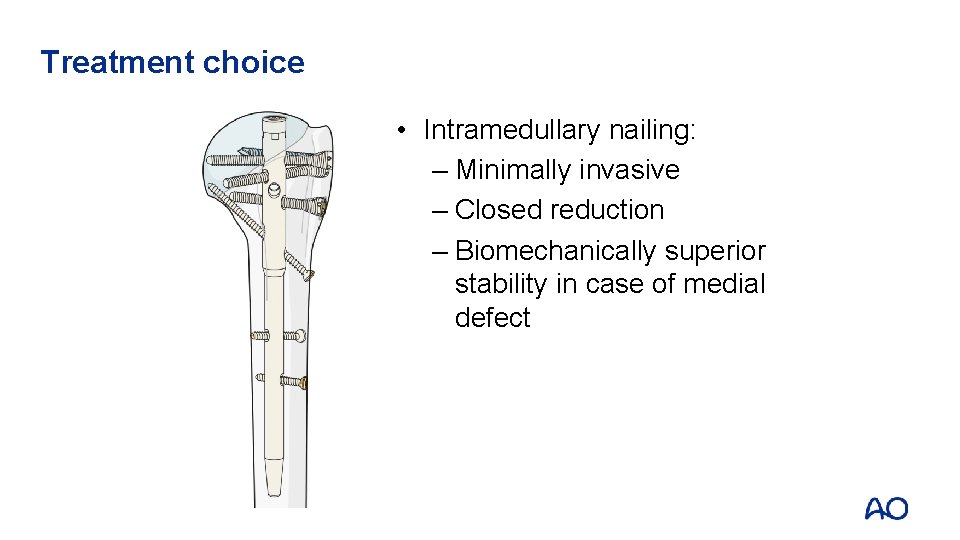
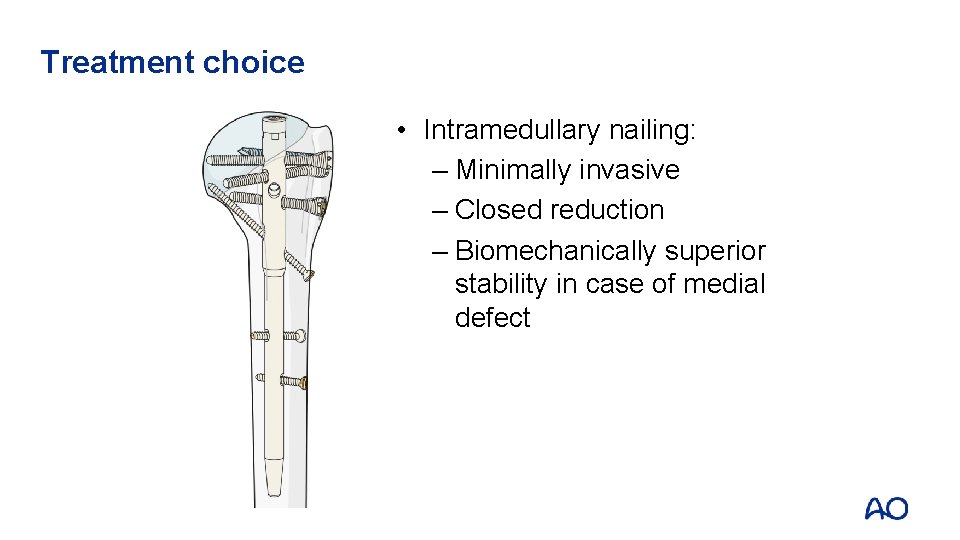
Treatment choice • Intramedullary nailing: – Minimally invasive – Closed reduction – Biomechanically superior stability in case of medial defect
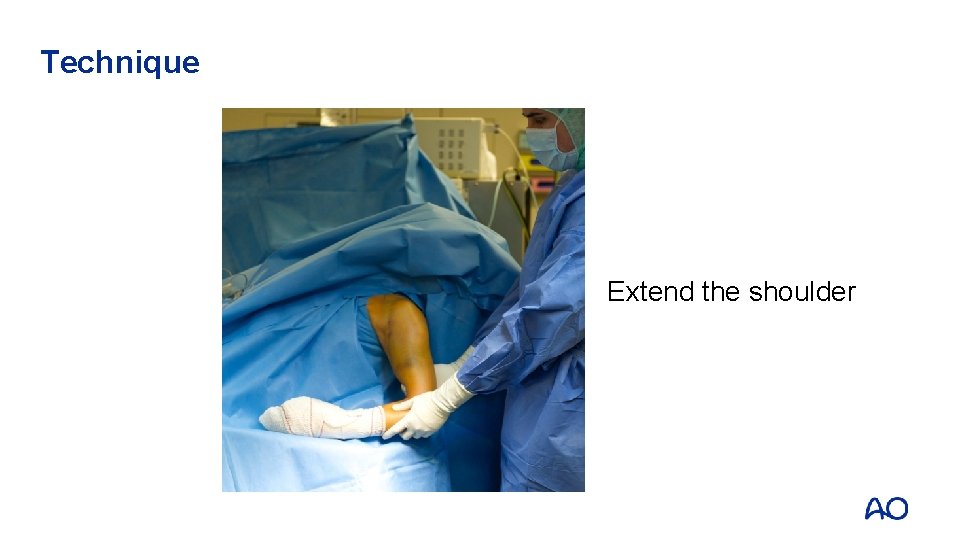
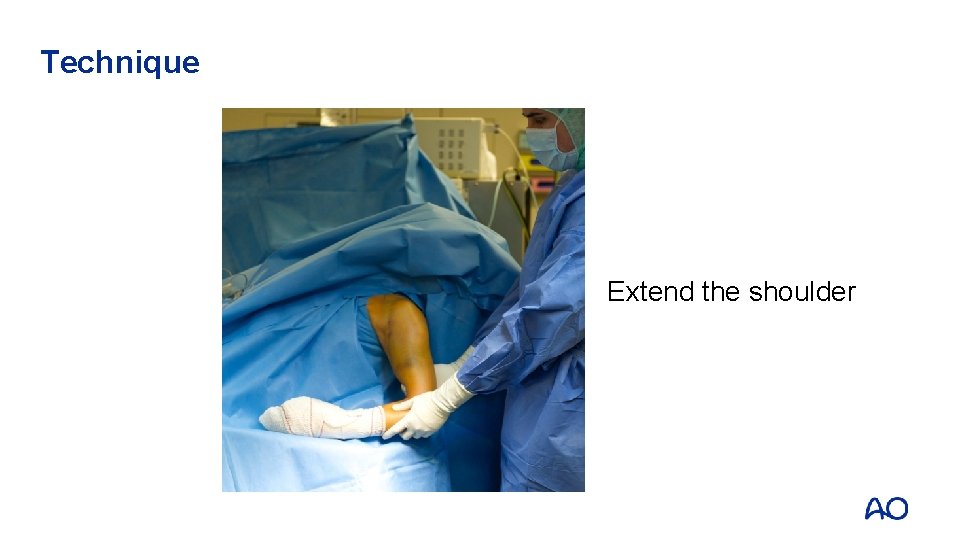
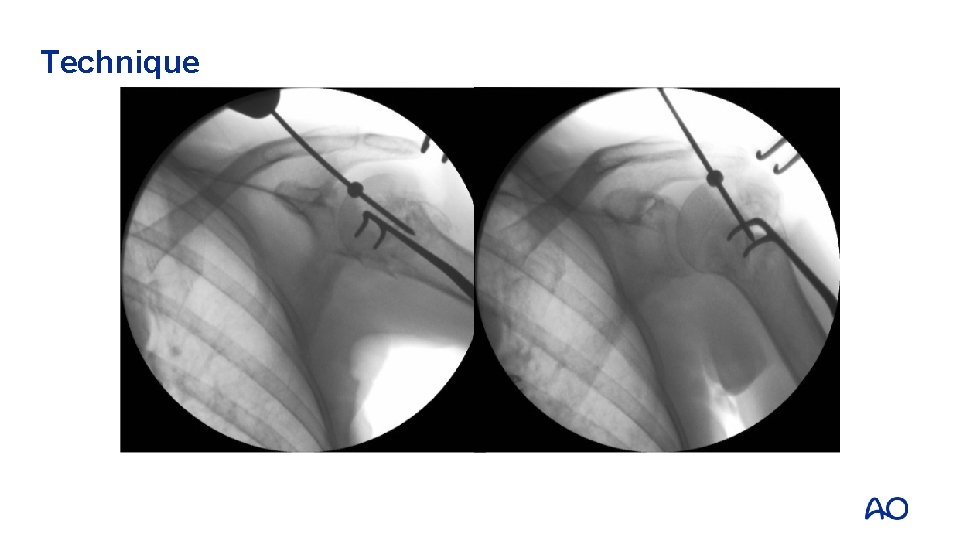
Technique Extend the shoulder
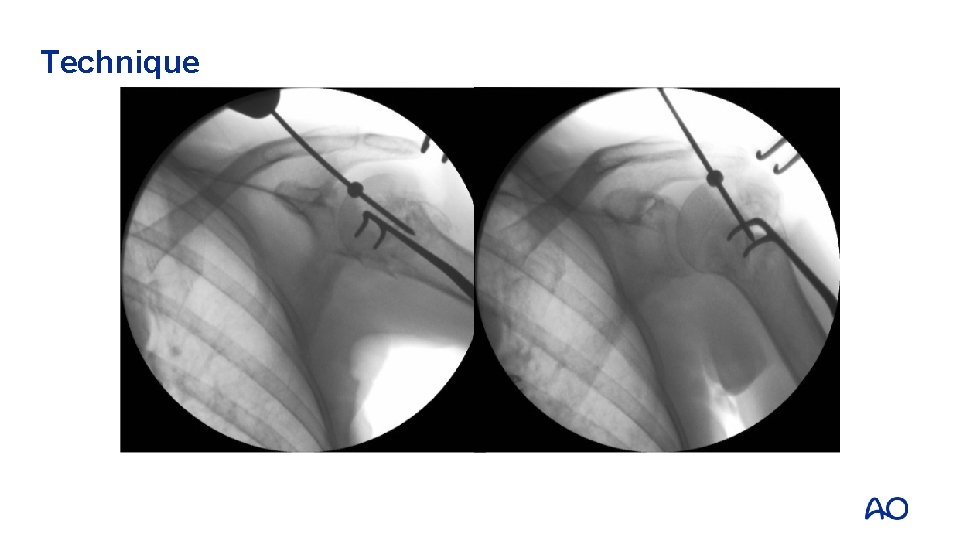
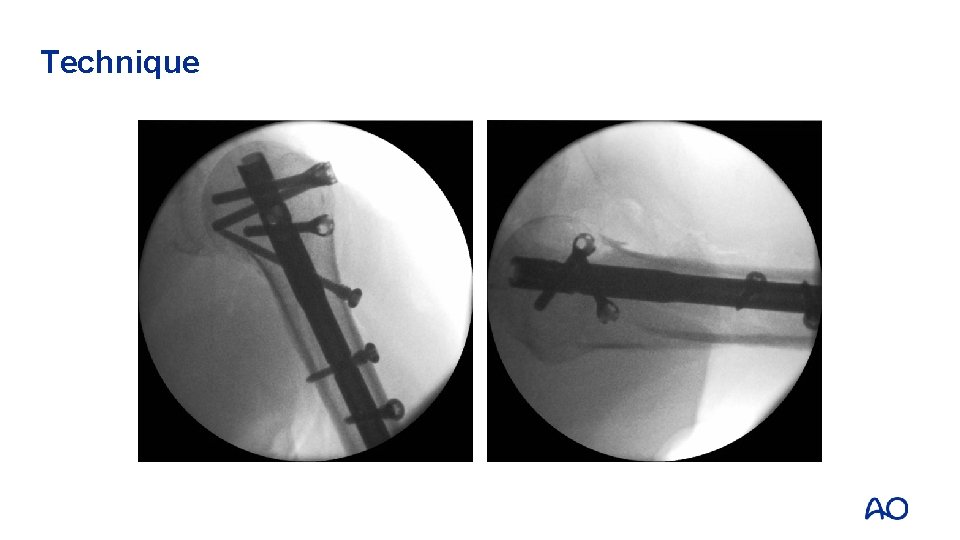
Technique

Technique
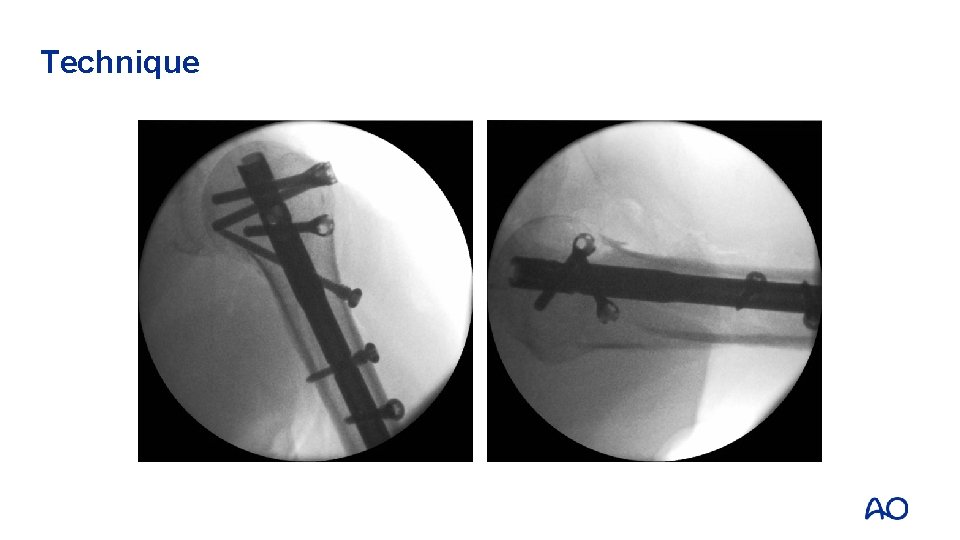
Technique
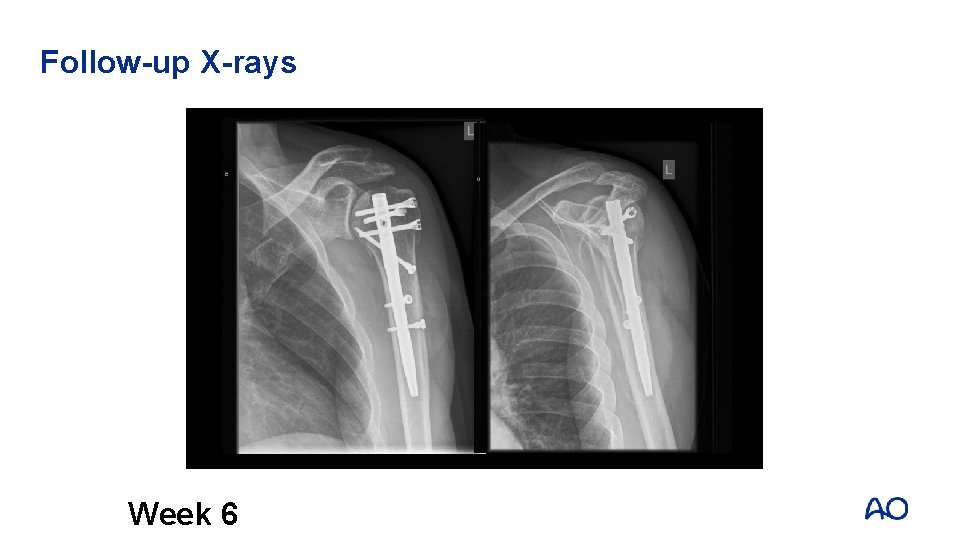
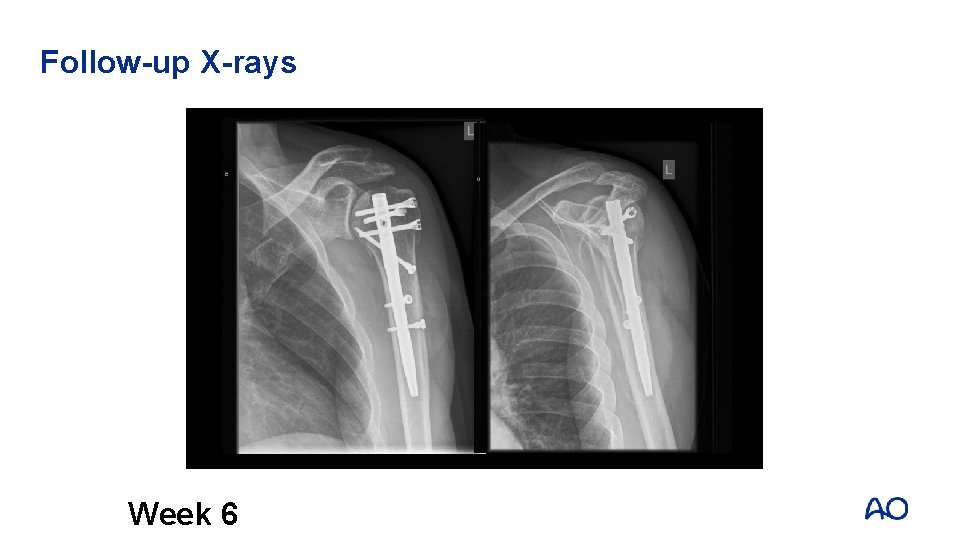
Follow-up X-rays Week 6
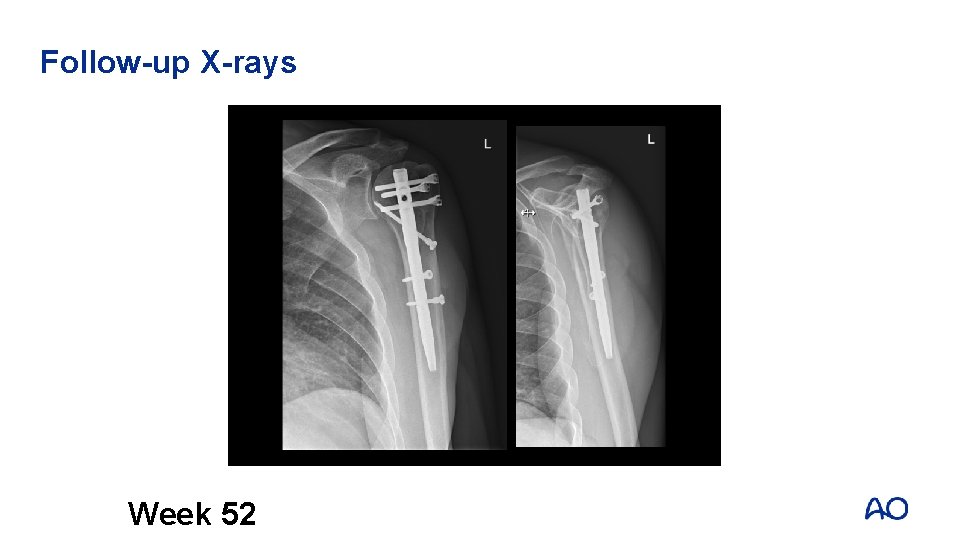
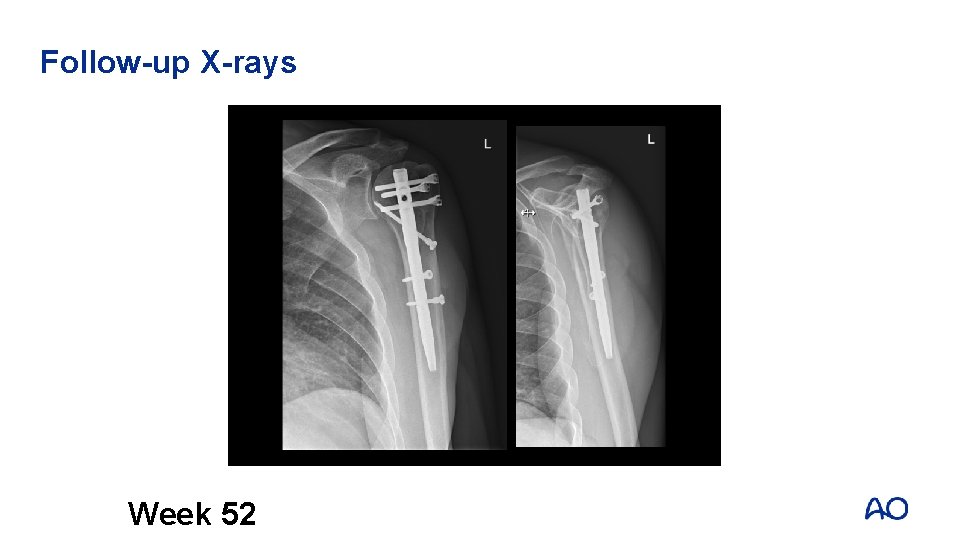
Follow-up X-rays Week 52
Take-home messages • Evaluate H-G-L-S and displacement (varus/valgus and posterior tilt). • Evaluate defects and osteoporosis. • Evaluate biological parameters (patient needs – comorbidities – vascularization head – rotator cuff). • Importance of anatomical reduction and reconstruction posteromedial support. • Exact operative technique, respecting the anatomical key-structures.