Midshaft humerus fractures Abel David MSIII University of
Midshaft humerus fractures Abel David, MS-III University of Virginia School of Medicine August 4, 2016
Epidemiology • Accounts for approximately: – 3% of all fractures – 20% of humeral fractures • Primary mechanisms of humerus fractures include: – Motor vehicle crashes – Violent injury – Accidental falls • In 3 -year epidemiological study, with n=249 consecutive humeral shaft fractures, demonstrated a bimodal distribution: – A peak in the 3 rd decade, majority males, high energy – A larger peak in the 7 th decade, majority females, low energy University of Virginia Orthopaedic Surgery
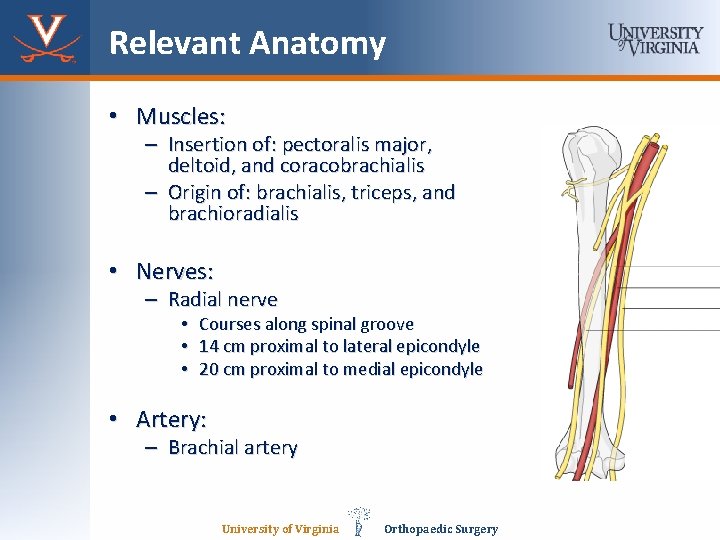
Relevant Anatomy • Muscles: – Insertion of: pectoralis major, deltoid, and coracobrachialis – Origin of: brachialis, triceps, and brachioradialis • Nerves: – Radial nerve • Courses along spinal groove • 14 cm proximal to lateral epicondyle • 20 cm proximal to medial epicondyle • Artery: – Brachial artery University of Virginia Orthopaedic Surgery
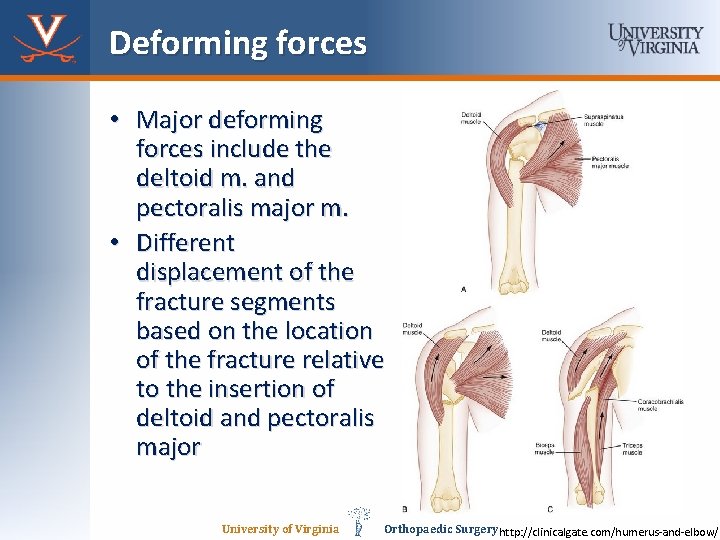
Deforming forces • Major deforming forces include the deltoid m. and pectoralis major m. • Different displacement of the fracture segments based on the location of the fracture relative to the insertion of deltoid and pectoralis major University of Virginia Orthopaedic Surgery http: //clinicalgate. com/humerus-and-elbow/
Case Report: M. B. 19 y/o F • M. B. is a 19 -year-old female who presented to the UVA ED as a trauma alert, she was the restrained occupant of a high-speed, rollover MVC. Her orthopedic injuries included: right radial shaft fracture, left humeral shaft fracture, and right forearm laceration with exposed FDS muscle/tendon. • No PMHx or PSHx University of Virginia Orthopaedic Surgery
Case Report: M. B. 19 y/o F • Right Forearm – Right forearm tender to palpation, mild deformity, 6 cm laceration with exposed muscle belly – Intact motor to AIN/PIN/U nerves – SILT M/R/U nerve distributions – Compartments soft and compressible – 2+ radial pulse • Left Arm – No deformities noted, no open wounds – Motor intact to wrist flexion/extension, finger flexion/extension/intrinsics – Intact motor to AIN/PIN/U nerve – SILT M/R/U distributions – Compartments soft and compressible – 2+ radial pulse University of Virginia Orthopaedic Surgery
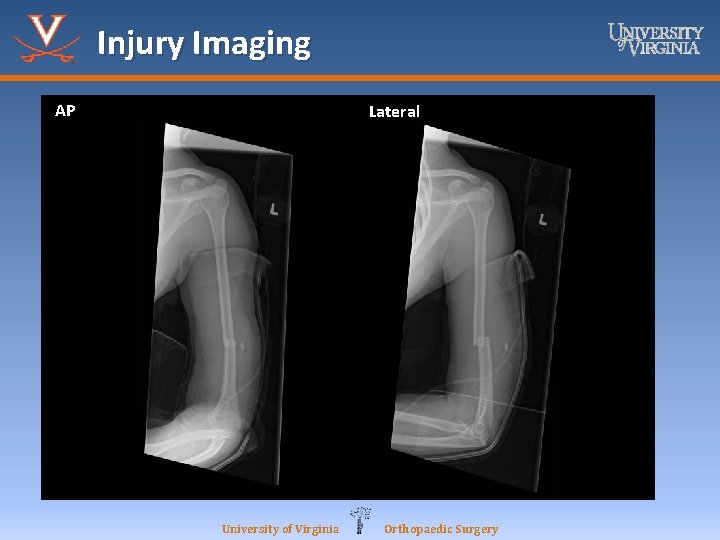
Injury Imaging AP Lateral University of Virginia Orthopaedic Surgery
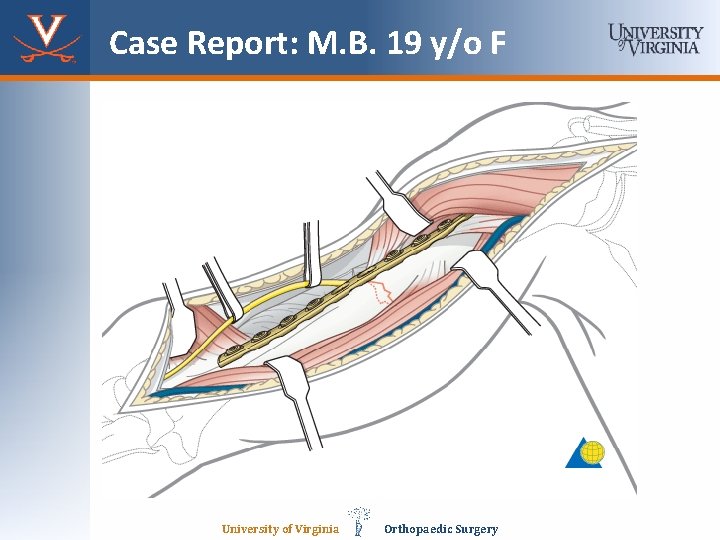
Case Report: M. B. 19 y/o F University of Virginia Orthopaedic Surgery
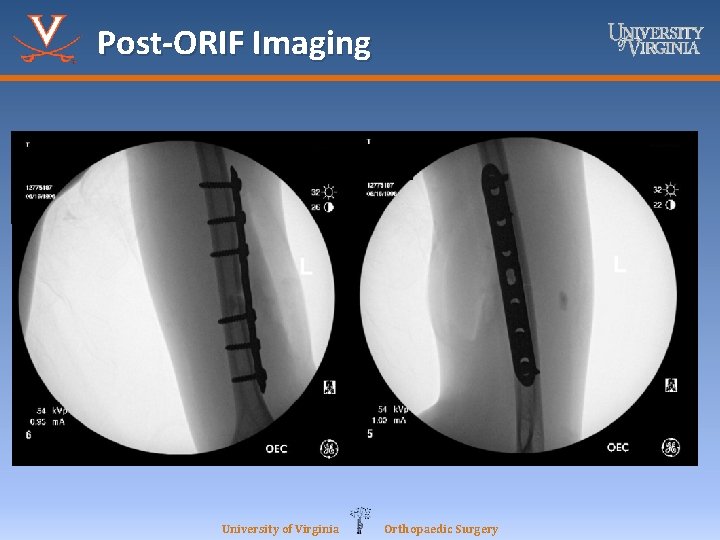
Post-ORIF Imaging University of Virginia Orthopaedic Surgery
Follow-up 2 weeks later • Remained NWB in bilateral UE with a splint on her right forearm and a sling on her left arm • Pain was well controlled, no signs or symptoms concerning for site infection, no constitutional symptoms, • ROM, strength, neurovascular status continue to remain stable • Imaging confirmed no hardware issues or fracture displacement University of Virginia Orthopaedic Surgery
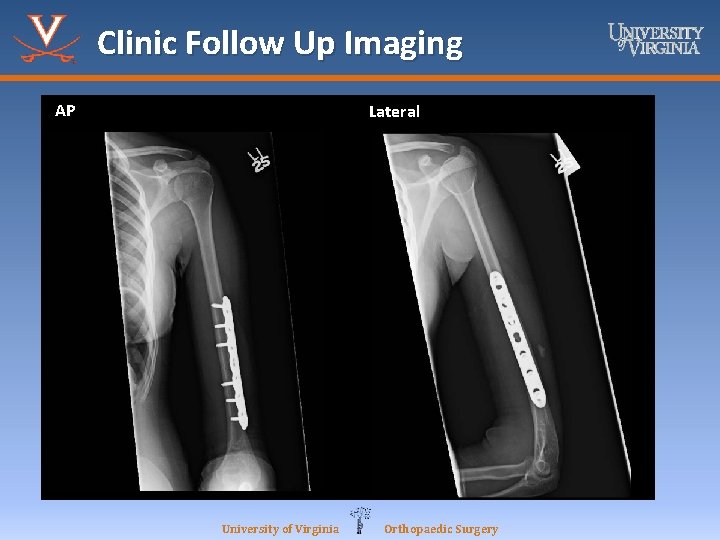
Clinic Follow Up Imaging AP Lateral University of Virginia Orthopaedic Surgery
Classification • No classification scheme of humeral shaft fractures • Traditionally described by: – Location: proximal, middle, or distal – Type of fracture line: transverse, oblique, spiral, comminuted, or segmental – Open vs. closed • AO/OTA fracture descriptions University of Virginia Orthopaedic Surgery
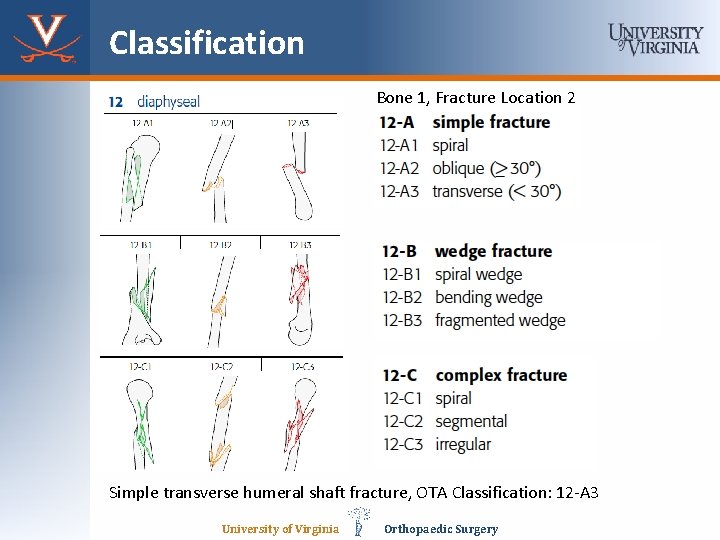
Classification Bone 1, Fracture Location 2 Simple transverse humeral shaft fracture, OTA Classification: 12 -A 3 University of Virginia Orthopaedic Surgery
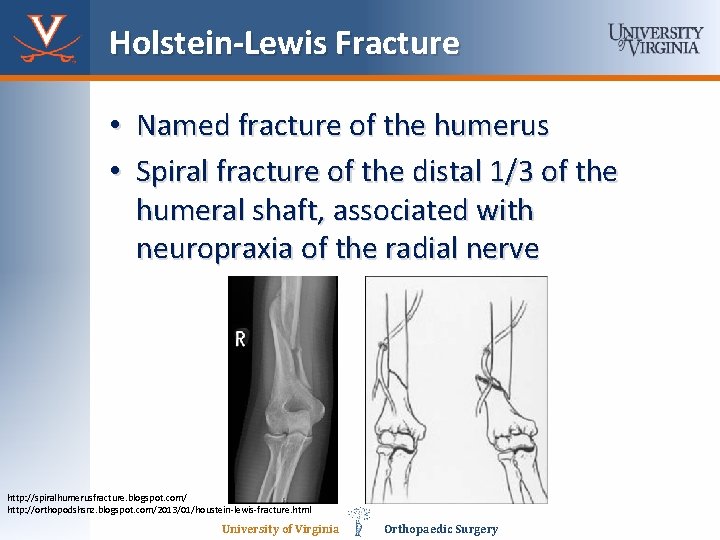
Holstein-Lewis Fracture • Named fracture of the humerus • Spiral fracture of the distal 1/3 of the humeral shaft, associated with neuropraxia of the radial nerve http: //spiralhumerusfracture. blogspot. com/ http: //orthopodshsnz. blogspot. com/2013/01/houstein-lewis-fracture. html University of Virginia Orthopaedic Surgery
Management • Non-operative management – Coaptation splint followed by functional brace • Operative management – Closed reduction, intramedullary nailing – Open reduction internal fixation University of Virginia Orthopaedic Surgery
Non-operative Management • Indicated in majority of humeral shaft fractures • Criteria for acceptable alignment: – < 20˚ of anterior angulation – < 30˚ of varus/valgus angulation – < 3 cm of shortening • Absolutely contraindicated in brachial plexus injury, vascular injury requiring repair, and severe tissue/bone loss University of Virginia Orthopaedic Surgery
Operative management, ORIF • Indications: – Open fracture – Vascular injury requiring repair – Brachial plexus injury – Compartment syndrome – Ipsilateral forearm fracture (floating elbow) – Relative: polytrauma University of Virginia Orthopaedic Surgery
Operative management, IMN • Relative indications – Pathologic fractures – Segmental fractures – Severe osteoporotic bone University of Virginia Orthopaedic Surgery
Non-operative v. operative • Plate fixation vs. functional bracing in 51 consecutive patients (19 with plate and 21 with functional bracing) – Jawa et al. • Demonstrated that operative treatment achieved more predictable alignment and quicker return of function • There was a higher risk of iatrogenic radial nerve injury, infection, and increased reoperation rates • Functional bracing was associated with skin problems, and angular deformity but function and ROM were usually acceptable University of Virginia Orthopaedic Surgery
ORIF v. IMN • Similar numbers of patients had nonunion, infection, and iatrogenic nerve injury Mean hospital stay, blood loss, and operation time were not significantly different • In two RCTs, the reoperation risk for IMN was three times that for plates (Changulani et al. Chapman et al. ) • In one RCT, patients who received IMN had more shoulder pain and decreased shoulder ROM (Changulani et al. ) University of Virginia Orthopaedic Surgery
Complications • • Malunion Non-union Radial nerve palsy Brachial artery injury University of Virginia Orthopaedic Surgery
Prognosis of Humeral Fractures • Non-union is associated with: – Long oblique fracture pattern – Alcohol abuse – Obesity – Comminuted fractures – Open fractures – Fractures in the middle third of the humeral shaft – Transverse fractures University of Virginia Orthopaedic Surgery
Summary • Relatively common fracture seen in 3 rd decade males with high energy mechanisms and in 7 th decade females with low energy mechanisms • Neurovascular assessment is important, especially the evaluation of radial nerve function and for brachial artery injury • Majority are managed non-operatively with good outcomes with a coaptation splint and functional brace • Operative management has a more predictable alignment and quicker return of function, but higher rates of iatrogenic nerve injury/infection • Additional RCTs are still needed to further validate University of Virginia Orthopaedic Surgery
References 1. 2. 3. 4. 5. 6. 7. 8. 9. Tytherleigh-Strong G, Walls N, Mc. Queen MM (1998) The epidemiology of humeral shaft fractures. J Bone Joint Surg Br; 80: 249 -53. Houwelingen AV, Mc. Kee MD (2004) Management and Complications of Humeral Shaft Fractures. University of Toronto Medical Journal; 81: 96102. Jawa A, Mc. Carty P, Doornberg J, et al (2006) Extraarticular distal third diaphysealfractures of the humerus. A comparison of functional bracing and plate fixation. J Bone Joint Surg Am; 88: 23437. Changulani M, Jain UK, Keswani T (2006) Comparison of the use of the humerusintramedullary nail and dynamic compression plate for the management of diaphysealfractures of the humerus. A randomised controlled study. Int Orthop. Mc. Cormack RG, Brien D, Buckley RE, et al (2000) Fixation of fractures of the shaft of the humerus by dynamic compression plate or intramedullary nail. A prospective, randomised trial. J Bone Joint Surg Br; 82: 3369. Chapman JR, Henley MB, Agel J, et al (2000) Randomized prospective study of humeralshaft fracture fixation: intramedullary nails versus plates. J Orthop Trauma; 14: 1626. https: //www 2. aofoundation. org/wps/portal/surgery http: //www. orthobullets. com/ University of Virginia Orthopaedic Surgery
- Slides: 24