Radiography of Proximal Humerus and Shoulder Girdle Part
- Slides: 19
Radiography of Proximal Humerus and Shoulder Girdle Part I
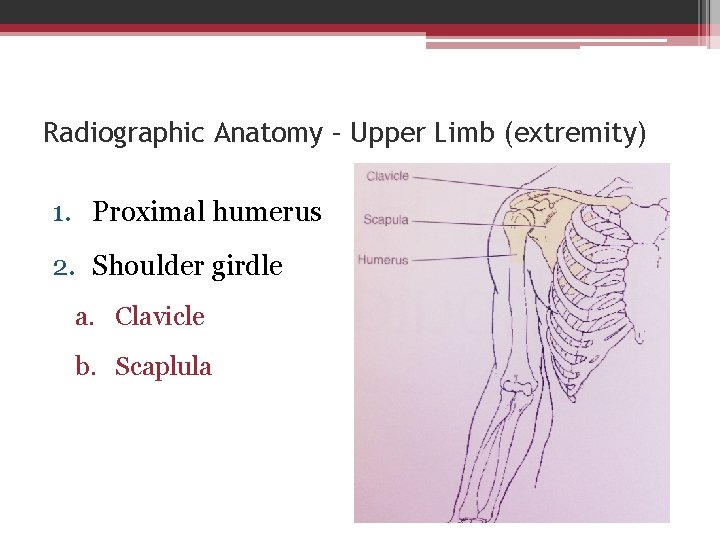
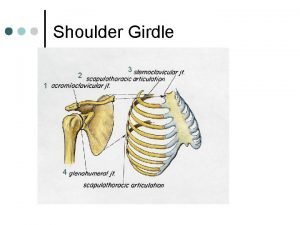
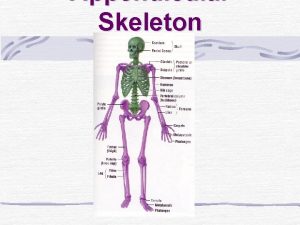
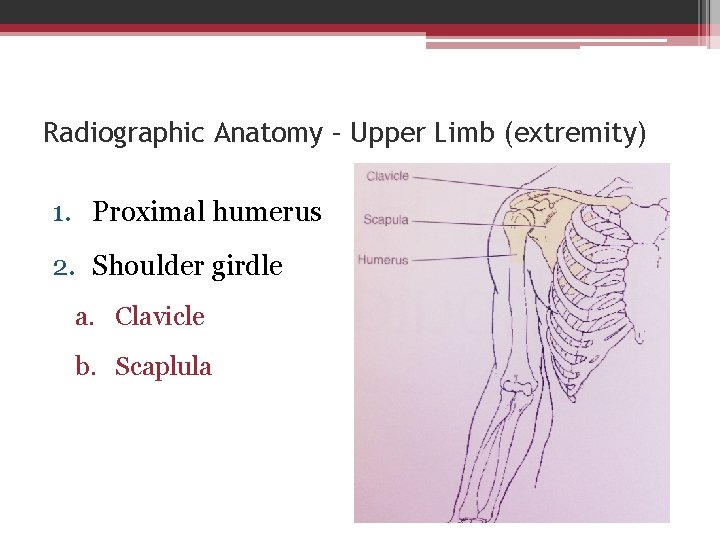
Radiographic Anatomy – Upper Limb (extremity) 1. Proximal humerus 2. Shoulder girdle a. Clavicle b. Scaplula
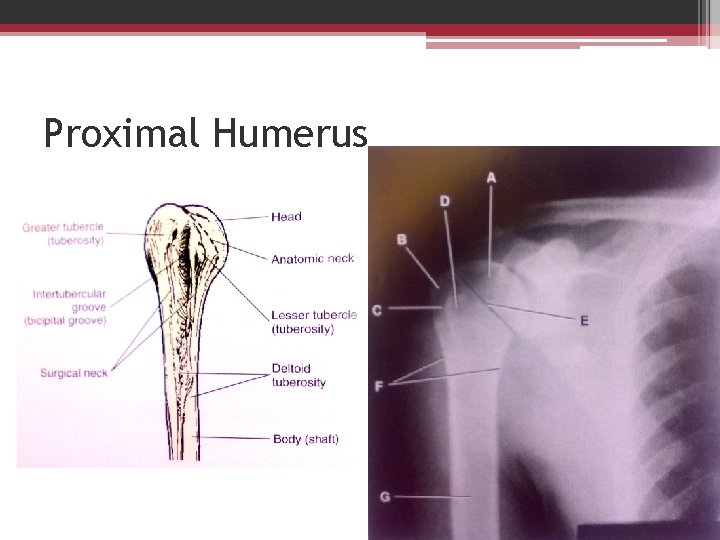
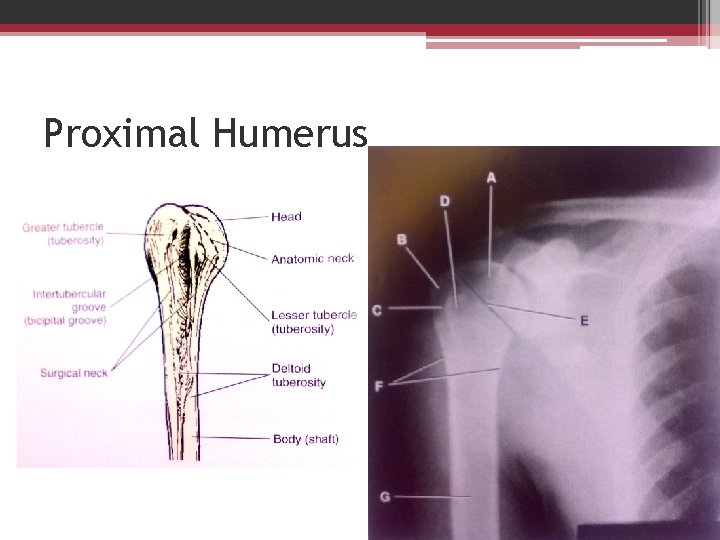
Proximal Humerus
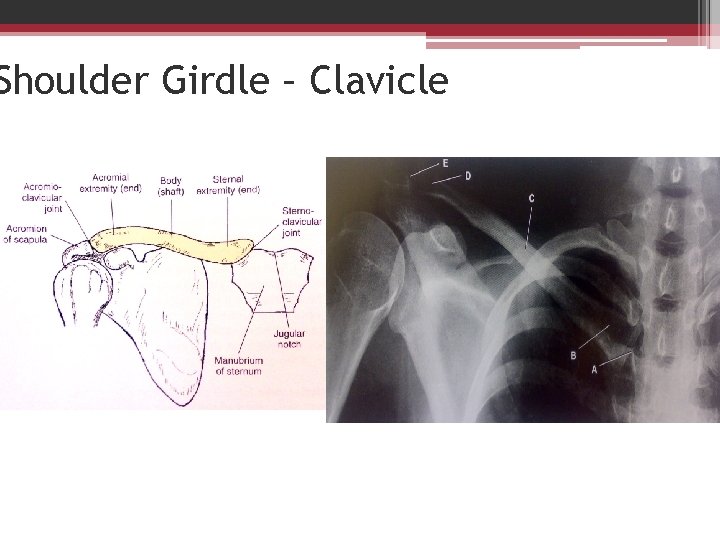
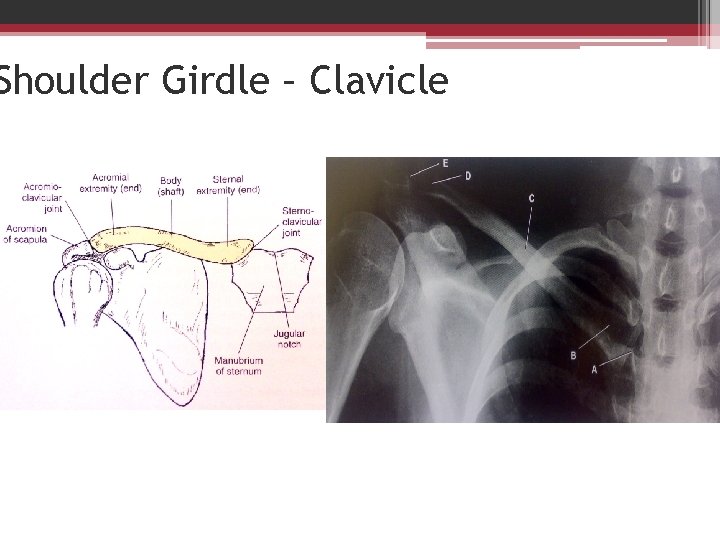
Shoulder Girdle – Clavicle
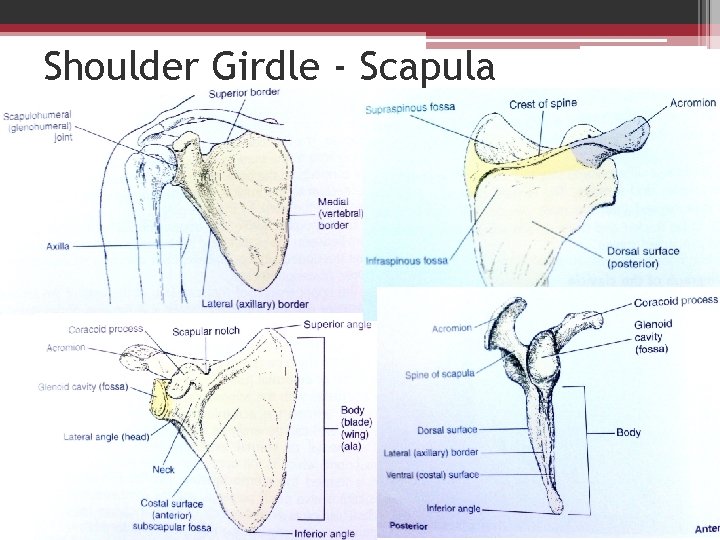
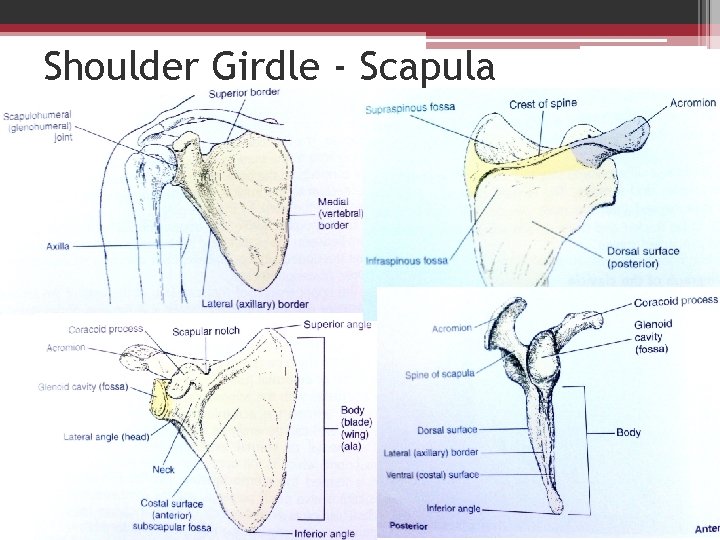
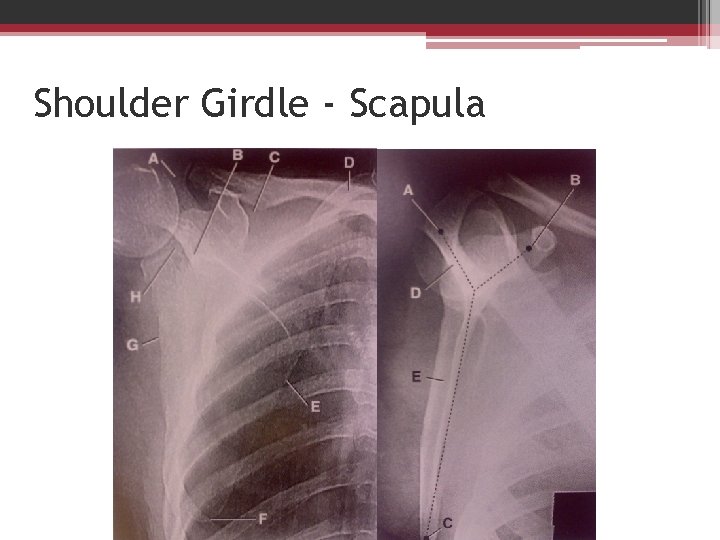
Shoulder Girdle - Scapula
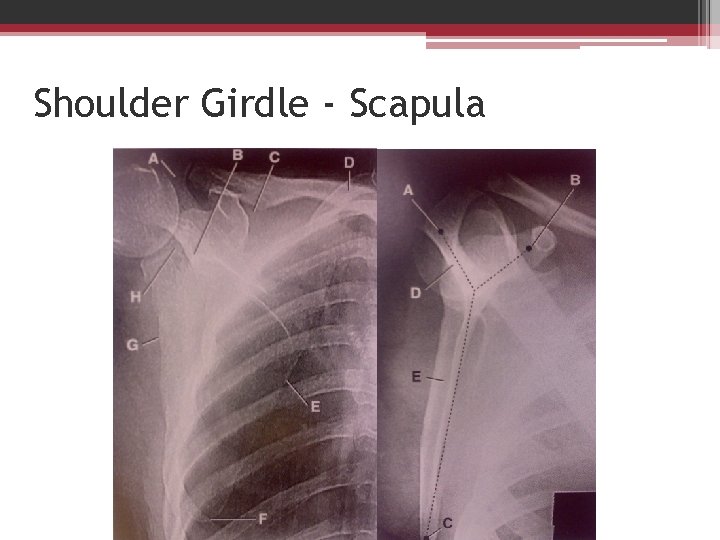
Shoulder Girdle - Scapula
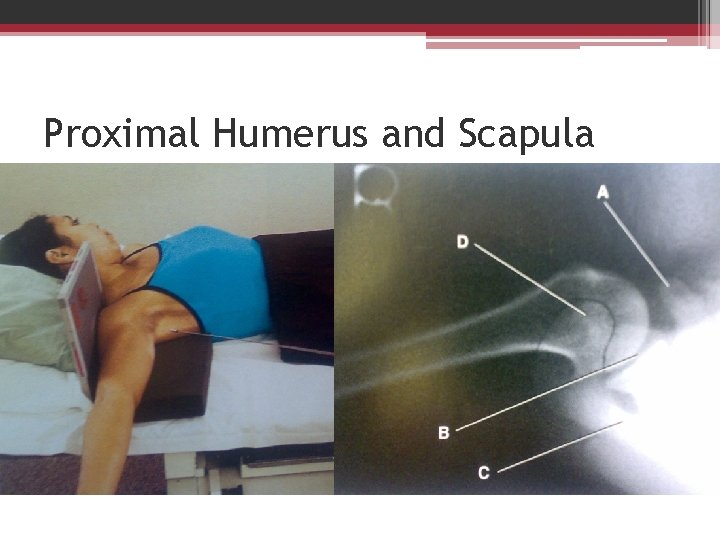
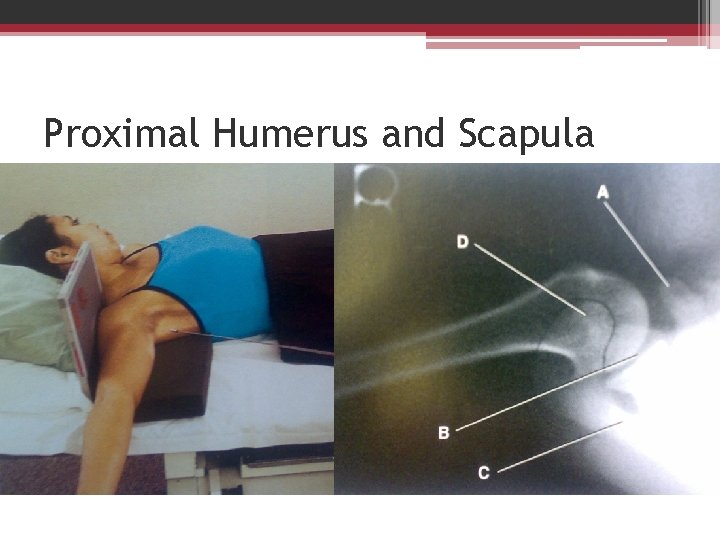
Proximal Humerus and Scapula
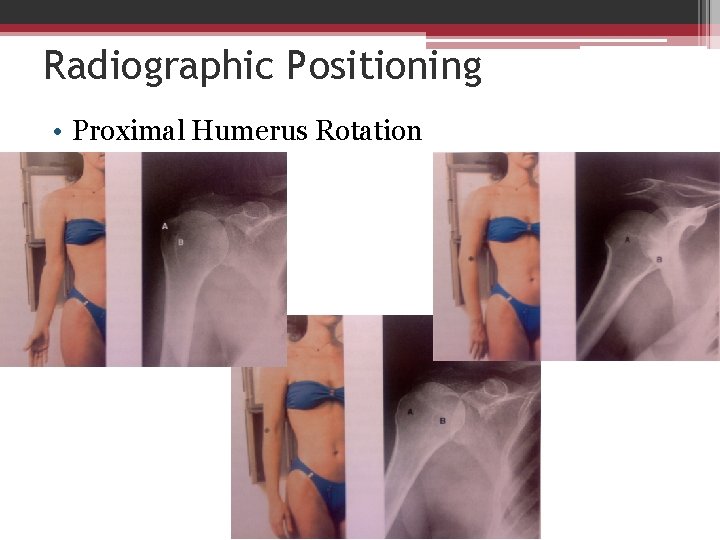
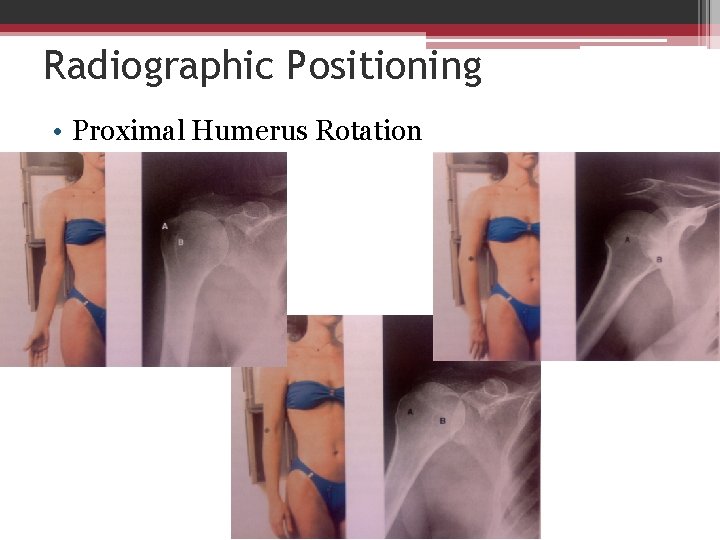
Radiographic Positioning • Proximal Humerus Rotation
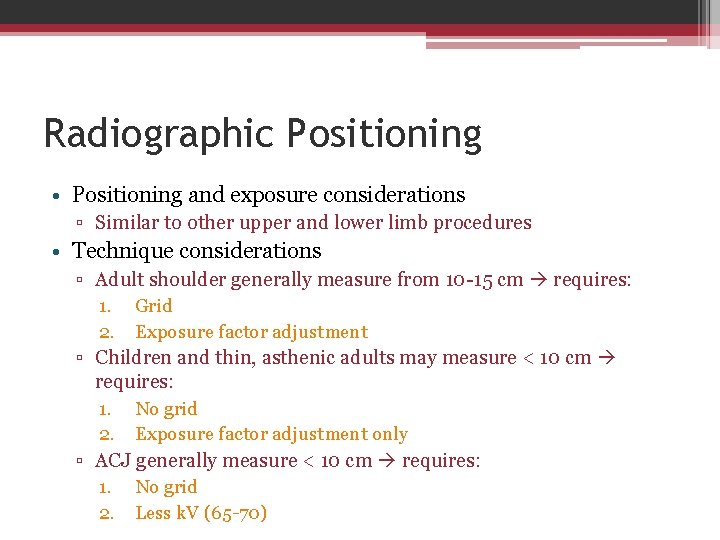
Radiographic Positioning • Positioning and exposure considerations ▫ Similar to other upper and lower limb procedures • Technique considerations ▫ Adult shoulder generally measure from 10 -15 cm requires: 1. Grid 2. Exposure factor adjustment ▫ Children and thin, asthenic adults may measure < 10 cm requires: 1. No grid 2. Exposure factor adjustment only ▫ ACJ generally measure < 10 cm requires: 1. No grid 2. Less k. V (65 -70)
Radiographic Positioning • Technique considerations for average adult shoulder: 1. Medium k. V, 70 -80 with grid if > 10 cm (if < 10 cm, 60 -70 k. V without grid) 2. Higher m. A with short exposure time 3. Small FS 4. Center cell if AEC is used 5. Adequate m. As for sufficient density (to visualize ST, bone margins, and trabicular margins of all bones) 6. 100 -110 cm (40 -44 inches) SID, except for ACJ, which requires 180 cm (72 inches) SID for less divergence
Radiographic Positioning • Shield ▫ Use lead vinyl-covered shield over the patient’s lap or gonadal area ▫ Protect thyroid, lungs, and breast by 1. Close collimation 2. Contact shield
Radiographic Positioning • Pediatric patients ▫ ▫ Patient motion should be restricted Use immobilization device such as sponge, tape, or sand bags Ask family for help ensure protection for help Speak to child in a soothing manner and with language the child can readily understand to ensure maximal cooperation • Geriatric patients ▫ Provide clear and complete instructions ▫ Routine examination might be altered to accommodate the older patient’s physical condition ▫ Use adequate immobilization device ▫ Exposure factors may need to be reduced
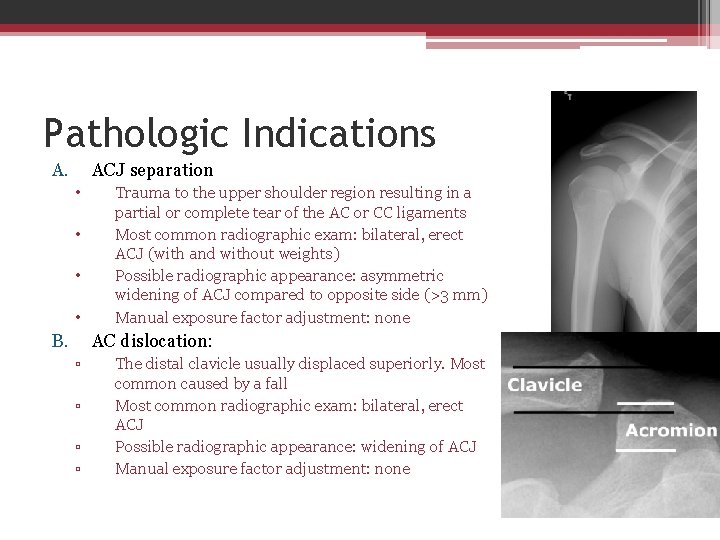
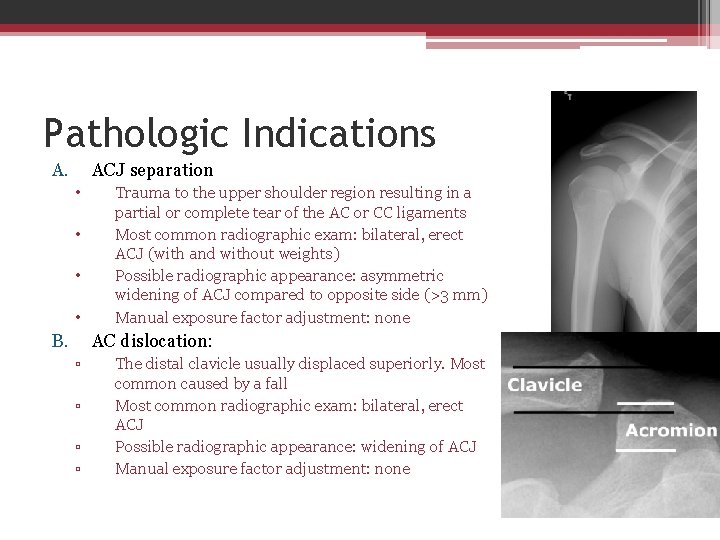
Pathologic Indications A. ACJ separation • • B. Trauma to the upper shoulder region resulting in a partial or complete tear of the AC or CC ligaments Most common radiographic exam: bilateral, erect ACJ (with and without weights) Possible radiographic appearance: asymmetric widening of ACJ compared to opposite side (>3 mm) Manual exposure factor adjustment: none AC dislocation: ▫ ▫ The distal clavicle usually displaced superiorly. Most common caused by a fall Most common radiographic exam: bilateral, erect ACJ Possible radiographic appearance: widening of ACJ Manual exposure factor adjustment: none
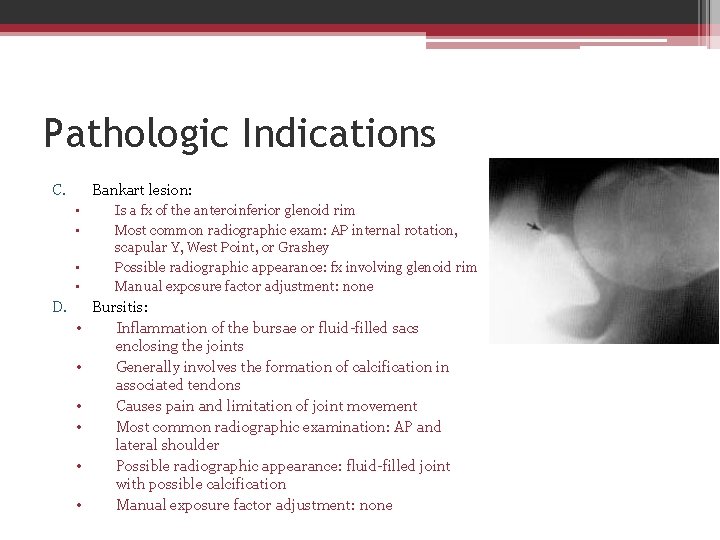
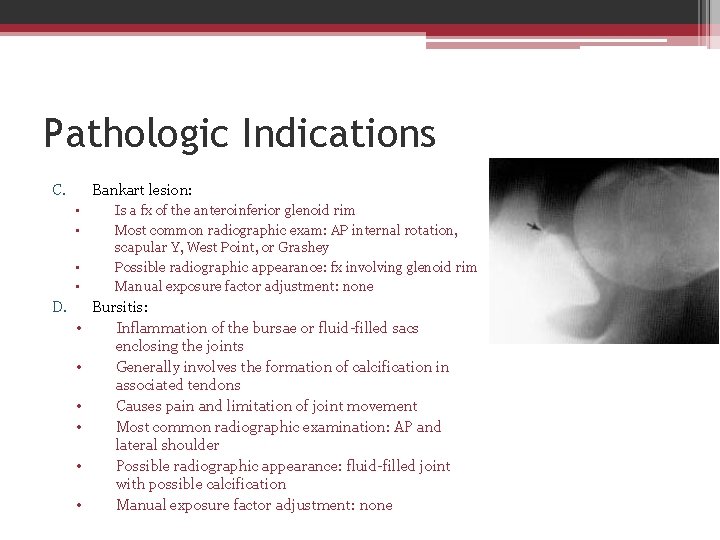
Pathologic Indications C. Bankart lesion: • • D. • • • Is a fx of the anteroinferior glenoid rim Most common radiographic exam: AP internal rotation, scapular Y, West Point, or Grashey Possible radiographic appearance: fx involving glenoid rim Manual exposure factor adjustment: none Bursitis: Inflammation of the bursae or fluid-filled sacs enclosing the joints Generally involves the formation of calcification in associated tendons Causes pain and limitation of joint movement Most common radiographic examination: AP and lateral shoulder Possible radiographic appearance: fluid-filled joint with possible calcification Manual exposure factor adjustment: none
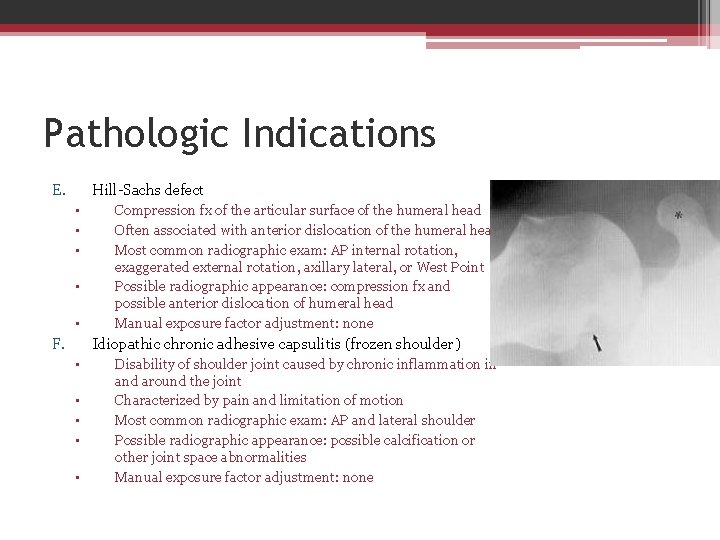
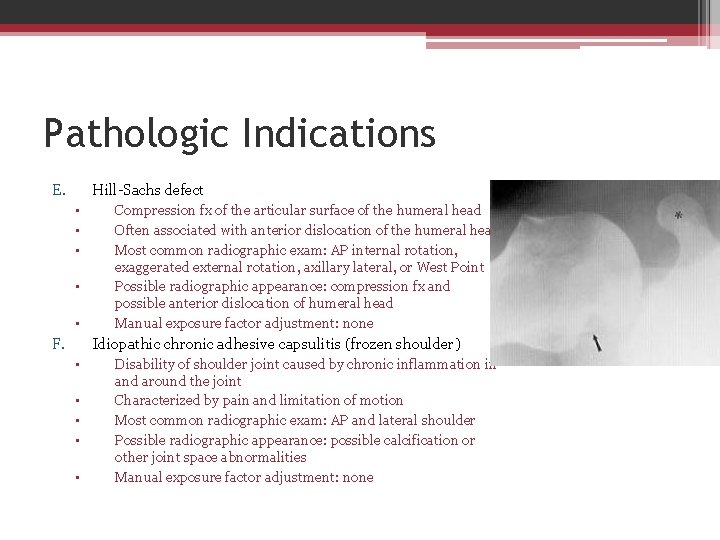
Pathologic Indications E. Hill-Sachs defect • • • F. Compression fx of the articular surface of the humeral head Often associated with anterior dislocation of the humeral head Most common radiographic exam: AP internal rotation, exaggerated external rotation, axillary lateral, or West Point Possible radiographic appearance: compression fx and possible anterior dislocation of humeral head Manual exposure factor adjustment: none Idiopathic chronic adhesive capsulitis (frozen shoulder) • • • Disability of shoulder joint caused by chronic inflammation in and around the joint Characterized by pain and limitation of motion Most common radiographic exam: AP and lateral shoulder Possible radiographic appearance: possible calcification or other joint space abnormalities Manual exposure factor adjustment: none
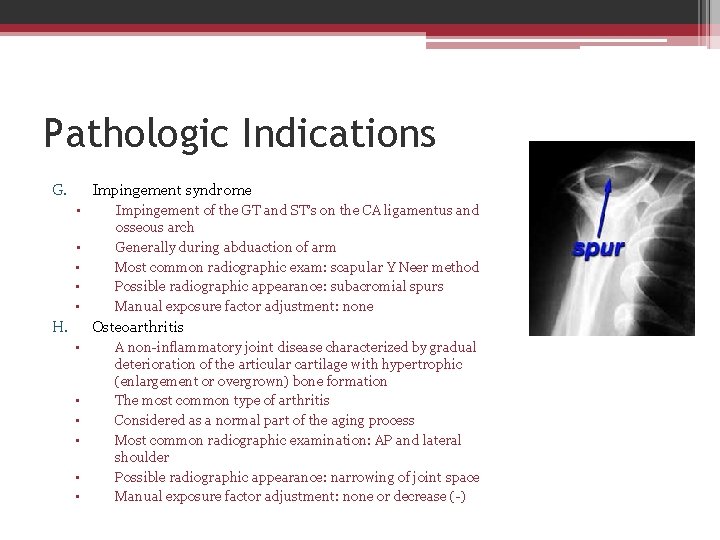
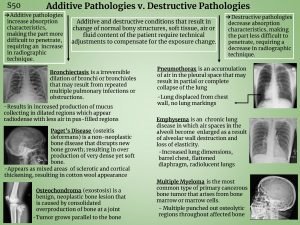
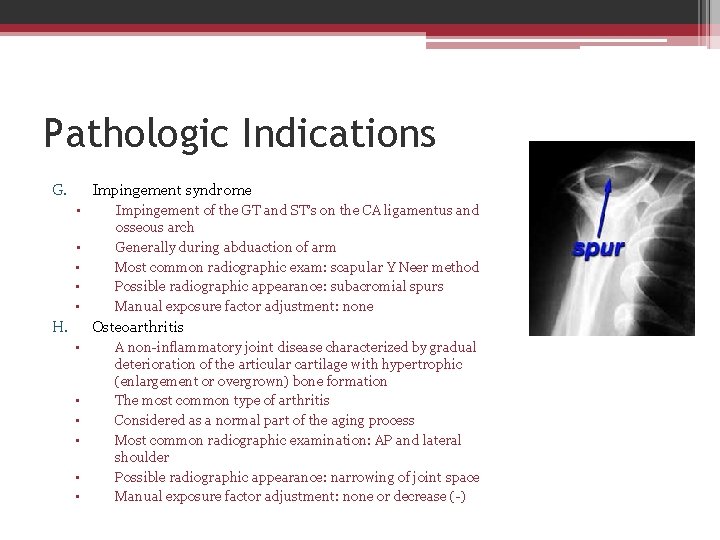
Pathologic Indications G. Impingement syndrome • • • H. Impingement of the GT and ST’s on the CA ligamentus and osseous arch Generally during abduaction of arm Most common radiographic exam: scapular Y Neer method Possible radiographic appearance: subacromial spurs Manual exposure factor adjustment: none Osteoarthritis • • • A non-inflammatory joint disease characterized by gradual deterioration of the articular cartilage with hypertrophic (enlargement or overgrown) bone formation The most common type of arthritis Considered as a normal part of the aging process Most common radiographic examination: AP and lateral shoulder Possible radiographic appearance: narrowing of joint space Manual exposure factor adjustment: none or decrease (-)
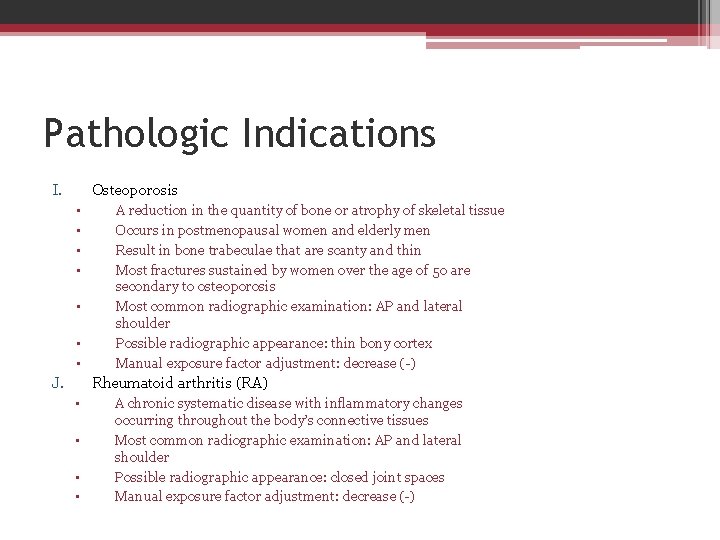
Pathologic Indications I. Osteoporosis • • J. A reduction in the quantity of bone or atrophy of skeletal tissue Occurs in postmenopausal women and elderly men Result in bone trabeculae that are scanty and thin Most fractures sustained by women over the age of 50 are secondary to osteoporosis Most common radiographic examination: AP and lateral shoulder Possible radiographic appearance: thin bony cortex Manual exposure factor adjustment: decrease (-) Rheumatoid arthritis (RA) • • A chronic systematic disease with inflammatory changes occurring throughout the body’s connective tissues Most common radiographic examination: AP and lateral shoulder Possible radiographic appearance: closed joint spaces Manual exposure factor adjustment: decrease (-)
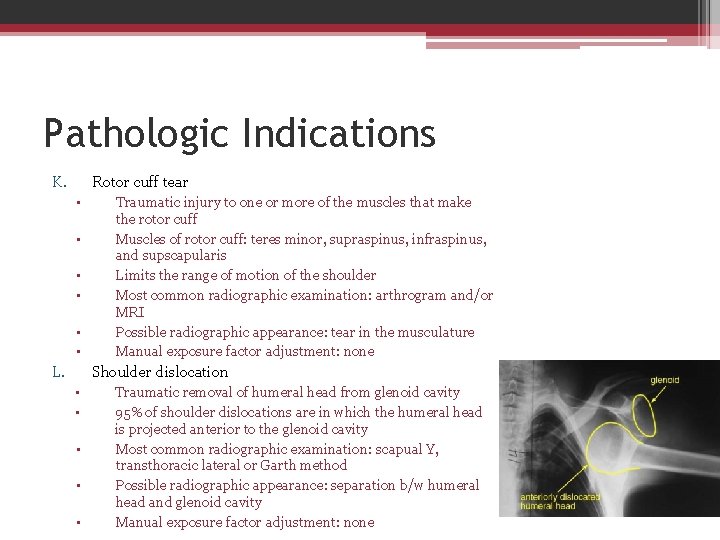
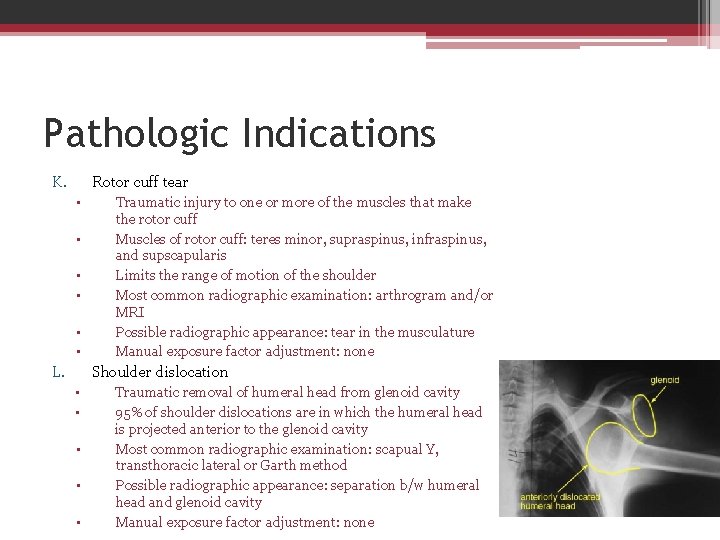
Pathologic Indications K. Rotor cuff tear • • • L. Traumatic injury to one or more of the muscles that make the rotor cuff Muscles of rotor cuff: teres minor, supraspinus, infraspinus, and supscapularis Limits the range of motion of the shoulder Most common radiographic examination: arthrogram and/or MRI Possible radiographic appearance: tear in the musculature Manual exposure factor adjustment: none Shoulder dislocation • • • Traumatic removal of humeral head from glenoid cavity 95% of shoulder dislocations are in which the humeral head is projected anterior to the glenoid cavity Most common radiographic examination: scapual Y, transthoracic lateral or Garth method Possible radiographic appearance: separation b/w humeral head and glenoid cavity Manual exposure factor adjustment: none
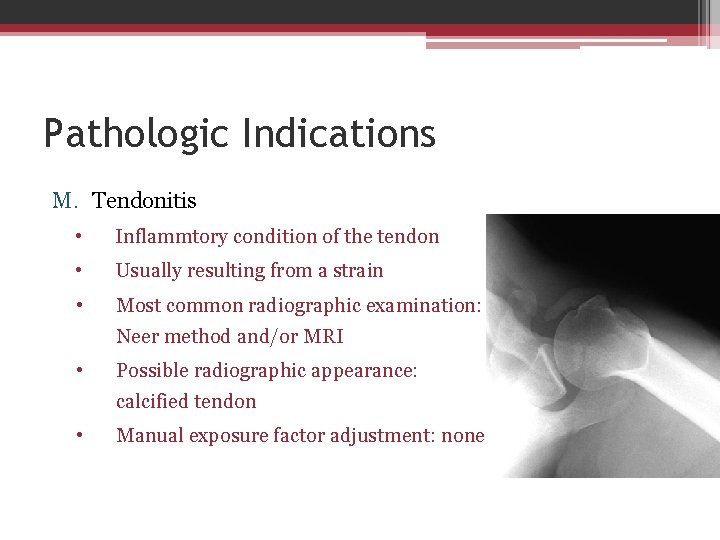
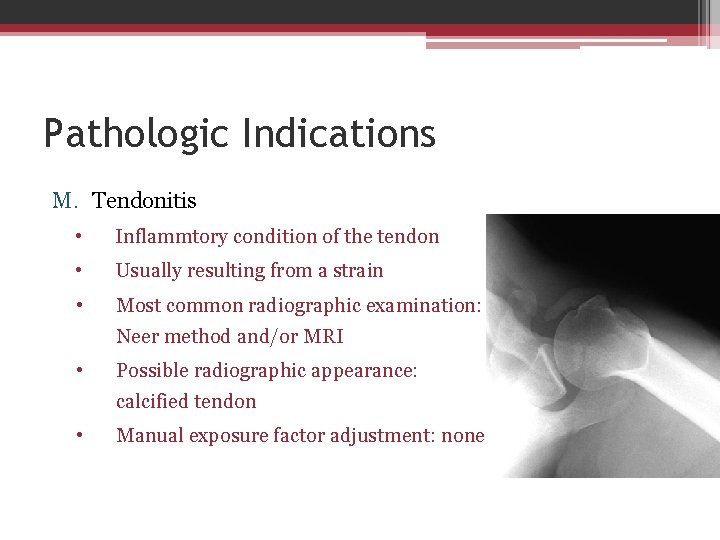
Pathologic Indications M. Tendonitis • Inflammtory condition of the tendon • Usually resulting from a strain • Most common radiographic examination: Neer method and/or MRI • Possible radiographic appearance: calcified tendon • Manual exposure factor adjustment: none
 Radial groove of humerus
Radial groove of humerus Coaptation splint
Coaptation splint Shoulder girdle muscles
Shoulder girdle muscles Scapula bony landmarks
Scapula bony landmarks Shoulder girdle landmarks
Shoulder girdle landmarks Muscles that attach to sacrum
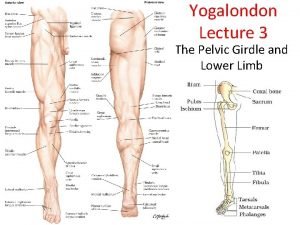
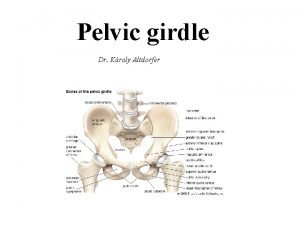
Muscles that attach to sacrum Pelvic images
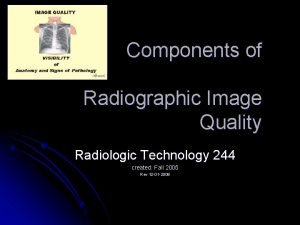
Pelvic images Sharpness of radiographic image
Sharpness of radiographic image Soot and whitewash radiography
Soot and whitewash radiography Is osteoporosis additive or destructive
Is osteoporosis additive or destructive Linen girdle
Linen girdle Linen girdle
Linen girdle Anterior muscles of the neck
Anterior muscles of the neck Vogts white limbal girdle
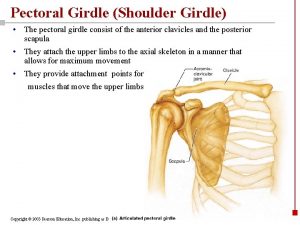
Vogts white limbal girdle Pectoral girdle diagram
Pectoral girdle diagram Pectoral girdle
Pectoral girdle Concept map on vertebrates
Concept map on vertebrates Limb girdle weakness
Limb girdle weakness Polimegatismo endoteliale
Polimegatismo endoteliale Thorax
Thorax