Pressure Ulcer Prevention at North Memorial So whats

- Slides: 24
Pressure Ulcer Prevention at North Memorial
So what’s the big deal ?
Why We Practice Pressure Ulcer Prevention n Maintenance of skin integrity and pressure ulcer prevention is a nursing sensitive indicator of quality nursing care (American Nurses Association).
Why We Practice Pressure Ulcer Prevention n It’s a community expectation.
Why We Practice Pressure Ulcer Prevention n Pressure ulcers are a reportable complication. ¨ www. health. state. mn. us/patientsafety Patient Safety Link n Adverse Health Events in Minnesota n ¨ Avoidable vs. Unavoidable
Why We Practice Pressure Ulcer Prevention It is more cost effective to prevent a pressure ulcer than to treat one. n Average cost per ulcer = $27, 000 n Annual US healthcare costs are over $3. 6 billion n
Why We Practice Pressure Ulcer Prevention n It’s the right thing to do !!!!
Components of a Pressure Ulcer Prevention Program n A clear process for identifying a patient's risk for developing pressure ulcers. n Strategies aimed at pressure ulcer prevention for the patient at risk.
Components of a Pressure Ulcer Prevention Program n Pressure ulcer prevention and treatment initiatives should be: ¨ Evidence based ICSI (Institute for Clinical Systems Improvement) Guidelines (2006) www. mnpatientsafety. org n WOCN Clinical Practice Guideline (2003). Prevention and Management of Pressure Ulcers. www. wocn. org n NPUAP (National Pressure Ulcer Advisory Panel) www. npuap. org n
Risk Assessment n n Should be performed at the point of entry to a health care facility and repeated on a regularly scheduled basis or with any change in condition. At the time of patient "hand offs". WOCN Guideline for Prevention and Management of Pressure Ulcers (2003).
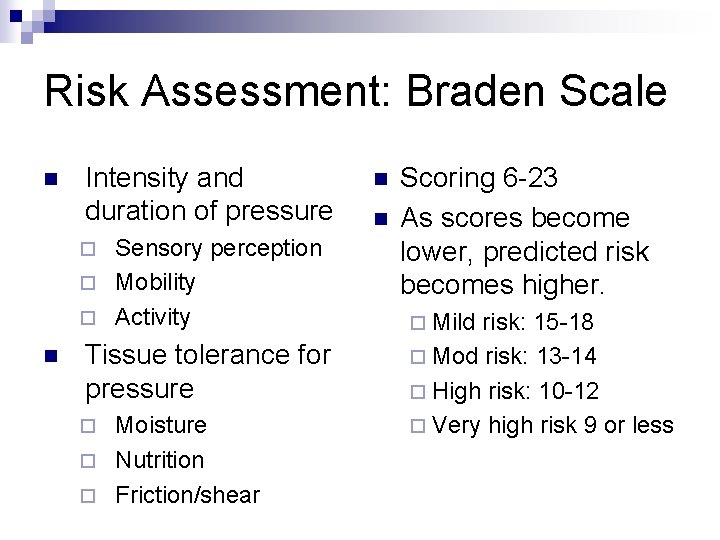
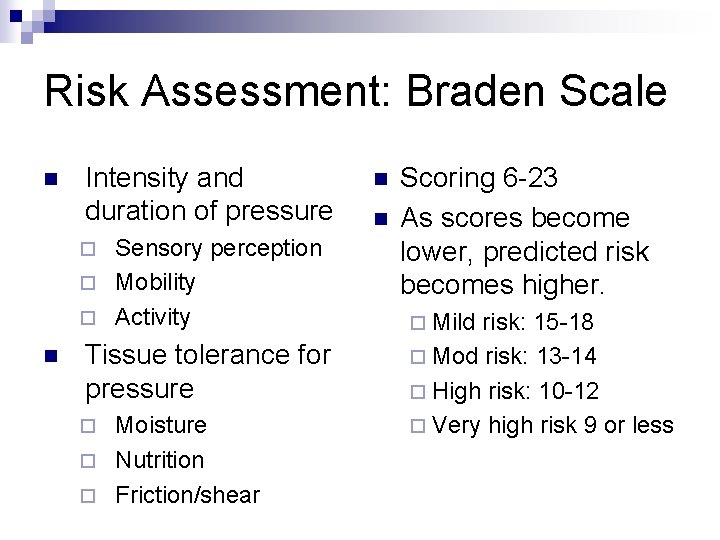
Risk Assessment: Braden Scale n Intensity and duration of pressure Sensory perception ¨ Mobility ¨ Activity ¨ n Tissue tolerance for pressure Moisture ¨ Nutrition ¨ Friction/shear ¨ n n Scoring 6 -23 As scores become lower, predicted risk becomes higher. ¨ Mild risk: 15 -18 ¨ Mod risk: 13 -14 ¨ High risk: 10 -12 ¨ Very high risk 9 or less
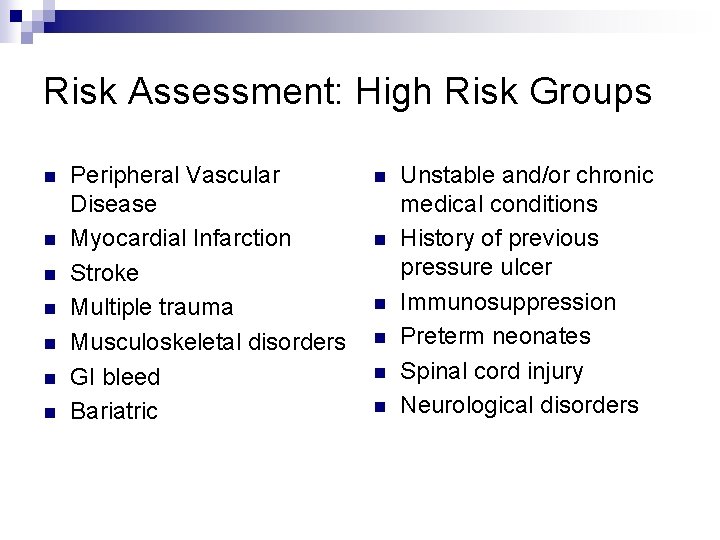
Risk Assessment: High Risk Groups n n n n Peripheral Vascular Disease Myocardial Infarction Stroke Multiple trauma Musculoskeletal disorders GI bleed Bariatric n n n Unstable and/or chronic medical conditions History of previous pressure ulcer Immunosuppression Preterm neonates Spinal cord injury Neurological disorders
Risk Assessment: Skin Inspection n n A head to toe inspection and palpation should be done on every patient upon admission, particularly over pressure points. Repeat every 8 -24 hours ¨ Inspect ¨ Palpate ¨ Ask ICSI (2006)
Risk Assessment Documentation n Communication n Patient Education n
Skin Safety: Pressure Ulcer Prevention Minimize or eliminate friction and shear. n Minimize pressure n Manage moisture n Maintain adequate nutrition/hydration n
Skin Safety: Friction and Shear Friction: n The force of two surfaces moving across each other n Can cause superficial abrasions or blisters
Skin Safety: Friction and Shearing Force: n Skin sticks to surface n Deeper tissues move in opposite direction n Capillaries kink n Local ischemia
Skin Safety: Minimize Pressure Schedule regular and frequent turning and repositioning for bed and chair bound individuals. n Use support surfaces on beds and chairs to reduce or relieve pressure. n Relieve pressure to heels by using pillows or other devices. n
Skin Safety: Manage Moisture Skin hydration issues n Dry skin ¨ Skin with too little moisture 2. 5 times more likely to ulcerate than healthy skin. n Skin moist from incontinence ¨ 5 times more likely to ulcerate than dry skin.
Skin Safety: Manage Moisture Implement a toileting schedule n Use ph-balanced cleansers n Contain urine or stool n Avoid chux, briefs, diapers. n
Skin Safety: Maintain adequate nutrition and hydration Maintain adequate nutrition that is compatible with the individual’s wishes or condition. n Consult a nutritionist in cases of suspected or identified nutritional deficiencies. n
Skin Safety Documentation n Communication n Patient/Caregiver Education n ¨ Causes and risk factors ¨ Ways to minimize risk n Implementation
Is your process in place? Risk assessment done on admission and at appropriate intervals? ü Appropriate prevention strategies initiated for patients at risk? ü Appropriate referrals initiated? ü Patient/caregiver education done? ü Document, document. ü

Questions ?
 Primary prevention secondary prevention tertiary prevention
Primary prevention secondary prevention tertiary prevention Sskin bundle hse
Sskin bundle hse Nasal cannula pressure ulcer prevention
Nasal cannula pressure ulcer prevention Gastric ulcer
Gastric ulcer Antrectomy
Antrectomy Anatomy of an ulcer
Anatomy of an ulcer Typhoid and tuberculous ulcer
Typhoid and tuberculous ulcer Types of gastric ulcer
Types of gastric ulcer Billroth ii anatomy
Billroth ii anatomy Bedsore grade
Bedsore grade Pressure ulcer safety cross template
Pressure ulcer safety cross template Pressure ulcer pico question
Pressure ulcer pico question Braden scale score
Braden scale score Category 4 pressure ulcer
Category 4 pressure ulcer Pressure ulcer clipart
Pressure ulcer clipart Depuap
Depuap True north vs magnetic north
True north vs magnetic north North east and north cumbria integrated care system
North east and north cumbria integrated care system Lesson 1 the industrial north
Lesson 1 the industrial north The north pole ____ a latitude of 90 degrees north
The north pole ____ a latitude of 90 degrees north Patella type 3
Patella type 3 Pressure support vs pressure control
Pressure support vs pressure control Pressure mapping for pressure ulcers
Pressure mapping for pressure ulcers Intrapulmonary pressure vs intrapleural pressure
Intrapulmonary pressure vs intrapleural pressure Oncotic pressure vs osmotic pressure
Oncotic pressure vs osmotic pressure