Peripheral nerve injuries Structure of a nerve It
























- Slides: 75
Peripheral nerve injuries.

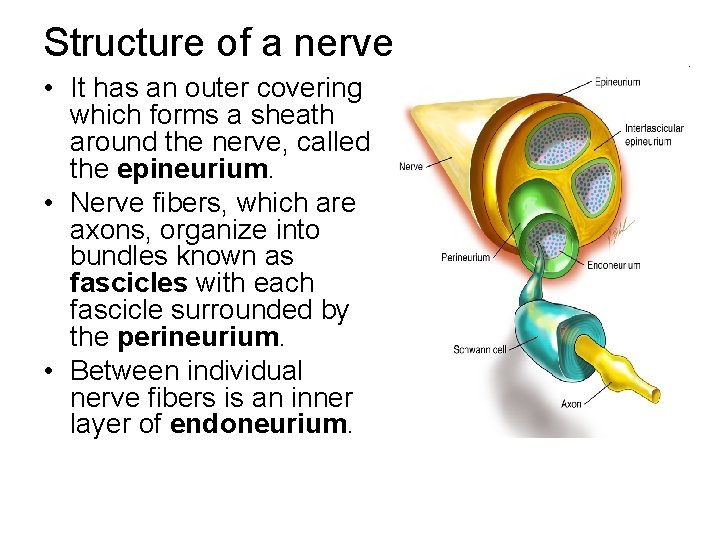
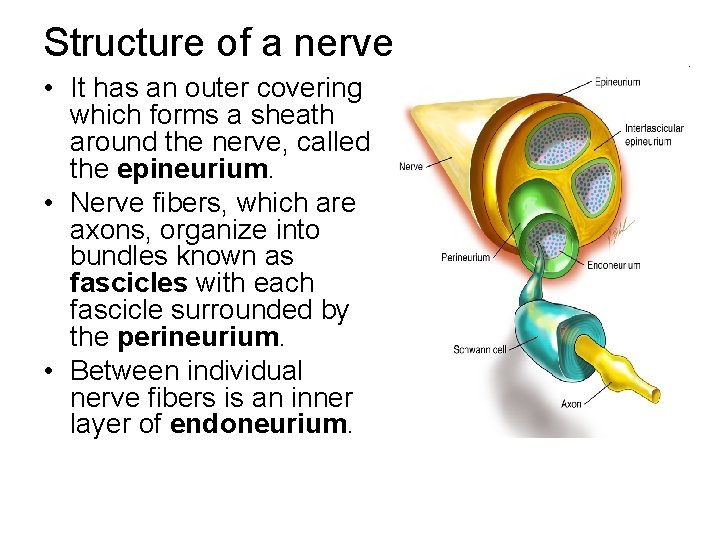
Structure of a nerve • It has an outer covering which forms a sheath around the nerve, called the epineurium. • Nerve fibers, which are axons, organize into bundles known as fascicles with each fascicle surrounded by the perineurium. • Between individual nerve fibers is an inner layer of endoneurium.

Peripheral nerve injury Dermotome : • is an area of skin supplied by a single spinal root Myotome : • Represents a muscle unit supplied by a single spinal root
Seddon's classification Neurapraxia -- temporary paralysis of a nerve caused by lack of blood flow or by pressure on the affected nerve with no loss of structural continuity. Axonotmesis – • neural tube intact, but axons are disrupted. • nerves are likely to recover. Neurotmesis – • the neural tube is severed. • Injuries are likely permanent without repair.
Symptomatology of Peripheral Nerve Disease • • Impairment of motor function Diminution or loss of tendon reflexes Sensory loss Paresthesias, pain, dysesthesias Sensory ataxia and tremor Deformity and trophic changes Autonomic dysfunction Fasciculations, cramps and spasms
Typical deformities : • Wrist drop ---- radial nerve injury • Claw hand ---- ulnar nerve injury • Foot drop ---- lateral popliteal nerve injury • Ape thumb ---- median nerve injury • Winging of scapula ---- thoracodorsal nerve injury • Pointing index ---- median nerve injury
Simple screening tests • Ulnar nerve injury : – Loss of pain at tip of the little finger • Medial nerve injury : – Loss of pain at tip of index finger • Radial nerve injury : – Inability to extend thumb
Incidence of Peripheral nerve injury • Radial nerve ------ commonly injuried • Ulnar nerve ------- 30 % • Median nerve ----- 15 % • Lumbosacral plexus ---- 3 %
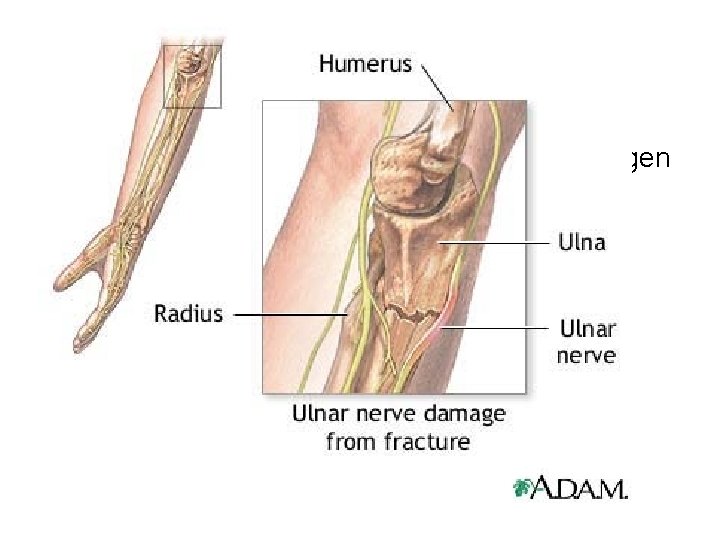
Ulnar nerve • Ulnar nerve injuries gives rise to claw hand deformity
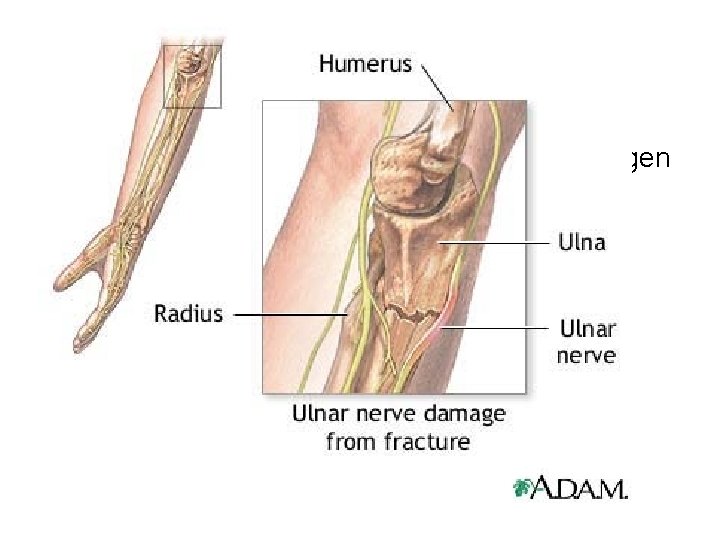
Ulnar nerve injury Causes : General causes : metabolic diseases , collagen diseases , malignancies , endogenous or exogenous toxins , chemical or mechanical trauma , etc.

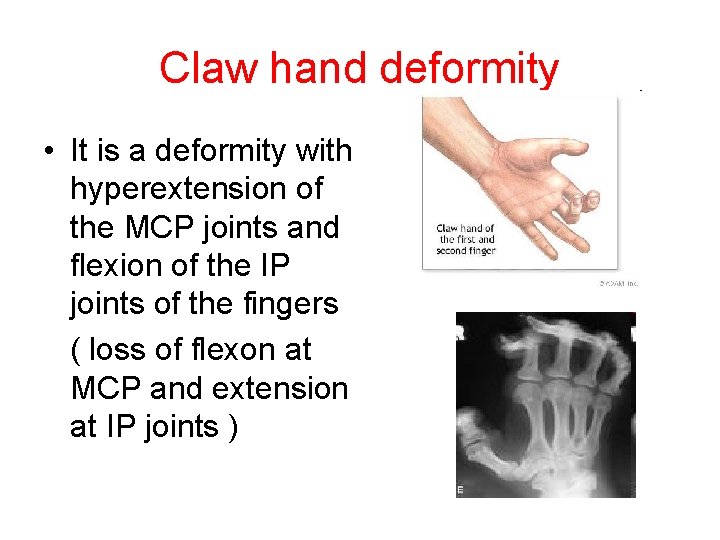
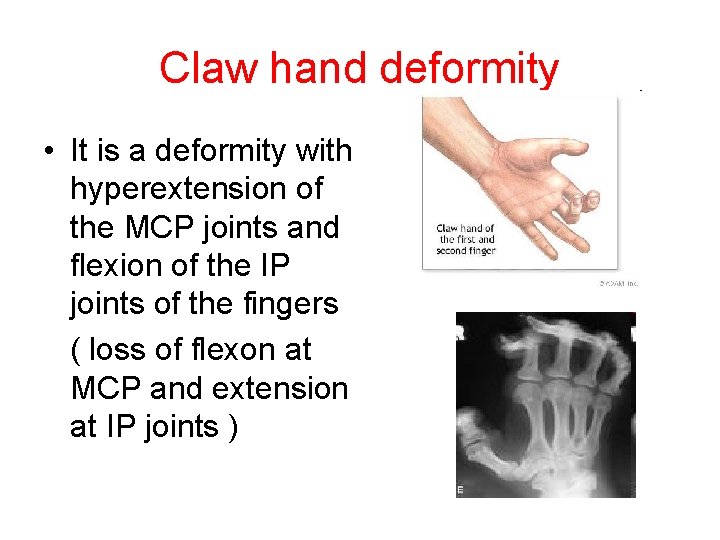
Claw hand deformity • It is a deformity with hyperextension of the MCP joints and flexion of the IP joints of the fingers ( loss of flexon at MCP and extension at IP joints )
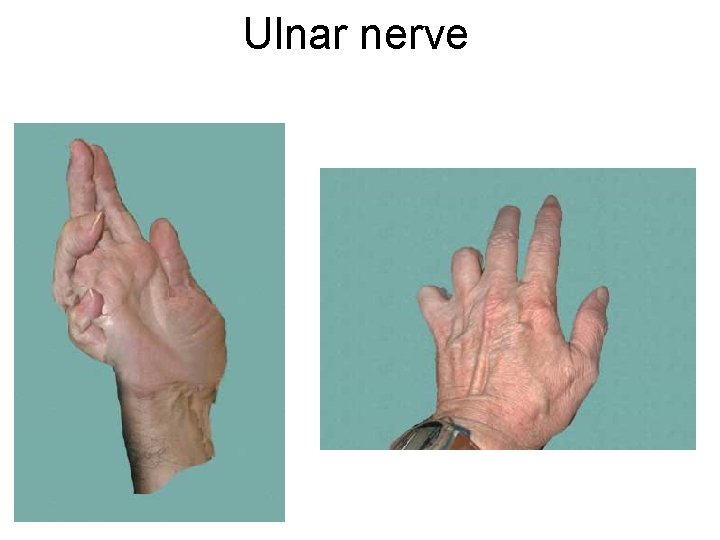
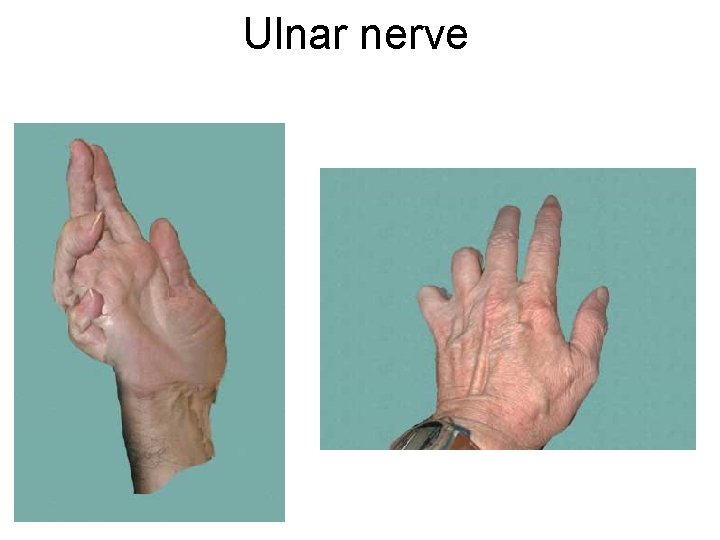
Ulnar nerve
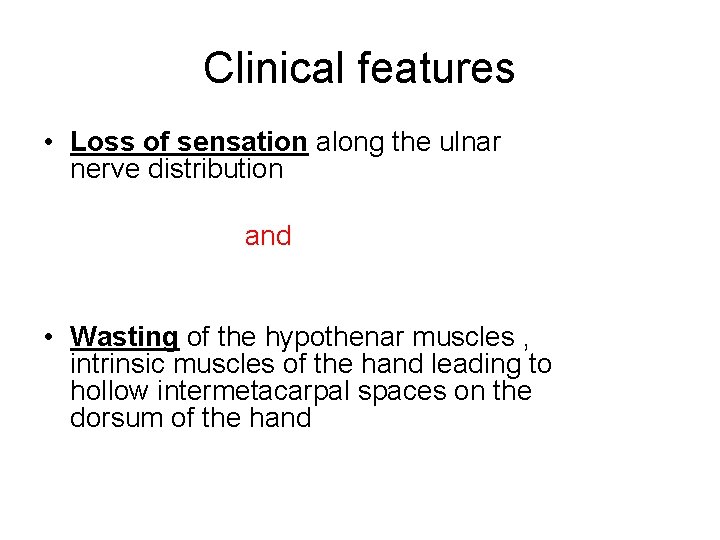
Clinical features • Loss of sensation along the ulnar nerve distribution and • Wasting of the hypothenar muscles , intrinsic muscles of the hand leading to hollow intermetacarpal spaces on the dorsum of the hand


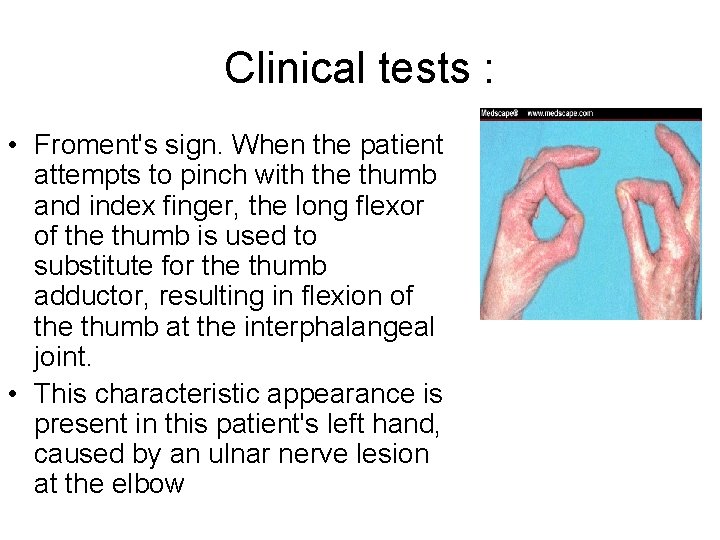
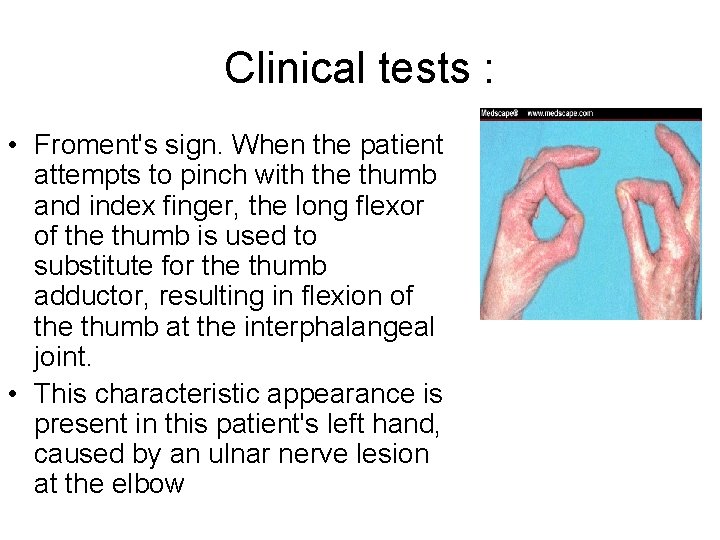
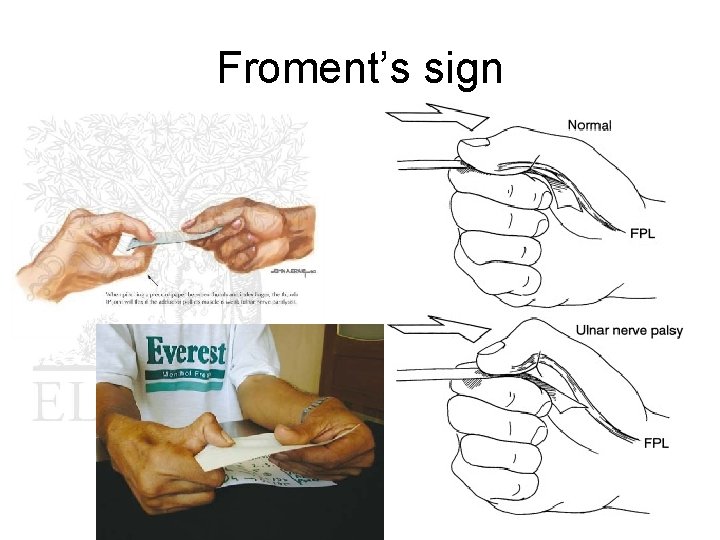
Clinical tests : • Froment's sign. When the patient attempts to pinch with the thumb and index finger, the long flexor of the thumb is used to substitute for the thumb adductor, resulting in flexion of the thumb at the interphalangeal joint. • This characteristic appearance is present in this patient's left hand, caused by an ulnar nerve lesion at the elbow
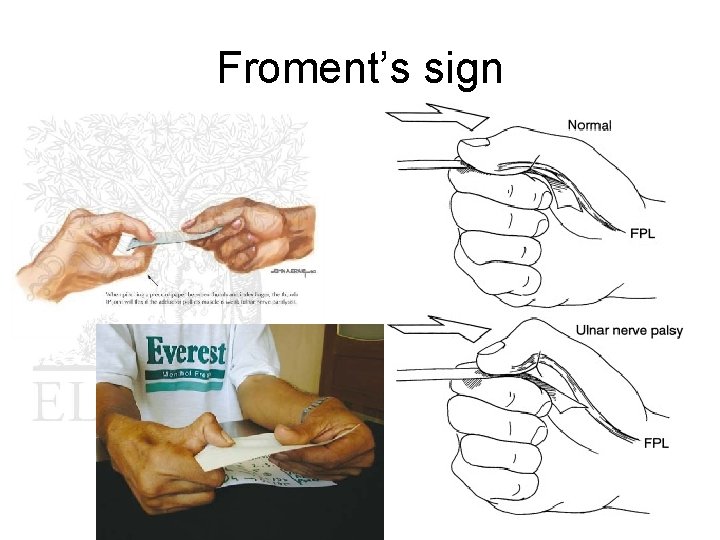
Froment’s sign
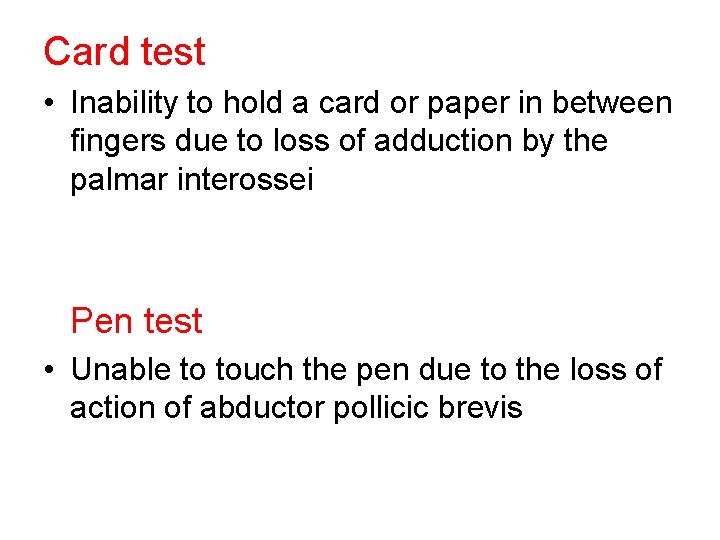
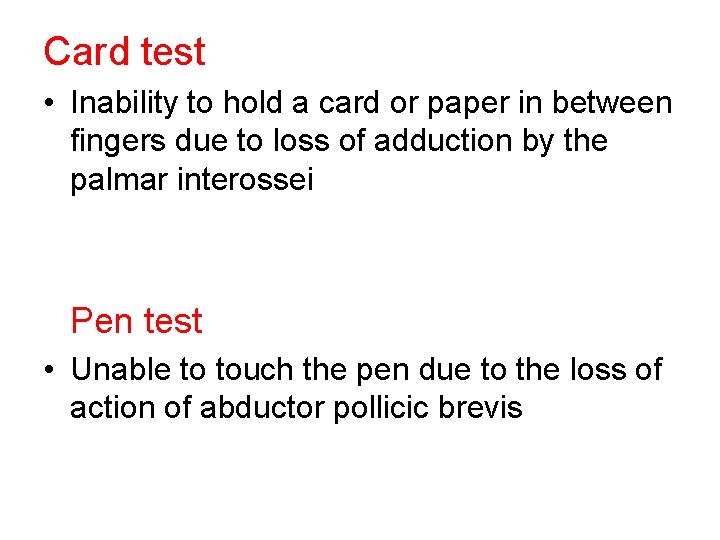
Card test • Inability to hold a card or paper in between fingers due to loss of adduction by the palmar interossei Pen test • Unable to touch the pen due to the loss of action of abductor pollicic brevis


Radial nerve injury Causes : General causes : metabolic diseases , collagen diseases , malignancies , endogenous or exogenous toxins , chemical or mechanical trauma , etc.
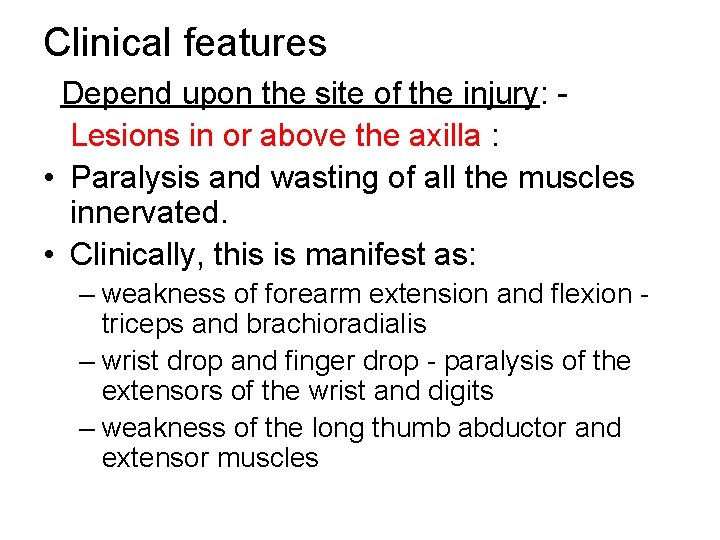
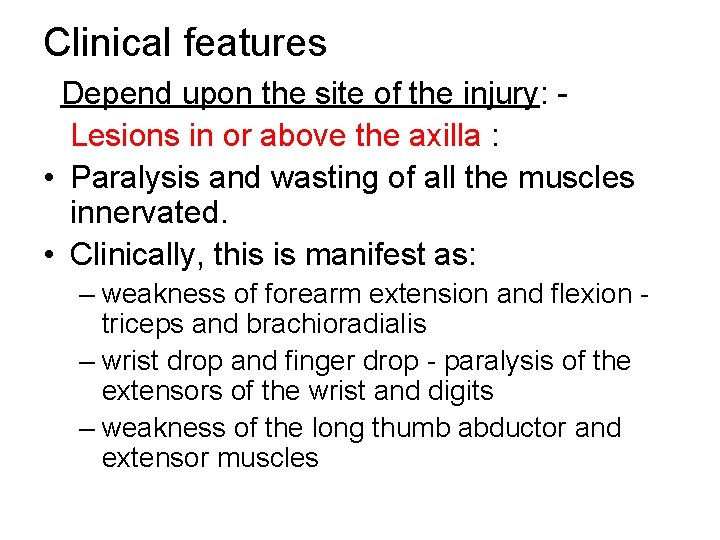
Clinical features Depend upon the site of the injury: Lesions in or above the axilla : • Paralysis and wasting of all the muscles innervated. • Clinically, this is manifest as: – weakness of forearm extension and flexion triceps and brachioradialis – wrist drop and finger drop - paralysis of the extensors of the wrist and digits – weakness of the long thumb abductor and extensor muscles
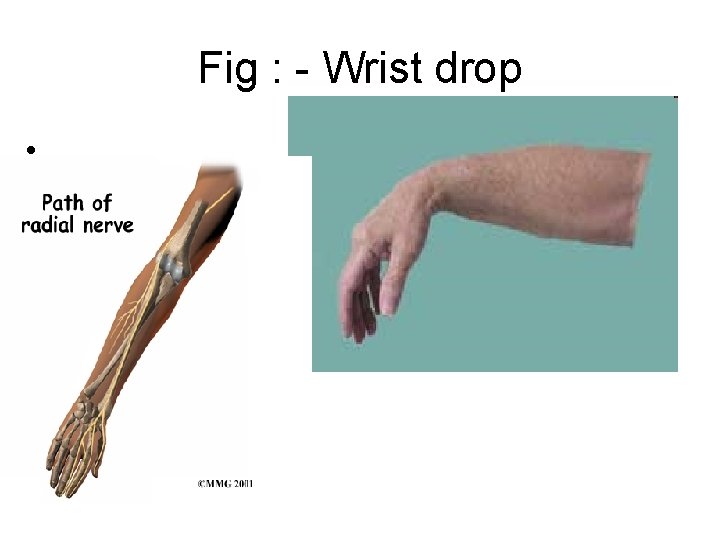
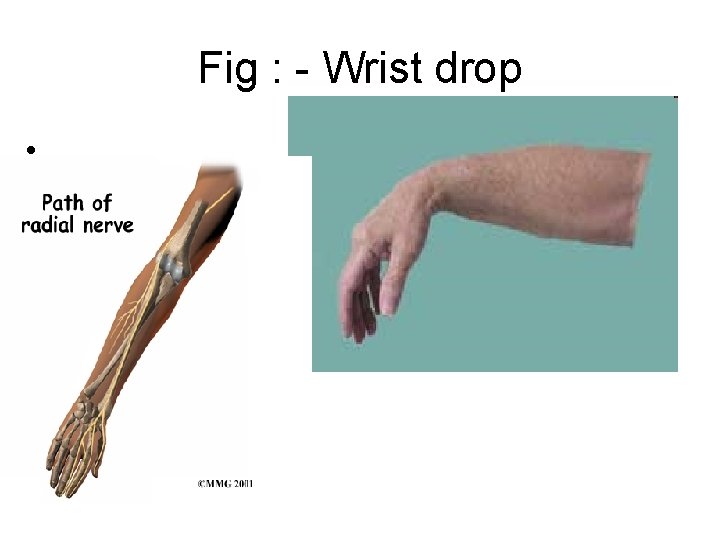
Fig : - Wrist drop • .
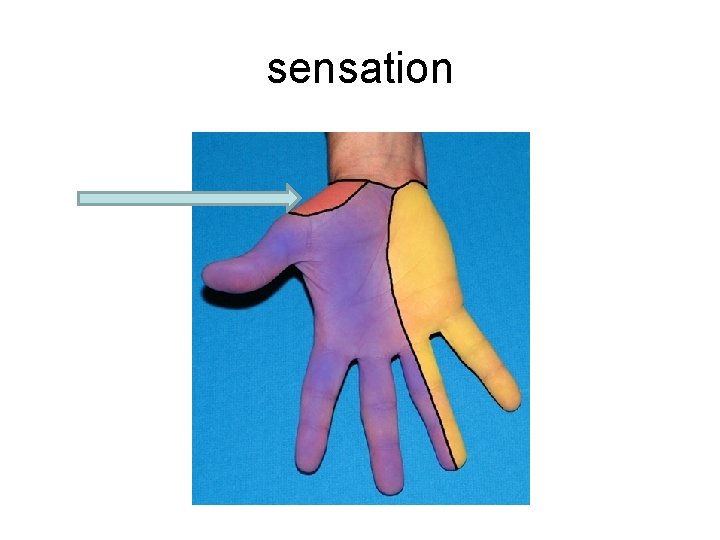
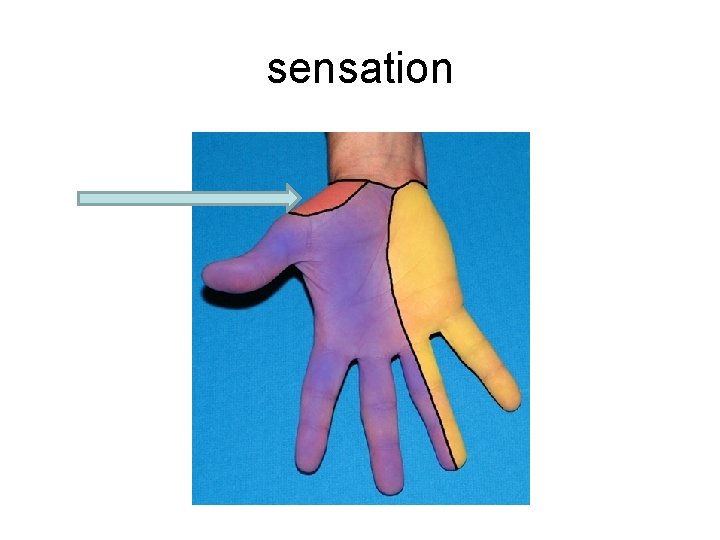
sensation
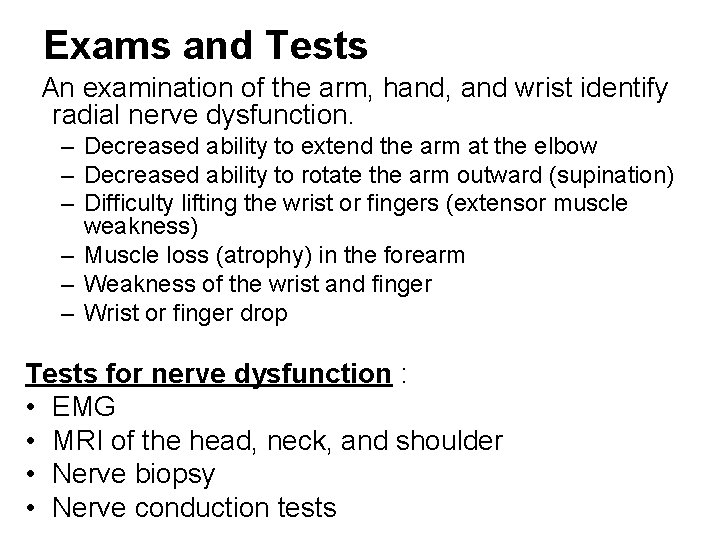
Exams and Tests An examination of the arm, hand, and wrist identify radial nerve dysfunction. – Decreased ability to extend the arm at the elbow – Decreased ability to rotate the arm outward (supination) – Difficulty lifting the wrist or fingers (extensor muscle weakness) – Muscle loss (atrophy) in the forearm – Weakness of the wrist and finger – Wrist or finger drop Tests for nerve dysfunction : • EMG • MRI of the head, neck, and shoulder • Nerve biopsy • Nerve conduction tests
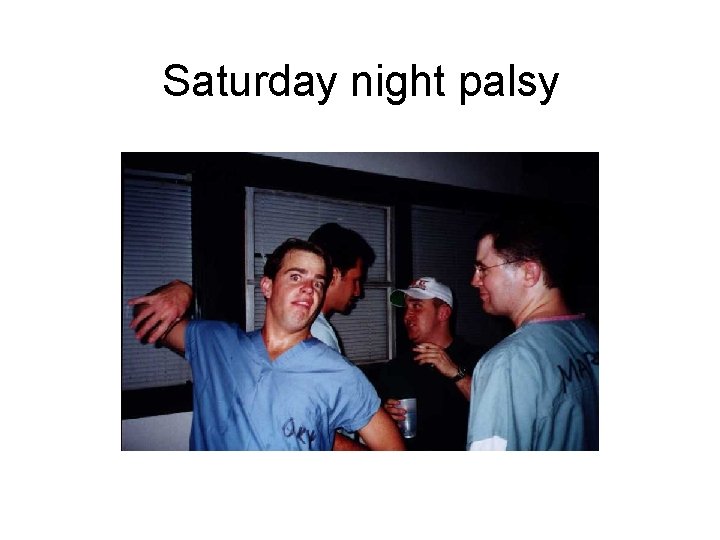
Saturday night palsy

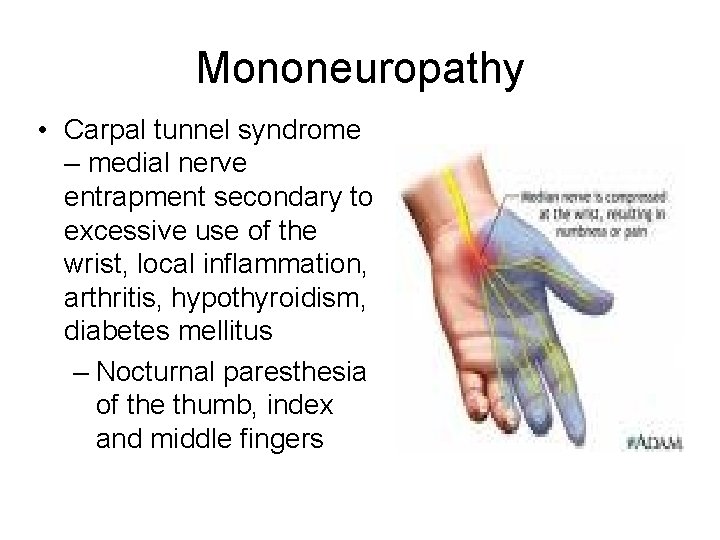
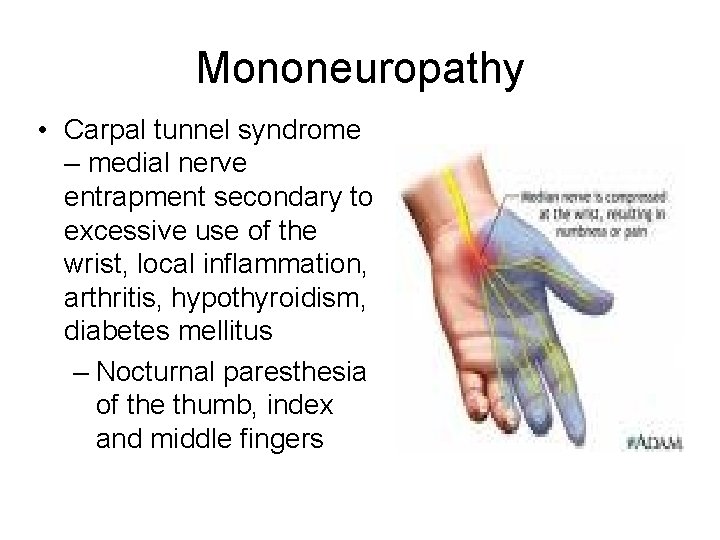
Mononeuropathy • Carpal tunnel syndrome – medial nerve entrapment secondary to excessive use of the wrist, local inflammation, arthritis, hypothyroidism, diabetes mellitus – Nocturnal paresthesia of the thumb, index and middle fingers
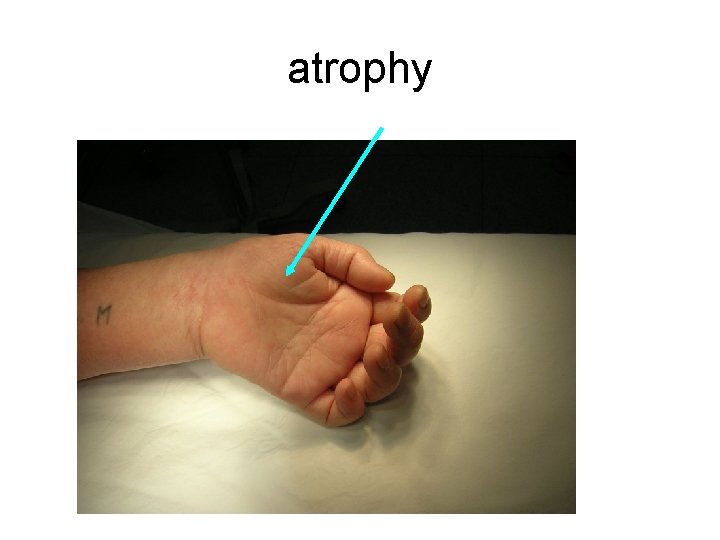
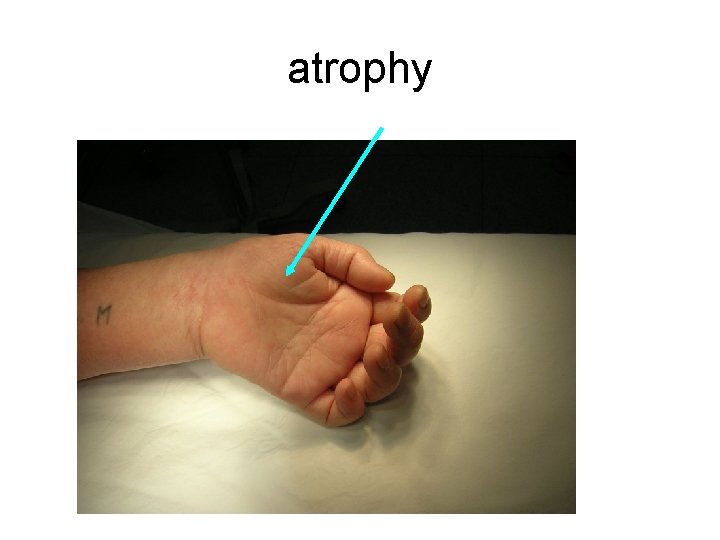
atrophy

Sciatic nerve injury • • Thickest nerve in the body Leprosy is the commonest cause High stepping gait is the characterisic Conservative treatment is indicated up to one year
Foot drop Causes • General causes : metabolic diseases , collagen diseases , malignancies , endogenous or exogenous toxins , chemical or mechanical trauma , etc. Local : At the spine : – Spina bifida – Tumors – Disc prolapse
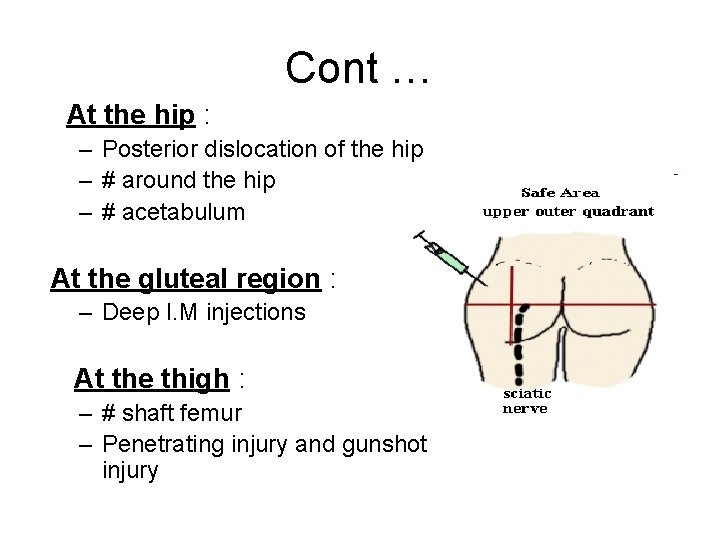
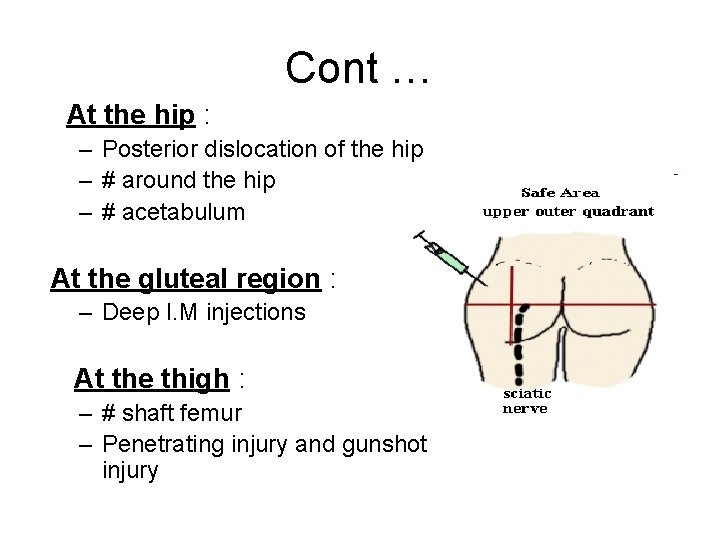
Cont … At the hip : – Posterior dislocation of the hip – # around the hip – # acetabulum At the gluteal region : – Deep I. M injections At the thigh : – # shaft femur – Penetrating injury and gunshot injury
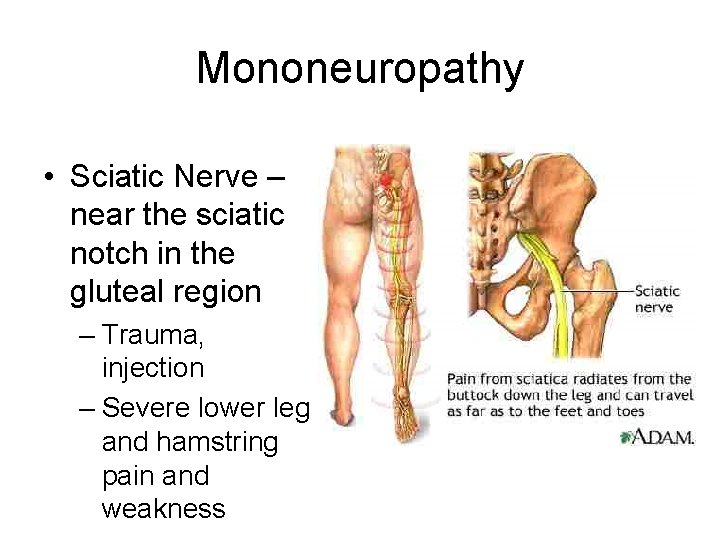
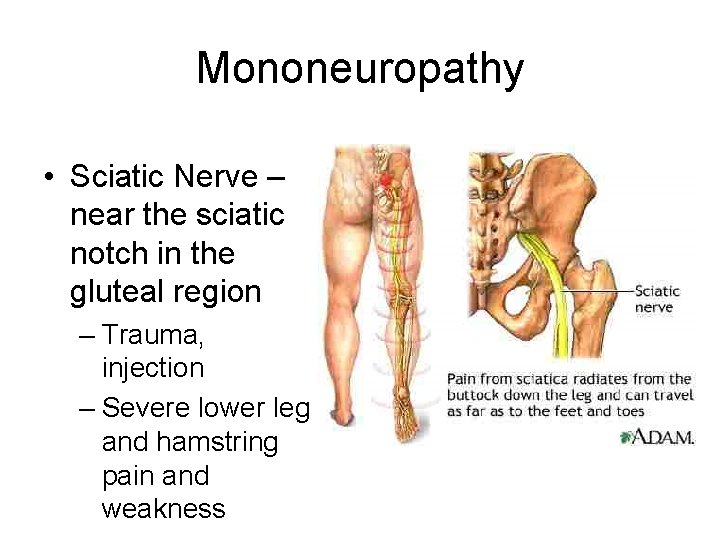
Mononeuropathy • Sciatic Nerve – near the sciatic notch in the gluteal region – Trauma, injection – Severe lower leg and hamstring pain and weakness
Cont … At the knee ( common causes ) – Forcible inversion of the knee – Dislocation of knee – # lateral condyle of tibia – Tight plaster casts around the knee – Surgical damage during application of skeletal traction – Gunshot injuries , incised and penetrating injuries
Clinical features Foot drop : Complete ( sciatic or lateral popliteal nerve injury ) Incomplete ( superficial or deep peroneal nerve ) – High lesions ------total foot drop – Low lesions ------ incomplete foot drop



Short Leg AFO with Fixed Hinge (doesn’t flex at ankle joint)
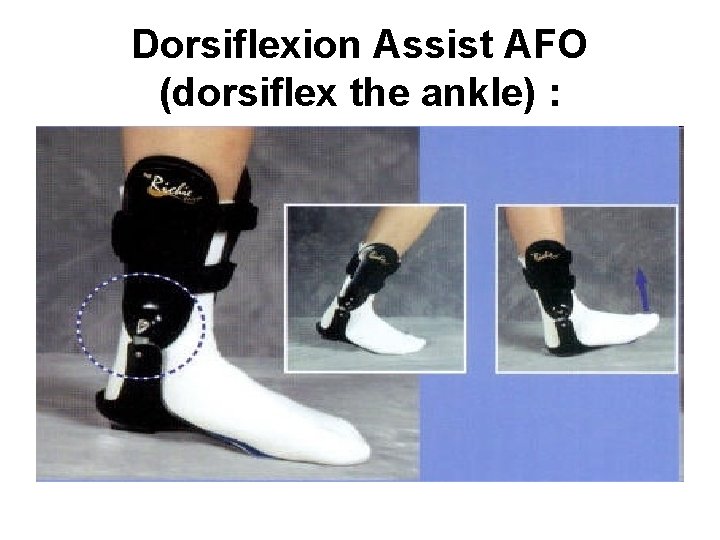
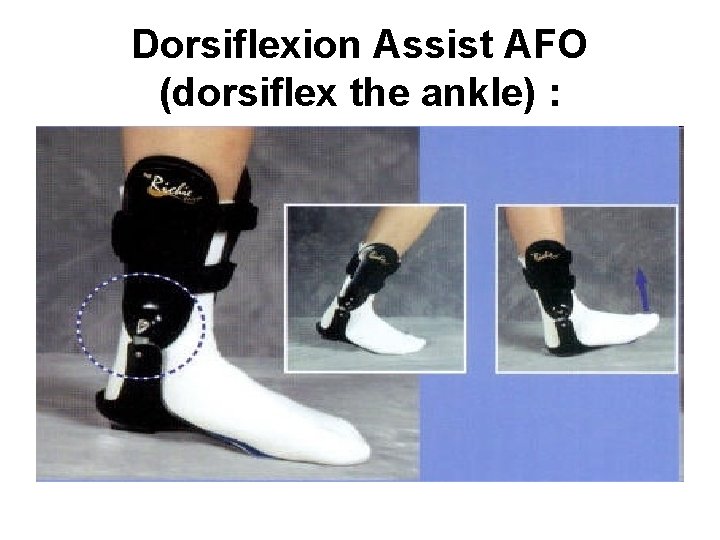
Dorsiflexion Assist AFO (dorsiflex the ankle) :

Plantarflexion Stop AFO:
Brachial plexus damage
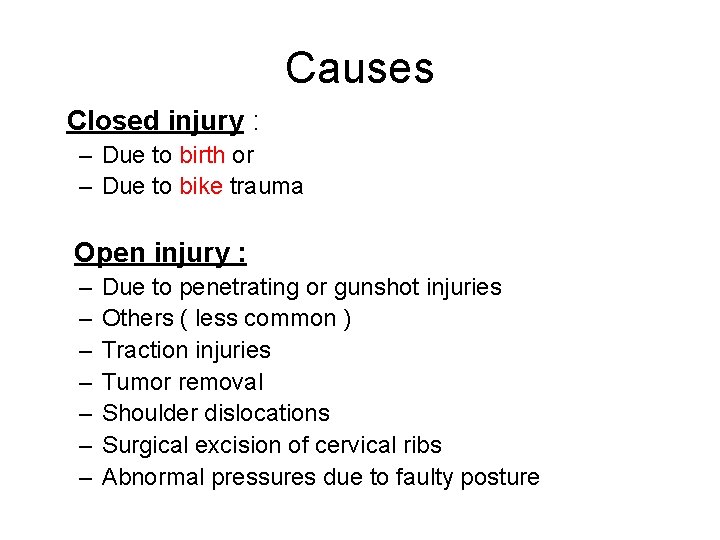
Causes Closed injury : – Due to birth or – Due to bike trauma Open injury : – – – – Due to penetrating or gunshot injuries Others ( less common ) Traction injuries Tumor removal Shoulder dislocations Surgical excision of cervical ribs Abnormal pressures due to faulty posture


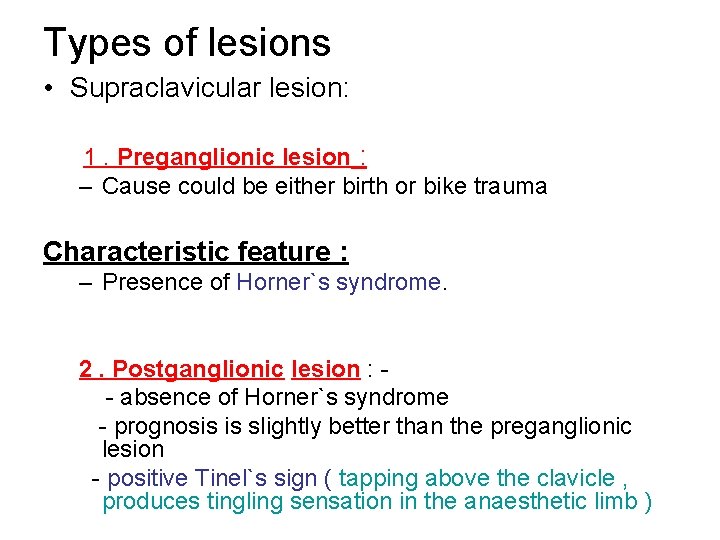
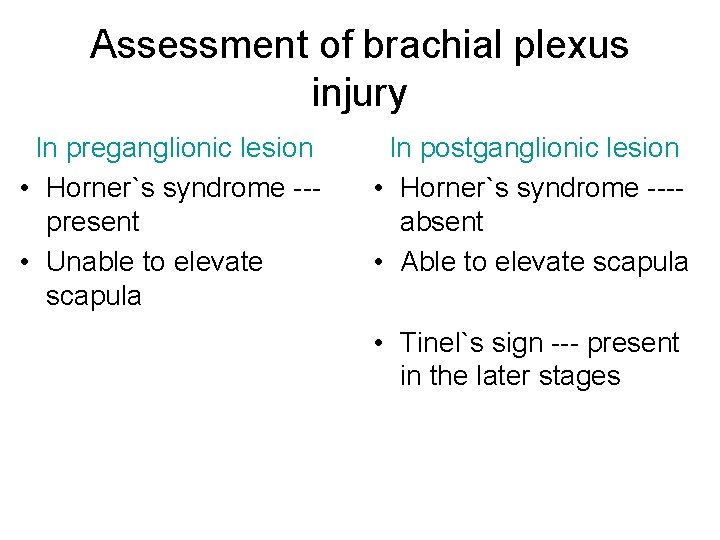
Types of lesions • Supraclavicular lesion: 1. Preganglionic lesion : – Cause could be either birth or bike trauma Characteristic feature : – Presence of Horner`s syndrome. 2. Postganglionic lesion : - absence of Horner`s syndrome - prognosis is slightly better than the preganglionic lesion - positive Tinel`s sign ( tapping above the clavicle , produces tingling sensation in the anaesthetic limb )
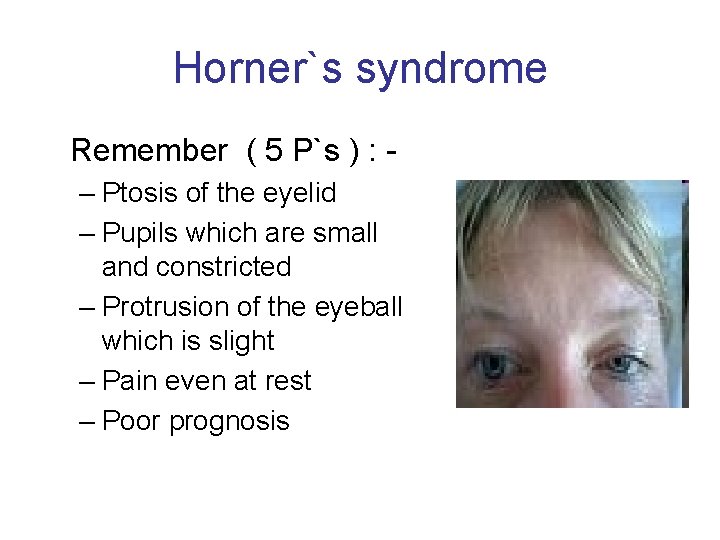
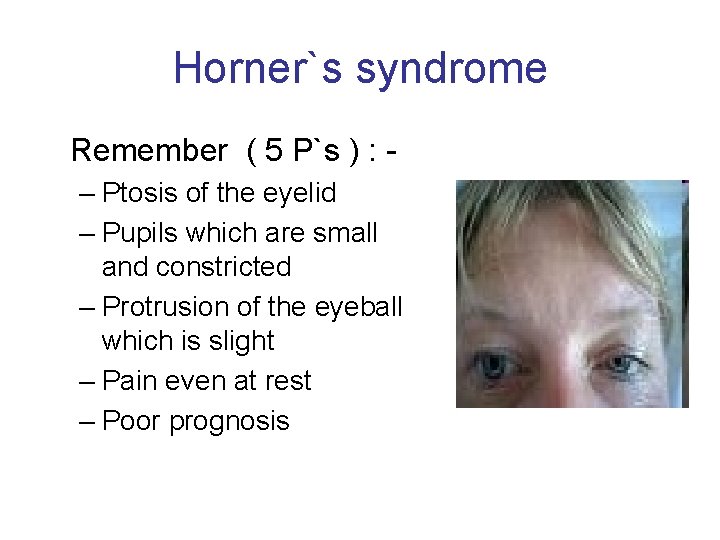
Horner`s syndrome Remember ( 5 P`s ) : – Ptosis of the eyelid – Pupils which are small and constricted – Protrusion of the eyeball which is slight – Pain even at rest – Poor prognosis
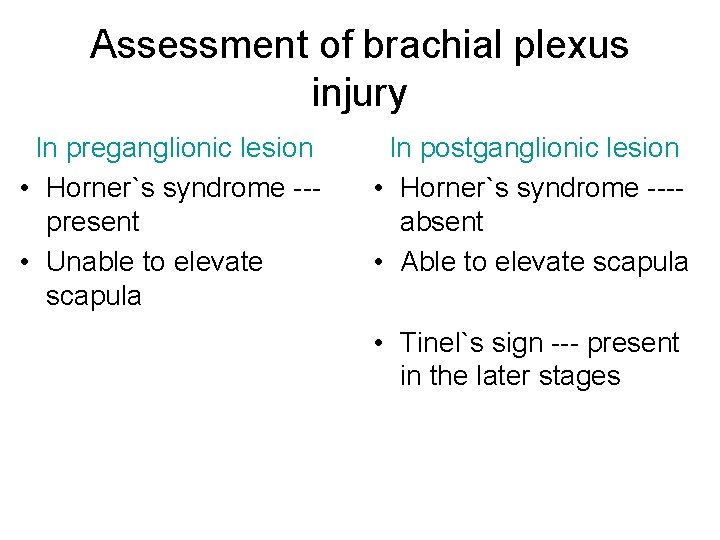
Assessment of brachial plexus injury In preganglionic lesion • Horner`s syndrome --present • Unable to elevate scapula In postganglionic lesion • Horner`s syndrome ---absent • Able to elevate scapula • Tinel`s sign --- present in the later stages
Investigation • X – ray ( to rule out # ) • CT scan ( study cross – section anatomy ) • MRI ( study the soft tissue damages ) • Electromyogram (EMG or electromyography) • Nerve conduction study
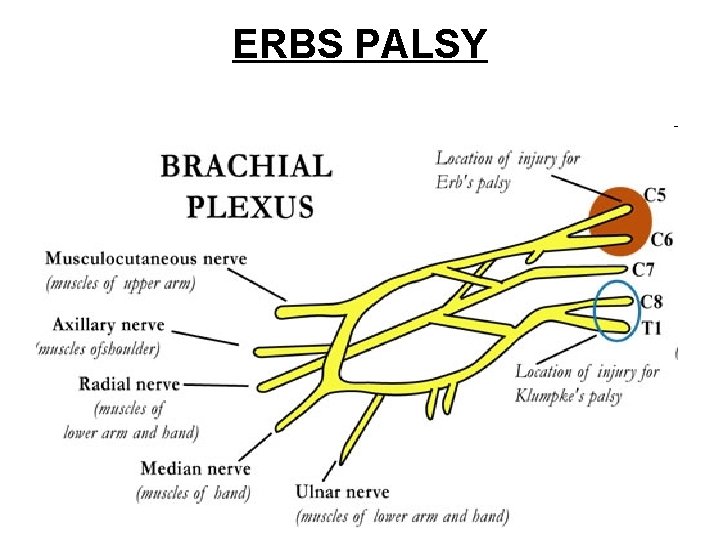
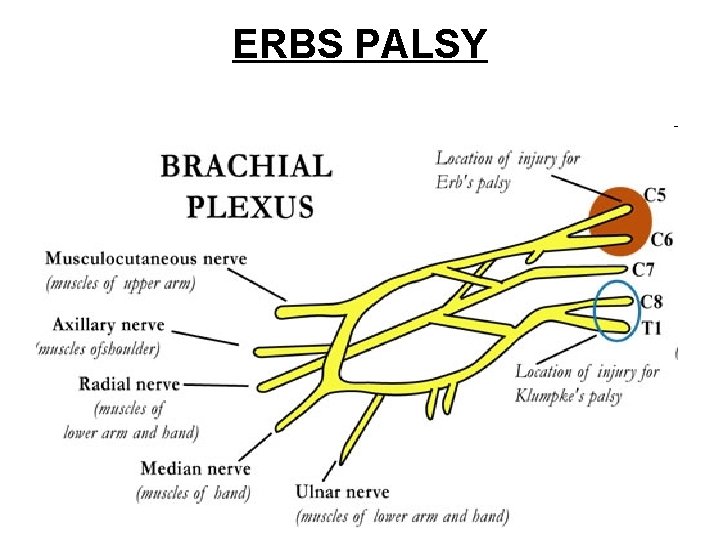
ERBS PALSY
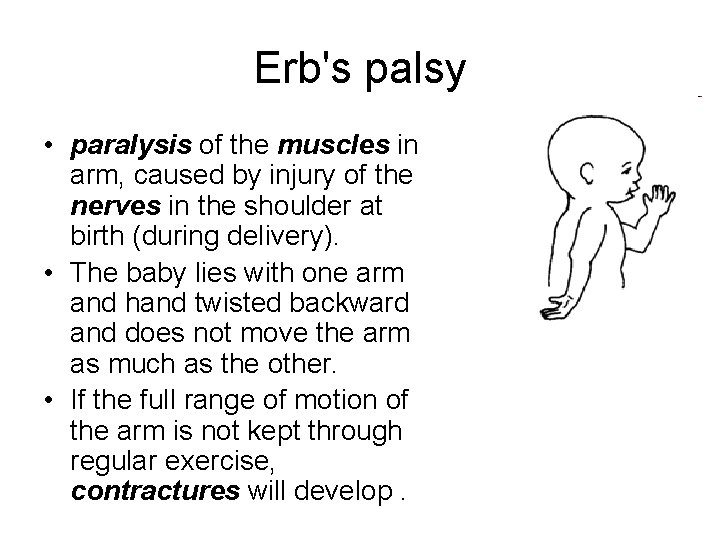
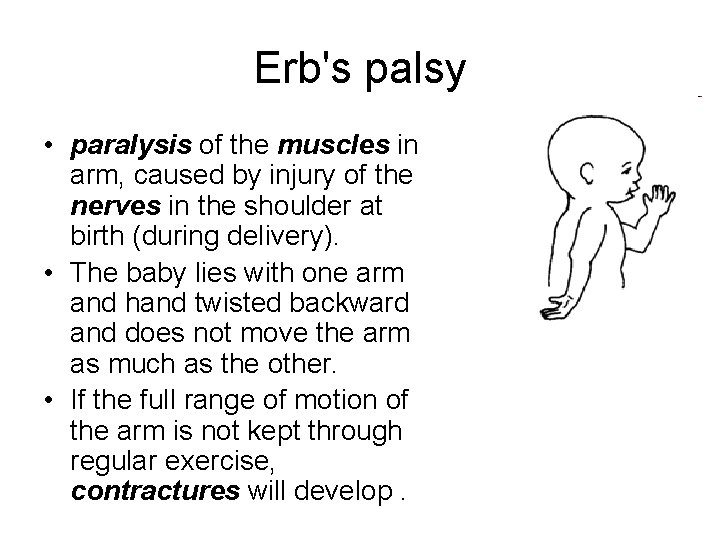
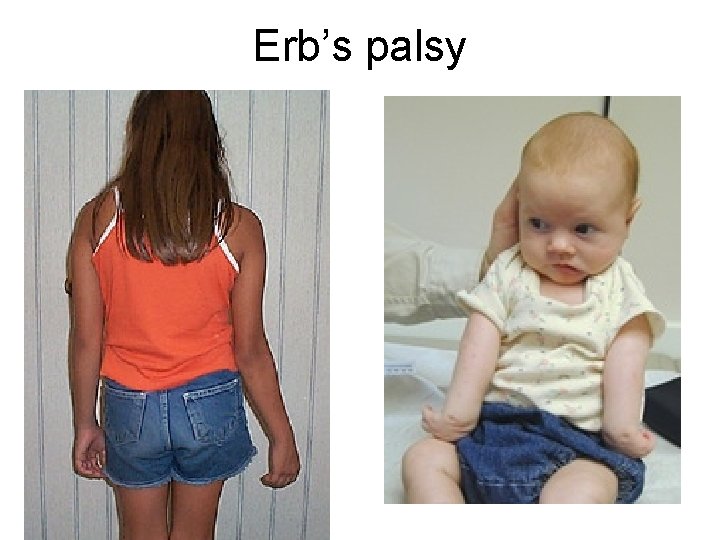
Erb's palsy • paralysis of the muscles in arm, caused by injury of the nerves in the shoulder at birth (during delivery). • The baby lies with one arm and hand twisted backward and does not move the arm as much as the other. • If the full range of motion of the arm is not kept through regular exercise, contractures will develop.
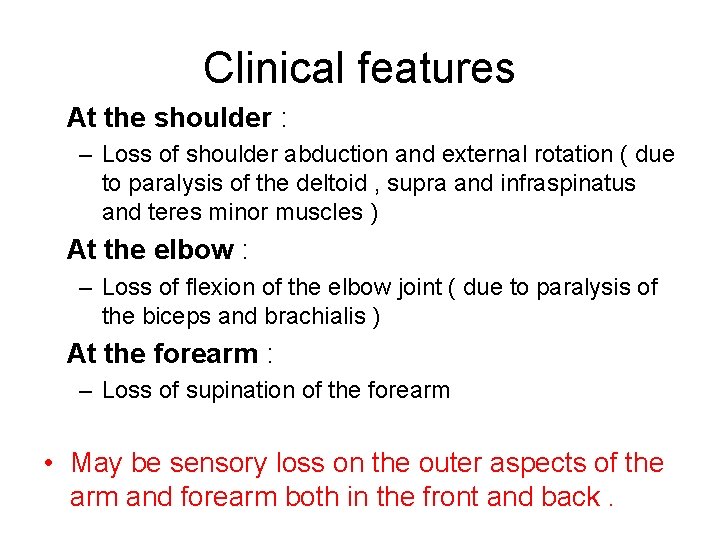
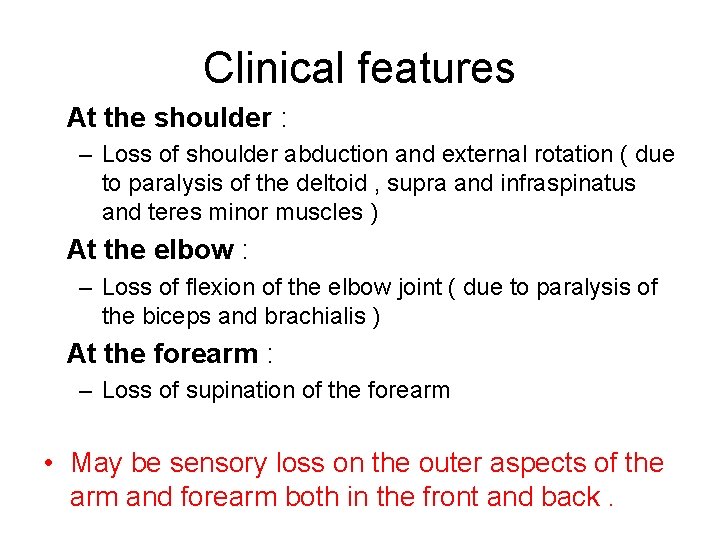
Clinical features At the shoulder : – Loss of shoulder abduction and external rotation ( due to paralysis of the deltoid , supra and infraspinatus and teres minor muscles ) At the elbow : – Loss of flexion of the elbow joint ( due to paralysis of the biceps and brachialis ) At the forearm : – Loss of supination of the forearm • May be sensory loss on the outer aspects of the arm and forearm both in the front and back.
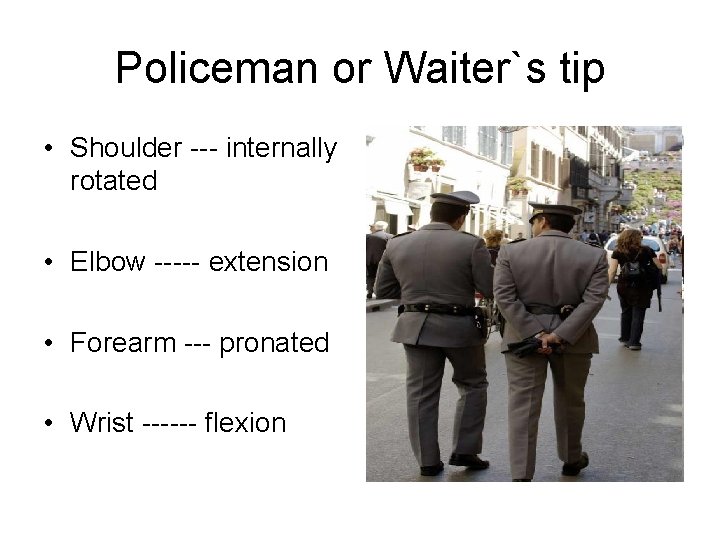
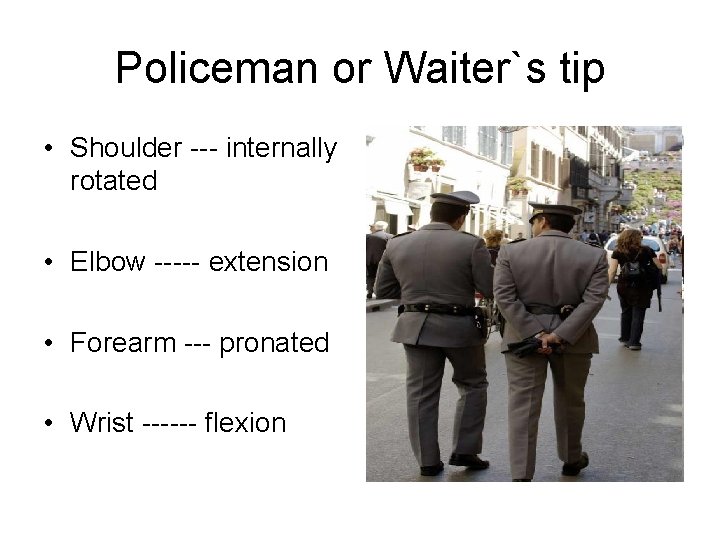
Policeman or Waiter`s tip • Shoulder --- internally rotated • Elbow ----- extension • Forearm --- pronated • Wrist ------ flexion
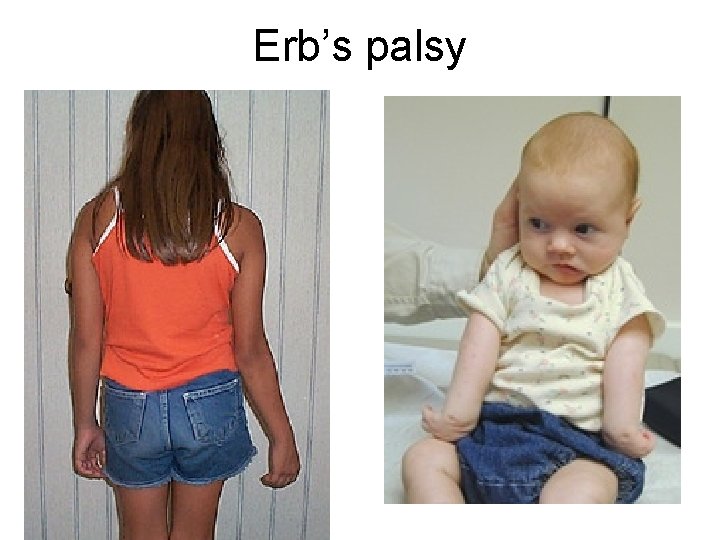
Erb’s palsy

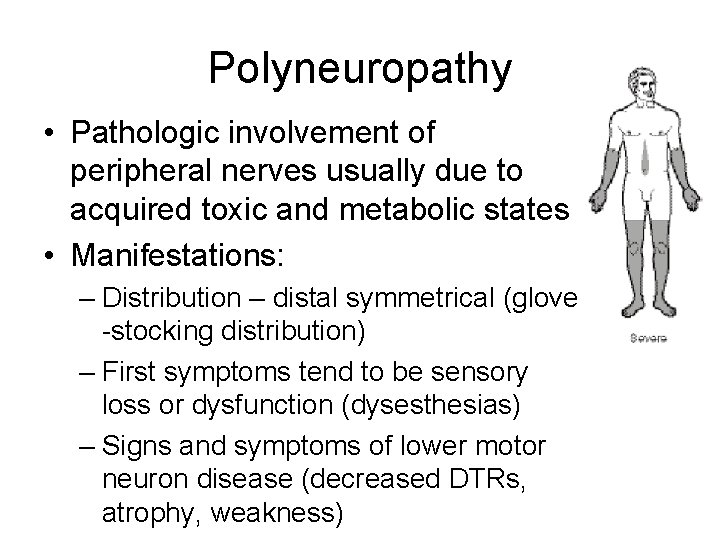
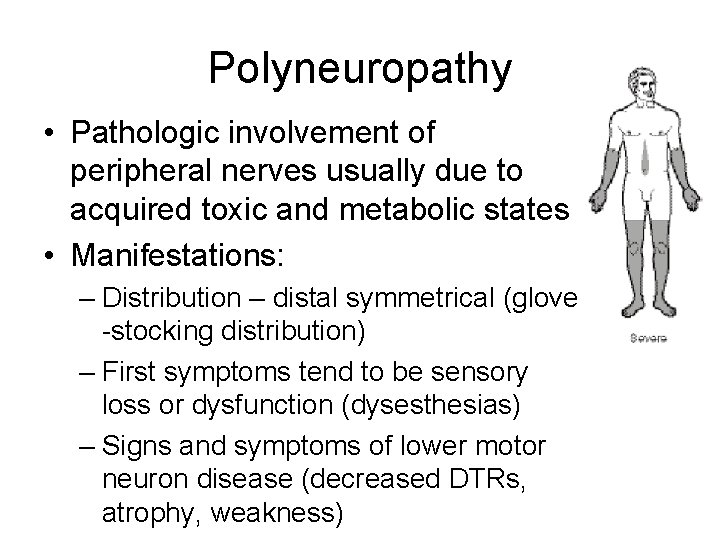
Polyneuropathy • Pathologic involvement of peripheral nerves usually due to acquired toxic and metabolic states • Manifestations: – Distribution – distal symmetrical (glove -stocking distribution) – First symptoms tend to be sensory loss or dysfunction (dysesthesias) – Signs and symptoms of lower motor neuron disease (decreased DTRs, atrophy, weakness)
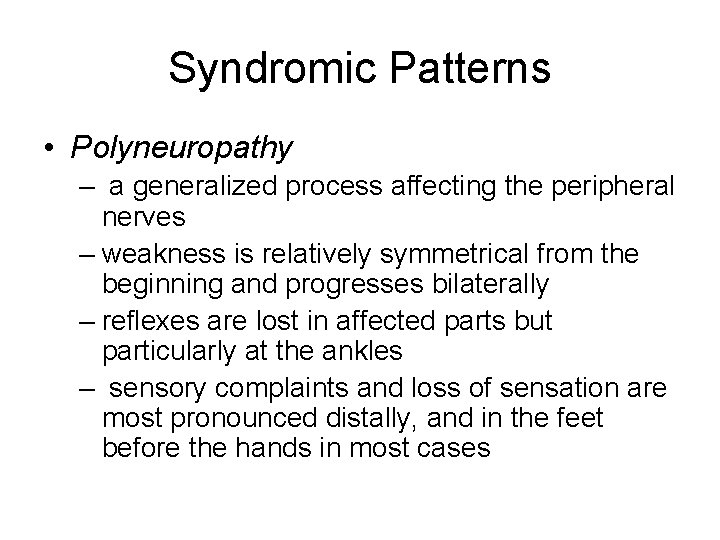
Syndromic Patterns • Polyneuropathy – a generalized process affecting the peripheral nerves – weakness is relatively symmetrical from the beginning and progresses bilaterally – reflexes are lost in affected parts but particularly at the ankles – sensory complaints and loss of sensation are most pronounced distally, and in the feet before the hands in most cases


Common Causes of Polyneuropathy • • Diabetes mellitus Uremia Vit. B deficiency Critical illness Hypothyroidism Carcinomas HIV alcohol
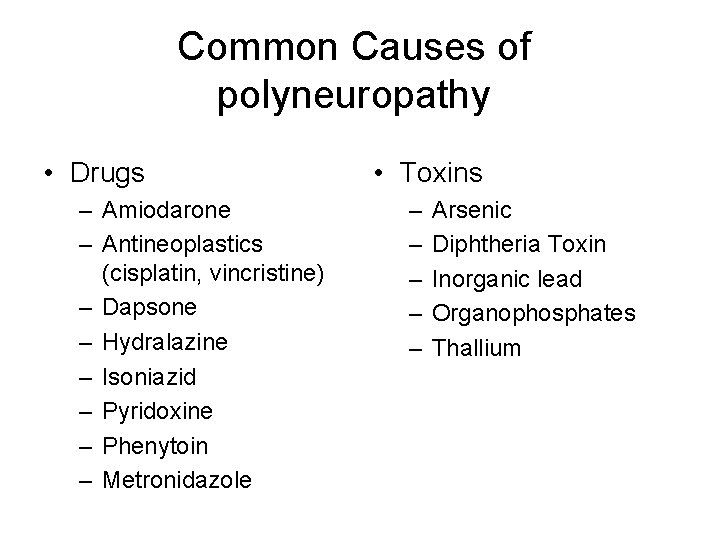
Common Causes of polyneuropathy • Drugs – Amiodarone – Antineoplastics (cisplatin, vincristine) – Dapsone – Hydralazine – Isoniazid – Pyridoxine – Phenytoin – Metronidazole • Toxins – – – Arsenic Diphtheria Toxin Inorganic lead Organophosphates Thallium


Guillain-Barre syndrome (ghee-YA-buh-RAY) • is a disorder in which your body's immune system attacks your nerves. • Weakness and tingling in your extremities are usually the first symptoms. • These sensations can quickly spread, eventually paralyzing your whole body.
• The exact cause of Guillain-Barre syndrome is unknown, but it is often preceded by an infectious illness such as a respiratory infection or the stomach flu. • Luckily, Guillain-Barre syndrome is uncommon, affecting only 1 -5 people per 100, 000.
Symptoms • begins with tingling and weakness starting in your feet and legs and spreading to your upper body and arms. • These symptoms may begin — often not causing much notice — in your fingers and toes. • As the disorder progresses, muscle weakness can evolve into paralysis.

Signs and symptoms of Guillain. Barre syndrome • Prickling, "pins and needles" sensations in your fingers, toes or both • Weakness or tingling sensations in your legs that spread to your upper body • Unsteady walking or inability to walk • Difficulty with eye movement, facial movement, speaking, chewing or swallowing • Severe pain in your lower back • Difficulty with bladder control or intestinal functions • Rapid heart rate • Low or high blood pressure • Difficulty breathing


Treatment • Plasmapheresis. rids plasma of certain antibodies that contribute to the immune system attack on the peripheral nerves. • Intravenous immunoglobulin. High doses of immunoglobulin can block the damaging antibodies that may contribute to Guillain-Barre syndrome. • These treatments are equally effective.
