Patient Safety Chapter 38 1212022 NRS 105 2011Collings





- Slides: 24
Patient Safety Chapter 38 1/21/2022 NRS 105 2011_Collings 1
JCAHO 2011 National Patient Safety Goals: Long term care § Identify residents correctly § Use at least two ways to identify residents. For example, use the resident’s name and date of birth. This is done to make sure that each resident gets the medicine and treatment meant for them § Use medicines safely § Take extra care with residents who take medicines to thin their blood. § Record and pass along correct information about a resident’s medicines. Find out what medicines the resident is taking. Compare those medicines to new medicines given to the resident. Make sure the resident knows which medicines to take when they are at home. Tell the resident it is important to bring their up-to-date list of medicines every time they visit a doctor. § Prevent infection § Use the hand cleaning guidelines from the Centers for Disease Control and Prevention or the World Health Organization. § Use proven guidelines to prevent infection of the blood from central lines. 1/21/2022 NRS 105 2011_Collings 2
JCAHO – LT Care 2010 § Prevent residents from falling § Find out which residents are most likely to fall. For example, is the resident taking any medicines that might make them weak, dizzy or sleepy? Take action to prevent falls for these residents. § Prevent bed sores § Find out which residents are most likely to have bed sores. Take action to prevent bed sores in these patients. From time to time, re-check residents for bed sores. § Check resident medicines § Find out what medicines each resident is taking. Make sure that it is OK for the resident to take any new medicines with their current medicines. § Give a list of the resident’s medicines to their next caregiver. Give the list to the resident’s regular doctor before the resident goes home. § Give a list of the resident’s medicines to the resident and their family before they go home. Explain the list. (2011, http: //www. jointcommission. org/assets/1/6/LTC_NPSG_6 -10 -11. pdf) 1/21/2022 NRS 105 2011_Collings 3
Environmental Safety § A safe environment includes meeting basic needs, reducing physical hazards, reducing the transmission of pathogens, maintaining sanitation, and controlling pollution. § A safe environment also includes one where threat of attack from biological, chemical, or nuclear weapons is prevented or minimized. 1/21/2022 NRS 105 2011_Collings 4
Basic Needs § Oxygen § Nutrition § Temperature and Humidity 1/21/2022 NRS 105 2011_Collings 5
Physical Hazards § Lighting § Obstacles § Bathroom Hazards § Security 1/21/2022 NRS 105 2011_Collings 6
Environment Safety § Transmission of Pathogens § Pollution § Air pollution § Water pollution § Noise pollution § Terrorism § Bioterrorism 1/21/2022 NRS 105 2011_Collings 7

Risks at Developmental Stages § Infant, Toddler, Preschool § School aged child § Adolescent § Adult § Older Adult 1/21/2022 NRS 105 2011_Collings 8
Individual Risk Factors § Lifestyle § Impaired Mobility § Sensory or communication Impairment § Lack of Safety Awareness 1/21/2022 NRS 105 2011_Collings 9
Risks in the Health Care Agency § Falls § Patient-Inherent Accidents § Procedure-related Accidents § Equipment-related Accidents § Medication errors 1/21/2022 NRS 105 2011_Collings 10
Nursing Diagnosis § Risk for injury § Related to: § General weakness § Right or Left sided weakness § Side effects of medication § Poor eyesight § As evidenced by: § Recent falls § New CVA § Confusion § Macular degeneration 1/21/2022 NRS 105 2011_Collings 11
Implementation § Risk for injury related to (r/t) generalized weakness as evidenced by recent falls § Pt. will ask for help to the bathroom each time this shift § Call light will be in reach at all times § Pt will not fall this shift § Work with other care providers to make sure patient is seen q hour § Document on rounding sheet 1/21/2022 NRS 105 2011_Collings 12
Use of Restraints in the Health Care Setting § Physical or chemical means of stopping a patient from being free to move. § Used only in emergency situations to ensure the patient’s safety. § Restraint orders must be specific and timelimited. 1/21/2022 NRS 105 2011_Collings 13
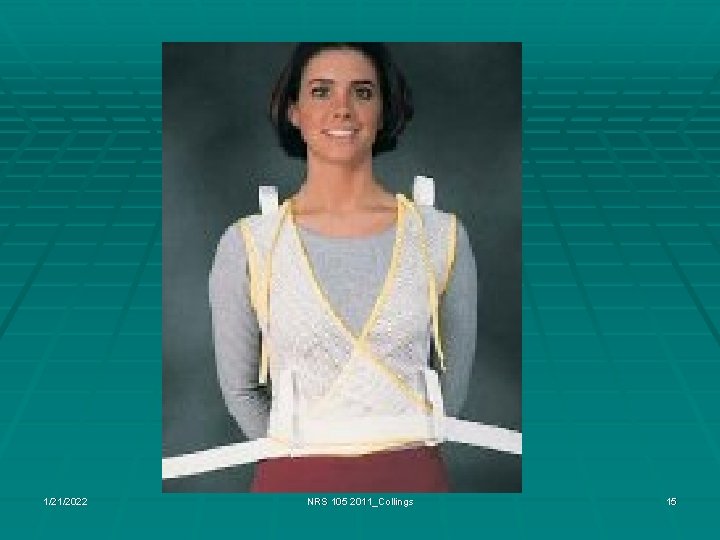
Restraints & Alternatives § Bed rails may be considered restraints § Usually OK to have 2 up § 4 up considered a restraint § Contributes to more frequent, severe injury § Alternatives to restraints – § § 1/21/2022 Check on pt. at least hourly Place close to nurse’s station Control environment, re-orient pt frequently Provide call light, personal needs, access to BR NRS 105 2011_Collings 14
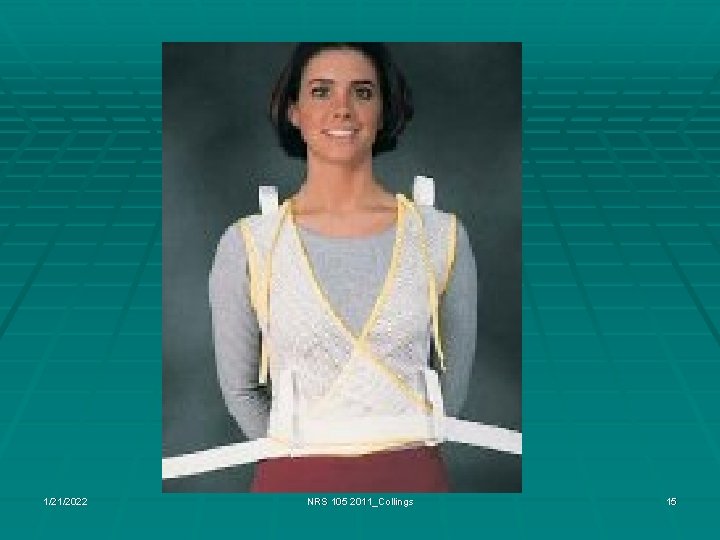
1/21/2022 NRS 105 2011_Collings 15

1/21/2022 NRS 105 2011_Collings 16
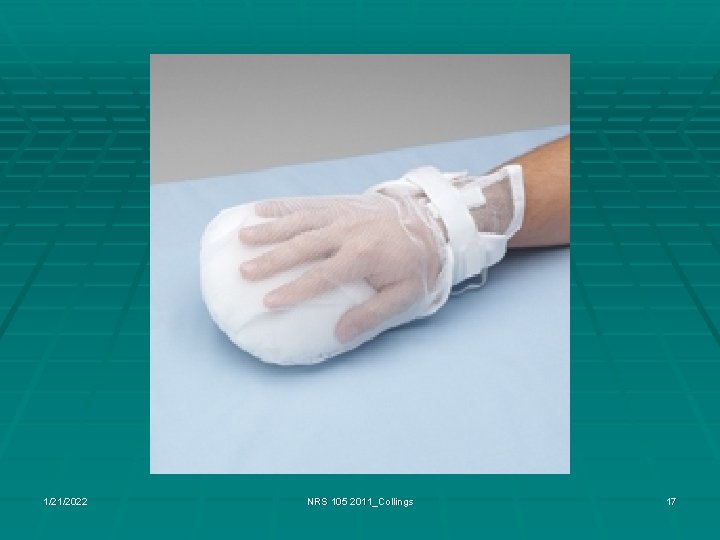
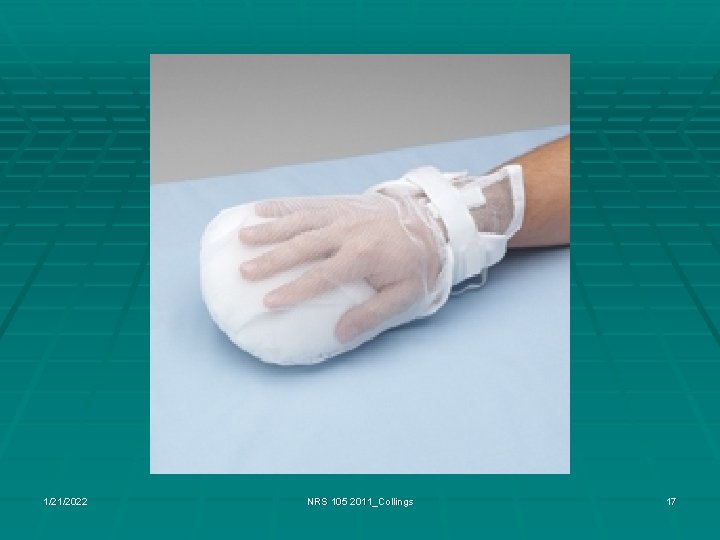
1/21/2022 NRS 105 2011_Collings 17

1/21/2022 NRS 105 2011_Collings 18
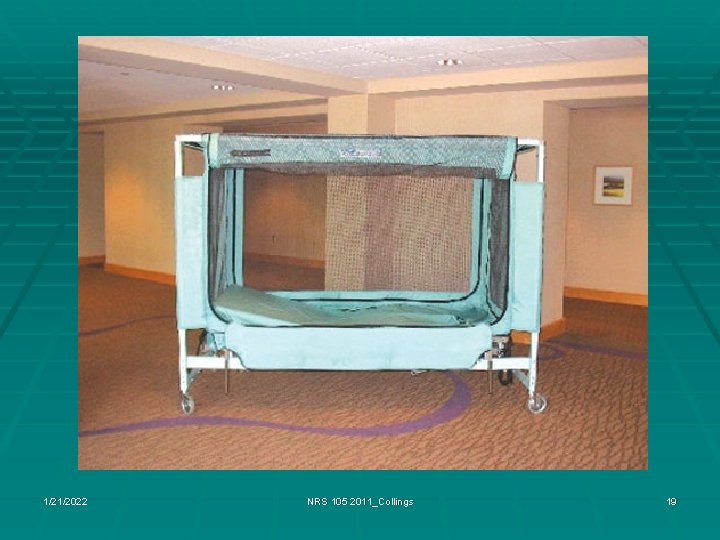
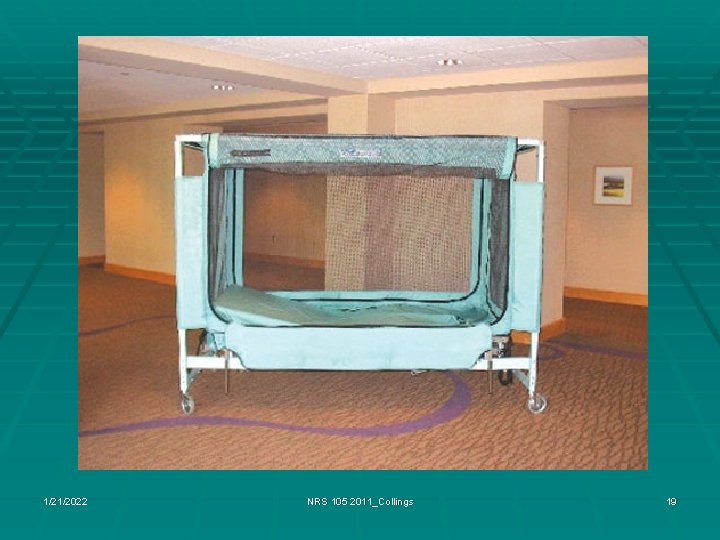
1/21/2022 NRS 105 2011_Collings 19

1/21/2022 NRS 105 2011_Collings 20
Other Mechanisms to Prevent Falls § Tab Alarms § Arm Bands § ID outside of Patient room § Notice Inside the Patient room § Colors of gowns, slippers, blankets § Bed Alarms § Chair Alarms 1/21/2022 NRS 105 2011_Collings 21
Restraint Use § Must have a physician order § May apply in emergency, then get order § Order must be rewritten every 24 h. § No automatic renewal, verbal order § Restraint policies are specific to health care setting § Nursing documentation must occur at least every two hours § Including need for continued restraint use, skin assessment 1/21/2022 NRS 105 2011_Collings 22

Complications from Restraints § Skin breakdown § Constipation § Pneumonia § Incontinence § Urinary retention § Nerve damage § Circulatory damage 1/21/2022 NRS 105 2011_Collings 23
Questions? Discussion? 1/21/2022 NRS 105 2011_Collings 24
 A nurse floats to a busy surgical unit
A nurse floats to a busy surgical unit Chapter 20 patient environment and safety
Chapter 20 patient environment and safety Patient 2 patient
Patient 2 patient Nrs украина
Nrs украина Poker chip tool pain scale
Poker chip tool pain scale Nrs 453
Nrs 453 Levels of critical thinking in nursing
Levels of critical thinking in nursing Nrs 439
Nrs 439 Keylozis nedir tıp
Keylozis nedir tıp Nrs kipumittari
Nrs kipumittari Nrs 240
Nrs 240 Nrs 122
Nrs 122 Nrs 101
Nrs 101 Nrs 2002 başlangıç taraması
Nrs 2002 başlangıç taraması Enteral beslenme ürünlerinin veriliş şekilleri
Enteral beslenme ürünlerinin veriliş şekilleri Ifta audit fines
Ifta audit fines Nrs 453
Nrs 453 Nrs 2030
Nrs 2030 Painad meetinstrument
Painad meetinstrument Dyspnoe de repos
Dyspnoe de repos Nrs
Nrs Rskl § 1-6
Rskl § 1-6 Nrs skala
Nrs skala Nevada gaming registration
Nevada gaming registration Nrs 639
Nrs 639