Oxygenation Chapter 40 682021 NRS 105 320 S
![SPECIAL OXYGEN CONSIDERATIONS ACROSS THE LIFE SPAN • INFANTS AND TODDLERS – SURFACTANT [newborn] SPECIAL OXYGEN CONSIDERATIONS ACROSS THE LIFE SPAN • INFANTS AND TODDLERS – SURFACTANT [newborn]](https://slidetodoc.com/presentation_image_h2/6160a57b52d18ce195e5b2c5307649a0/image-13.jpg)

![Case study #2 • 72 yo female Denver resident c/o SOB [dyspnea], dizziness and Case study #2 • 72 yo female Denver resident c/o SOB [dyspnea], dizziness and](https://slidetodoc.com/presentation_image_h2/6160a57b52d18ce195e5b2c5307649a0/image-26.jpg)
![Interventions • • Focus on: treating underlying cause [abx, O 2] adaptation [meds, breathing Interventions • • Focus on: treating underlying cause [abx, O 2] adaptation [meds, breathing](https://slidetodoc.com/presentation_image_h2/6160a57b52d18ce195e5b2c5307649a0/image-28.jpg)










![Evaluation • Ask pt. to demonstrate techniques [cough, breathing] • Assess dyspnea, cough, sputum, Evaluation • Ask pt. to demonstrate techniques [cough, breathing] • Assess dyspnea, cough, sputum,](https://slidetodoc.com/presentation_image_h2/6160a57b52d18ce195e5b2c5307649a0/image-89.jpg)
- Slides: 90
Oxygenation Chapter 40
6/8/2021 NRS 105. 320 S 2009 2
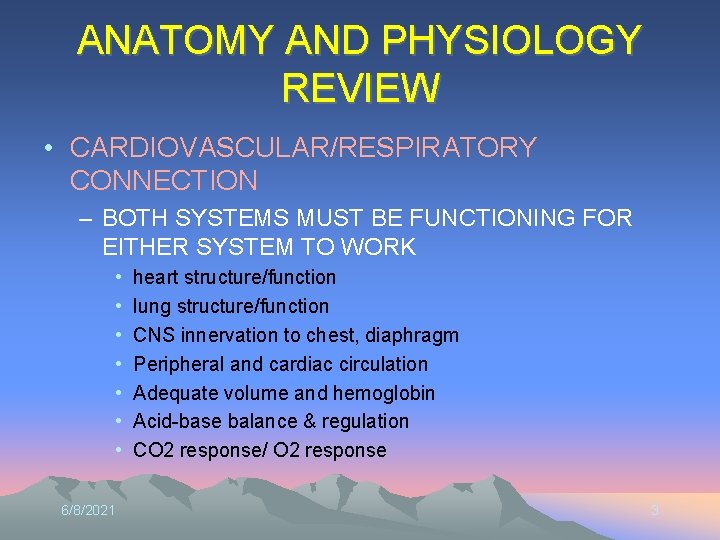
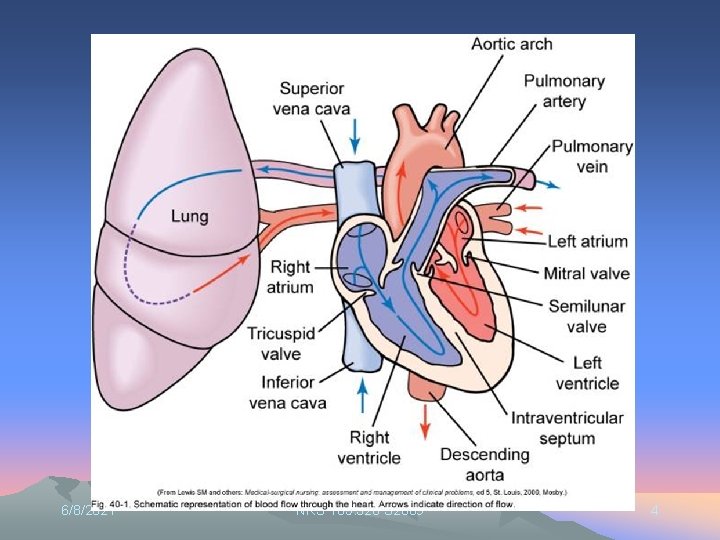
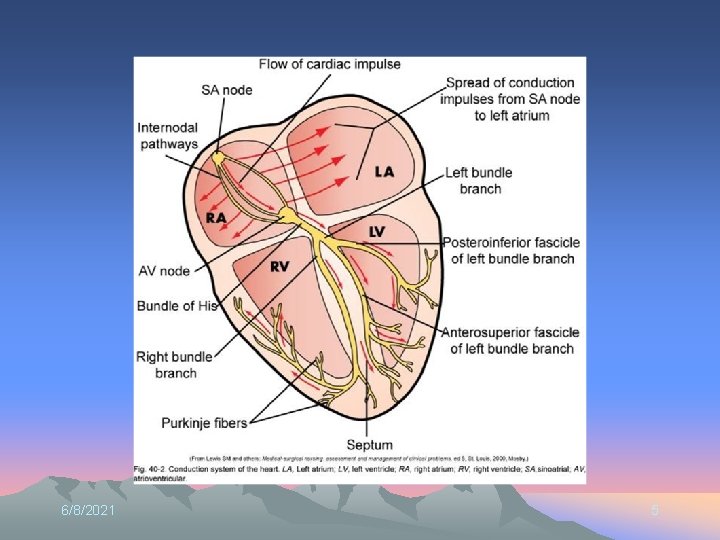
ANATOMY AND PHYSIOLOGY REVIEW • CARDIOVASCULAR/RESPIRATORY CONNECTION – BOTH SYSTEMS MUST BE FUNCTIONING FOR EITHER SYSTEM TO WORK • • 6/8/2021 heart structure/function lung structure/function CNS innervation to chest, diaphragm Peripheral and cardiac circulation Adequate volume and hemoglobin Acid-base balance & regulation CO 2 response/ O 2 response 3
6/8/2021 NRS 105. 320 S 2009 4
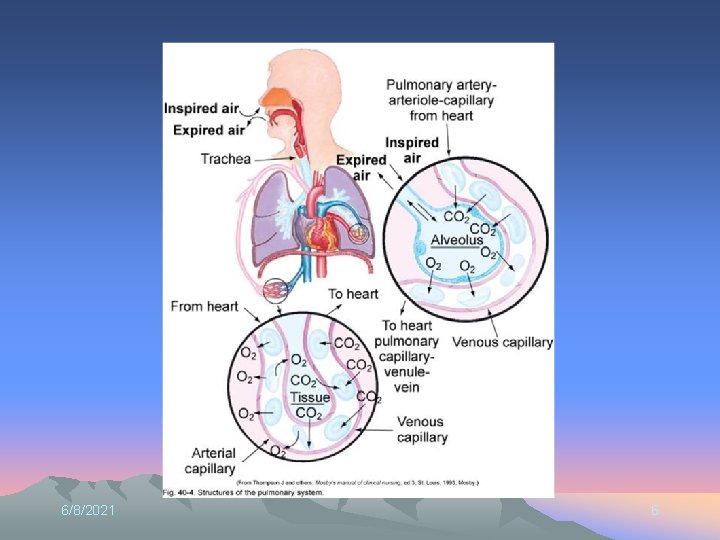
6/8/2021 5
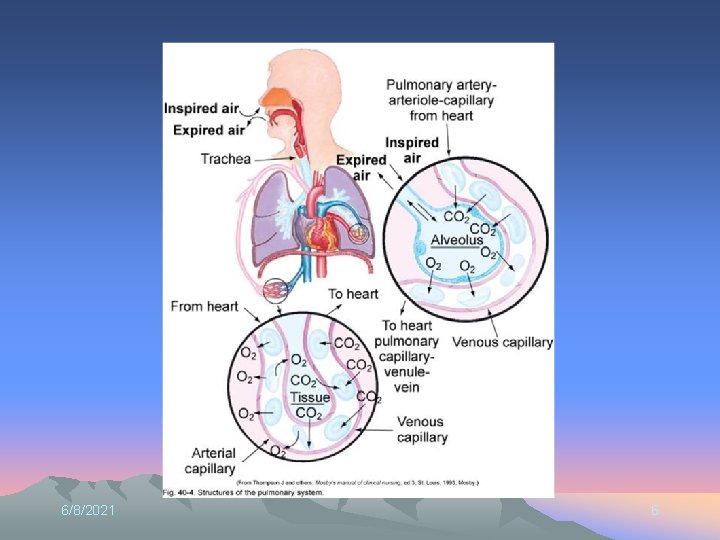
6/8/2021 6
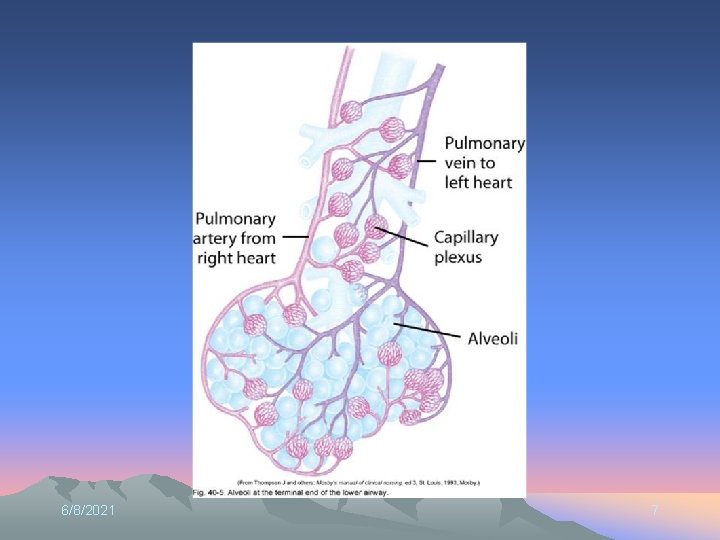
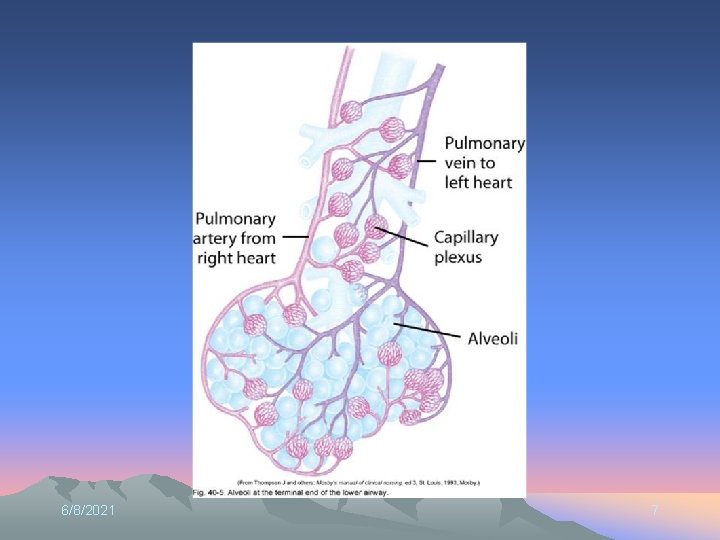
6/8/2021 7
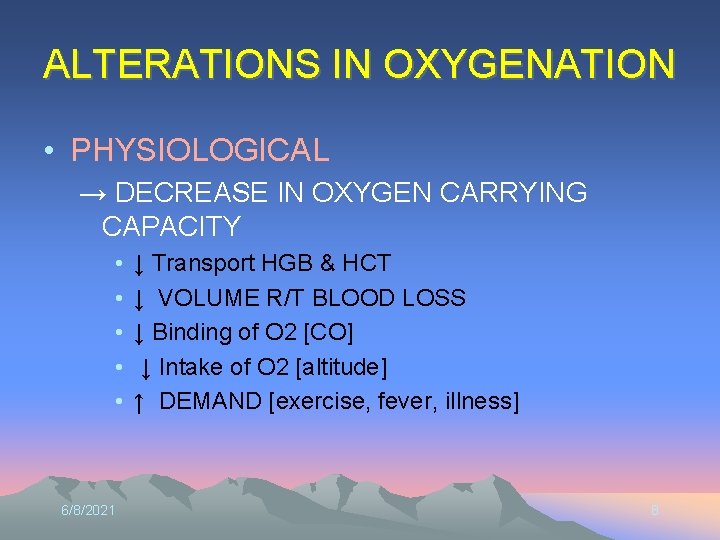
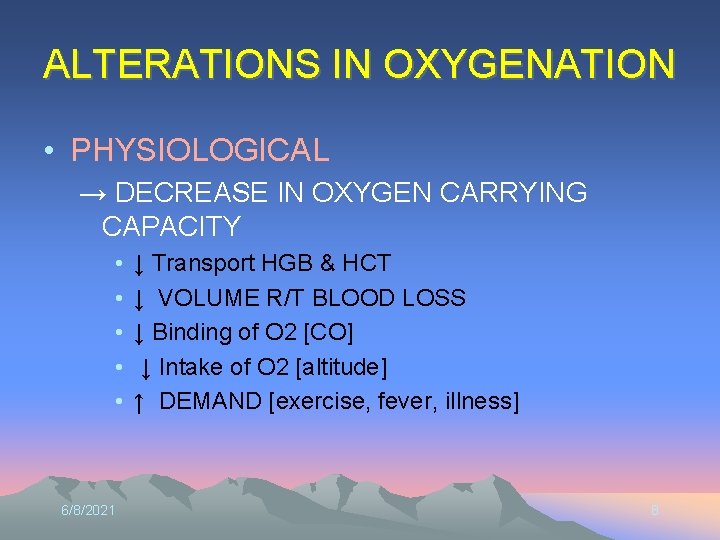
ALTERATIONS IN OXYGENATION • PHYSIOLOGICAL → DECREASE IN OXYGEN CARRYING CAPACITY • • • 6/8/2021 ↓ Transport HGB & HCT ↓ VOLUME R/T BLOOD LOSS ↓ Binding of O 2 [CO] ↓ Intake of O 2 [altitude] ↑ DEMAND [exercise, fever, illness] 8
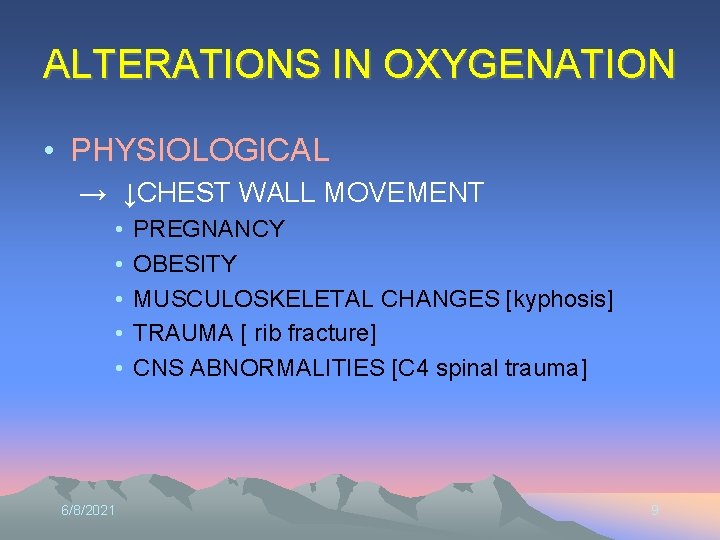
ALTERATIONS IN OXYGENATION • PHYSIOLOGICAL → ↓CHEST WALL MOVEMENT • • • 6/8/2021 PREGNANCY OBESITY MUSCULOSKELETAL CHANGES [kyphosis] TRAUMA [ rib fracture] CNS ABNORMALITIES [C 4 spinal trauma] 9
ALTERATIONS IN OXYGENATION • Physiological→ Changes in Delivery of O 2 – Diffusion in lungs [alveolar] • atelectasis, ↓surface area, ↓blood supply, pressure • Secretions [pneumonia, COPD] – Transport to tissues • Cardiac output • circulation [PVD, trauma, volume, vasoconstriction] • Cardiac perfusion
ALTERATIONS IN OXYGENATION • PHYSIOLOGICAL – CHRONIC DISEASES • COPD: CO 2 drive absent R/T chronic high p. CO 2 – Dependent on pa. O 2 drive; ↓compliance, atelectasis, ↓clearance of airways • POLYCYTHEMIA: response to chronic hypoxemia – CONDUCTION DISTURBANCES – HEART FAILURE 6/8/2021 11
ALTERATIONS IN RESPIRATORY FUNCTIONING We breathe to take in O 2 and eliminate CO 2 • HYPERVENTILATION: – in excess of what is needed to eliminate CO 2 • HYPOVENTILATION: – inadequate to meet O 2 needs OR to eliminate CO 2 • HYPOXIA • INADEQUATE TISSUE OXYGENATION • HYPOXEMIA • DECREASED OXYGEN CONCENTRATION IN THE ARTERIAL BLOOD 6/8/2021 12
![SPECIAL OXYGEN CONSIDERATIONS ACROSS THE LIFE SPAN INFANTS AND TODDLERS SURFACTANT newborn SPECIAL OXYGEN CONSIDERATIONS ACROSS THE LIFE SPAN • INFANTS AND TODDLERS – SURFACTANT [newborn]](https://slidetodoc.com/presentation_image_h2/6160a57b52d18ce195e5b2c5307649a0/image-13.jpg)
SPECIAL OXYGEN CONSIDERATIONS ACROSS THE LIFE SPAN • INFANTS AND TODDLERS – SURFACTANT [newborn] – Risk for URI – Shorter airways • OLDER ADULTS – DEGENERATIVE PROCESSES • Compliance, chest wall movement, accumulated pollutants, cardiac and perfusion changes, alveolar changes, cilia decrease – CHRONIC DISEASE • HTN, Respiratory, Cardiac, Renal… 6/8/2021 13
LIFESTYLE FACTORS • • • 6/8/2021 NUTRITION EXERCISE SMOKING SUBSTANCE ABUSE STRESS ENVIRONMENTAL FACTORS 14
Nursing Process • Nursing History: Ability to meet O 2 needs Cardiac function Respiratory function Pain Fatigue Dyspnea Cough Wheezing Respiratory Infections Allergies Risk Factors Medications
PHYSICAL ASSESSMENT • INSPECTION – GENERAL APPEARANCE – LOC – SYSTEMIC CIRCULATION – BREATHING PATTERNS – CHEST WALL MOVEMENT 6/8/2021 16
PHYSICAL ASSESSMENT • PALPATION – THORACIC EXCURSION – AREAS OF TENDERNESS – EXTREMITIES – CAPILLARY REFILL 6/8/2021 17
PHYSICAL ASSESSMENT • PERCUSSION – AREAS OF CONSOLIDATION • AUSCULTATION – NORMAL V. ABNORMAL LUNG SOUNDS 6/8/2021 18
PHYSICAL ASSESSMENT • DIAGNOSTIC TESTS – – – – – 6/8/2021 PULSE OXIMETER PEAK EXPIRATORY FLOW RATE ARTERIAL BLOOD GASES CHEST X-RAY SPUTUM SPECIMEN PULMONARY FUNCTION TESTING BRONCHOSCOPY VENTILATION-PERFUSION LUNG SCAN [V/Q] THORACENTESIS CT / MRI 19

6/8/2021 20
Case Study #1 • 36 yo male visiting from Austin, TX with sudden onset” dizzy, confused, headache and hard to breathe” this afternoon. No obvious trauma. No significant medical history; friend states “he’s in great shape – an athlete – he comes here to bike and climb. He’s climbing the fourteeners!” • VS: T 37. 3; P 90, R 36, B/P 108/58, SPO 2 80% on RA • Assessment: pale, anxious, confused, c/o headache. Oriented to person only. Sinus tachycardia; deep, labored resp. with fine crackles at bases. Extremities cool to touch and pale.
What’s going on? • • What is abnormal? What do you think the cause is? What should the interventions be? Nursing diagnosis for this patient?
Nursing Diagnoses • • • Activity Intolerance Impaired Gas Exchange Ineffective Airway Clearance Ineffective Breathing Pattern Risk for Infection
Goals • Pt will: – Maintain airway – Clear secretions effectively – Increase hydrations [to mobilize secretions] – Improve Oxygenation [SPO 2] – Increase activity tolerance – Report decreased Dyspnea [scale 0 -10] – Decrease risk factors – Show resolution/ improvement in underlying cause
INTERVENTIONS • HEALTH PROMOTION – VACCINATIONS – HEALTHY LIFESTYLE BEHAVIOR – ENVIRONMENTAL AWARENESS – EDUCATION • Reduce risk factors 6/8/2021 25
![Case study 2 72 yo female Denver resident co SOB dyspnea dizziness and Case study #2 • 72 yo female Denver resident c/o SOB [dyspnea], dizziness and](https://slidetodoc.com/presentation_image_h2/6160a57b52d18ce195e5b2c5307649a0/image-26.jpg)
Case study #2 • 72 yo female Denver resident c/o SOB [dyspnea], dizziness and fatigue. Family reports she seems “pleasantly confused” today. HX of DM with renal failure treated with oral Glucophage • VS: T 36. 2 C, P 86, R 30, B/P 160/88, SPO 2 90 on RA • Labs: Na+ 136, K+ 3. 0, HCT 40, Hgb 14; • ABG: ph 7. 32, Pa. O 2 80, PCO 2 46, HCO 3 - 18 • Assessment: Oriented to person, knows she is ‘not at home’. Lungs clear, respirations rapid and deep w/o use of accessory muscles. Other findings WNL for age
What to do? • • • Any more info you need? Labs? What in her history raises a flag? What is the problem? What interventions are appropriate? Nursing diagnoses for this patients?
![Interventions Focus on treating underlying cause abx O 2 adaptation meds breathing Interventions • • Focus on: treating underlying cause [abx, O 2] adaptation [meds, breathing](https://slidetodoc.com/presentation_image_h2/6160a57b52d18ce195e5b2c5307649a0/image-28.jpg)
Interventions • • Focus on: treating underlying cause [abx, O 2] adaptation [meds, breathing techniques] preventing complications [TC&DB, IS] – managing Dyspnea [O 2, position, activity] – Maintaining Airway [Suction, cough, IS] – Mobilizing Secretions [hydration, TC&DB, meds] – Prevent infection/complication
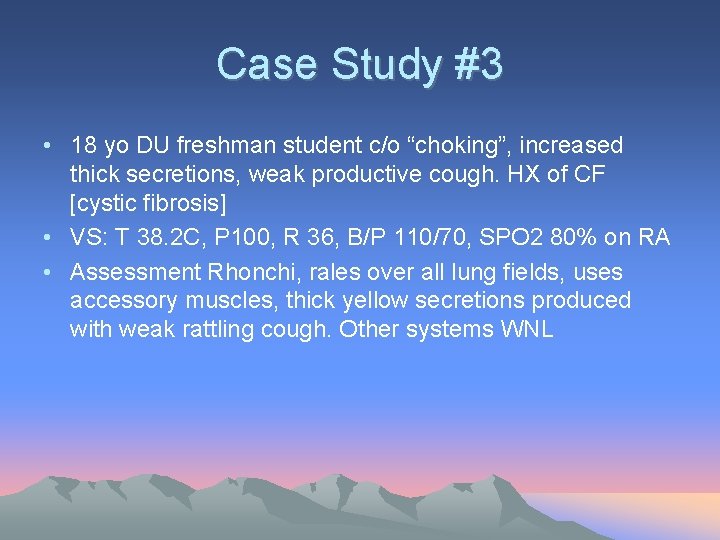
Case Study #3 • 18 yo DU freshman student c/o “choking”, increased thick secretions, weak productive cough. HX of CF [cystic fibrosis] • VS: T 38. 2 C, P 100, R 36, B/P 110/70, SPO 2 80% on RA • Assessment Rhonchi, rales over all lung fields, uses accessory muscles, thick yellow secretions produced with weak rattling cough. Other systems WNL
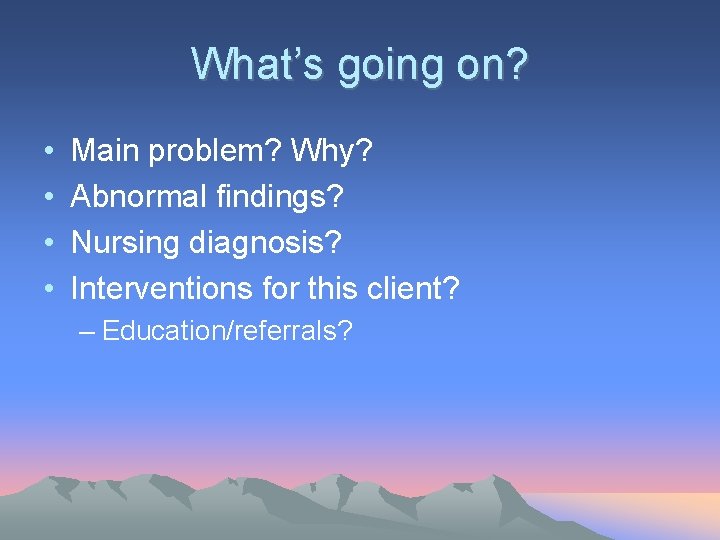
What’s going on? • • Main problem? Why? Abnormal findings? Nursing diagnosis? Interventions for this client? – Education/referrals?
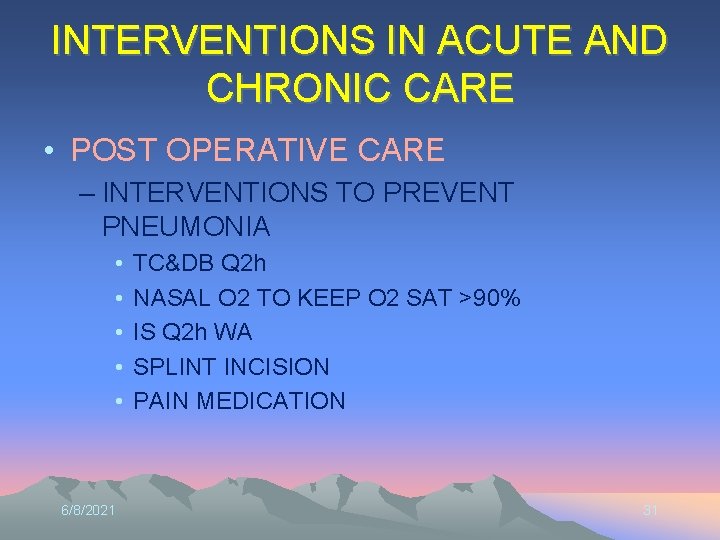
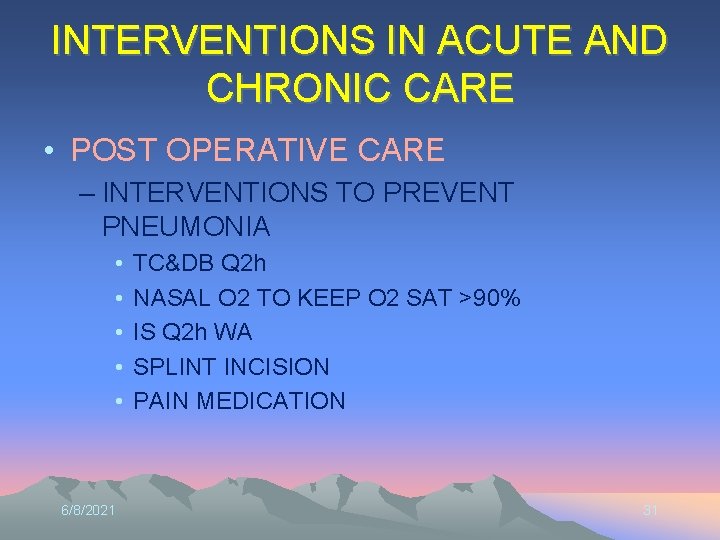
INTERVENTIONS IN ACUTE AND CHRONIC CARE • POST OPERATIVE CARE – INTERVENTIONS TO PREVENT PNEUMONIA • • • 6/8/2021 TC&DB Q 2 h NASAL O 2 TO KEEP O 2 SAT >90% IS Q 2 h WA SPLINT INCISION PAIN MEDICATION 31
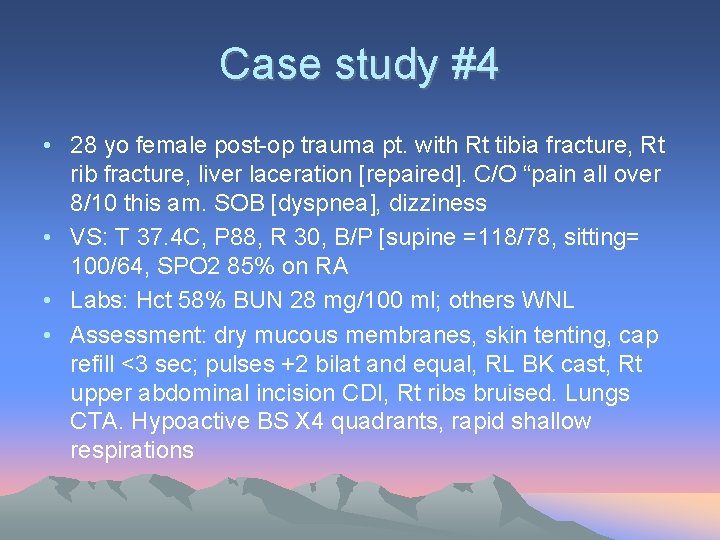
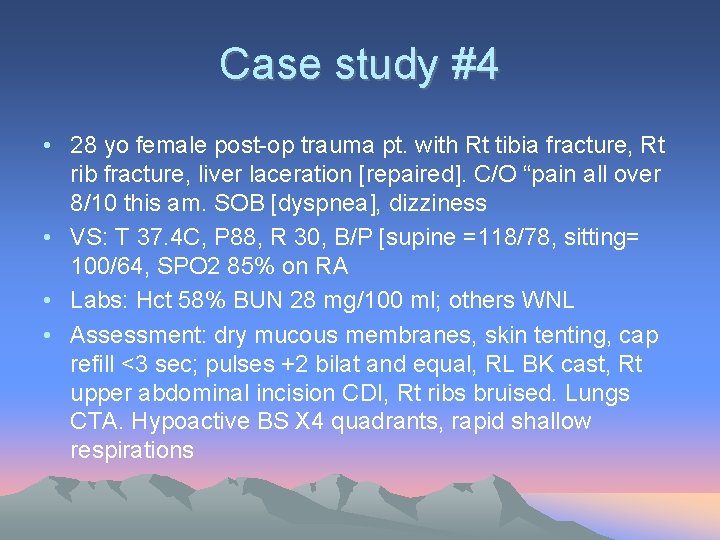
Case study #4 • 28 yo female post-op trauma pt. with Rt tibia fracture, Rt rib fracture, liver laceration [repaired]. C/O “pain all over 8/10 this am. SOB [dyspnea], dizziness • VS: T 37. 4 C, P 88, R 30, B/P [supine =118/78, sitting= 100/64, SPO 2 85% on RA • Labs: Hct 58% BUN 28 mg/100 ml; others WNL • Assessment: dry mucous membranes, skin tenting, cap refill <3 sec; pulses +2 bilat and equal, RL BK cast, Rt upper abdominal incision CDI, Rt ribs bruised. Lungs CTA. Hypoactive BS X 4 quadrants, rapid shallow respirations
What is wrong? • • Abnormal Findings? History? Nursing diagnoses? Interventions?
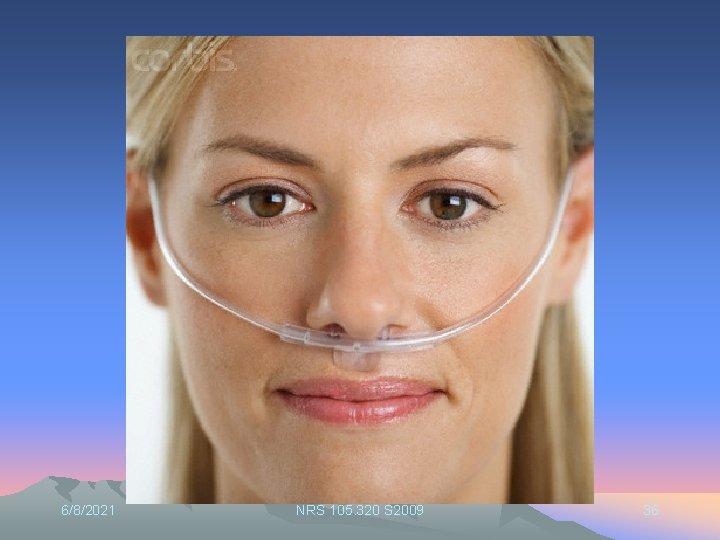
Oxygen • • Yes, it is a medication Can cause harm Ordered by Physician Standing orders - emergency
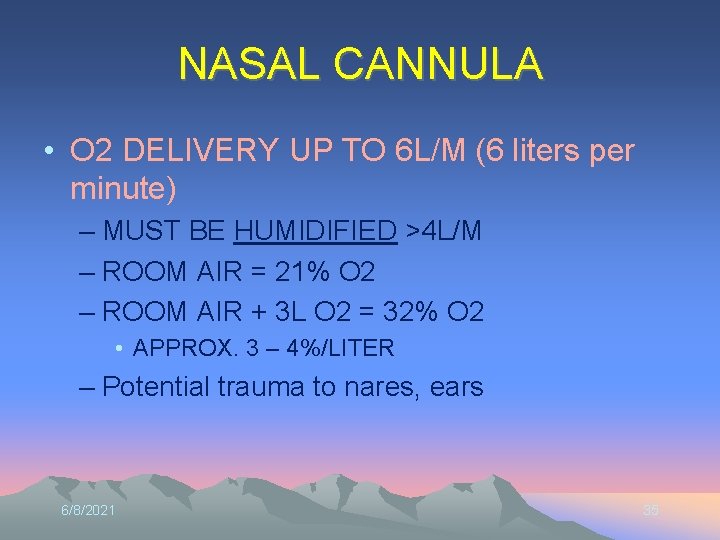
NASAL CANNULA • O 2 DELIVERY UP TO 6 L/M (6 liters per minute) – MUST BE HUMIDIFIED >4 L/M – ROOM AIR = 21% O 2 – ROOM AIR + 3 L O 2 = 32% O 2 • APPROX. 3 – 4%/LITER – Potential trauma to nares, ears 6/8/2021 35
6/8/2021 NRS 105. 320 S 2009 36
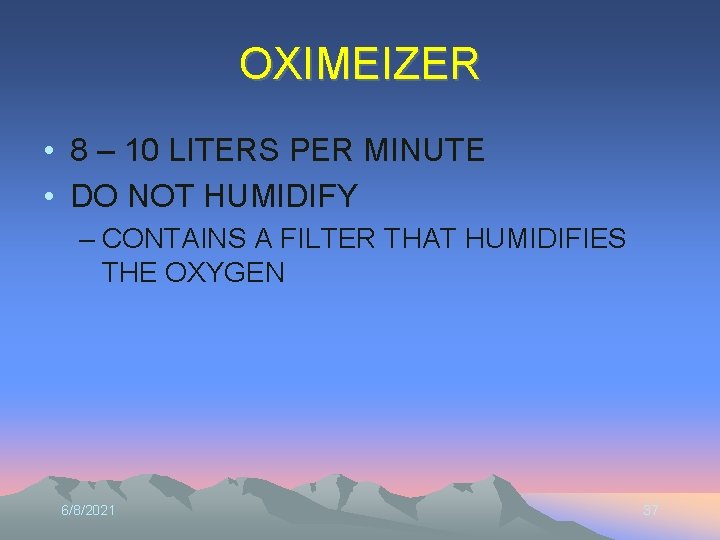
OXIMEIZER • 8 – 10 LITERS PER MINUTE • DO NOT HUMIDIFY – CONTAINS A FILTER THAT HUMIDIFIES THE OXYGEN 6/8/2021 37
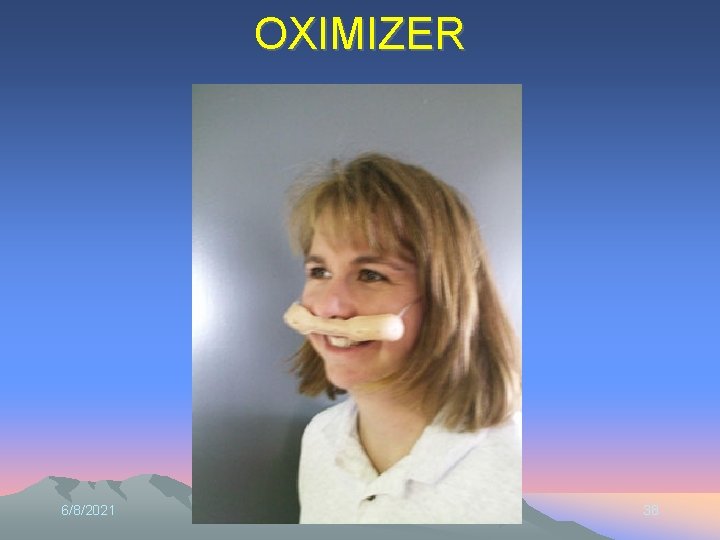
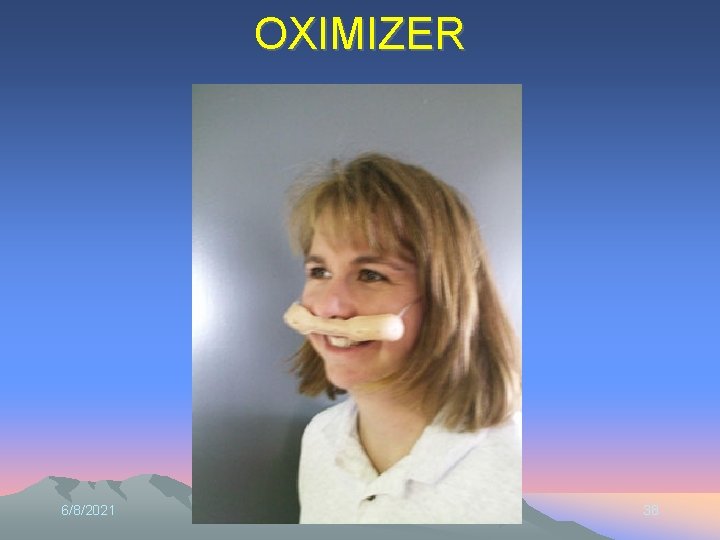
OXIMIZER 6/8/2021 NRS 105. 320 S 2009 38
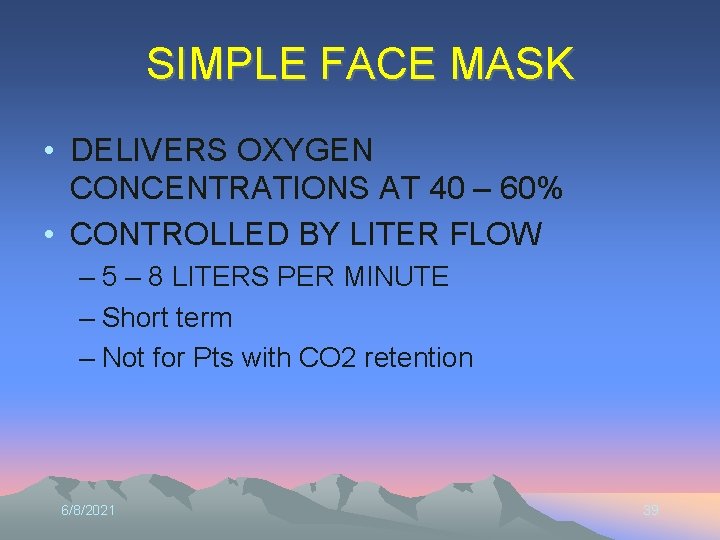
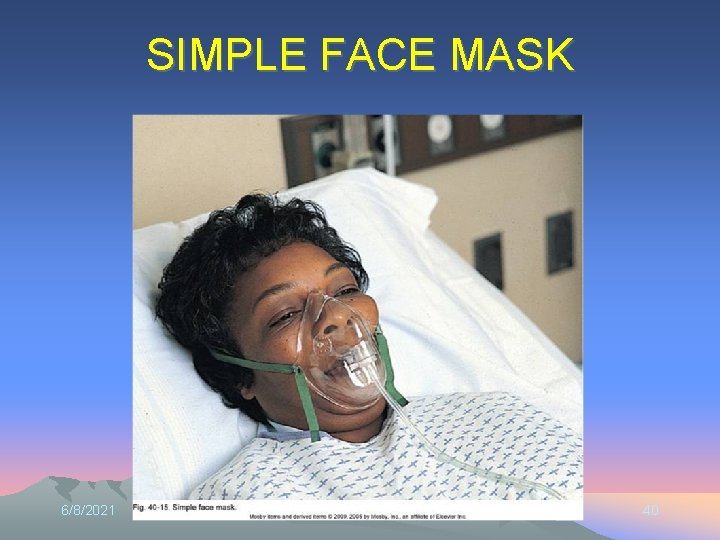
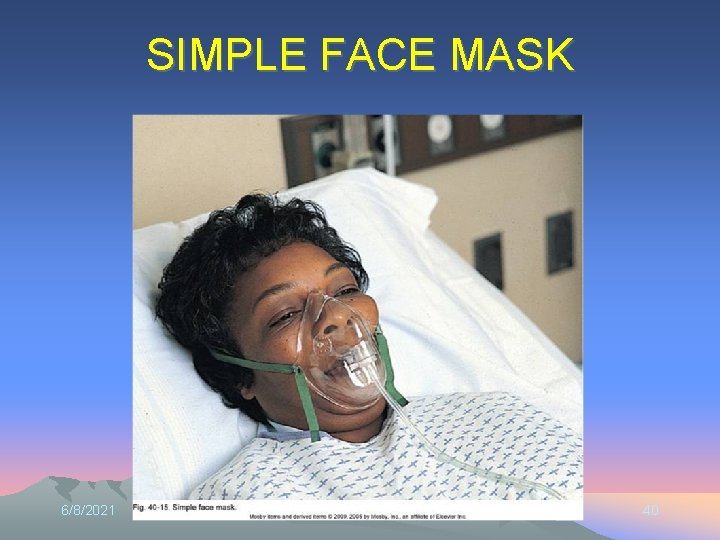
SIMPLE FACE MASK • DELIVERS OXYGEN CONCENTRATIONS AT 40 – 60% • CONTROLLED BY LITER FLOW – 5 – 8 LITERS PER MINUTE – Short term – Not for Pts with CO 2 retention 6/8/2021 39
SIMPLE FACE MASK 6/8/2021 NRS 105. 320 S 2009 40
NON REBREATHER MASK • DELIVERS THE HIGHEST LEVEL OF OXYGEN POSSIBLE WITH A MASK – 95 – 100% – LITER FLOW 10 – 15 LITERS PER MINUTE – ONE WAY VALVE BETWEEN RESERVOIR AND MASK • PREVENTS ROOM AIR FROM MIXING WITH O 2 6/8/2021 41

NONREBREATHER MASK 6/8/2021 NRS 105. 320 S 2009 42
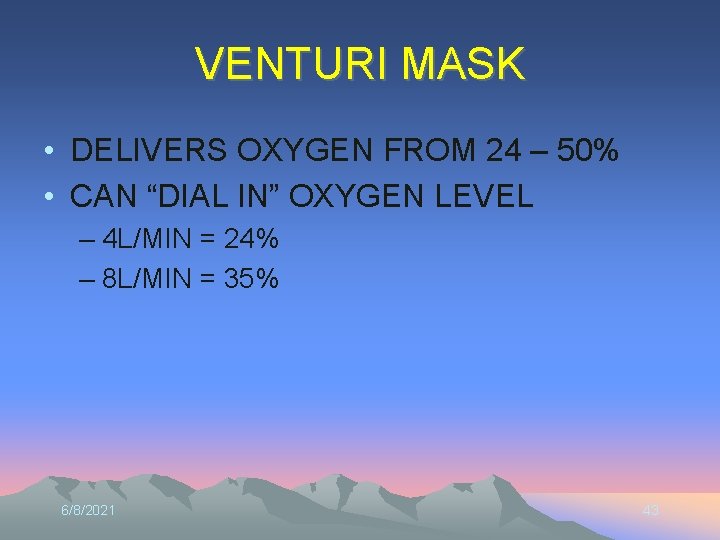
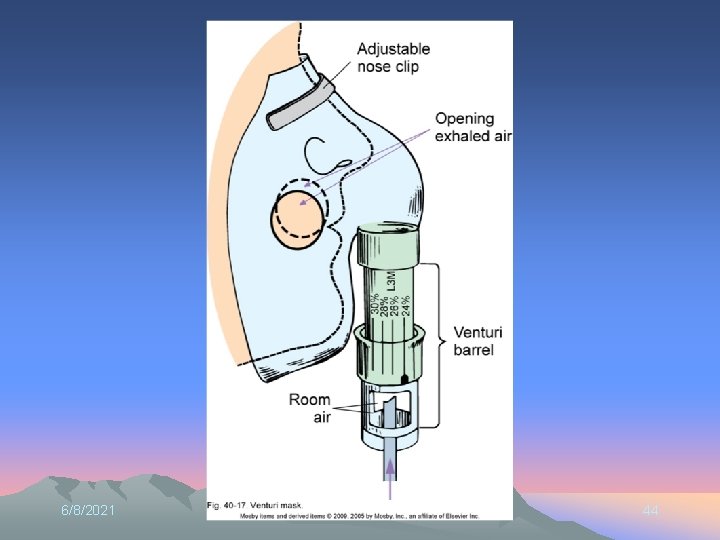
VENTURI MASK • DELIVERS OXYGEN FROM 24 – 50% • CAN “DIAL IN” OXYGEN LEVEL – 4 L/MIN = 24% – 8 L/MIN = 35% 6/8/2021 43
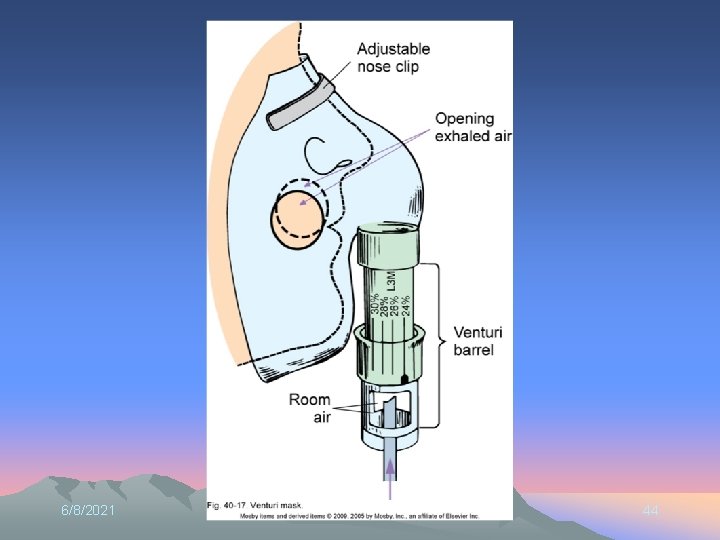
6/8/2021 NRS 105. 320 S 2009 44
OXYGEN FACE TENT 6/8/2021 NRS 105. 320 S 2009 45

6/8/2021 NRS 105. 320 S 2009 46
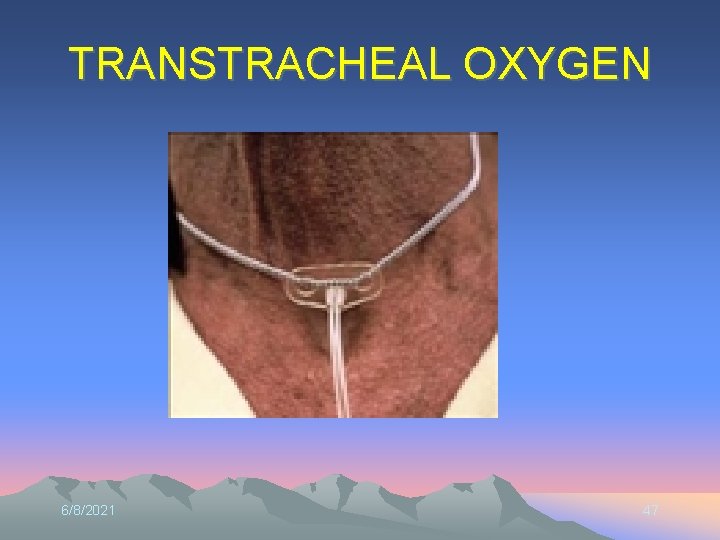
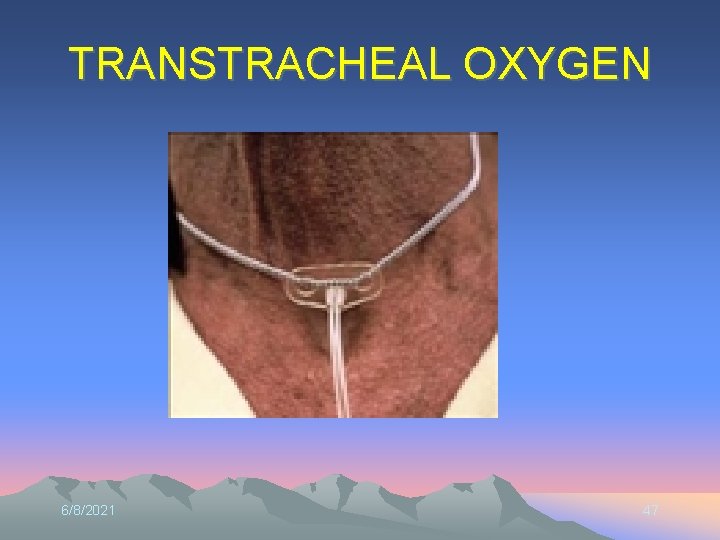
TRANSTRACHEAL OXYGEN 6/8/2021 47

6/8/2021 NRS 105. 320 S 2009 48

6/8/2021 49

6/8/2021 50
6/8/2021 51
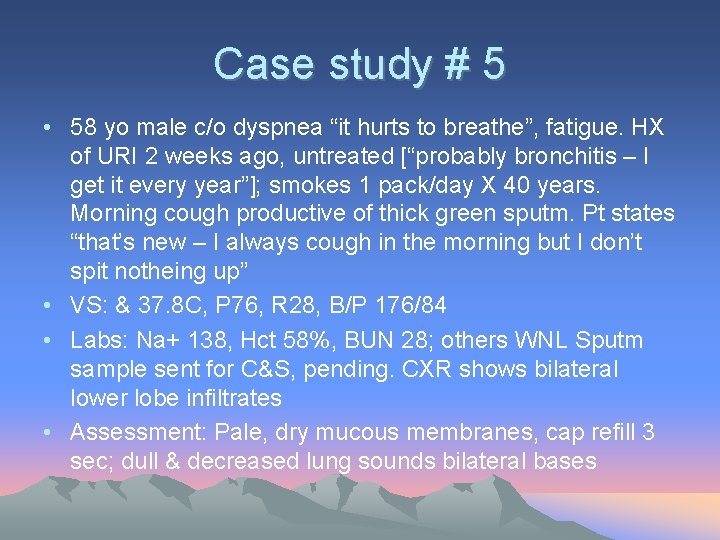
Case study # 5 • 58 yo male c/o dyspnea “it hurts to breathe”, fatigue. HX of URI 2 weeks ago, untreated [“probably bronchitis – I get it every year”]; smokes 1 pack/day X 40 years. Morning cough productive of thick green sputm. Pt states “that’s new – I always cough in the morning but I don’t spit notheing up” • VS: & 37. 8 C, P 76, R 28, B/P 176/84 • Labs: Na+ 138, Hct 58%, BUN 28; others WNL Sputm sample sent for C&S, pending. CXR shows bilateral lower lobe infiltrates • Assessment: Pale, dry mucous membranes, cap refill 3 sec; dull & decreased lung sounds bilateral bases
What is wrong? • • • Abnormal Findings? History? Nursing diagnoses? Interventions? Additional info you need?
INTERVENTIONS IN ACUTE AND CHRONIC CARE • DYSPNEA – PATIENT ASSESSMENT – APPLY OXYGEN? – UNDERLYING CAUSE • ASTHMA • CHRONIC HEART FAILURE • COPD 6/8/2021 54
ASSESSMENT FINDINGS • THICK SECRETIONS – DO THEY NEED OXYGEN? – UPPER AIRWAY? – LOWER AIRWAY? – ASSESS SECRETIONS • • • 6/8/2021 HUMIDIFY HYDRATION NEBULIZER CHEST PHYSIOTHERAPY SUCTIONING 55
ASSESSMENT FINDINGS • WHEEZING (WHY ARE THEY WHEEZING? ) – OXYGEN? – BRONCHODILATOR – CONTINUED ASSESSMENT 6/8/2021 56
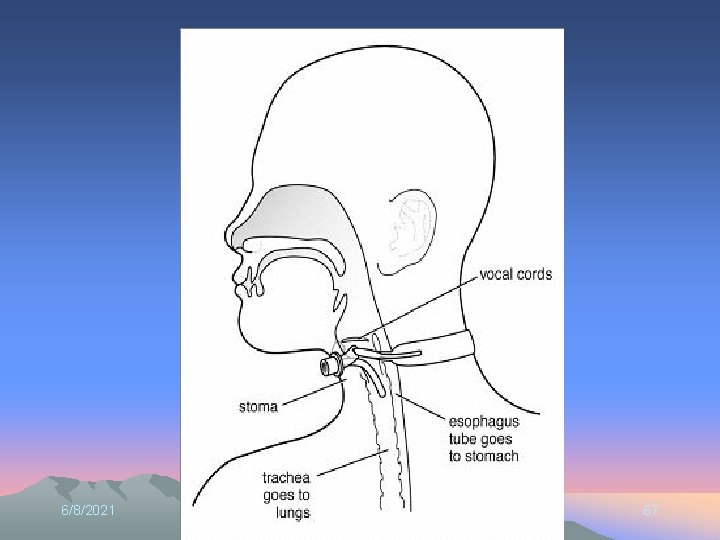
AIRWAY • NATURAL • ARTIFICIAL – NASAL – ORAL – ENDOTRACHEAL – TRACHEOSTOMY 6/8/2021 57
ARTIFICIAL AIRWAYS 6/8/2021 58
CARE OF THE PATIENT WITH AN ARTIFICIAL AIRWAY • ORAL AIRWAY – MAINTAINS AN OPEN AIRWAY • DURING DECREASED LEVEL OF CONSCIOUSNESS • SEDATION • SEIZURES – MADE OF HARD PLASTIC • ATTEND TO ANY PRESSURE AREAS ON LIPS, MOUTH, TONGUE • HOLLOW TO FACILITATE SUCTIONING 6/8/2021 59

6/8/2021 60
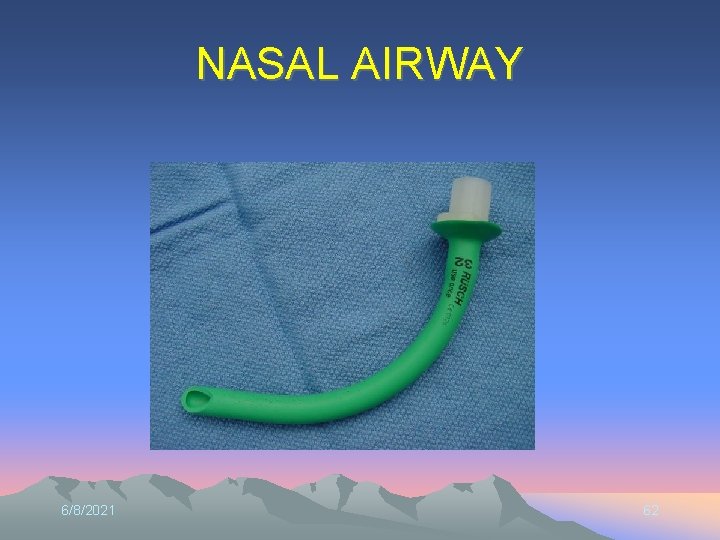
NASOTRACHEAL, NASOPHARYNGEAL OROPHARYNGEAL, OROTRACHEAL SUCTIONING • WHEN PATIENT IS UNABLE TO COUGH UP THICK PULMONARY SECRETIONS • PASS CATHETER THROUGH NOSE [less gagging] OR MOUTH 6/8/2021 61
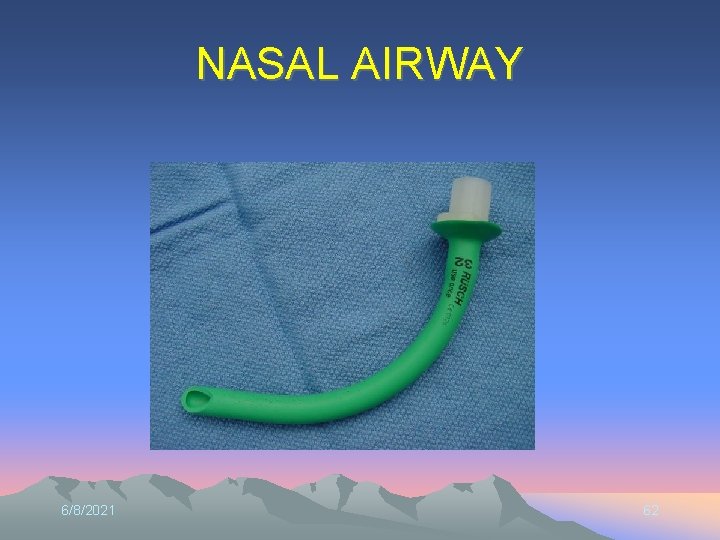
NASAL AIRWAY 6/8/2021 62
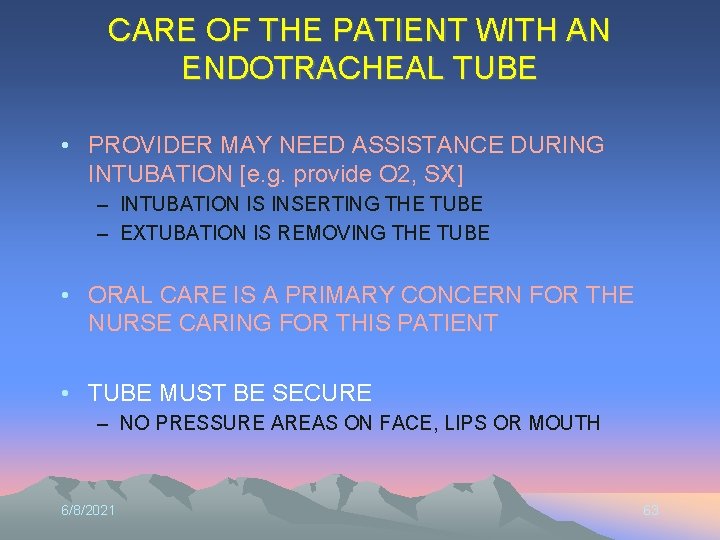
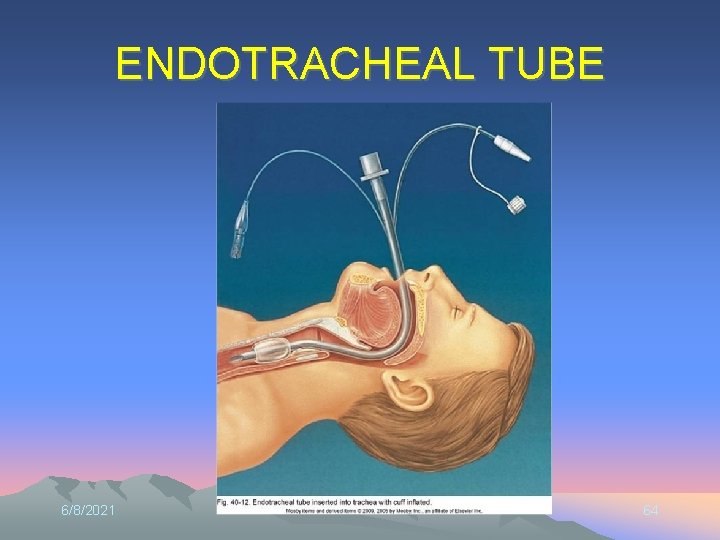
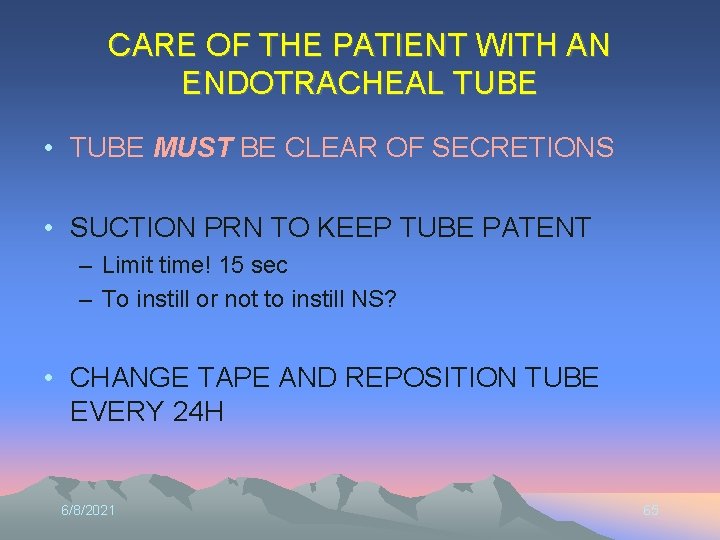
CARE OF THE PATIENT WITH AN ENDOTRACHEAL TUBE • PROVIDER MAY NEED ASSISTANCE DURING INTUBATION [e. g. provide O 2, SX] – INTUBATION IS INSERTING THE TUBE – EXTUBATION IS REMOVING THE TUBE • ORAL CARE IS A PRIMARY CONCERN FOR THE NURSE CARING FOR THIS PATIENT • TUBE MUST BE SECURE – NO PRESSURE AREAS ON FACE, LIPS OR MOUTH 6/8/2021 63
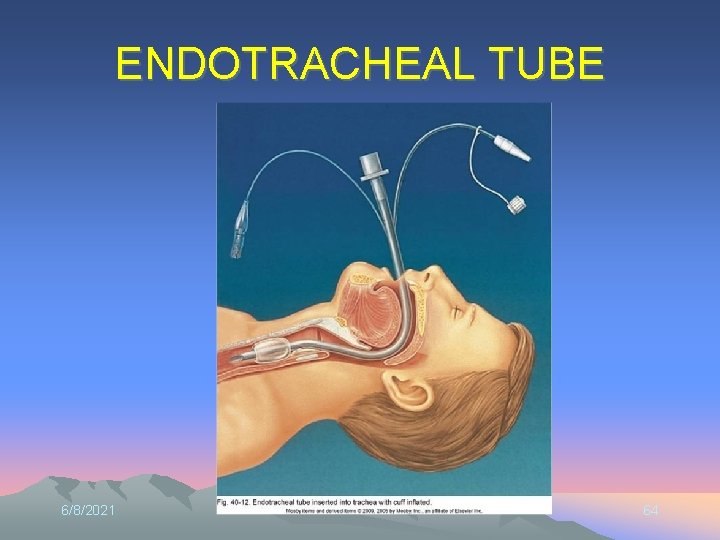
ENDOTRACHEAL TUBE 6/8/2021 64
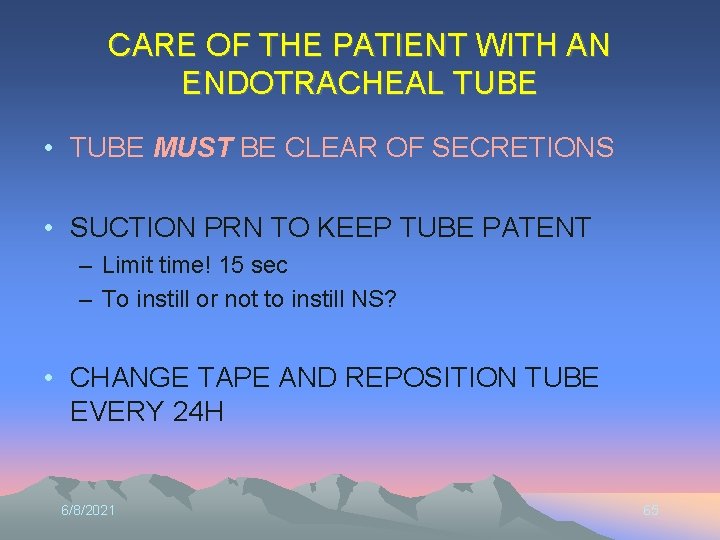
CARE OF THE PATIENT WITH AN ENDOTRACHEAL TUBE • TUBE MUST BE CLEAR OF SECRETIONS • SUCTION PRN TO KEEP TUBE PATENT – Limit time! 15 sec – To instill or not to instill NS? • CHANGE TAPE AND REPOSITION TUBE EVERY 24 H 6/8/2021 65
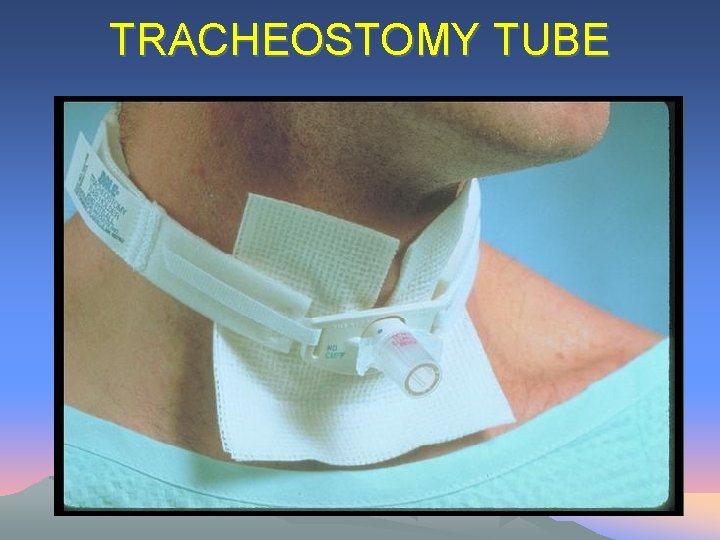
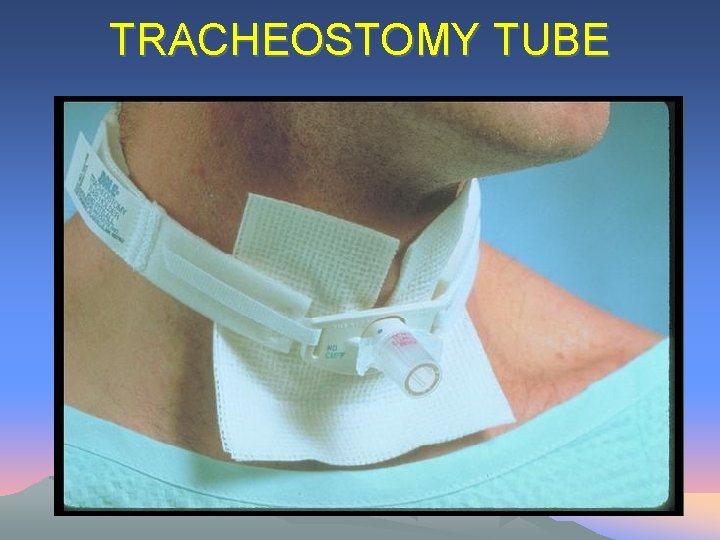
TRACHEOSTOMY TUBE 6/8/2021 66
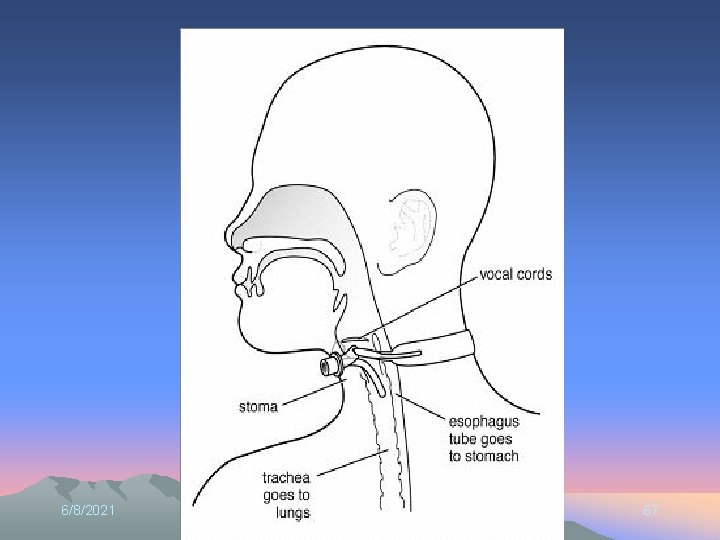
6/8/2021 67

6/8/2021 68

6/8/2021 69
CARE OF THE PATIENT WITH A TRACHEOSTOMY • TUBE MUST BE CLEAR OF SECRETIONS • SUCTION PRN TO KEEP TUBE PATENT • CHANGE DRESSING AND INNER CANNULA EVERY 24 H – IF INNER CANNULA IS NOT DISPOSABLE, REMOVE, CLEAN AND REPLACE 6/8/2021 70
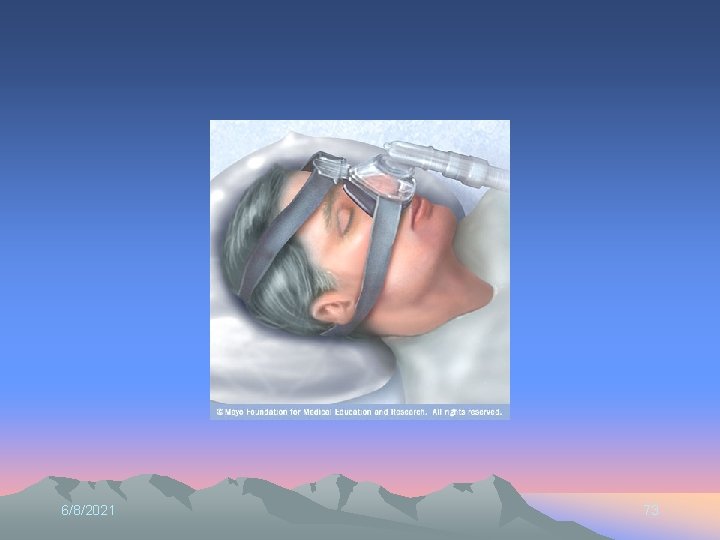
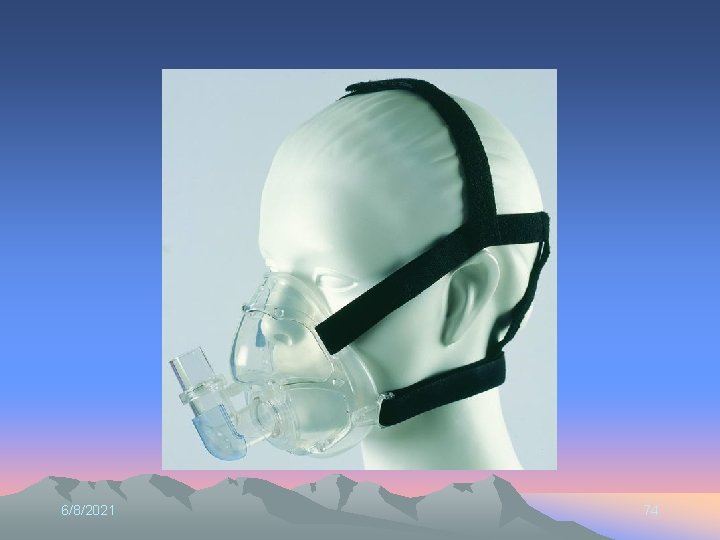
SLEEP APNEA • OBSTRUCTIVE SLEEP APNEA – one or more pauses in breathing or shallow breaths while you sleep. – can last from a few seconds to minutes. – occur 5 to 30 times or more an hour. – normal breathing then starts again, sometimes with a loud snort or choking sound • CENTRAL SLEEP APNEA – less common type of sleep apnea. – area of your brain that controls breathing doesn't send the correct signals – no effort to breathe for brief periods. 6/8/2021 71
CPAP / Bi. PAP • Congestive heart failure • Lung disorders resulting in high CO 2 • Patients for whom intubation is not possible • Sleep apnea • Surfactant deficiency/ atelectasis • Less invasive than intubation, trach 6/8/2021 72
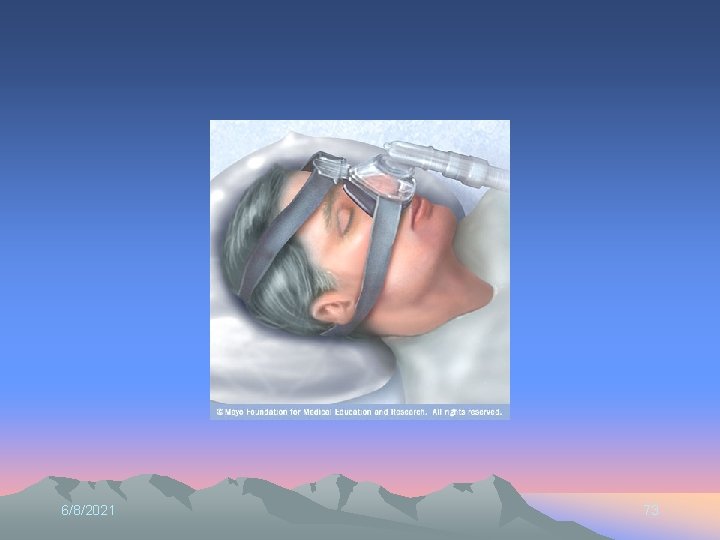
6/8/2021 73
6/8/2021 74
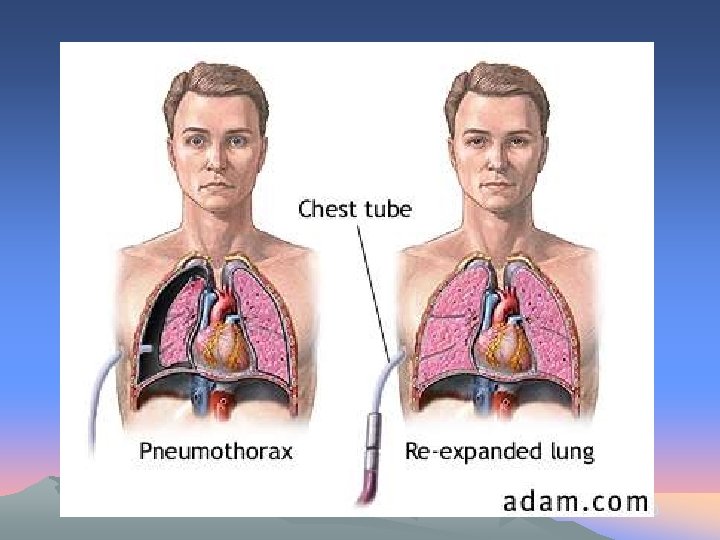
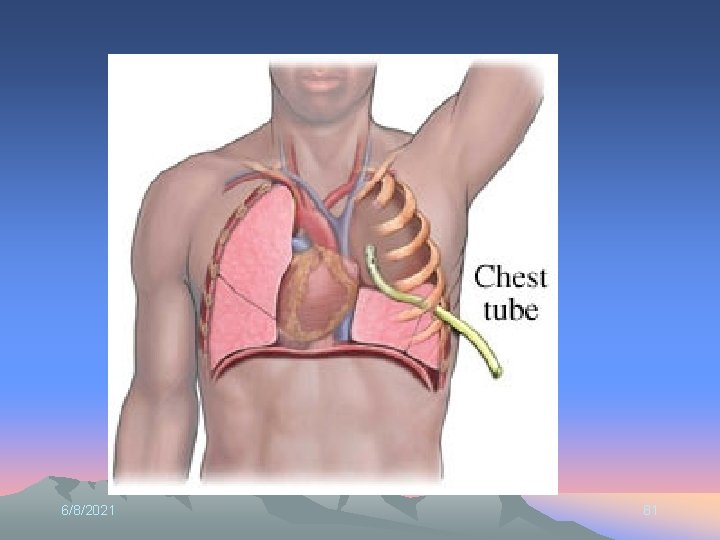
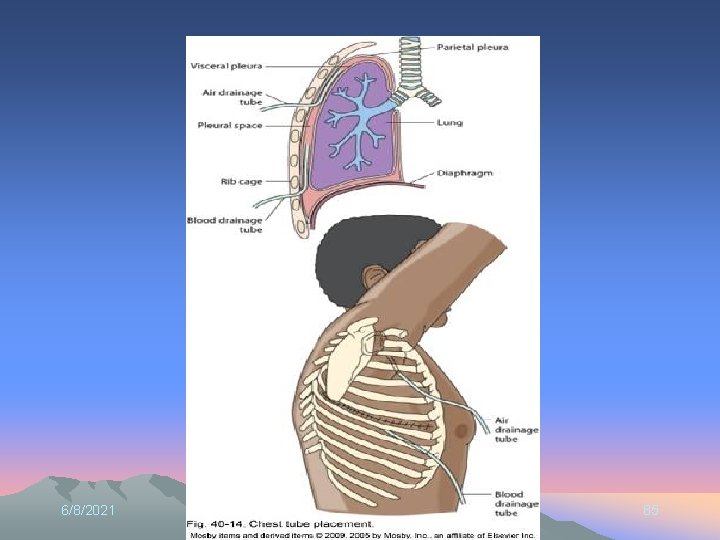
CARE OF THE PATIENT WITH A CHEST TUBE 6/8/2021 75
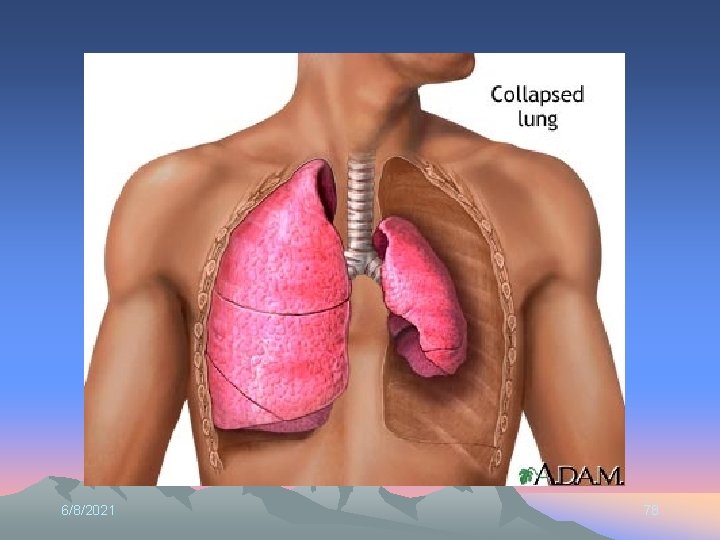
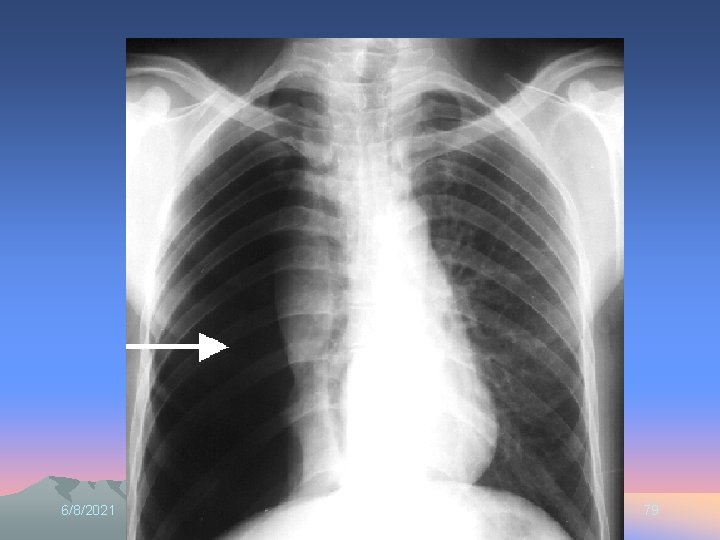
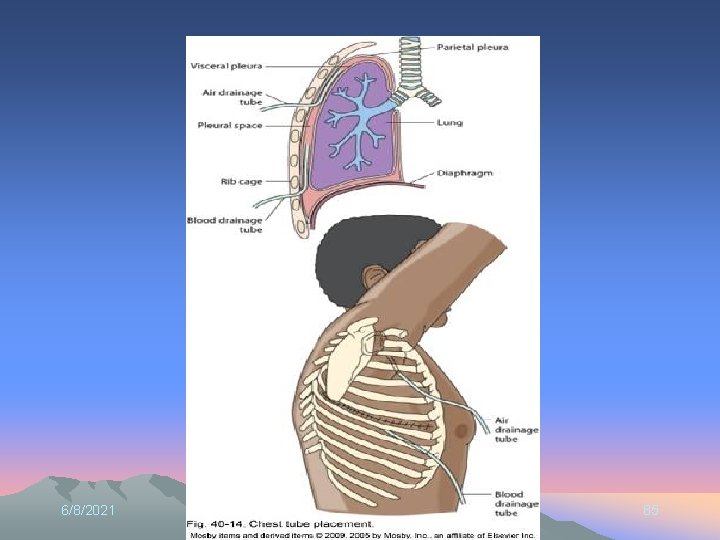
CHEST TUBES • PURPOSE – RE-EXPAND THE LUNG • HOW? – RELEASE AIR – DRAIN FLUID 6/8/2021 76
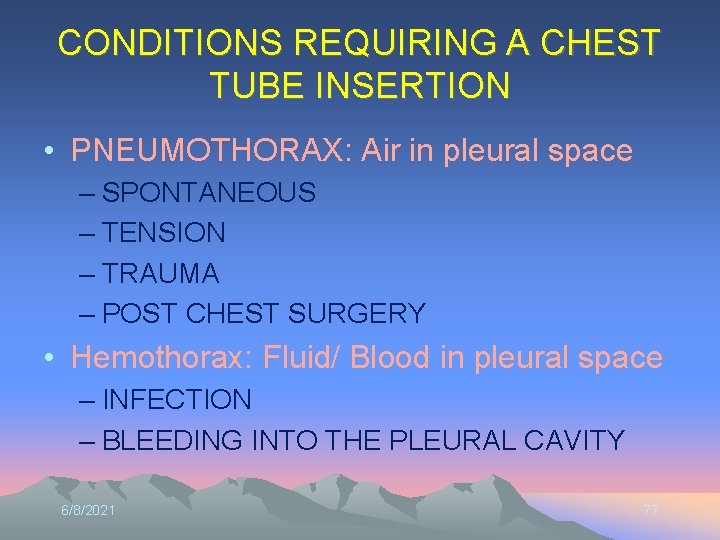
CONDITIONS REQUIRING A CHEST TUBE INSERTION • PNEUMOTHORAX: Air in pleural space – SPONTANEOUS – TENSION – TRAUMA – POST CHEST SURGERY • Hemothorax: Fluid/ Blood in pleural space – INFECTION – BLEEDING INTO THE PLEURAL CAVITY 6/8/2021 77
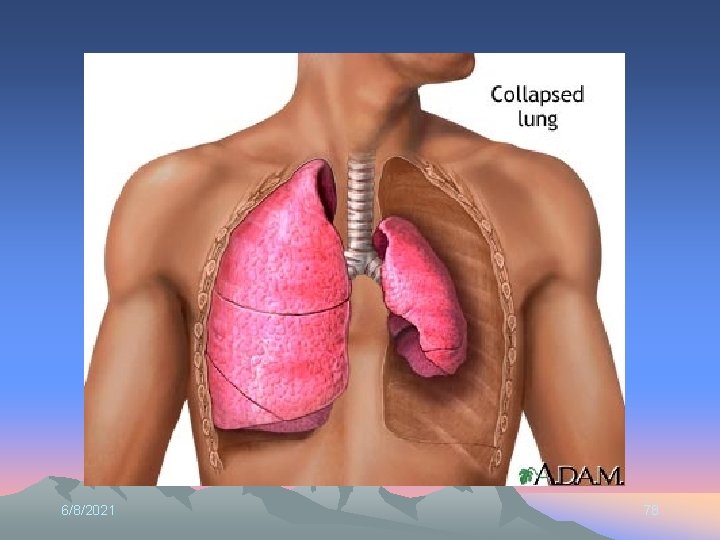
6/8/2021 78
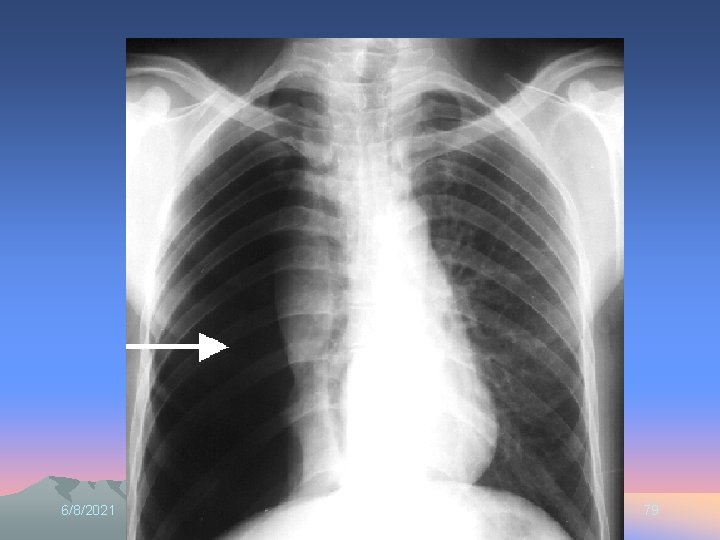
6/8/2021 79
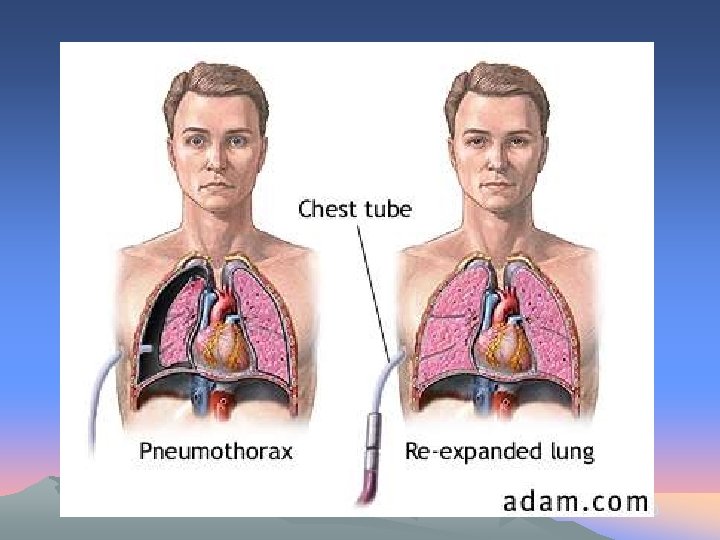
6/8/2021 80
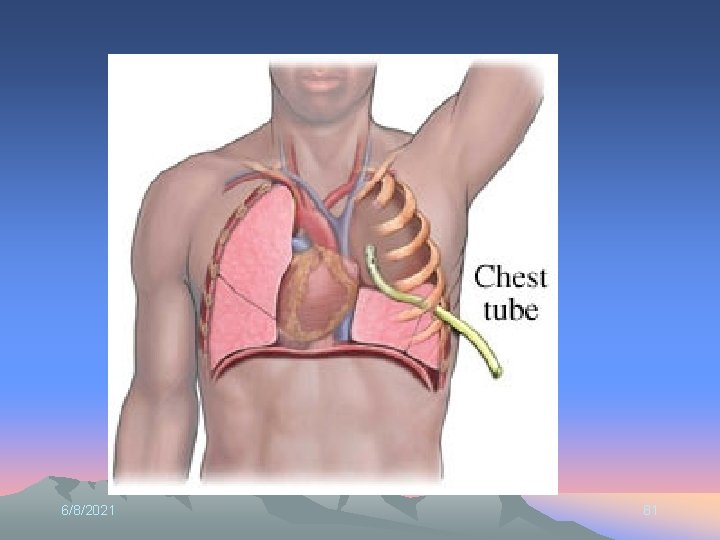
6/8/2021 81
6/8/2021 82
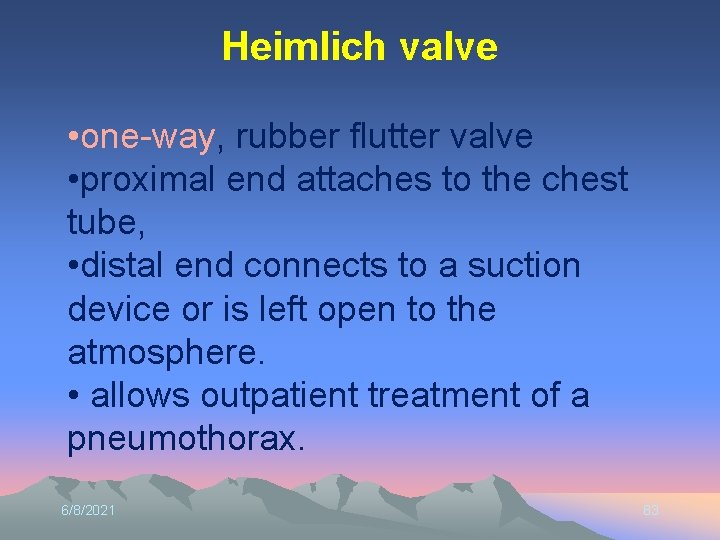
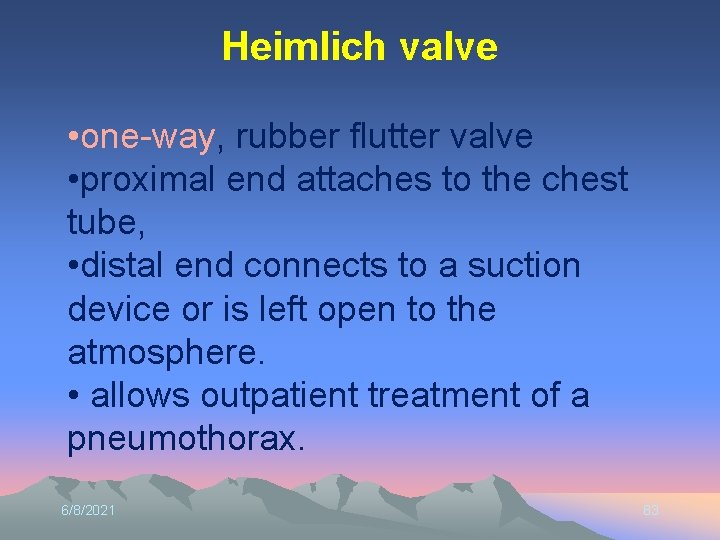
Heimlich valve • one-way, rubber flutter valve • proximal end attaches to the chest tube, • distal end connects to a suction device or is left open to the atmosphere. • allows outpatient treatment of a pneumothorax. 6/8/2021 83

HEIMLICH VALVE 6/8/2021 84
6/8/2021 85

6/8/2021 86
CARE OF THE PATIENT WITH A CHEST TUBE • PATIENT ASSESSMENT – RESPIRATORY RATE – CHEST EXCURSION – SYMMETRY – OXYGENATION (PULSE OXIMETER) – BREATH SOUNDS – CREPITUS 6/8/2021 87
CARE OF THE PATIENT WITH A CHEST TUBE • ASSESS PATIENT AND SYSTEM – – – DRAINAGE [amount, type, etc] DRESSING [DRY AND INTACT? ] TUBE [KINKED? Straight? ] BE SURE IT DOES NOT DRAG ON THE FLOOR VERIFY SUCTION [Bubbling = working] & WATER SEAL [fluctuation w/ breathing, bubbling = air from pleural space or dislodged tube] ORDERS – NEVER RAISE COLLECTION CHAMBER ABOVE CHEST [INSERTION POINT]! 6/8/2021 88
![Evaluation Ask pt to demonstrate techniques cough breathing Assess dyspnea cough sputum Evaluation • Ask pt. to demonstrate techniques [cough, breathing] • Assess dyspnea, cough, sputum,](https://slidetodoc.com/presentation_image_h2/6160a57b52d18ce195e5b2c5307649a0/image-89.jpg)
Evaluation • Ask pt. to demonstrate techniques [cough, breathing] • Assess dyspnea, cough, sputum, SPO 2, respiratory rate/ depth/effort • Goal met? Not met? Partially met? • Revision or continuation of plan?
Try This • • • Divide into 6 groups For each scenario, determine: What you think is going on Priority Nursing Diagnosis Goals The focus of your interventions – E. g. mobilize secretions, teach to TC&DB