Patient case study Overweight patient diagnosed with T
- Slides: 34
Patient case study Overweight patient diagnosed with T 2 D January 2021 SC-CRP-07658
Disclaimer • This patient case is hypothetical and has been developed in collaboration with Professor Cliff Bailey (Aston University, UK) • The statements reflect recommendations and suggestions from the ACROSS T 2 D Steering Committee for this specific clinical case and do not necessarily represent the opinions of The Boehringer Ingelheim and Lilly Alliance • Any data mentioned herein may be abbreviated and not exact 2
How to use this case study Robert – 50 -year-old male • This interactive patient case study is designed as a self-learning experience or to be incorporated into presentations and workshops. It has been developed to reflect a typical patient under the care of a PCP • Please follow Robert over the course of two sequential appointments and consider the multiple-choice questions to assess appropriate management steps PCP, primary care physician 3
Robert is a 50 -year-old male who is concerned about feeling tired and sleeping poorly. This is Robert’s first appointment with a PCP. You ask Robert about his presenting complaints, his medical history and his current lifestyle. Robert is not a real patient PCP, primary care physician 4
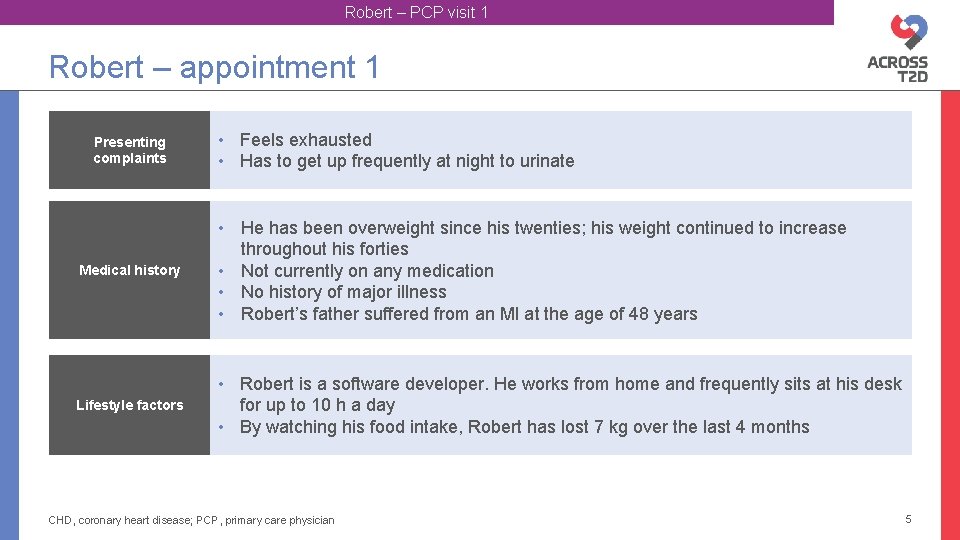
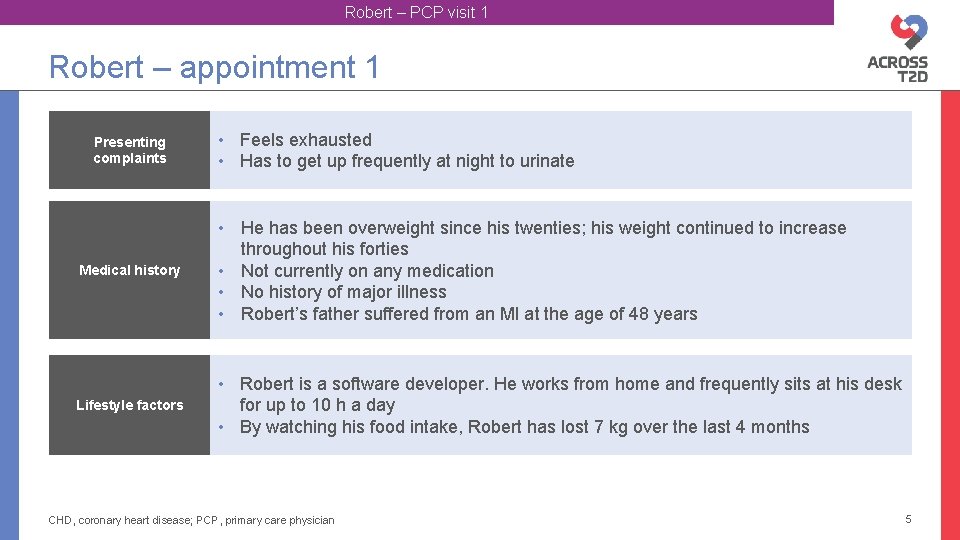
Robert – PCP visit 1 Robert – appointment 1 Presenting complaints • Feels exhausted • Has to get up frequently at night to urinate Medical history • He has been overweight since his twenties; his weight continued to increase throughout his forties • Not currently on any medication • No history of major illness • Robert’s father suffered from an MI at the age of 48 years Lifestyle factors • Robert is a software developer. He works from home and frequently sits at his desk for up to 10 h a day • By watching his food intake, Robert has lost 7 kg over the last 4 months CHD, coronary heart disease; PCP, primary care physician 5
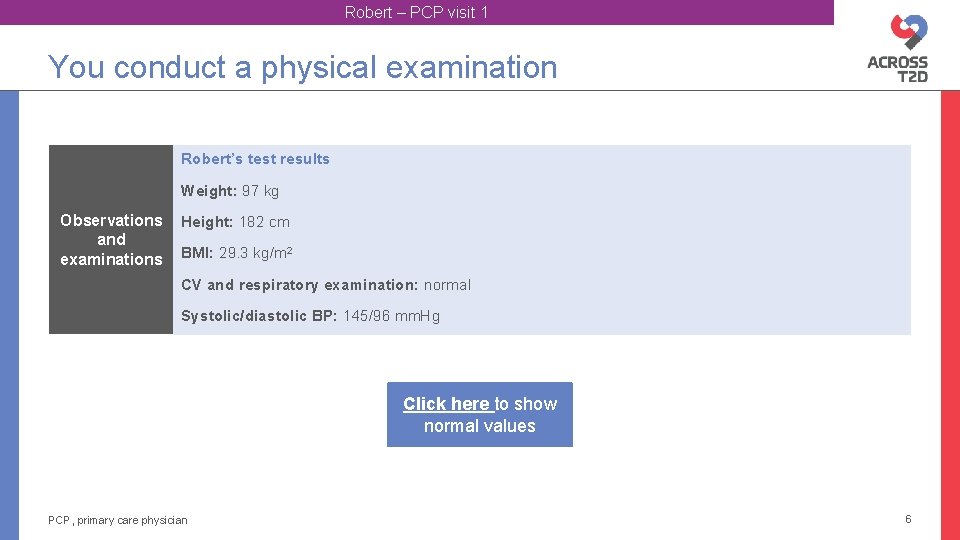
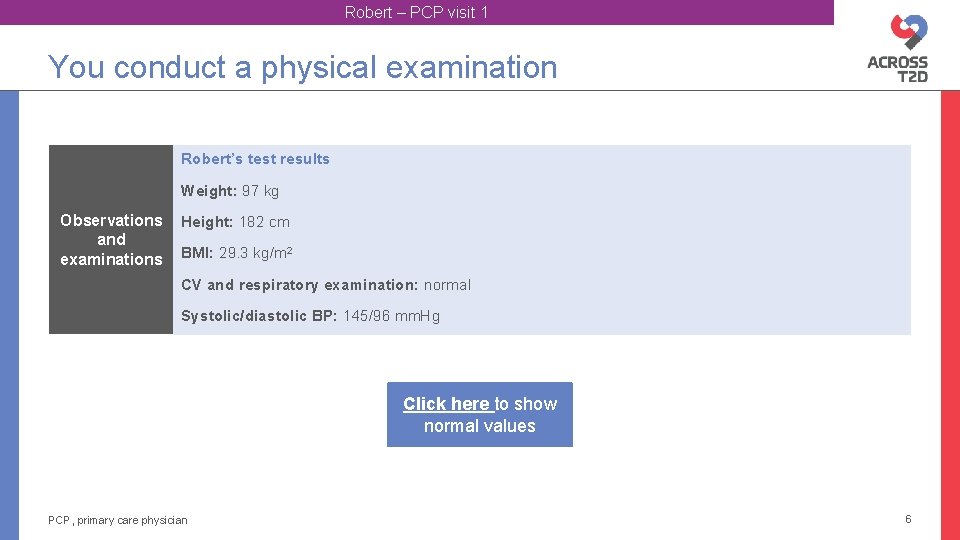
Robert – PCP visit 1 You conduct a physical examination Robert’s test results Weight: 97 kg Observations and examinations Height: 182 cm BMI: 29. 3 kg/m 2 CV and respiratory examination: normal Systolic/diastolic BP: 145/96 mm. Hg Click here to show normal values PCP, primary care physician 6
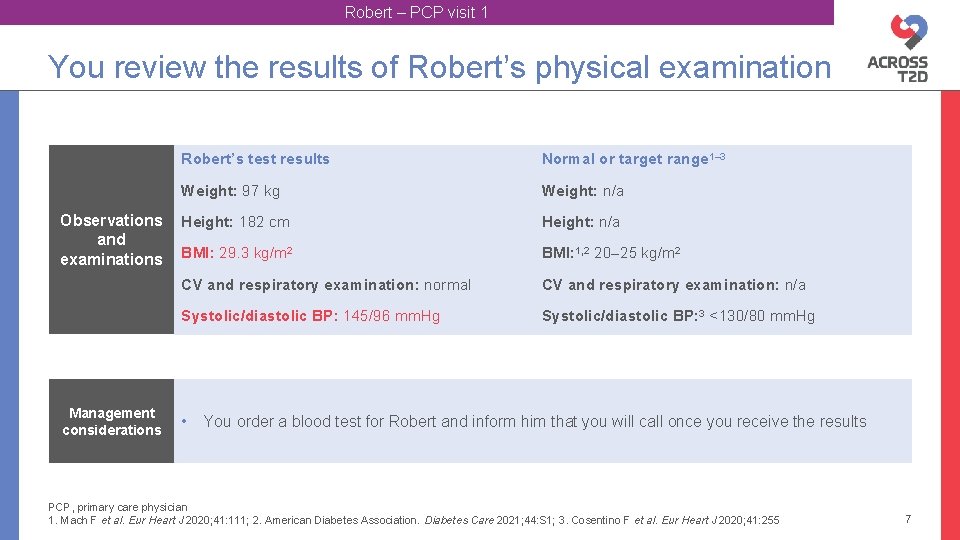
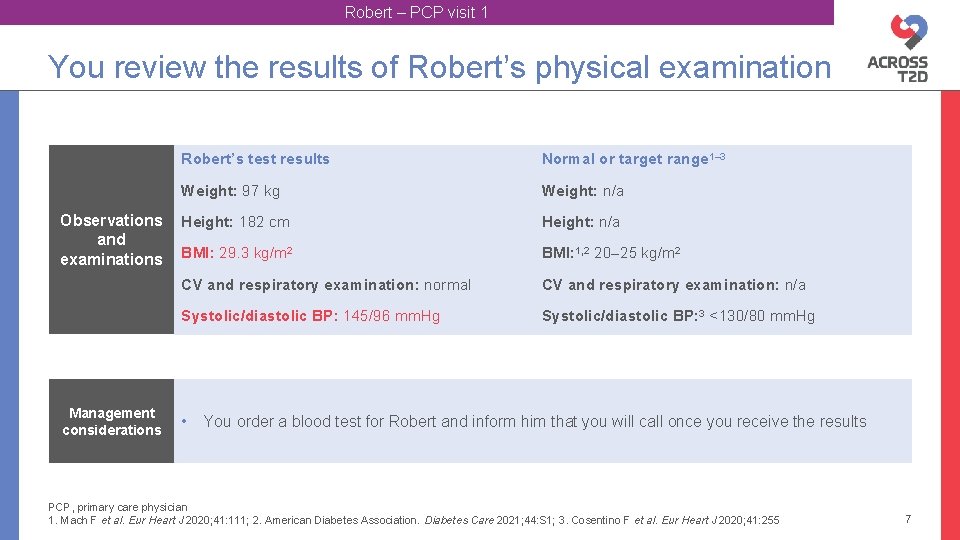
Robert – PCP visit 1 You review the results of Robert’s physical examination Observations and examinations Management considerations Robert’s test results Normal or target range 1– 3 Weight: 97 kg Weight: n/a Height: 182 cm Height: n/a BMI: 29. 3 kg/m 2 BMI: 1, 2 20– 25 kg/m 2 CV and respiratory examination: normal CV and respiratory examination: n/a Systolic/diastolic BP: 145/96 mm. Hg Systolic/diastolic BP: 3 <130/80 mm. Hg • You order a blood test for Robert and inform him that you will call once you receive the results PCP, primary care physician 1. Mach F et al. Eur Heart J 2020; 41: 111; 2. American Diabetes Association. Diabetes Care 2021; 44: S 1; 3. Cosentino F et al. Eur Heart J 2020; 41: 255 7
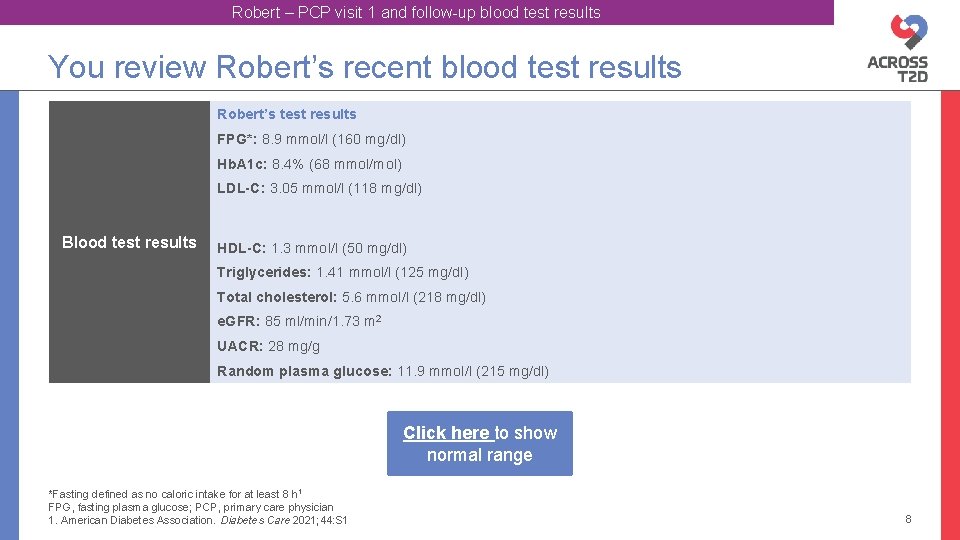
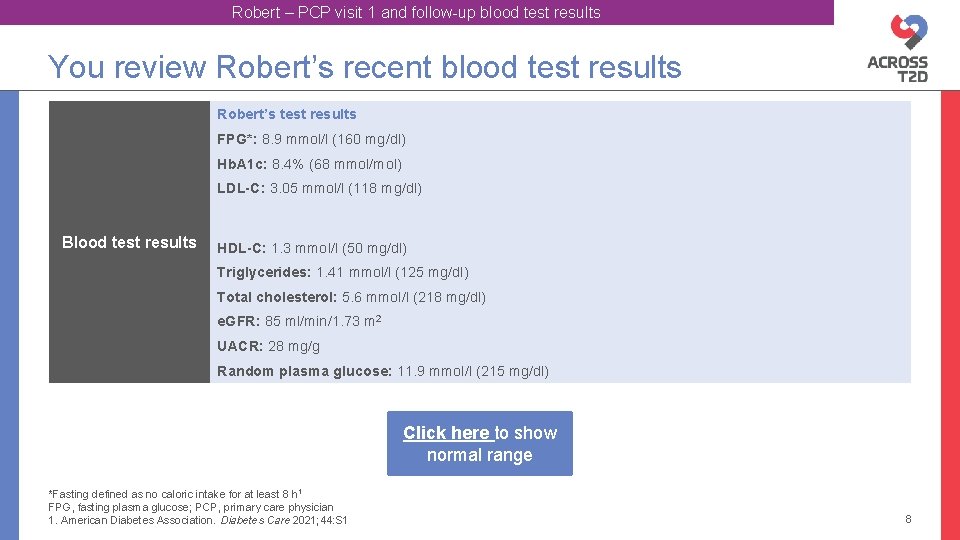
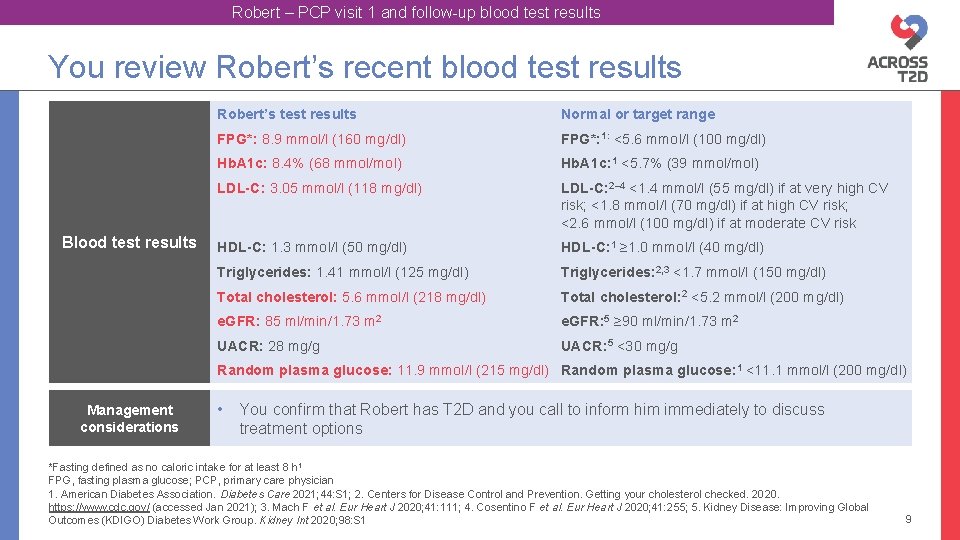
Robert – PCP visit 1 and follow-up blood test results You review Robert’s recent blood test results Robert’s test results FPG*: 8. 9 mmol/l (160 mg/dl) Hb. A 1 c: 8. 4% (68 mmol/mol) LDL-C: 3. 05 mmol/l (118 mg/dl) Blood test results HDL-C: 1. 3 mmol/l (50 mg/dl) Triglycerides: 1. 41 mmol/l (125 mg/dl) Total cholesterol: 5. 6 mmol/l (218 mg/dl) e. GFR: 85 ml/min/1. 73 m 2 UACR: 28 mg/g Random plasma glucose: 11. 9 mmol/l (215 mg/dl) Click here to show normal range *Fasting defined as no caloric intake for at least 8 h 1 FPG, fasting plasma glucose; PCP, primary care physician 1. American Diabetes Association. Diabetes Care 2021; 44: S 1 8
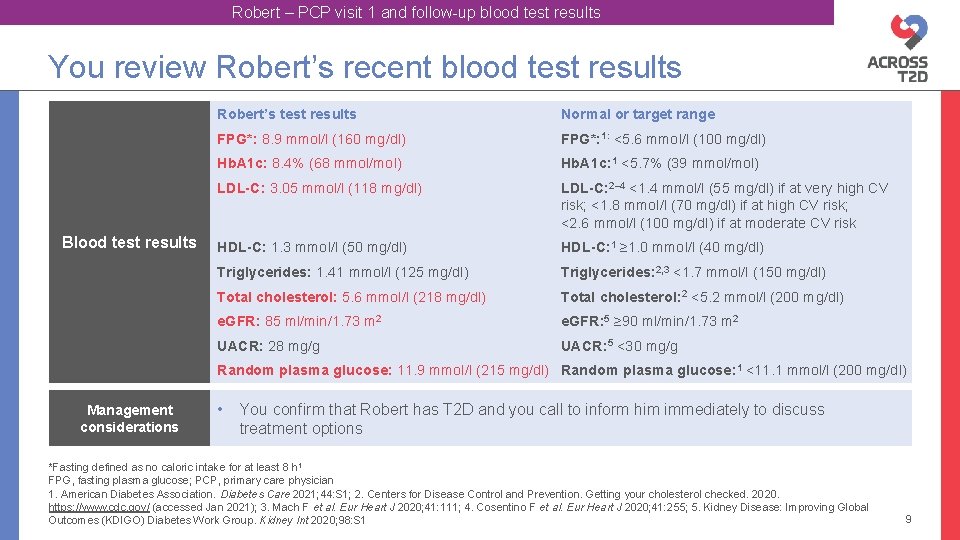
Robert – PCP visit 1 and follow-up blood test results You review Robert’s recent blood test results Blood test results Robert’s test results Normal or target range FPG*: 8. 9 mmol/l (160 mg/dl) FPG*: 1: <5. 6 mmol/l (100 mg/dl) Hb. A 1 c: 8. 4% (68 mmol/mol) Hb. A 1 c: 1 <5. 7% (39 mmol/mol) LDL-C: 3. 05 mmol/l (118 mg/dl) LDL-C: 2– 4 <1. 4 mmol/l (55 mg/dl) if at very high CV risk; <1. 8 mmol/l (70 mg/dl) if at high CV risk; <2. 6 mmol/l (100 mg/dl) if at moderate CV risk HDL-C: 1. 3 mmol/l (50 mg/dl) HDL-C: 1 ≥ 1. 0 mmol/l (40 mg/dl) Triglycerides: 1. 41 mmol/l (125 mg/dl) Triglycerides: 2, 3 <1. 7 mmol/l (150 mg/dl) Total cholesterol: 5. 6 mmol/l (218 mg/dl) Total cholesterol: 2 <5. 2 mmol/l (200 mg/dl) e. GFR: 85 ml/min/1. 73 m 2 e. GFR: 5 ≥ 90 ml/min/1. 73 m 2 UACR: 28 mg/g UACR: 5 <30 mg/g Random plasma glucose: 11. 9 mmol/l (215 mg/dl) Random plasma glucose: 1 <11. 1 mmol/l (200 mg/dl) Management considerations • You confirm that Robert has T 2 D and you call to inform him immediately to discuss treatment options *Fasting defined as no caloric intake for at least 8 h 1 FPG, fasting plasma glucose; PCP, primary care physician 1. American Diabetes Association. Diabetes Care 2021; 44: S 1; 2. Centers for Disease Control and Prevention. Getting your cholesterol checked. 2020. https: //www. cdc. gov/ (accessed Jan 2021); 3. Mach F et al. Eur Heart J 2020; 41: 111; 4. Cosentino F et al. Eur Heart J 2020; 41: 255; 5. Kidney Disease: Improving Global Outcomes (KDIGO) Diabetes Work Group. Kidney Int 2020; 98: S 1 9
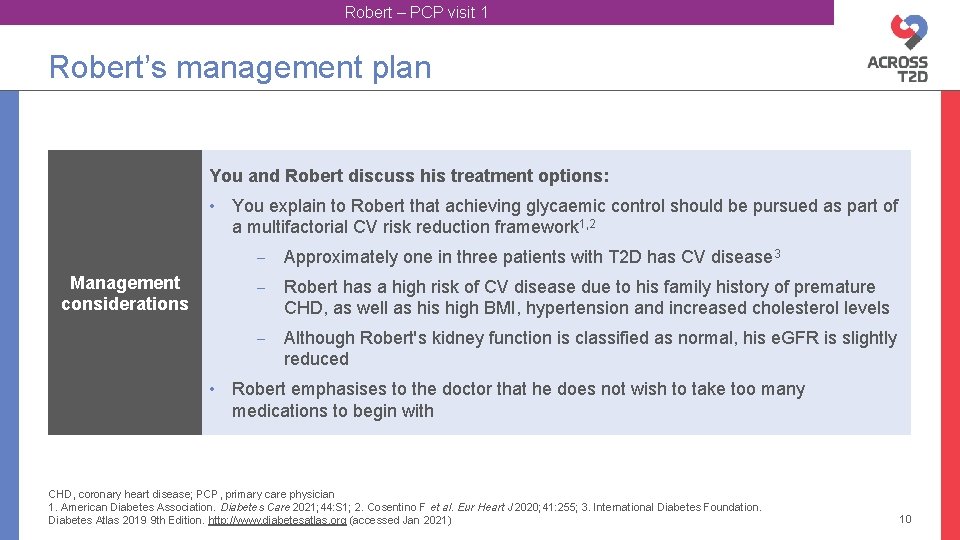
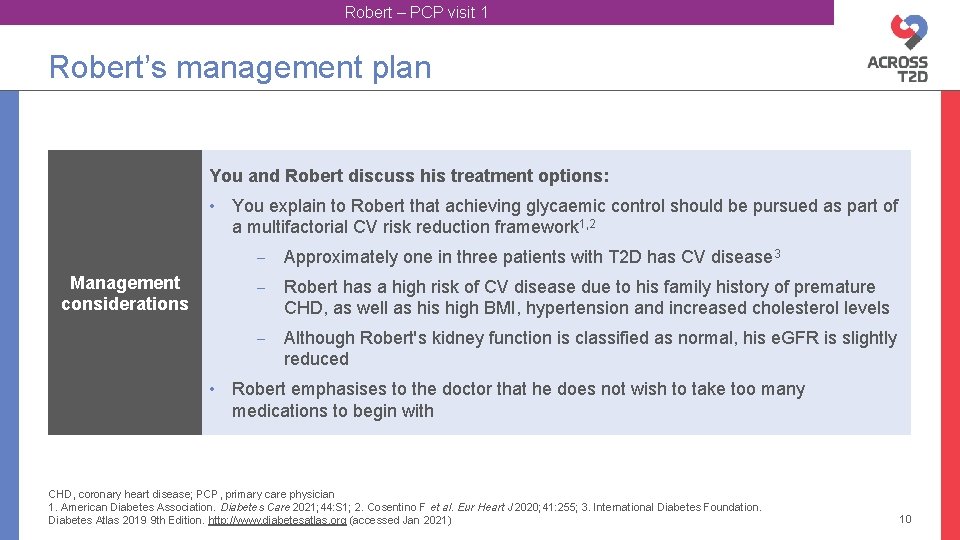
Robert – PCP visit 1 Robert’s management plan You and Robert discuss his treatment options: • You explain to Robert that achieving glycaemic control should be pursued as part of a multifactorial CV risk reduction framework 1, 2 ‒ Approximately one in three patients with T 2 D has CV disease 3 Management considerations ‒ Robert has a high risk of CV disease due to his family history of premature CHD, as well as high BMI, hypertension and increased cholesterol levels ‒ Although Robert's kidney function is classified as normal, his e. GFR is slightly reduced • Robert emphasises to the doctor that he does not wish to take too many medications to begin with CHD, coronary heart disease; PCP, primary care physician 1. American Diabetes Association. Diabetes Care 2021; 44: S 1; 2. Cosentino F et al. Eur Heart J 2020; 41: 255; 3. International Diabetes Foundation. Diabetes Atlas 2019 9 th Edition. http: //www. diabetesatlas. org (accessed Jan 2021) 10
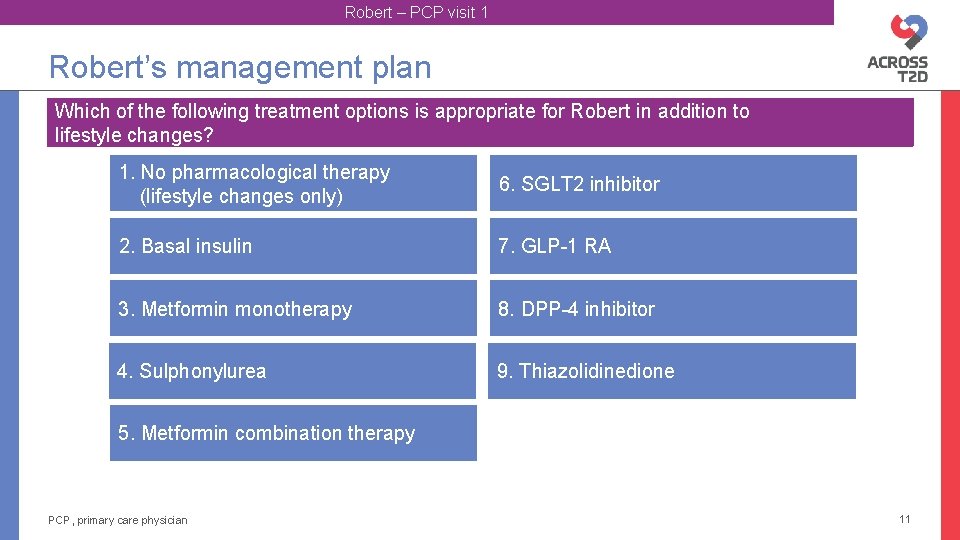
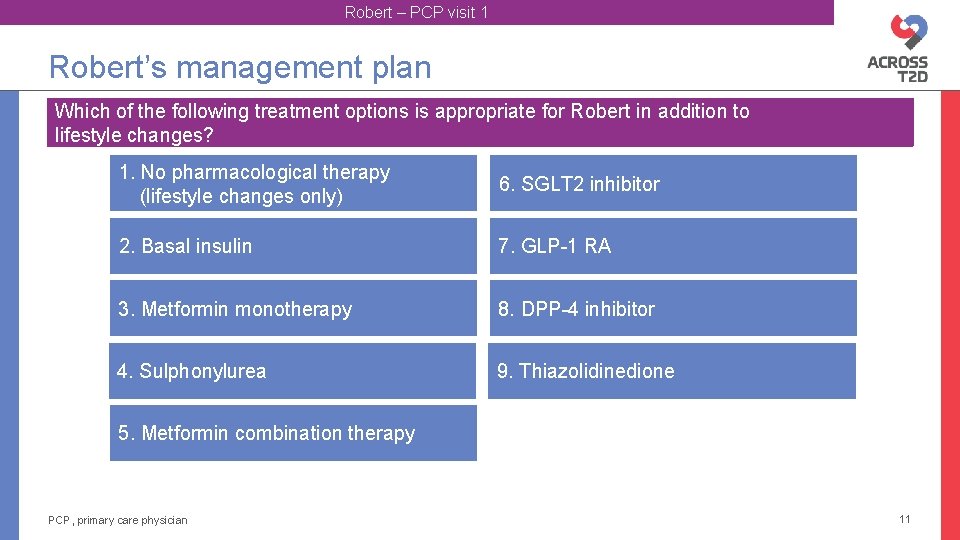
Robert – PCP visit 1 Robert’s management plan Which of the following treatment options is appropriate for Robert in addition to lifestyle changes? 1. No pharmacological therapy (lifestyle changes only) 6. SGLT 2 inhibitor 2. Basal insulin 7. GLP-1 RA 3. Metformin monotherapy 8. DPP-4 inhibitor 4. Sulphonylurea 9. Thiazolidinedione 5. Metformin combination therapy PCP, primary care physician 11
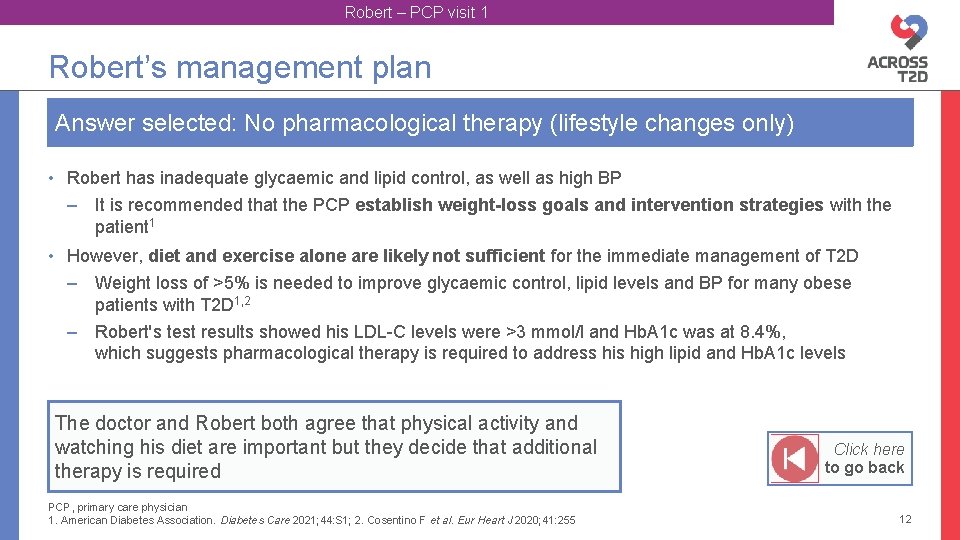
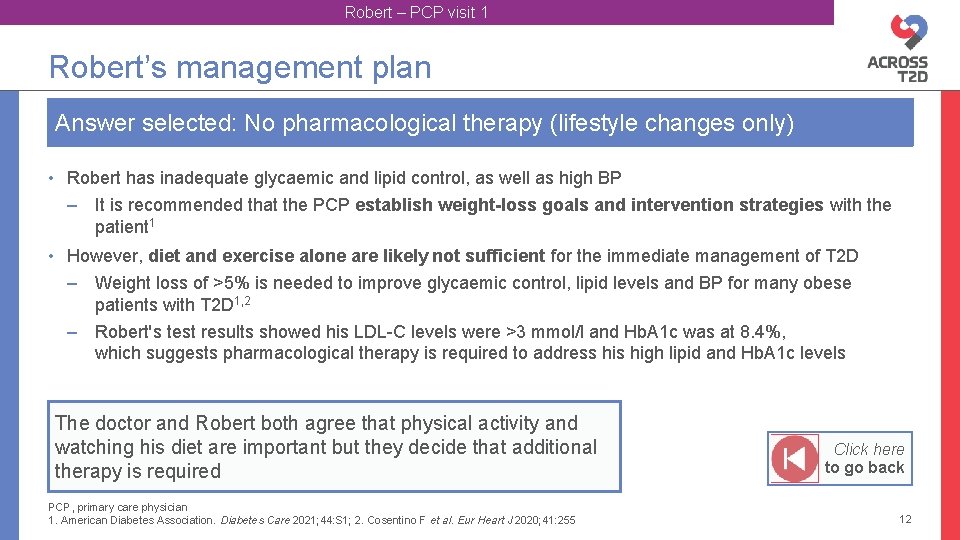
Robert – PCP visit 1 Robert’s management plan Answer selected: No pharmacological therapy (lifestyle changes only) • Robert has inadequate glycaemic and lipid control, as well as high BP – It is recommended that the PCP establish weight-loss goals and intervention strategies with the patient 1 • However, diet and exercise alone are likely not sufficient for the immediate management of T 2 D – Weight loss of >5% is needed to improve glycaemic control, lipid levels and BP for many obese patients with T 2 D 1, 2 – Robert's test results showed his LDL-C levels were >3 mmol/l and Hb. A 1 c was at 8. 4%, which suggests pharmacological therapy is required to address high lipid and Hb. A 1 c levels The doctor and Robert both agree that physical activity and watching his diet are important but they decide that additional therapy is required PCP, primary care physician 1. American Diabetes Association. Diabetes Care 2021; 44: S 1; 2. Cosentino F et al. Eur Heart J 2020; 41: 255 Click here to go back 12
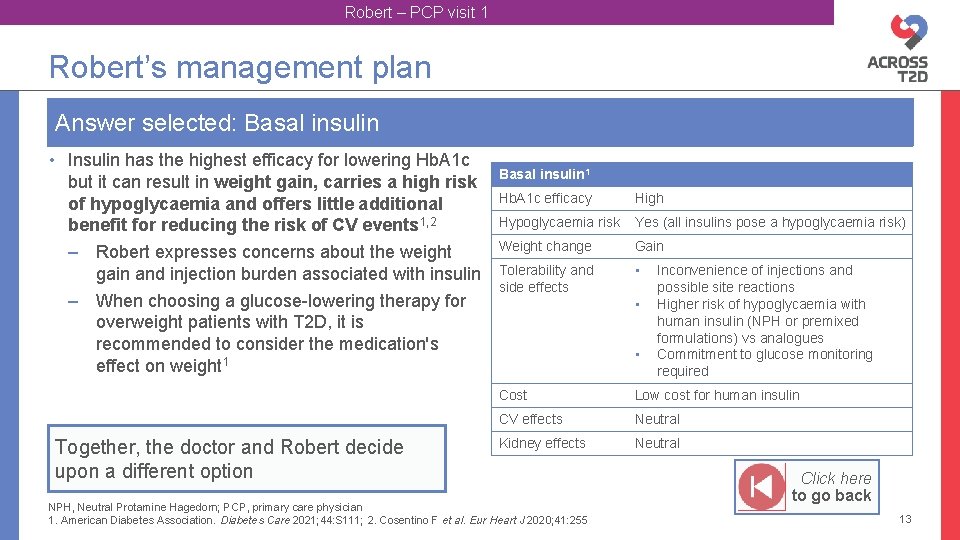
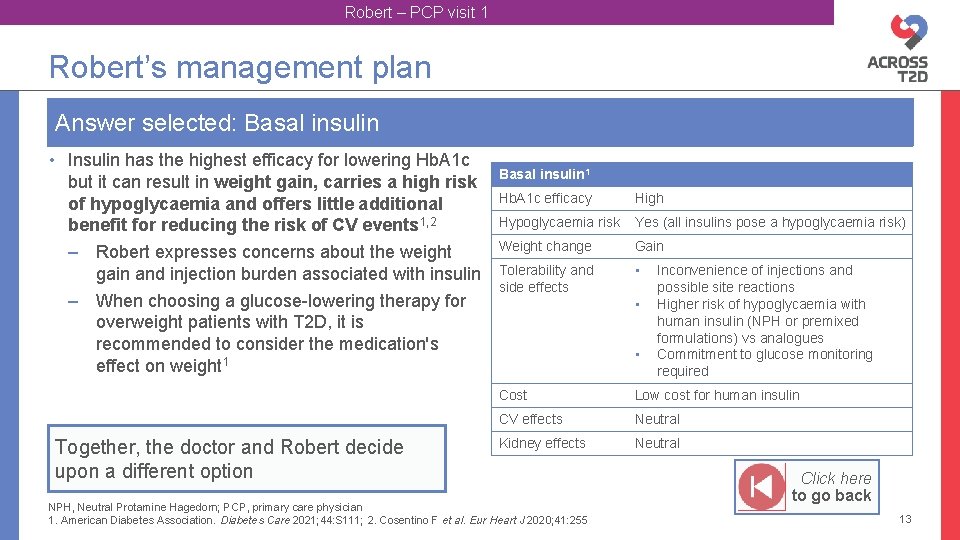
Robert – PCP visit 1 Robert’s management plan Answer selected: Basal insulin • Insulin has the highest efficacy for lowering Hb. A 1 c but it can result in weight gain, carries a high risk of hypoglycaemia and offers little additional benefit for reducing the risk of CV events 1, 2 – Robert expresses concerns about the weight gain and injection burden associated with insulin – When choosing a glucose-lowering therapy for overweight patients with T 2 D, it is recommended to consider the medication's effect on weight 1 Together, the doctor and Robert decide upon a different option Basal insulin 1 Hb. A 1 c efficacy High Hypoglycaemia risk Yes (all insulins pose a hypoglycaemia risk) Weight change Gain Tolerability and side effects • • • Inconvenience of injections and possible site reactions Higher risk of hypoglycaemia with human insulin (NPH or premixed formulations) vs analogues Commitment to glucose monitoring required Cost Low cost for human insulin CV effects Neutral Kidney effects Neutral NPH, Neutral Protamine Hagedorn; PCP, primary care physician 1. American Diabetes Association. Diabetes Care 2021; 44: S 111; 2. Cosentino F et al. Eur Heart J 2020; 41: 255 Click here to go back 13
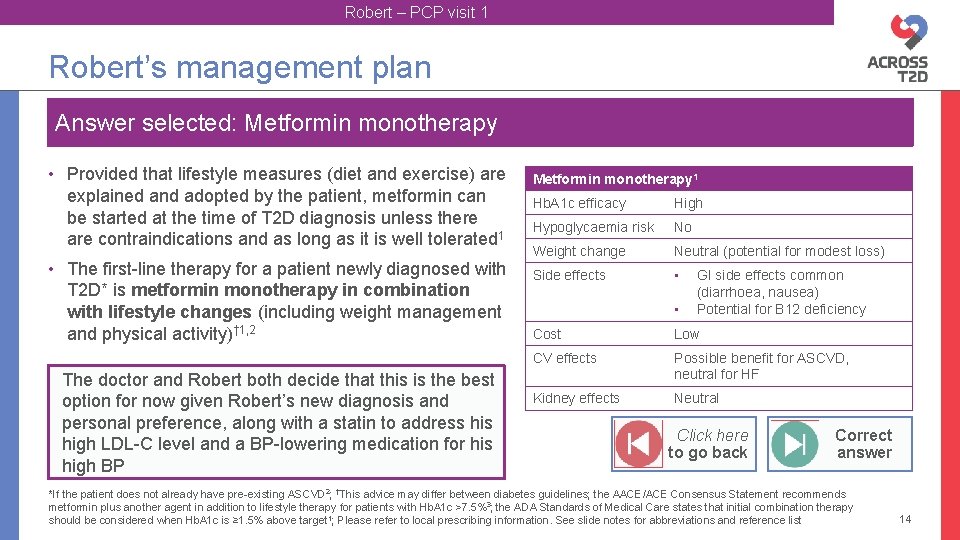
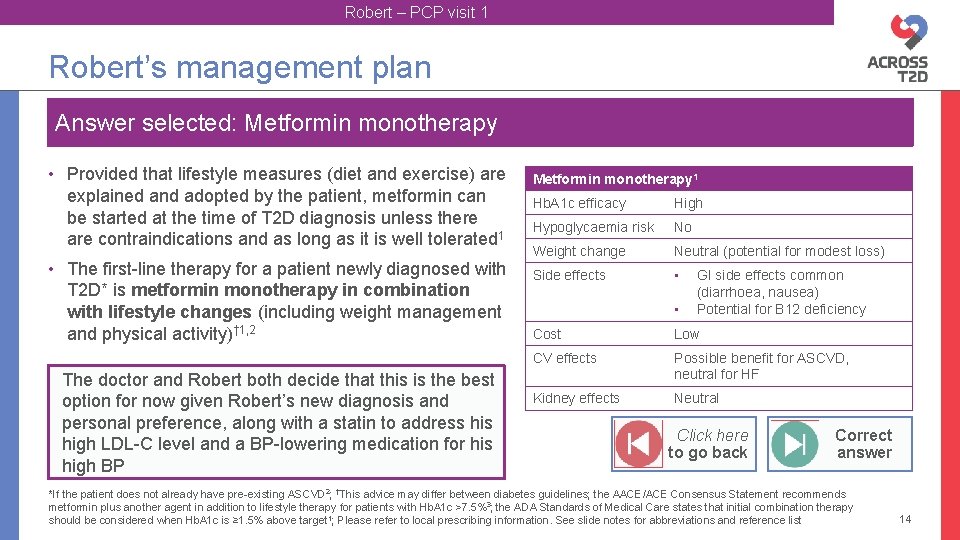
Robert – PCP visit 1 Robert’s management plan Answer selected: Metformin monotherapy • Provided that lifestyle measures (diet and exercise) are explained and adopted by the patient, metformin can be started at the time of T 2 D diagnosis unless there are contraindications and as long as it is well tolerated 1 • The first-line therapy for a patient newly diagnosed with T 2 D* is metformin monotherapy in combination with lifestyle changes (including weight management and physical activity)† 1, 2 The doctor and Robert both decide that this is the best option for now given Robert’s new diagnosis and personal preference, along with a statin to address high LDL-C level and a BP-lowering medication for his high BP Metformin monotherapy 1 Hb. A 1 c efficacy High Hypoglycaemia risk No Weight change Neutral (potential for modest loss) Side effects • • GI side effects common (diarrhoea, nausea) Potential for B 12 deficiency Cost Low CV effects Possible benefit for ASCVD, neutral for HF Kidney effects Neutral Click here to go back Correct answer *If the patient does not already have pre-existing ASCVD 2; †This advice may differ between diabetes guidelines; the AACE/ACE Consensus Statement recommends metformin plus another agent in addition to lifestyle therapy for patients with Hb. A 1 c >7. 5%3; the ADA Standards of Medical Care states that initial combination therapy should be considered when Hb. A 1 c is ≥ 1. 5% above target 1; Please refer to local prescribing information. See slide notes for abbreviations and reference list 14
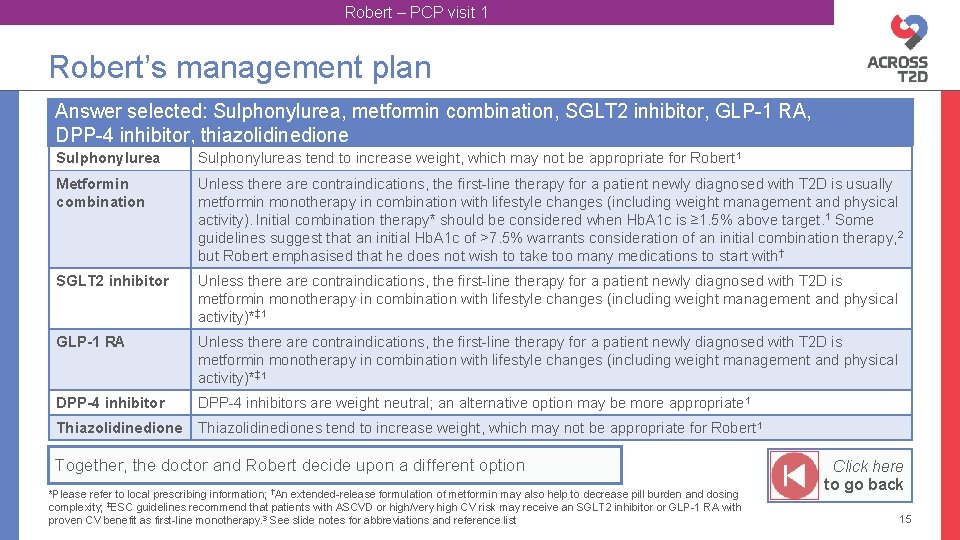
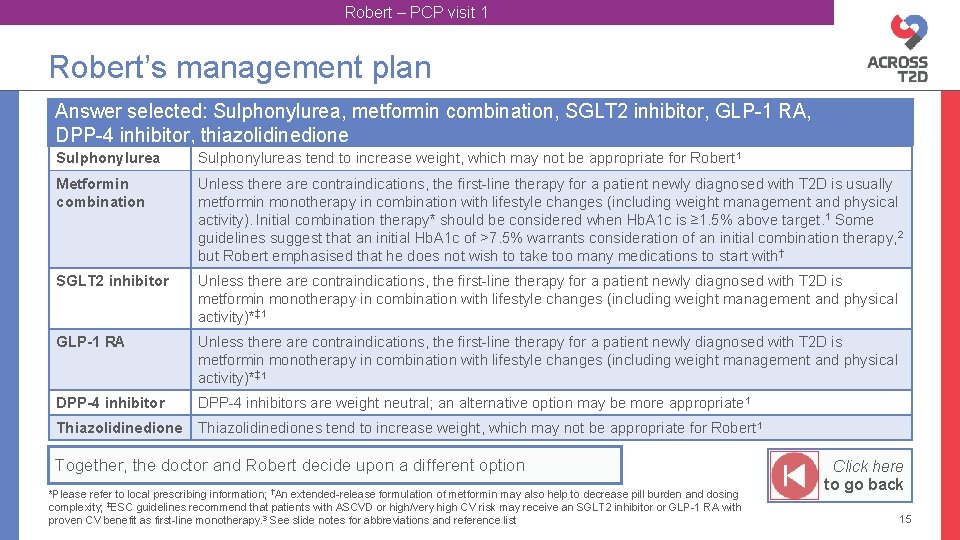
Robert – PCP visit 1 Robert’s management plan Answer selected: Sulphonylurea, metformin combination, SGLT 2 inhibitor, GLP-1 RA, DPP-4 inhibitor, thiazolidinedione Sulphonylureas tend to increase weight, which may not be appropriate for Robert 1 Metformin combination Unless there are contraindications, the first-line therapy for a patient newly diagnosed with T 2 D is usually metformin monotherapy in combination with lifestyle changes (including weight management and physical activity). Initial combination therapy* should be considered when Hb. A 1 c is ≥ 1. 5% above target. 1 Some guidelines suggest that an initial Hb. A 1 c of >7. 5% warrants consideration of an initial combination therapy, 2 but Robert emphasised that he does not wish to take too many medications to start with† SGLT 2 inhibitor Unless there are contraindications, the first-line therapy for a patient newly diagnosed with T 2 D is metformin monotherapy in combination with lifestyle changes (including weight management and physical activity)*‡ 1 GLP-1 RA Unless there are contraindications, the first-line therapy for a patient newly diagnosed with T 2 D is metformin monotherapy in combination with lifestyle changes (including weight management and physical activity)*‡ 1 DPP-4 inhibitors are weight neutral; an alternative option may be more appropriate 1 Thiazolidinediones tend to increase weight, which may not be appropriate for Robert 1 Together, the doctor and Robert decide upon a different option *Please refer to local prescribing information; †An extended-release formulation of metformin may also help to decrease pill burden and dosing complexity; ‡ESC guidelines recommend that patients with ASCVD or high/very high CV risk may receive an SGLT 2 inhibitor or GLP-1 RA with proven CV benefit as first-line monotherapy. 3 See slide notes for abbreviations and reference list Click here to go back 15
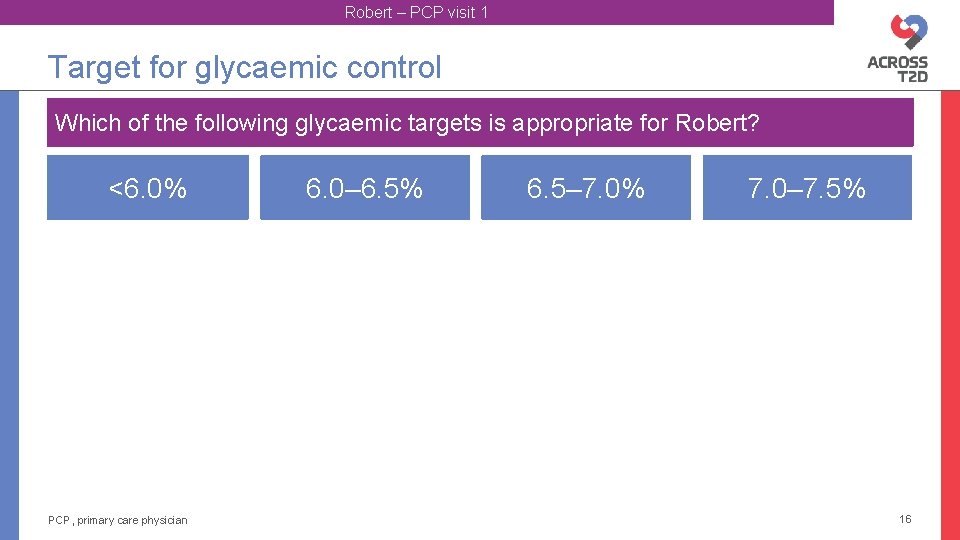
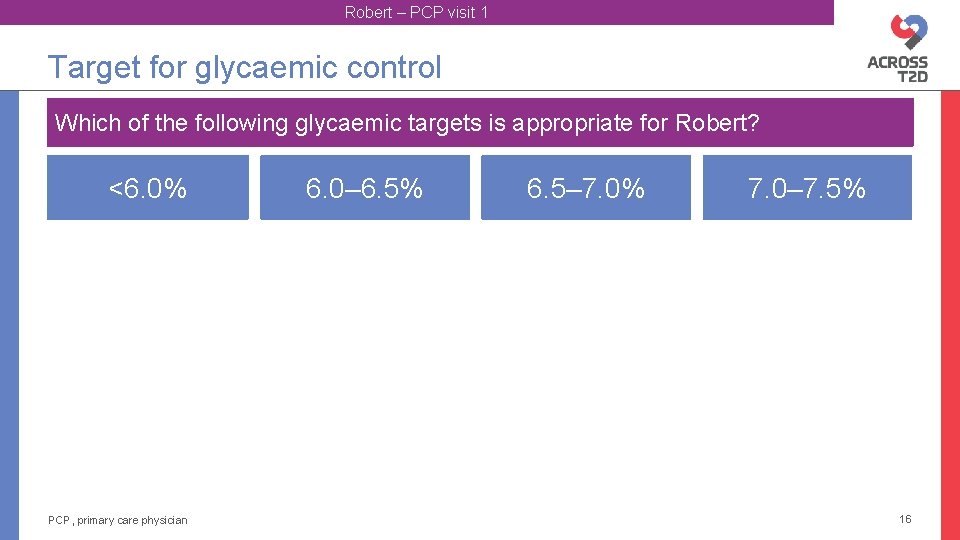
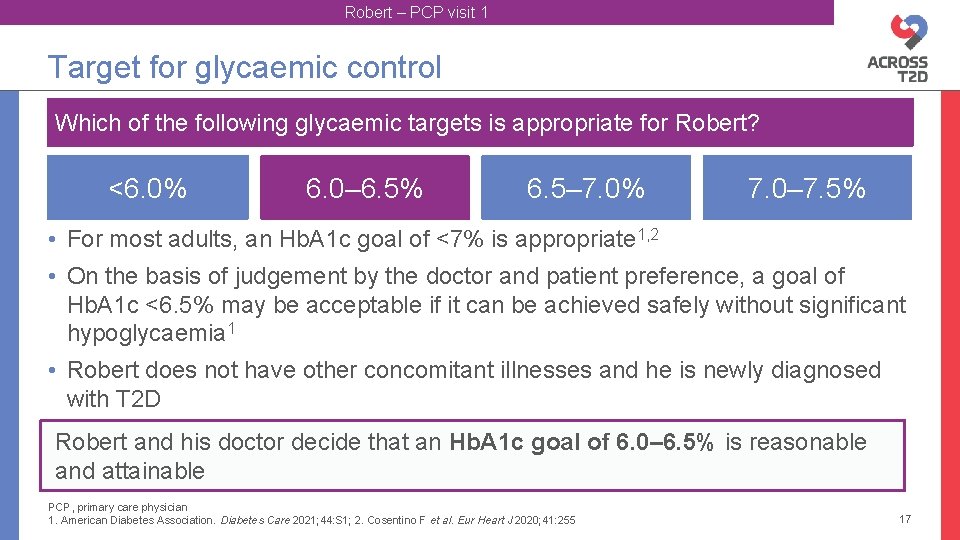
Robert – PCP visit 1 Target for glycaemic control Which of the following glycaemic targets is appropriate for Robert? <6. 0% PCP, primary care physician 6. 0– 6. 5% 6. 5– 7. 0% 7. 0– 7. 5% 16
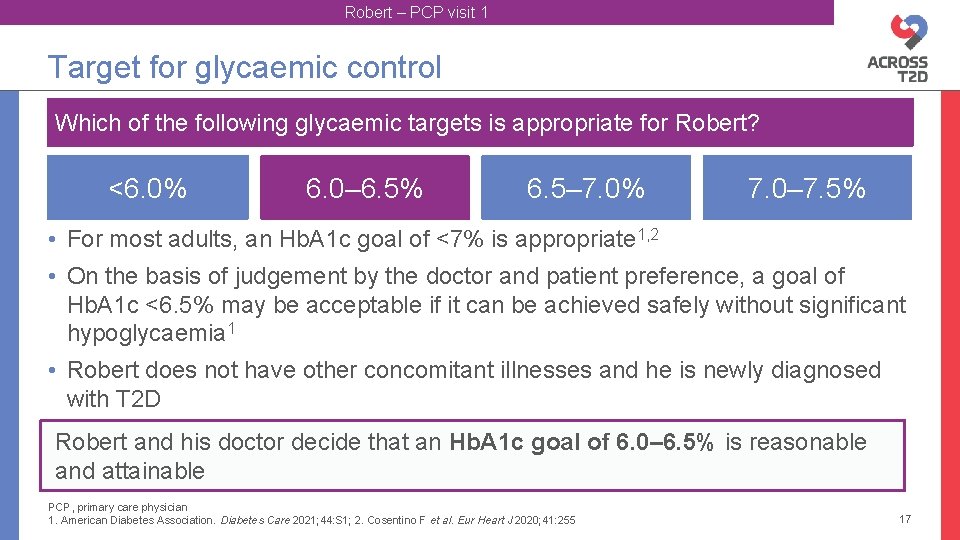
Robert – PCP visit 1 Target for glycaemic control Which of the following glycaemic targets is appropriate for Robert? <6. 0% 6. 0– 6. 5% 6. 5– 7. 0% 7. 0– 7. 5% • For most adults, an Hb. A 1 c goal of <7% is appropriate 1, 2 • On the basis of judgement by the doctor and patient preference, a goal of Hb. A 1 c <6. 5% may be acceptable if it can be achieved safely without significant hypoglycaemia 1 • Robert does not have other concomitant illnesses and he is newly diagnosed with T 2 D Robert and his doctor decide that an Hb. A 1 c goal of 6. 0– 6. 5% is reasonable and attainable PCP, primary care physician 1. American Diabetes Association. Diabetes Care 2021; 44: S 1; 2. Cosentino F et al. Eur Heart J 2020; 41: 255 17
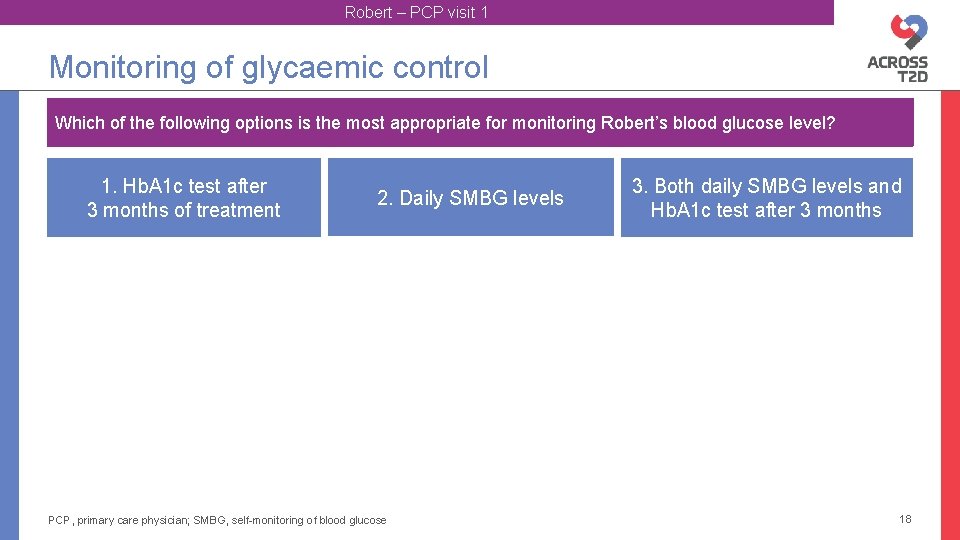
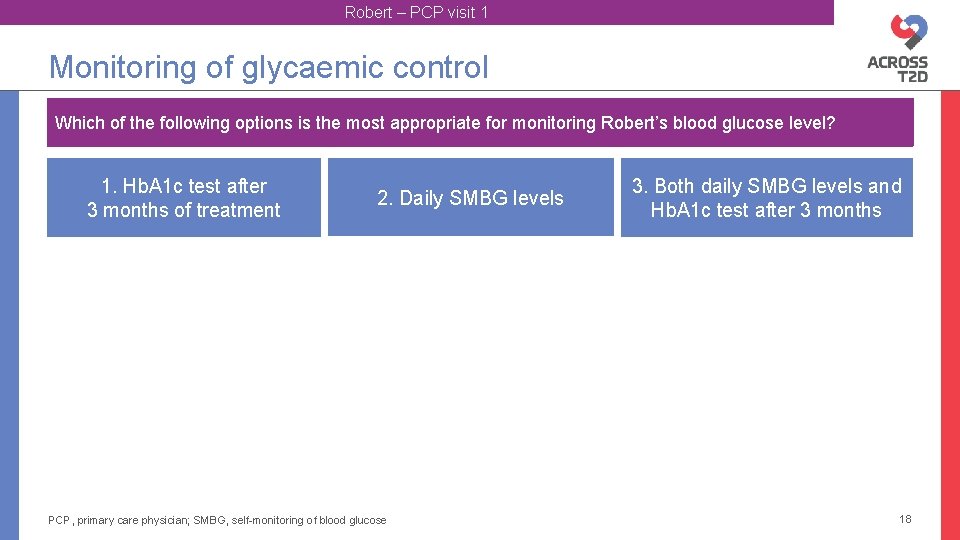
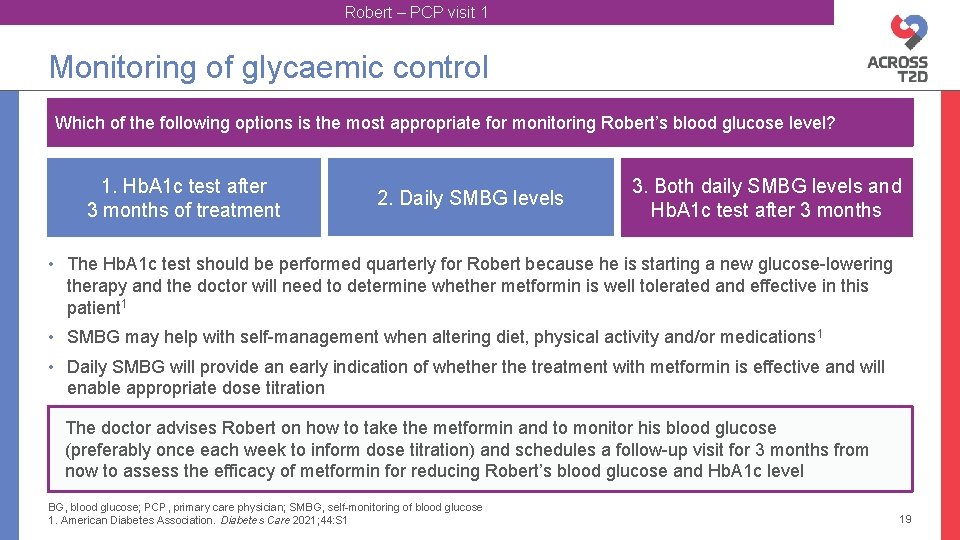
Robert – PCP visit 1 Monitoring of glycaemic control Which of the following options is the most appropriate for monitoring Robert’s blood glucose level? 1. Hb. A 1 c test after 3 months of treatment 2. Daily SMBG levels PCP, primary care physician; SMBG, self-monitoring of blood glucose 3. Both daily SMBG levels and Hb. A 1 c test after 3 months 18
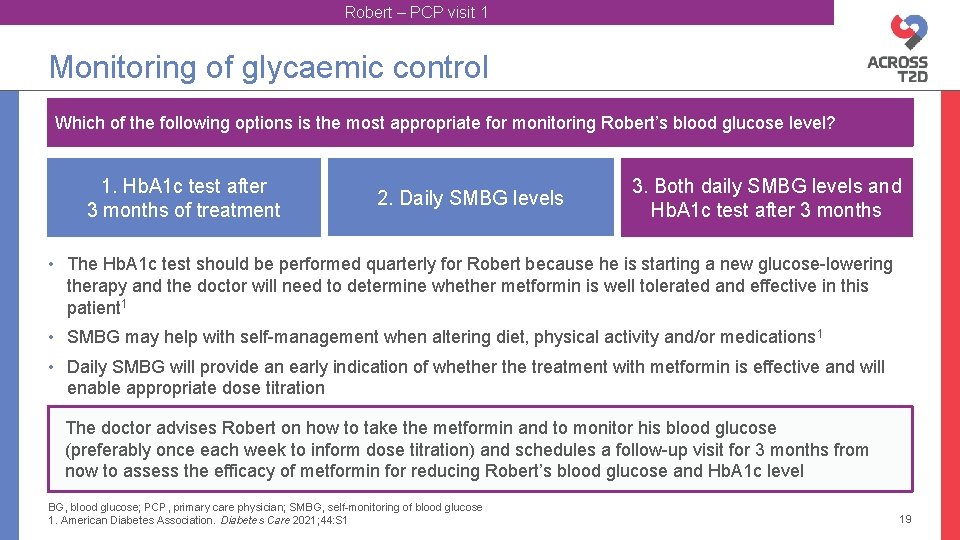
Robert – PCP visit 1 Monitoring of glycaemic control Which of the following options is the most appropriate for monitoring Robert’s blood glucose level? 1. Hb. A 1 c test after 3 months of treatment 2. Daily SMBG levels 3. Both daily SMBG levels and Hb. A 1 c test after 3 months • The Hb. A 1 c test should be performed quarterly for Robert because he is starting a new glucose-lowering therapy and the doctor will need to determine whether metformin is well tolerated and effective in this patient 1 • SMBG may help with self-management when altering diet, physical activity and/or medications 1 • Daily SMBG will provide an early indication of whether the treatment with metformin is effective and will enable appropriate dose titration The doctor advises Robert on how to take the metformin and to monitor his blood glucose (preferably once each week to inform dose titration) and schedules a follow-up visit for 3 months from now to assess the efficacy of metformin for reducing Robert’s blood glucose and Hb. A 1 c level BG, blood glucose; PCP, primary care physician; SMBG, self-monitoring of blood glucose 1. American Diabetes Association. Diabetes Care 2021; 44: S 1 19
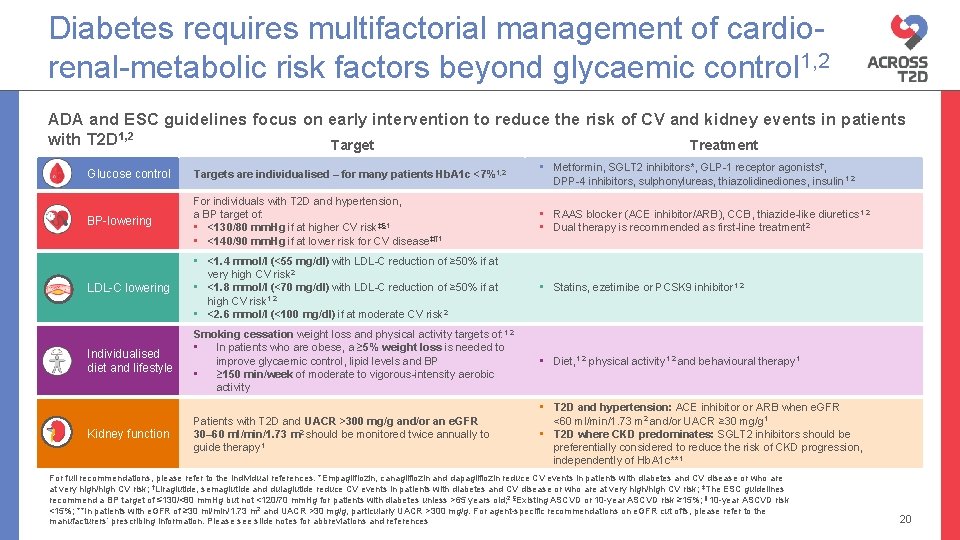
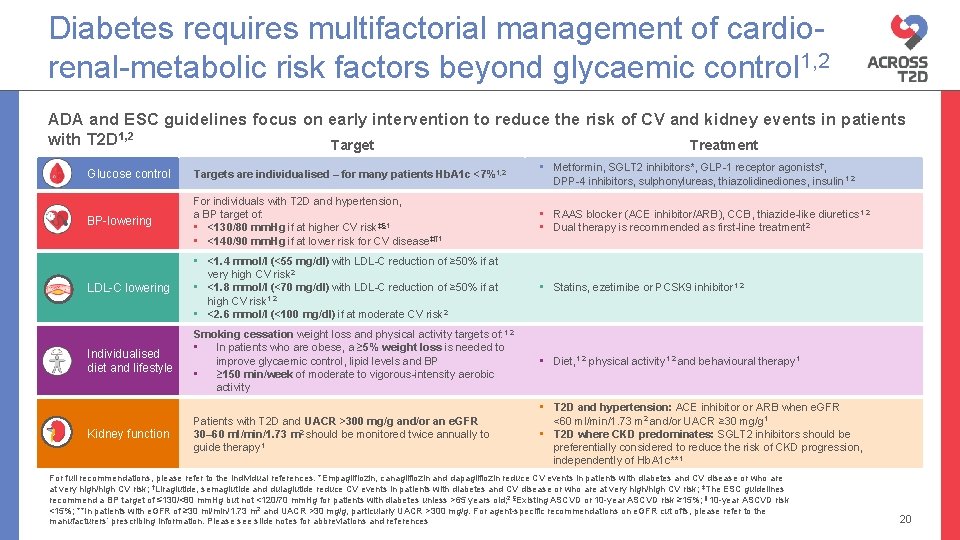
Diabetes requires multifactorial management of cardiorenal-metabolic risk factors beyond glycaemic control 1, 2 ADA and ESC guidelines focus on early intervention to reduce the risk of CV and kidney events in patients with T 2 D 1, 2 Target Treatment Glucose control Targets are individualised – for many patients Hb. A 1 c <7%1, 2 • Metformin, SGLT 2 inhibitors*, GLP-1 receptor agonists†, DPP-4 inhibitors, sulphonylureas, thiazolidinediones, insulin 1, 2 BP-lowering For individuals with T 2 D and hypertension, a BP target of: • <130/80 mm. Hg if at higher CV risk‡§ 1 • <140/90 mm. Hg if at lower risk for CV disease‡¶ 1 • RAAS blocker (ACE inhibitor/ARB), CCB, thiazide-like diuretics 1, 2 • Dual therapy is recommended as first-line treatment 2 LDL-C lowering • <1. 4 mmol/l (<55 mg/dl) with LDL-C reduction of ≥ 50% if at very high CV risk 2 • <1. 8 mmol/l (<70 mg/dl) with LDL-C reduction of ≥ 50% if at high CV risk 1, 2 • <2. 6 mmol/l (<100 mg/dl) if at moderate CV risk 2 • Statins, ezetimibe or PCSK 9 inhibitor 1, 2 Individualised diet and lifestyle Smoking cessation weight loss and physical activity targets of: 1, 2 • In patients who are obese, a ≥ 5% weight loss is needed to improve glycaemic control, lipid levels and BP • ≥ 150 min/week of moderate to vigorous-intensity aerobic activity • Diet, 1, 2 physical activity 1, 2 and behavioural therapy 1 Patients with T 2 D and UACR >300 mg/g and/or an e. GFR 30– 60 ml/min/1. 73 m 2 should be monitored twice annually to guide therapy 1 • T 2 D and hypertension: ACE inhibitor or ARB when e. GFR <60 ml/min/1. 73 m 2 and/or UACR ≥ 30 mg/g 1 • T 2 D where CKD predominates: SGLT 2 inhibitors should be preferentially considered to reduce the risk of CKD progression, independently of Hb. A 1 c**1 Kidney function For full recommendations, please refer to the individual references. *Empagliflozin, canagliflozin and dapagliflozin reduce CV events in patients with diabetes and CV disease or who are at very high/high CV risk; †Liraglutide, semaglutide and dulaglutide reduce CV events in patients with diabetes and CV disease or who are at very high/high CV risk; ‡The ESC guidelines recommend a BP target of ≤ 130/<80 mm. Hg but not <120/70 mm. Hg for patients with diabetes unless >65 years old; 2 §Existing ASCVD or 10 -year ASCVD risk ≥ 15%; ¶ 10 -year ASCVD risk <15%; **In patients with e. GFR of ≥ 30 ml/min/1. 73 m 2 and UACR >30 mg/g, particularly UACR >300 mg/g. For agent-specific recommendations on e. GFR cut offs, please refer to the manufacturers’ prescribing information. Please see slide notes for abbreviations and references 20
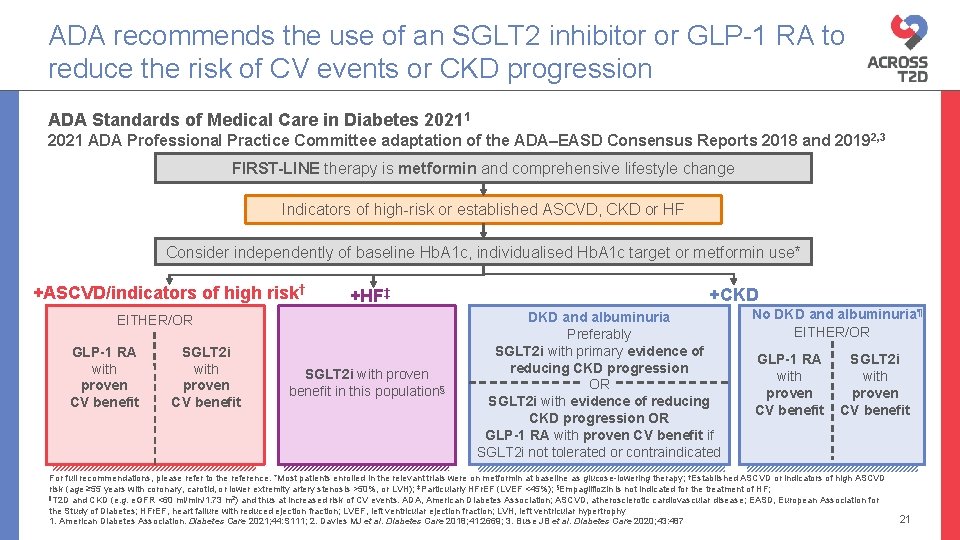
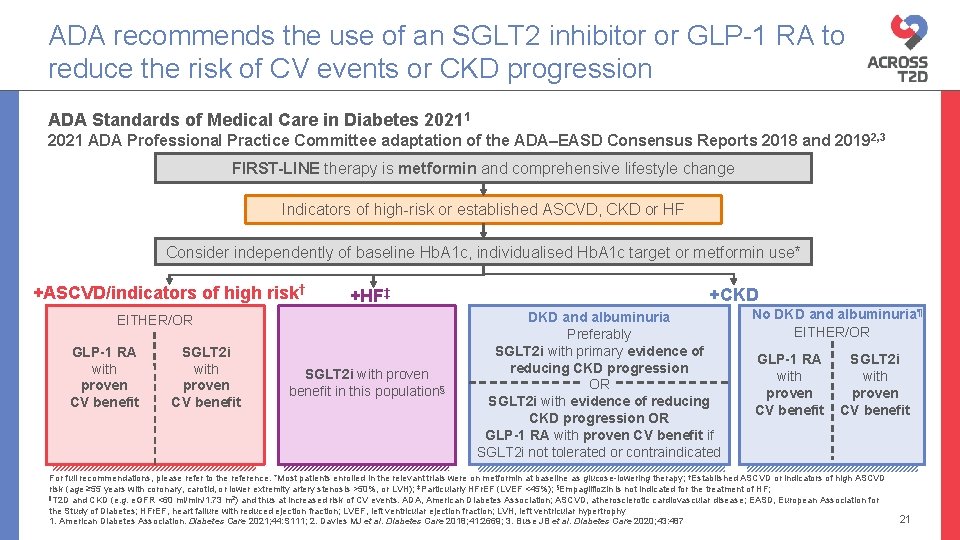
ADA recommends the use of an SGLT 2 inhibitor or GLP-1 RA to reduce the risk of CV events or CKD progression ADA Standards of Medical Care in Diabetes 20211 2021 ADA Professional Practice Committee adaptation of the ADA–EASD Consensus Reports 2018 and 2019 2, 3 FIRST-LINE therapy is metformin and comprehensive lifestyle change Indicators of high-risk or established ASCVD, CKD or HF Consider independently of baseline Hb. A 1 c, individualised Hb. A 1 c target or metformin use* +ASCVD/indicators of high risk† +HF‡ EITHER/OR GLP-1 RA with proven CV benefit SGLT 2 i with proven benefit in this population§ +CKD DKD and albuminuria Preferably SGLT 2 i with primary evidence of reducing CKD progression OR SGLT 2 i with evidence of reducing CKD progression OR GLP-1 RA with proven CV benefit if SGLT 2 i not tolerated or contraindicated No DKD and albuminuria¶ EITHER/OR GLP-1 RA with proven CV benefit SGLT 2 i with proven CV benefit For full recommendations, please refer to the reference. *Most patients enrolled in the relevant trials were on metformin at baseline as glucose-lowering therapy; †Established ASCVD or indicators of high ASCVD risk (age ≥ 55 years with coronary, carotid, or lower extremity artery stenosis >50%, or LVH); ‡Particularly HFr. EF (LVEF <45%); §Empagliflozin is not indicated for the treatment of HF; ¶T 2 D and CKD (e. g. e. GFR <60 ml/min/1. 73 m 2) and thus at increased risk of CV events. ADA, American Diabetes Association; ASCVD, atherosclerotic cardiovascular disease; EASD, European Association for the Study of Diabetes; HFr. EF, heart failure with reduced ejection fraction; LVEF, left ventricular ejection fraction; LVH, left ventricular hypertrophy 1. American Diabetes Association. Diabetes Care 2021; 44: S 111; 2. Davies MJ et al. Diabetes Care 2018; 41: 2669; 3. Buse JB et al. Diabetes Care 2020; 43: 487 21
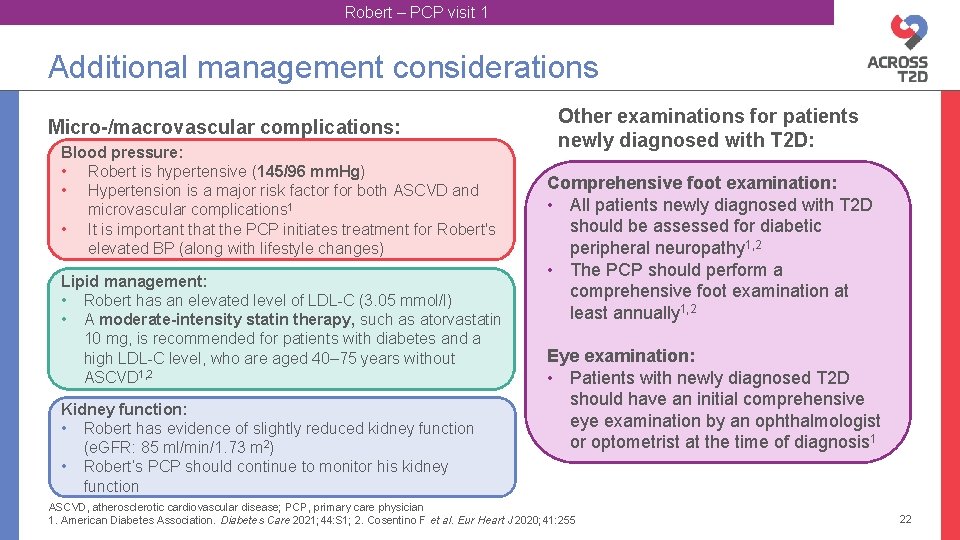
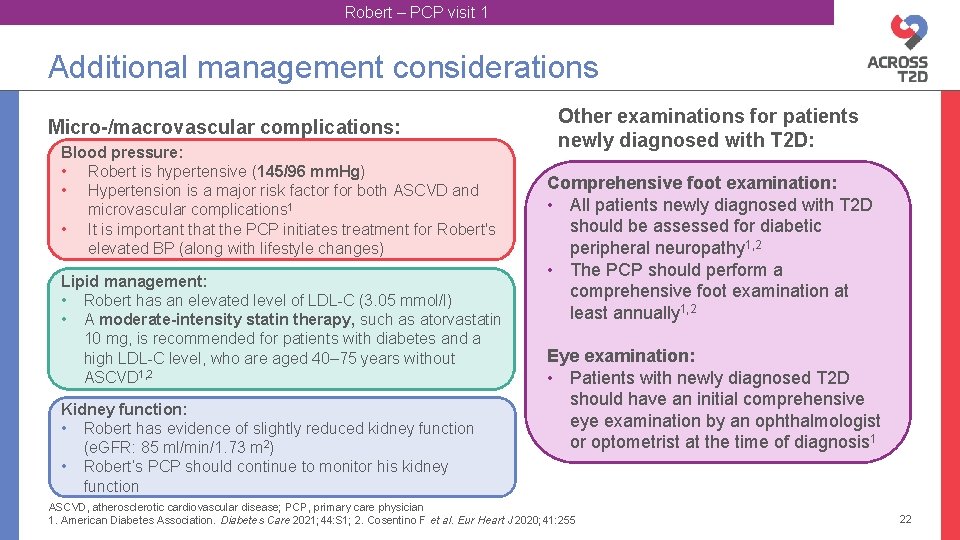
Robert – PCP visit 1 Additional management considerations Micro-/macrovascular complications: Blood pressure: • Robert is hypertensive (145/96 mm. Hg) • Hypertension is a major risk factor for both ASCVD and microvascular complications 1 • It is important that the PCP initiates treatment for Robert's elevated BP (along with lifestyle changes) Lipid management: • Robert has an elevated level of LDL-C (3. 05 mmol/l) • A moderate-intensity statin therapy, such as atorvastatin 10 mg, is recommended for patients with diabetes and a high LDL-C level, who are aged 40– 75 years without ASCVD 1, 2 Kidney function: • Robert has evidence of slightly reduced kidney function (e. GFR: 85 ml/min/1. 73 m 2) • Robert’s PCP should continue to monitor his kidney function Other examinations for patients newly diagnosed with T 2 D: Comprehensive foot examination: • All patients newly diagnosed with T 2 D should be assessed for diabetic peripheral neuropathy 1, 2 • The PCP should perform a comprehensive foot examination at least annually 1, 2 Eye examination: • Patients with newly diagnosed T 2 D should have an initial comprehensive eye examination by an ophthalmologist or optometrist at the time of diagnosis 1 ASCVD, atherosclerotic cardiovascular disease; PCP, primary care physician 1. American Diabetes Association. Diabetes Care 2021; 44: S 1; 2. Cosentino F et al. Eur Heart J 2020; 41: 255 22
Robert – PCP visit 2 Robert – 3 months later… Robert has returned for his 3 -month follow-up appointment at the clinic. You review his blood glucose control and overall diabetes care. PCP, primary care physician 23
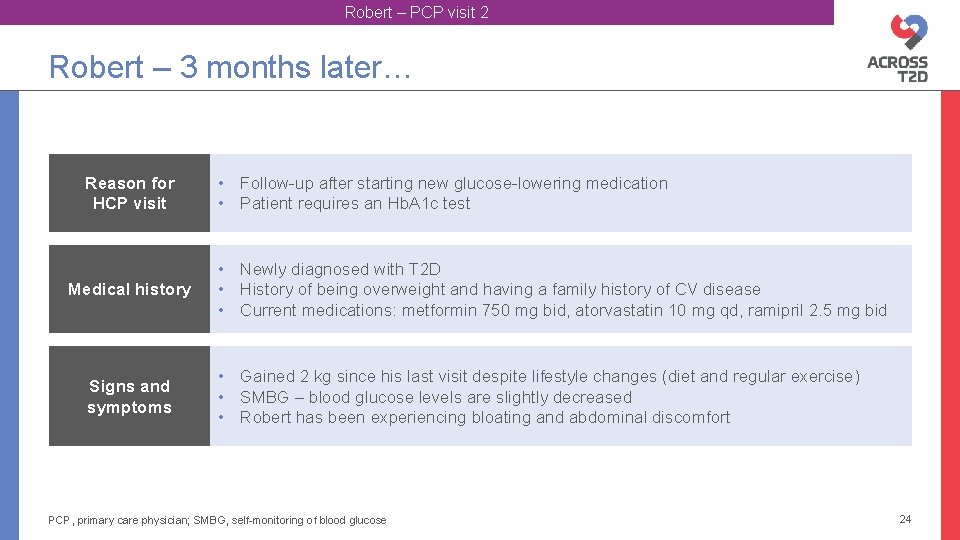
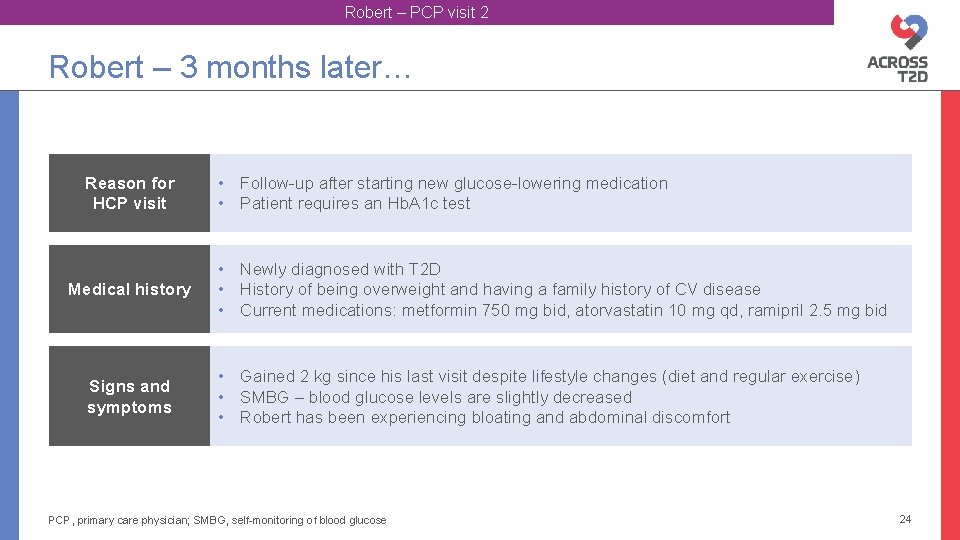
Robert – PCP visit 2 Robert – 3 months later… Reason for HCP visit Medical history Signs and symptoms • Follow-up after starting new glucose-lowering medication • Patient requires an Hb. A 1 c test • Newly diagnosed with T 2 D • History of being overweight and having a family history of CV disease • Current medications: metformin 750 mg bid, atorvastatin 10 mg qd, ramipril 2. 5 mg bid • Gained 2 kg since his last visit despite lifestyle changes (diet and regular exercise) • SMBG – blood glucose levels are slightly decreased • Robert has been experiencing bloating and abdominal discomfort PCP, primary care physician; SMBG, self-monitoring of blood glucose 24
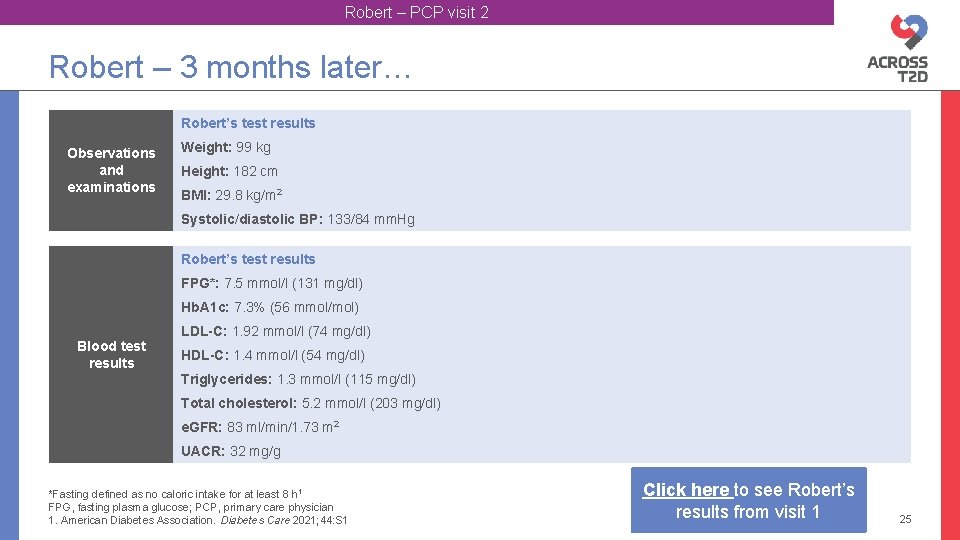
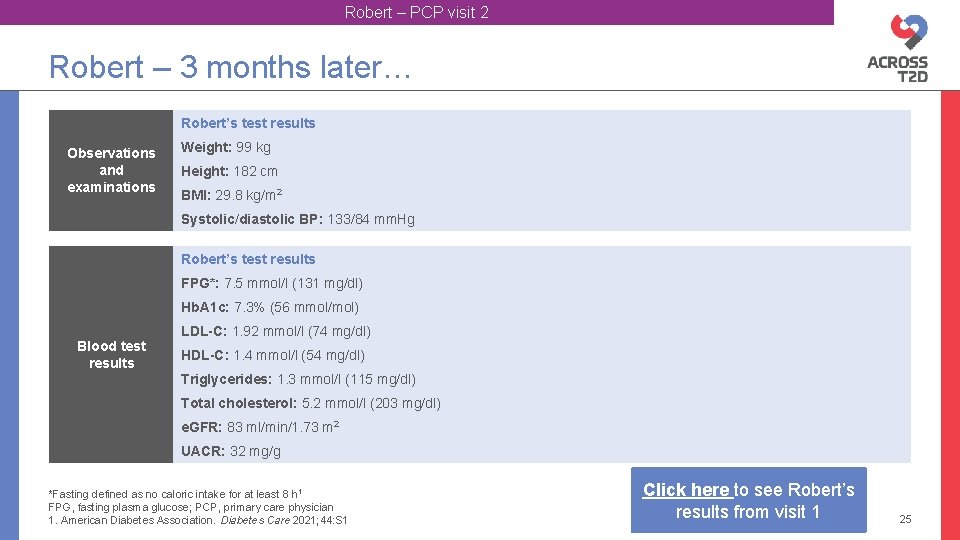
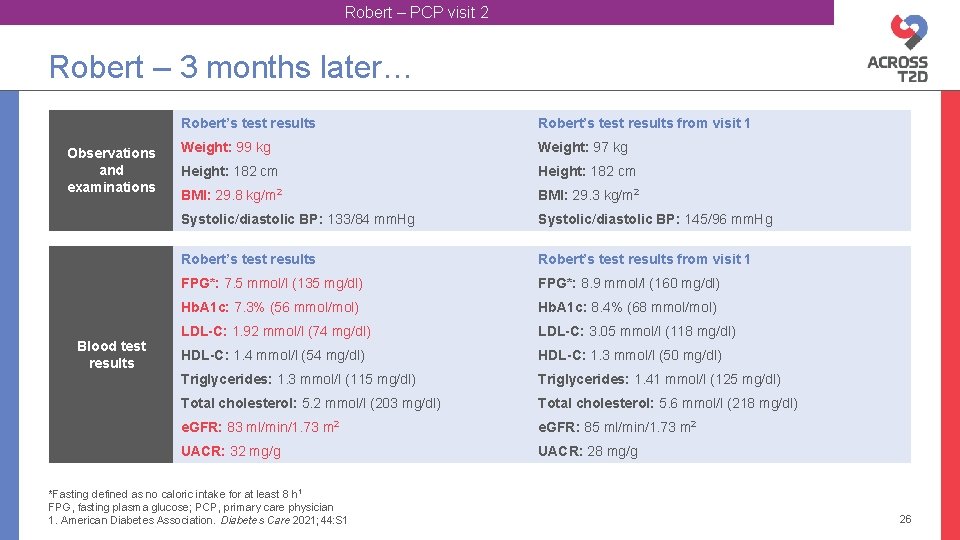
Robert – PCP visit 2 Robert – 3 months later… Robert’s test results Observations and examinations Weight: 99 kg Height: 182 cm BMI: 29. 8 kg/m 2 Systolic/diastolic BP: 133/84 mm. Hg Robert’s test results FPG*: 7. 5 mmol/l (131 mg/dl) Hb. A 1 c: 7. 3% (56 mmol/mol) LDL-C: 1. 92 mmol/l (74 mg/dl) Blood test results HDL-C: 1. 4 mmol/l (54 mg/dl) Triglycerides: 1. 3 mmol/l (115 mg/dl) Total cholesterol: 5. 2 mmol/l (203 mg/dl) e. GFR: 83 ml/min/1. 73 m 2 UACR: 32 mg/g *Fasting defined as no caloric intake for at least 8 h 1 FPG, fasting plasma glucose; PCP, primary care physician 1. American Diabetes Association. Diabetes Care 2021; 44: S 1 Click here to see Robert’s results from visit 1 25
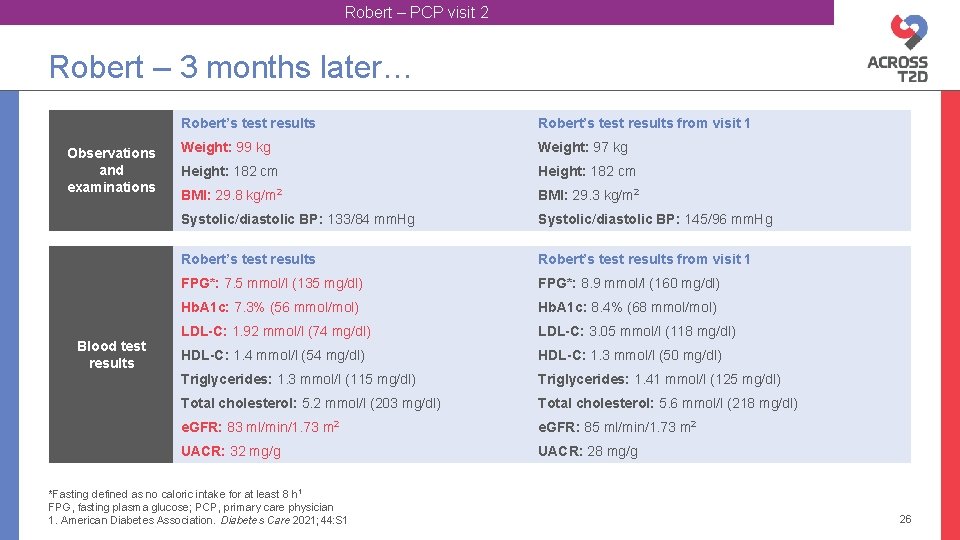
Robert – PCP visit 2 Robert – 3 months later… Observations and examinations Blood test results Robert’s test results from visit 1 Weight: 99 kg Weight: 97 kg Height: 182 cm BMI: 29. 8 kg/m 2 BMI: 29. 3 kg/m 2 Systolic/diastolic BP: 133/84 mm. Hg Systolic/diastolic BP: 145/96 mm. Hg Robert’s test results from visit 1 FPG*: 7. 5 mmol/l (135 mg/dl) FPG*: 8. 9 mmol/l (160 mg/dl) Hb. A 1 c: 7. 3% (56 mmol/mol) Hb. A 1 c: 8. 4% (68 mmol/mol) LDL-C: 1. 92 mmol/l (74 mg/dl) LDL-C: 3. 05 mmol/l (118 mg/dl) HDL-C: 1. 4 mmol/l (54 mg/dl) HDL-C: 1. 3 mmol/l (50 mg/dl) Triglycerides: 1. 3 mmol/l (115 mg/dl) Triglycerides: 1. 41 mmol/l (125 mg/dl) Total cholesterol: 5. 2 mmol/l (203 mg/dl) Total cholesterol: 5. 6 mmol/l (218 mg/dl) e. GFR: 83 ml/min/1. 73 m 2 e. GFR: 85 ml/min/1. 73 m 2 UACR: 32 mg/g UACR: 28 mg/g *Fasting defined as no caloric intake for at least 8 h 1 FPG, fasting plasma glucose; PCP, primary care physician 1. American Diabetes Association. Diabetes Care 2021; 44: S 1 26
Discussion Would you have considered adding an agent with proven CV benefits earlier in the management of this patient? 27
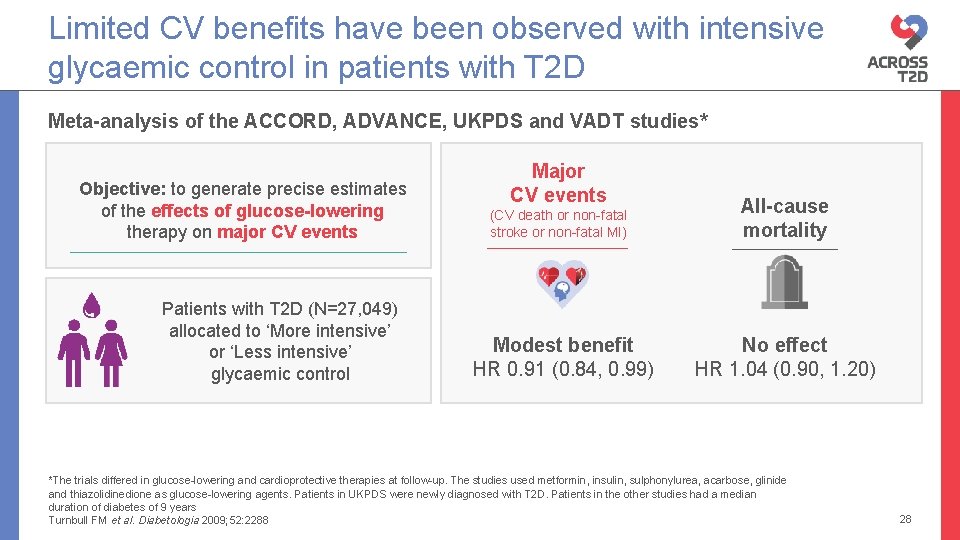
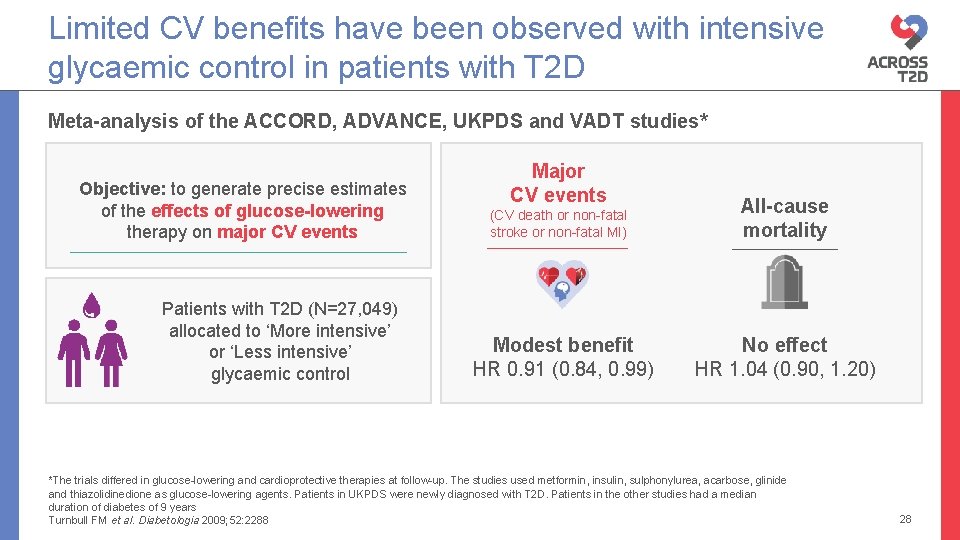
Limited CV benefits have been observed with intensive glycaemic control in patients with T 2 D Meta-analysis of the ACCORD, ADVANCE, UKPDS and VADT studies* Objective: to generate precise estimates of the effects of glucose-lowering therapy on major CV events Patients with T 2 D (N=27, 049) allocated to ‘More intensive’ or ‘Less intensive’ glycaemic control Major CV events (CV death or non-fatal stroke or non-fatal MI) Modest benefit HR 0. 91 (0. 84, 0. 99) All-cause mortality No effect HR 1. 04 (0. 90, 1. 20) *The trials differed in glucose-lowering and cardioprotective therapies at follow-up. The studies used metformin, insulin, sulphonylurea, acarbose, glinide and thiazolidinedione as glucose-lowering agents. Patients in UKPDS were newly diagnosed with T 2 D. Patients in the other studies had a median duration of diabetes of 9 years Turnbull FM et al. Diabetologia 2009; 52: 2288 28
Robert – PCP visit 2 Robert – 3 months later… Which of the following treatment options is appropriate for Robert? 1. Metformin + DPP-4 inhibitor 2. Metformin + SGLT 2 inhibitor 3. Metformin + GLP-1 RA PCP, primary care physician 29
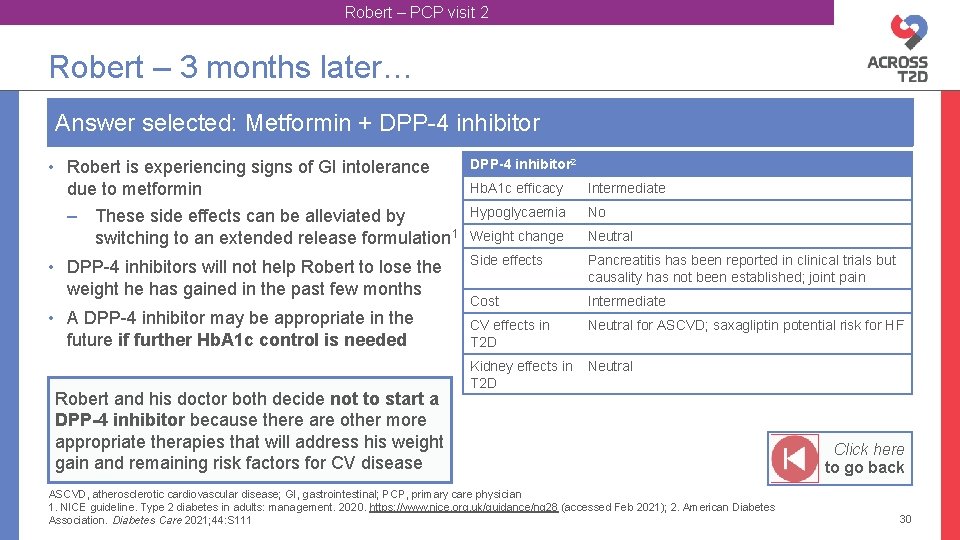
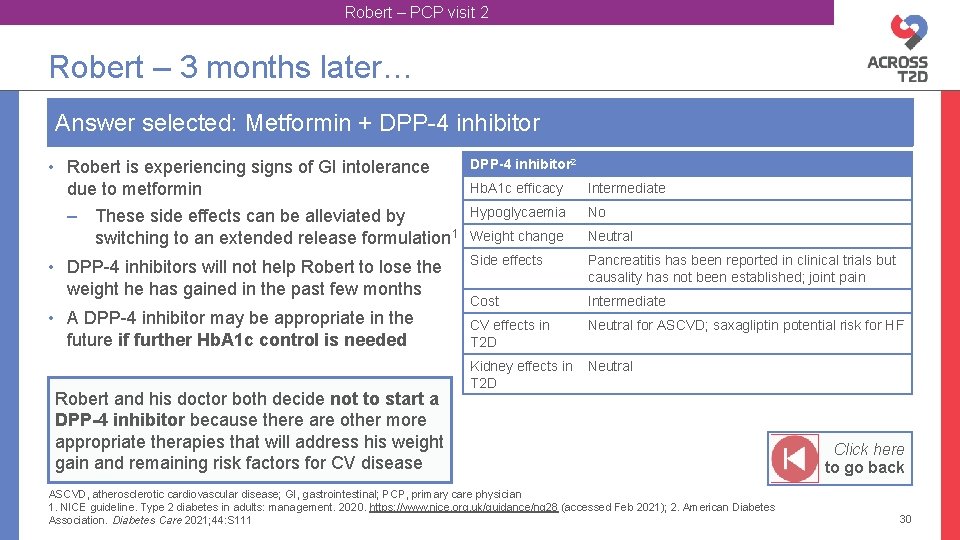
Robert – PCP visit 2 Robert – 3 months later… Answer selected: Metformin + DPP-4 inhibitor • Robert is experiencing signs of GI intolerance due to metformin – These side effects can be alleviated by switching to an extended release formulation 1 DPP-4 inhibitor 2 • DPP-4 inhibitors will not help Robert to lose the weight he has gained in the past few months • A DPP-4 inhibitor may be appropriate in the future if further Hb. A 1 c control is needed Robert and his doctor both decide not to start a DPP-4 inhibitor because there are other more appropriate therapies that will address his weight gain and remaining risk factors for CV disease Hb. A 1 c efficacy Intermediate Hypoglycaemia No Weight change Neutral Side effects Pancreatitis has been reported in clinical trials but causality has not been established; joint pain Cost Intermediate CV effects in T 2 D Neutral for ASCVD; saxagliptin potential risk for HF Kidney effects in T 2 D Neutral ASCVD, atherosclerotic cardiovascular disease; GI, gastrointestinal; PCP, primary care physician 1. NICE guideline. Type 2 diabetes in adults: management. 2020. https: //www. nice. org. uk/guidance/ng 28 (accessed Feb 2021); 2. American Diabetes Association. Diabetes Care 2021; 44: S 111 Click here to go back 30
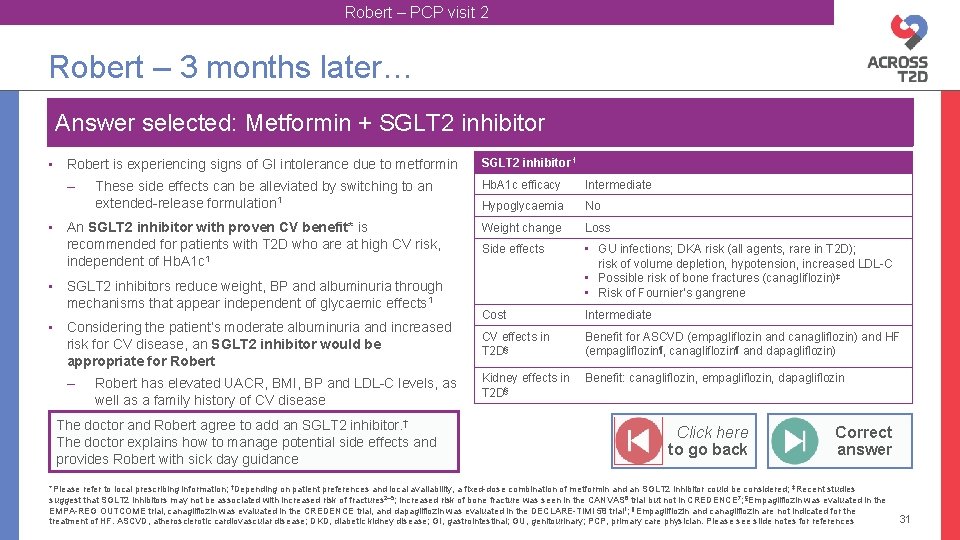
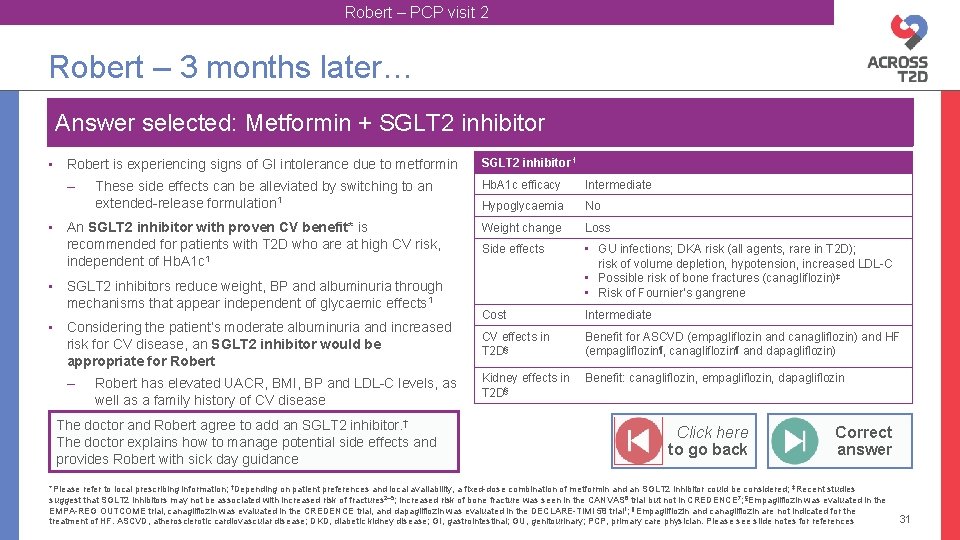
Robert – PCP visit 2 Robert – 3 months later… Answer selected: Metformin + SGLT 2 inhibitor • Robert is experiencing signs of GI intolerance due to metformin – These side effects can be alleviated by switching to an extended-release formulation 1 • An SGLT 2 inhibitor with proven CV benefit* is recommended for patients with T 2 D who are at high CV risk, independent of Hb. A 1 c 1 • SGLT 2 inhibitors reduce weight, BP and albuminuria through mechanisms that appear independent of glycaemic effects 1 • Considering the patient’s moderate albuminuria and increased risk for CV disease, an SGLT 2 inhibitor would be appropriate for Robert – Robert has elevated UACR, BMI, BP and LDL-C levels, as well as a family history of CV disease The doctor and Robert agree to add an SGLT 2 inhibitor. † The doctor explains how to manage potential side effects and provides Robert with sick day guidance SGLT 2 inhibitor 1 Hb. A 1 c efficacy Intermediate Hypoglycaemia No Weight change Loss Side effects • GU infections; DKA risk (all agents, rare in T 2 D); risk of volume depletion, hypotension, increased LDL-C • Possible risk of bone fractures (canagliflozin)‡ • Risk of Fournier’s gangrene Cost Intermediate CV effects in T 2 D§ Benefit for ASCVD (empagliflozin and canagliflozin) and HF (empagliflozin¶, canagliflozin¶ and dapagliflozin) Kidney effects in T 2 D§ Benefit: canagliflozin, empagliflozin, dapagliflozin Click here to go back Correct answer *Please refer to local prescribing information; †Depending on patient preferences and local availability, a fixed-dose combination of metformin and an SGLT 2 inhibitor could be considered; ‡Recent studies suggest that SGLT 2 inhibitors may not be associated with increased risk of fractures 2– 5; Increased risk of bone fracture was seen in the CANVAS 6 trial but not in CREDENCE 7; §Empagliflozin was evaluated in the EMPA-REG OUTCOME trial, canagliflozin was evaluated in the CREDENCE trial, and dapagliflozin was evaluated in the DECLARE-TIMI 58 trial 1; ¶Empagliflozin and canagliflozin are not indicated for the treatment of HF. ASCVD, atherosclerotic cardiovascular disease; DKD, diabetic kidney disease; GI, gastrointestinal; GU, genitourinary; PCP, primary care physician. Please see slide notes for references 31
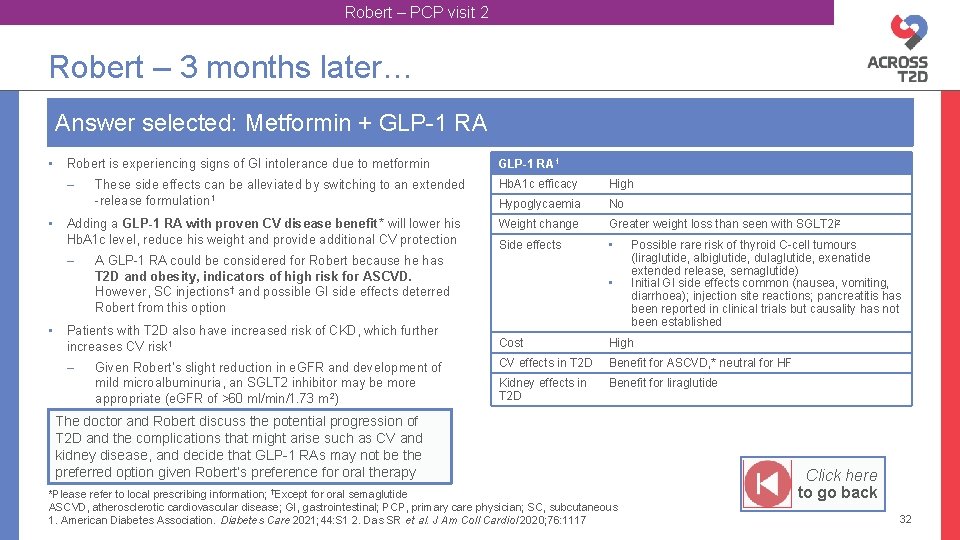
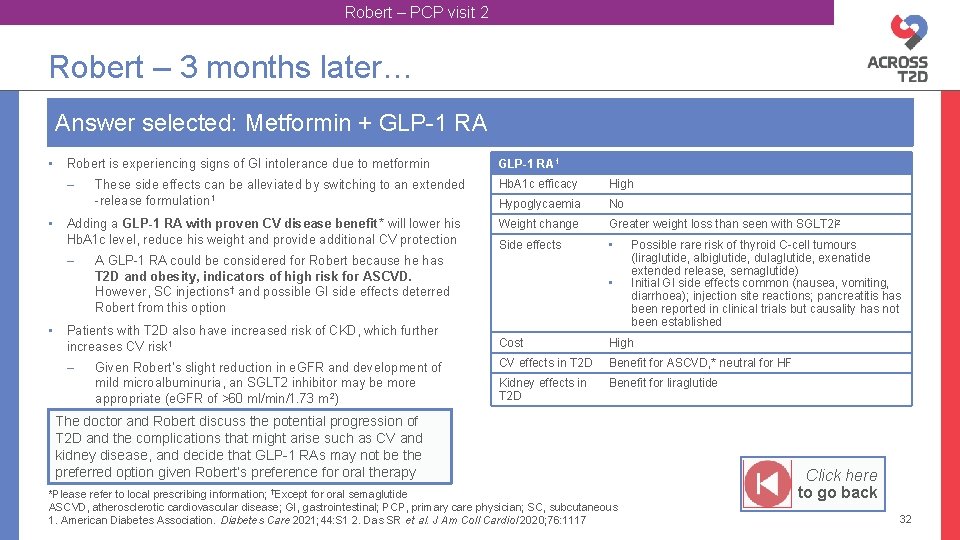
Robert – PCP visit 2 Robert – 3 months later… Answer selected: Metformin + GLP-1 RA • • Robert is experiencing signs of GI intolerance due to metformin GLP-1 RA 1 – Hb. A 1 c efficacy High Hypoglycaemia No Weight change Greater weight loss than seen with SGLT 2 i 2 Side effects • Adding a GLP-1 RA with proven CV disease benefit* will lower his Hb. A 1 c level, reduce his weight and provide additional CV protection – • These side effects can be alleviated by switching to an extended -release formulation 1 A GLP-1 RA could be considered for Robert because he has T 2 D and obesity, indicators of high risk for ASCVD. However, SC injections† and possible GI side effects deterred Robert from this option • Possible rare risk of thyroid C-cell tumours (liraglutide, albiglutide, dulaglutide, exenatide extended release, semaglutide) Initial GI side effects common (nausea, vomiting, diarrhoea); injection site reactions; pancreatitis has been reported in clinical trials but causality has not been established Patients with T 2 D also have increased risk of CKD, which further increases CV risk 1 Cost High – CV effects in T 2 D Benefit for ASCVD, * neutral for HF Kidney effects in T 2 D Benefit for liraglutide Given Robert’s slight reduction in e. GFR and development of mild microalbuminuria, an SGLT 2 inhibitor may be more appropriate (e. GFR of >60 ml/min/1. 73 m 2) The doctor and Robert discuss the potential progression of T 2 D and the complications that might arise such as CV and kidney disease, and decide that GLP-1 RAs may not be the preferred option given Robert’s preference for oral therapy †Except *Please refer to local prescribing information; for oral semaglutide ASCVD, atherosclerotic cardiovascular disease; GI, gastrointestinal; PCP, primary care physician; SC, subcutaneous 1. American Diabetes Association. Diabetes Care 2021; 44: S 1 2. Das SR et al. J Am Coll Cardiol 2020; 76: 1117 Click here to go back 32
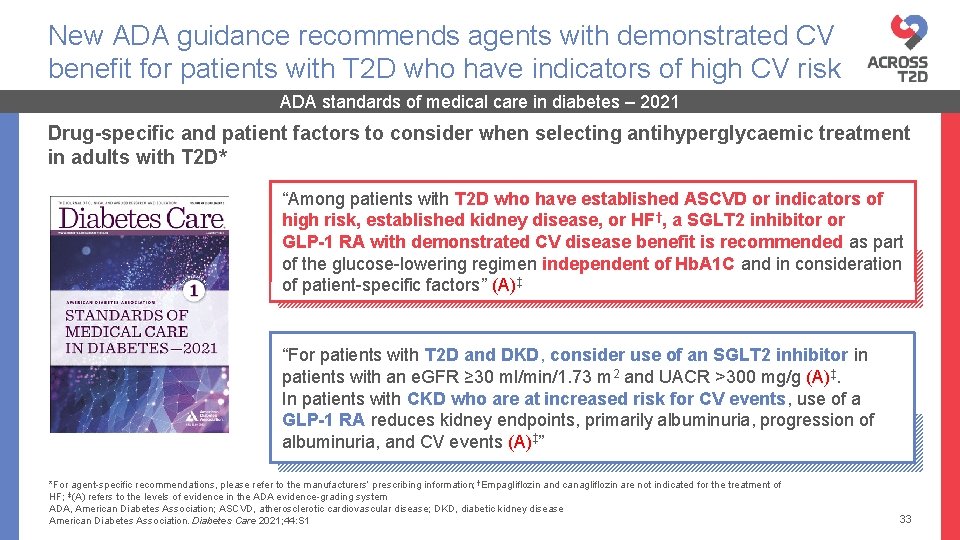
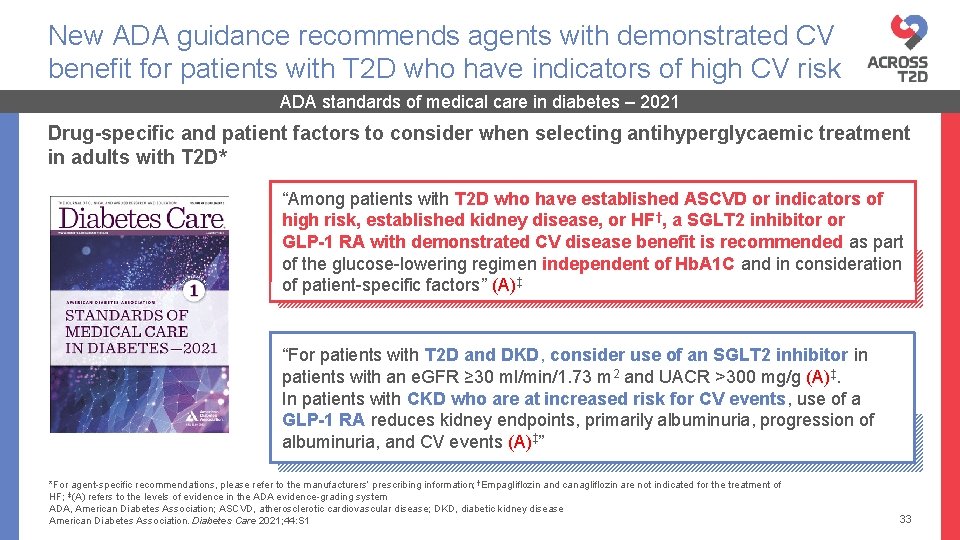
New ADA guidance recommends agents with demonstrated CV benefit for patients with T 2 D who have indicators of high CV risk ADA standards of medical care in diabetes – 2021 Drug-specific and patient factors to consider when selecting antihyperglycaemic treatment in adults with T 2 D* “Among patients with T 2 D who have established ASCVD or indicators of high risk, established kidney disease, or HF†, a SGLT 2 inhibitor or GLP-1 RA with demonstrated CV disease benefit is recommended as part of the glucose-lowering regimen independent of Hb. A 1 C and in consideration of patient-specific factors” (A)‡ “For patients with T 2 D and DKD, consider use of an SGLT 2 inhibitor in patients with an e. GFR ≥ 30 ml/min/1. 73 m 2 and UACR >300 mg/g (A)‡. In patients with CKD who are at increased risk for CV events, use of a GLP-1 RA reduces kidney endpoints, primarily albuminuria, progression of albuminuria, and CV events (A)‡” ( *For agent-specific recommendations, please refer to the manufacturers’ prescribing information; †Empagliflozin and canagliflozin are not indicated for the treatment of HF; ‡(A) refers to the levels of evidence in the ADA evidence-grading system ADA, American Diabetes Association; ASCVD, atherosclerotic cardiovascular disease; DKD, diabetic kidney disease American Diabetes Association. Diabetes Care 2021; 44: S 1 33
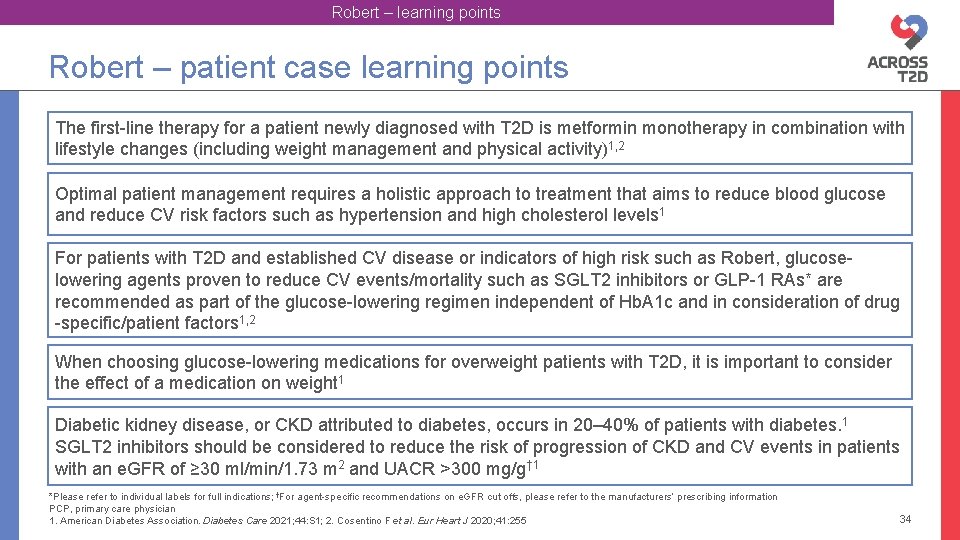
Robert – learning points Robert – patient case learning points The first-line therapy for a patient newly diagnosed with T 2 D is metformin monotherapy in combination with lifestyle changes (including weight management and physical activity)1, 2 Optimal patient management requires a holistic approach to treatment that aims to reduce blood glucose and reduce CV risk factors such as hypertension and high cholesterol levels 1 For patients with T 2 D and established CV disease or indicators of high risk such as Robert, glucoselowering agents proven to reduce CV events/mortality such as SGLT 2 inhibitors or GLP-1 RAs* are recommended as part of the glucose-lowering regimen independent of Hb. A 1 c and in consideration of drug -specific/patient factors 1, 2 When choosing glucose-lowering medications for overweight patients with T 2 D, it is important to consider the effect of a medication on weight 1 Diabetic kidney disease, or CKD attributed to diabetes, occurs in 20– 40% of patients with diabetes. 1 SGLT 2 inhibitors should be considered to reduce the risk of progression of CKD and CV events in patients with an e. GFR of ≥ 30 ml/min/1. 73 m 2 and UACR >300 mg/g† 1 *Please refer to individual labels for full indications; †For agent-specific recommendations on e. GFR cut offs, please refer to the manufacturers’ prescribing information PCP, primary care physician 1. American Diabetes Association. Diabetes Care 2021; 44: S 1; 2. Cosentino F et al. Eur Heart J 2020; 41: 255 34