Ovarian tumours Plan Nonneoplastic conditions Ovarian neoplasms 1
- Slides: 19
Ovarian tumours
Plan • Non-neoplastic conditions • Ovarian neoplasms
1 non-neoplastic conditions • 1. 1 functional cysts – Follicular cysts: follicle -> no ovulation -> persistent Gn. RH stimulation -> cyst formation – Corpus luteum cysts: follicle -> ovulation -> persisting Progesterone producing cyst -> eventual involution – These cysts are confined to the reproductive years and to those not using hormonal c/c
Functional cysts • Can be asymptomatic / pain / menstrual irregularity • Principle: If a young woman complains of pain, EXAMINE. – If cyst present: Unilateral? Is it benign? – Then Ultrasound! – CA 125 usually <35
Ultrasound criteria: Most likely benign • • • Unilocular Thin walled Smooth walls Echo free contents Unilateral Usually <8 cm in diameter
If most likely benign: • Most will undergo regression with menstruation – Can wait (not if pain is a problem) – Hormonal suppresion of Gn. RH stimulation • OC: best and convenient • or Provera 5 mg 2 x per day for 10 days (progesterone treatment) • + NSAIDs for pain • And reassess after menstruation
Complications of a cyst • Torsion – Mechanism – clinical: acute pain, nausea, faint – Tenderness, mass, acute abdomen – Diff dx: Ectopic pregnancy – Ultrasound, Hb, h. CG – Treatment: laparotomy + adnexectomy • Bleeding • Rupture
1. 2 non-functional non-neoplastic cysts • • Endometriomas Theca-lutein cysts Par-ovarian cysts Residual ovarian syndrome: posthysterectomy; pain and dyspareunia: ovary stuck to the vault. – Surgical management: removal or suspension
Ovarian neoplasms • Types: – Epithelial – Stromal – Germ cell – Metastatic • Behaviour: – Benign / borderline malignancy / malignant
• Uncommon but very important: Gynaecologic cancer with poorest prognosis • Causes: Probably genetic factors • Risk factors: age 40 -65 y – Own or family history of breast / ovary / endometrium / colon cancer – Never pregnant / infertility / low parity
• Protection: OCs, oophorectomy with strong family history • Screening: poor!! CA 125 + u/sound used: low pick up and predictability • Clinical picture – History: few complaints, non specific: tired, pain, urinary and GIT complaints, abdominal distension, only 1% bleeds
• Examination: ascites, mass in abdomen and pelvis, solid, bilateral, tender • Tests – CA 125: useful as marker if patient has raised value – FBC, sedimentation, U&E, LFT, CXR, ultrasound – Bowel: diff dx: Ba enema / colonoscopy / occult blood
Ultrasound criteria for POTENTIALLY MALIGNANT • • Solid / semicystic Multilocular Thick walled Papillary growths on walls of cysts and tumour • Bilateral • Ascites
Staging • Surgical, also 1 -4 system • I: confined to ovary / ovaries (15%) • II: also uterus, tubes, bladder and rectal walls, pelvic peritoneum (10%) • III: upper abdomen, peritoneum, omentum, lymph nodes (60%) • IV: lungs, liver, other organs (15%)
Management • Principle: Surgery followed by chemotherapy • Operations: – Staging laparotomy: for confined disease: TAH BSO omentectomy, nodes and ascites – Cytoreduction: for intraperitoneal spread: aim to do same and not leave tumour larger than 1 cm behind – Interval cytoreduction: apparently inoperable: biopsy and chemo X 3, then surgery
Further treatment • Chemotherapy: for stages 1 c onwards: 6 courses • Prognosis: 5 years survival: Stage I: 90%, Stage II 40%, Stage III 30%, Stage IV 10% • Causes of death – Intestinal obstruction, metastases, cachexia – Needs pain control and care, nutritional support and ascites control
Histologic types of tumours • Epithelial – Serous, mucinous, endometroid, clear cell, mixed • Stromal – Granulosa, theca, G+T, sertoli, leydig S+L, mixed, lipoid • Germ cell – Dysgerminoma, yolk sac, embryonal, mixed – Benign cystic teratoma
Group characteristics • Epithelial: “common”, 45 -65 y, imitates other mullerian epithelia: serous, mucinous, endometroid, clear cell. Can be Benign, borderline malignant or malignant • Stromal: rare, any age, low grade malignant behaviour; hormone producing: E: G, T. A: S, L • Germ cell: very rare; children and adolescents, highly malignant, unilateral. Chemosensitive.
Exception: Benign cystic teratoma • Most common ovarian tumour if children and young adults. Usually unilateral, few symptoms: pain, torsion, bleeding. • Contains tissue from all 3 embryonic layers • On section: hair, sebaceous material, bone and teeth • Rx: ovarian cystectomy with conservation of normal ovarian tissue
 Tongue rough edges
Tongue rough edges Dr kiran bidari
Dr kiran bidari Functions of the ovary
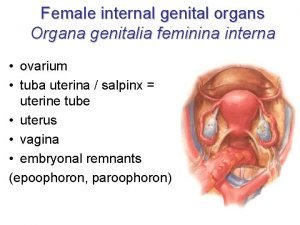
Functions of the ovary Female reproductive system
Female reproductive system Ovarian cancer marker
Ovarian cancer marker Ovarian cyst rupture discharge look like
Ovarian cyst rupture discharge look like Labeled female reproductive system
Labeled female reproductive system Portio
Portio Ovarian cancer causes
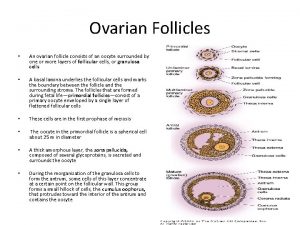
Ovarian cancer causes Ovarian follicle
Ovarian follicle Ovarian cyst
Ovarian cyst Ovarian cycle
Ovarian cycle Ovarian teratoma
Ovarian teratoma Corpus albicans
Corpus albicans Ovarian cancer brca
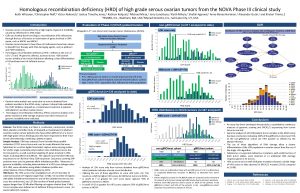
Ovarian cancer brca Hrd score ovarian cancer
Hrd score ovarian cancer Theca cells
Theca cells Duck penis
Duck penis Ovarian benign tumor
Ovarian benign tumor Sru consensus ovarian cysts
Sru consensus ovarian cysts