New CDC Guidelines on Isolation Precautions for Asymptomatic
- Slides: 24
New CDC Guidelines on Isolation Precautions for Asymptomatic and Symptomatic Patients and Employees Barbara Pelletreau, Patient Safety Shelli Hoffman, Employee Health Lead, Human Resources Roy Boukidjian, Infection Prevention, Patient Safety Marcy Goodman, Infection Prevention, Patient Safety July 28, 2020
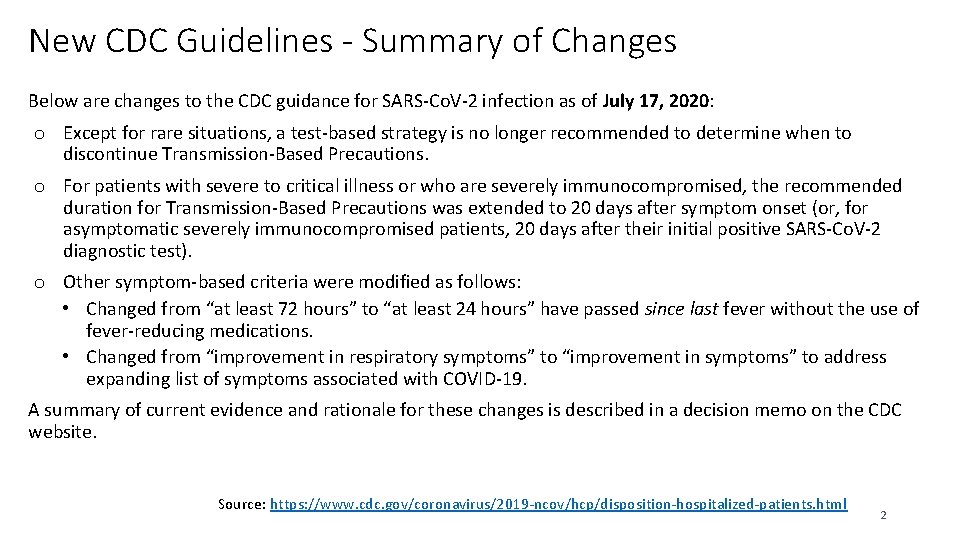
New CDC Guidelines - Summary of Changes Below are changes to the CDC guidance for SARS-Co. V-2 infection as of July 17, 2020: o Except for rare situations, a test-based strategy is no longer recommended to determine when to discontinue Transmission-Based Precautions. o For patients with severe to critical illness or who are severely immunocompromised, the recommended duration for Transmission-Based Precautions was extended to 20 days after symptom onset (or, for asymptomatic severely immunocompromised patients, 20 days after their initial positive SARS-Co. V-2 diagnostic test). o Other symptom-based criteria were modified as follows: • Changed from “at least 72 hours” to “at least 24 hours” have passed since last fever without the use of fever-reducing medications. • Changed from “improvement in respiratory symptoms” to “improvement in symptoms” to address expanding list of symptoms associated with COVID-19. A summary of current evidence and rationale for these changes is described in a decision memo on the CDC website. Source: https: //www. cdc. gov/coronavirus/2019 -ncov/hcp/disposition-hospitalized-patients. html 2
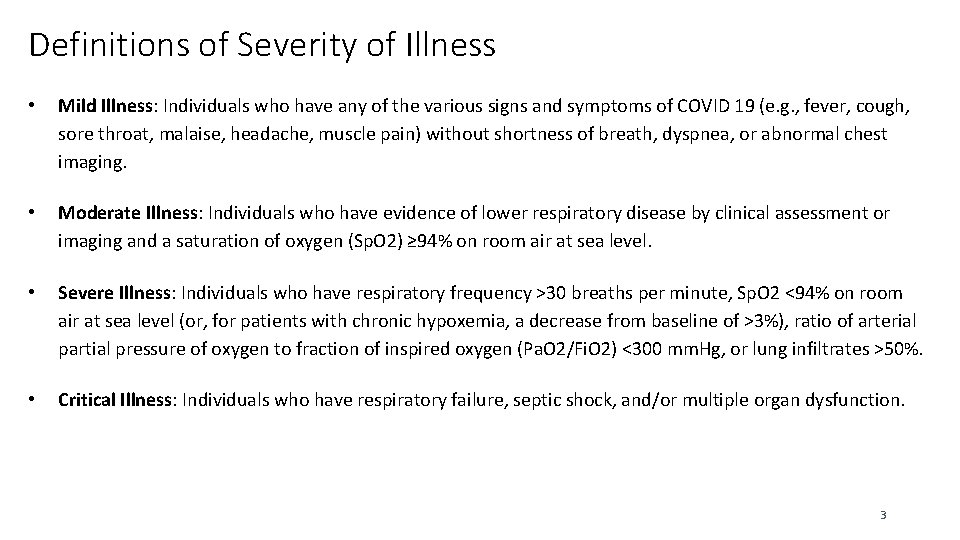
Definitions of Severity of Illness • Mild Illness: Individuals who have any of the various signs and symptoms of COVID 19 (e. g. , fever, cough, sore throat, malaise, headache, muscle pain) without shortness of breath, dyspnea, or abnormal chest imaging. • Moderate Illness: Individuals who have evidence of lower respiratory disease by clinical assessment or imaging and a saturation of oxygen (Sp. O 2) ≥ 94% on room air at sea level. • Severe Illness: Individuals who have respiratory frequency >30 breaths per minute, Sp. O 2 <94% on room air at sea level (or, for patients with chronic hypoxemia, a decrease from baseline of >3%), ratio of arterial partial pressure of oxygen to fraction of inspired oxygen (Pa. O 2/Fi. O 2) <300 mm. Hg, or lung infiltrates >50%. • Critical Illness: Individuals who have respiratory failure, septic shock, and/or multiple organ dysfunction. 3
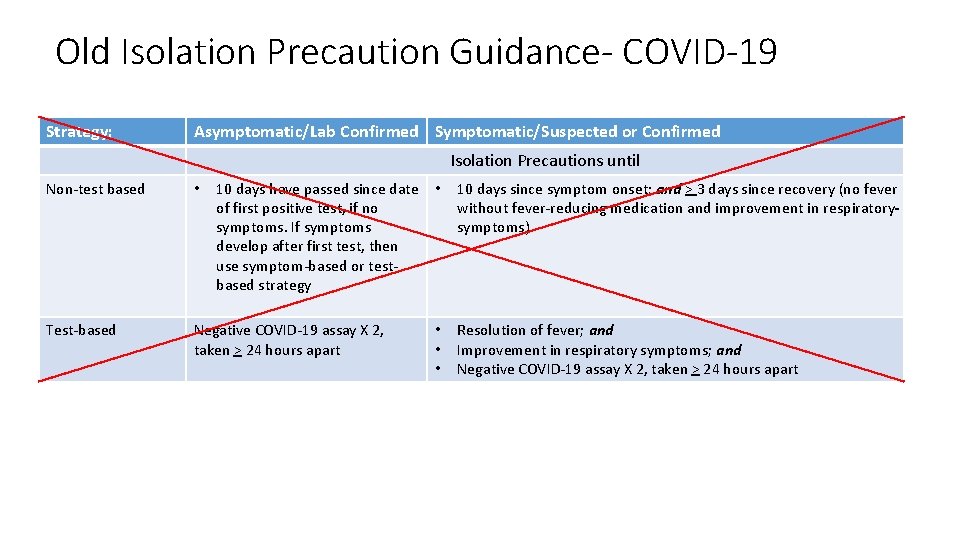
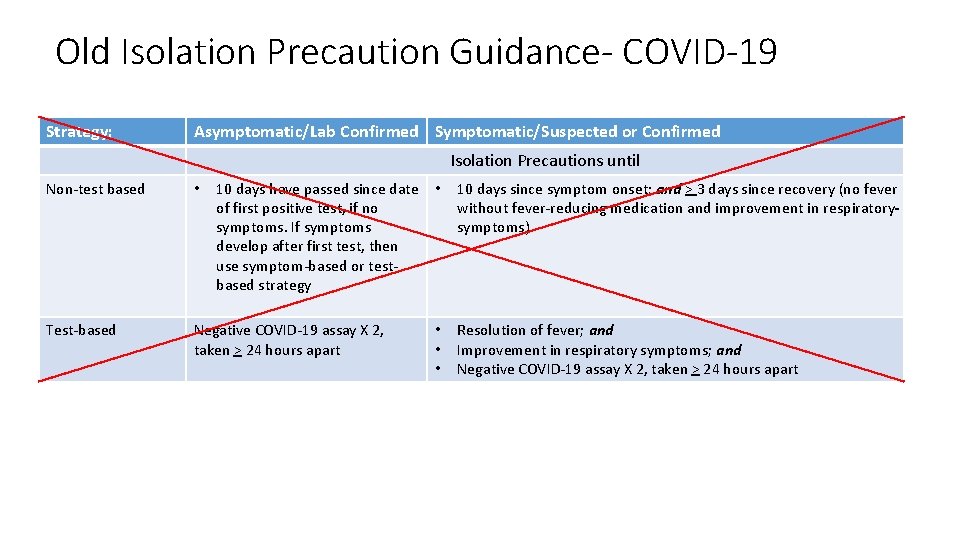
Old Isolation Precaution Guidance- COVID-19 Strategy: Asymptomatic/Lab Confirmed Symptomatic/Suspected or Confirmed Isolation Precautions until Non-test based • 10 days have passed since date • of first positive test, if no symptoms. If symptoms develop after first test, then use symptom-based or testbased strategy Test-based Negative COVID-19 assay X 2, taken > 24 hours apart • • • 10 days since symptom onset; and > 3 days since recovery (no fever without fever-reducing medication and improvement in respiratory symptoms) Resolution of fever; and Improvement in respiratory symptoms; and Negative COVID-19 assay X 2, taken > 24 hours apart
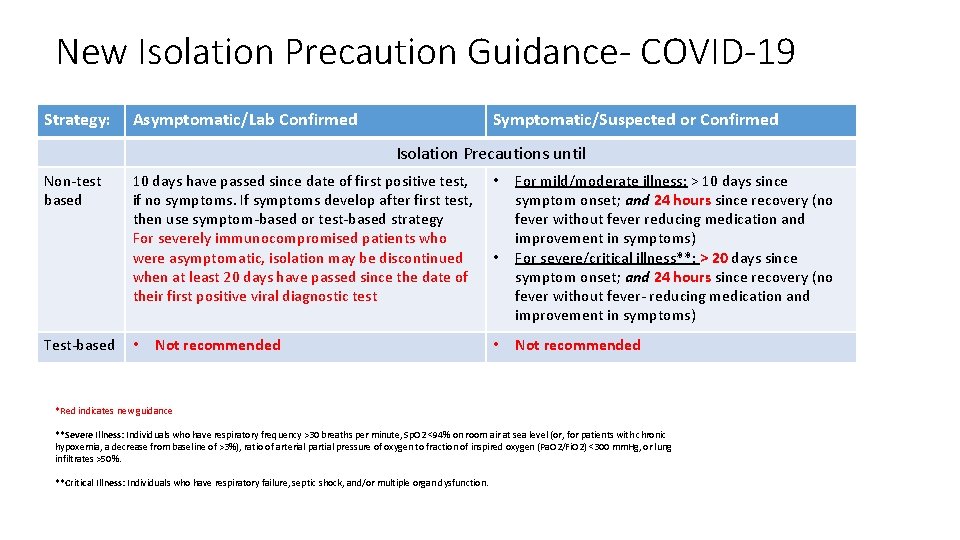
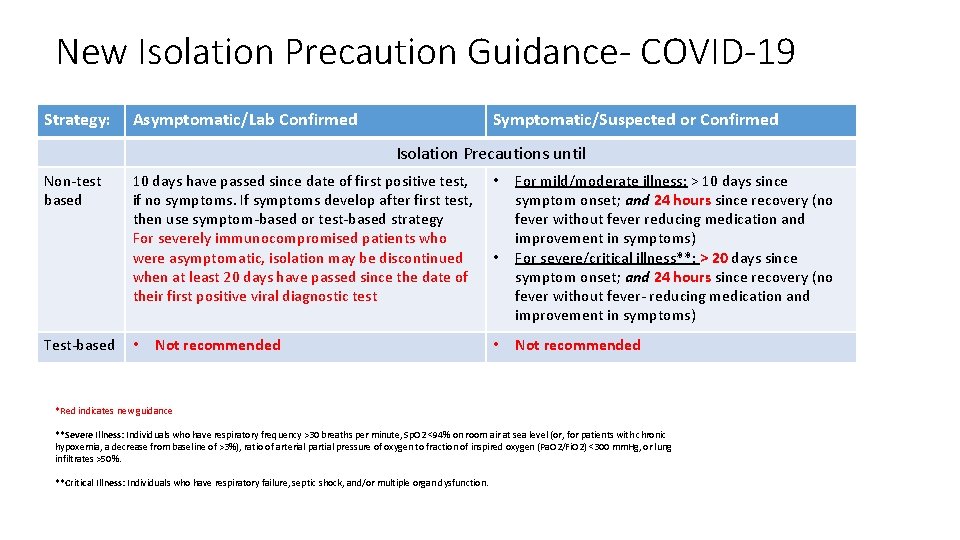
New Isolation Precaution Guidance- COVID-19 Strategy: Asymptomatic/Lab Confirmed Symptomatic/Suspected or Confirmed Isolation Precautions until Non-test based Test-based 10 days have passed since date of first positive test, if no symptoms. If symptoms develop after first test, then use symptom-based or test-based strategy For severely immunocompromised patients who were asymptomatic, isolation may be discontinued when at least 20 days have passed since the date of their first positive viral diagnostic test • Not recommended • • • For mild/moderate illness: > 10 days since symptom onset; and 24 hours since recovery (no fever without fever reducing medication and improvement in symptoms) For severe/critical illness**: > 20 days since symptom onset; and 24 hours since recovery (no fever without fever- reducing medication and improvement in symptoms) Not recommended *Red indicates new guidance **Severe Illness: Individuals who have respiratory frequency >30 breaths per minute, Sp. O 2 <94% on room air at sea level (or, for patients with chronic hypoxemia, a decrease from baseline of >3%), ratio of arterial partial pressure of oxygen to fraction of inspired oxygen (Pa. O 2/Fi. O 2) <300 mm. Hg, or lung infiltrates >50%. **Critical Illness: Individuals who have respiratory failure, septic shock, and/or multiple organ dysfunction.
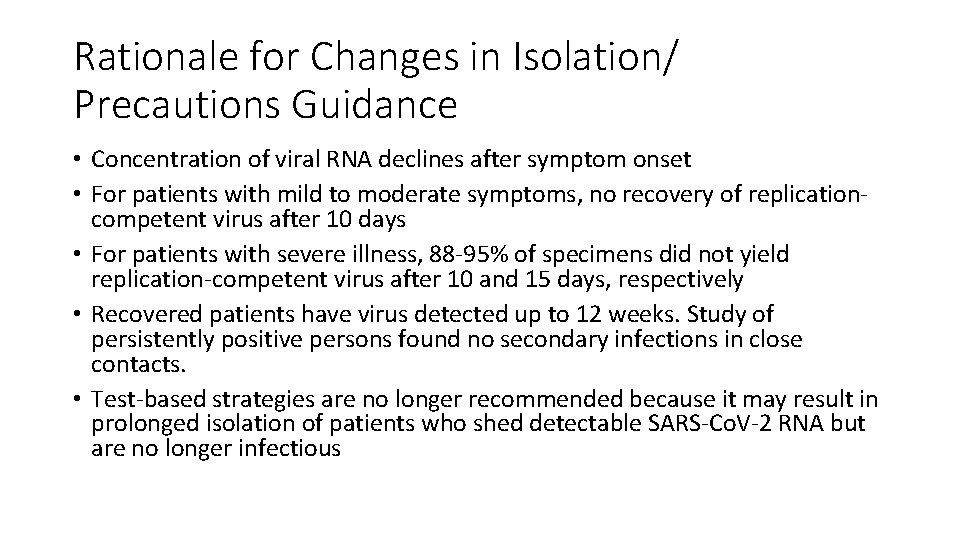
Rationale for Changes in Isolation/ Precautions Guidance • Concentration of viral RNA declines after symptom onset • For patients with mild to moderate symptoms, no recovery of replicationcompetent virus after 10 days • For patients with severe illness, 88 -95% of specimens did not yield replication-competent virus after 10 and 15 days, respectively • Recovered patients have virus detected up to 12 weeks. Study of persistently positive persons found no secondary infections in close contacts. • Test-based strategies are no longer recommended because it may result in prolonged isolation of patients who shed detectable SARS-Co. V-2 RNA but are no longer infectious
A reminder … CDC published the changes presented in this slide deck on July 17 and provided a document supporting these changes. However, like all changes and like in the past, CDC always suggests that healthcare providers coordinate with their local Public Health Department.
Scenario #1 - Patient A healthy 25 year old is admitted following a serious motor vehicle accident. On Day 2 of hospitalization, this patient develops a low grade fever and a new loss of sense of smell. This patient is now put into isolation precautions and tested for COVID-19. The results are positive. Their fever resolves by Hospital Day 6 and they do not develop new symptoms. It is now Hospital Day 12 and they are ready to transfer to a rehab facility. Does the patient need to continue to be under isolation precautions? Can this patient transfer to another facility?
Response #1 Isolation precautions may be discontinued for a person with mild to moderate COVID-19 illness 10 days after symptom onset if symptoms have improved and they are afebrile. By Day 12, this patient meets criteria for discontinuing precautions. Meeting criteria for discontinuation of precautions is not a prerequisite for discharge from a facility. In this scenario, the patient may be transferred to another facility without further restriction. If precautions were still required, the patient could be discharged, but they should go to a facility with the ability to adhere to isolation precautions.
Scenario #2 - Patient A healthy pregnant mother to be is admitted in labor and delivery. COVID-19 test results taken two weeks ago were positive but the patient never developed symptoms. Should this patient be isolated? Should this patient be retested for COVID-19 upon admission?
Response #2 When a person is asymptomatic, the date of first positive COVID-19 test may be used to determine the length of isolation precautions. In this scenario, more than 10 days have passed since testing and transmission-based isolation precautions are not indicated. Re-testing of this person is not recommended, as a person may have virus detected for several weeks even though they are no longer infectious. Follow the facility policy regarding source control for supporting partners.
Scenario #3 - Patient After 3 weeks, a patient with COVID-19 is being transferred out of the ICU to a lower acuity floor with no isolation precautions. The patient continues to have some COVID-19 symptoms but is better each day and no fever. Staff questions the no isolation precautions and contacts the Infection Preventionist for clarification. What should the Infection Preventionist tell the concerned staff members?
Response #3 The communicability of COVID-19 diminishes over time. Even people who are critically ill with COVID-19 appear to be non-infectious 20 days after symptom onset. Discontinuing isolation precautions that are no longer required to prevent transmission conserves PPE. Staff should continue to practice universal source control and perform hand hygiene consistently.
Scenario #4 - Patient A COVID-19 positive patient has been in ICU for 6 weeks on a ventilator. Recently the patient made significant improvement – no longer needing a ventilator. The patient’s symptoms continuously improved including no temperature and no fever reducing medications. The attending physician writes an order that the patient no longer needs isolation and can be transferred to a lower level of care tomorrow. The nurse questions the isolation removal order and contacts the Infection Preventionist for clarification. What should the Infection Preventionist convey to the nurse?
Response #4 The communicability of COVID-19 diminishes over time. Individuals with moderate to severe symptoms should remain in isolation for 20 days since symptoms first appeared and 24 hours have passed since last fever with no fever reducing medication as well as improvement in other symptoms. The patient meets this criteria thus isolation is no longer needed. The Infection Preventionist should review the patient status and discuss the question and any further concern the nurse may have in relation to COVID-19.
Scenario #5 - Patient A patient that was discharged to a skilled nursing facility (SNF) tested positive for COVID-19 with mild symptoms several weeks after discharge. The patient improved and became symptom free. He continued his stay at the SNF until he sustained a fall two weeks later. The patient was readmitted to the hospital. Does the patient need to be in isolation?
Response #5 The patient does not need to be in isolation as more than 10 days have passed since first symptom onset and has had no elevated temperatures. The patient should be treated for the diagnosis established for this visit.
Scenario #6 – Employee An employee tested positive for COVID-19 and has continued to have moderate symptoms for two weeks. After two weeks, the employee is feeling much better and is ready to return to work; however, they continue to have some minor intermittent symptoms, but no fever. The employee contacts Employee Health Coordinator to see if they can return to work tomorrow. And if so, how should they answer the screening questions when they arrive?
Response #6 The communicability of COVID-19 diminishes over time. Individuals with mild to moderate symptoms can return to work after 10 days from on set or positive COVID-19 test, and symptoms are improving and no temperature for 24 hours without fever reducing medications. When the employee arrives tomorrow they should answer yes to symptoms, have their temperature taken and let the screeners know that they were approved to return to work by Employee Health.
Scenario #7 - Employee A hospital physical therapist is considered immunocompromised due to long-term, high-dose steroid use. Three days ago, they developed a headache, fatigue and diarrhea and have stayed off work. They have no known exposure to COVID-19. On the fourth day, they call Employee Health as they are feeling slightly better. The physical therapist asks Employee Health when can they return to work. What should the Employee Health Coordinate say to the employee?
Response #7 The symptoms described may be related to COVID-19. The employee should consult with their personal clinician and stay off work pending evaluation. If the individual is diagnosed with COVID-19, the CDC recommends that symptomatic, immunocompromised persons be restricted from working for 20 days from symptom onset and at least 24 hours since recovery. The facility should consult the public health department on the management of employees with COVID-19 symptoms/infections.
Scenario #8 - Employee has an ill family member at home who was recently tested for COVID-19 and tested positive. The employee is not symptomatic but has called Employee Health to ask if they should be working or not. The local Public Health has said that this employee can return to work. Other employees are voicing concerns and does not want this employee to return to work. What should the facility do?
Response #8 Employee Health should provide forms to the employee to track/record their symptoms in the morning and evening. If the employee has any symptoms, they should immediately contact Employee Health and not come to work. The employee can work as long as they strictly adhere to universal source control. The hospital should be screening all employees for temperature and symptoms each day upon arrival and prior to entering the facility (no screening on units). Educating employees on COVID-19 best practices is key, including signage. We are seeing COVID-19 spread between employees in breakrooms.
For questions: Roy Boukidjian, Patient Safety Roy. boukidjian@dignityhealth. org Barbara Pelletreau, Patient Safety Barbara. pelletreau@dignityhealth. org Shelli Hofmann, Human Resources Shelli. hofmann@dignityhealth. org