My Case 72 F with IFG pw dysarthria




- Slides: 32
My Case • 72 F with IFG, p/w dysarthria, left weakness, veering to left, admitted with CVA. Dysarthria resolved, left weakness very minimal if at all noticeable, still unsteady on feet requiring use of walker. • Day prior to discharge, patient was not using walker, fell in the bathroom hit the side of head • Stat CT head showed scalp hematoma, no ICH.
Falls- something that should NEVER happen Kristie Akamine, R 3 Hospitalist Elective December 11, 2014
“Never Event” • Term introduced 2001 • In reference to shocking medical errors that should NEVER occur • Serious (resulting in death or significant disability), usually preventable • Revised in 2011: 29 events grouped into 6 categories: surgical, product/device, pt protection, care management, environmental, radiologic, and criminal
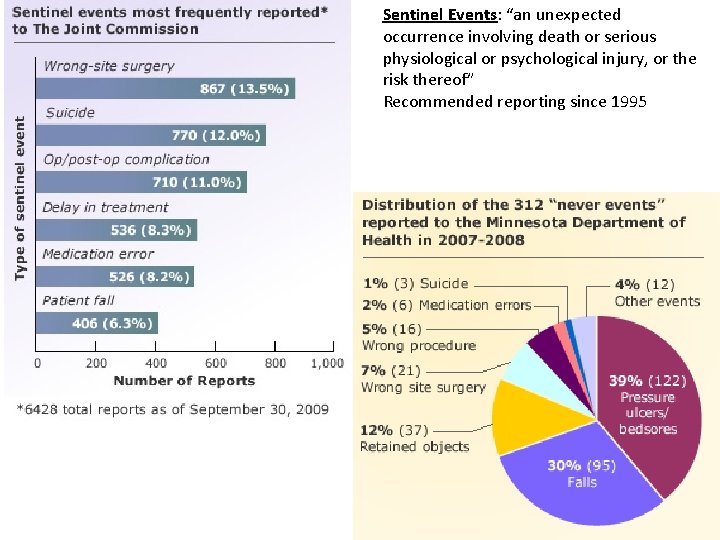
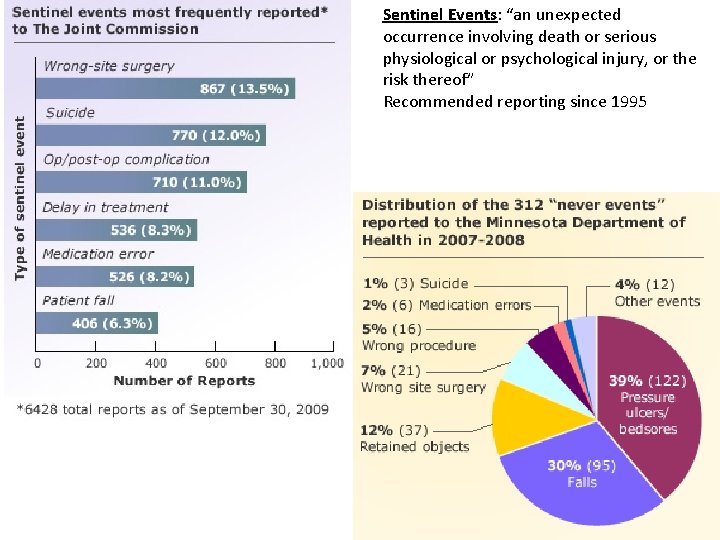
Sentinel Events: “an unexpected occurrence involving death or serious physiological or psychological injury, or the risk thereof” Recommended reporting since 1995
Never Events, 2011 • Surgical Events – Surgery performed on wrong part of body – Surgery performed on wrong patient – Wrong surg performed on wrong patient – Unintended retention of a foreign object in a pt after surgery – Intraoperative or immediate postoperative/postprocedure death in an American Society Anesthesiologist Class I pt
Never Events • Product or Device Events – Pt death or serious injury a/w use of contaminated drugs, devices, or biologics provided by health care setting – Pt death or injury a/w use or fxn of a device in pt care, in which the device is used for fxns other than as intended – Pt death or injury a/w IV air embolism that occurs while being care for in a health care setting
Never Events • Pt Protection Events – Discharge or release of a pt/resident of any age, who is unable to make decisions, to other than an authorized person – Pt death or serious disability a/w pt elopement (disappearance) – Pt suicide, attempted suicide, or self-harm resulting in serious disability, while being care for in a health care facility
Never Events • Care Management Events – Death or injury a/w med error – Death or injury a/w unsafe admin of blood products – Maternal death or serious injury a/w labor or delivery in a low-risk pregnancy while being care for in a health care setting – Death or serious injury of a neonate a/w labor/delivery in a low-risk pregnancy – Artificial insemination with the wrong donor sperm/egg – Death or injury a/w fall while being cared for in a health setting – Any stage 3, 4, or unstageable pressure ulcer acquired after admission/presentation to a health care facility – Death or serious disability resulting from the irretrievable loss of an irreplaceable biologic specimen – Death or injury from failure to f/u or communicate lab, path, or radiology results
Never Events • Environmental Events – Pt/staff death/disability a/w an electric shock in the course of a patient care process in a health care setting – Any incident in which a line designated for O 2 or other gas to be delivered to a patient contains no gas, the wrong gas, or is contaminated by toxic substances – Pt/staff death/injury a/w burn incurred from any source in the course of a patient care process in a health care setting – Pt death/injury a/w use of restraints or bedrails while being cared for in a health care setting
Never Events • Radiologic events – Death/ injury of pt/staff a/w introduction of a metallic object into the MRI area • Criminal events – Any instance of care ordered by or provided by someone impersonating a MD, RN, Pharm. D, other licensed provider – Abduction of a patient/resident of any age – Sexual abuse/assault on pt w/in /on the grounds of a health care setting – Death/injury of pt/staff from a physical assault (i. e. , battery) that occurs w/in / on grounds of a health care settin
Never Events • Most Never Events are very rare • Wrong-site surgery may occur q 5 -10 yrs • However, when they occur, they are devastating; 71% never events over past 12 yrs were FATAL • On a population basis, >4 k surgical never events occur yearly in US
FALLS • 700 K to 1 mil pts suffer a fall/yr in US hospitals – 30 -50% inpt falls result in an injury – 1 -3% result in fractures • Need to get pts OOB ASAP to improve independence – A pt who is not permitted to walk alone can become a pt who is unable to walk alone
Why It’s SO IMPORTANT to prevent falls in hospitals… • Patient outcomes: incr M&M, satisfaction • Fracture, SDH, injury requiring surg, death – Falls fear of falling downward spiral of reduced mobility loss of fxn greater risk of falls • $$$$: neg effect on hospital costs, pt cost – Incr LOS – Litigation
COSTS • Since 2008, CMS do NOT pay hospitals for the extra care a/w inpatient fall – Private insurers followed 2009 – Estimated non-reimbursed hospital costs related to falls 2008 -2009 were $7. 6 mil – Hospitals with high rates of hospital-acquired conditions receive a 1% cut in Medicare payments for all discharges • Increase in hospital’s operational costs for serious fall-related injury is >$13 K & LOS incr by 6. 27 days
Risk Factors • Older age – >80% falls inpt are 65+ yo – Incontinence/frequency • • Units: Geri, psychogeriatrics, neuro, rehab H/o falls Cognitive impairment Visual impairment Dizziness, vertigo, postural hypo. TN Environmental hazards Impaired mobility Certain meds: neuroleptics, benzo, antidepressants, sedatives (zolpidem)
4 types • Accidental: when low-risk pts trip over IV pole, fall OOB when they reach to get something • Anticipated physiological: MC type of falls; occur in pts who have RFs that can be ID’d in advance, incl abnormal gait, high-risk med, urinary frequency, or dementia • Unanticipated physiological: in pts who have a low risk of falls in general but suffer an event—sz, CVA, syncope that couldn’t have been predicted • Behavioral or intentional: when pt acts out • #1 & 2 are preventable
How do we prevent falls? ? • While many falls can be avoided, prevention is complex bc many things are associated with falls – Weak muscles – use of cane/walker – environmental factors (bed positioning at optimal ht) – process of care factors (RN not responding promptly to call bells)
How do we prevent falls? ? • Unlike hospital-acquired infections, which can be addressed by adopting evidence-based protocols relevant to all hospitals, there is NO bundle of prevention for practices that has been proven to eliminate all falls • Multifaceted fall prevention programs have been shown to reduce RR for falls by 30%
Preventing Inpatient Falls • Multidisciplinary (rather than solely RNs) responsibilities for intervention • Focus on prevention, detection, tx of delirium, including dip -testing urine for indications of infection • Review & d/c of “culprit” meds • Post-fall review used as opportunity to plan 2 o prevention, incl careful hx to ID syncope • Early access to mobility aids, exercise • Individualized plan of care that is responsive to pt needs • Provision of safe footwear (rather than advice) • Staff & pt education

• Controversial: – Ultralow beds – Movement alarms – Hip protectors
• Hourly rounding – Teach back method • • • Hand rails Nonslip flooring Improving lines of site Standardize interventions for pts at risk for falling Customize interventions for pts at highest risk of fall-related injury
Inpatient Fall Prevention Strategies: • Falls prevention protocols using validated risk assessment tool on admission and repeated at regular intervals
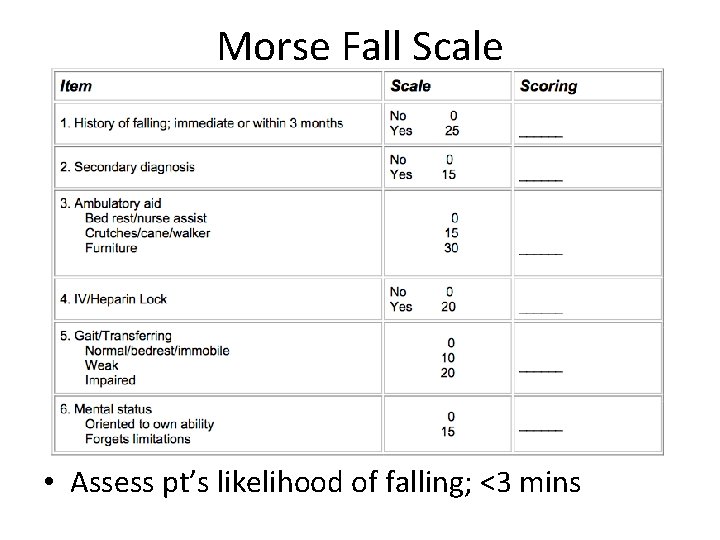
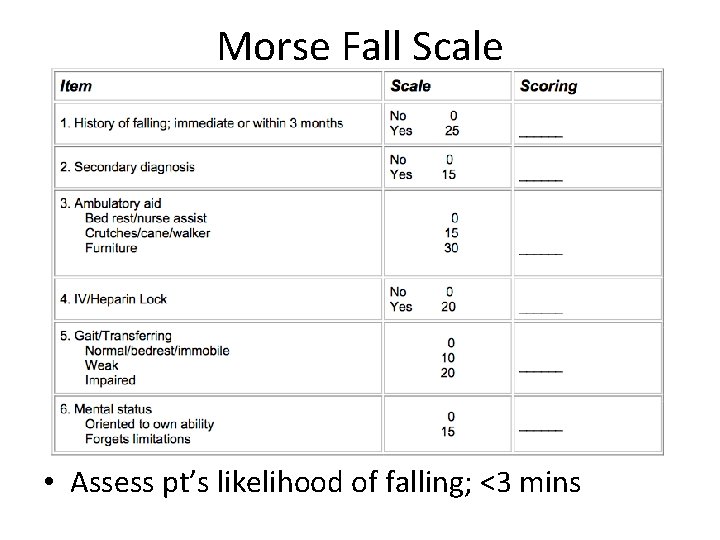
Morse Fall Scale • Assess pt’s likelihood of falling; <3 mins
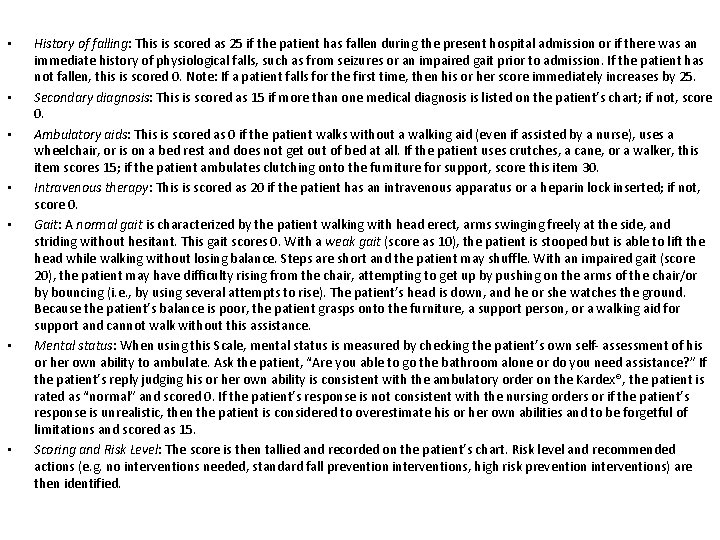
• • History of falling: This is scored as 25 if the patient has fallen during the present hospital admission or if there was an immediate history of physiological falls, such as from seizures or an impaired gait prior to admission. If the patient has not fallen, this is scored 0. Note: If a patient falls for the first time, then his or her score immediately increases by 25. Secondary diagnosis: This is scored as 15 if more than one medical diagnosis is listed on the patient’s chart; if not, score 0. Ambulatory aids: This is scored as 0 if the patient walks without a walking aid (even if assisted by a nurse), uses a wheelchair, or is on a bed rest and does not get out of bed at all. If the patient uses crutches, a cane, or a walker, this item scores 15; if the patient ambulates clutching onto the furniture for support, score this item 30. Intravenous therapy: This is scored as 20 if the patient has an intravenous apparatus or a heparin lock inserted; if not, score 0. Gait: A normal gait is characterized by the patient walking with head erect, arms swinging freely at the side, and striding without hesitant. This gait scores 0. With a weak gait (score as 10), the patient is stooped but is able to lift the head while walking without losing balance. Steps are short and the patient may shuffle. With an impaired gait (score 20), the patient may have difficulty rising from the chair, attempting to get up by pushing on the arms of the chair/or by bouncing (i. e. , by using several attempts to rise). The patient’s head is down, and he or she watches the ground. Because the patient’s balance is poor, the patient grasps onto the furniture, a support person, or a walking aid for support and cannot walk without this assistance. Mental status: When using this Scale, mental status is measured by checking the patient’s own self- assessment of his or her own ability to ambulate. Ask the patient, “Are you able to go the bathroom alone or do you need assistance? ” If the patient’s reply judging his or her own ability is consistent with the ambulatory order on the Kardex®, the patient is rated as “normal” and scored 0. If the patient’s response is not consistent with the nursing orders or if the patient’s response is unrealistic, then the patient is considered to overestimate his or her own abilities and to be forgetful of limitations and scored as 15. Scoring and Risk Level: The score is then tallied and recorded on the patient’s chart. Risk level and recommended actions (e. g. no interventions needed, standard fall prevention interventions, high risk prevention interventions) are then identified.

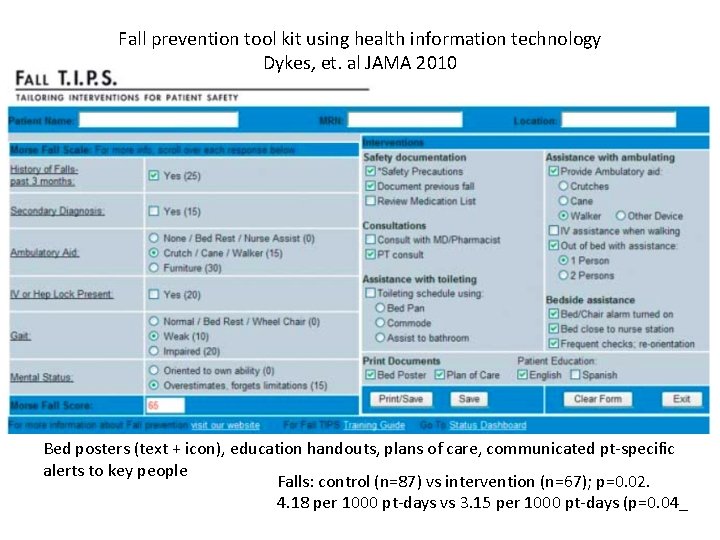
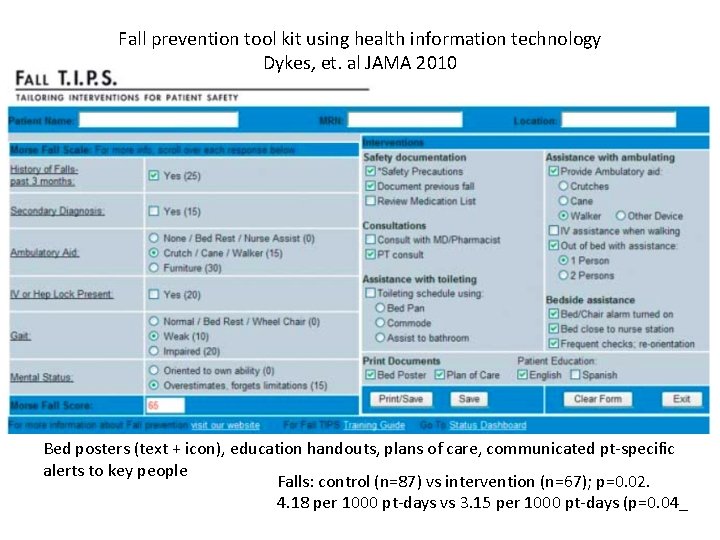
Fall prevention tool kit using health information technology Dykes, et. al JAMA 2010 Bed posters (text + icon), education handouts, plans of care, communicated pt-specific alerts to key people Falls: control (n=87) vs intervention (n=67); p=0. 02. 4. 18 per 1000 pt-days vs 3. 15 per 1000 pt-days (p=0. 04_
Fall Prevention Strategies • Identify / assess fall risk • Common falls prevention protocol – education, environmental safety measures & alerting staff that any pt may fall – COMMUNICATION • Bundle to increase surveillance thru identifiers – colored arm bands, door stickers, chart stickers, colored clothing, room location • Technological approaches – bed/chair alarms, bed rails, webcams, beds with netting, specially designed floor cushion pads, low beds

Fall Prevention Strategies • Technology: wireless staff phones & hallway monitor screens – When call bell or chair alarm goes off phones and wall screen. If member responsible is busy, message is sent to next staff member until someone responds – Reminds RNs to do hourly rounding & display screens – 6% RRR for falls in 325 hospitals in 2012 $16 mil saved
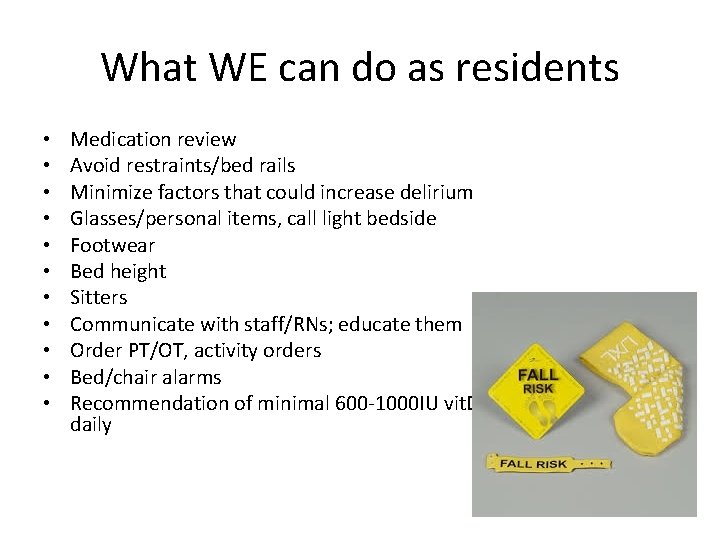
What WE can do as residents • • • Medication review Avoid restraints/bed rails Minimize factors that could increase delirium Glasses/personal items, call light bedside Footwear Bed height Sitters Communicate with staff/RNs; educate them Order PT/OT, activity orders Bed/chair alarms Recommendation of minimal 600 -1000 IU vit. D daily
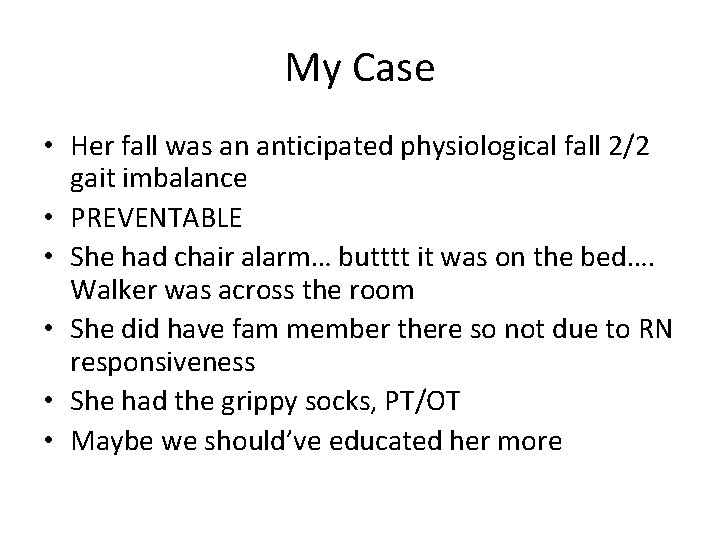
My Case • Her fall was an anticipated physiological fall 2/2 gait imbalance • PREVENTABLE • She had chair alarm… butttt it was on the bed…. Walker was across the room • She did have fam member there so not due to RN responsiveness • She had the grippy socks, PT/OT • Maybe we should’ve educated her more

References • AHRQ Patient Safety Network – Multiple journal articles linked from this site • Hospitals & Health Networks (H&HN). www. hhnmag. com • Up-To-Date
 Ifg diabete
Ifg diabete Ifg urbino
Ifg urbino Uam ifg
Uam ifg Dysdiodokinesia
Dysdiodokinesia Dysarthria clumsy hand syndrome
Dysarthria clumsy hand syndrome Dysarthria types
Dysarthria types Hypokinetic dysarthria
Hypokinetic dysarthria Flaccid vs spastic dysarthria
Flaccid vs spastic dysarthria Dysarthria clumsy hand syndrome
Dysarthria clumsy hand syndrome Best worst and average case
Best worst and average case Average case complexity of binary search
Average case complexity of binary search Bubble sort best case and worst case
Bubble sort best case and worst case Case western reserve university case school of engineering
Case western reserve university case school of engineering Ambiguous case triangles
Ambiguous case triangles Bubble sort best case and worst case
Bubble sort best case and worst case Short case vs long case
Short case vs long case Bubble sort best case and worst case
Bubble sort best case and worst case Fbi virtual case file case study
Fbi virtual case file case study Case study 11
Case study 11 Plaque index
Plaque index Clarkson lumber company case
Clarkson lumber company case Latin vocative case
Latin vocative case Law of sines ssa
Law of sines ssa Illy coffee case study
Illy coffee case study National land finance cooperative society
National land finance cooperative society E-commerce for a small supermarket case study
E-commerce for a small supermarket case study Hoover dam case study
Hoover dam case study Desain case control
Desain case control Fc5 torrent
Fc5 torrent Case study definition
Case study definition Lymphoma case presentation
Lymphoma case presentation Sheryl fleisch
Sheryl fleisch Amazon and whole foods merger case study
Amazon and whole foods merger case study