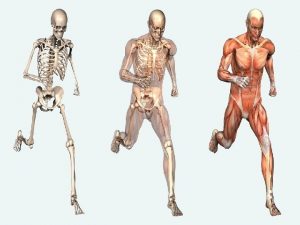
Musculoskeletal System Hannah OHandley RN MSN CPNP Epiphysis



- Slides: 47
Musculoskeletal System Hannah O’Handley RN, MSN, CPNP
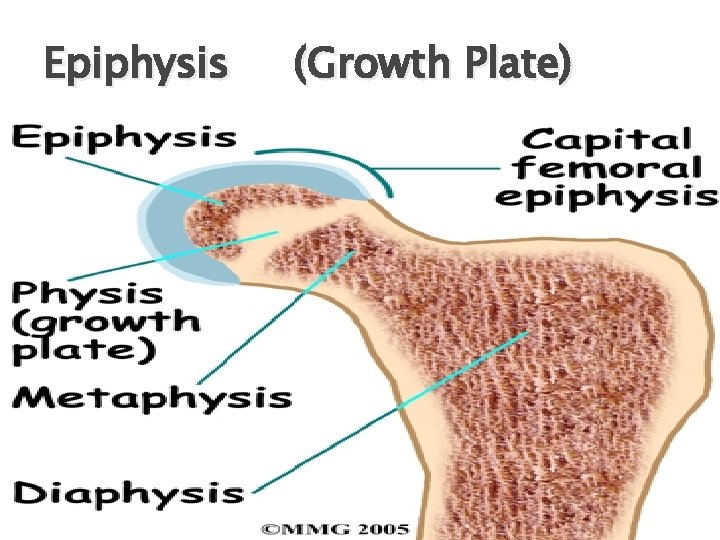
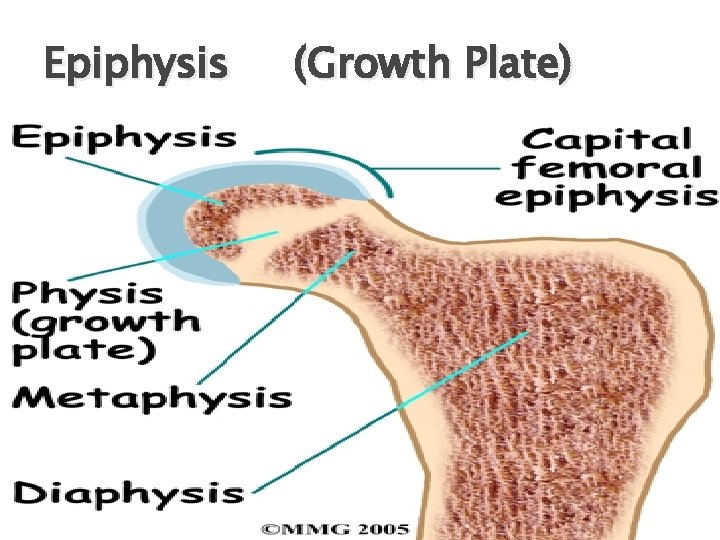
Epiphysis (Growth Plate)
Traction Skin ◦ Pull applied to skin ◦ Causes traction on bones and muscles Skeletal surgically placed Pins, wires or tongs through distal end of bone
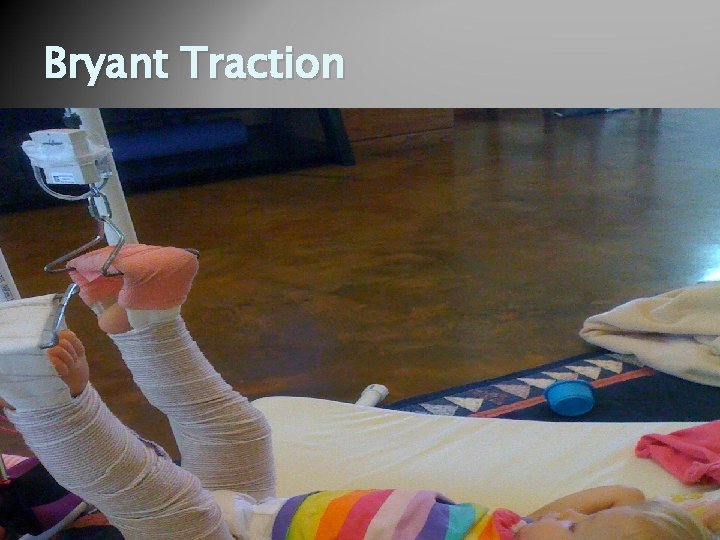
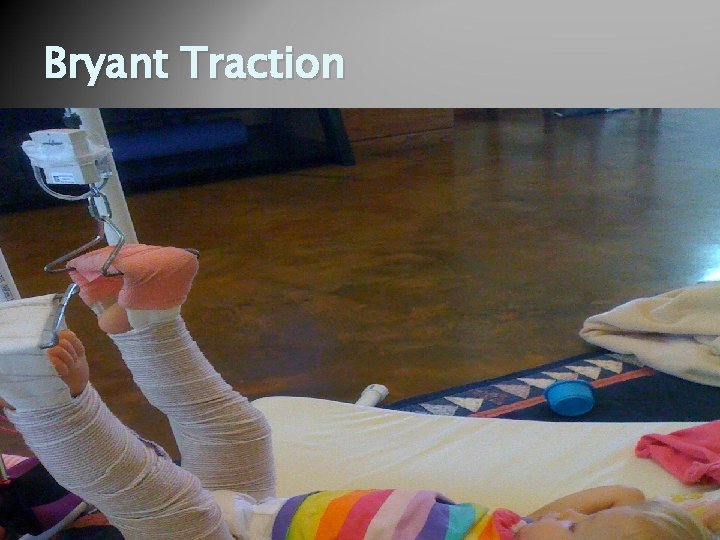
Bryant Traction

Congenital Musculoskeletal Defects
Duchenne’s Muscular Dystrophy (DMD) Progressive degeneration of symmetric skeletal muscles Gene mutation results in absence of dystrophin (protein in skeletal muscles) X-linked recessive trait ◦ Affects boys almost exclusively Onset between 3 -6 years
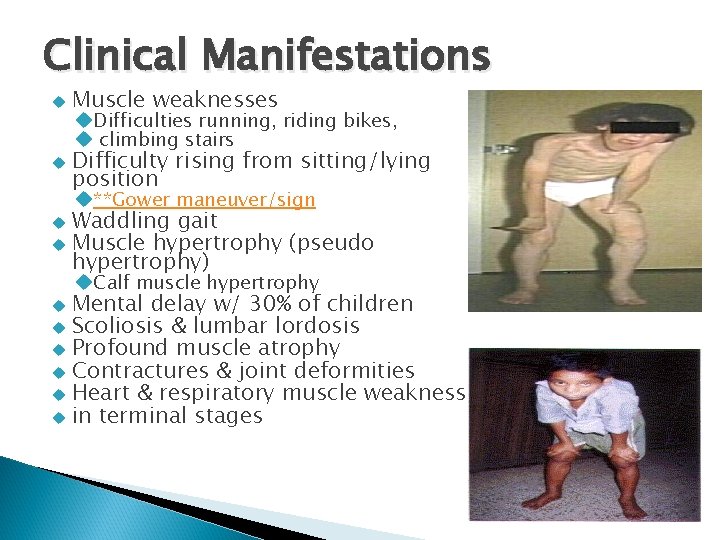
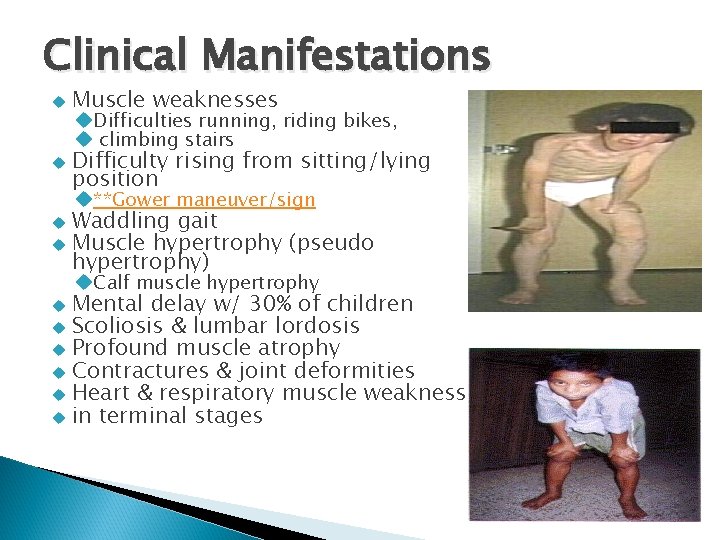
Clinical Manifestations Muscle weaknesses Difficulty rising from sitting/lying position Difficulties running, riding bikes, climbing stairs **Gower maneuver/sign Waddling gait Muscle hypertrophy (pseudo hypertrophy) Calf muscle hypertrophy Mental delay w/ 30% of children Scoliosis & lumbar lordosis Profound muscle atrophy Contractures & joint deformities Heart & respiratory muscle weakness in terminal stages
Diagnosis DMD Clinical symptoms **Polymerase Chain Reaction (PCR) for the dystrophin gene mutation Serum Enzyme assay Muscle biopsy EMG Creatine kinase levels
Therapeutic Management Goals of treatment: Maintain optimal function Prevent contractures No effective treatment exists Corticosteroids used Research on gene & stem cell therapy Multidisciplinary Approach Care PT, OT, Neurologist, Orthopedist Assist family with care & coping Prevent & treat respiratory infections Cardiac Evaluation Genetic Counseling
Nursing Care for DMD Physical NANDA’s Activity Intolerance Ineffective Breathing Pattern Impaired Skin Integrity Risk for infection Risk of Constipation Risk for Falls Imbalanced Nutrition Psychosocial NANDA’s Caregiver Role Strain Anxiety, Hopelessness Compromised family coping Anticipatory Grievance
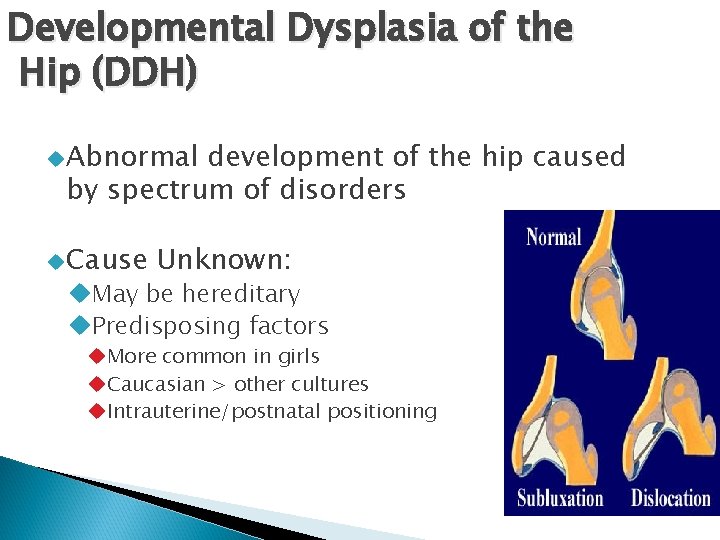
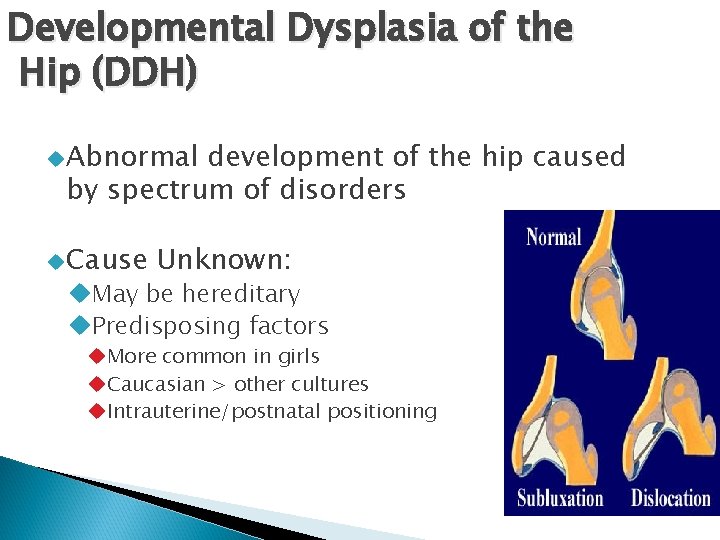
Developmental Dysplasia of the Hip (DDH) Abnormal development of the hip caused by spectrum of disorders Cause Unknown: May be hereditary Predisposing factors More common in girls Caucasian > other cultures Intrauterine/postnatal positioning
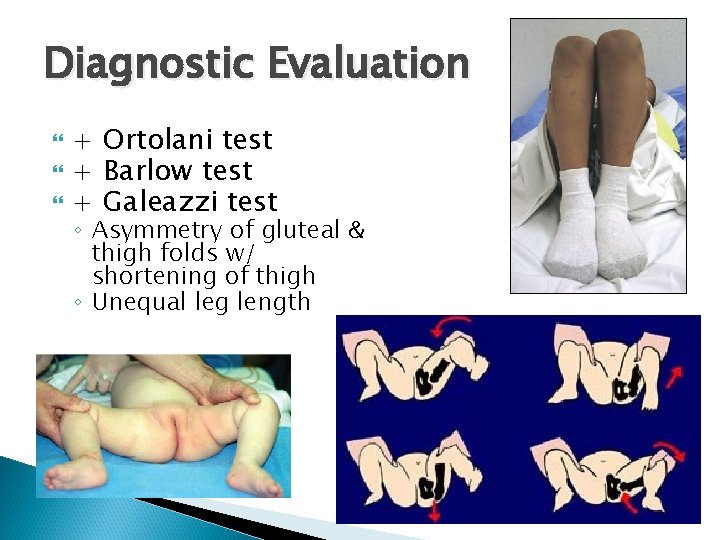
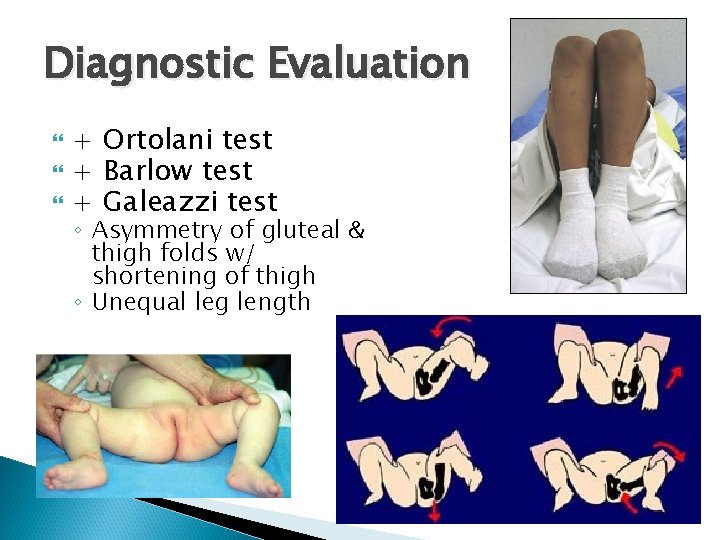
Diagnostic Evaluation + Ortolani test + Barlow test + Galeazzi test ◦ Asymmetry of gluteal & thigh folds w/ shortening of thigh ◦ Unequal leg length
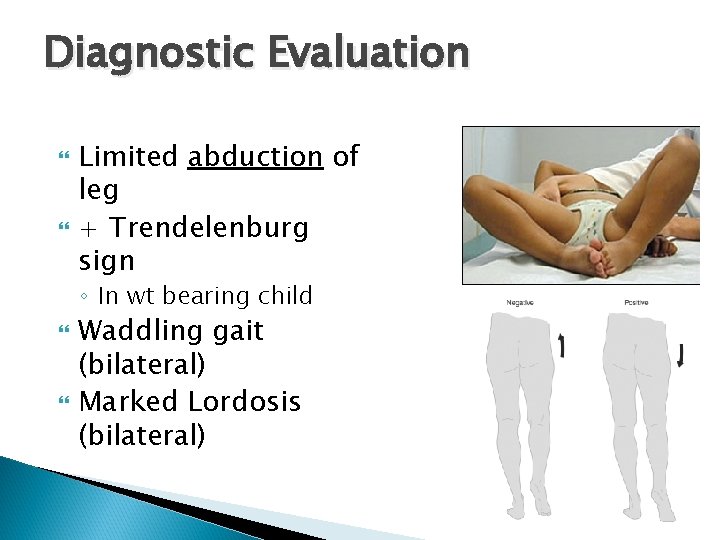
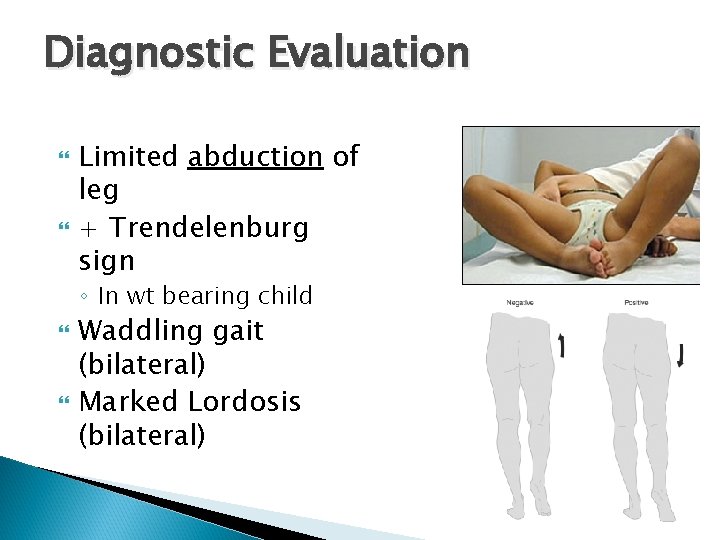
Diagnostic Evaluation Limited abduction of leg + Trendelenburg sign ◦ In wt bearing child Waddling gait (bilateral) Marked Lordosis (bilateral)
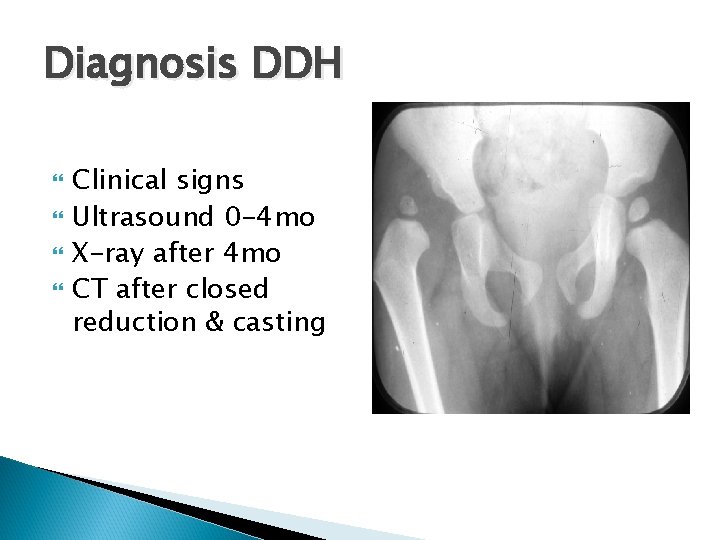
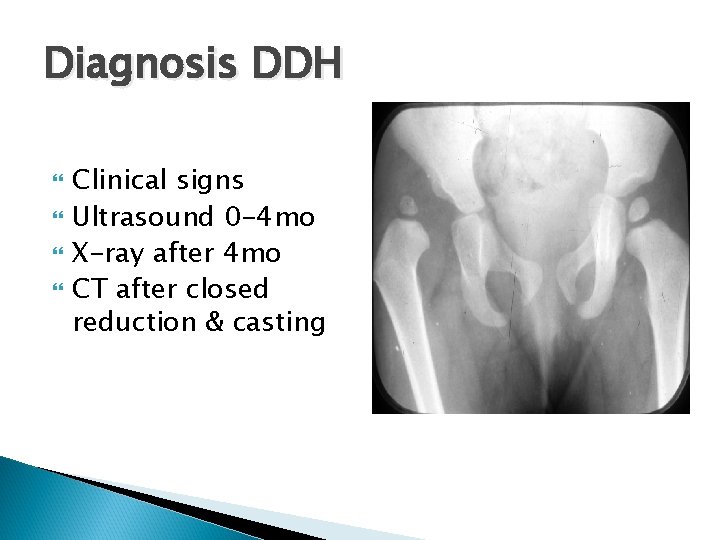
Diagnosis DDH Clinical signs Ultrasound 0 -4 mo X-ray after 4 mo CT after closed reduction & casting
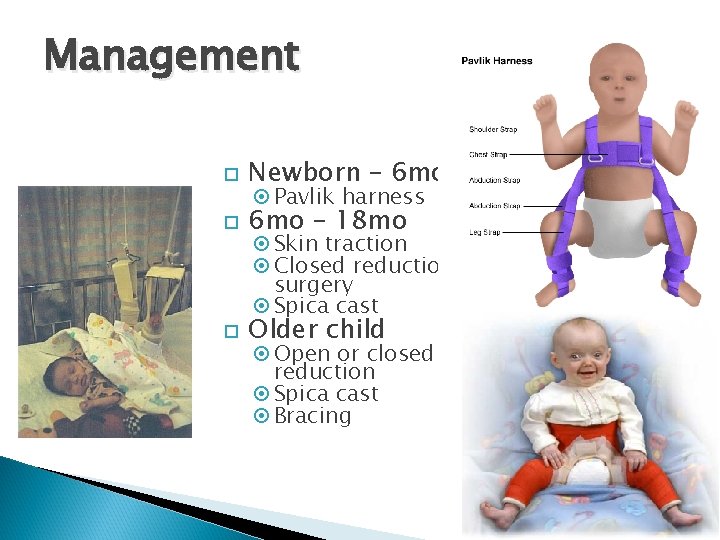
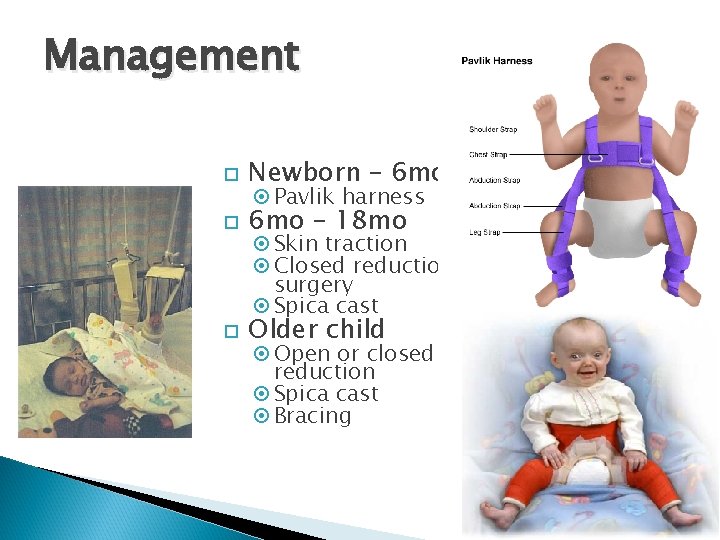
Management Newborn – 6 mo – 18 mo Older child Pavlik harness Skin traction Closed reduction surgery Spica cast Open or closed reduction Spica cast Bracing
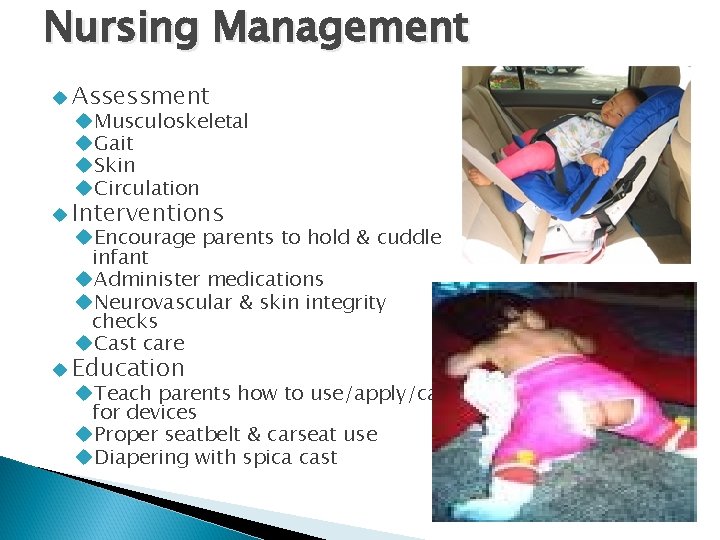
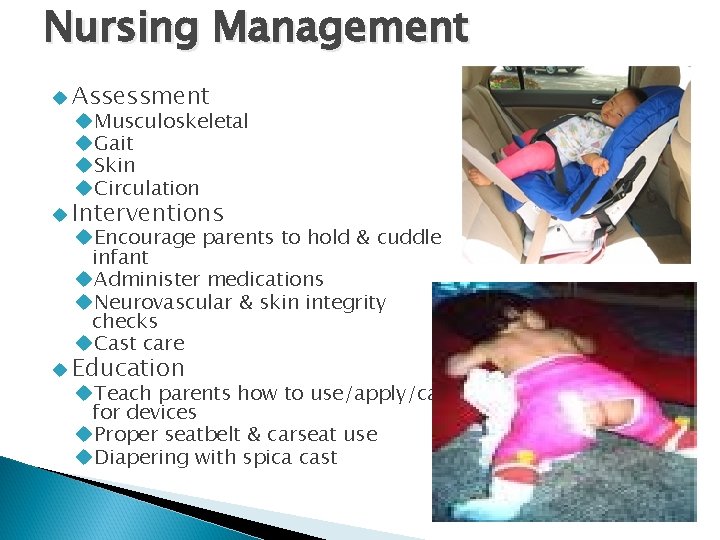
Nursing Management Assessment Musculoskeletal Gait Skin Circulation Interventions Encourage parents to hold & cuddle infant Administer medications Neurovascular & skin integrity checks Cast care Education Teach parents how to use/apply/care for devices Proper seatbelt & carseat use Diapering with spica cast
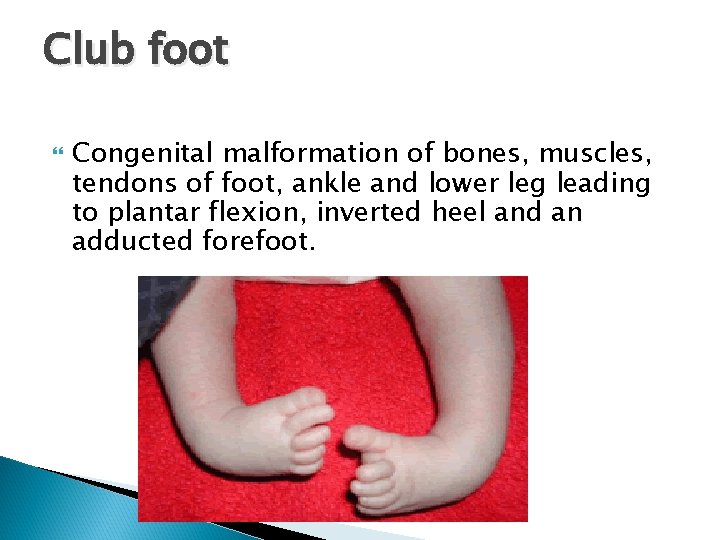
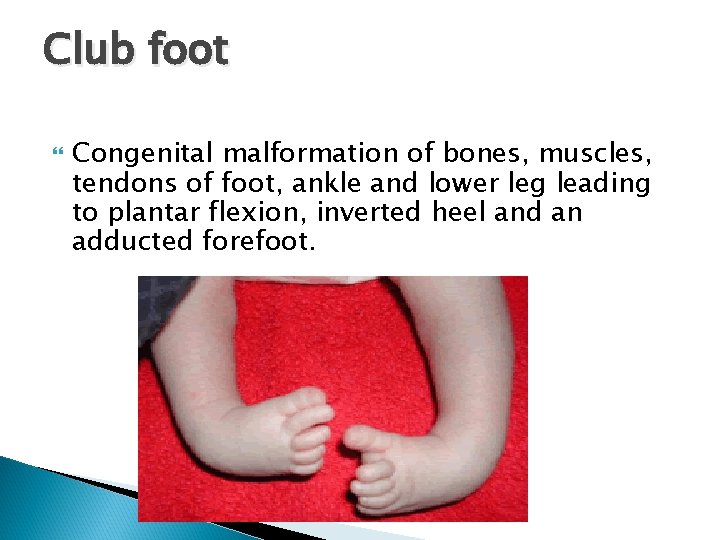
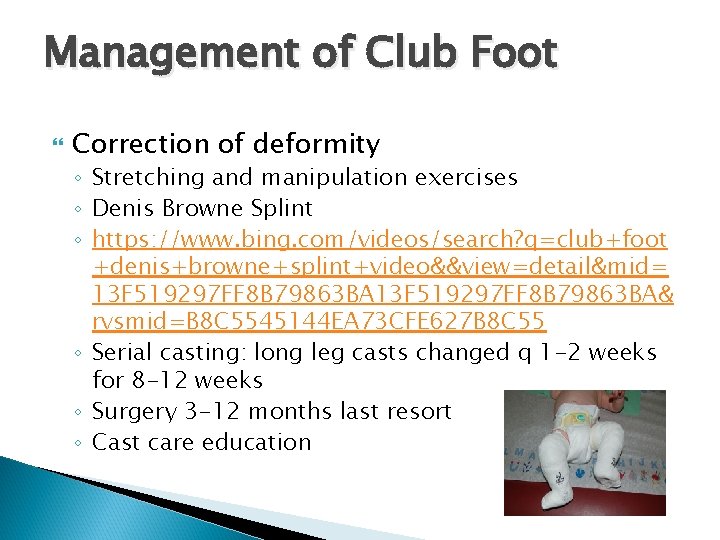
Club foot Congenital malformation of bones, muscles, tendons of foot, ankle and lower leg leading to plantar flexion, inverted heel and an adducted forefoot.
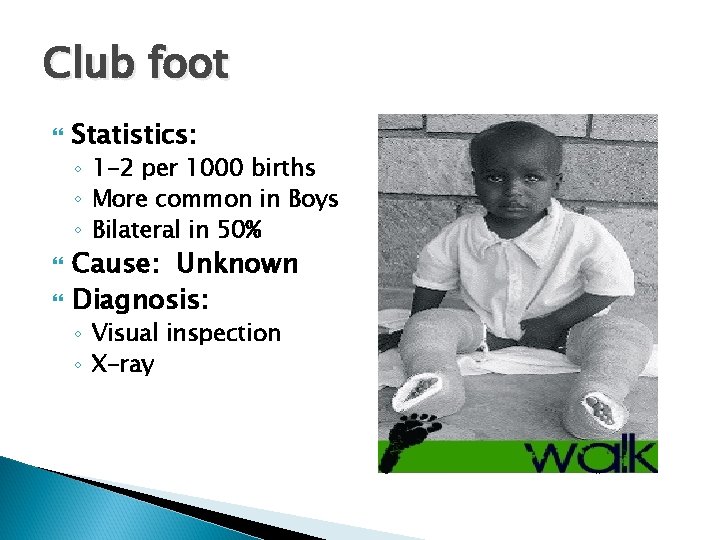
Club foot Statistics: ◦ 1 -2 per 1000 births ◦ More common in Boys ◦ Bilateral in 50% Cause: Unknown Diagnosis: ◦ Visual inspection ◦ X-ray
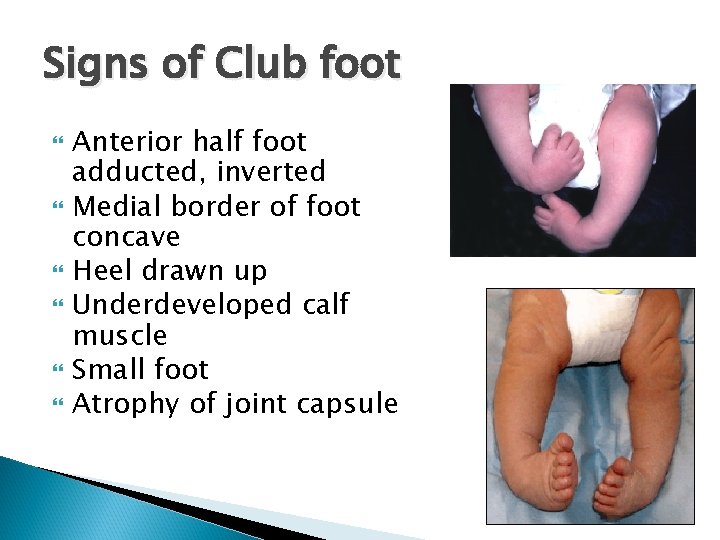
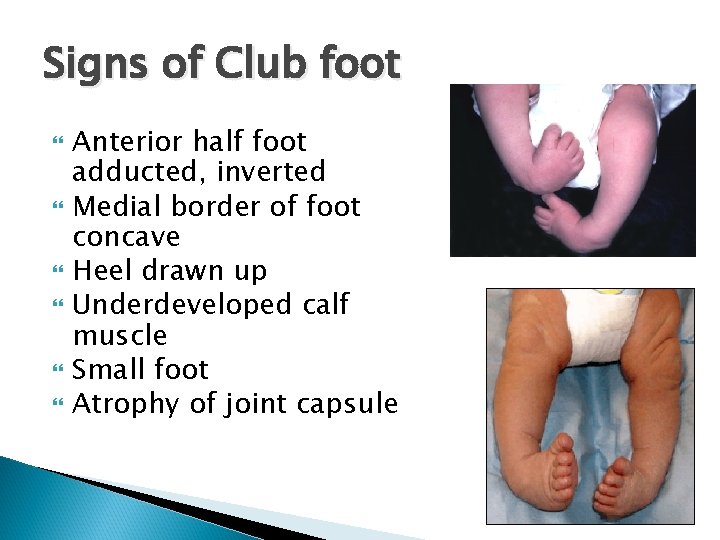
Signs of Club foot Anterior half foot adducted, inverted Medial border of foot concave Heel drawn up Underdeveloped calf muscle Small foot Atrophy of joint capsule

Denis Browne Splint
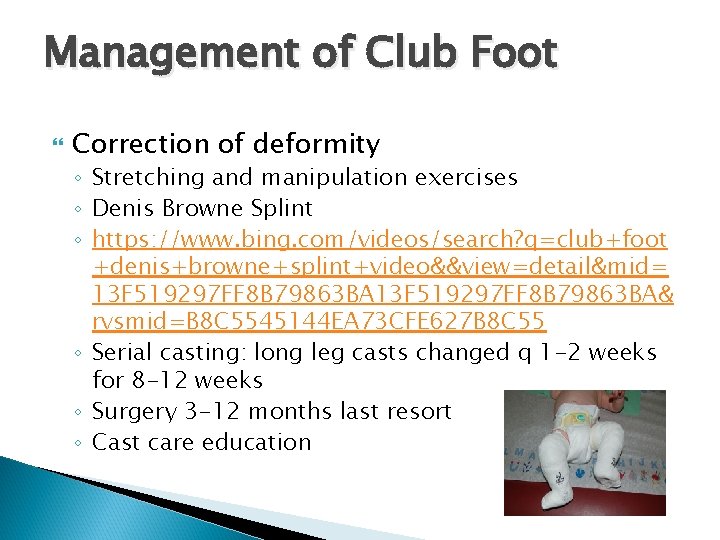
Management of Club Foot Correction of deformity ◦ Stretching and manipulation exercises ◦ Denis Browne Splint ◦ https: //www. bing. com/videos/search? q=club+foot +denis+browne+splint+video&&view=detail&mid= 13 F 519297 FF 8 B 79863 BA& rvsmid=B 8 C 5545144 EA 73 CFE 627 B 8 C 55 ◦ Serial casting: long leg casts changed q 1 -2 weeks for 8 -12 weeks ◦ Surgery 3 -12 months last resort ◦ Cast care education
Osteogenesis Imperfecta (OI): Brittle Bone Disease Genetic defect in the production of collagen resulting in faulty bone mineralization, abnormal bone architecture & increased susceptibility to fracture 1 : 30, 000 births 6 types with varying severity

OI Diagnosis & Management Diagnosis Therapeutic Management Multiple fx in various stages of healing Blue sclerae DEXA & Elevated Alk Phos Supportive care Pamidronate infusions Braces & splints PT Surgery High Calcium & vitamin D diet Nursing Management Assessment Education Support
Infectious Musculoskeletal Disorders
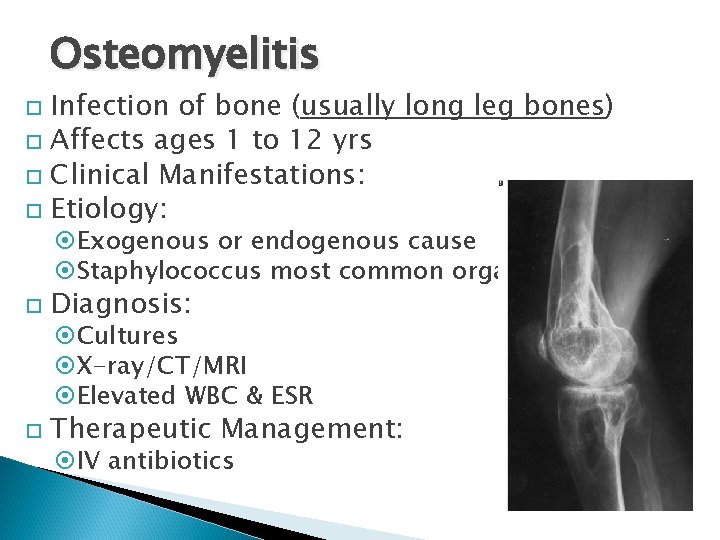
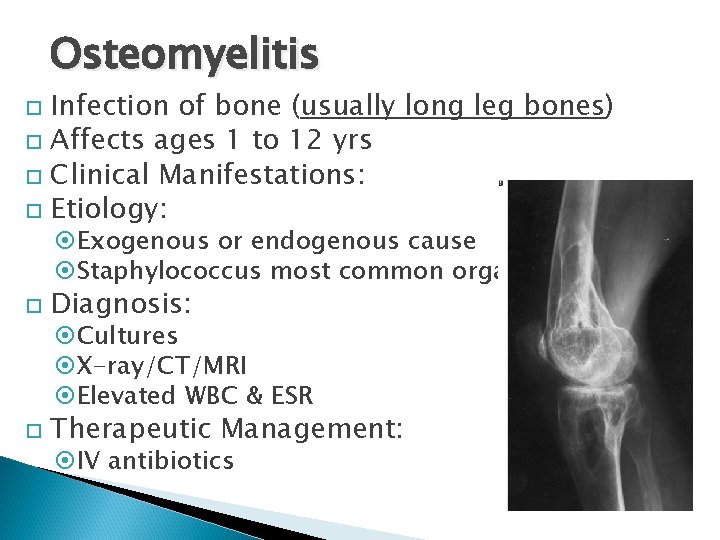
Osteomyelitis Infection of bone (usually long leg bones) Affects ages 1 to 12 yrs Clinical Manifestations: Etiology: Exogenous or endogenous cause Staphylococcus most common organism Diagnosis: Therapeutic Management: Cultures X-ray/CT/MRI Elevated WBC & ESR IV antibiotics
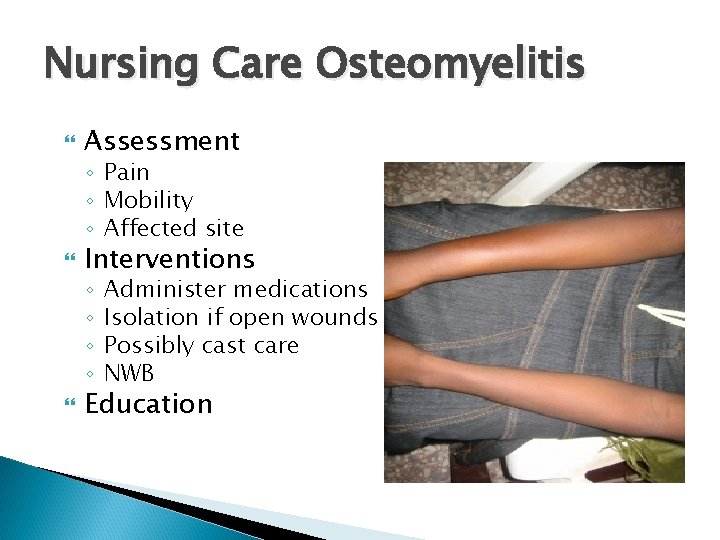
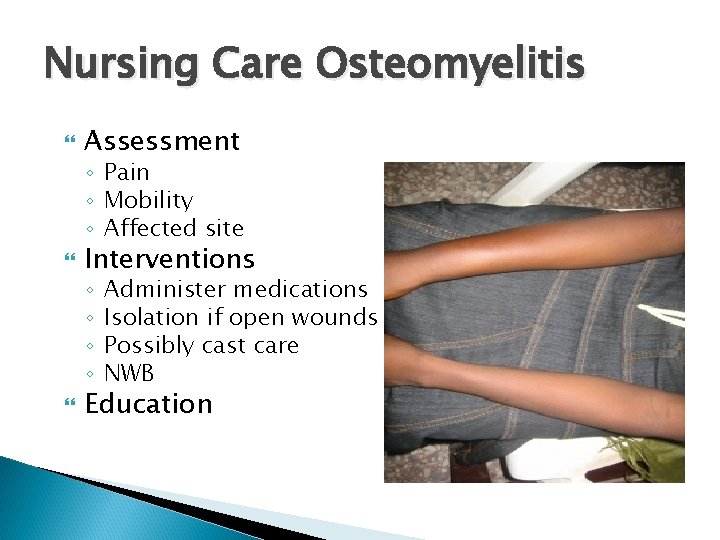
Nursing Care Osteomyelitis Assessment ◦ Pain ◦ Mobility ◦ Affected site Interventions ◦ ◦ Administer medications Isolation if open wounds Possibly cast care NWB Education
Acquired Musculoskeletal Defects
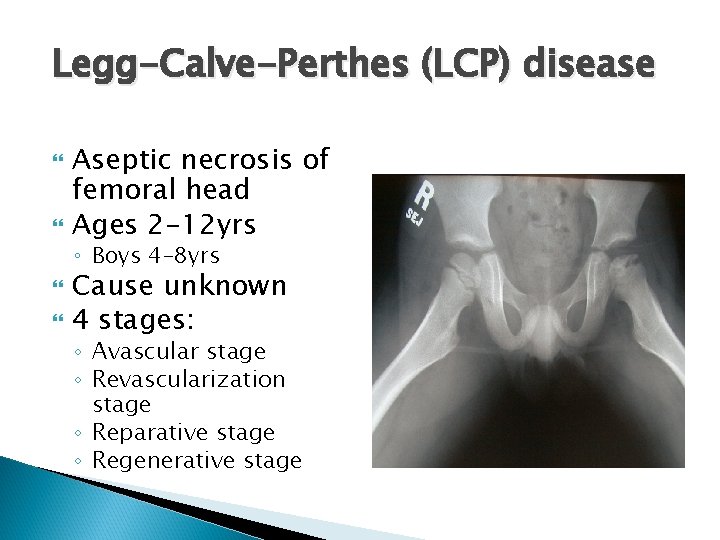
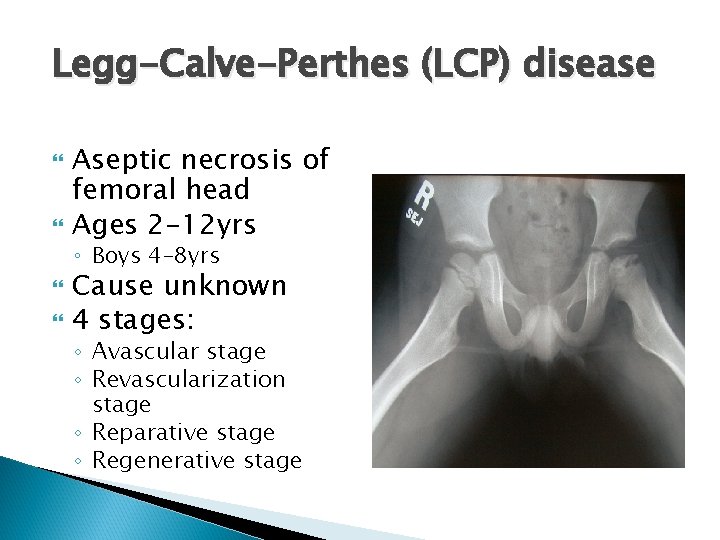
Legg-Calve-Perthes (LCP) disease Aseptic necrosis of femoral head Ages 2 -12 yrs ◦ Boys 4 -8 yrs Cause unknown 4 stages: ◦ Avascular stage ◦ Revascularization stage ◦ Reparative stage ◦ Regenerative stage
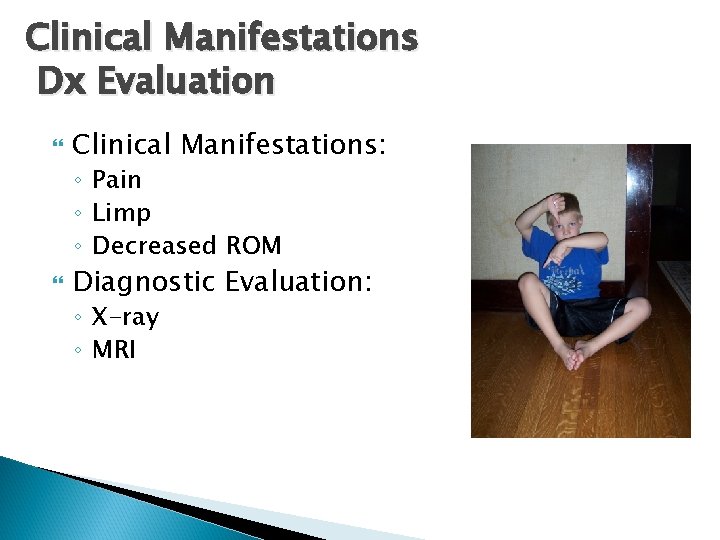
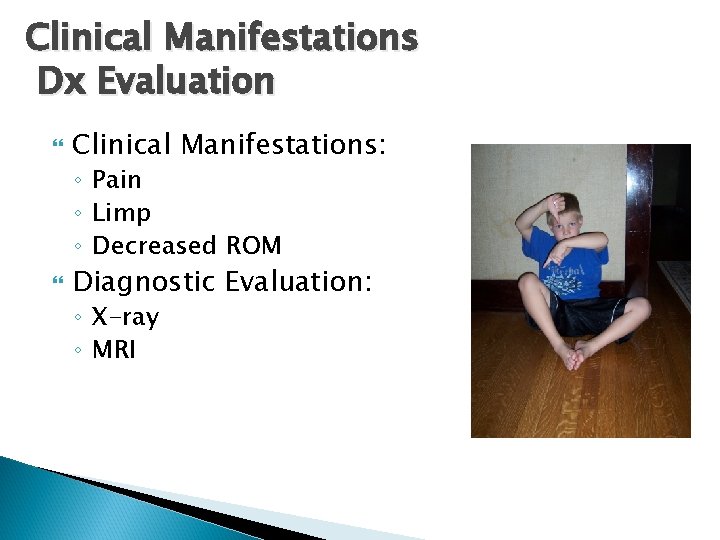
Clinical Manifestations Dx Evaluation Clinical Manifestations: ◦ Pain ◦ Limp ◦ Decreased ROM Diagnostic Evaluation: ◦ X-ray ◦ MRI
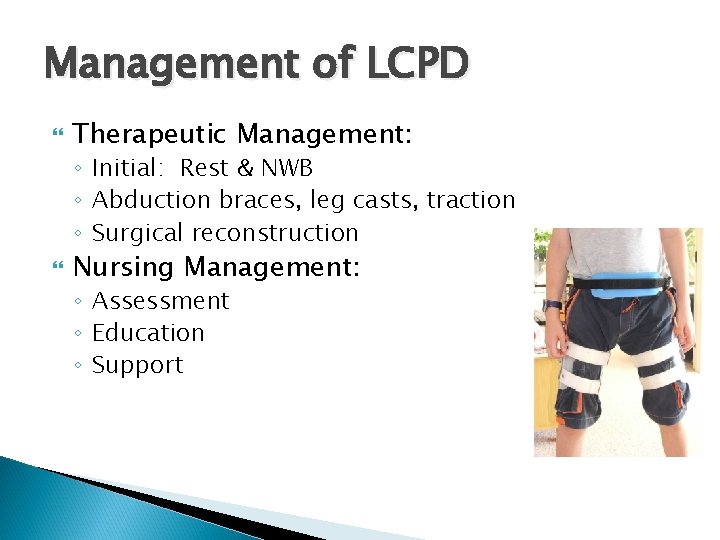
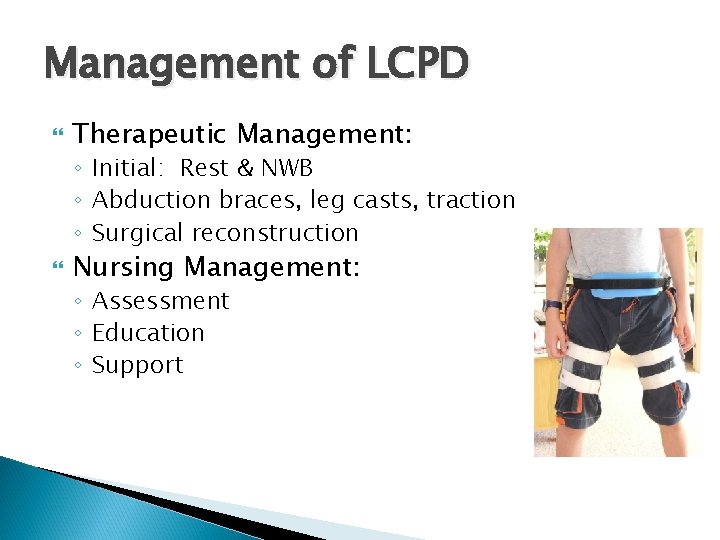
Management of LCPD Therapeutic Management: ◦ Initial: Rest & NWB ◦ Abduction braces, leg casts, traction ◦ Surgical reconstruction Nursing Management: ◦ Assessment ◦ Education ◦ Support
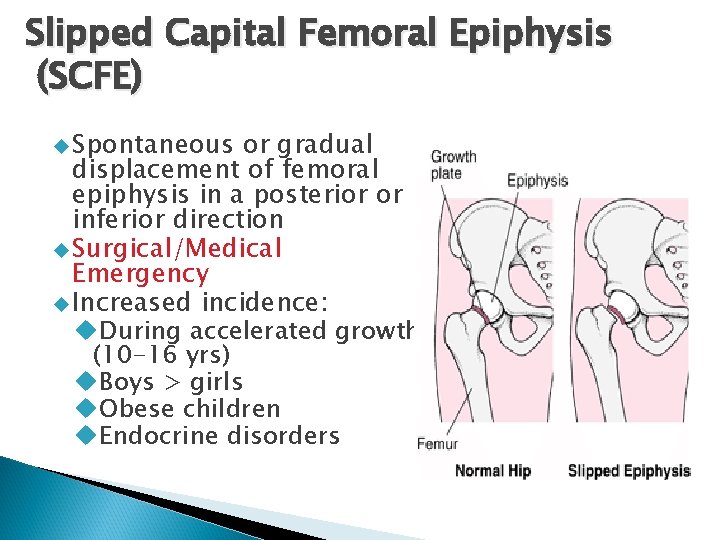
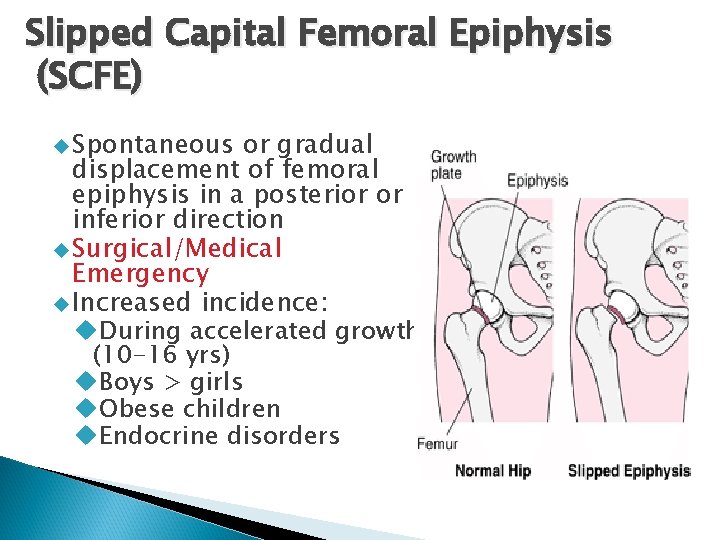
Slipped Capital Femoral Epiphysis (SCFE) Spontaneous or gradual displacement of femoral epiphysis in a posterior or inferior direction Surgical/Medical Emergency Increased incidence: During accelerated growth (10 -16 yrs) Boys > girls Obese children Endocrine disorders
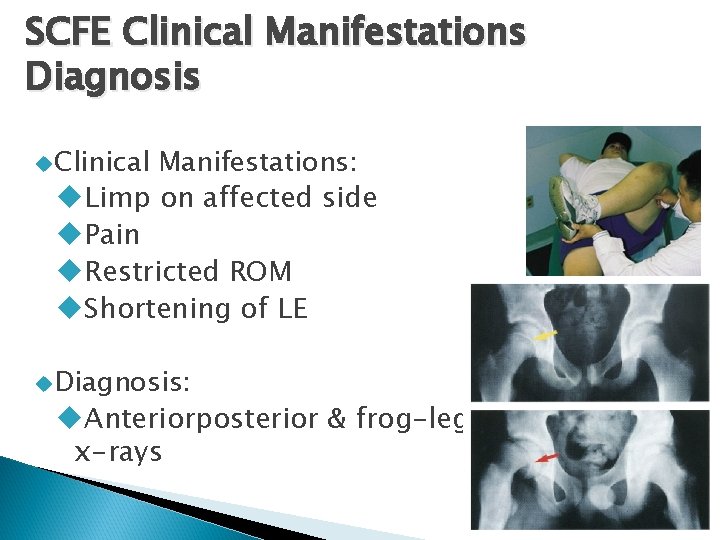
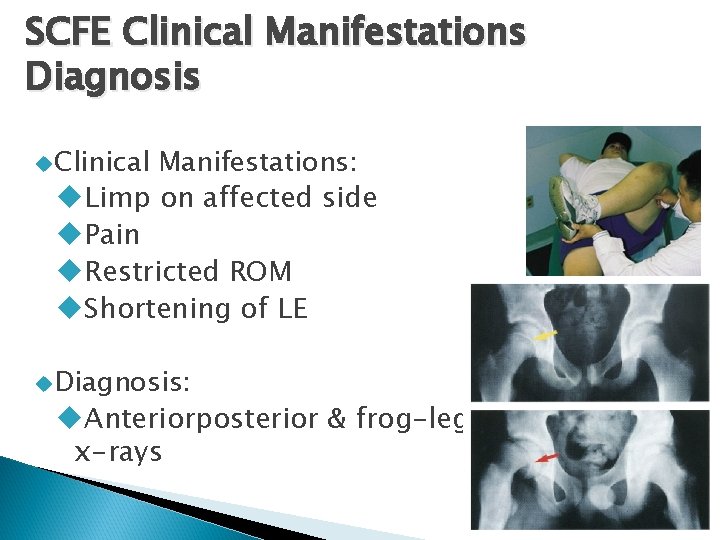
SCFE Clinical Manifestations Diagnosis Clinical Manifestations: Limp on affected side Pain Restricted ROM Shortening of LE Diagnosis: Anteriorposterior & frog-leg x-rays
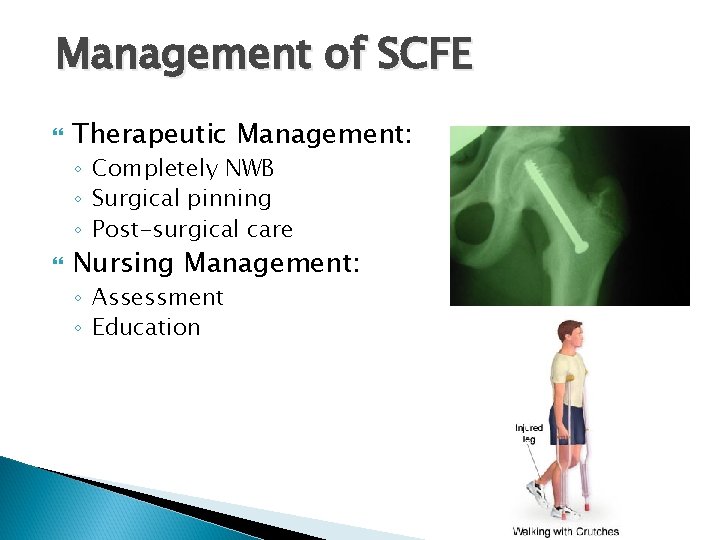
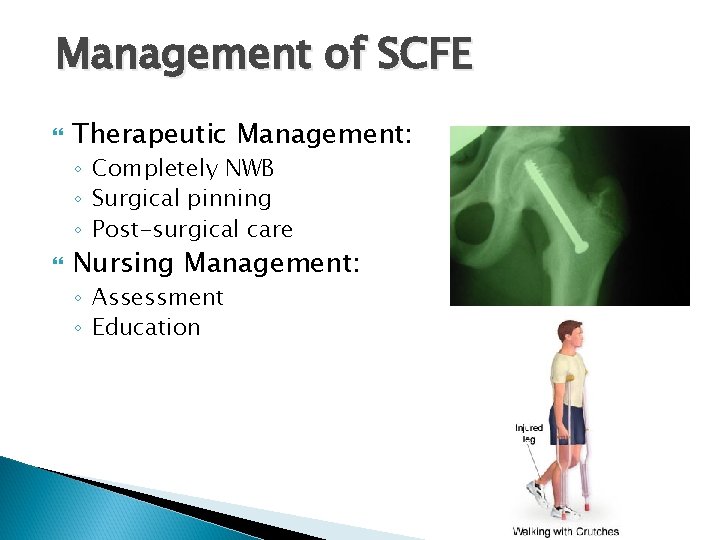
Management of SCFE Therapeutic Management: ◦ Completely NWB ◦ Surgical pinning ◦ Post-surgical care Nursing Management: ◦ Assessment ◦ Education
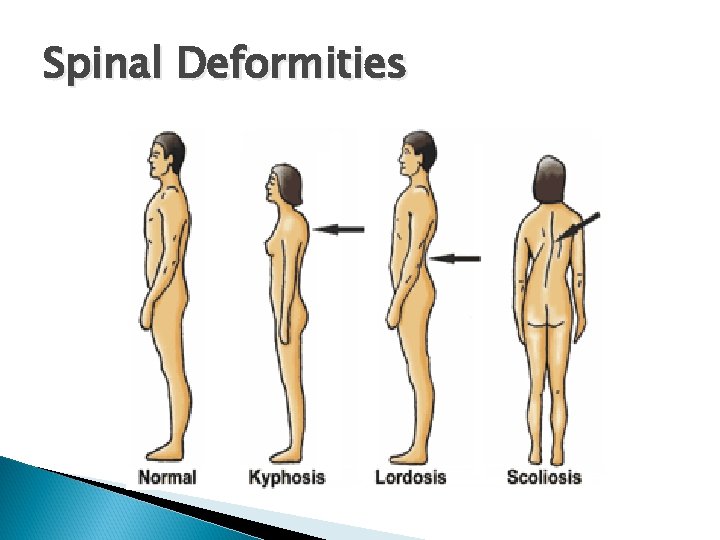
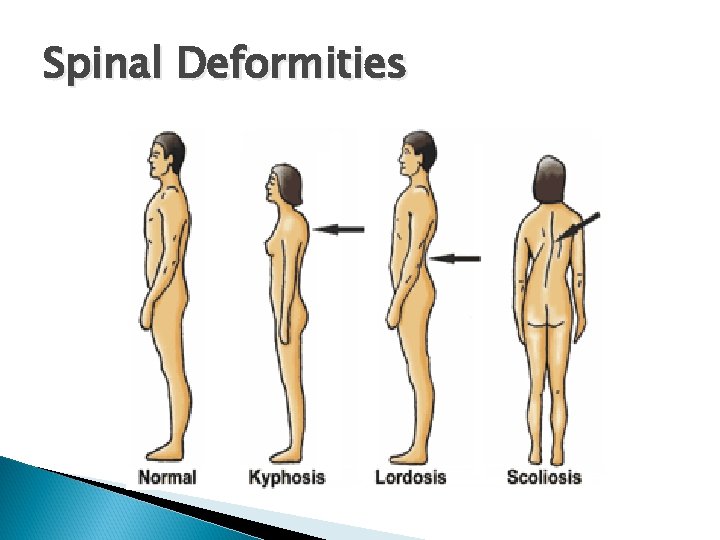
Spinal Deformities
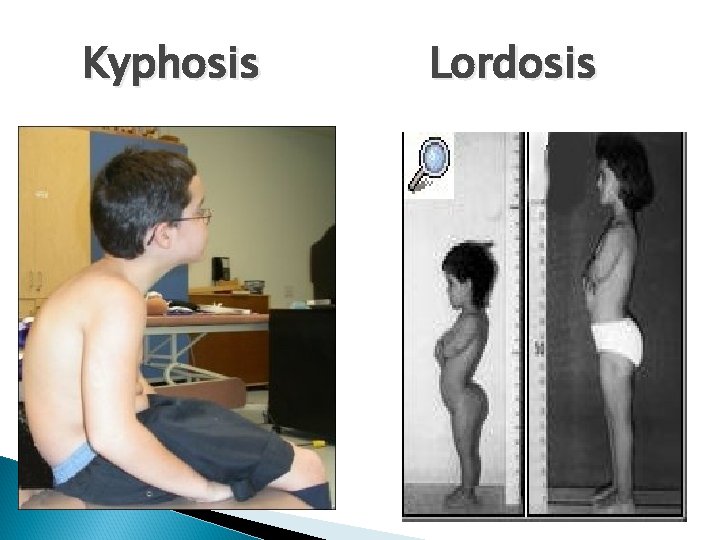
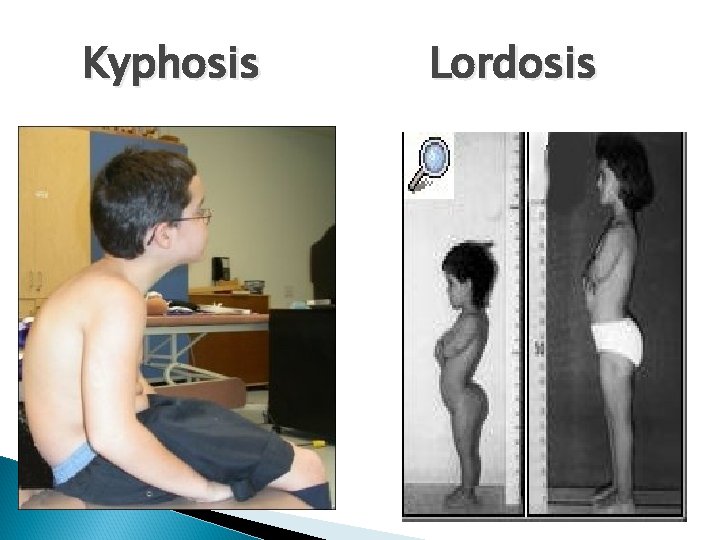
Kyphosis Lordosis
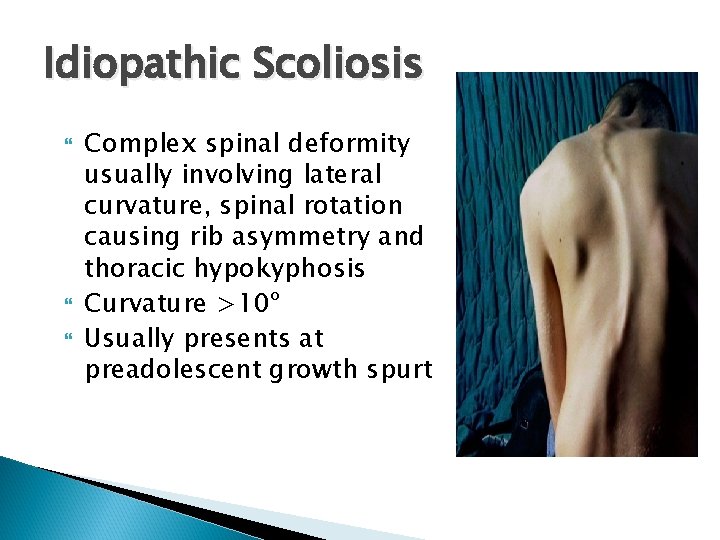
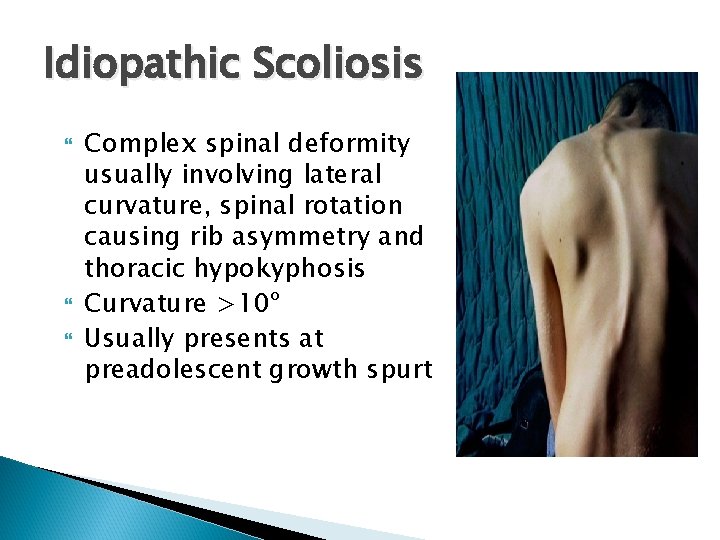
Idiopathic Scoliosis Complex spinal deformity usually involving lateral curvature, spinal rotation causing rib asymmetry and thoracic hypokyphosis Curvature >10º Usually presents at preadolescent growth spurt
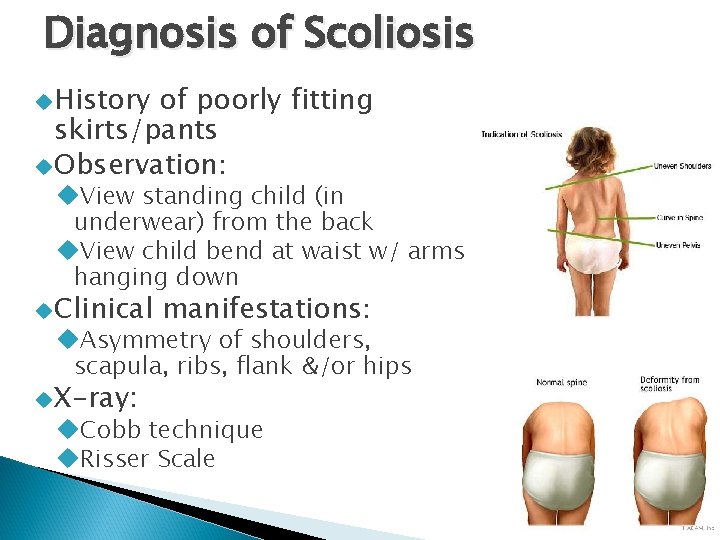
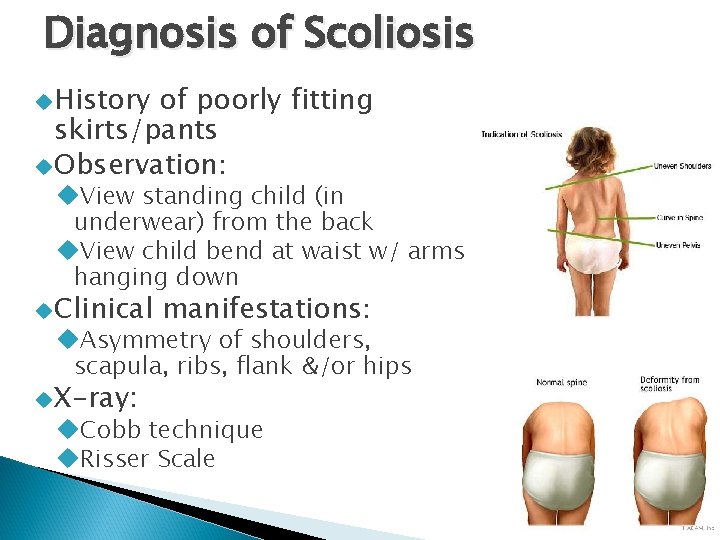
Diagnosis of Scoliosis History of poorly fitting skirts/pants Observation: View standing child (in underwear) from the back View child bend at waist w/ arms hanging down Clinical manifestations: Asymmetry of shoulders, scapula, ribs, flank &/or hips X-ray: Cobb technique Risser Scale
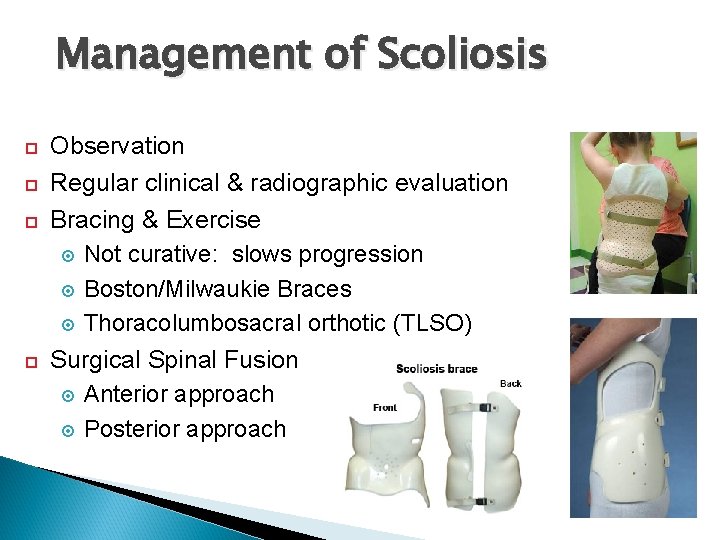
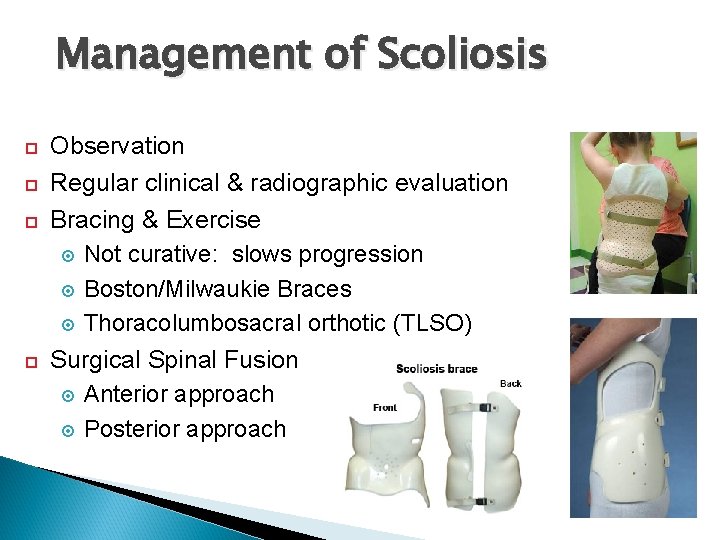
Management of Scoliosis Observation Regular clinical & radiographic evaluation Bracing & Exercise Not curative: slows progression Boston/Milwaukie Braces Thoracolumbosacral orthotic (TLSO) Surgical Spinal Fusion Anterior approach Posterior approach
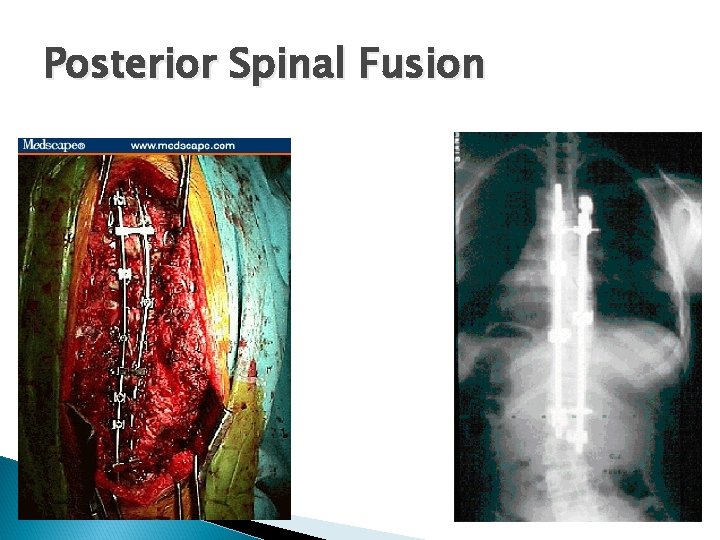
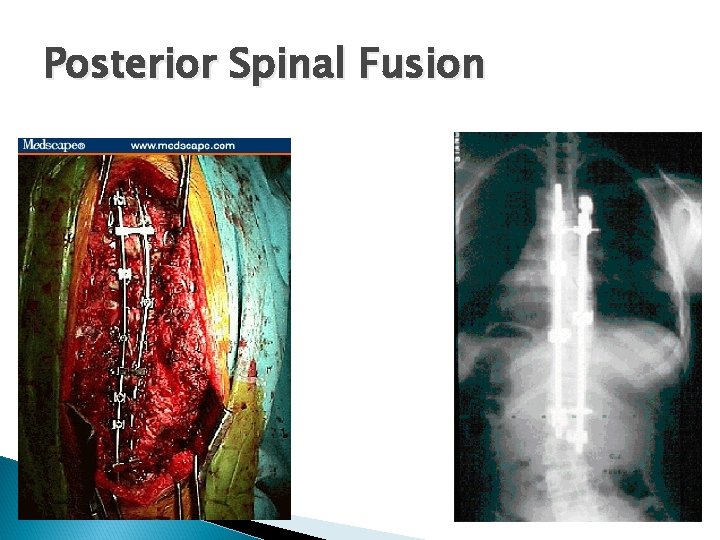
Posterior Spinal Fusion
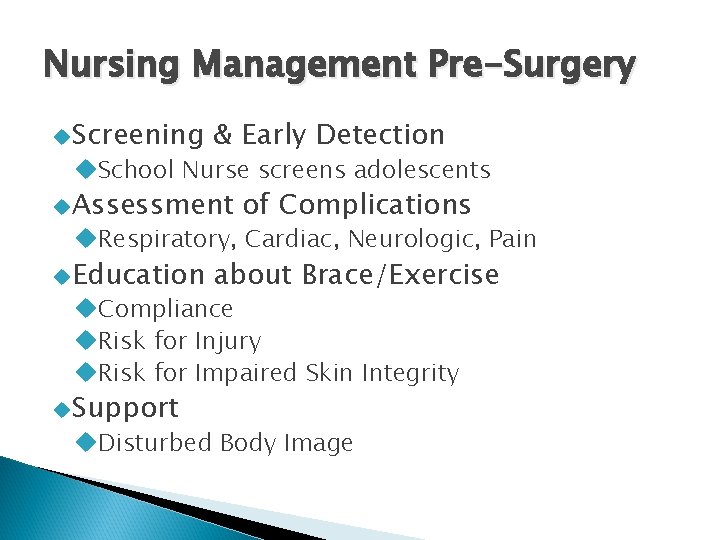
Nursing Management Pre-Surgery Screening & Early Detection School Nurse screens adolescents Assessment of Complications Respiratory, Cardiac, Neurologic, Pain Education about Brace/Exercise Compliance Risk for Injury Risk for Impaired Skin Integrity Support Disturbed Body Image
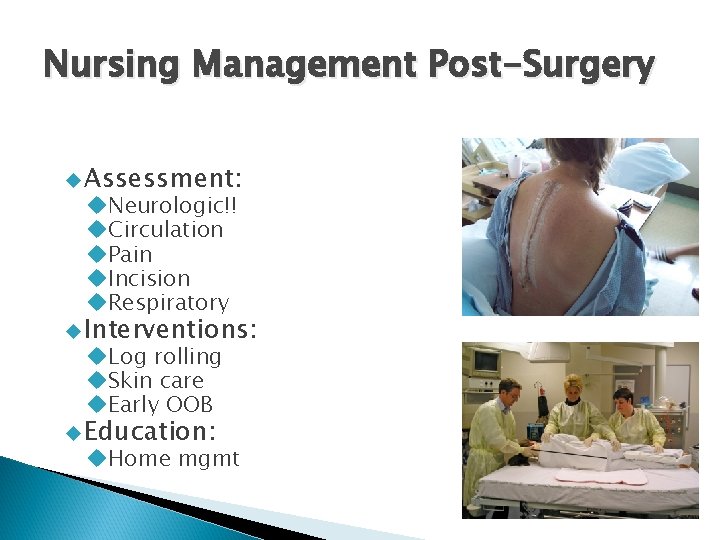
Nursing Management Post-Surgery Assessment: Neurologic!! Circulation Pain Incision Respiratory Interventions: Log rolling Skin care Early OOB Education: Home mgmt
A critical post op assessment for an adolescent with scoliosis who has undergone a spinal fusion is: A. Urinary Output B. Bowel Elimination C. Infection D. Sensation and movement of extremities Rationale?
While a child’s body cast is still damp, the nurse should: A. B. C. D. Attempt to dry the cast using a hairdryer Refrain from placing pillows under the cast Avoid using the palms of the hands on the cast when positioning the child Turn the child q 2 hours
A child returns from surgery in a hip spica cast. The nurse’s first action is to: A. B. C. D. Circle and note the date and time of any drainage on the cast. Note any rough edges on the cast. Assess the cast for areas of dampness. Check circulation to the toes.
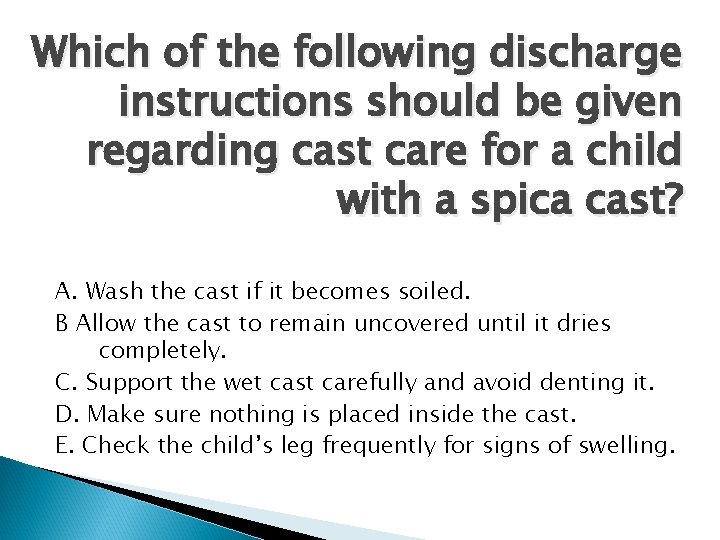
Which of the following discharge instructions should be given regarding cast care for a child with a spica cast? A. Wash the cast if it becomes soiled. B Allow the cast to remain uncovered until it dries completely. C. Support the wet cast carefully and avoid denting it. D. Make sure nothing is placed inside the cast. E. Check the child’s leg frequently for signs of swelling.
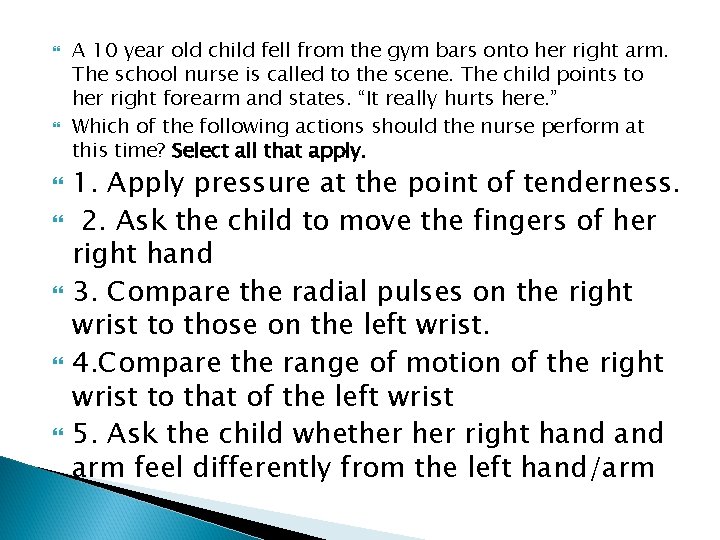
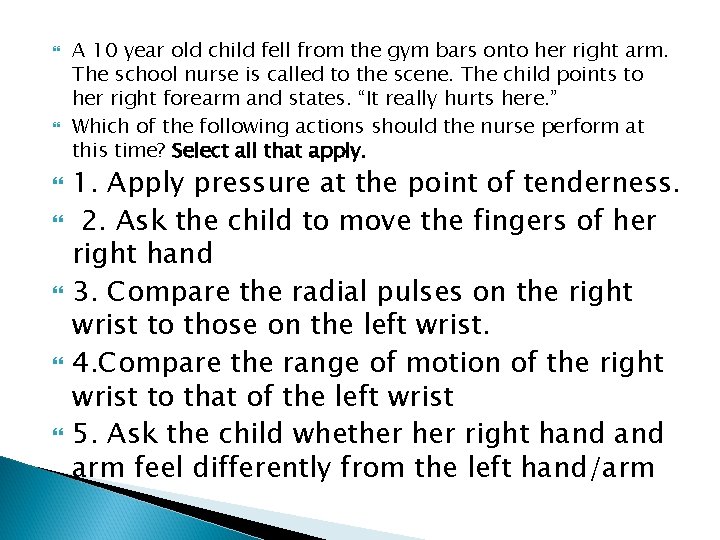
A 10 year old child fell from the gym bars onto her right arm. The school nurse is called to the scene. The child points to her right forearm and states. “It really hurts here. ” Which of the following actions should the nurse perform at this time? Select all that apply. 1. Apply pressure at the point of tenderness. 2. Ask the child to move the fingers of her right hand 3. Compare the radial pulses on the right wrist to those on the left wrist. 4. Compare the range of motion of the right wrist to that of the left wrist 5. Ask the child whether right hand arm feel differently from the left hand/arm
 Cpnp create an account
Cpnp create an account Eu cosmetic product notification portal (cpnp)
Eu cosmetic product notification portal (cpnp) Epiphysis metaphysis diaphysis
Epiphysis metaphysis diaphysis Epiphysis fuga
Epiphysis fuga Trabecula directriz histologia
Trabecula directriz histologia Epiphyseal growth plates
Epiphyseal growth plates How to know if your growth plates have closed
How to know if your growth plates have closed Proximal epiphysis
Proximal epiphysis Vertebral column labeled
Vertebral column labeled Epiphysis
Epiphysis The musculoskeletal system chapter 21
The musculoskeletal system chapter 21 Musculoskeletal system
Musculoskeletal system Chapter 6 musculoskeletal system
Chapter 6 musculoskeletal system Chapter 15 musculoskeletal system step by step
Chapter 15 musculoskeletal system step by step Unit 41 musculoskeletal system
Unit 41 musculoskeletal system Musculoskeletal system
Musculoskeletal system Musculoskeletal medical terminology
Musculoskeletal medical terminology Diseases of the musculoskeletal system
Diseases of the musculoskeletal system Assessment of the musculoskeletal system
Assessment of the musculoskeletal system Muscle strength scale
Muscle strength scale Musculoskeletal system
Musculoskeletal system Objective data for musculoskeletal system
Objective data for musculoskeletal system Instant messenger msn
Instant messenger msn Msn
Msn Chamberlain fnp practicum handbook
Chamberlain fnp practicum handbook Microsoft eou
Microsoft eou Msn wetter jakutsk
Msn wetter jakutsk Msn dating
Msn dating Msn messenger chat rooms
Msn messenger chat rooms Messenger
Messenger Legal nurse consultant report template
Legal nurse consultant report template Msn
Msn Msn 1886
Msn 1886 Alverno direct entry msn
Alverno direct entry msn Msn
Msn Bebo messenger
Bebo messenger Msn yoga
Msn yoga Vital signs definition
Vital signs definition How many curves are in a standard paper clip
How many curves are in a standard paper clip Pediatric dosage calculations for nurses
Pediatric dosage calculations for nurses Msn ph
Msn ph L fon
L fon Gpio_set_mask
Gpio_set_mask Barb bancroft
Barb bancroft Bruit msn
Bruit msn Msn cloud storage
Msn cloud storage Icd 10 code for musculoskeletal spasm
Icd 10 code for musculoskeletal spasm Muscle loss icd 10
Muscle loss icd 10