Minimally Invasive Parathyroidectomy for Primary Hyperparathyroidism Joint Hospital


- Slides: 24
Minimally Invasive Parathyroidectomy for Primary Hyperparathyroidism Joint Hospital Surgical Grand Round 18 April 2009 Dr. David KW Leung United Christian Hospital
Outline ß ß Primary hyperparathyroidism Surgical treatment Þ Þ ß Bilateral neck exploration Minimally invasive parathyroidectomy (MIP) Conclusion
Definition Primary hyperparathyroidism A sporadic or familial disorder associated with hyper. Ca, elevated or inappropriately raised PTH levels and parathyroid gland enlargement Bailey & Love’s Short Practice of Surgery
Parathyroidectomy Conventional bilateral cervical exploration Minimally invasive/ Limited parathyroidectomy
Bilateral neck exploration ß ß ‘Gold standard’ Pre-op localization of abnormal parathyroid gland not mandatory The success is based on a thorough knowledge of the anatomy and embryological evolution of the glands Success rate – 95 -98%
Bilateral neck exploration ß To identify all 4 parathyroid glands Þ Þ Only enlarged glands are removed whether single- or multiple- gland disease found If 4 glands are enlarged, subtotal parathyroidectomy is performed; leaving a single vascularized gland remnant no larger than a normal parathyroid
Limited/minimal invasive parathyroidectomy ß The need for routine bilateral neck exploration being challenged because: Þ Þ Þ Pathology of the disease Improvement of pre-op localization studies Introduction of quick parathyroid hormone assay (QPTH) Confirm removal of all hyper-functioning parathyroid tissue
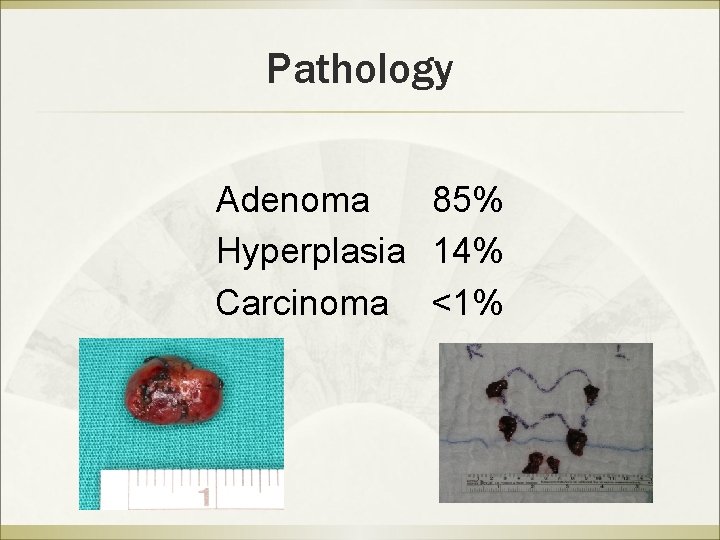
Pathology Adenoma 85% Hyperplasia 14% Carcinoma <1%
Imaging and pre-op localization Ultrasound technetium-99 M sestamibi scan (MIBI) CT scan MRI parathyroid angiography/ selective venous sampling
Ultrasound ß ß Sensitivity 70 -80% Lower sensitivity in re-operative cases False-positive (15 -20%) due to muscle, vessels, thyroid nodules, LN and oesophageal pathology has difficulty locating abnormalities in the retro-oesophageal, retrosternal, retrotracheal and deep cervical areas
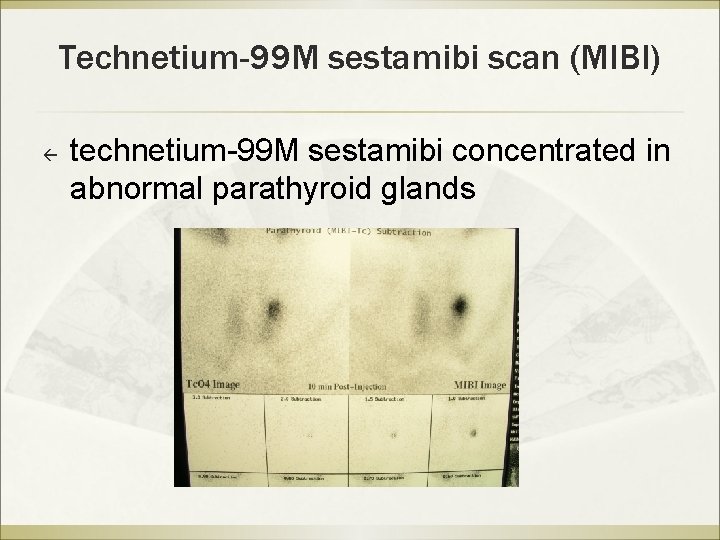
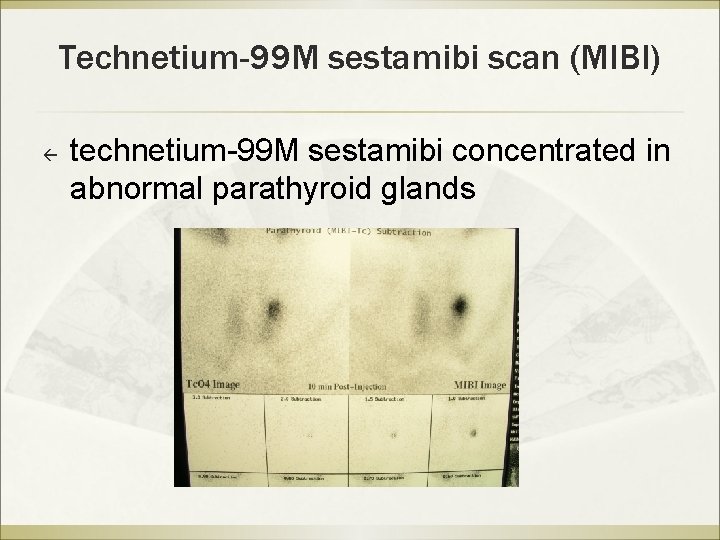
Technetium-99 M sestamibi scan (MIBI) ß technetium-99 M sestamibi concentrated in abnormal parathyroid glands
Technetium-99 M sestamibi scan (MIBI) ß Sensitivity 80 -100% ß drawbacks Þ Þ Not always identify patients with multiple adenomas or four-gland hyperplasia Failed to localized small adenomas
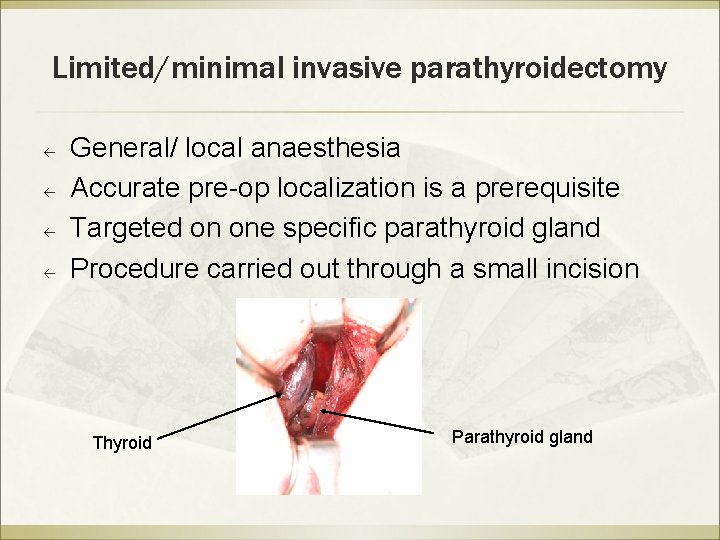
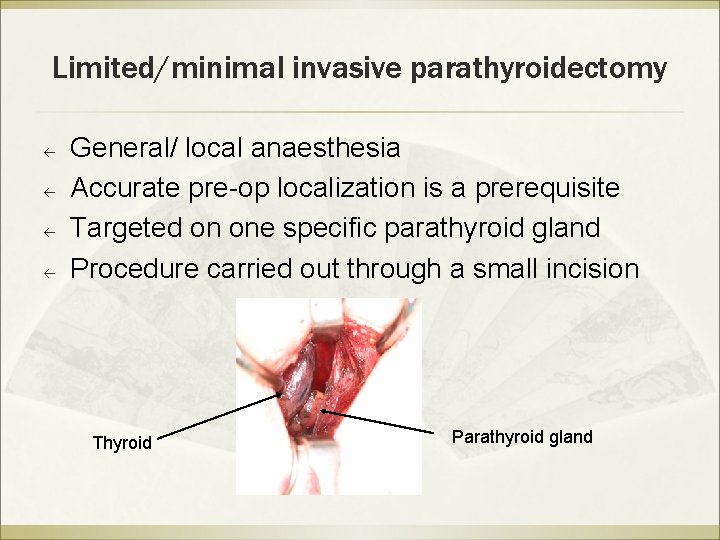
Limited/minimal invasive parathyroidectomy ß ß General/ local anaesthesia Accurate pre-op localization is a prerequisite Targeted on one specific parathyroid gland Procedure carried out through a small incision Thyroid Parathyroid gland
Limited/minimal invasive parathyroidectomy ß Exclusion Þ Þ Suspected multiple - gland disease on imaging studies History of familial hyperparathyroidism or multiple endocrine neoplasia
Evidence-based?
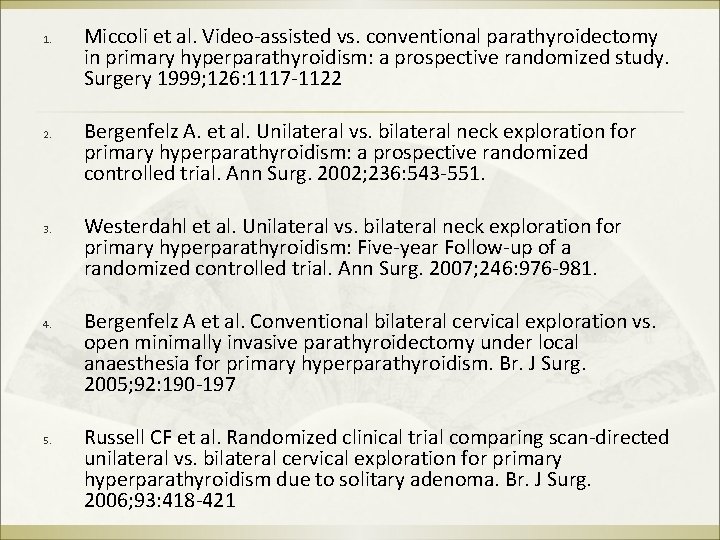
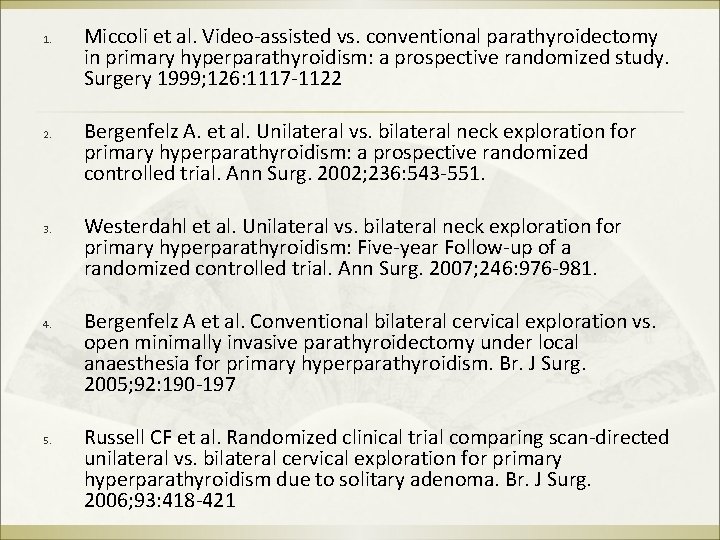
1. 2. 3. 4. 5. Miccoli et al. Video-assisted vs. conventional parathyroidectomy in primary hyperparathyroidism: a prospective randomized study. Surgery 1999; 126: 1117 -1122 Bergenfelz A. et al. Unilateral vs. bilateral neck exploration for primary hyperparathyroidism: a prospective randomized controlled trial. Ann Surg. 2002; 236: 543 -551. Westerdahl et al. Unilateral vs. bilateral neck exploration for primary hyperparathyroidism: Five-year Follow-up of a randomized controlled trial. Ann Surg. 2007; 246: 976 -981. Bergenfelz A et al. Conventional bilateral cervical exploration vs. open minimally invasive parathyroidectomy under local anaesthesia for primary hyperparathyroidism. Br. J Surg. 2005; 92: 190 -197 Russell CF et al. Randomized clinical trial comparing scan-directed unilateral vs. bilateral cervical exploration for primary hyperparathyroidism due to solitary adenoma. Br. J Surg. 2006; 93: 418 -421
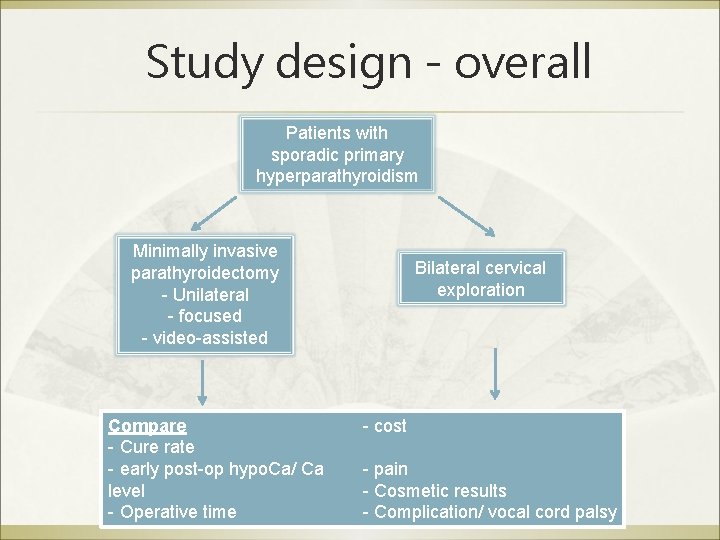
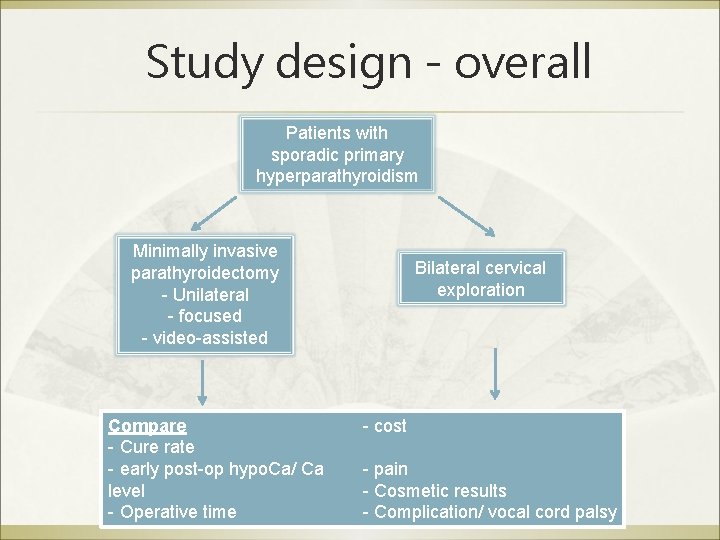
Study design - overall Patients with sporadic primary hyperparathyroidism Minimally invasive parathyroidectomy - Unilateral - focused - video-assisted Compare - Cure rate - early post-op hypo. Ca/ Ca level - Operative time Bilateral cervical exploration - cost - pain - Cosmetic results - Complication/ vocal cord palsy
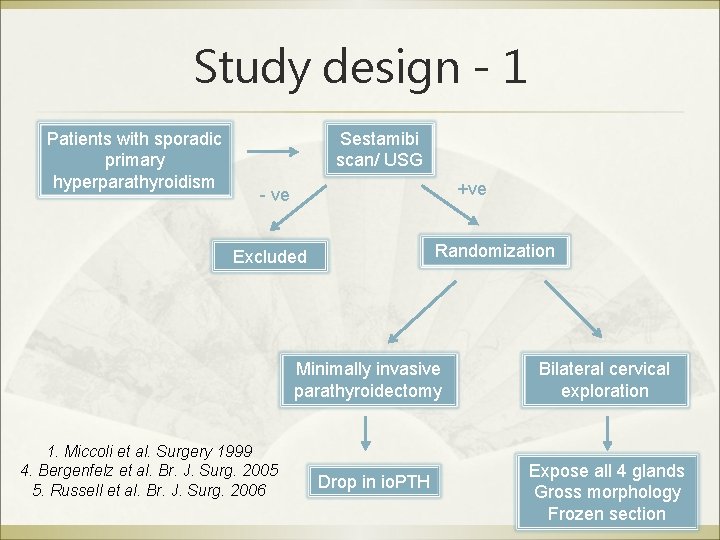
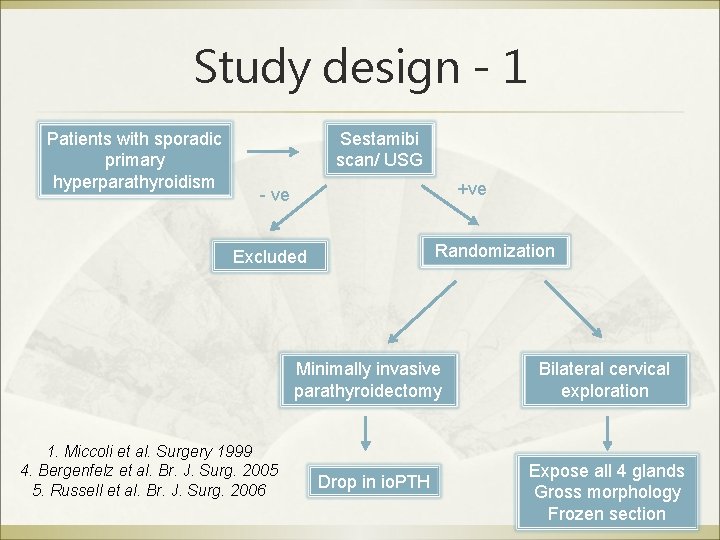
Study design - 1 Patients with sporadic primary hyperparathyroidism Sestamibi scan/ USG +ve - ve Randomization Excluded Minimally invasive parathyroidectomy 1. Miccoli et al. Surgery 1999 4. Bergenfelz et al. Br. J. Surg. 2005 5. Russell et al. Br. J. Surg. 2006 Drop in io. PTH Bilateral cervical exploration Expose all 4 glands Gross morphology Frozen section

Study design - 2 Patients with sporadic primary hyperparathyroidism Randomization Minimally invasive parathyroidectomy +ve Sestamibi scan - ve Bilateral cervical exploration Explore +ve side Explore left side first 2. Bergenfelz et al. Ann. Surg. 2002 3. Westerdahl et al. Ann. Surg. 2007 If no enlarged gland on first explored side Stop if one enlarged gland found + drop in io. PTH
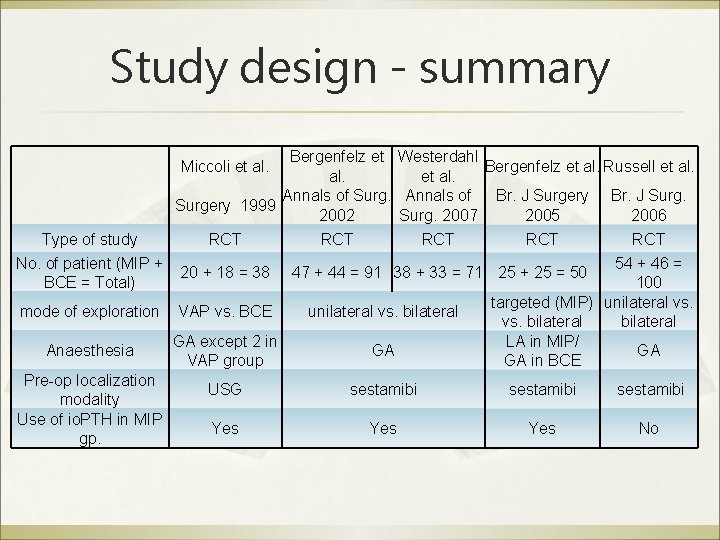
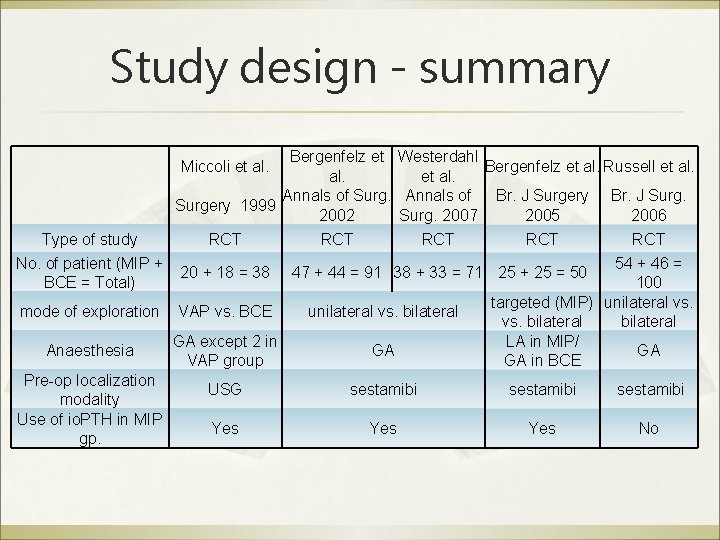
Study design - summary Bergenfelz et Westerdahl Bergenfelz et al. Russell et al. Annals of Surg. Annals of Br. J Surgery 1999 2002 Surg. 2007 2005 2006 Miccoli et al. Type of study RCT No. of patient (MIP + BCE = Total) 20 + 18 = 38 mode of exploration VAP vs. BCE unilateral vs. bilateral Anaesthesia GA except 2 in VAP group GA USG sestamibi Yes Yes No Pre-op localization modality Use of io. PTH in MIP gp. RCT RCT 54 + 46 = 100 targeted (MIP) unilateral vs. bilateral LA in MIP/ GA GA in BCE 47 + 44 = 91 38 + 33 = 71 25 + 25 = 50
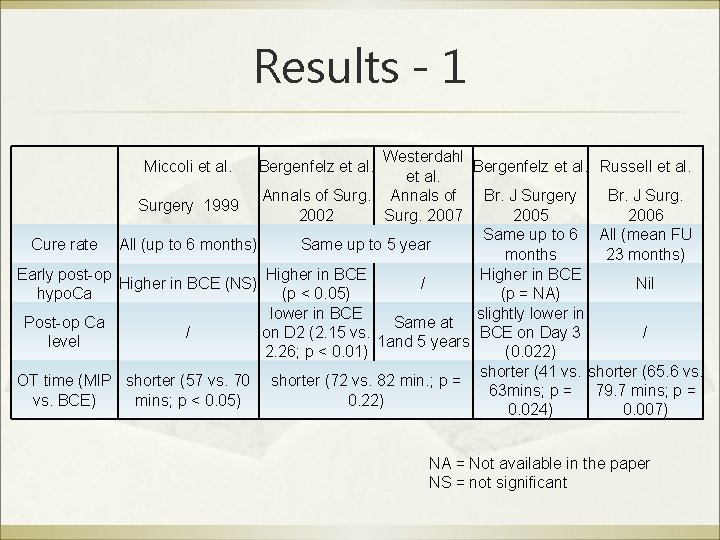
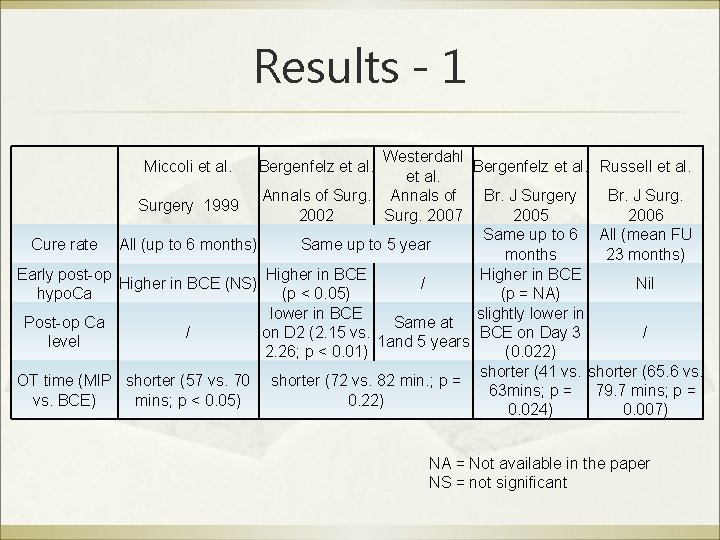
Results - 1 Westerdahl Bergenfelz et al. Russell et al. Annals of Surg. Annals of Br. J Surgery 1999 2002 Surg. 2007 2005 2006 Same up to 6 All (mean FU Cure rate All (up to 6 months) Same up to 5 year months 23 months) Early post-op Higher in BCE (NS) / Nil hypo. Ca (p < 0. 05) (p = NA) lower in BCE slightly lower in Post-op Ca Same at on D 2 (2. 15 vs. BCE on Day 3 / / level 1 and 5 years 2. 26; p < 0. 01) (0. 022) shorter (41 vs. shorter (65. 6 vs. OT time (MIP shorter (57 vs. 70 shorter (72 vs. 82 min. ; p = 63 mins; p = 79. 7 mins; p = vs. BCE) mins; p < 0. 05) 0. 22) 0. 024) 0. 007) Miccoli et al. Bergenfelz et al. NA = Not available in the paper NS = not significant
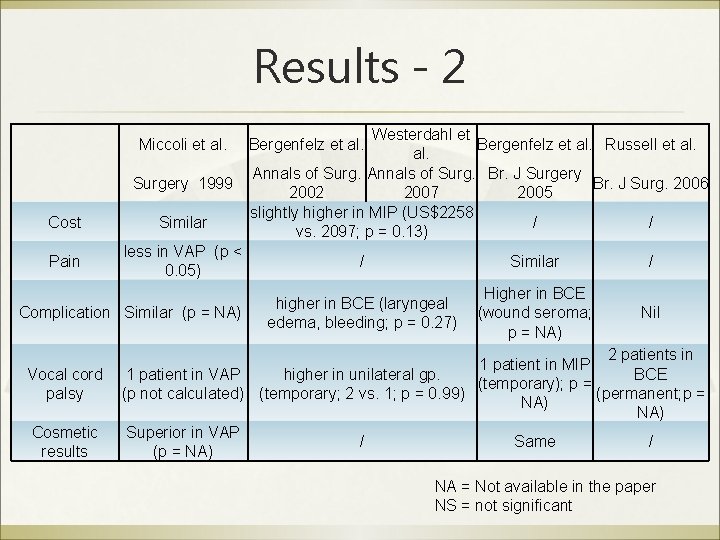
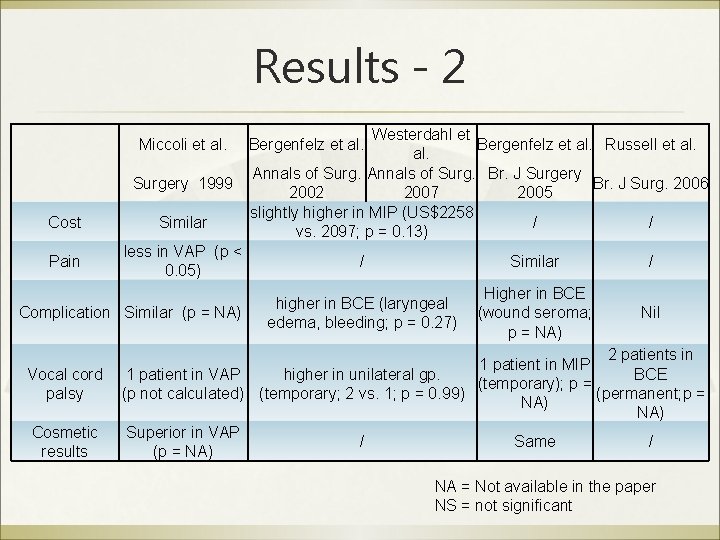
Results - 2 Miccoli et al. Surgery 1999 Cost Similar Pain less in VAP (p < 0. 05) Complication Similar (p = NA) Vocal cord palsy Cosmetic results Westerdahl et Bergenfelz et al. Russell et al. Annals of Surg. Br. J Surgery Br. J Surg. 2006 2002 2007 2005 slightly higher in MIP (US$2258 / / vs. 2097; p = 0. 13) Bergenfelz et al. / Similar / higher in BCE (laryngeal edema, bleeding; p = 0. 27) Higher in BCE (wound seroma; p = NA) Nil 2 patients in 1 patient in MIP BCE 1 patient in VAP higher in unilateral gp. (temporary); p = (p not calculated) (temporary; 2 vs. 1; p = 0. 99) (permanent; p = NA) Superior in VAP / Same / (p = NA) NA = Not available in the paper NS = not significant
Conclusion ß ß MIP is as effective as conventional bilateral neck exploration for primary hyperparathyroidism Advantage Þ Þ Þ Less early post-operative hypo. Ca Can be done under LA Shorter operative time

Thank you Questions?
 Minimally invasive surgery
Minimally invasive surgery Hyperparathyroidism symptoms
Hyperparathyroidism symptoms Minimally conscious state
Minimally conscious state Causes of secondary hyperparathyroidism
Causes of secondary hyperparathyroidism Hypercalciemia
Hypercalciemia Phosrenal
Phosrenal 3ry hyperparathyroidism
3ry hyperparathyroidism Tertiary hyperparathyroidism
Tertiary hyperparathyroidism Exotic species definition
Exotic species definition Invasive ductal carcinoma with medullary features
Invasive ductal carcinoma with medullary features Invasive species characteristics
Invasive species characteristics Invasive species characteristics
Invasive species characteristics Invasive species characteristics
Invasive species characteristics Indiana invasive species council
Indiana invasive species council Invasive species laws
Invasive species laws Aspergilloma treatment duration
Aspergilloma treatment duration Non invasive halo brace
Non invasive halo brace Invasive species compendium
Invasive species compendium Sesleria autumnalis invasive
Sesleria autumnalis invasive Non invasive ventilation
Non invasive ventilation Non invasive ventilation
Non invasive ventilation Valid safeguards in antt
Valid safeguards in antt Invasive mushroom species
Invasive mushroom species Invasive species investigator worksheet
Invasive species investigator worksheet Invasive candidiasis
Invasive candidiasis