Disease of Parathyroid Dr Faiza A Qari Function
















- Slides: 40
Disease of Parathyroid Dr Faiza. A. Qari
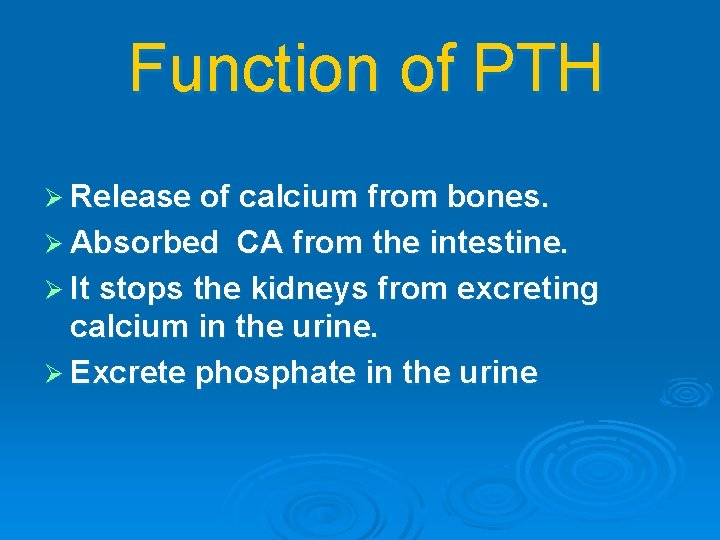
Function of PTH Ø Release of calcium from bones. Ø Absorbed CA from the intestine. Ø It stops the kidneys from excreting calcium in the urine. Ø Excrete phosphate in the urine
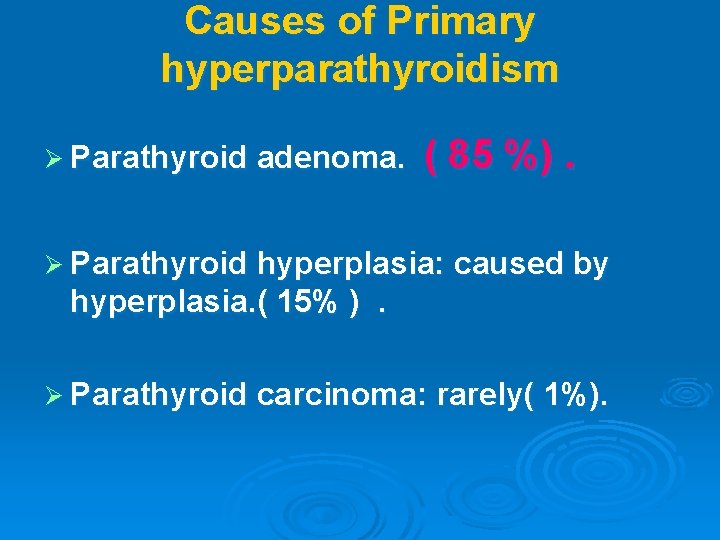
Causes of Primary hyperparathyroidism Ø Parathyroid adenoma. ( 85 %). Ø Parathyroid hyperplasia: caused by hyperplasia. ( 15% ). Ø Parathyroid carcinoma: rarely( 1%).
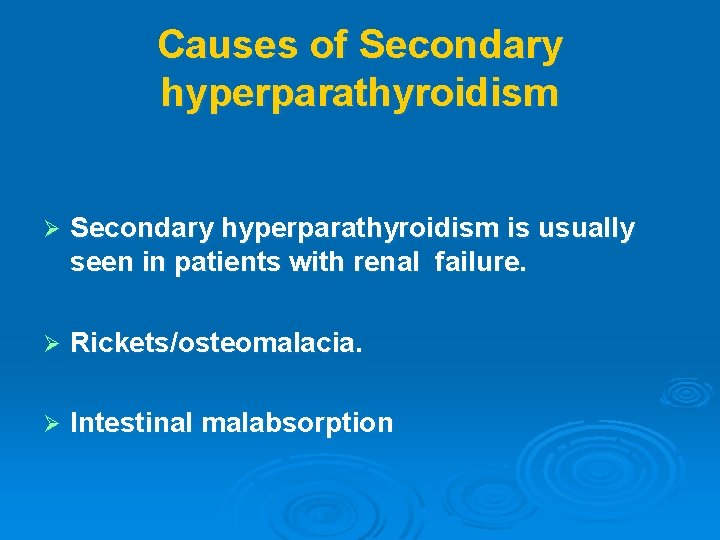
Causes of Secondary hyperparathyroidism Ø Secondary hyperparathyroidism is usually seen in patients with renal failure. Ø Rickets/osteomalacia. Ø Intestinal malabsorption
Tertiary hyperparathyroidism Ø Chronic kidney failure or in people who have had a kidney transplant.
Symptoms of hyperparathyroidism NO symptoms, or only have mild symptoms. Symptoms of hypercalcaemia Tiredness. Weak and easily tired muscles. Bone pains. Nausea (feeling sick), vomiting and feeling off your food. Constipation. Abdominal pain. Feeling very thirsty and passing urine frequently. Depression/low mood. confusion, loss of consciousness, heart rhythm disturbances and, rarely, death. Ø high blood pressure Ø Ø Ø Ø Ø

Symptoms of hyperparathyroidism Ø "Bones, stones, abdominal groans, and psychic moans ". Ø Skeletal manifestations-- ---pseudogout, and chondrocalcinosis , osteitis fibrosa cystica, causing subperiosteal resorption, and the skull causing the radiologic appearance known as salt and pepper skull. Ø Renal manifestations ---polyuria, kidney stones, hypercalciuria, and rarely nephrocalcinosis.

S/S of hyperparathyroidism GIT --- anorexia, nausea, vomiting, abdominal pain, constipation, peptic ulcer disease, and acute pancreatitis. Ø CNS and psychologic ---- proximal myopathy, weakness and easy fatigability, depression, inability to concentrate, and memory problems Ø CVS--- hypertension, bradycardia, QT interval prolongation, and left ventricular hypertrophy. Ø Signs ---- Non speciefic Ø

Complications of hyperparathyroidism Ø Kidney stones. CRF Ø Corneal calcification. Ø osteopenia. Ø Pancreatitis. Ø Peptic (stomach) ulceration
Lab Studies Ø Elevated (PTH) levels in the setting of hypercalcemia (10 -65 pg/m. L). Ø Po 4 is normal --, ALP is normal , corrected CA is high. Ø Urinary calcium excretion elevated.
Imaging Studies Ø Ultrasonography and 99 m. Tc sestamibi scanning have the advantages of being widely available and relatively inexpensive compared but is operator-dependent. Ø Radiology ---- subperiosteal resorption at the radial sides of the phalanges, distal phalangeal tufts, and distal clavicles. Ø Skull Xray ---- pepar salt apperance . Ø (DXA) at the hip and spine ---- ostoprosis.







Emergency treatment of hypercalacemia Ø Goal of treatment is to reduce the calcium level to below 11. 5 mg/d Ø IV 0. 9 % saline 6 -10 /l Ø In patients with profound hypercalcemia presenting with severe alterations of mental status, loop diuretics facilitate the urinary excretion of calcium and can prevent the volume overload
Treatment Ø Ø Ø Ø Ø Parathroidoctomy is the only definitive treatment ----. induces normocalcemia in 95 -98% of patients. indications for surgery, Patients with overt clinical manifestations of disease Age younger than 50 years Serum calcium concentration more than 1 mg/d. L above upper limit of reference range Urinary calcium excretion greater than 400 mg/d Low or declining bone mineral density Reduction in creatinine clearance of 30% or more Reduction of bone mineral density greater than 2. 5 standard deviations below the reference range for bone density in terms of age, gender, and race (T score <2. 5)

Follow up Ø A decline in serum calcium level occurs within 24 hours of successful surgery. Additionally, serum PTH levels fall within minutes of a successful parathyroidectomy. Ø Blood calcium levels fall to low reference range values for 3 -5 days until the remaining parathyroid tissue resumes hormone secretion. Ø Severe postoperative hypocalcemia is likely only if osteitis fibrosa cystica is present or if injury to all the normal parathyroid glands occurs during surgery.
Hypoparathyroidism Biochemical hallmarks of PTH insufficiency are hypocalcemia and hyperphosphatemia
S/S of Hypocalcemia Ø Asymptomatic. Ø Neurologic: paresthesias, muscle cramping, tetany, or seizures. Ø Cardiac: prolongation of the QTc interval. arrhythmias, ventricular tachycardia. Ø Respiratory: Laryngospasm, stridor and significant airway obstruction.
Signs of hypocalcemia. l l Trousseau sign. Chvostek sign



Causes of Hypoparathyroidism Ø Acquired hypoparathyroidism ----after neck irradiation or surgery. Ø Inherited
Lab Studies Ø Total and ionized calcium are low. , serum po 4 is high Ø Intact PTH is low. Ø (BUN) and creatinine Ø Urine calcium and creatinine ratio: Urine calcium is elevated in PTH-resistant and PTH-deficient states and particularly elevated in calcium-sensing receptor mutations.
Treatment Ø Hypocalcemia that produces symptoms, such as seizure, tetany, and laryngospasm, requires intravenous calcium and continuous monitoring for cardiac arrhythmias. Ø Oral calcium and vitamin D are initiated as soon as possible (eg, when the patient is tolerating oral feeds). Ø The active form of vitamin D, 1, 25 -dihydroxyvitamin D, is preferred in the treatment of hypoparathyroidism

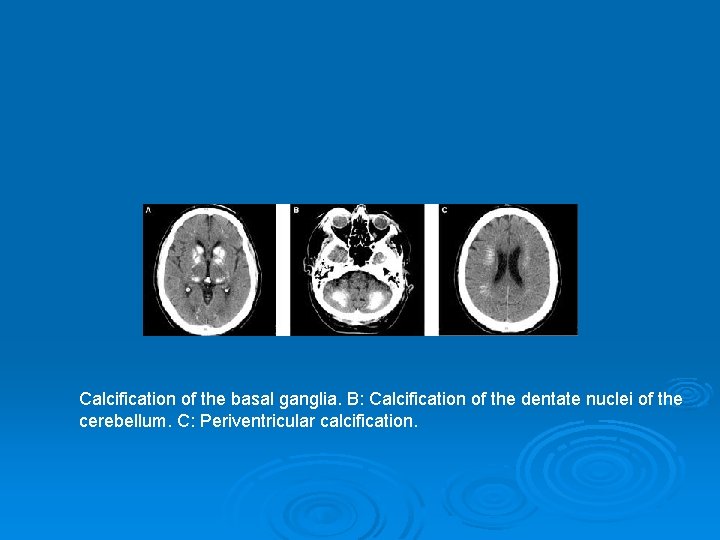
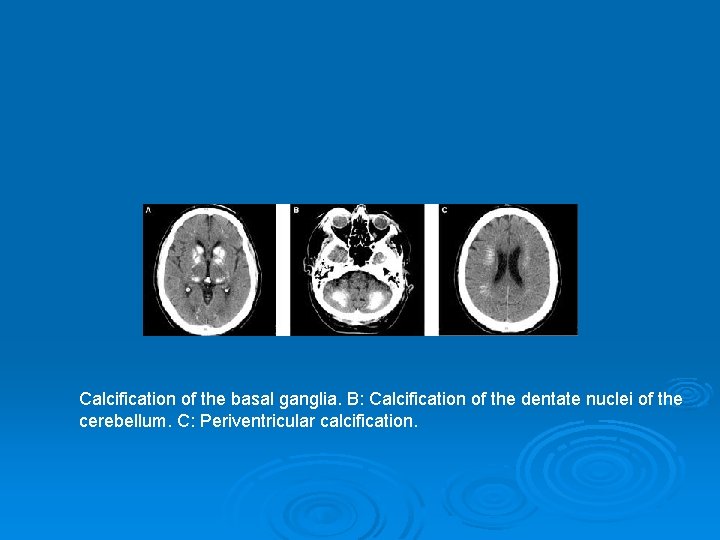
Calcification of the basal ganglia. B: Calcification of the dentate nuclei of the cerebellum. C: Periventricular calcification.
