Scenario A 50 year old female has had





- Slides: 59

Scenario A 50 year old female has had three vertebral fractures. She has also had a number of kidney stones. Routine labs revealed hypercalcemia.
Effects of Parathyroid Hormone on Bone Mineral Metabolism
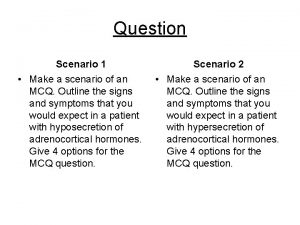
Lecture Objectives At the end of the lecture students will be able to • Define the importance of calcium in bone mineral metabolism • Explain the action of Parathyroid Hormone on gut, bone and kidney. • Describe the role of 1, 25 -dihydroxy vitamin D and calcitonin in calcium homeostasis • List the symptoms of hyper and hypoparathyroidism
Physiological Importance of Calcium • Ca salts in bone provide structural integrity of the skeleton. • Ca ions in extracellular and intracellular fluids is essential for biochemical processes like: – Neuoromuscular excitability and signal transduction – Blood coagulation – Hormonal secretion – Enzymatic regulation – Neuron excitation

Three Forms of Circulating Ca 2+
Regulation of Calcium • The important role that calcium plays in so many processes dictates that its concentration, both extracellularly and intracellularly, be maintained within a very narrow range. • This is achieved by an elaborate system of controls
Calcium and phosphorous • Calcium is tightly regulated with Phosphorous in the body. • Phosphorous is an essential mineral necessary for ATP, c. AMP second messenger systems, and other roles • Ca 2+ normally ranges from 8. 5 -10 mg/dl in the plasma. • PO 4 normal plasma concentration is 3. 0 -4. 5 mg/dl.
Extracellular Calcium • When extracellular calcium falls below normal, the nervous system becomes progressively more excitable because of increase permeability of neuronal membranes to sodium. • Hyperexcitability causes tetanic contractions – Hypocalcemic tetany
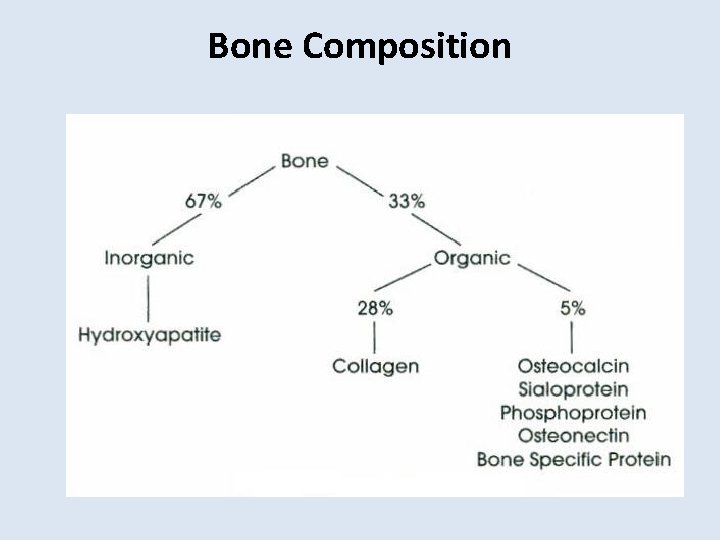
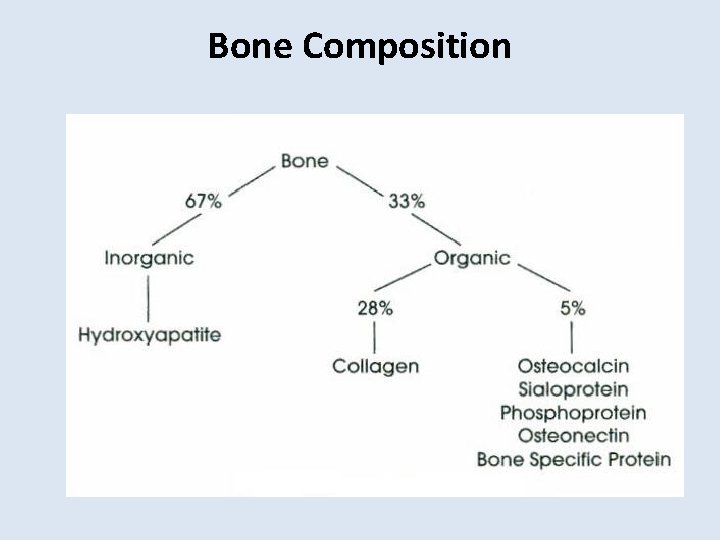
Bone Composition
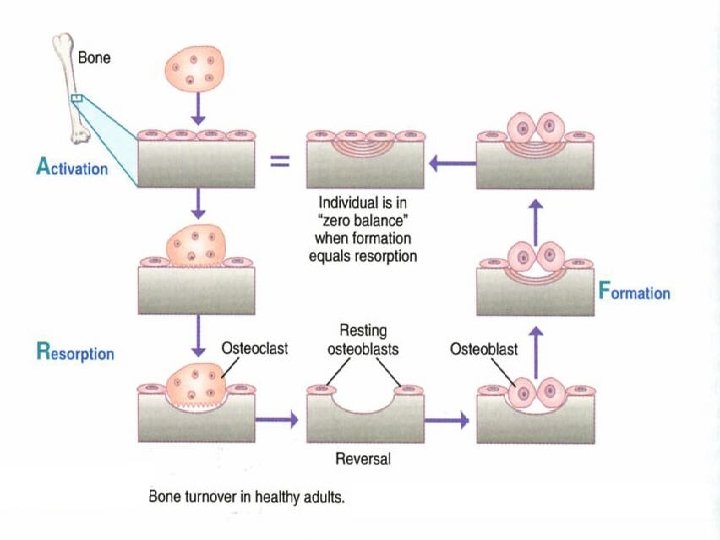
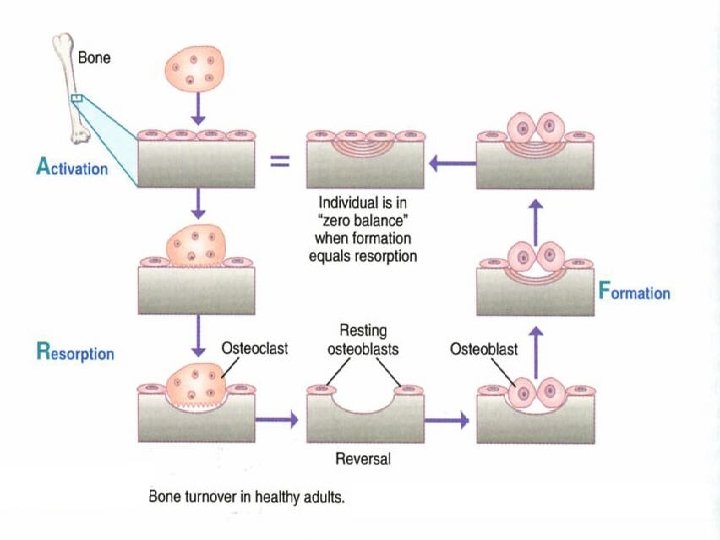
Bones • 99% of the Calcium in our bodies is found in our bones which serve as a reservoir for Ca++ storage. • 10% of total adult bone mass turns over each year during remodeling process • During growth rate of bone formation exceeds resorption and skeletal mass increases. • Once adult bone mass is achieved equal rates of formation and resorption maintain bone mass until age of about 30 years when rate of resorption begins to exceed formation and bone mass slowly decreases.
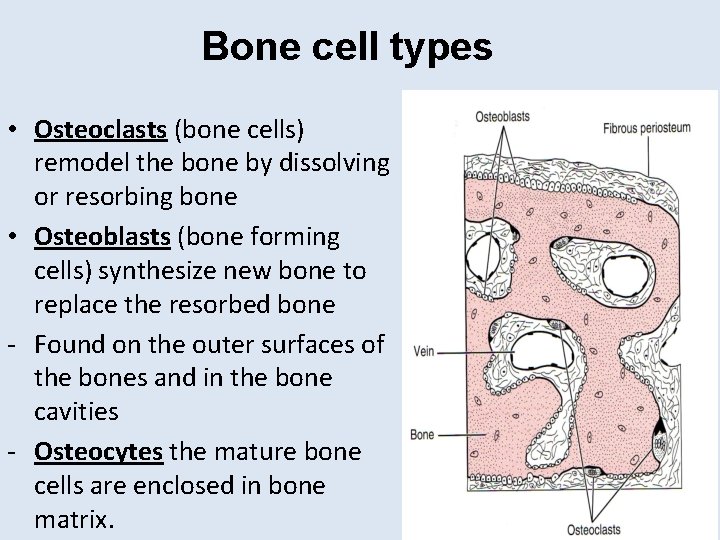
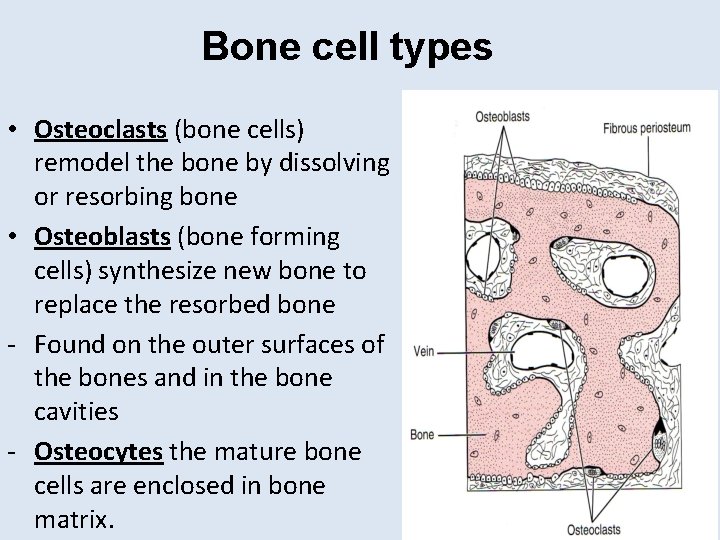
Bone cell types • Osteoclasts (bone cells) remodel the bone by dissolving or resorbing bone • Osteoblasts (bone forming cells) synthesize new bone to replace the resorbed bone - Found on the outer surfaces of the bones and in the bone cavities - Osteocytes the mature bone cells are enclosed in bone matrix.
Bone formation • Active osteoblasts synthesize and extrude collagen • Collagen fibrils form arrays of an organic matrix called the osetoid. • Calcium phosphate is deposited in the osteoid and becomes mineralized • Mineralization is combination of Ca. P 04, OH-, and H 3 CO 3– hydroxyapatite.
Osteoblast and Osteoclast Function Osteoblasts Osteoclasts • Bone formation • Synthesis of matrix protein • Mineralization • Bone resorption – Degradation of proteins by enzymes – Acidification
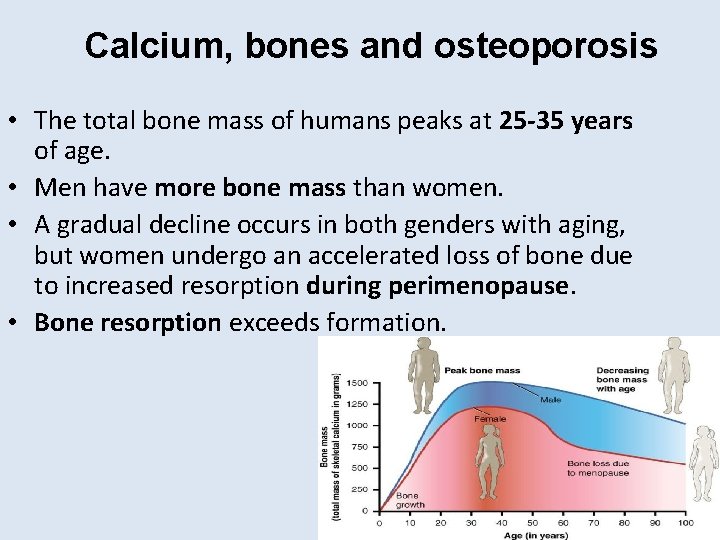
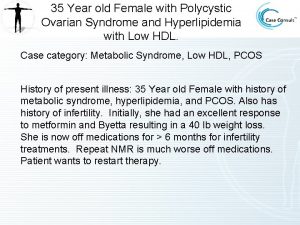
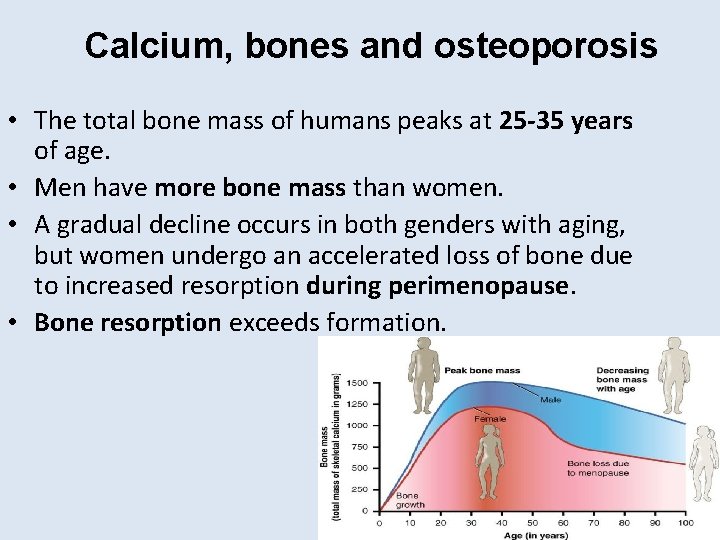
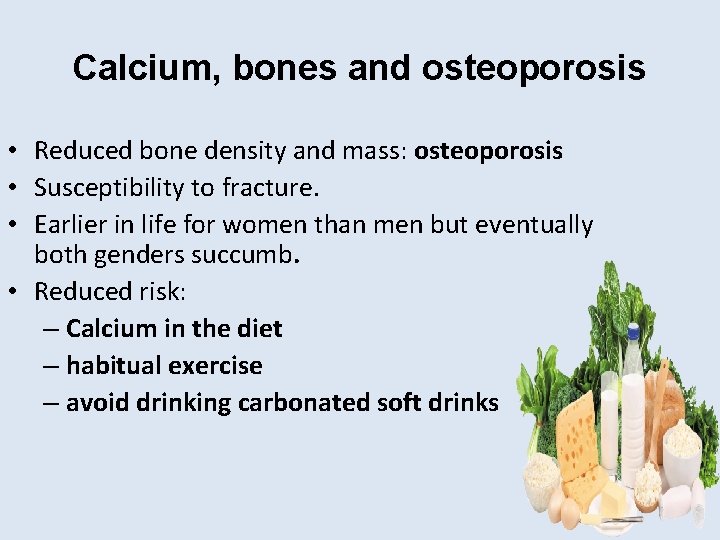
Calcium, bones and osteoporosis • The total bone mass of humans peaks at 25 -35 years of age. • Men have more bone mass than women. • A gradual decline occurs in both genders with aging, but women undergo an accelerated loss of bone due to increased resorption during perimenopause. • Bone resorption exceeds formation.
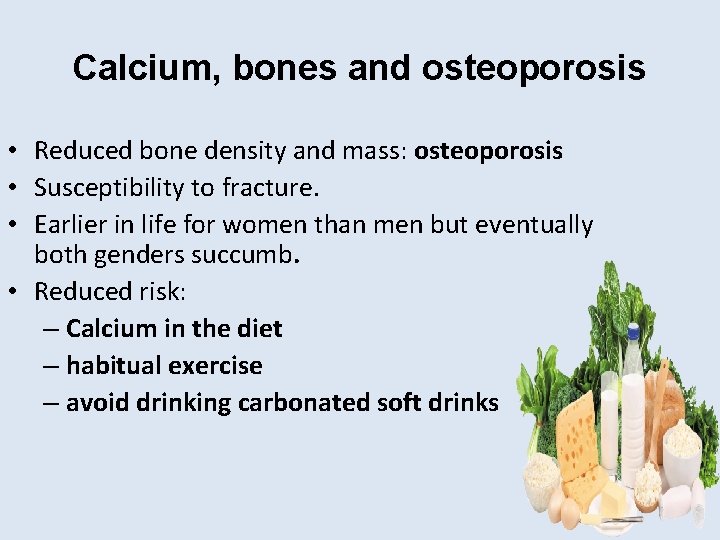
Calcium, bones and osteoporosis • Reduced bone density and mass: osteoporosis • Susceptibility to fracture. • Earlier in life for women than men but eventually both genders succumb. • Reduced risk: – Calcium in the diet – habitual exercise – avoid drinking carbonated soft drinks
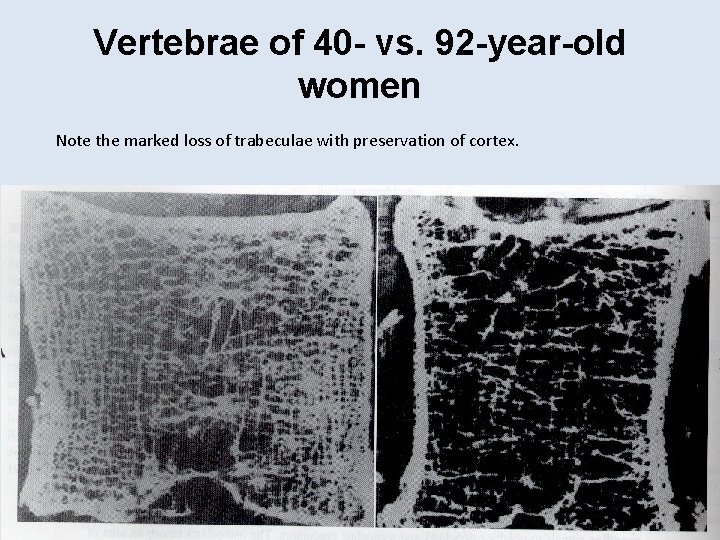
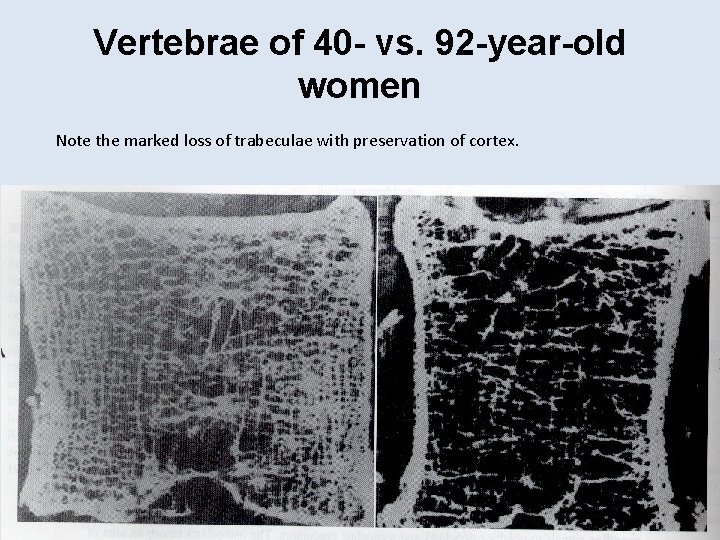
Vertebrae of 40 - vs. 92 -year-old women Note the marked loss of trabeculae with preservation of cortex.
Calcium Homeostasis 1. 2. 3. Parathyroid Hormone Calcitonin 1, 25 -dihydroxy vitamin D
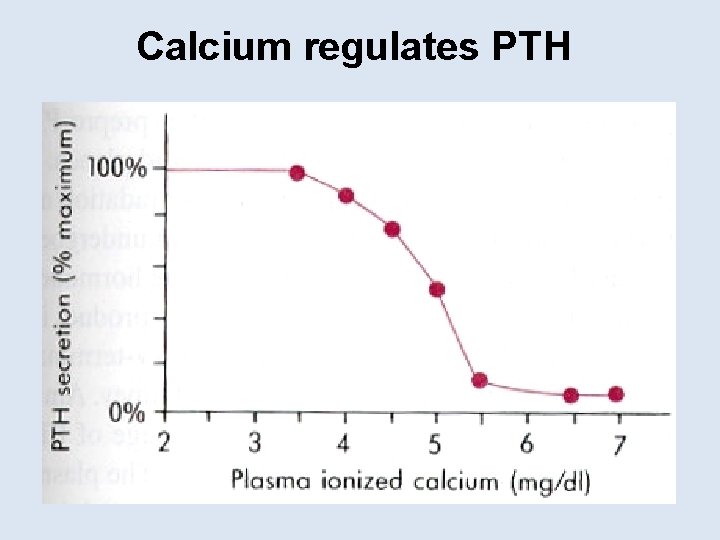
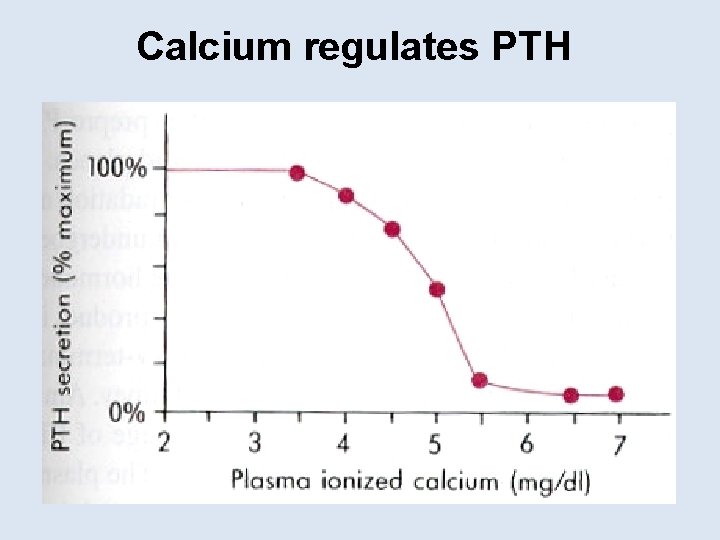
Calcium regulates PTH
Key Organs Involved • Gut • Bone • Kidneys
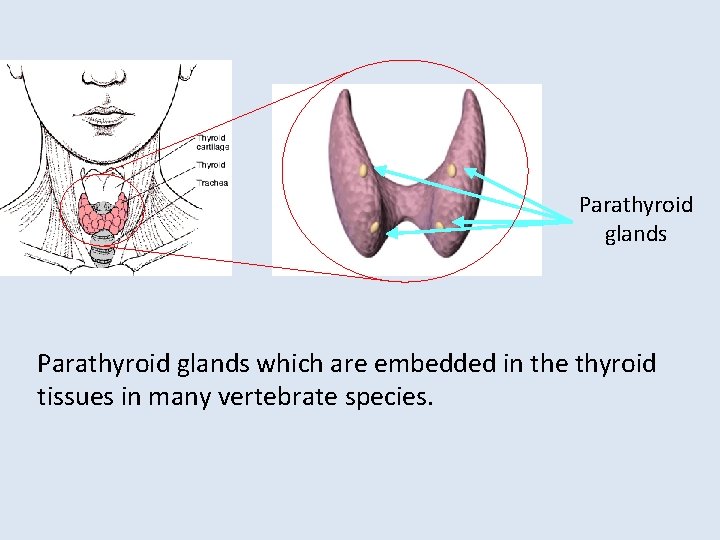
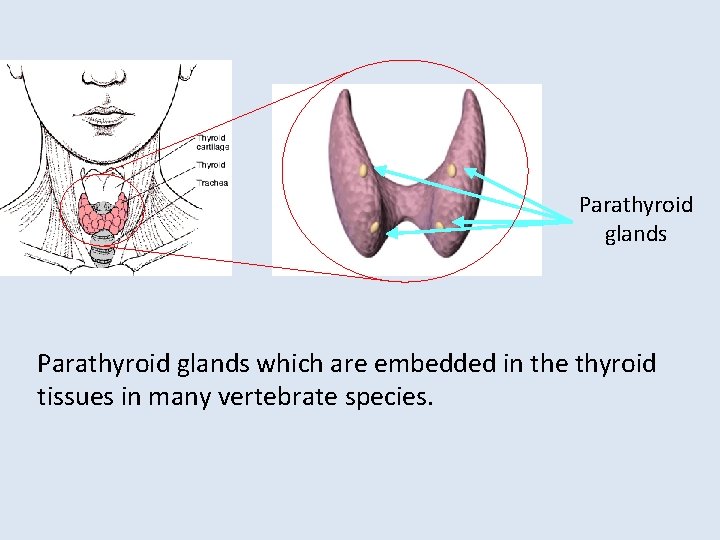
Parathyroid glands which are embedded in the thyroid tissues in many vertebrate species.
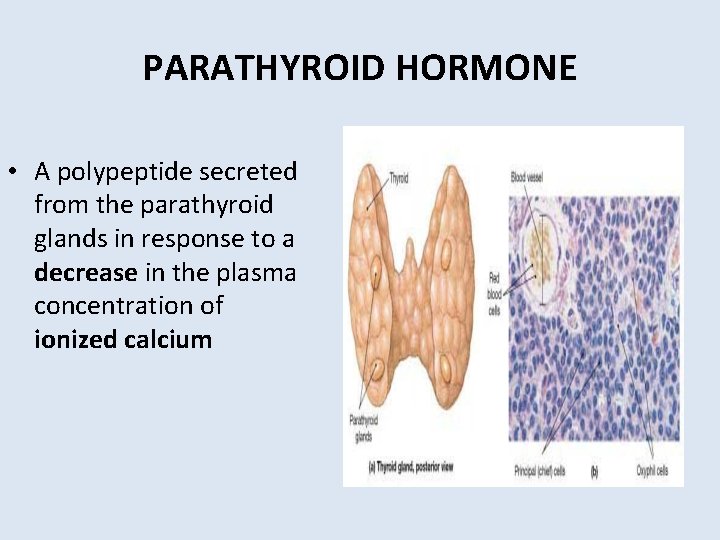
PARATHYROID HORMONE • A polypeptide secreted from the parathyroid glands in response to a decrease in the plasma concentration of ionized calcium
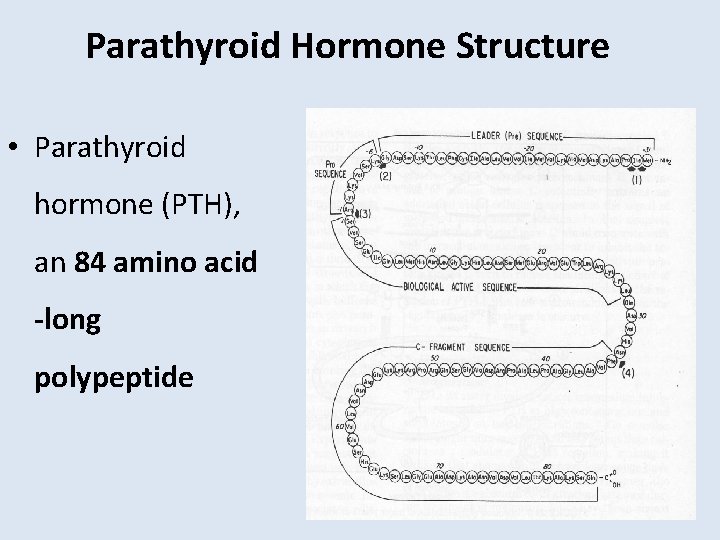
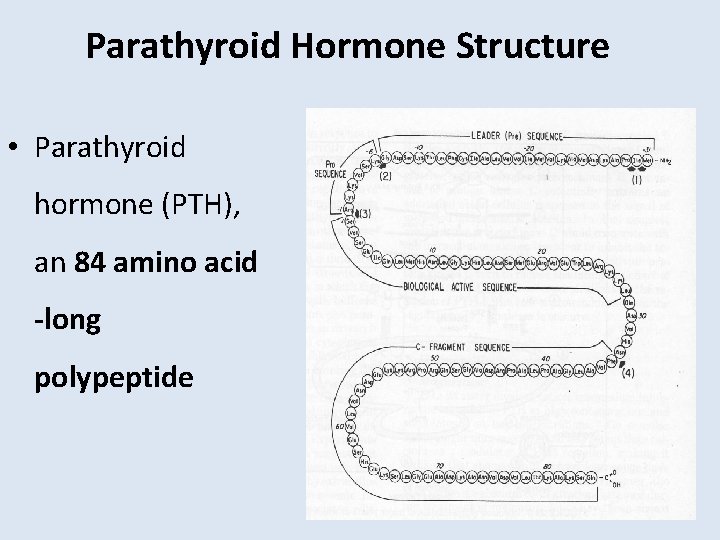
Parathyroid Hormone Structure • Parathyroid hormone (PTH), an 84 amino acid -long polypeptide
Regulation of PTH • PTH secretion responds to small alterations in plasma Ca 2+ within seconds. • An acute decrease of Ca results in marked increase of PTH m. RNA increase of PTH synthesis • PTH secretion also is stimulated by low levels of 1, 25 dihydroxy vitamin D
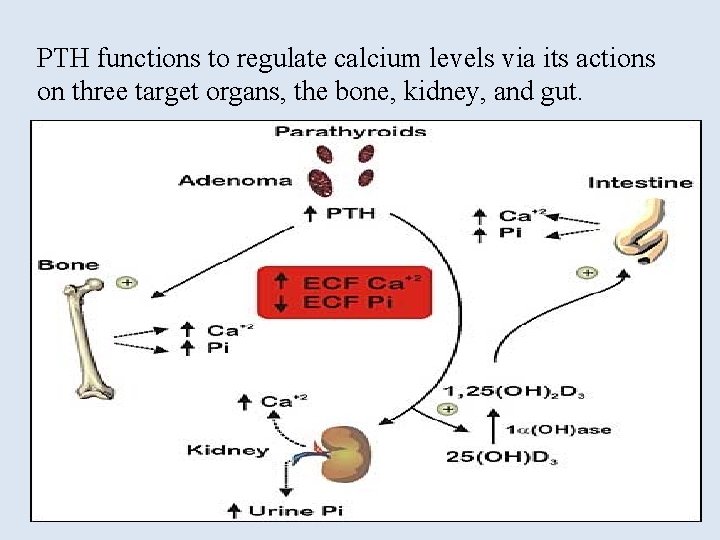
PTH increases Ca concentration by: 1: Action on the Bone Increased PTH secretion leads to an increase in bone resorption by stimulating osteoclasts and promotes the release of calcium and phosphate into the circulation
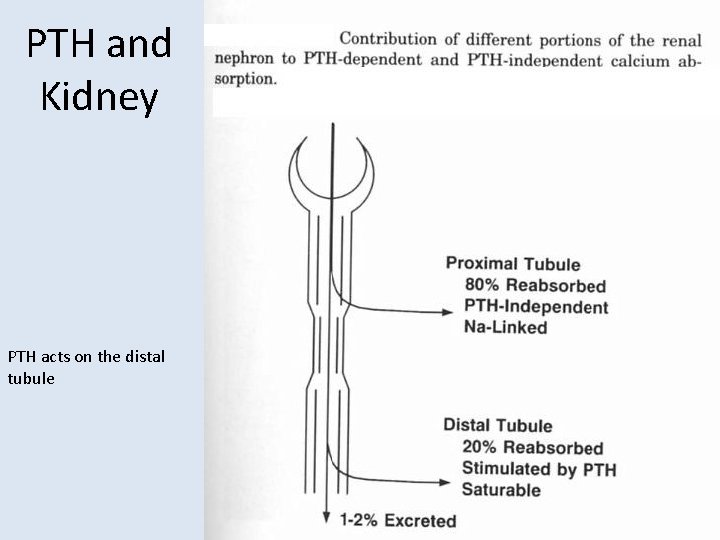
PTH increases Ca concentration by: 2: Action on the Kidney At the kidney, PTH acts to limit calcium excretion at the distal convoluted tubule via an active transport mechanism. It augments renal calcium reabsorption PTH also inhibits phosphate reabsorption (at the Proximal convoluted tubule) and bicarbonate reabsorption.
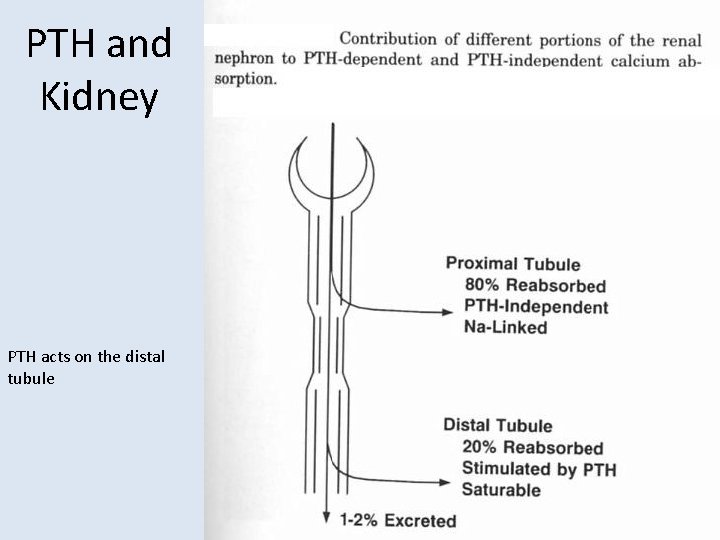
PTH and Kidney PTH acts on the distal tubule
PTH increases Ca concentration by: 3: Action on the Gut PTH also stimulates renal 1 - Hydroxylase activity, leading to an increase in 1, 25 -dihydroxy vitamin D, which Stimulates the absorption of Ca in the intestine
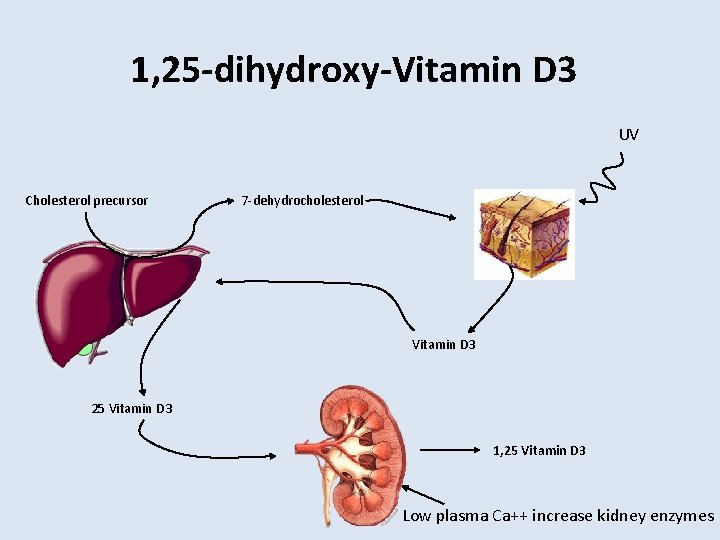
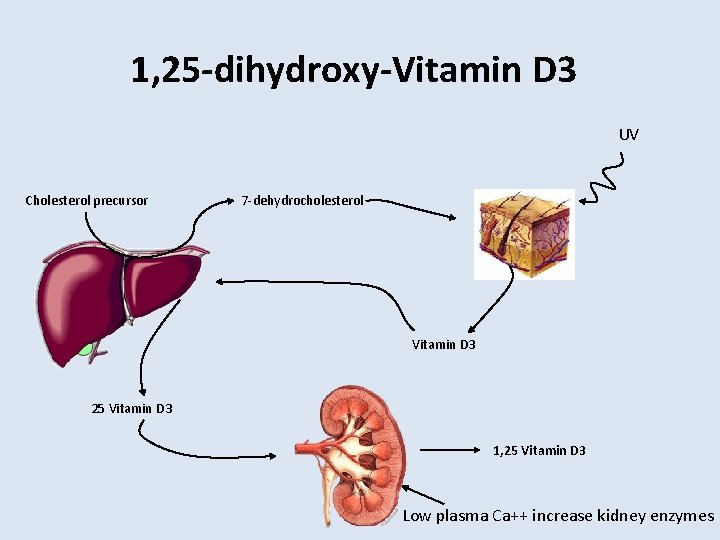
1, 25 -dihydroxy-Vitamin D 3 UV Cholesterol precursor 7 -dehydrocholesterol Vitamin D 3 25 Vitamin D 3 1, 25 Vitamin D 3 Low plasma Ca++ increase kidney enzymes
1, 25 -dihydroxy-vitamin. D 3 ( Calcitriol) Vitamin D itself is inactive, it requires modification to the active metabolite, 1, 25 -dihydroxy-D 3 is one of the principal regulator of Ca++. The first hydroxylation reaction takes place in the liver yielding 25 -hydroxy D 3. Then 25 -hydroxy D 3 is transported to the kidney where the second hydroxylation reaction takes place.
1, 25 -dihydroxy-vitamin D 3 promotes intestinal calcium absorption • 1, 25 -dihydroxy-D 3 acts via steroid hormone like receptor to increase transcriptional and translational activity • One gene product is calcium-binding protein (Ca. BP) • Ca. BP facilitates calcium uptake by intestinal cells • calbindin (calcium-binding protein) – regulated by the active form of vitamin D
1, 25 -dihydroxy-Vitamin D Actions on Bones • Another important target for 1, 25 -(OH)2 -D 3 is the bone. • Osteoblasts, but not osteoclasts have vitamin D receptors. • 1, 25 -(OH)2 -D 3 acts on osteoblasts which produce a paracrine signal that activates osteoclasts to resorb Ca++ from the bone matrix. • 1, 25 -(OH)2 -D 3 also stimulates osteocytic osteolysis.
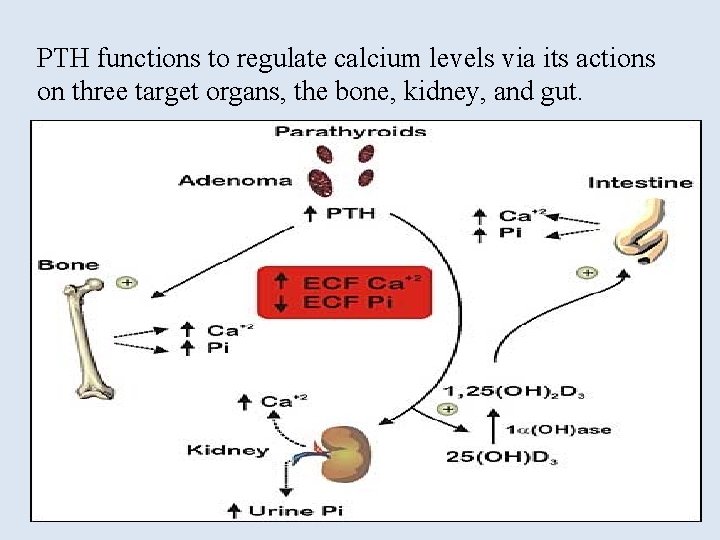
PTH functions to regulate calcium levels via its actions on three target organs, the bone, kidney, and gut.
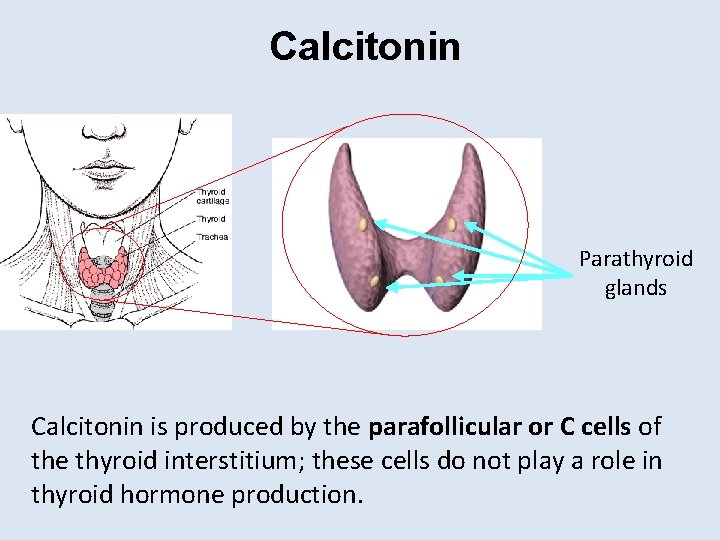
Calcitonin Parathyroid glands Calcitonin is produced by the parafollicular or C cells of the thyroid interstitium; these cells do not play a role in thyroid hormone production.
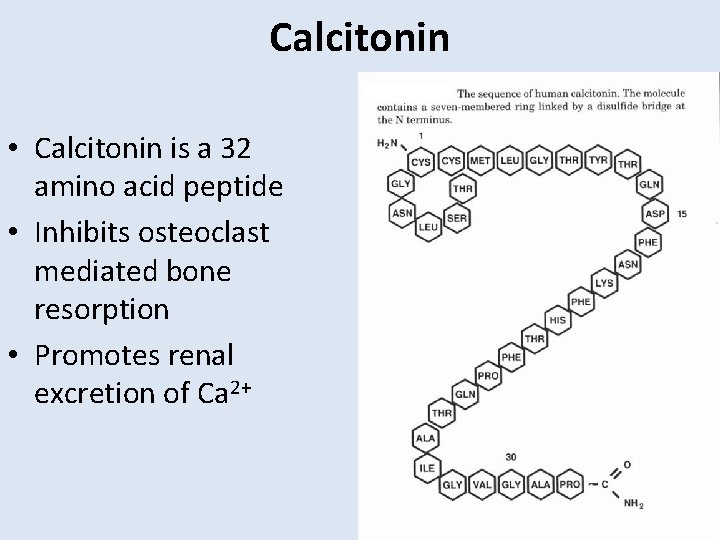
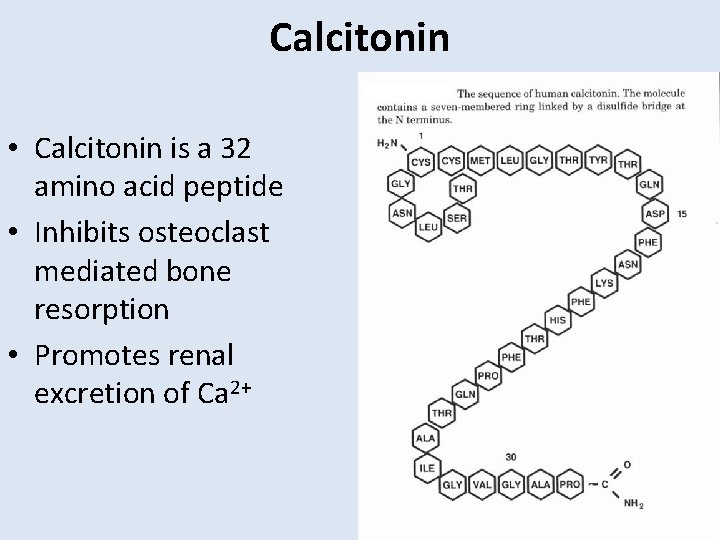
Calcitonin • Calcitonin is a 32 amino acid peptide • Inhibits osteoclast mediated bone resorption • Promotes renal excretion of Ca 2+
Calcitonin • The major stimulus of calcitonin secretion is a rise in plasma Ca 2+ levels • PTH and vitamin D act to increase plasma Ca 2+ only calcitonin causes a decrease in plasma Ca 2+. • Calcitonin is a physiological antagonist to PTH with regard to Ca 2+ homeostasis
PTH Actions • The overall action of PTH is to increase plasma Ca++ levels and decrease plasma phosphate levels. • PTH acts directly on the bones to stimulate Ca++ resorption and kidney to stimulate Ca++ reabsorption in the distal tubule of the kidney and to inhibit reabosorptioin of phosphate (thereby stimulating its excretion). • PTH also acts indirectly on intestine by stimulating 1, 25 -(OH)2 -D synthesis.
Disorders of the Parathyroid Glands
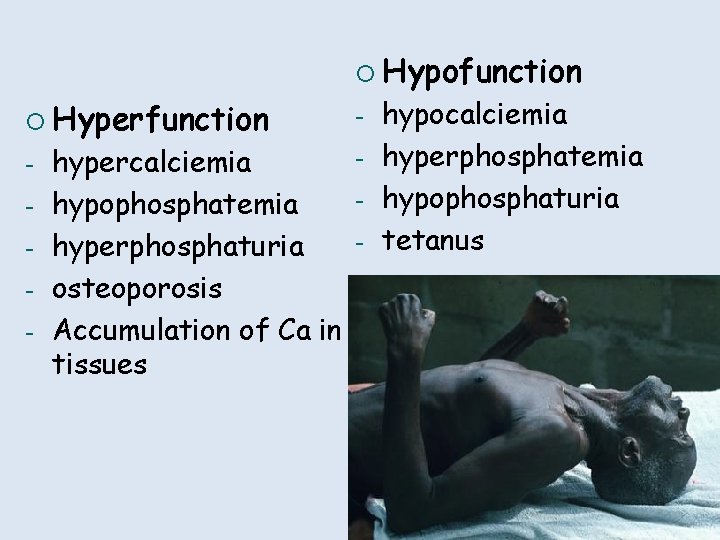
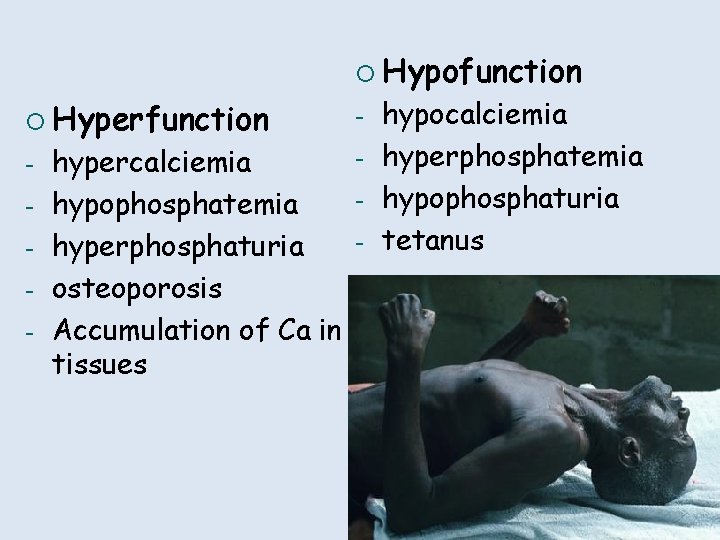
¡ Hypofunction ¡ Hyperfunction - hypercalciemia hypophosphatemia hyperphosphaturia osteoporosis Accumulation of Са in tissues - hypocalciemia hyperphosphatemia hypophosphaturia tetanus
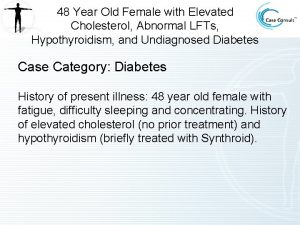
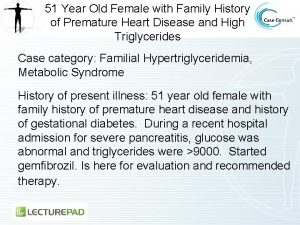
Hyperparathyroidism • Enlargement of a single gland or parathyroid adenoma in approximately 80% of cases, multiple adenomas or hyperplasia in 15 to 20% of patients and parathyroid carcinoma in 1% of patients
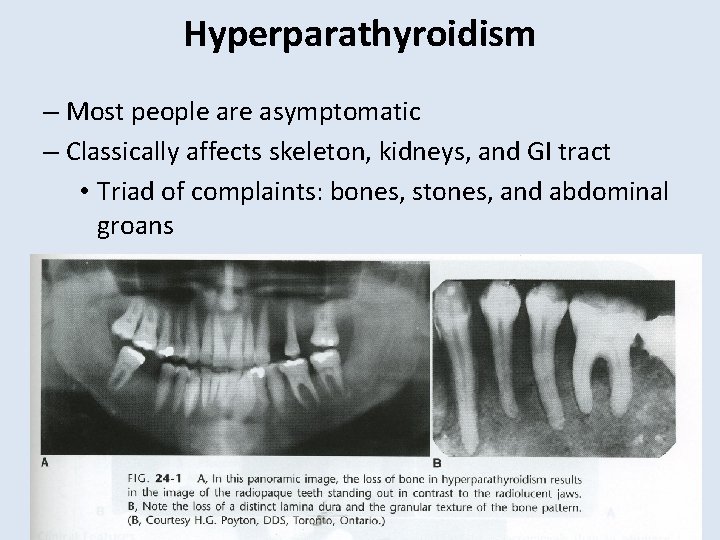
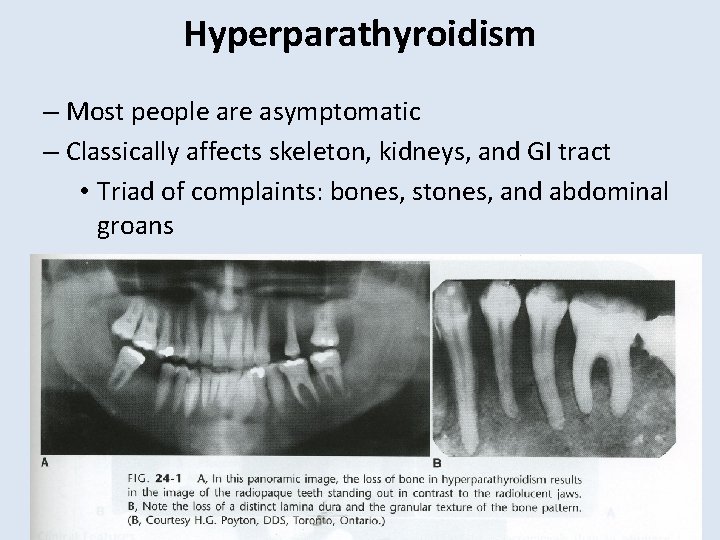
Hyperparathyroidism – Most people are asymptomatic – Classically affects skeleton, kidneys, and GI tract • Triad of complaints: bones, stones, and abdominal groans – Renal stones are most common single presenting complaint – Usually due to an adenoma (tumor)
Hyperparathyroidism • The disorder is characterized by hypercalcemia, hypercalcuria, hypophosphatemia, and hyperphosphaturia • Most common complication are renal stones made of calcium phosphate • Most serious complication is the deposition of calcium in the kidney tubules resulting in impaired renal function
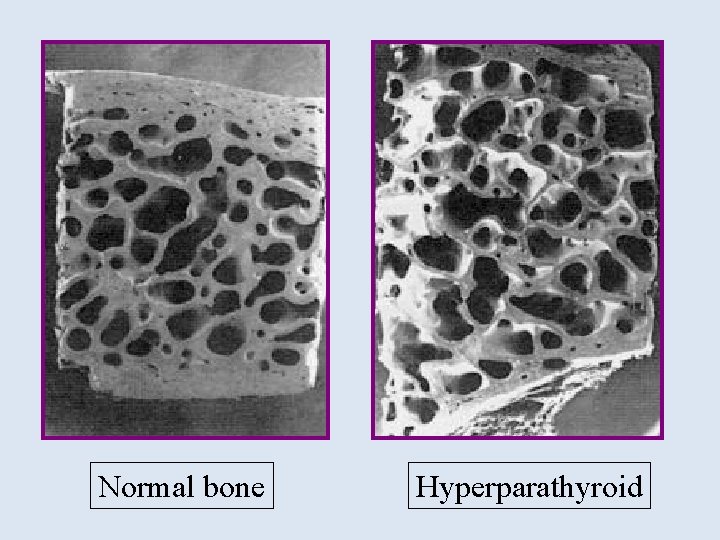
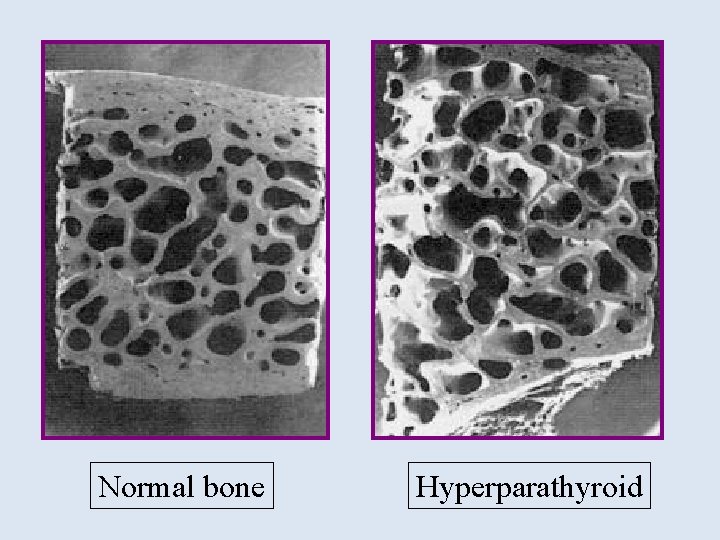
Normal bone Hyperparathyroid

Primary Hyperparathyroidism • Calcium homeostatic loss due to excessive PTH secretion • Due to excess PTH secreted from adenomatous or hyperplastic parathyroid tissue • Hypercalcemia results from combined effects of PTHinduced bone resorption, intestinal calcium absorption and renal tubular reabsorption • Surgery is the most common treatment for primary hyperparathyroidism.
Secondary Hyperparathyroidism Secondary hyperparathyroidism occurs as a result of another disease that initially causes low levels of calcium in the body and over time, increased parathyroid hormone levels occur. This is due to chronic stimulation of the parathyroid glands by a chronic decrease in the ionic calcium level in the blood
Secondary Hyperparathyroidism • In pts with chronic renal failure • Deficiency of 1, 25 -dihydroxy vitamin D as a result of loss of renal tissue, low calcium intake, decreased calcium absorption, and abnormal parathyroid cell response • Normally treated medically
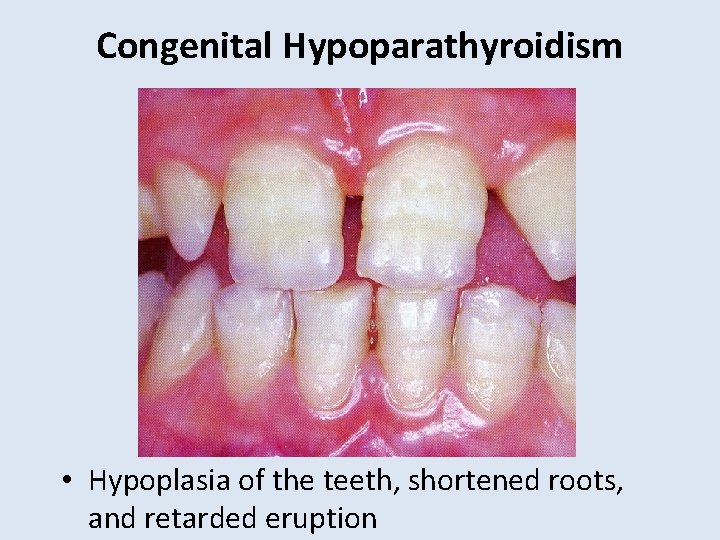
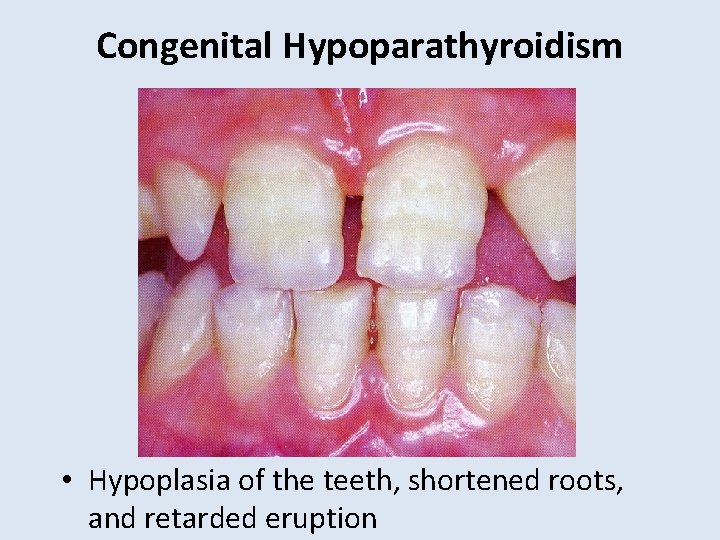
Congenital Hypoparathyroidism • Hypoplasia of the teeth, shortened roots, and retarded eruption
Hypoparathyroidism • Deficient secretion of PTH which manifests itself biochemically by hypocalcemia, hyperphospatemia diminished or absent circulating PTH and , often causing cramping and twitching of muscles or tetany. • The condition can be inherited, but it is also encountered after thyroid or parathyroid gland surgery, and it can be caused by immune system-related damage
Pseudohypoparathysoidism A rare familial disorders with target tissue resistance to PTH. There is hypocalcaemia, hyperphosphataemia, with increased parathyroid gland function. There is also a variety of congenital defects in the growth and development of skeleton including: • Short statue • Short metacarpal and metatarsal bones

Pseudohypoparathyroidism Elfin facies, short stature, enamel hypoplasia

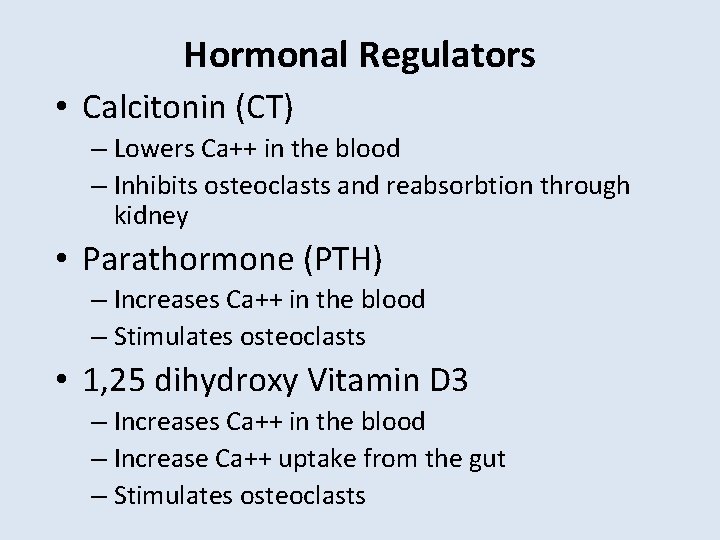
Hormonal Regulators • Calcitonin (CT) – Lowers Ca++ in the blood – Inhibits osteoclasts and reabsorbtion through kidney • Parathormone (PTH) – Increases Ca++ in the blood – Stimulates osteoclasts • 1, 25 dihydroxy Vitamin D 3 – Increases Ca++ in the blood – Increase Ca++ uptake from the gut – Stimulates osteoclasts
PRACTICE QUESTIONS
Q 1. Secretion of which hormone is stimulated by hypercalciemia and it acts to lower the serum levels of calcium: a) b) c) d) 1, 25 -dihydroxy vitamin D Calcitonin Parathyroid hormone Thyroid hormone Correct Answer: B • Explanation • 1, 25 -dihydroxy vitamin D: It stimulates the absorption of Calcium in the intestine. • Calcitonin: It acts to decrease plasma Calcium levels. • Parathyroid hormone: It increases Calcium concentration by the action on gut, bone and kidney. • Thyroid hormone: Primarily responsible for regulation of body metabolism
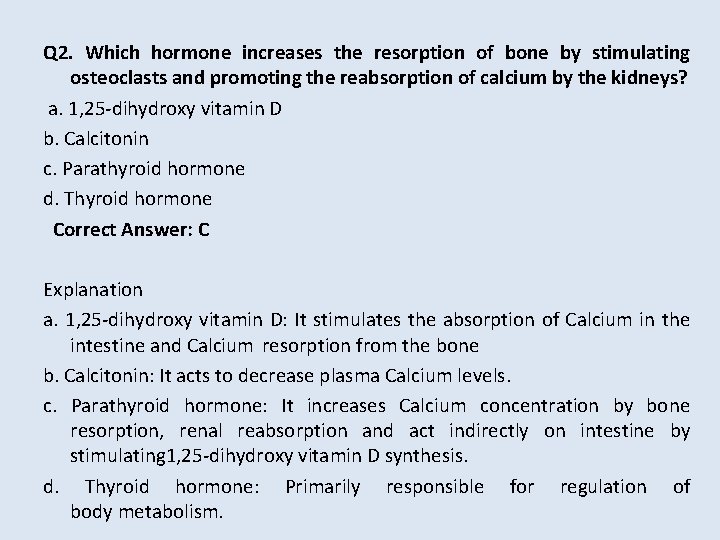
Q 2. Which hormone increases the resorption of bone by stimulating osteoclasts and promoting the reabsorption of calcium by the kidneys? a. 1, 25 -dihydroxy vitamin D b. Calcitonin c. Parathyroid hormone d. Thyroid hormone Correct Answer: C Explanation a. 1, 25 -dihydroxy vitamin D: It stimulates the absorption of Calcium in the intestine and Calcium resorption from the bone b. Calcitonin: It acts to decrease plasma Calcium levels. c. Parathyroid hormone: It increases Calcium concentration by bone resorption, renal reabsorption and act indirectly on intestine by stimulating 1, 25 -dihydroxy vitamin D synthesis. d. Thyroid hormone: Primarily responsible for regulation of body metabolism.
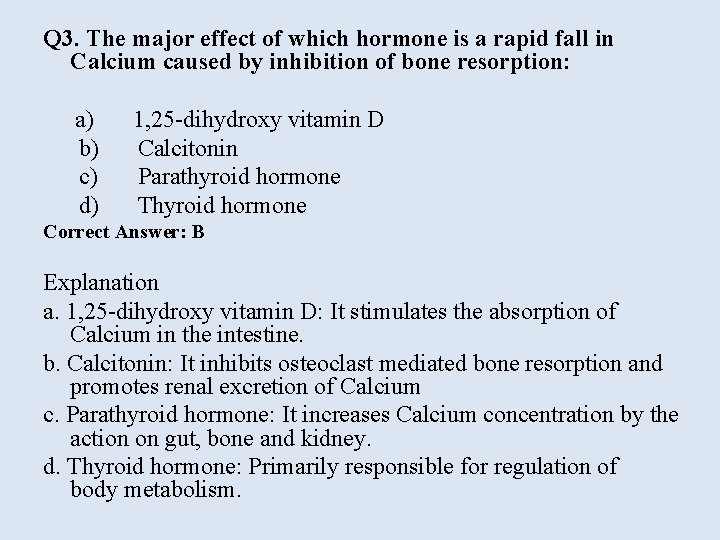
Q 3. The major effect of which hormone is a rapid fall in Calcium caused by inhibition of bone resorption: a) 1, 25 -dihydroxy vitamin D b) Calcitonin c) Parathyroid hormone d) Thyroid hormone Correct Answer: B Explanation a. 1, 25 -dihydroxy vitamin D: It stimulates the absorption of Calcium in the intestine. b. Calcitonin: It inhibits osteoclast mediated bone resorption and promotes renal excretion of Calcium c. Parathyroid hormone: It increases Calcium concentration by the action on gut, bone and kidney. d. Thyroid hormone: Primarily responsible for regulation of body metabolism.
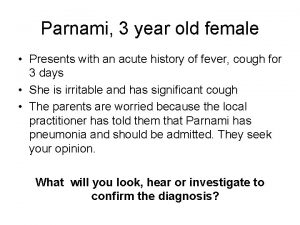
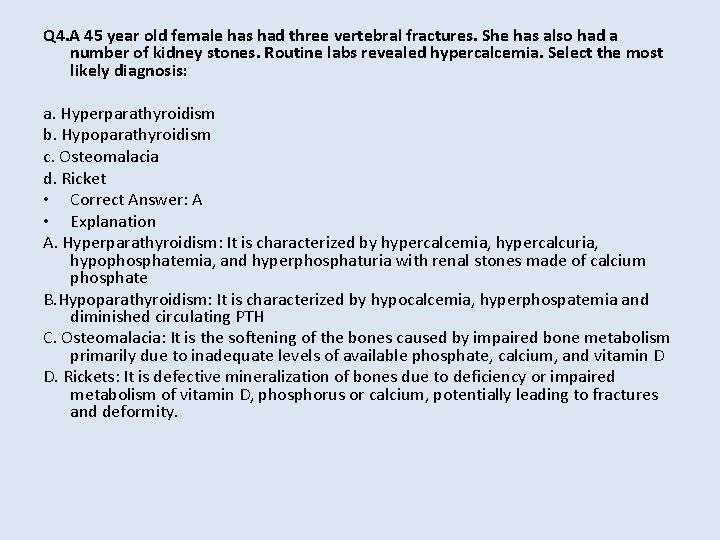
Q 4. A 45 year old female has had three vertebral fractures. She has also had a number of kidney stones. Routine labs revealed hypercalcemia. Select the most likely diagnosis: a. Hyperparathyroidism b. Hypoparathyroidism c. Osteomalacia d. Ricket • Correct Answer: A • Explanation A. Hyperparathyroidism: It is characterized by hypercalcemia, hypercalcuria, hypophosphatemia, and hyperphosphaturia with renal stones made of calcium phosphate B. Hypoparathyroidism: It is characterized by hypocalcemia, hyperphospatemia and diminished circulating PTH C. Osteomalacia: It is the softening of the bones caused by impaired bone metabolism primarily due to inadequate levels of available phosphate, calcium, and vitamin D D. Rickets: It is defective mineralization of bones due to deficiency or impaired metabolism of vitamin D, phosphorus or calcium, potentially leading to fractures and deformity.
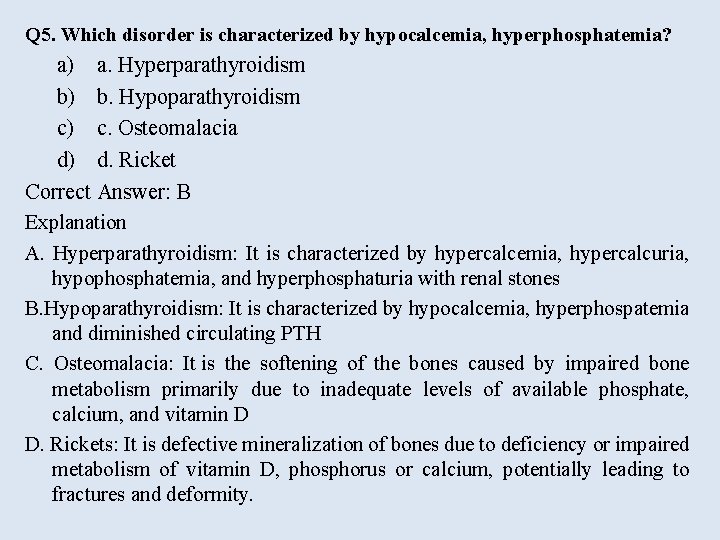
Q 5. Which disorder is characterized by hypocalcemia, hyperphosphatemia? a) a. Hyperparathyroidism b) b. Hypoparathyroidism c) c. Osteomalacia d) d. Ricket Correct Answer: B Explanation A. Hyperparathyroidism: It is characterized by hypercalcemia, hypercalcuria, hypophosphatemia, and hyperphosphaturia with renal stones B. Hypoparathyroidism: It is characterized by hypocalcemia, hyperphospatemia and diminished circulating PTH C. Osteomalacia: It is the softening of the bones caused by impaired bone metabolism primarily due to inadequate levels of available phosphate, calcium, and vitamin D D. Rickets: It is defective mineralization of bones due to deficiency or impaired metabolism of vitamin D, phosphorus or calcium, potentially leading to fractures and deformity.
 A 26 year old female presents
A 26 year old female presents I to have breakfast before i went to school
I to have breakfast before i went to school I had had breakfast before i went to school
I had had breakfast before i went to school At the beginning of the year isabel had $120 in the bank
At the beginning of the year isabel had $120 in the bank Old macdonald had a farm français
Old macdonald had a farm français Parallelism rules
Parallelism rules Old macdonald had a farm in spanish
Old macdonald had a farm in spanish Goodbye year 6 poem
Goodbye year 6 poem Pulse rate normal range
Pulse rate normal range What were daisy's assets as an eighteen year old
What were daisy's assets as an eighteen year old 42 year old woman
42 year old woman Plep examples
Plep examples Average height of a 3 year old in centimeters
Average height of a 3 year old in centimeters 9-year-old physical development
9-year-old physical development Eight year old hyphen
Eight year old hyphen Average weight for 8-year-old boy
Average weight for 8-year-old boy Weight for 11 year old
Weight for 11 year old 9-year-old physical development
9-year-old physical development Brigance test for 5 year old
Brigance test for 5 year old Brigance calculator
Brigance calculator One year old marcus turns away in disgust
One year old marcus turns away in disgust Adhd in 3 year old
Adhd in 3 year old Newborn infants typically prefer
Newborn infants typically prefer Raul and sophia were having a picnic
Raul and sophia were having a picnic Osha tree trimming safety book
Osha tree trimming safety book Net force and acceleration quick check
Net force and acceleration quick check Organelle case study answer key
Organelle case study answer key 10 year old sarah stands on a skateboard
10 year old sarah stands on a skateboard A 23 year old male experienced severe head trauma
A 23 year old male experienced severe head trauma Beautiful bonsai tree
Beautiful bonsai tree Cystisis
Cystisis 43 year old woman
43 year old woman 27-year old
27-year old Jose trips over his untied shoelace
Jose trips over his untied shoelace Squid use jet propulsion for rapid escapes
Squid use jet propulsion for rapid escapes 27-year old
27-year old Cpr for 1 year old
Cpr for 1 year old 12 year old
12 year old Fever in toddler
Fever in toddler 27-year old
27-year old A 41 year old man presents with slow irregular breathing
A 41 year old man presents with slow irregular breathing Whats your name how old are you
Whats your name how old are you Once upon a time there lived a little country girl
Once upon a time there lived a little country girl Once upon a time there lived an old man and an old woman
Once upon a time there lived an old man and an old woman Once upon a time there lived a family of bears
Once upon a time there lived a family of bears The day with nandu
The day with nandu Ben has had problems with the pipes in his apartment
Ben has had problems with the pipes in his apartment How many constitutions has georgia had
How many constitutions has georgia had How many constitutions has missouri had
How many constitutions has missouri had Have has
Have has What does cato say to katniss that makes her pause
What does cato say to katniss that makes her pause Why is it difficult to get poison in mantua?
Why is it difficult to get poison in mantua? Real life applications of piecewise functions
Real life applications of piecewise functions Anecdote sentence examples
Anecdote sentence examples User scenario
User scenario Use case scenario example
Use case scenario example Use case description level
Use case description level Penjelasan use case diagram
Penjelasan use case diagram Use case scenario
Use case scenario How to create a scenario pivot table in excel
How to create a scenario pivot table in excel