Mental Health Emergencies Stephen Warnick Jr M D
- Slides: 34
Mental Health Emergencies Stephen Warnick Jr. , M. D.
Objective Identify mental health emergencies Learn safe ways to deal with emotionally charged individuals Become comfortable with mental health petitions and escorting patients hospital Discuss your facility’s emergency plan
Patient with history of behavioral issues Start safe Place patient in room with easy entrance/exit Room in view of staff members Keep door open Have front desk flag the chart Bring it up at huddles
Anticipate Tough Encounters Controlled medication confrontations Front desk often sniffs this out first Clinician often can anticipate Front desk noticing patient acting odd MAs know a patient acts inappropriate sexually
INTERACTIVE What are ways that we can flag patients that have potential for safety issues? How do we communicate to each other about potential safety issues?
Petitions and Certs Petitions can be filled out and EMS or police have to take to hospital Police often do not like to take patient with just petition BUT THEY CAN - a person does NOT have to go to hospital. EMS will not take combative patients (okay for suicidal patient)
INTERACTIVE Break into teams of 3 -4 How would you handle a suicidal patient who was willing to go to the hospital? How would you handle a patient who needed to go to the hospital but didn’t want to go?
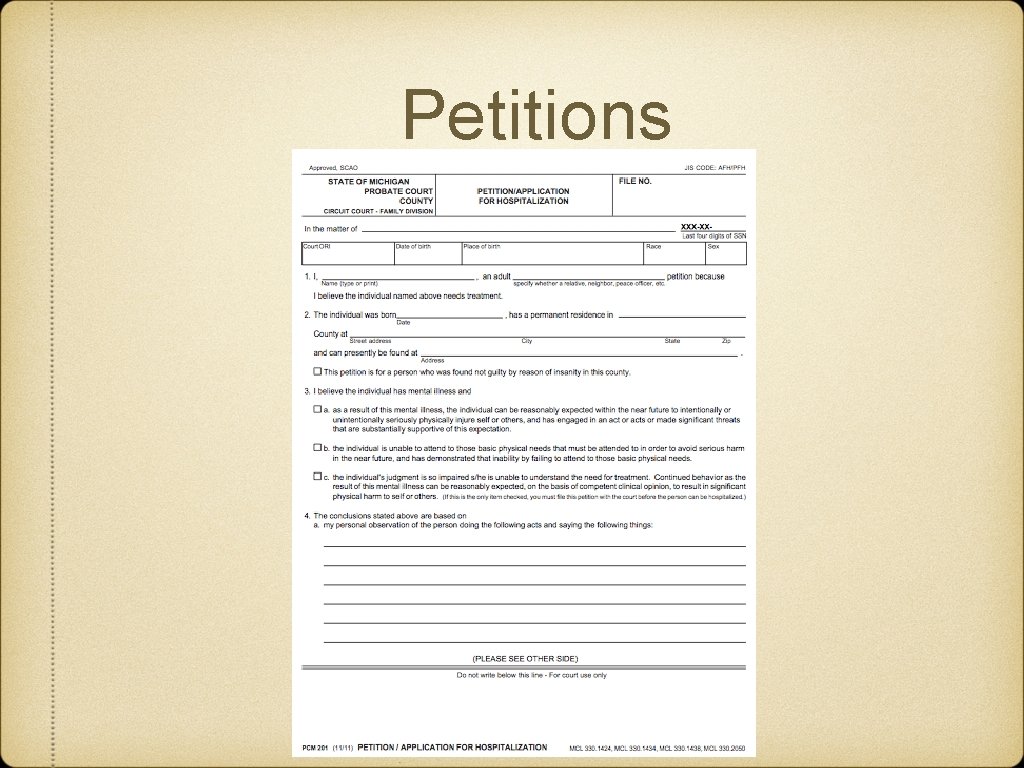
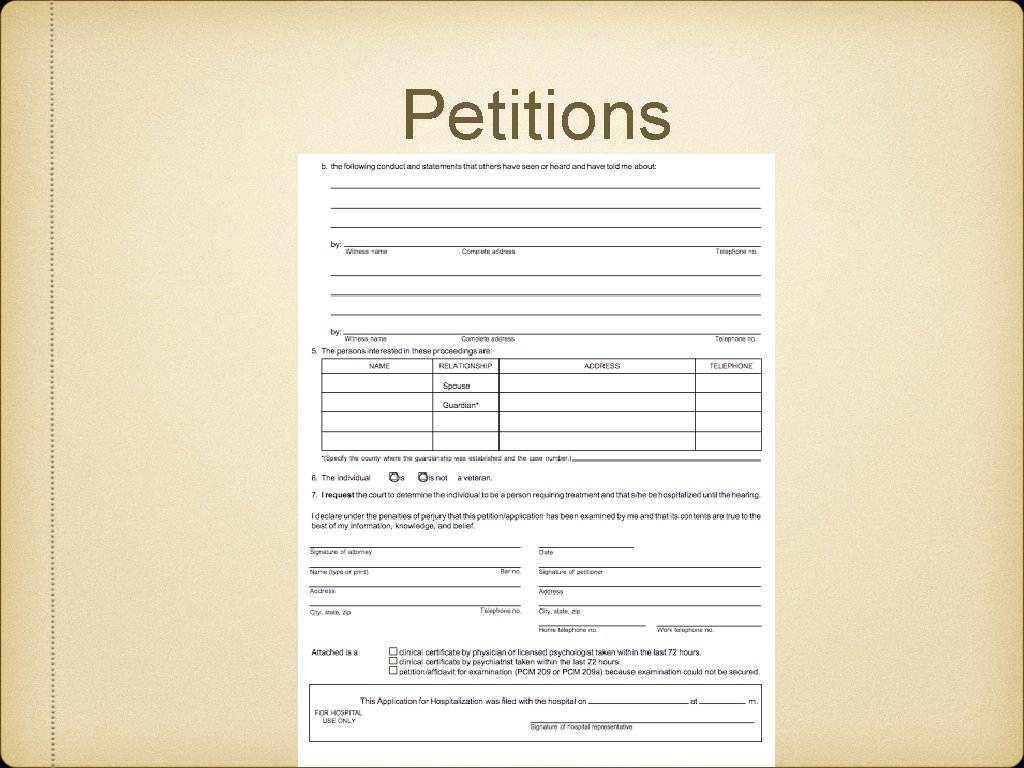
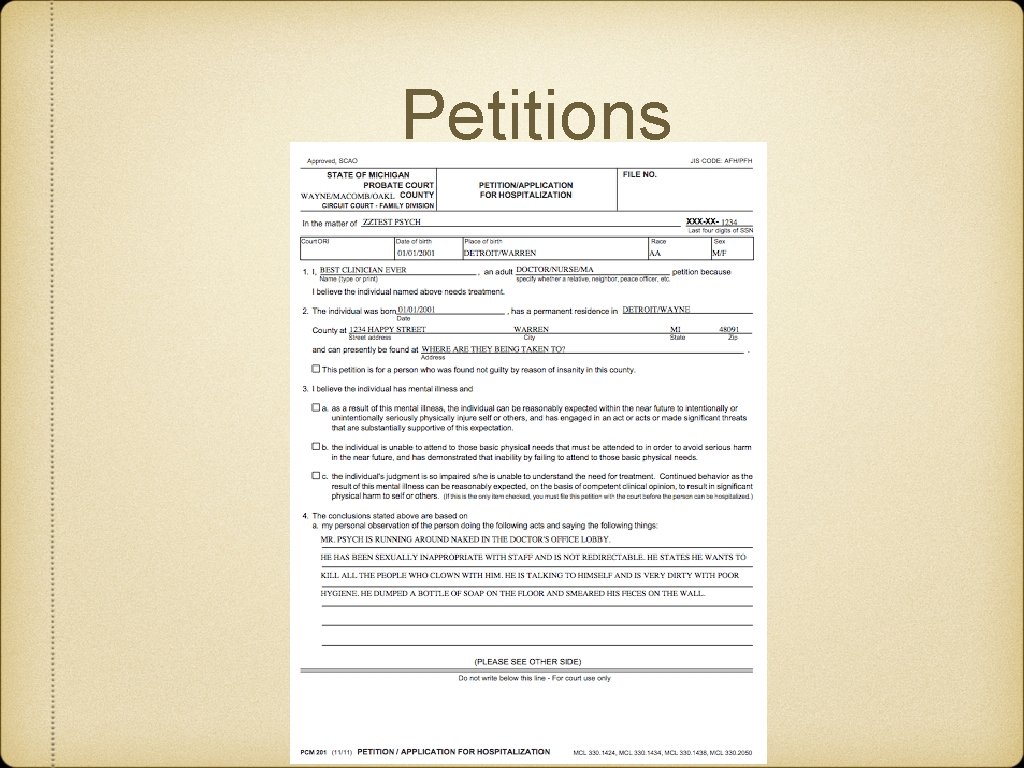
Petitions Anybody can fill out a petition Friend, family, MAA, doctor
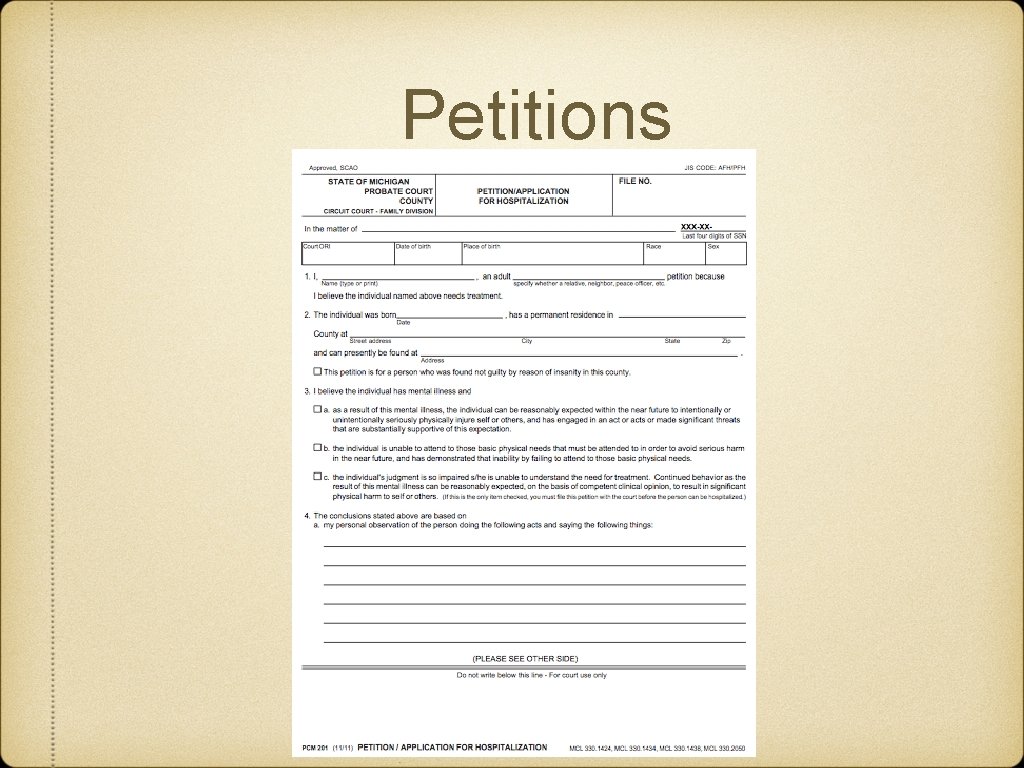
Petitions
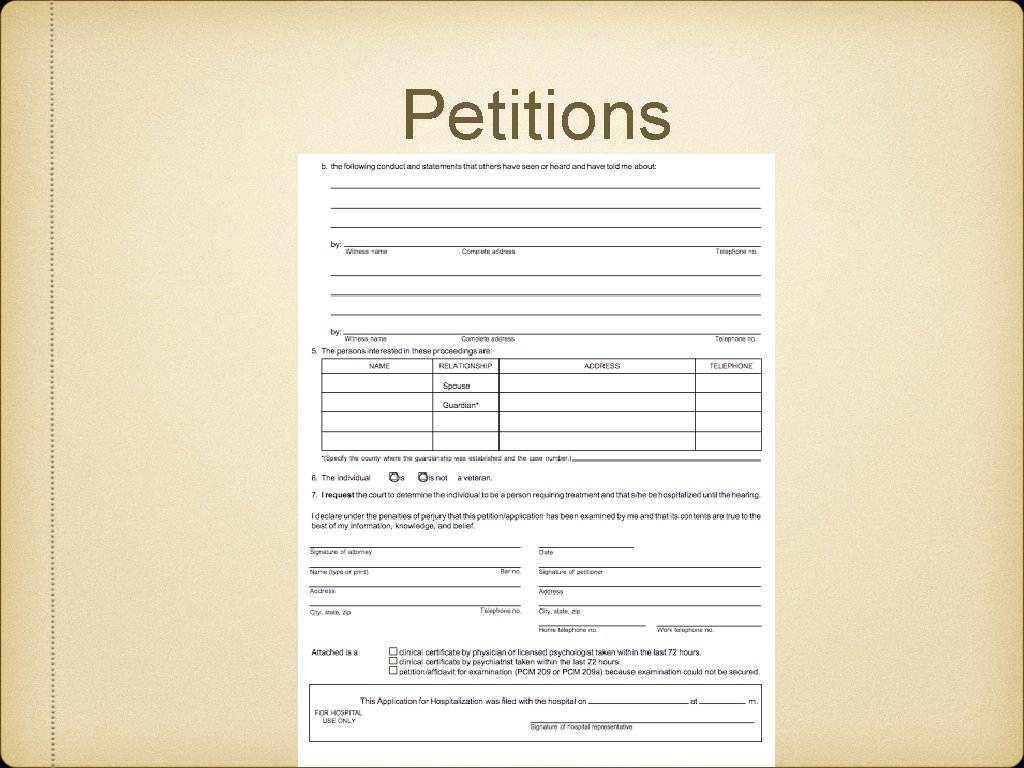
Petitions
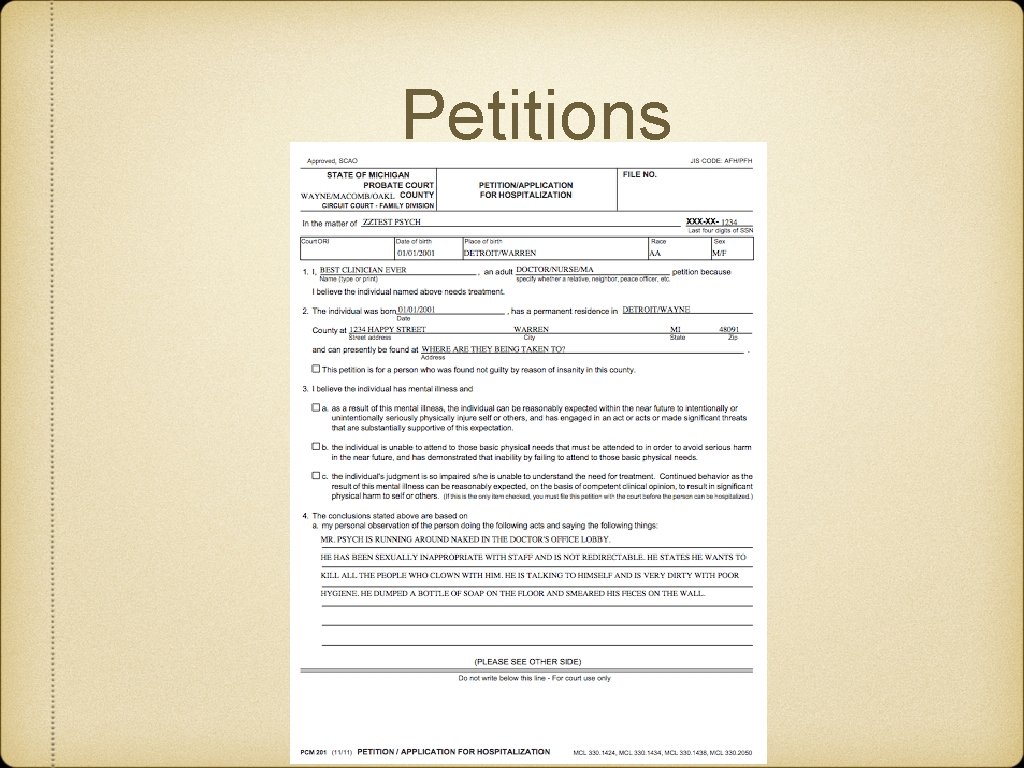
Petitions
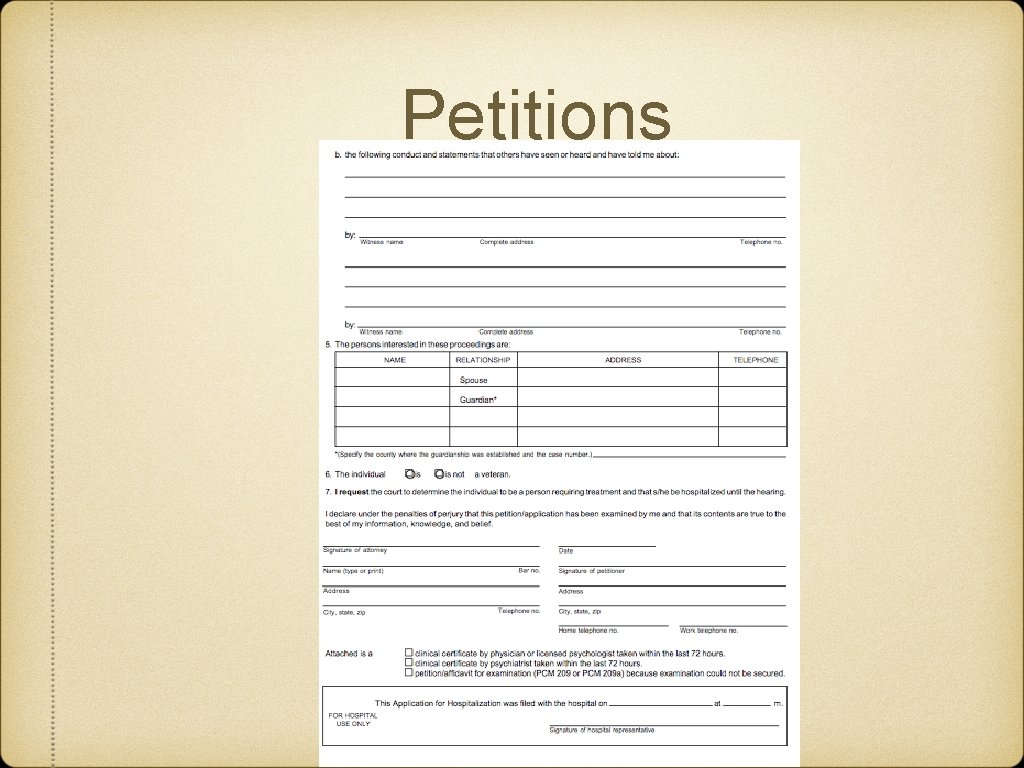
Petitions
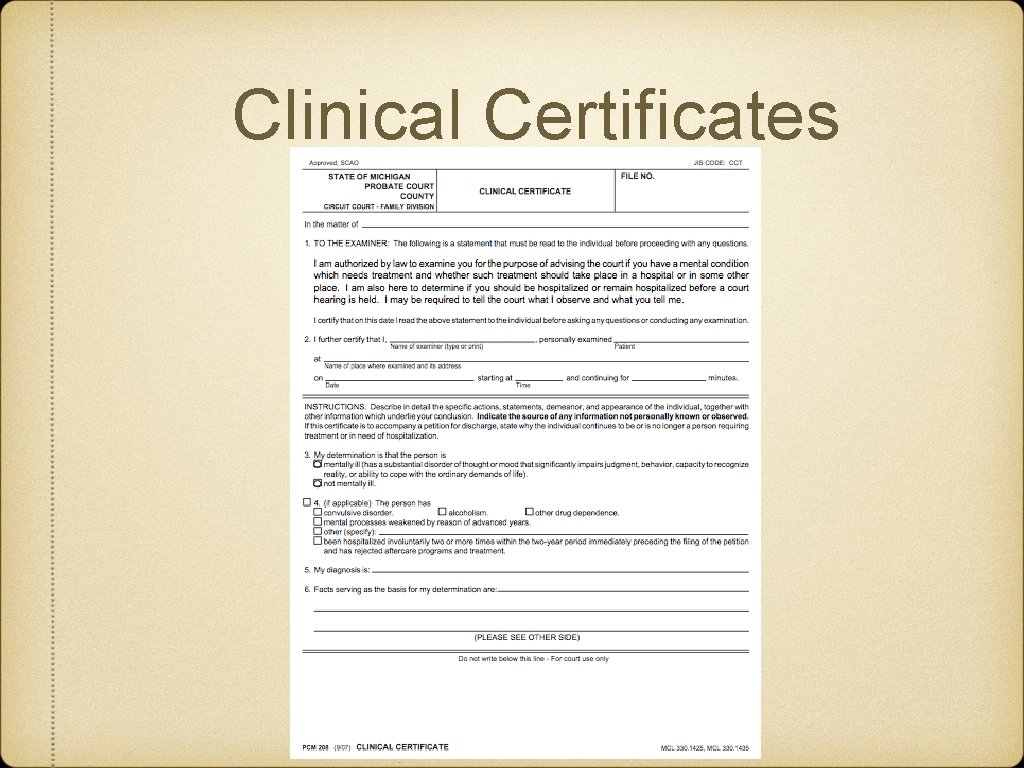
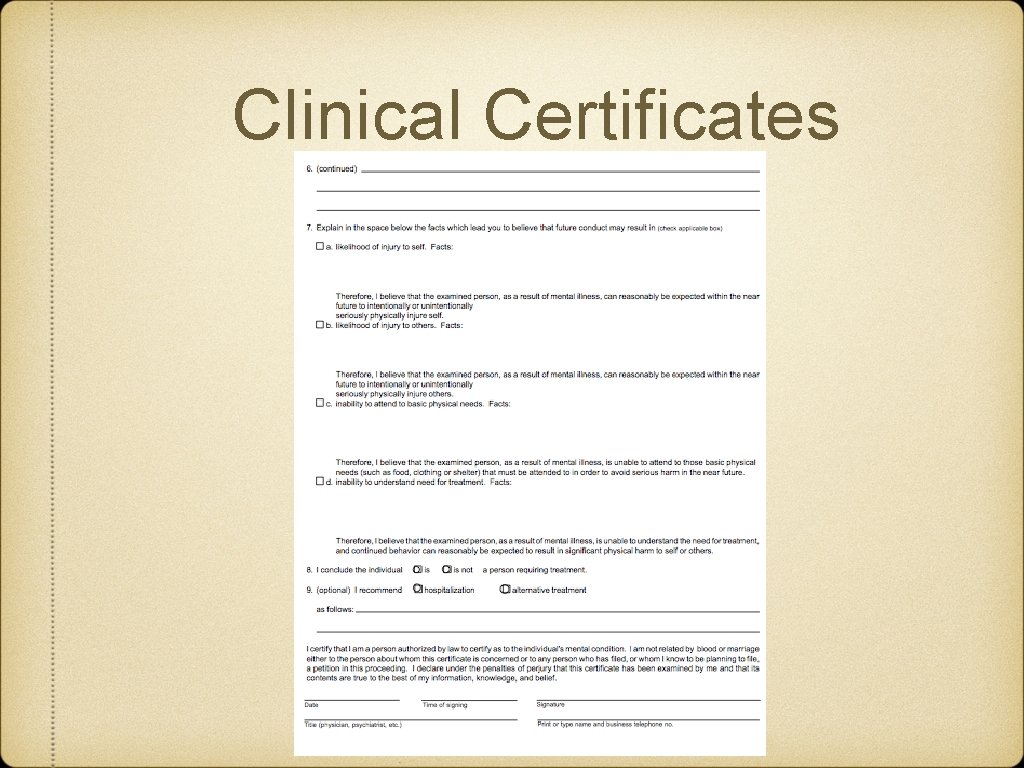
Clinical Certificates Initial can be filled out by any doctor Second can be filled out by psychiatrist or psychologist Patient can be probated with petition and 2 clinical certificates
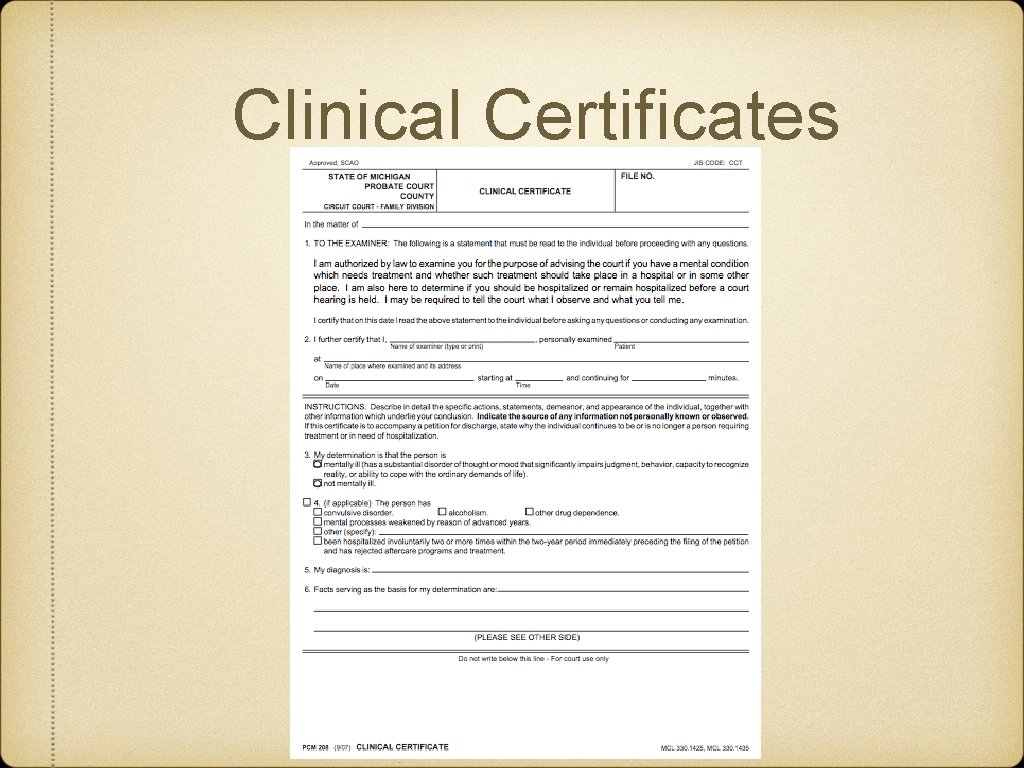
Clinical Certificates
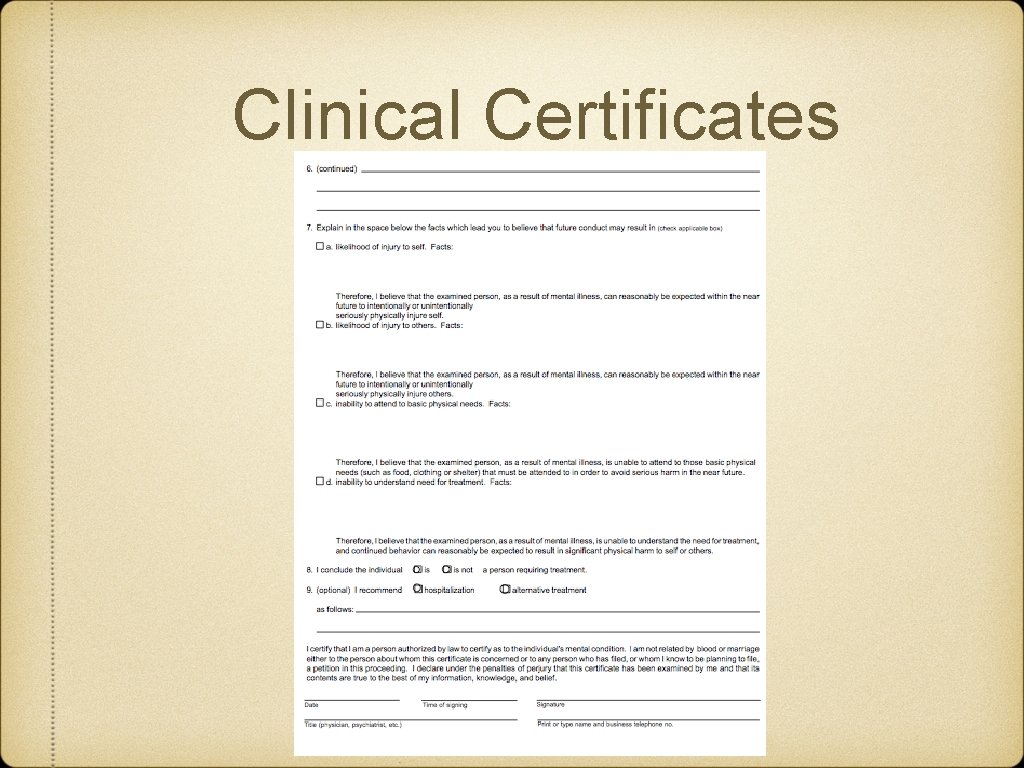
Clinical Certificates
SUICIDAL PATIENT
Emergency Resources for Suicidal Patient National Suicide Prevention Hotline: 1 -800 -273 -TALK The Crisis Center DRH The Crisis Center Sinai Grace
Suicide Risk Assessments PHQ-9 question 9 has a question about self-harm Can miss up to 25% of suicidal patients though. Risk of suicide increases 0. 3% annually for those who answer nearly every day
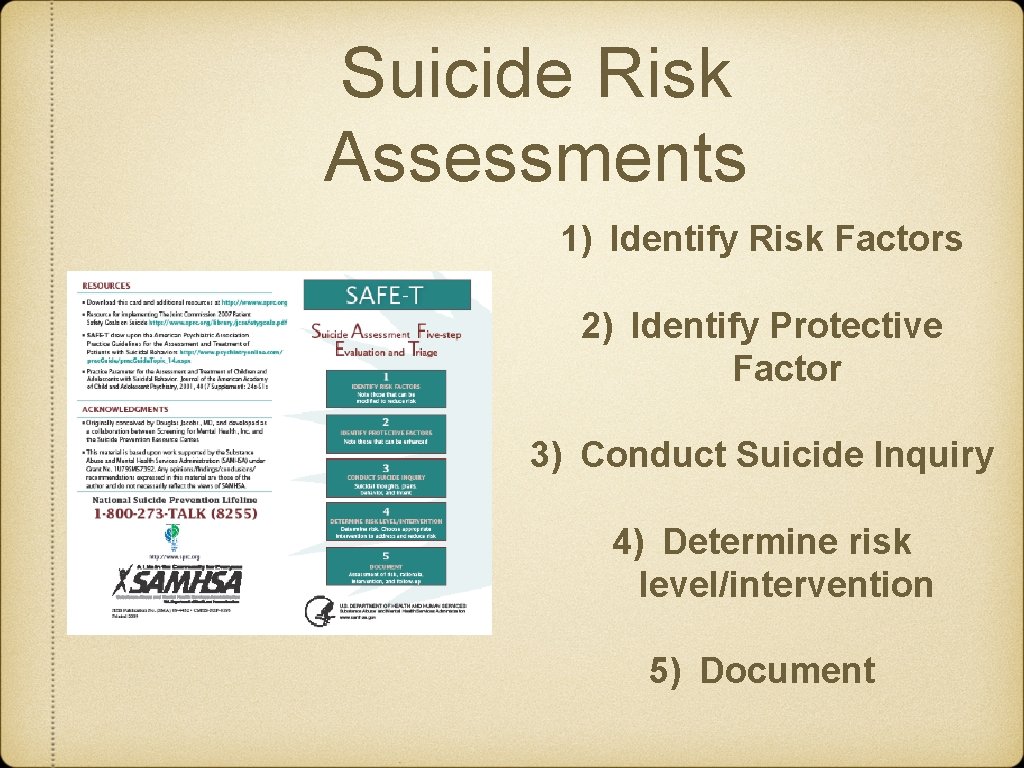
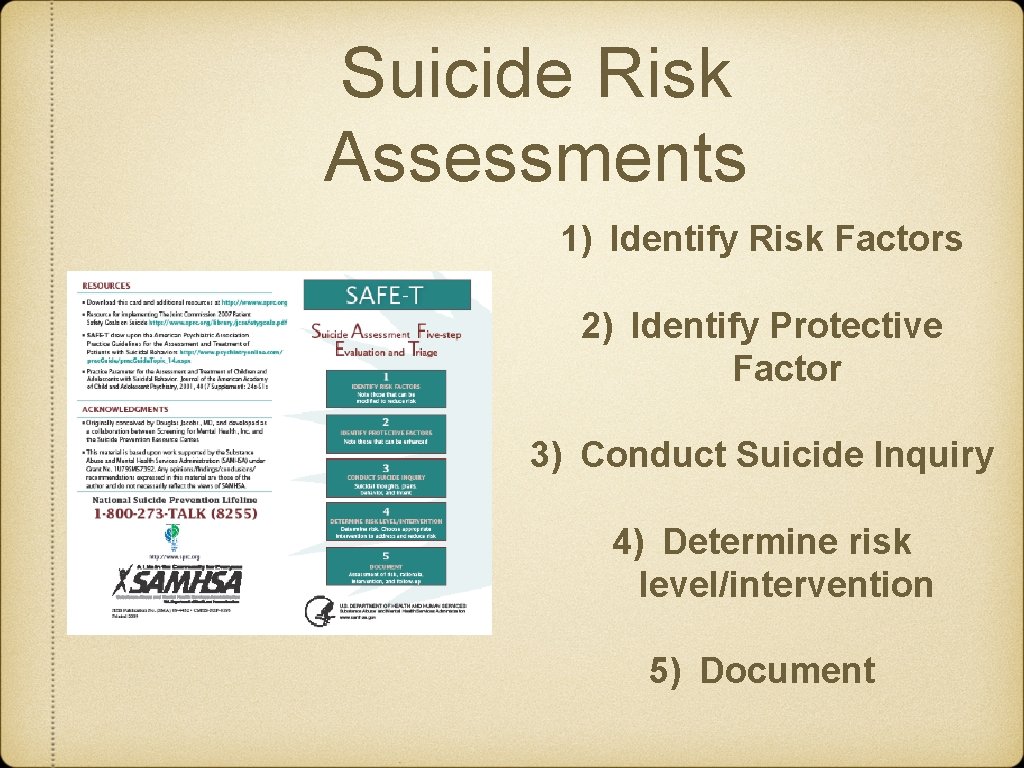
Suicide Risk Assessments 1) Identify Risk Factors 2) Identify Protective Factor 3) Conduct Suicide Inquiry 4) Determine risk level/intervention 5) Document
Suicide Risk Assement SAD PERSONS Sex Age Depression Prior History Ethanol Abuse Rational Thinking Loss Support System Loss
What about cutting? Non-suicidal self-injury (cutting, parasuicide) Does increase risk for self-harm in future Up to 17% of college students, 20% female HS, 9% male HS Focus on what is causing the cutting rather than on cutting itself
PSYCHOTIC PATIENT
Video- Dealing with Non. Violent Psychoses https: //www. youtube. com/watch? feature=player_ detailpage&v=w. SAq 7 Rwuh. Gs
Auditory Hallucination Exercise BREAK INTO GROUPS OF THREE
Auditory Hallucination Debrief What were your thoughts on this exercise? Was it difficult as the interviewer? How did it feel to be the patient? What did the auditory hallucination observe in interaction?
INTOXICATED PATIENT
How to handle intoxication Is patient safe? Trouble breathing? Decreased mental status? Vital signs- HTN, hypotension, tachycardia How did they get to clinic? Discuss risk of withdrawal
AGITATED PATIENT
Violence Risk Assessments There a lot of proprietary assessments Many predictors: previous history of violence, substance abuse, history of incarceration, family violence Up to 50% of medical providers victims of violence during their careers
How to Handle Violent Patient Like BLS Get yourself safe first Somebody call for help WHO DO YOU CALL? Talk to the patient - don’t lie. Trust your gut and act early. Avoid direct eye contact
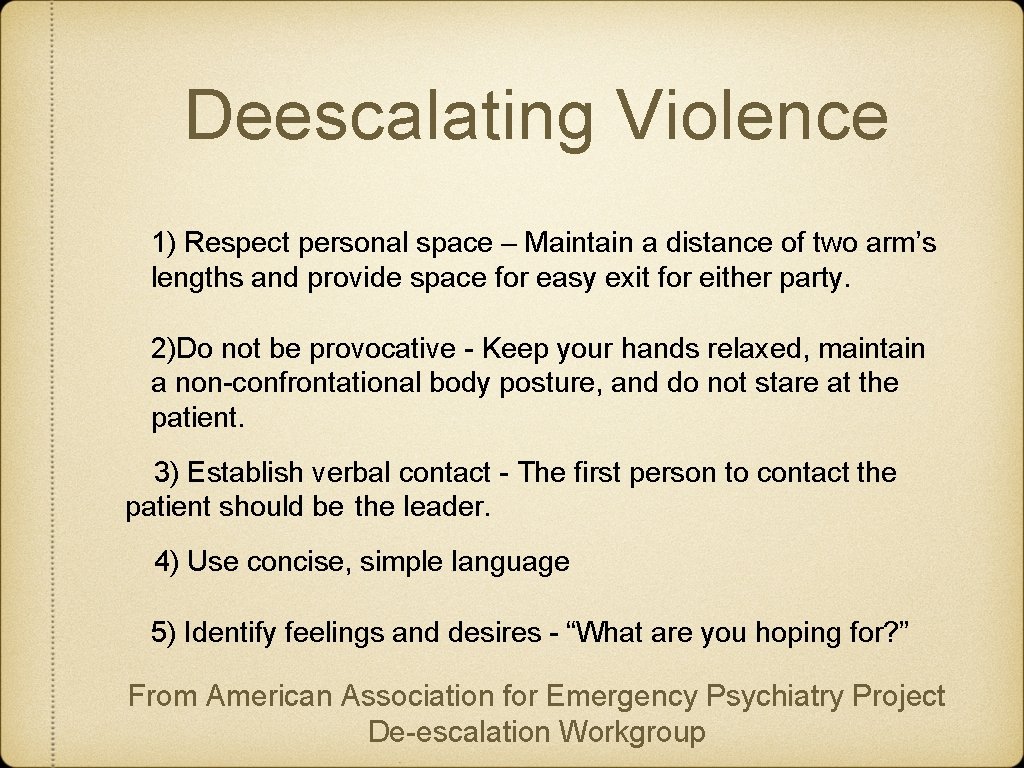
Deescalating Violence 1) Respect personal space – Maintain a distance of two arm’s lengths and provide space for easy exit for either party. 2)Do not be provocative - Keep your hands relaxed, maintain a non-confrontational body posture, and do not stare at the patient. 3) Establish verbal contact - The first person to contact the patient should be the leader. 4) Use concise, simple language 5) Identify feelings and desires - “What are you hoping for? ” From American Association for Emergency Psychiatry Project De-escalation Workgroup
Deescalating Violence 6) Listen closely to what the patient is saying - After listening, restate what the patient said to improve mutual understanding (eg, “Tell me if I have this right…”). 7) Agree or agree to disagree – (a) Agree with clear specific truths; (b) agree in general: “Yes everyone should be treated respectfully; (c) agree with minority situations: “There are others who would feel like you”. 8) Lay down the law and set clear limits - Inform the patient that violence or abuse cannot be tolerated. 9) Offer choices and optimism - Patients feel empowered if they have some choice in matters. 10) Debrief the patient and staff From American Association for Emergency Psychiatry Project De-escalation Workgroup
CASE STUDY Patient is seen pacing around the front talking to herself and holding her head. MAA calls for office manager and comes get a physician Physician tells MAA to call police Patient moved from waiting room to an open office with door opened and patient constantly spoken to
Resources Kitchener, B. A. , & Jorm, A. F. (2002). Mental Health First Aid training for the public: Evaluation of effects knowledge, attitudes and helping behavior. BMC Psychiatry, 2(10), 1 -6. Whitlock J, Eckenrode J, Silverman D (2006). Self-injurious behaviors in a college population. Pediatrics. 117, 1939 -1948. Laye-Gindhu A, Schonert-Rechl KA (2005). Nonsuicidal self-harm among community adolescents: understanding the “whats” and “whys” of self-harm. Journal of Youth and Adolescence. 4, 447 -457. Richmond JS, Berlin JS, Fishkind AB, Holloman GH Jr, Zeller SL, Wilson MP, Rifai MA, Ng AT SO. Verbal De-escalation of the Agitated Patient: Consensus Statement of the American Association for Emergency Psychiatry Project BETA Deescalation Workgroup. West J Emerg Med. 2012 Feb; 13(1): 17 -25.
 Stephen warnick
Stephen warnick Mental health and mental illness chapter 20
Mental health and mental illness chapter 20 Jeopardy mental health
Jeopardy mental health I can prevent most surface emergencies (problems) by
I can prevent most surface emergencies (problems) by Chapter 16 respiratory emergencies
Chapter 16 respiratory emergencies Major nutritional deficiency diseases in emergencies
Major nutritional deficiency diseases in emergencies Lesson 6: cardiac emergencies and using an aed
Lesson 6: cardiac emergencies and using an aed Environmental emergencies emt
Environmental emergencies emt Chapter 23 gynecologic emergencies
Chapter 23 gynecologic emergencies Chapter 22 psychiatric emergencies
Chapter 22 psychiatric emergencies Endocrine and hematologic emergencies
Endocrine and hematologic emergencies Chapter 18 neurologic emergencies
Chapter 18 neurologic emergencies Emt chapter 18 gastrointestinal and urologic emergencies
Emt chapter 18 gastrointestinal and urologic emergencies Chapter 28 first aid and emergencies
Chapter 28 first aid and emergencies Chapter 16 respiratory emergencies
Chapter 16 respiratory emergencies Pumberton sign
Pumberton sign Chapter 35 geriatric emergencies
Chapter 35 geriatric emergencies Chapter 13 handling emergencies
Chapter 13 handling emergencies Chapter 12 behavioral emergencies
Chapter 12 behavioral emergencies Chapter 32 environmental emergencies
Chapter 32 environmental emergencies Chapter 17 cardiovascular emergencies
Chapter 17 cardiovascular emergencies Psychiatric emergencies
Psychiatric emergencies Qut security contact number for emergencies
Qut security contact number for emergencies Immunologic emergencies
Immunologic emergencies A 41 year old man presents with slow irregular breathing
A 41 year old man presents with slow irregular breathing Peninsula
Peninsula Lenawee community mental health authority
Lenawee community mental health authority Van buren community mental health
Van buren community mental health Chapter 3 lesson 3 expressing emotions in healthful ways
Chapter 3 lesson 3 expressing emotions in healthful ways Together for mental health
Together for mental health What is mental health act 2007
What is mental health act 2007 Health triangle mental examples
Health triangle mental examples Titles for mental health presentation
Titles for mental health presentation Health committee introduction
Health committee introduction Wellness in mind nottingham
Wellness in mind nottingham