Local Anaesthesia In Dentistry Masola JW Snr Lect








- Slides: 43
Local Anaesthesia In Dentistry Masola JW: Snr. Lect. Oral & Maxillofacial Surgery Malawi College of Health Sciences
Objectives 1. Define terms: Local analgesia, local anesthetic, general anesthesia, paresthesia, and dysesthesia: 2. Explain the uses of LA in dentistry 3. Explain the advantages of using LA 4. Evaluate how pain can be controlled 5. Mention 3 techniques used for giving LA in dentistry 6. Explain the methods of checking for the effectiveness of LA. 7. Describe the common complications of LA and their management 8. Explain how to conduct pre-anesthesia examinations and patient management. Local Anesthesia in Dentistry E-Learning Resource 2
Definitions • Local analgesia means loss of pain sensation in a limited region and the patient is conscious. • Local Anesthetic is a drug which act upon contact with nerve tissues and renders the tissues incapable of transmitting an impulse on stimulation. Local Anesthesia in Dentistry E-Learning Resource 3
Definitions • Anesthesia is obtained by placing a local anesthetic solution near the sensory nerves so as to temporarily prevent conduction of pain impulses to the brain. Local Anesthesia in Dentistry E-Learning Resource 4
Definitions • General anesthesia a drug which act upon the central nervous system to render the entire body non responsive to pain perception and the patient is unconscious • Anesthesia or Hypoesthesia: loss or decrease respectively, of sensation in an area. • Paresthesia: Subjective sensation of burning, tingling, needles and pins, numbness, etc. • Dysesthesia: Abnormal unpleasant sensation to normal stimulus, e. g. , burning sensation to simple touch Local Anesthesia in Dentistry E-Learning Resource 5
Ways of Administering Anaesthesia Anesthesia can be administered through the following ways: – Intramuscular injection – Topically – Intravenous (iv) Local Anesthesia in Dentistry E-Learning Resource 6
TECHNIQUES OF DENTAL LOCAL ANESTHESIA There are three different techniques used in dental anesthesia: 1. local infiltration technique 2. nerve block 3. periodontal ligament injection (Intraligamental) Local Anesthesia in Dentistry E-Learning Resource 7
DENTAL USES OF LOCAL ANESTHESIA Oral & Maxillofacial Surgery
DENTAL USES OF LOCAL ANESTHESIA 1. Elimination of Pain During Dental Treatment Painless routine dental treatment such as extraction, conservation of teeth, treatment of dry socket, minor oral surgery such as the removal of small cysts and tumors, periodontal surgery. It also can be used for the rapid relief of pain before active measures begin to act. Local Anesthesia in Dentistry E-Learning Resource 9
2. Diagnostic Purposes Major part of the face receives its sensory supply from the Trigeminal Nerve which also innervates jaws, teeth & other structures such as the maxillary antrum. Severe pain may originate from any of these, and it may be impossible for the patient to localize it accurately, possibly because of the phenomenon of Referred pain. When a nerve has several branches, pain originating from a structure innervated by one branch may be misinterpreted by the patient as being localized in another structure innervated by a different branch. Local Anesthesia in Dentistry E-Learning Resource 10

DENTAL USES OF LOCAL ANESTHESIA 3. Scaling & root planning 4. Gingival curettage 5. Extreme cases of gingival inflammation and discomfort 6. Instrumentation of extreme hypersensitive teeth Local Anesthesia in Dentistry E-Learning Resource 11
Surgery Procedures • I&D • Tooth extraction • Biopsy • Sequestrectomy • Fracture reduction and fixation Local Anesthesia in Dentistry Procedures • Cystectomy • Arrest hemorrhage • Create a dry surgical site • Pain relief • Conservative treatment (nervous patients) E-Learning Resource 12
An abscess in a mandibular premolar region may cause symptoms of acute pain in a maxillary tooth on the same side. Fortunately, pain from a lesion innervated by Trigeminal nerve is not referred across midline. The only exception is incisors region, where innervations come from network of nerves from both sides. LA is given to block a nerve in a particular region and if pain is relieved, then the causative lesion is in the tissue innervated by that nerve. Local Anesthesia in Dentistry E-Learning Resource 13
Pain Control • Pain is an unpleasant sensory & emotional experience associated with actual or potential tissue damage , or described in terms of such damage. ” • Pain Perception: PP It is the physio-anatomical process by which pain is received & transmitted by neural structures from the end organs through the perceptive & conductive mechanisms. This phase of pain is practically the same in all healthy persons, but it can be affected by disease and toxic states. Local Anesthesia in Dentistry E-Learning Resource 14
Contraindications to LA Some of these are not absolute CI but circumstantial only: 1. Presence of infection in pathway of needle insertion. 2. Presence of a history of allergic reaction to LA drug. 3. When patient is below the age of reason. 4. Patient is unable to cooperate due to mental disorder. 5. In major oral surgery when LA is unfavorable. 6. When patient refuses LA due to fear or apprehension. 7. Patients with uncontrolled hyperthyroidism when LA might precipitate a thyroid crisis. 8. Patients with advanced renal diseases or liver cirrhosis. Local Anesthesia in Dentistry E-Learning Resource 15
Pain Control • Pain Reaction: PR It is the patient's manifestation of his perception of pain experience. The reaction will differ from person to person & from day to day in the same person. Manifestations such as facial expressions, crying out, tapping the feet; perspiring, tachycardia & alternation in respirations may be encountered. The degree of pain reaction is determined by patient's pain threshold. Local Anesthesia in Dentistry E-Learning Resource 16
Pain Control • Pain Threshold: A patient with a high pain threshold can tolerate pain. Pain threshold is inversely proportional to pain reaction. The pain threshold is affected by the following factors: 1. 2. 3. 4. Fatigue: ----causes low pain threshold. Age: ----Elder individuals have higher pain threshold than young. Sex: -----generally men have a higher pain threshold than women. Fear & Apprehension: ------cause low pain threshold Local Anesthesia in Dentistry E-Learning Resource 17
Pain Control Pain perception – Removal of cause (stimulus): environmental changes in tissues would be eliminated & the free nerve endings would not be excited & no impulses would be initiated. – Blocking Pathway of Painful Impulses: a LA solution is injected into tissues in proximity to nerves involved. Pain Reception • Raising Pain Threshold: by using analgesics. These drugs raise pain threshold centrally & therefore interfere with pain reaction, i. e. pain pathway will be intact but able to conduct impulses, but pain reaction will be decreased. There are other psychosomatic methods. • Preventing Pain Reaction by Cortical Depression: This is the scope of GA, depression of CNS to prevent any conscious reaction to a painful stimulus. Local Anesthesia in Dentistry E-Learning Resource 18
Pain Control • Sensations from jaws & teeth are conducted through sensory fibers of maxillary & mandibular divisions of Trigeminal nerve ( peripheral processes – dendrites). • These fibers receive impulses from their somatic sensory area & conduct them to their mother cells in the Gasserian ganglion from which they originate. Local Anesthesia in Dentistry E-Learning Resource 19
Pain Control • Pain Preceptors ( Nociceptors ) They are naked nerve endings, mostly unmyelinated fibers in the form of delicate loops , or long naked hair - like network. • Stimulus It is environmental change in the excitable tissue: – electrical in nature – thermal in nature – chemical in nature – mechanical in nature Local Anesthesia in Dentistry E-Learning Resource 20
Pain Control Threshold stimulus • Stimulus that is just sufficient to excite free nerve endings by minimal environmental change in tissue. • Sub-threshold stimulus will not excite fine nerve endings or create an impulse, regardless of its duration. Impulse • Wave of excitation that spreads along nerve fiber. • Self-propagating & of equal intensity regardless the degree of stimulation. Local Anesthesia in Dentistry E-Learning Resource 21
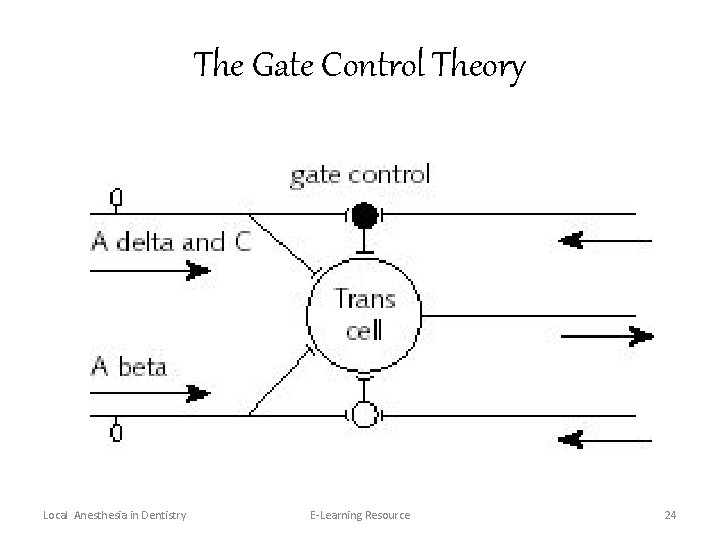
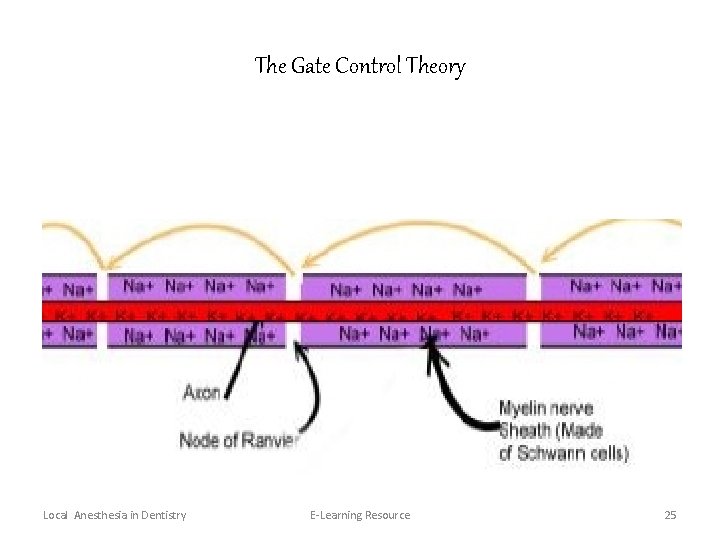
Pain Control • It was introduced by Melzock and Wall (1965) with hope of more accurately explaining mechanism of pain. • It affords an explanation for the fact that impulses conveying different sensations may be transmitted faithfully, modified or delayed. • It postulates that an intermediary cell acts as a “gate” to the transmitting cell (T) & normally inhibits activity. • The Substantia Gelatinosa (SG) in the dorsal horn of the spinal cord functions as a gate control mechanism that modulates ( inhibits or facilitates) afferent impulses before they influence the T cells. Local Anesthesia in Dentistry E-Learning Resource 22

The Gate Control Theory • This modulation also takes place in other synaptic sites in the CNS. • Excitatory & inhibitory influences occur on impulses at various levels in CNS so that perception & reaction become merely facets of the same mechanism rather than separate components of it. • The control is mediated by inhibitory chemical transmitter, the Encephalin ( Endorphins ), which are endogenous opioids released by short intermediary or control neurons. Local Anesthesia in Dentistry E-Learning Resource 23
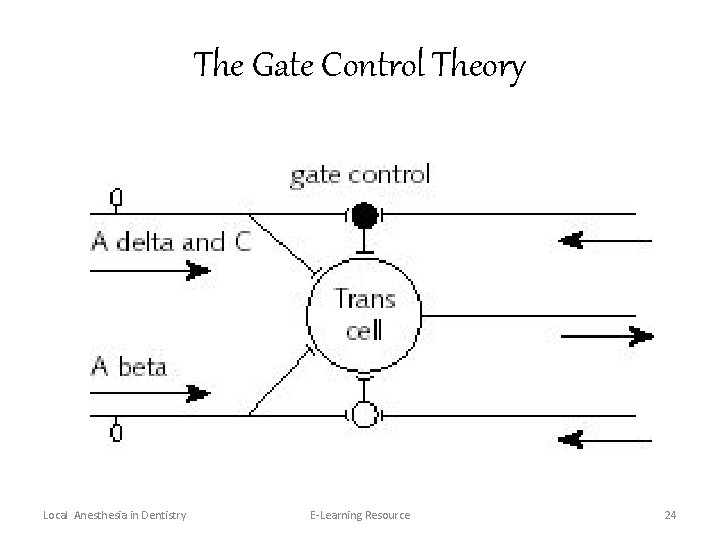
The Gate Control Theory Local Anesthesia in Dentistry E-Learning Resource 24
The Gate Control Theory Local Anesthesia in Dentistry E-Learning Resource 25
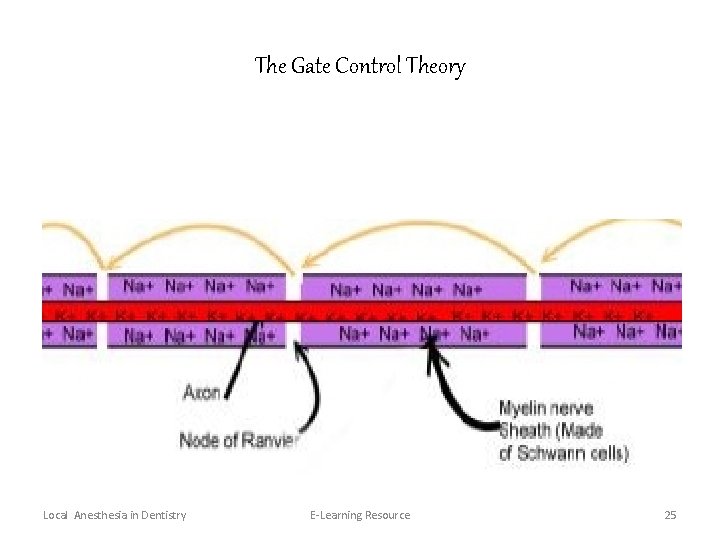
Nerve Conduction • It is the process of propagation of impulses through nerve. • Depends on electrical potential existing across nerve membrane. Resting Potential • High concentration of Na+ outside nerve membrane as it is slightly permeable to Na+. • High concentration of K+ inside it as it is freely permeable to K+ & Cl Local Anesthesia in Dentistry E-Learning Resource 26
Nerve Conduction Depolarization • Nerve excitation causes increased permeability of nerve membrane to Na+. • Na + rush into axon & causes depolarization ( become positive) • Na + influx Localized electrical circuits are established which cause further influx of Na + , & so progression of impulse. • K + efflux Behind the impulse, K + begin to leave axon. Repolarization • As impulse progresses, with efflux of K + , the nerve membrane become repolarized behind impulse. Local Anesthesia in Dentistry E-Learning Resource 27
Nerve Conduction Sodium Pump After impulse has passed & nerve membrane is repolarized Na + are once again actively expelled in order to increase external concentration & allow passage of another impulse. Local Anesthesia in Dentistry E-Learning Resource 28
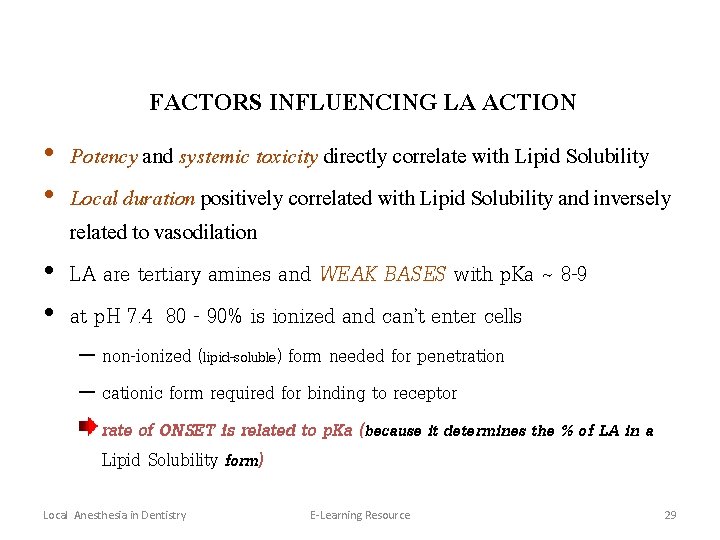
FACTORS INFLUENCING LA ACTION • Potency and systemic toxicity directly correlate with Lipid Solubility • Local duration positively correlated with Lipid Solubility and inversely related to vasodilation • LA are tertiary amines and WEAK BASES with p. Ka ~ 8 -9 • at p. H 7. 4 80 - 90% is ionized and can’t enter cells – non-ionized (lipid-soluble) form needed for penetration – cationic form required for binding to receptor rate of ONSET is related to p. Ka (because it determines the % of LA in a Lipid Solubility form) Local Anesthesia in Dentistry E-Learning Resource 29
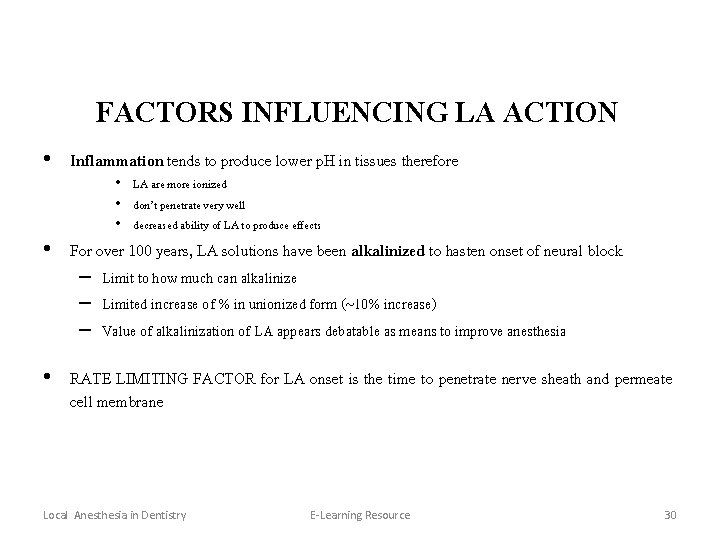
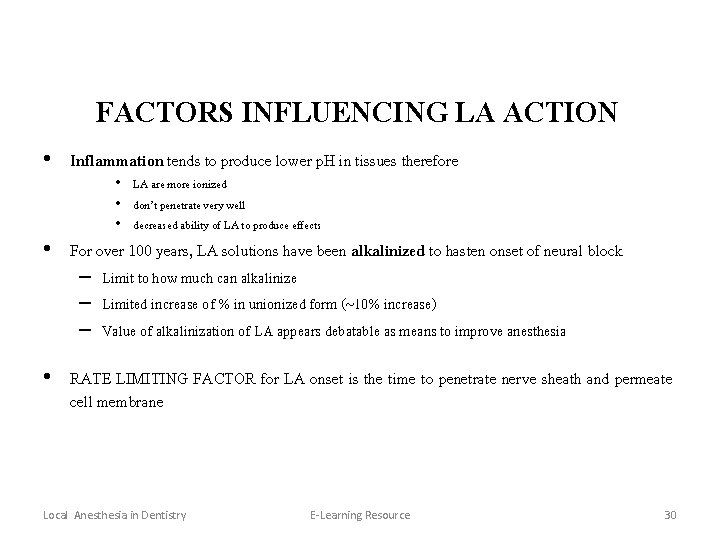
FACTORS INFLUENCING LA ACTION • Inflammation tends to produce lower p. H in tissues therefore • LA are more ionized • don’t penetrate very well • decreased ability of LA to produce effects • For over 100 years, LA solutions have been alkalinized to hasten onset of neural block – Limit to how much can alkalinize – Limited increase of % in unionized form (~10% increase) – Value of alkalinization of LA appears debatable as means to improve anesthesia • RATE LIMITING FACTOR for LA onset is the time to penetrate nerve sheath and permeate cell membrane Local Anesthesia in Dentistry E-Learning Resource 30
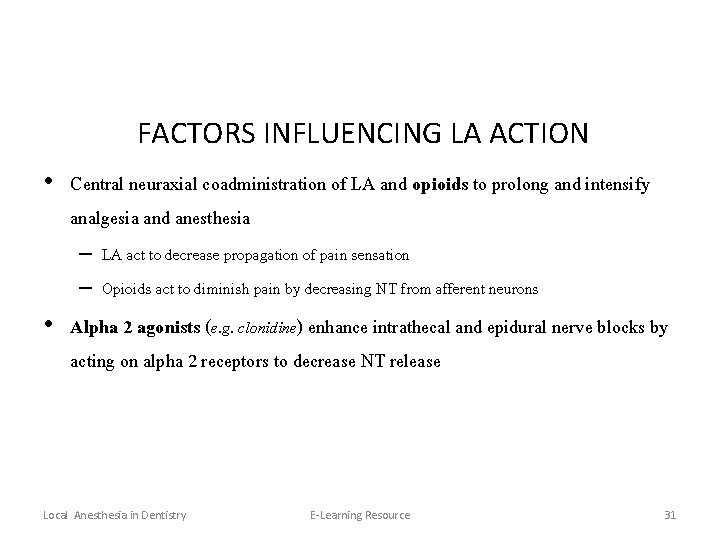
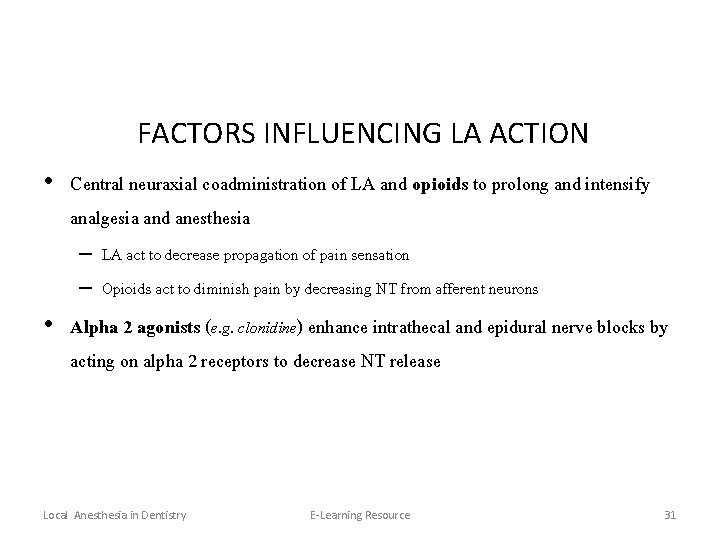
FACTORS INFLUENCING LA ACTION • Central neuraxial coadministration of LA and opioids to prolong and intensify analgesia and anesthesia – LA act to decrease propagation of pain sensation – Opioids act to diminish pain by decreasing NT from afferent neurons • Alpha 2 agonists (e. g. clonidine) enhance intrathecal and epidural nerve blocks by acting on alpha 2 receptors to decrease NT release Local Anesthesia in Dentistry E-Learning Resource 31

Systemic Effects (toxicities) • Extensions of pharmacological action • Primarily related to blocking sodium channels • Intensity is dependent on blood levels • Toxic levels of LA in blood will not occur if absorption (into systemic blood) is slow or metabolism is rapid • CNS (More sensitive than cardio) – Dose-related spectrum of effects and All effects are due to depression of neurons • First an apparent CNS stimulation (convulsions most serious) • Followed by CNS depression (death due to respir depression) • Premonitory signs include: ringing in ears, metalic taste, numbness around lips – Cocaine - euphoria (unique in its ability to stimulate CNS) – Lidocaine - sedation even at non-toxic doses Local Anesthesia in Dentistry E-Learning Resource 32
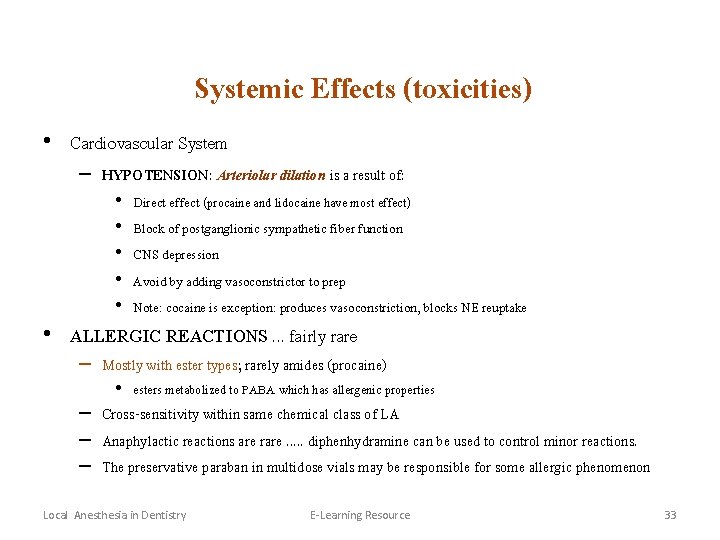
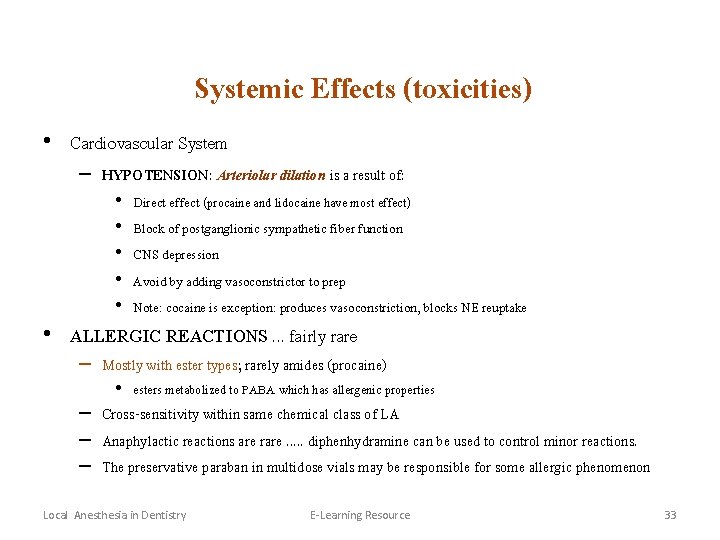
Systemic Effects (toxicities) • Cardiovascular System – HYPOTENSION: Arteriolar dilation is a result of: • • • Direct effect (procaine and lidocaine have most effect) Block of postganglionic sympathetic fiber function CNS depression Avoid by adding vasoconstrictor to prep Note: cocaine is exception: produces vasoconstriction, blocks NE reuptake • ALLERGIC REACTIONS. . . fairly rare – Mostly with ester types; rarely amides (procaine) • esters metabolized to PABA which has allergenic properties – Cross-sensitivity within same chemical class of LA – Anaphylactic reactions are rare. . . diphenhydramine can be used to control minor reactions. – The preservative paraban in multidose vials may be responsible for some allergic phenomenon Local Anesthesia in Dentistry E-Learning Resource 33
Systemic Effects (toxicities) • NEUROTOXICITY – LA can cause concentration-dependent nerve damage to central and peripheral NS – Mechanism(s) not clear – Permanent neurological injury is rare – May account for transient neurological symptoms after spinal anesthesia • Cauda equina syndrome Local Anesthesia in Dentistry E-Learning Resource 34
THINGS TO REMEMBER • • Give smallest volume and dose Make injections slowly to avoid inadvertent IV Have drugs available to manage adverse effects Don’t take food or liquids < 60 minutes after oral topical application. . gag, swallow, cough reflexes may be not working Local Anesthesia in Dentistry E-Learning Resource 35





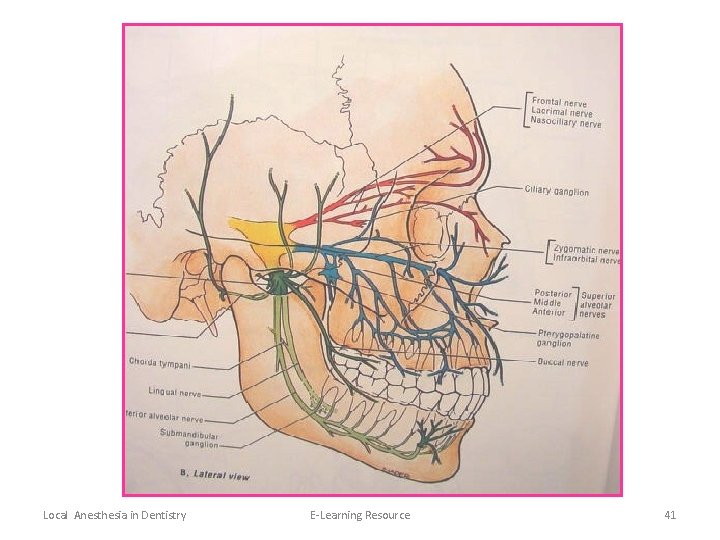
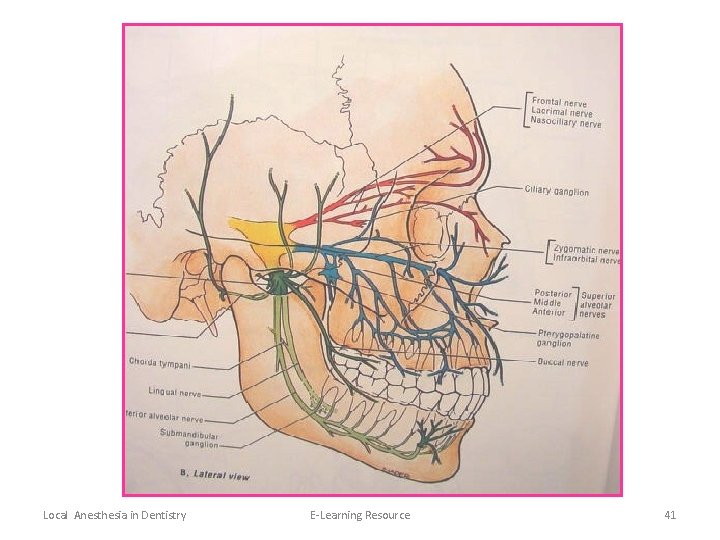
Local Anesthesia in Dentistry E-Learning Resource 41
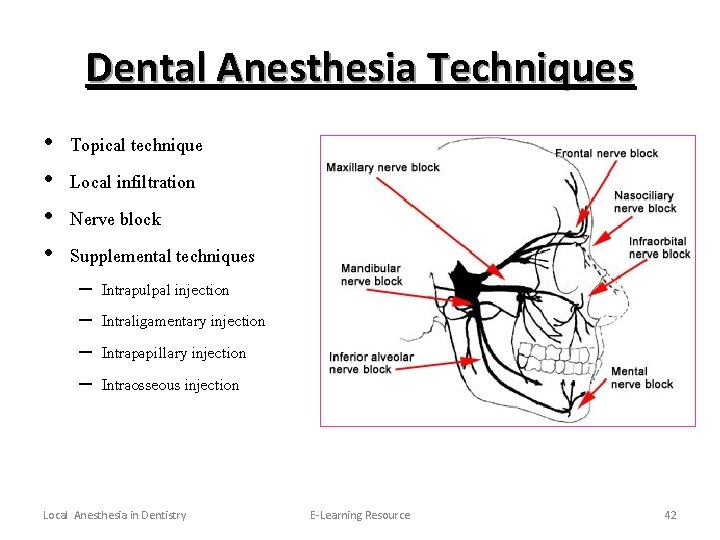
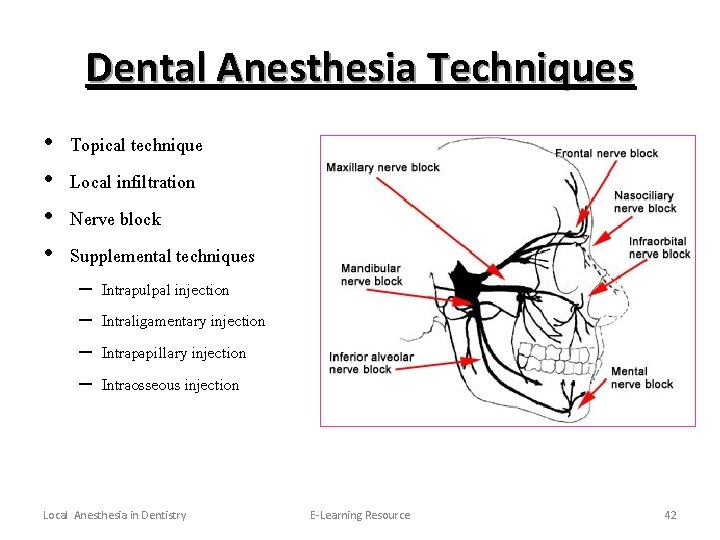
Dental Anesthesia Techniques • • Topical technique Local infiltration Nerve block Supplemental techniques – – Intrapulpal injection Intraligamentary injection Intrapapillary injection Intraosseous injection Local Anesthesia in Dentistry E-Learning Resource 42
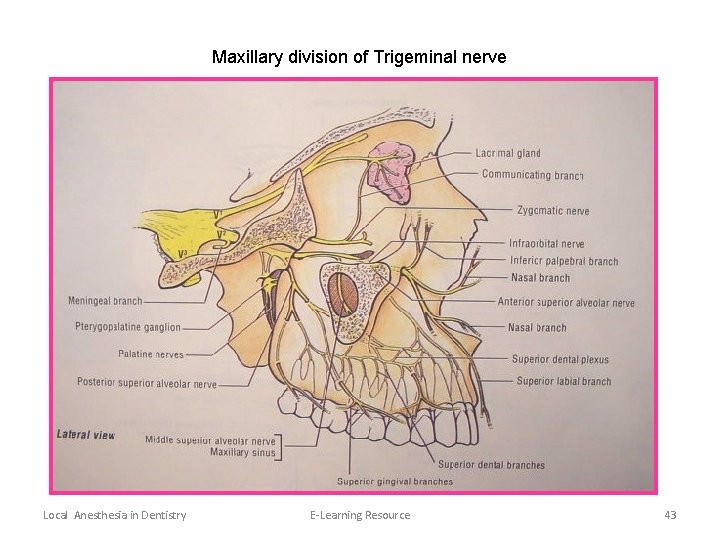
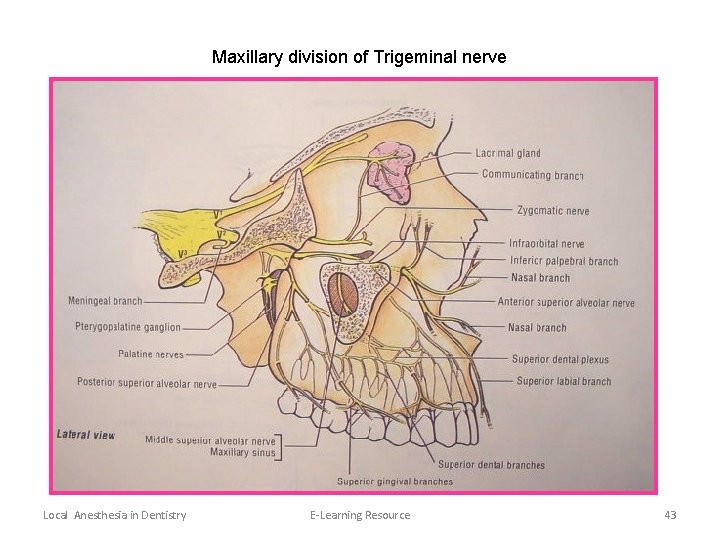
Maxillary division of Trigeminal nerve Local Anesthesia in Dentistry E-Learning Resource 43
 Var lect
Var lect Lidocaine max dose
Lidocaine max dose Appherensive
Appherensive Carotid sinus hypersensitivity
Carotid sinus hypersensitivity Hareket tremoru
Hareket tremoru Snr signal to noise ratio
Snr signal to noise ratio Contamination by extraneous signals from human sources
Contamination by extraneous signals from human sources Snr margin
Snr margin Spine palpation landmarks
Spine palpation landmarks Anaesthesia information management system
Anaesthesia information management system Lardosis
Lardosis Components of anaesthesia
Components of anaesthesia Snr formula for delta modulation
Snr formula for delta modulation Snr
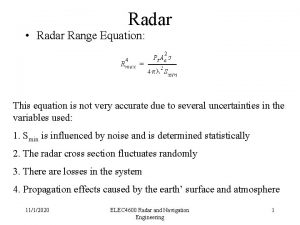
Snr Radar range equation snr
Radar range equation snr Imsi szám lekérdezése
Imsi szám lekérdezése Kraniosinostozis
Kraniosinostozis Netwk
Netwk Balanced anesthesia components
Balanced anesthesia components Tam akustik baret
Tam akustik baret Epidural catheter markings measurement
Epidural catheter markings measurement Snr
Snr Tychos snr
Tychos snr Snr
Snr Snr 공식
Snr 공식 Snr
Snr Snr menu
Snr menu Spinal anaesthesia site
Spinal anaesthesia site Dr pradnya joshi
Dr pradnya joshi Snr giraffe
Snr giraffe Thyromental distance fingers
Thyromental distance fingers Balanced anaesthesia ppt
Balanced anaesthesia ppt Snr signal to noise ratio
Snr signal to noise ratio Head tilt chin lift jaw thrust
Head tilt chin lift jaw thrust Radar systems analysis and design using matlab
Radar systems analysis and design using matlab Siliospinal refleks nedir
Siliospinal refleks nedir Structures pierced during spinal anaesthesia
Structures pierced during spinal anaesthesia Snr signal to noise ratio
Snr signal to noise ratio Neutron star
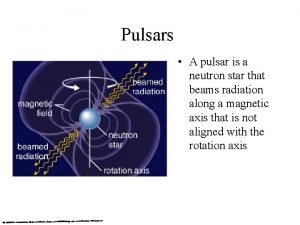
Neutron star Glaskow koma skalası nedir
Glaskow koma skalası nedir Snr 공식
Snr 공식 Two drawbacks of a think local act local
Two drawbacks of a think local act local Local vertical local horizontal frame
Local vertical local horizontal frame A think local act local multicountry type of strategy
A think local act local multicountry type of strategy