Life Threatening Dysrhythmias Life Threatening Dysrhythmias A lifethreatening

- Slides: 46
Life Threatening Dysrhythmias
Life Threatening Dysrhythmias A life-threatening dysrhythmia is any rhythm that is associated with cardiac compromise and potential drop in cardiac output. Ventricular dysrhytmias, V-Tach and V-Fib are considered the most lethal but any abnormal beat can propagate the lead to compromise cardiac output state. Rhythm disturbance is considered the primary cause of sudden cardiac death (SCD).
Sudden Cardiac Death Defined by AHA as death resulting from the sudden, abrupt loss of heart function in a person who may or may not have been previously diagnosed with heart disease. 400, 000 deaths per year 1, 000 deaths per day 80 -90% of SCD victims have CAD Rhythm disturbance is the primary cause of SCD Left Ventricular Dysfunction is the 2 nd leading cause of SCD Previous cardiac arrest is 3 rd leading cause of SCD
Cardiac Electrophysiology Automaticity: is the ability of each cardiac cell to generate a spontaneous impulse. The Sinoatrial (SA) node is the primary pacemaker of the heart because of the principles of: Lack of Competition and Frequency Dependent Inhibitions Conductivity: is the transmission of the electrical impulse to adjacent cells, creating a depolarizing wave and subsequent myocardial contraction.
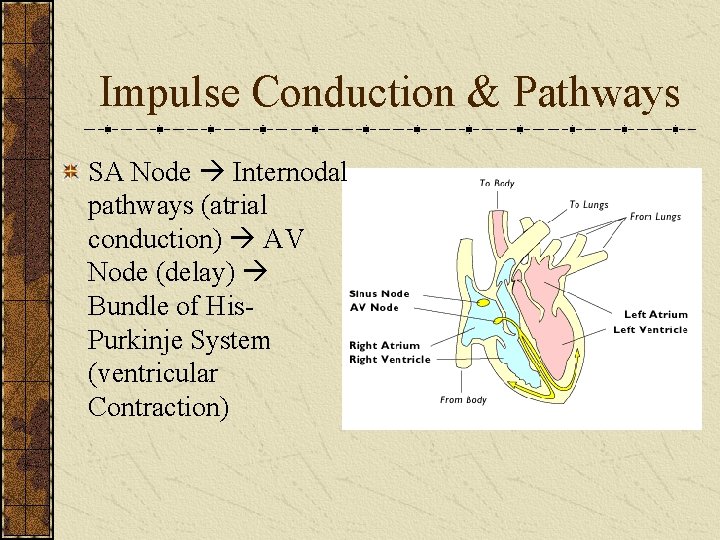
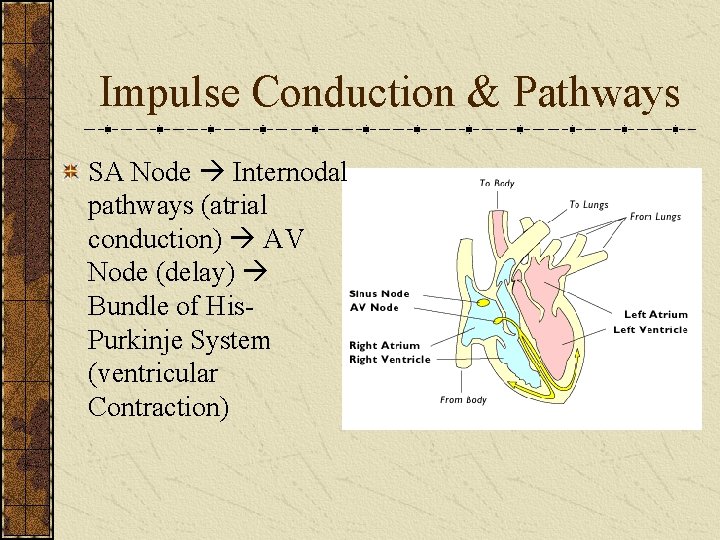
Impulse Conduction & Pathways SA Node Internodal pathways (atrial conduction) AV Node (delay) Bundle of His. Purkinje System (ventricular Contraction)
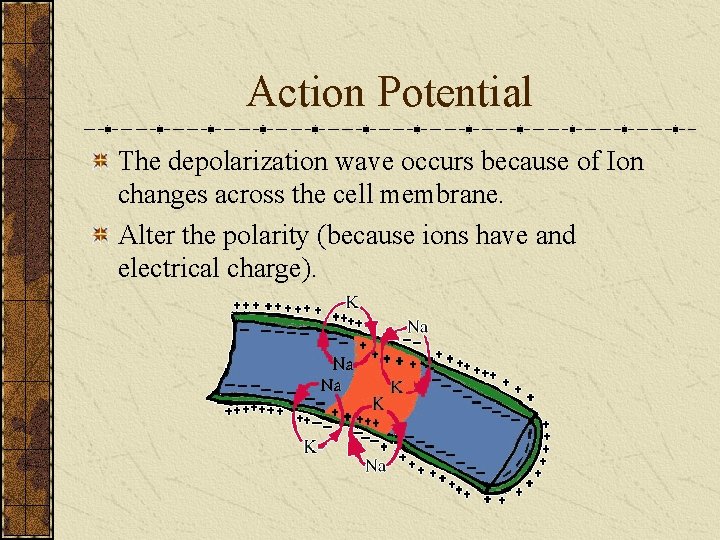
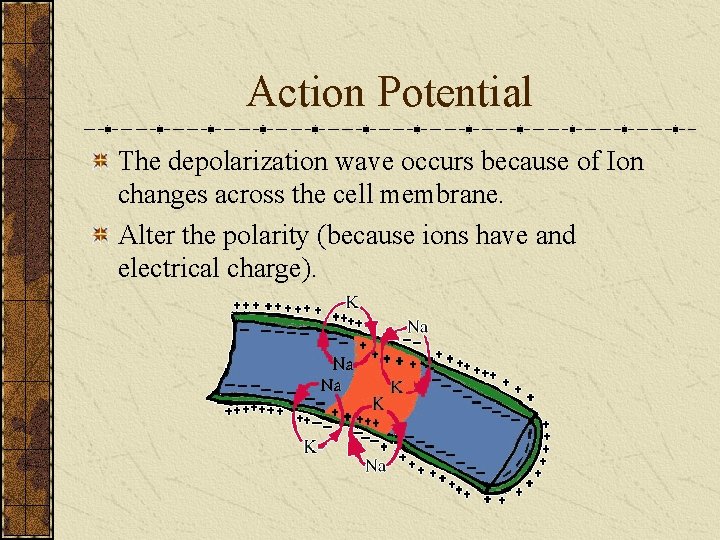
Action Potential The depolarization wave occurs because of Ion changes across the cell membrane. Alter the polarity (because ions have and electrical charge).
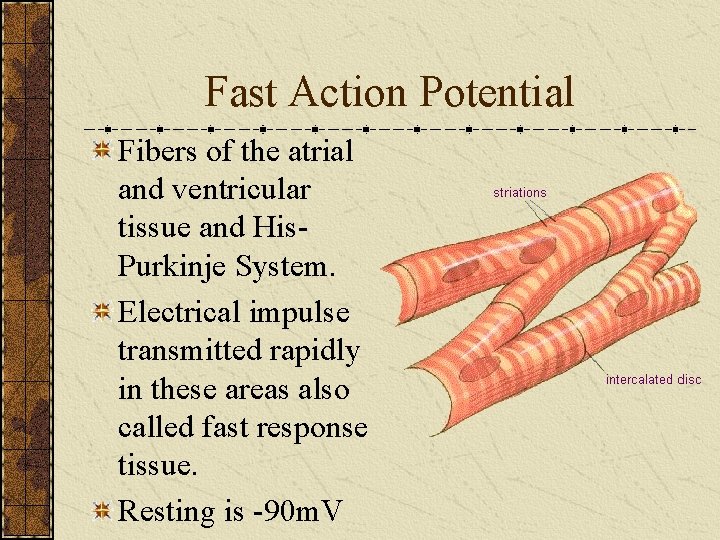
Fast Action Potential Fibers of the atrial and ventricular tissue and His. Purkinje System. Electrical impulse transmitted rapidly in these areas also called fast response tissue. Resting is -90 m. V
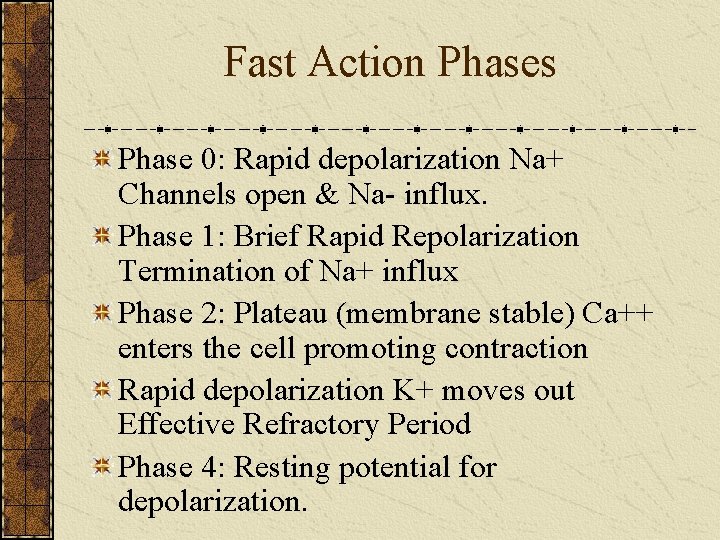
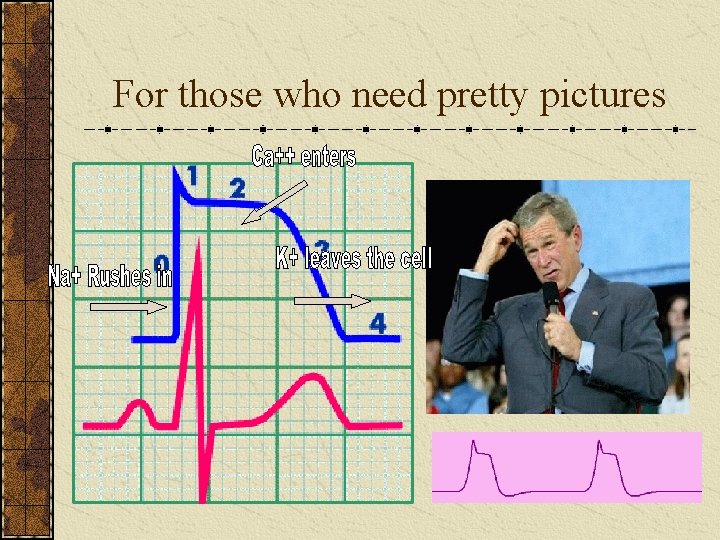
Fast Action Phases Phase 0: Rapid depolarization Na+ Channels open & Na- influx. Phase 1: Brief Rapid Repolarization Termination of Na+ influx Phase 2: Plateau (membrane stable) Ca++ enters the cell promoting contraction Rapid depolarization K+ moves out Effective Refractory Period Phase 4: Resting potential for depolarization.
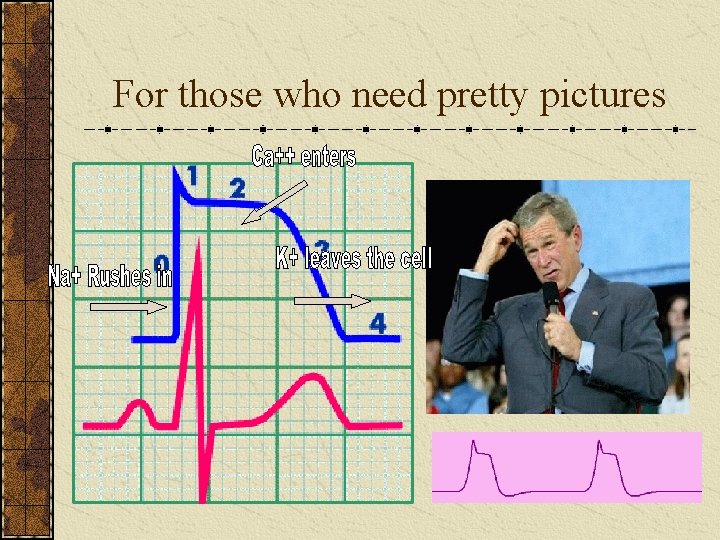
For those who need pretty pictures
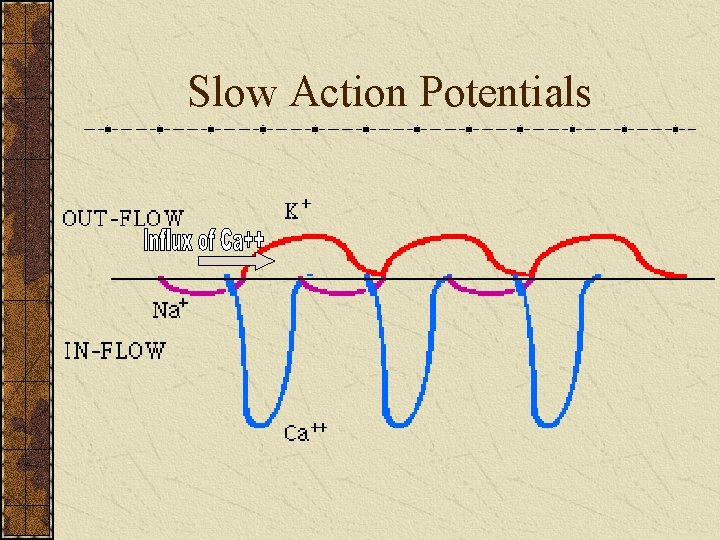
Slow Action Potential Resting is -60 70 m. V Phase 0: Slow depolarization of SA & AV slow influx of Ca++ Phase 1: There is no phase 1 Phase 2: Insignificant in relationship to depolarization Phase 3: Insignificant in relationship to depolarization Phase 4: Spontaneous (rapid) repolarization
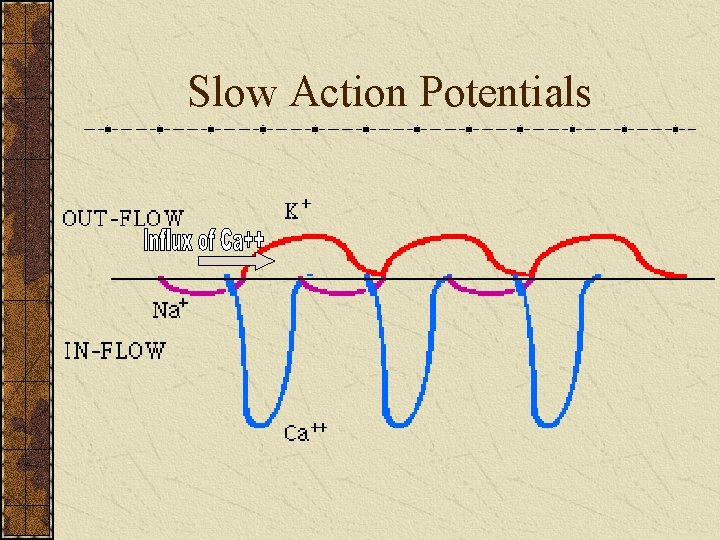
Slow Action Potentials
Pathophysiology Arrhythmias develop for many reasons and are classified in many ways. Primary cause: disturbance with the impulse formation or disturbance in conduction Named according to where the Foci began/originated and whether the rhythm is fast, slow, early, or late.
Some Causes of Arrhythmias Decreased Coronary Profusion (CAD) Impaired Myocardial O 2 Delivery (Hypoxia) Electrical disturbances Cardiac Muscle Injury Ischemia or infarction Defects in the Heart Muscle or Electrical System Cardiac Surgery Electrical Stimulation to the Heart Muscle Medication Wife’s Shopping Bill
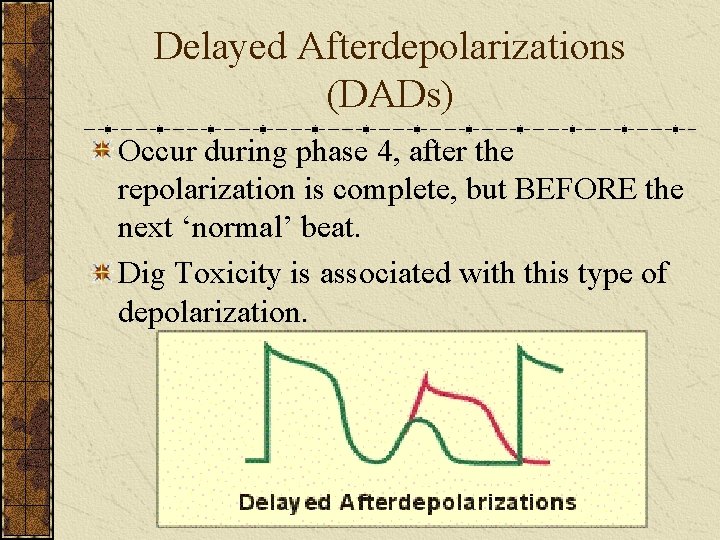
Disturbance with Impulse Formation Abnormal Automaticity: when a cell outside of the normal pathway fires. Happens with ischemia, acidosis, potassium shifts and catecholamine release. Triggered Activity: The initiation of an abnormal depolarization that is ‘triggered’ by a normal depolarization. During repolarization (phase 1 -4) there is an alteration which starts another depolarization (afterdepolarization). There are two types: Early Afterdepolarization and Delayed Afterdepolarizations
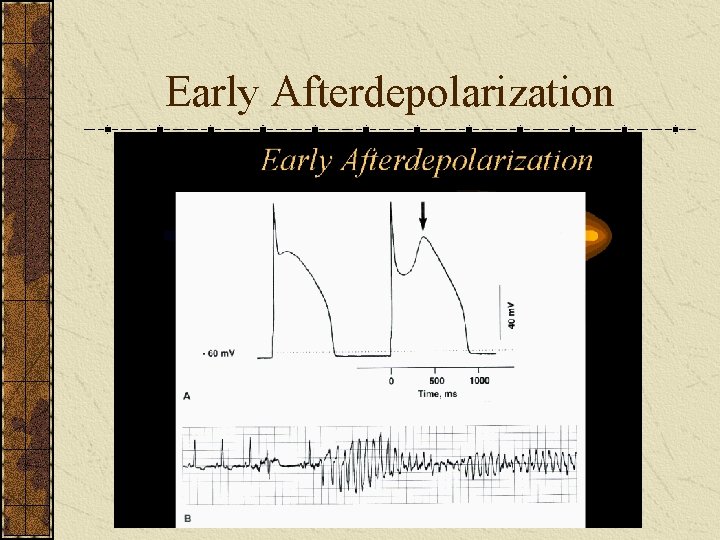
Early Afterdepolarization (EAD) EAD occurs during phase 2 & 3 of the action potential. Causes: Hypoxemia!, ischemia, electrolyte imbalances (Mg+), catecholamines, and antidysrhythmic agents. Results: Polymorphic reentry VT better known as Torsde De Pointes
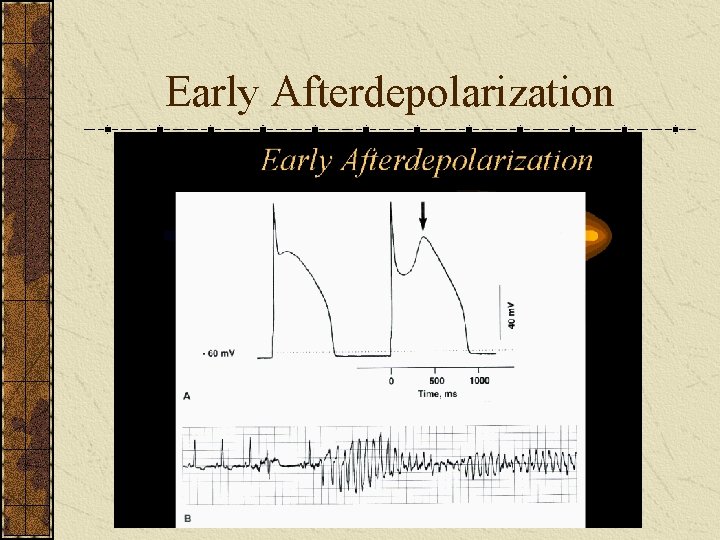
Early Afterdepolarization
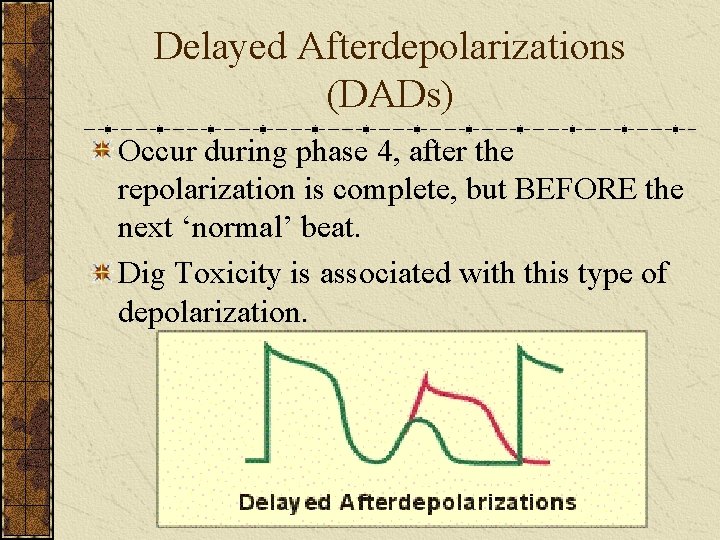
Delayed Afterdepolarizations (DADs) Occur during phase 4, after the repolarization is complete, but BEFORE the next ‘normal’ beat. Dig Toxicity is associated with this type of depolarization.
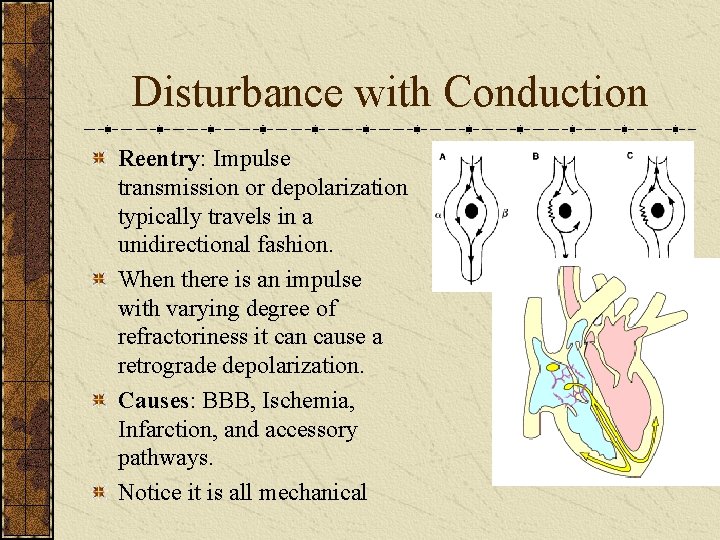
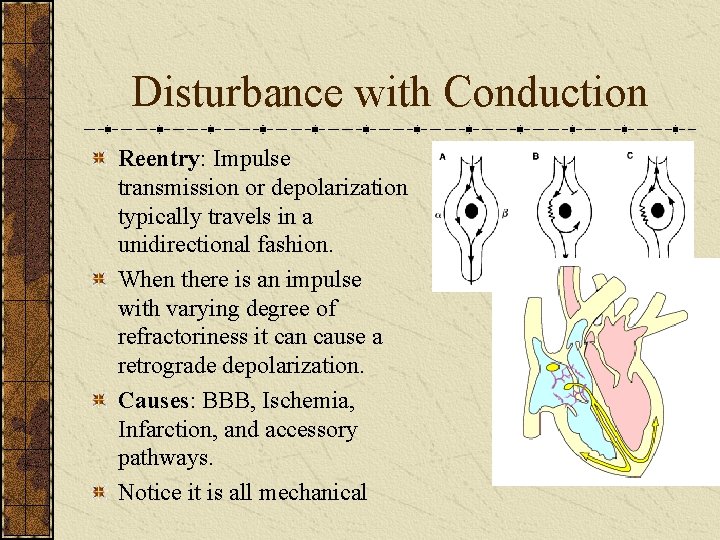
Disturbance with Conduction Reentry: Impulse transmission or depolarization typically travels in a unidirectional fashion. When there is an impulse with varying degree of refractoriness it can cause a retrograde depolarization. Causes: BBB, Ischemia, Infarction, and accessory pathways. Notice it is all mechanical

Atrioventricular Nodal Blocks A slowing or complete disruption in conduction of the impulse between the atria and the ventricle. Cause: Electrical or Anatomical block of the impulse or decreased profusion to the node.
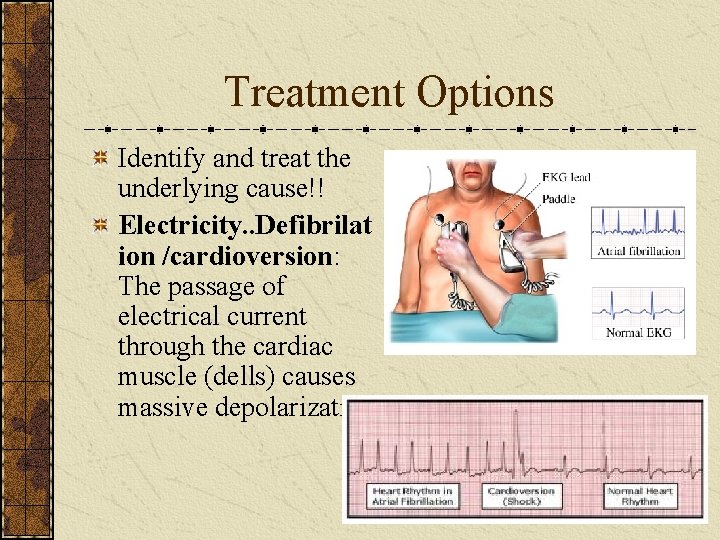
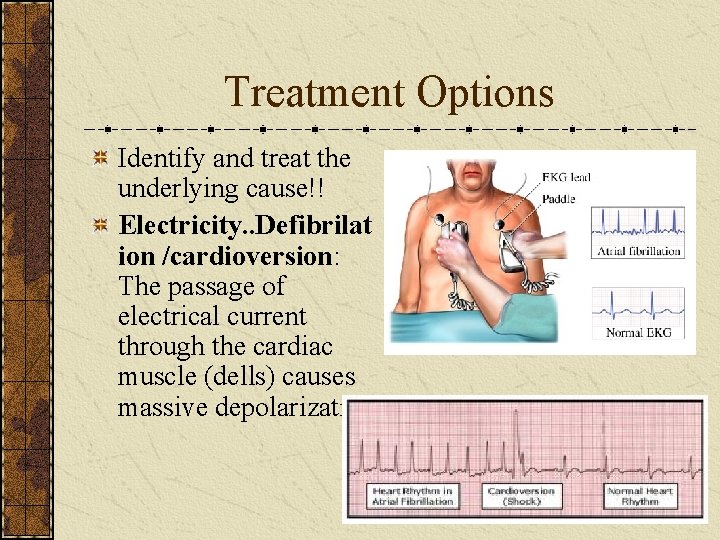
Treatment Options Identify and treat the underlying cause!! Electricity. . Defibrilat ion /cardioversion: The passage of electrical current through the cardiac muscle (dells) causes massive depolarization.
What might get in your way? Transthoracic Impedance: is the resistance to the current (from the defibrillator) from getting to the heart Impedance is determined by: v Chest Size v Presence of Chest Hair v Size of Paddles v The Phase of Ventilation
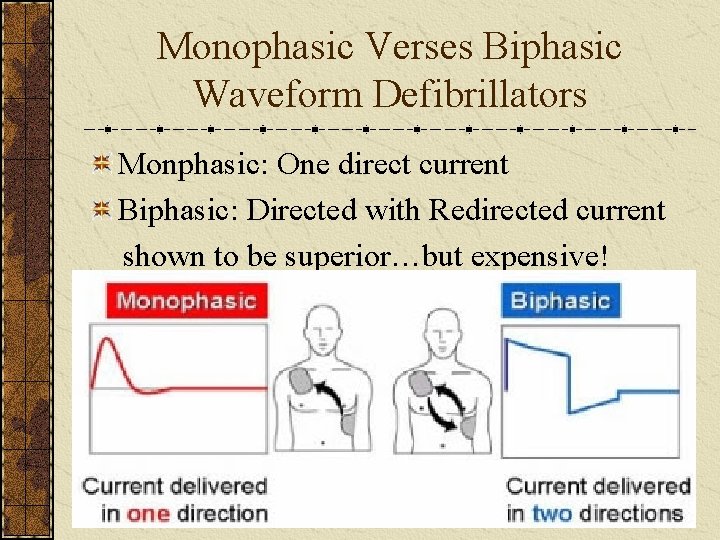
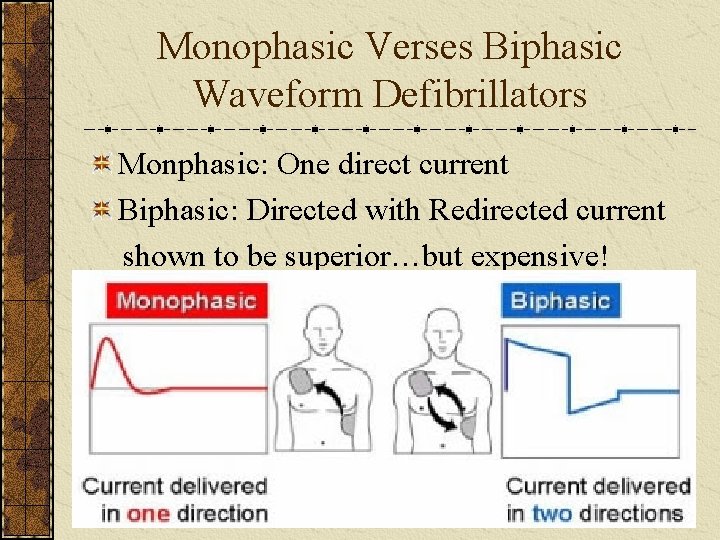
Monophasic Verses Biphasic Waveform Defibrillators Monphasic: One direct current Biphasic: Directed with Redirected current shown to be superior…but expensive!
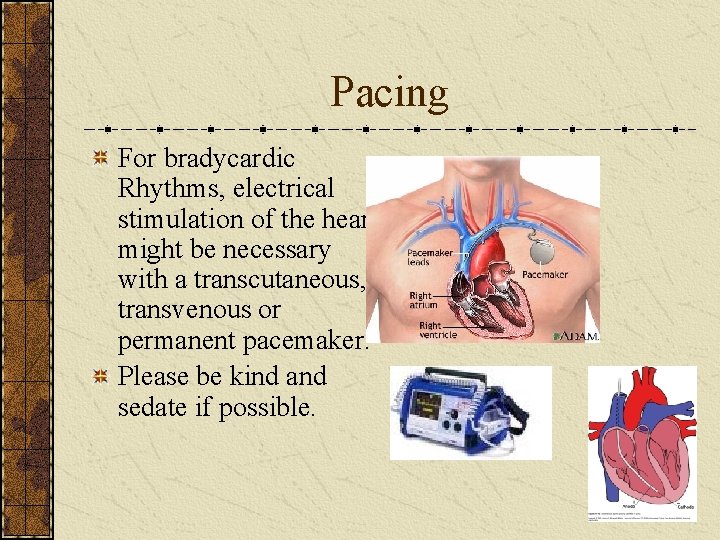
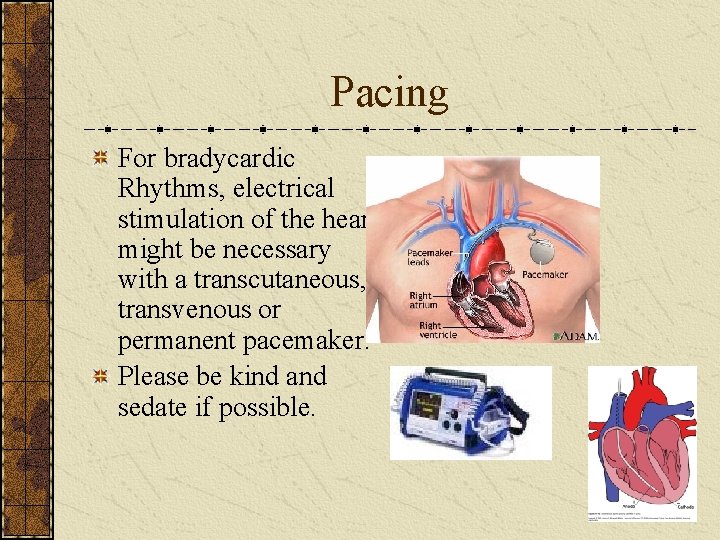
Pacing For bradycardic Rhythms, electrical stimulation of the heart might be necessary with a transcutaneous, transvenous or permanent pacemaker. Please be kind and sedate if possible.
Antidysrhythmic Agents Drugs are SECONDARY to other interventions. Sodium Channel Blockers (slow conduction velocity, negative Inotrope): Procainamide, Lidocaine, Dilantin Beta Blockers (inhibit SNS): Inderal, Esmolol Potassium Channel Blockers (delay repolarization, Prolong Q-T interval): Cordarone, Corvert (SVT) Calcium Channel Blockers (Decrease SA node firing, decrease O 2 demand contractility) Cardizem, Verapamil
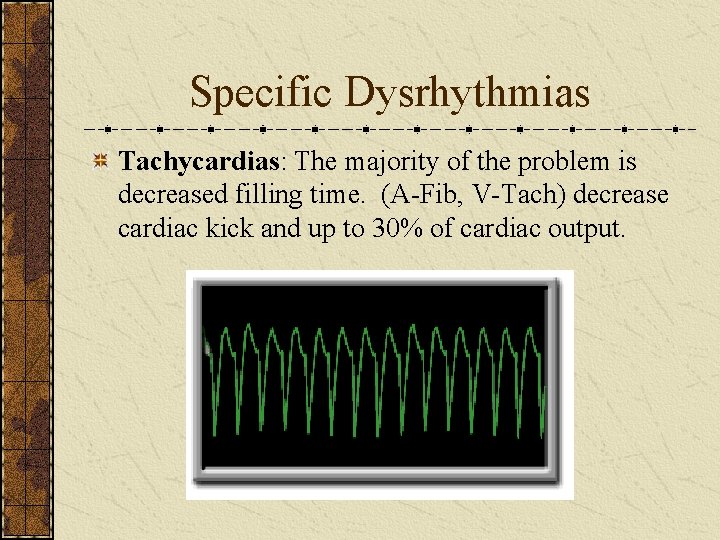
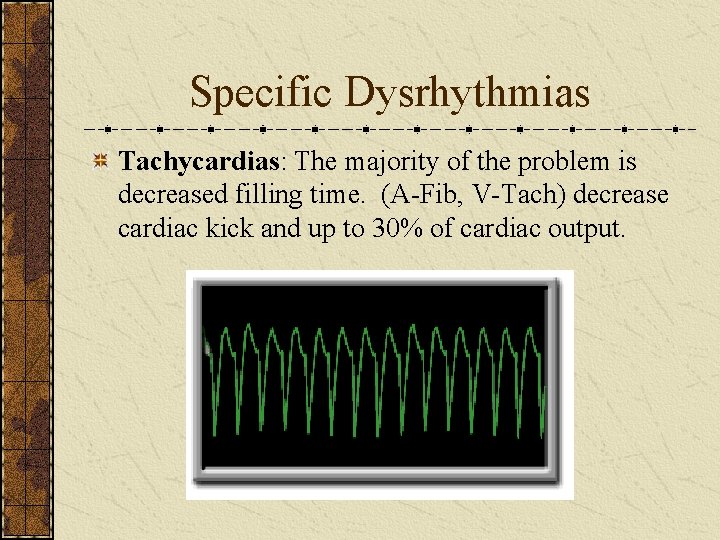
Specific Dysrhythmias Tachycardias: The majority of the problem is decreased filling time. (A-Fib, V-Tach) decrease cardiac kick and up to 30% of cardiac output.
Narrow QRS Complex (SVT) Tachycardias Rhythm: Sinus Tachycardia (ST) A-Fib, A-Flutter Atrial Tachy (reentry) Multifocal Atrial Tachycardia (AT) Junctional Tachycardia (JT) Accessory Pathway-Mediated AT with accessory pathways, AV reentry Tachy.
Treatment (stable) Evaluate Ventricular Function= is the patient stable? A-Fib or AF: The length and time of with rhythm. Consider WPW and LV impairment before determining Tx. v Control rate v Convert Rhythm v Provide Anticoagulation Vagal Stimulation Adenosine PSVT: B-Blockers, Ca++ Channel Blockers, Dig, Antiarrythmics and Cardioversion, If EF <40% Start with cardioversion. JT: B-Blockers, CCB, Amiodorone, NO CARDIOVERSION!! MAT: B-Blockers, CCB, Amiodorone, NO CARDIOVERSION!!
Unstable? IMMEDIATE CARDIOVERSION!! Then open your drug box.
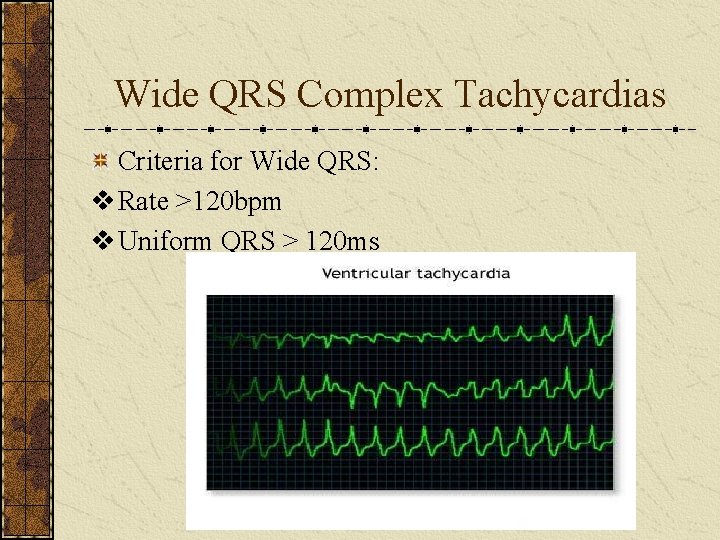
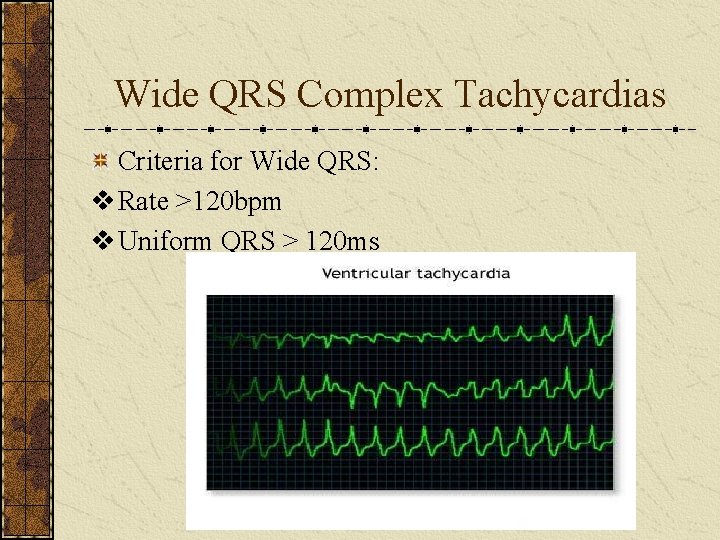
Wide QRS Complex Tachycardias Criteria for Wide QRS: v Rate >120 bpm v Uniform QRS > 120 ms
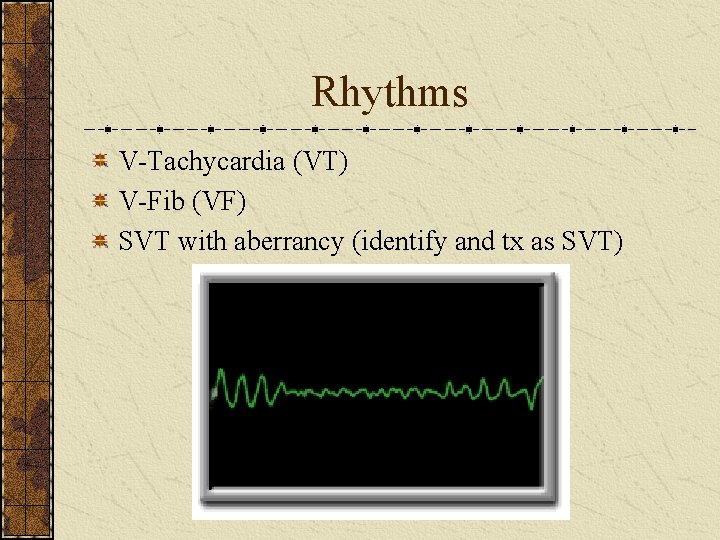
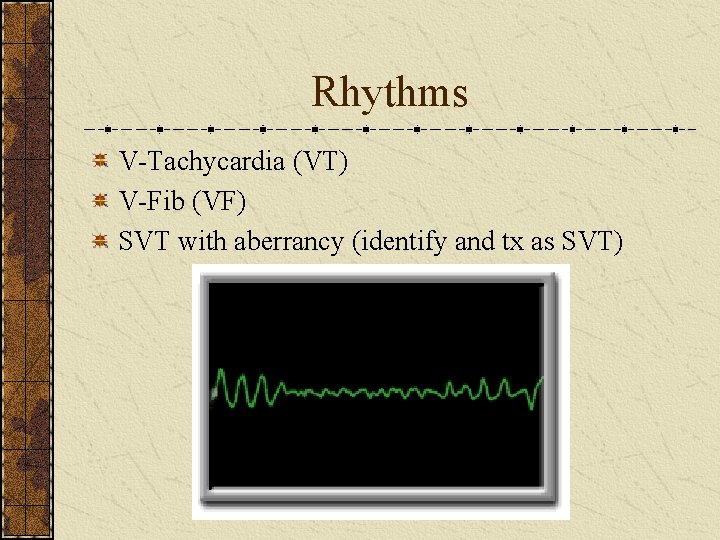
Rhythms V-Tachycardia (VT) V-Fib (VF) SVT with aberrancy (identify and tx as SVT)
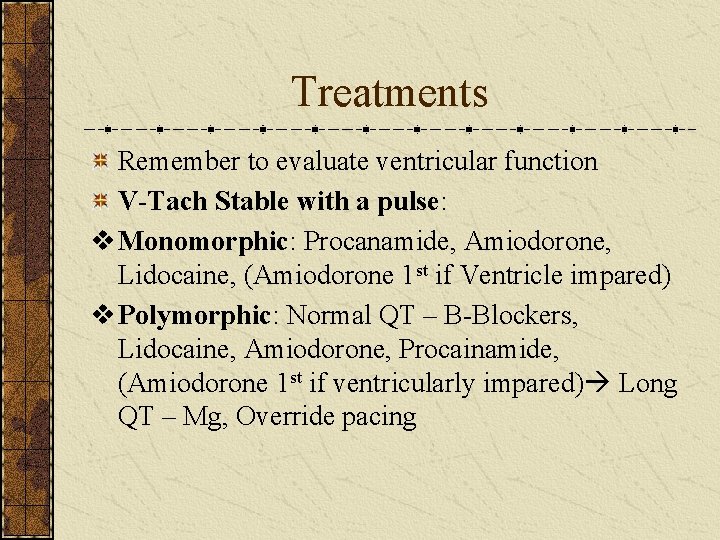
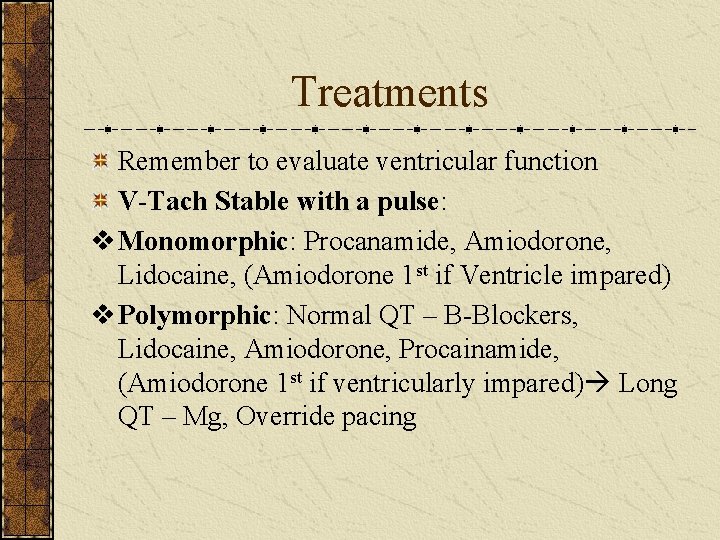
Treatments Remember to evaluate ventricular function V-Tach Stable with a pulse: v Monomorphic: Procanamide, Amiodorone, Lidocaine, (Amiodorone 1 st if Ventricle impared) v Polymorphic: Normal QT – B-Blockers, Lidocaine, Amiodorone, Procainamide, (Amiodorone 1 st if ventricularly impared) Long QT – Mg, Override pacing
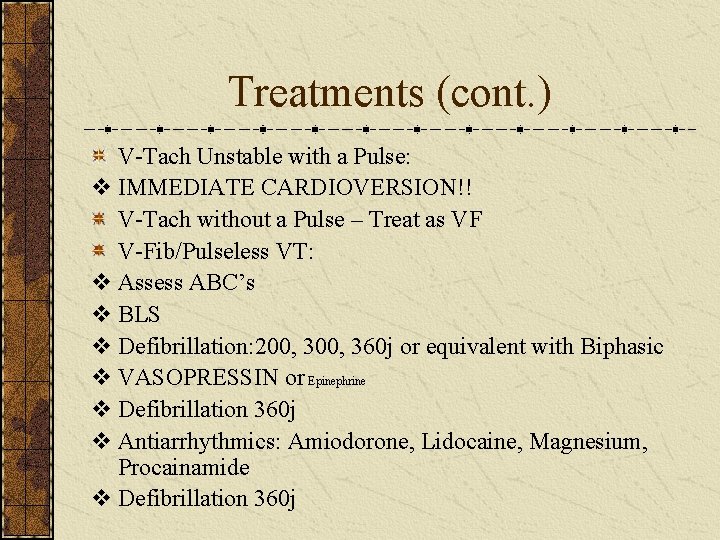
Treatments (cont. ) V-Tach Unstable with a Pulse: v IMMEDIATE CARDIOVERSION!! V-Tach without a Pulse – Treat as VF V-Fib/Pulseless VT: v Assess ABC’s v BLS v Defibrillation: 200, 360 j or equivalent with Biphasic v VASOPRESSIN or Epinephrine v Defibrillation 360 j v Antiarrhythmics: Amiodorone, Lidocaine, Magnesium, Procainamide v Defibrillation 360 j
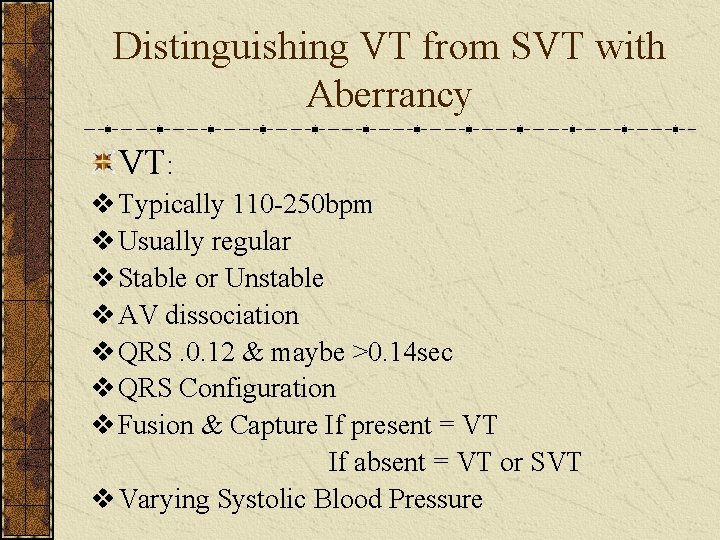
Distinguishing VT from SVT with Aberrancy VT: v Typically 110 -250 bpm v Usually regular v Stable or Unstable v AV dissociation v QRS. 0. 12 & maybe >0. 14 sec v QRS Configuration v Fusion & Capture If present = VT If absent = VT or SVT v Varying Systolic Blood Pressure
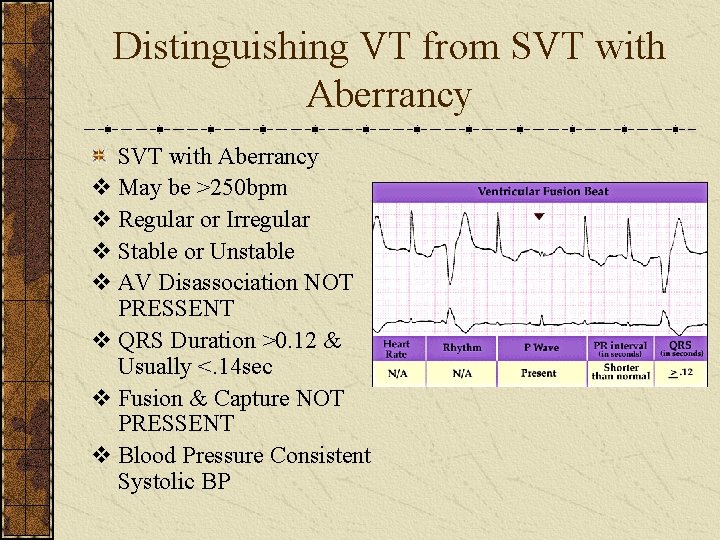
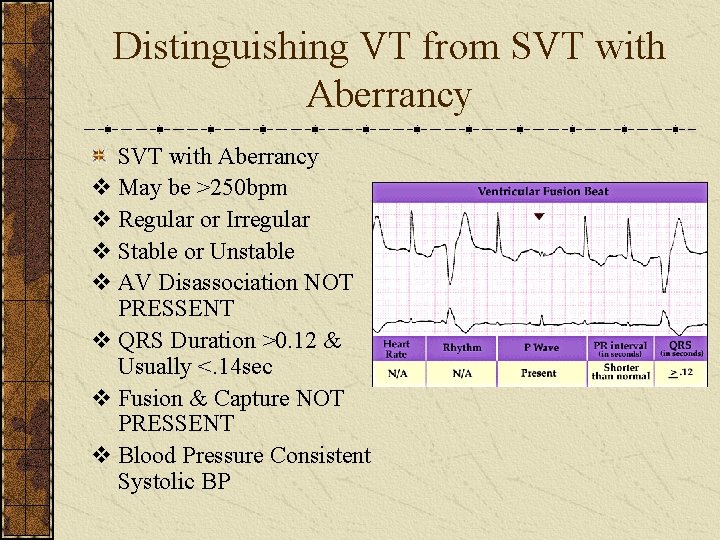
Distinguishing VT from SVT with Aberrancy v May be >250 bpm v Regular or Irregular v Stable or Unstable v AV Disassociation NOT PRESSENT v QRS Duration >0. 12 & Usually <. 14 sec v Fusion & Capture NOT PRESSENT v Blood Pressure Consistent Systolic BP
Other Helpful Tips History or Structural Heart Disease-Likely VT ECG Reflects Old MI-Likely VT Low LV EF-Likely VT Elderly Patients-Likely VT VT occurs More Frequently Than SVT with Aberrancy
Good Rule of Thumb SVT: V 1(usually)has a negative deflection V 6 (usually) has a positive deflection VT: V 1 (usually) has a positive deflection V 6 (usually) has a negative deflection Look at all the other criteria to be sure: P waves, complex with, regularity…etc.
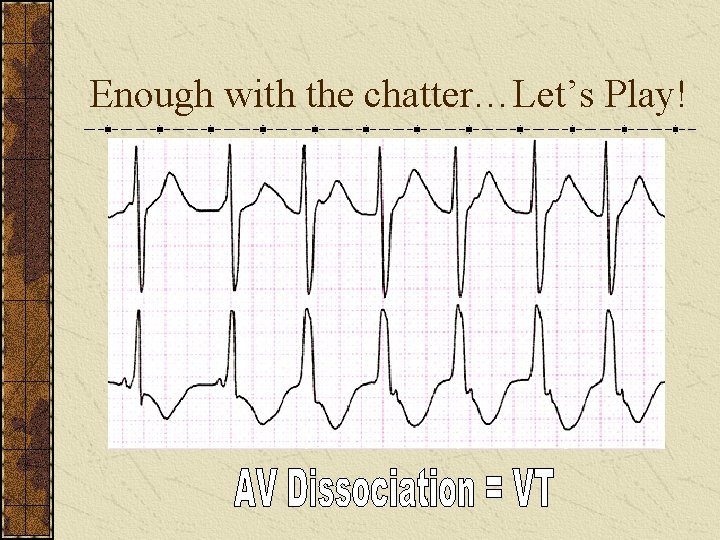
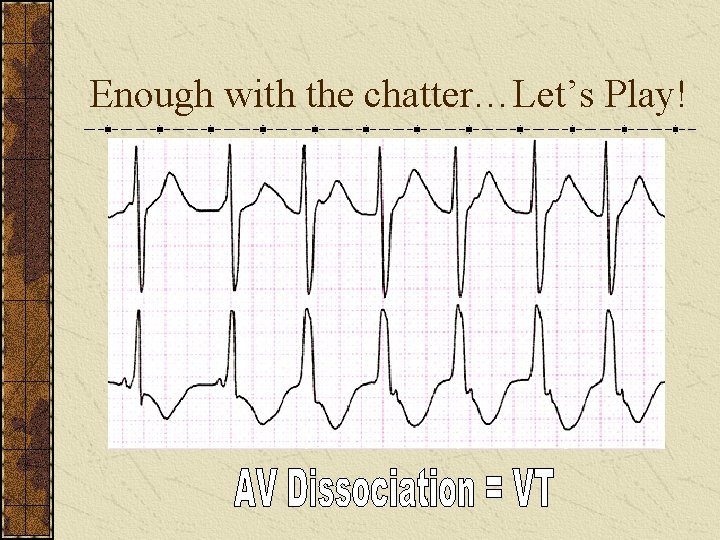
Enough with the chatter…Let’s Play!
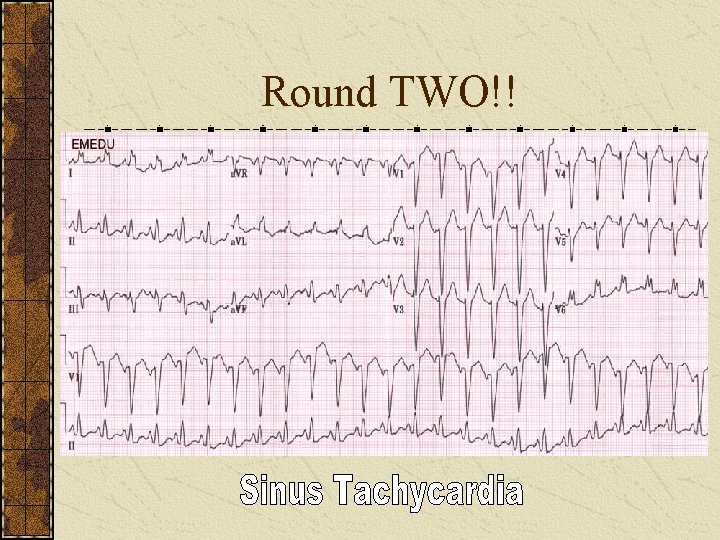
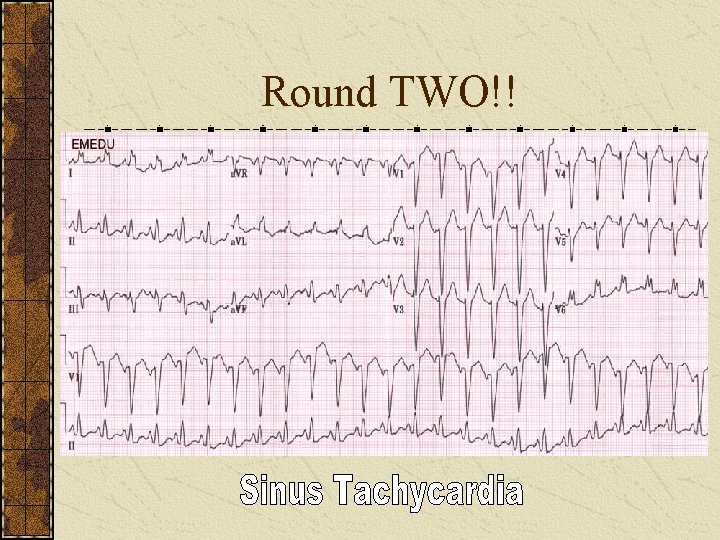
Round TWO!!
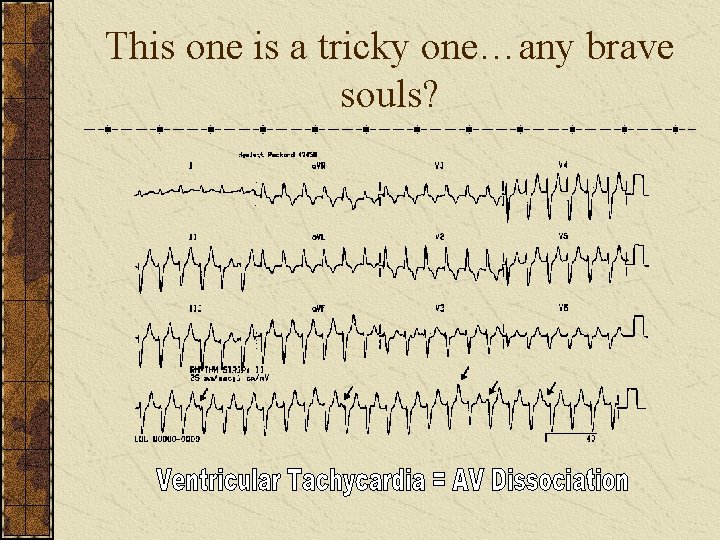
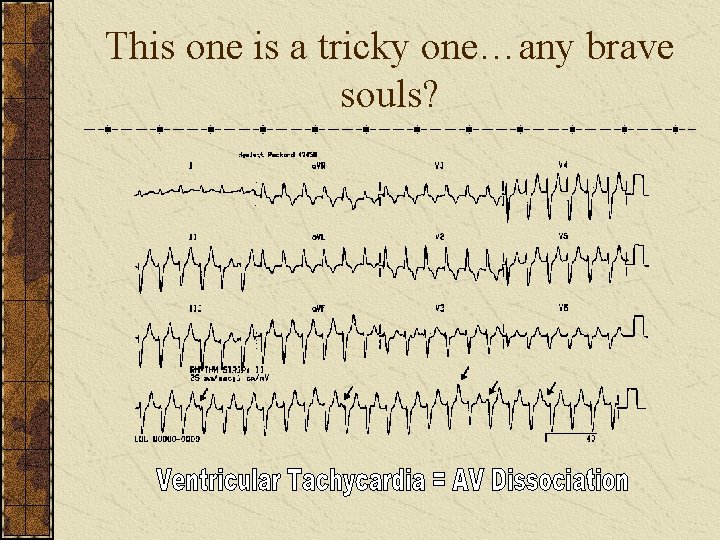
This one is a tricky one…any brave souls?
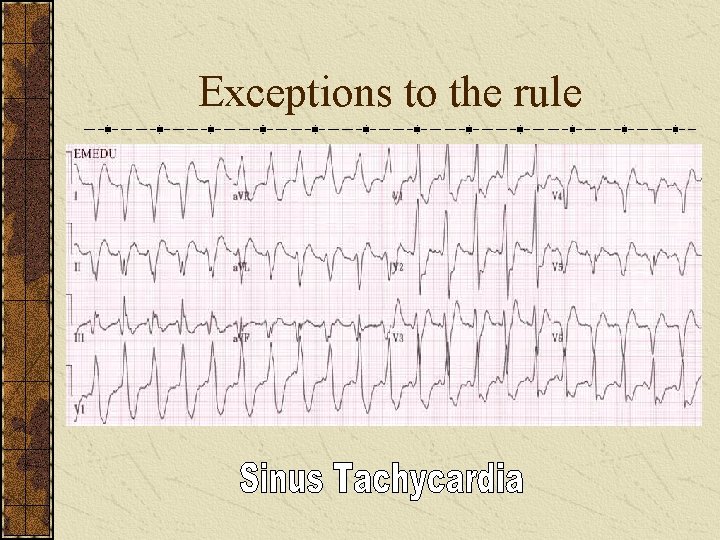
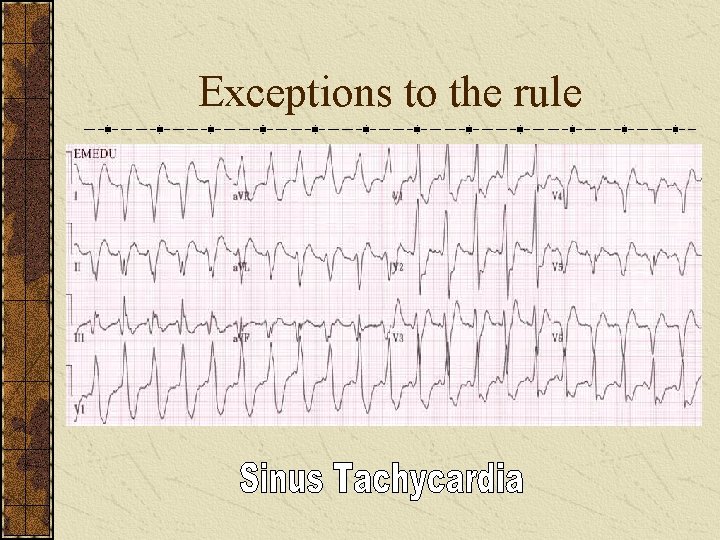
Exceptions to the rule
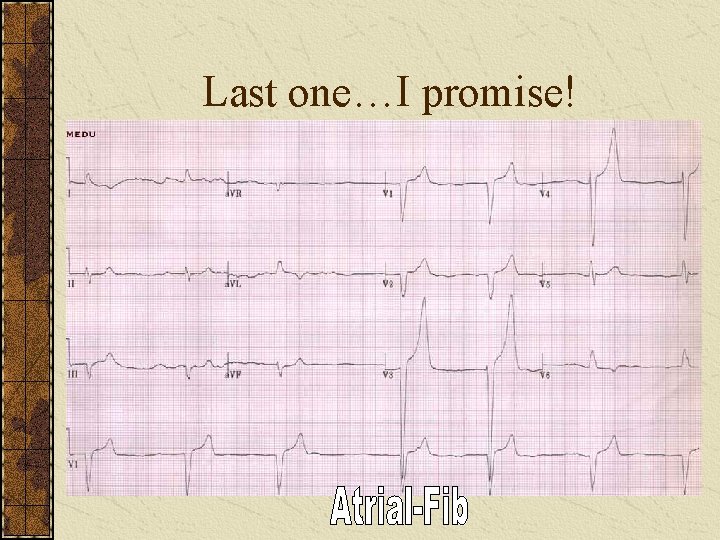
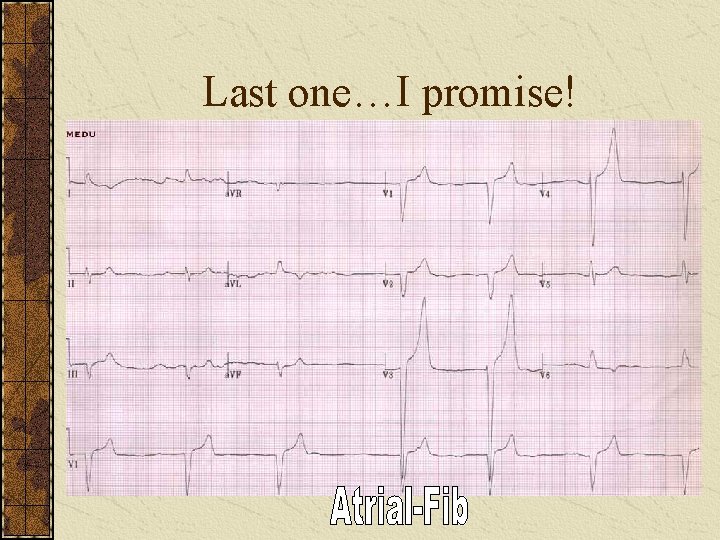
Last one…I promise!
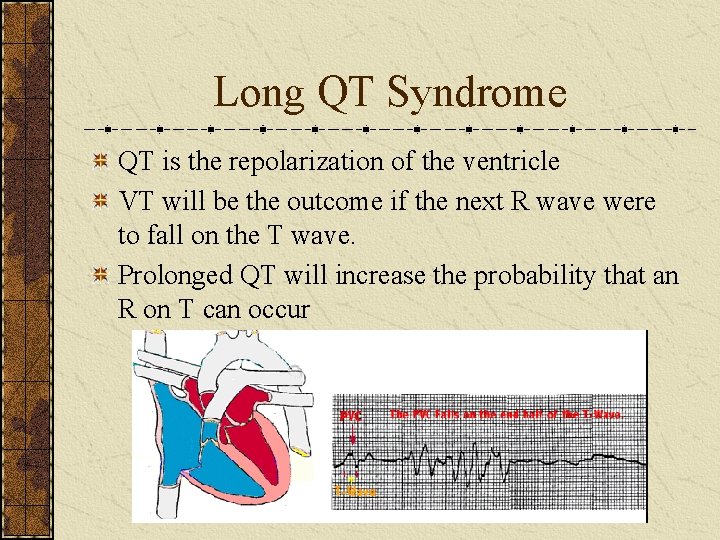
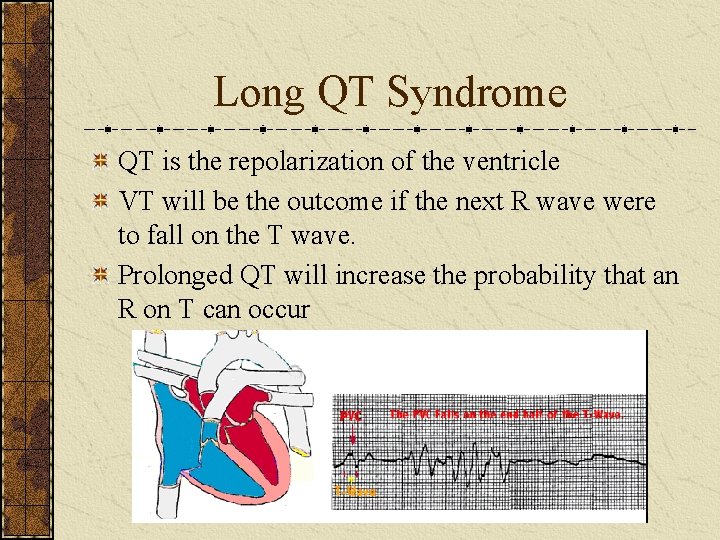
Long QT Syndrome QT is the repolarization of the ventricle VT will be the outcome if the next R wave were to fall on the T wave. Prolonged QT will increase the probability that an R on T can occur
Conditions that Lead to Long QT Syndrome Congenital Long QT Syndrome Exercise Induced QT Syndrome Drug Induced QT Syndrome (Many drugs lenghten QT) v Antiarrhythmics v Tricyclic Antidepressants v Antimicrobials (Erythromycin) v Cardene v Propulsid v Haldol
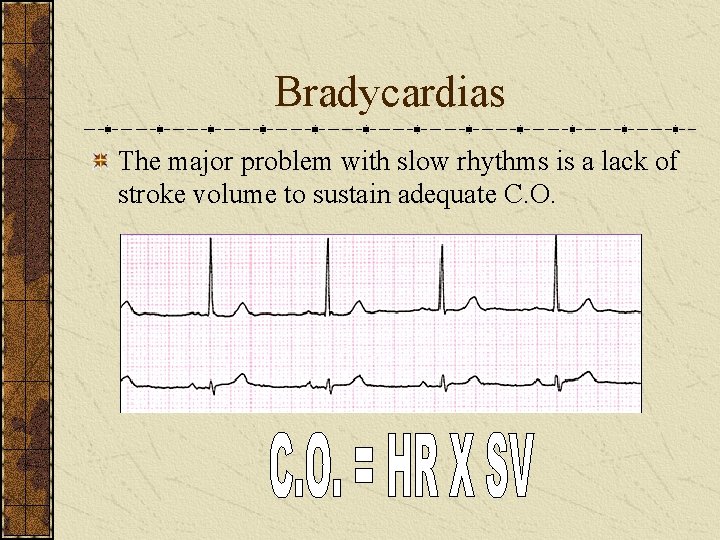
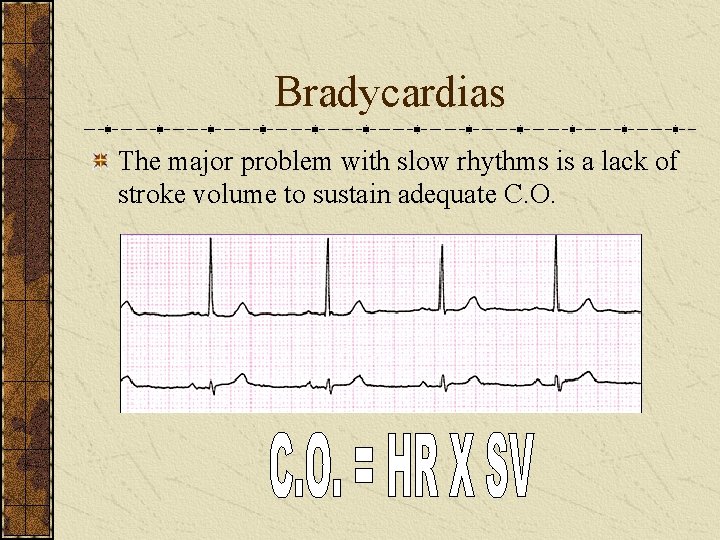
Bradycardias The major problem with slow rhythms is a lack of stroke volume to sustain adequate C. O.
Unstable Patient with Bradycardia ABCs & BLS Atropine Transcutaneous Pacing Dopamine Epinephrine Isoproterenol If the Rhythm is Type II 2 nd Degree or 3 rd Degree HB and the patient is UNSTABLE pace ASAP
Any Questions?
 Wap rhythm
Wap rhythm What is non threatening body language
What is non threatening body language Sociology chapter 7
Sociology chapter 7 Face goffman
Face goffman Non threatening body language
Non threatening body language What is non threatening body language
What is non threatening body language Examples of deviance in society
Examples of deviance in society Fie fie unknit that threatening unkind brow
Fie fie unknit that threatening unkind brow City and country life vocabulary
City and country life vocabulary Farm life vs city life
Farm life vs city life Real life application of factoring polynomials
Real life application of factoring polynomials Single life vs married life debate
Single life vs married life debate Difference between life skills and life orientation
Difference between life skills and life orientation Country life vs city life compare /contrast
Country life vs city life compare /contrast City life vs country life
City life vs country life What is the lesson of life of pi
What is the lesson of life of pi Boundaries meme
Boundaries meme The life that is truly life
The life that is truly life The idea life comes from life is
The idea life comes from life is Unit 8 country life and city life
Unit 8 country life and city life Your online life, permanent as a tattoo
Your online life, permanent as a tattoo You light up my life lab
You light up my life lab What is virtue ethics
What is virtue ethics Piecewise function example in real life
Piecewise function example in real life Eternal cycle of life
Eternal cycle of life Workshop worklife balance
Workshop worklife balance Wolverine's life cycle
Wolverine's life cycle Early life of william wordsworth
Early life of william wordsworth William shakespeare timeline
William shakespeare timeline When and where was shakespeare born
When and where was shakespeare born Non domesticated animals and uncultivated plant life
Non domesticated animals and uncultivated plant life When life kicks you let it kick you forward
When life kicks you let it kick you forward Life cycle of blowfly
Life cycle of blowfly What are the three major watersheds in virginia
What are the three major watersheds in virginia Cezanne still life
Cezanne still life Distribution life cycle
Distribution life cycle What drives you in life
What drives you in life Whats the opposite of a mammal
Whats the opposite of a mammal Iogp lsr
Iogp lsr Live your whole life virgin pulse
Live your whole life virgin pulse Awjm
Awjm The elixir of life by cv raman
The elixir of life by cv raman Easy topic about life
Easy topic about life Roles in your life
Roles in your life Trig functions in real life
Trig functions in real life Life career rainbow
Life career rainbow Half life formula
Half life formula